Table of Contents
Definition / general | Essential features | Terminology | Etiology | Clinical features | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Baardsen EM, Rosa M. Radiation atypia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/cervixradiationatypia.html. Accessed March 30th, 2025.
Definition / general
- Radiation can lead to cytologic features affecting any organ following radiotherapy (commonly those of the female reproductive, GI and GU tracts), which may be mistaken for neoplastic or preneoplastic conditions
- Cervical changes due to radiation are discussed below
Essential features
- Characteristic changes affect both squamous and glandular epithelial cells and include marked cellular and nuclear enlargement with preservation of nuclear to cytoplasmic (N:C) ratio, cytoplasmic vacuolization and cytoplasmic polychromasia
- Cytopathic effects may diminish but can persist many years
Terminology
- Reactive cellular changes associated with radiation
- Radiation changes
- Radiation atypia
Etiology
- Radiation therapy induces a wide spectrum of DNA changes, including nuclear base damage, single and double strand breaks and DNA crosslinks
- Affected cells undergo DNA repair, which may result in restoring cell function or transmitting these abnormalities to the descendent cells
Clinical features
- Clinical history is important
- Patients range in age from 34 to 68 years of age and received at least 36 Gy total dosage directed to the pelvis (Int J Gynecol Pathol 1996;15:242)
- May show ulceration shortly after radiation therapy
- Stenosis, especially of the endocervix, may develop weeks to as long as 17.5 years after completion of radiotherapy (Int J Gynecol Pathol 1996;15:242)
