Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1Cite this page: Metcalf BD, Chapel DB. Primary endometrioid adenocarcinoma (HPV independent). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/cervixprimaryendoadeno.html. Accessed March 31st, 2025.
Definition / general
- Rare, human papillomavirus (HPV) independent subtype of cervical adenocarcinoma, histologically indistinguishable from endometrioid adenocarcinoma of the endometrium or ovary
Essential features
- Usually low grade (predominantly gland forming) or rarely high grade (predominantly solid) endometrioid morphology according to the FIGO grading system
- Cervical involvement by endometrial endometrioid carcinoma is more common than primary cervical endometrioid carcinoma and must be excluded by clinical, radiographic and pathological correlation
- HPV independent: lacks conspicuous apical mitoses and basal apoptotic bodies on scanning magnification; negative to patchy p16 and negative high risk HPV assays
- Often but not always associated with endometriosis
Terminology
- Endometrioid adenocarcinoma of the uterine cervix
- Rare cases may be deemed minimal deviation endometrioid adenocarcinoma of the cervix, though precise diagnostic criteria for this designation are lacking (Am J Surg Pathol 1993;17:660)
- The International Endocervical Adenocarcinoma Criteria and Classification (IECC, published in 2018) more strictly codified cervical endometrioid carcinoma as an HPV independent tumor; previously, much of what had been called cervical endometrioid carcinoma was mucin depleted, HPV associated usual type endocervical adenocarcinoma with endometrioid carcinoma-like morphologic features (Am J Surg Pathol 2018;42:214)
ICD coding
Epidemiology
- In IECC cohort, endometrioid carcinoma accounts for 1.1% of primary endocervical adenocarcinomas (Gynecol Oncol Rep 2020;32:100579, Am J Surg Pathol 2018;42:214)
- Data published prior to 2018 IECC are unreliable, as they often include a high proportion of mucin depleted, HPV associated usual type endocervical adenocarcinomas with endometrioid carcinoma-like morphology
Sites
- Cervix
Pathophysiology
- Associated with and apparently arises from endometriosis in many cases (Histopathology 2020;76:112, Pathol Res Pract 2023;245:154452)
- Tuboendometrioid metaplasia has been hypothesized as an alternate precursor, though supporting data are absent (Am J Surg Pathol 1993;17:660, Pathol Res Pract 2024;254:155062)
Diagnosis
- May present with vaginal bleeding (Virchows Arch 2019;475:537)
- May be detected on cervical cancer screening in asymptomatic patients
- Diagnosis is primarily by characteristic endometrioid histomorphology
- Characteristic endometrioid immunoprofile is supportive