Gross description
- Possible surface irregularity but may show no abnormality (Int J Gynecol Pathol 1996;15:242)
- Irregularities may include fibrosis and induration
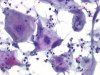
Microscopic (histologic) description
- Mucosa tends to be thin, friable and atrophic (Int J Gynecol Pathol 1996;15:242, Diagn Cytopathol 1995;13:107)
- Fibrosis and hyalinization of stroma with occasional atypical fibroblasts (Int J Gynecol Pathol 1996;15:242, Diagn Cytopathol 1995;13:107)
- Prominent cellular changes affecting both squamous and glandular epithelial cells may include nuclear enlargement and hyperchromasia associated with abundant cytoplasm, uniform nuclear spacing with minimal crowding, low mitotic index and cytoplasmic degeneration with vacuoles (Int J Gynecol Pathol 1996;15:242, Diagn Cytopathol 1995;13:107)
- Nuclear chromatin is often indistinct or smudged (Int J Gynecol Pathol 1996;15:242)
- Low nuclear to cytoplasmic (N:C) ratio
- Inflammation, including multinucleated giant cells / histiocytes (Diagn Cytopathol 1995;13:107)
- Irregular, ectatic vessels may be present (South Asian J Cancer 2014;3:159)
Microscopic (histologic) images
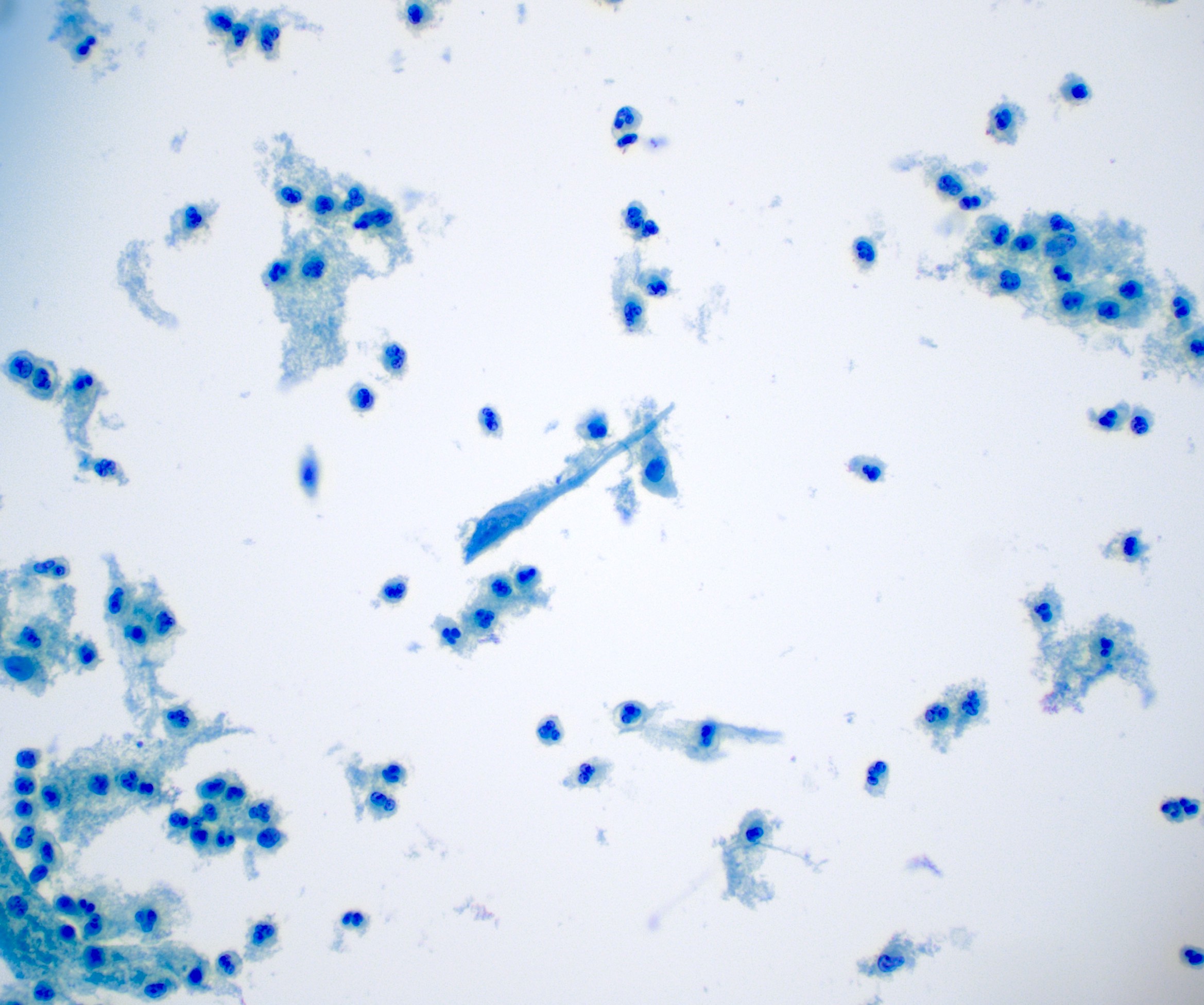
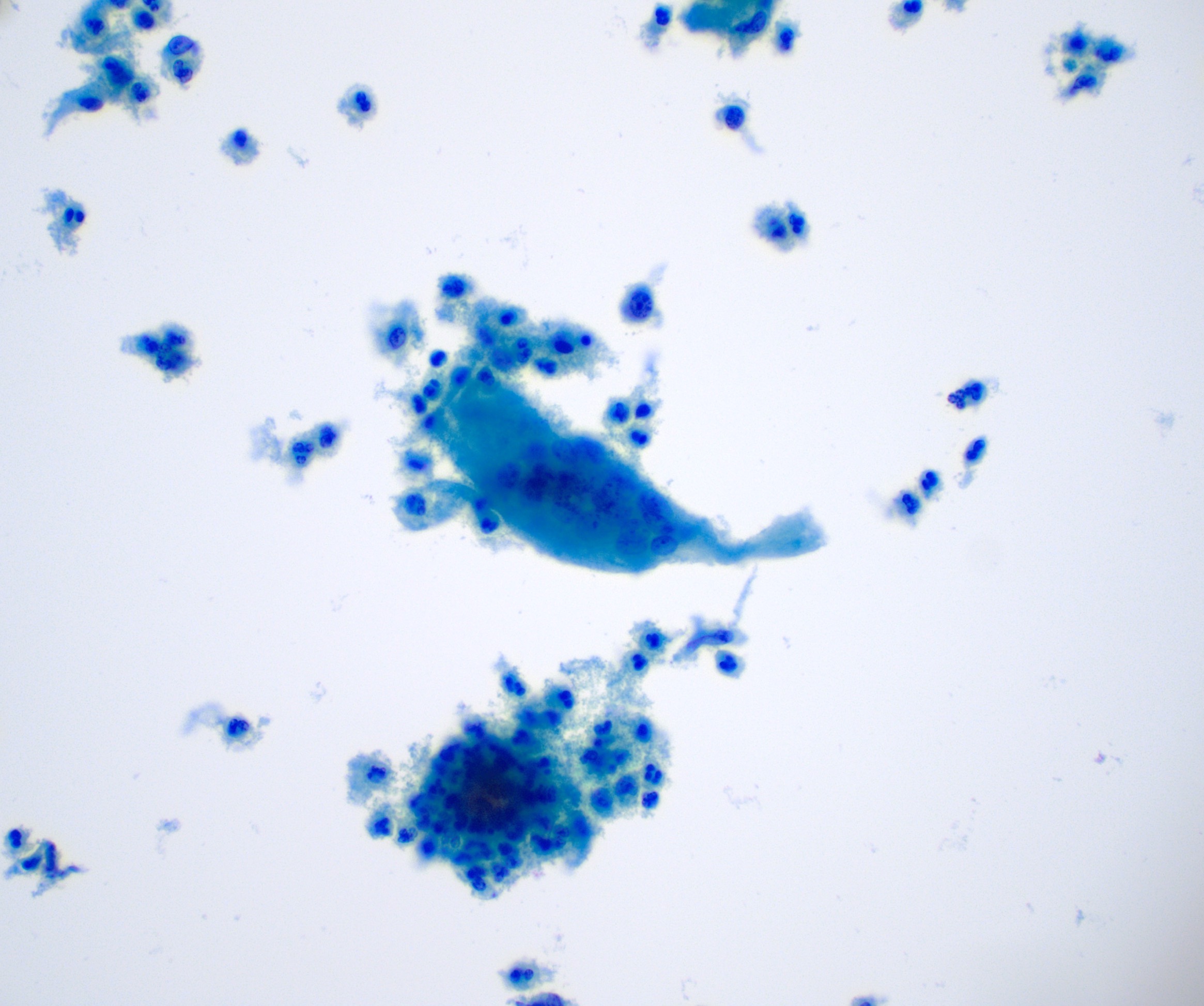
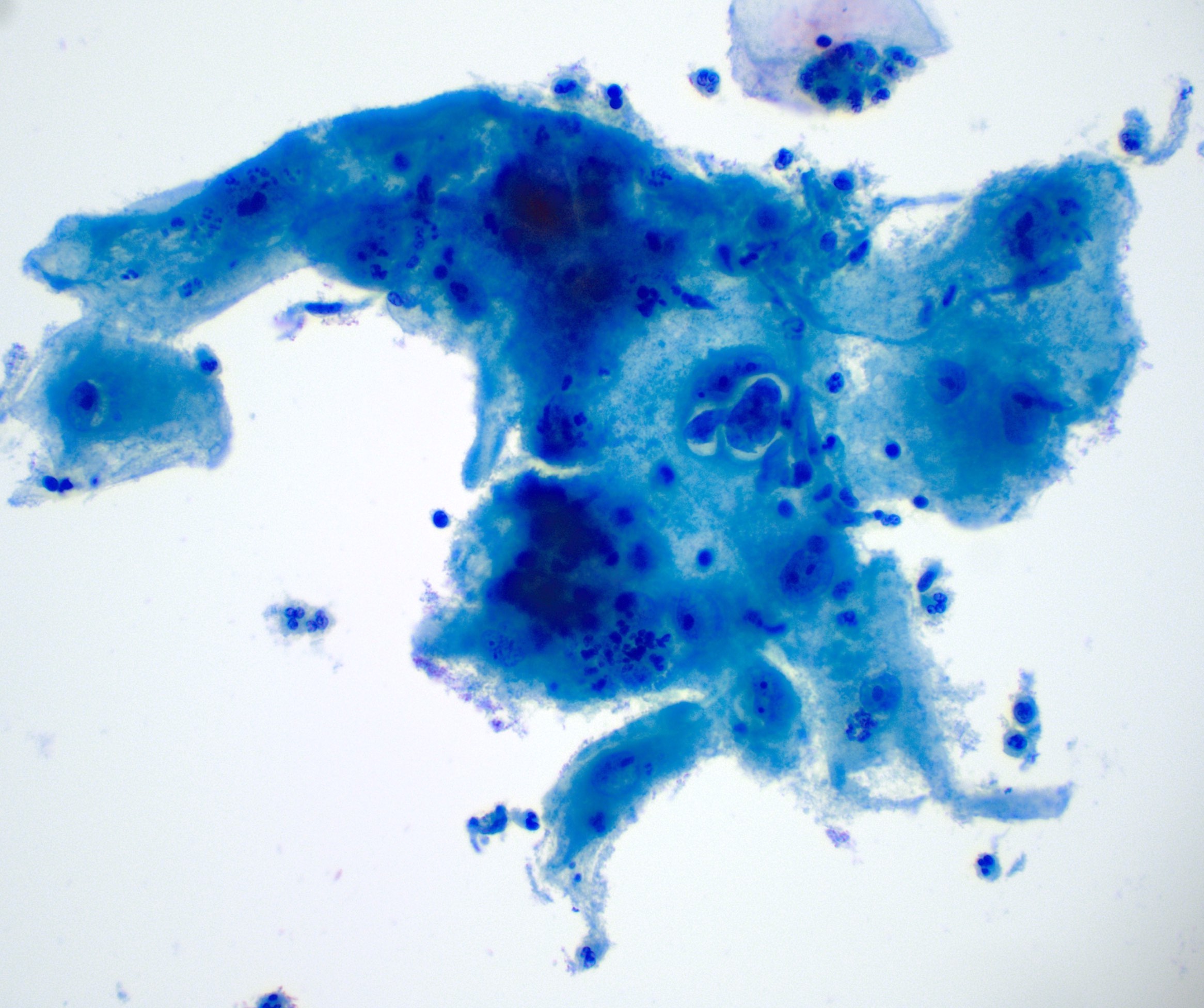
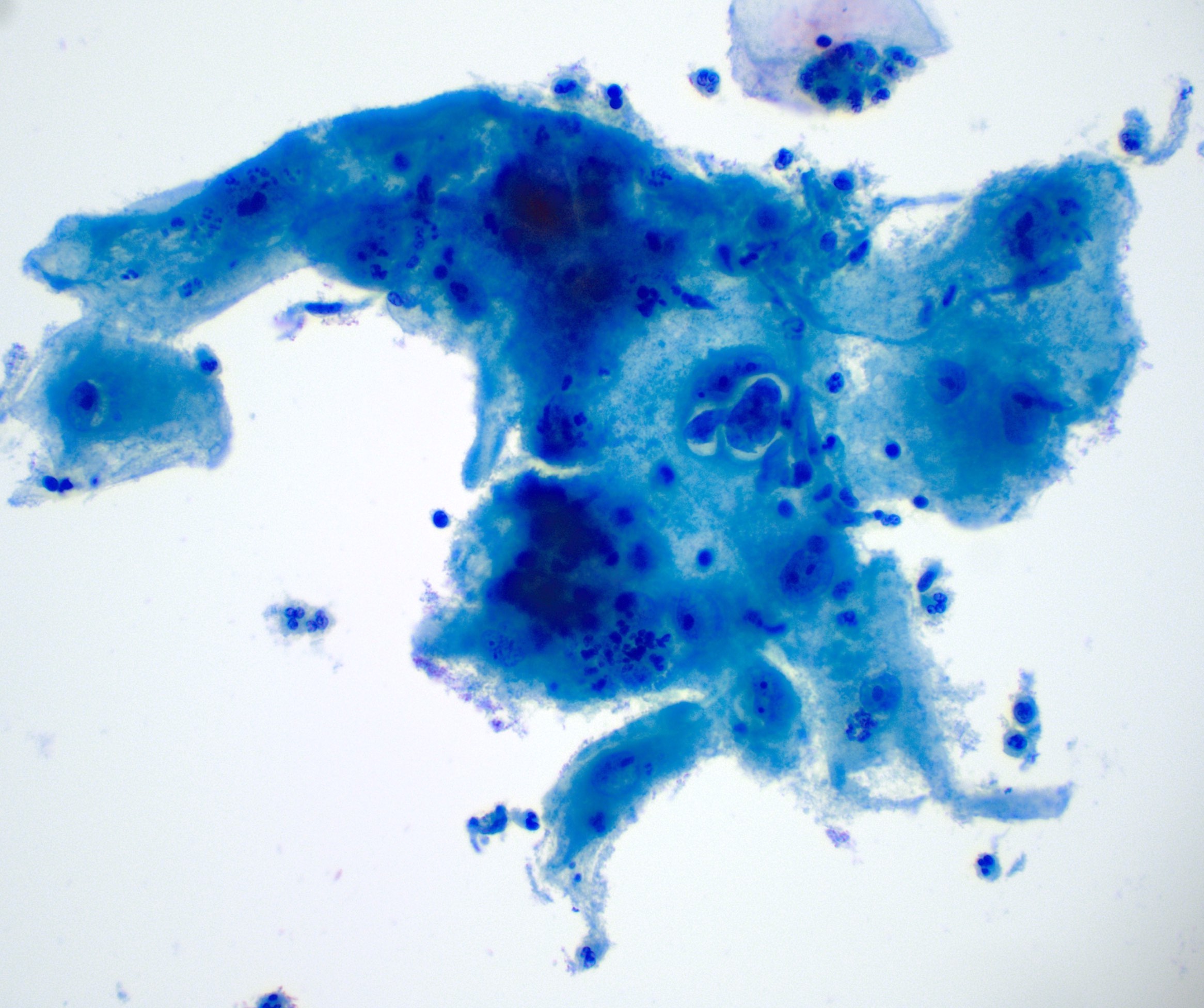
Cytology description
- Large, bizarre cells with nuclear enlargement (cytomegaly and karyomegaly) (Diagn Cytopathol 1990;6:243)
- Normal nuclear to cytoplasmic (N:C) ratio
- Smudgy or finely granular chromatin
- Prominent nucleoli
- Cytoplasmic vacuolization and polychromasia ("two tone" cytoplasm) (Diagn Cytopathol 1990;6:243)
- Binucleation or multinucleation is common
- Enlarged nuclei may show degenerative changes, including nuclear pallor, wrinkling or smudging of the chromatin and nuclear vacuolization
- "Clean" background comprised of inflammatory cells and occasionally endothelial cells (Nayar: The Bethesda System for Reporting Cervical Cytology, 3rd Edition, 2015)
Cytology images
Positive stains
- CEA expressed in scattered cells (Int J Gynecol Pathol 1996;15:242, Acta Cytol 1992;36:305)
Negative stains
Molecular / cytogenetics description
- Negative for HPV (in situ hybridization)
Sample pathology report
- Cytology specimen:
- Specimen type: Liquid based preparation.
- Specimen adequacy: Satisfactory for evaluation. Endocervical / transformation zone component present.
- Interpretation / result: Negative for intraepithelial lesion or malignancy. Reactive cellular changes associated with radiation.