- Clinical, radiologic and pathological correlation are essential to exclude cervical spread of a primary endometrial neoplasm; if feasible, it may be prudent to submit the entire endometrium for histologic examination prior to rendering a diagnosis of primary cervical endometrioid adenocarcinoma (Pathology 2021;53:568)
- p16 immunohistochemistry or high risk HPV in situ hybridization is recommended to confirm absence of HPV (Histopathology 2020;76:112)
Radiology description
- Magnetic resonance imaging (MRI) may help distinguish endometrial versus cervical primary site (Eur J Radiol 2020;130:109190, J Obstet Gynaecol Res 2020;46:536)
Prognostic factors
- Site specific prognostic factors for primary cervical endometrioid adenocarcinoma are unclear
- Prognostic data on HPV independent endocervical adenocarcinomas as a whole are skewed by predominance of gastric type adenocarcinomas (Virchows Arch 2019;475:537, Gynecol Oncol Rep 2020;32:100579)
- In one series, 4/4 patients with minimal deviation endometrioid adenocarcinoma of the cervix were disease free after 1 - 7 (median: 2) years of follow up (Am J Surg Pathol 1993;17:660)
Case reports
- 39 year old woman with a Pap smear showing atypical glandular cells (Pathol Res Pract 2024;254:155062)
- 49 year old woman with a 1 month history of abnormal vaginal bleeding and a cytologic diagnosis of adenocarcinoma (J Obstet Gynaecol Res 2020;46:536)
- 75 year old woman with postmenopausal bleeding and an initial diagnosis of endometrial endometrioid adenocarcinoma (Int J Gynecol Pathol 2023 Sep 22 [Epub ahead of print])
- 76 year old woman with postmenopausal bleeding and an exophytic cervical mass (Gynecol Oncol Rep 2020;32:100579)
Treatment
- National Comprehensive Cancer Network (NCCN) clinical practice guidelines for cervical cancer do not make recommendations specific to primary cervical endometrioid adenocarcinoma; recommendations are the same for squamous cell carcinoma, all types of adenocarcinoma and adenosquamous carcinoma (NCCN: Guidelines Detail - Cervical Cancer [Accessed 14 February 2024])
- Depending on stage, treatment options include
- Cone biopsy (with or without pelvic lymphadenectomy)
- Radical trachelectomy with pelvic lymphadenectomy (with or without para-aortic lymphadenectomy)
- Extrafascial or modified radical hysterectomy with pelvic lymphadenectomy (with or without para-aortic lymphadenectomy)
- Brachytherapy, pelvic external beam radiation therapy or platinum containing chemotherapy
- Depending on stage, treatment options include
Gross description
- May manifest as a polypoid, ulcerated or cystic cervical mass or be grossly occult
- To exclude cervical involvement by subtle endometrial endometrioid neoplasia, complete histologic examination of the endometrium is prudent, if feasible (Pathology 2021;53:568)
- Reference: J Obstet Gynaecol Res 2020;46:536
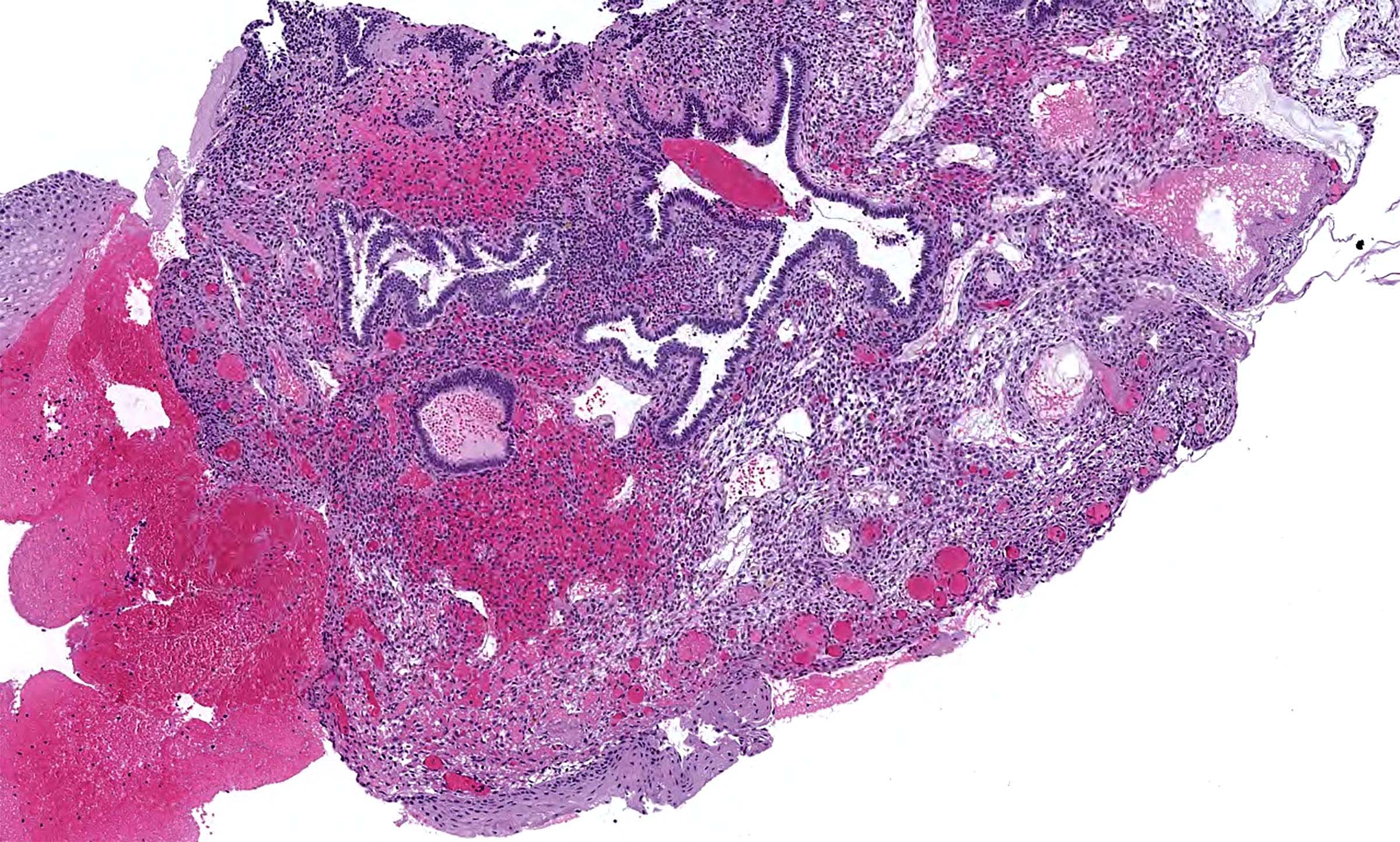
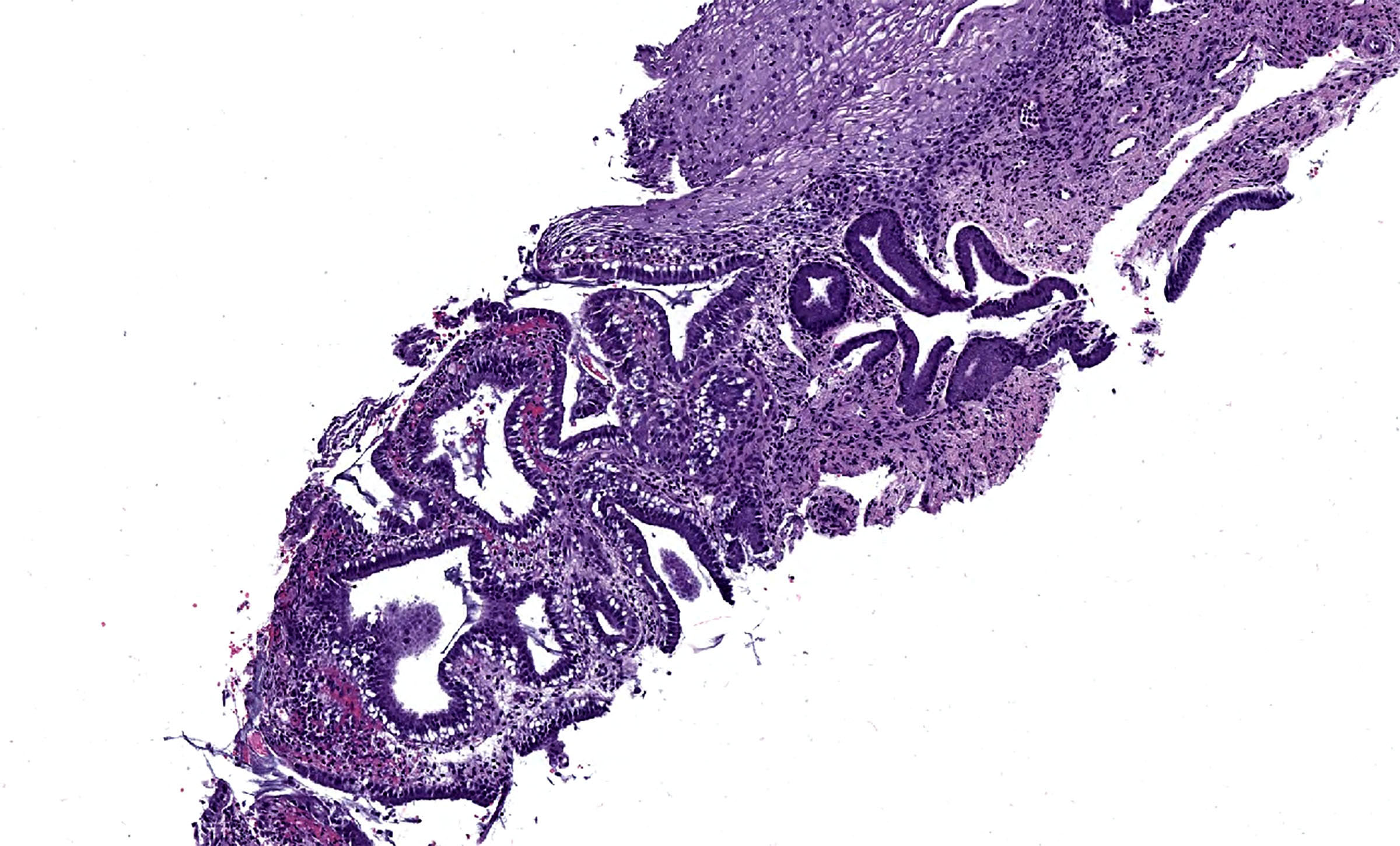
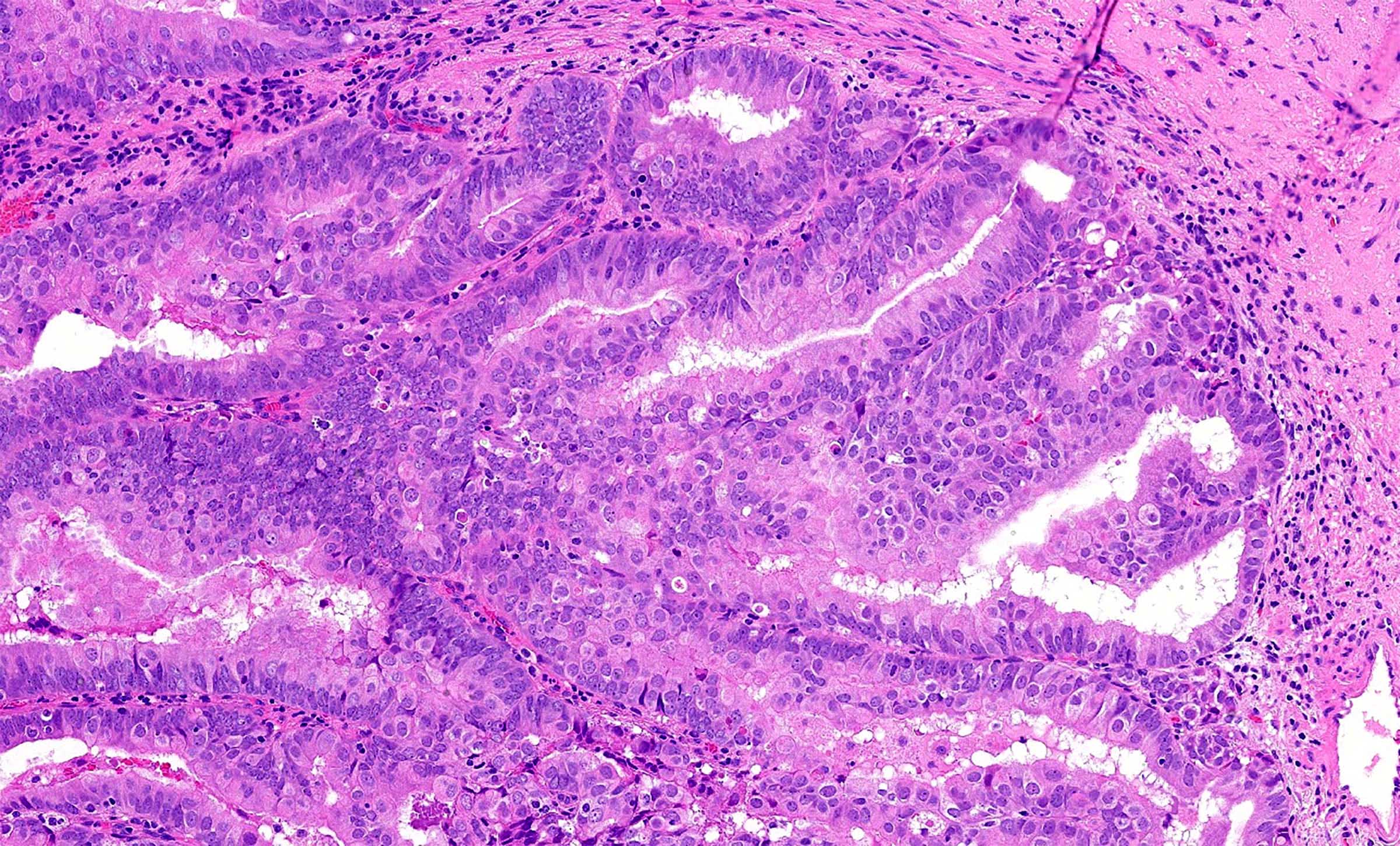
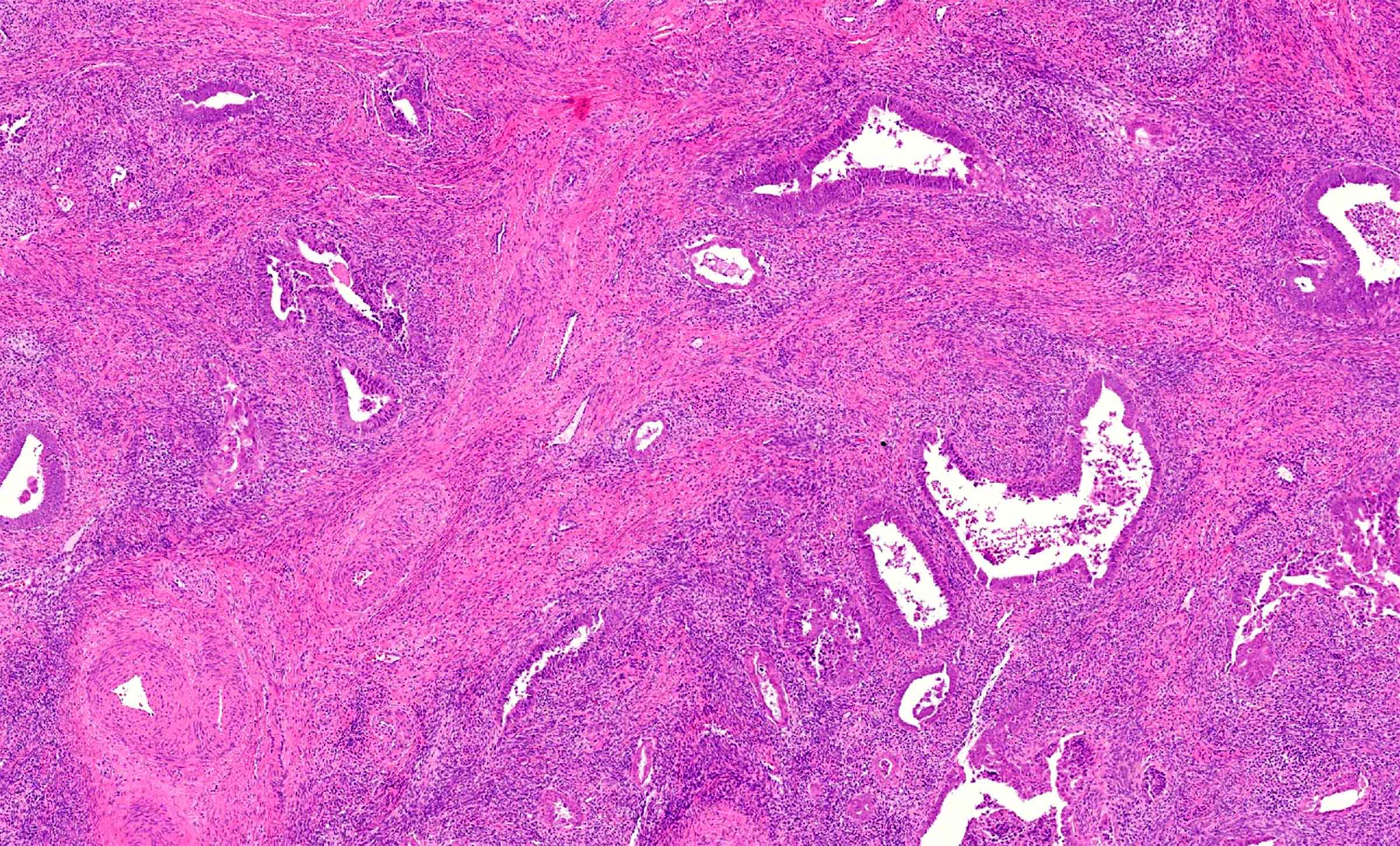