- Surgical specimen:
- Uterine cervix, biopsy:
- Squamous mucosa with moderate acute inflammation and reactive changes consistent with prior radiation therapy
- Endocervical epithelium with no significant histopathologic findings
- Negative for dysplasia and negative for malignancy
- Uterine cervix, biopsy:
Differential diagnosis
- Viral infection, such as herpes simplex virus:
- Ground glass nuclear appearance and Cowdry type A inclusions
- Recurrent squamous cell carcinoma or adenocarcinoma:
- Cells are typically more numerous, more nuclear atypia with coarsely textured chromatin and mitotic activity, invasion is present
- Low grade squamous intraepithelial lesion (LSIL):
- Characteristic koilocytes with cytoplasmic halos / cavities
- Atypical glandular cells and adenocarcinoma in situ:
- Cells should display nuclear atypia that exceeds that of reactive or reparative changes
- Generally specimens will be more cellular with many hyperchromatic crowded clusters and three dimensional sheets / strips with feathering and rosette formation
- Nuclear crowding / overlapping, hyperchromasia and increased N:C ratios can be seen (features not typically associated with radiation atypia)
- p16 will be diffusely positive (negative in radiation atypia)
Additional references
Board review style question #1
A 69 year old woman with a remote history of cervical adenocarcinoma presents with chief complaint of pelvic pain. On pelvic exam, the clinician notes nodularity of the vaginal cuff. A vaginal Pap smear is performed and shows rare atypical cells with large pleomorphic nuclei, prominent nucleoli and abundant vacuolated polychromatic cytoplasm. The remainder of the specimen is comprised of scattered squamous cells of varying maturation and inflammation. Which is the most likely diagnosis?
- Adenocarcinoma
- Atypical glandular cells of undetermined significance (AGUS)
- Glandular cells status posthysterectomy
- Reactive cellular changes associated with radiation
- Squamous cell carcinoma
Board review style answer #1
D. Reactive cellular changes associated with radiation
Invasive cervical adenocarcinoma is typically treated with simple or radical hysterectomy with radiation therapy or chemotherapy. It is assumed this patient received standard treatment, including radiation therapy. The cytologic features described are most representative of cellular changes seen after radiation therapy, which may persist for many years. Additionally, the background reflects a nonneoplastic process, further supporting the diagnosis.
Comment Here
Reference: Radiation atypia
Invasive cervical adenocarcinoma is typically treated with simple or radical hysterectomy with radiation therapy or chemotherapy. It is assumed this patient received standard treatment, including radiation therapy. The cytologic features described are most representative of cellular changes seen after radiation therapy, which may persist for many years. Additionally, the background reflects a nonneoplastic process, further supporting the diagnosis.
Comment Here
Reference: Radiation atypia
Board review style question #2
Which of the following is the appropriate management of this lesion seen on cervical Pap smear from a 32 year old woman?
- Colposcopy with endocervical sampling
- Immediate loop electrosurgical excision (LEEP)
- No HPV testing should be performed; routine screening with Pap smear only at 1 year
- Observation with colposcopy and cytology at 6 month intervals for 12 months
- Perform HPV cotesting; if negative, repeat cotesting at 5 years
Board review style answer #2
E. Perform HPV cotesting; if negative, repeat cotesting in 5 years
In the absence of an intraepithelial lesion or malignancy (NILM), reactive cellular changes associated with radiation (radiation atypia) should be managed according to the American Society for Colposcopy and Cervical Pathology (ASCCP) Consensus Guidelines. Per the Cytology NILM algorithm, women 30 years and older with negative cytology should undergo HPV cotesting (preferred):
Comment Here
Reference: Radiation atypia
In the absence of an intraepithelial lesion or malignancy (NILM), reactive cellular changes associated with radiation (radiation atypia) should be managed according to the American Society for Colposcopy and Cervical Pathology (ASCCP) Consensus Guidelines. Per the Cytology NILM algorithm, women 30 years and older with negative cytology should undergo HPV cotesting (preferred):
- If negative, continue routine screening (cotesting at 5 years or cytology alone at 3 years)
- If positive, repeat cotesting at 1 year or genotyping is indicated
- If HPV status is unknown / cannot be performed, repeat cytology at 3 years
Comment Here
Reference: Radiation atypia