Microscopic (histologic) description
- Morphology of cervical endometrioid adenocarcinoma is indistinguishable from its endometrial counterpart
- Variably fused, cribriform or labyrinthine tubular glands, lined by columnar cells with pseudostratified nuclei and mild to moderate nuclear atypia (Arch Pathol Lab Med 2014;138:453, Am J Surg Pathol 2018;42:214)
- May show morular, squamous, mucinous, ciliated, eosinophilic or secretory differentiation
- Extension from a primary endometrial endometrioid adenocarcinoma must be excluded histologically
- Often associated with cervical endometriosis
- Lacks morphologic features of HPV associated adenocarcinoma (floating luminal mitoses, basal apoptotic bodies) at scanning magnification (Am J Surg Pathol 2018;42:214)
- There is no currently validated grading system for primary endometrioid endocervical adenocarcinoma due to limited data but FIGO grading system can be applied (Int J Gynecol Pathol 2021;40:S66, Surg Pathol Clin 2019;12:281)
- Minimal deviation endometrioid adenocarcinoma of the cervix is comprised of more widely spaced, well differentiated glands and cysts with (at most) mild atypia, scarce mitoses and haphazard infiltration of cervical stroma
- Desmoplasia, if present, is focal
- Given its rarity, objective diagnostic criteria are not well established (Am J Surg Pathol 1993;17:660)
- Cervical involvement by endometrial endometrioid carcinoma may mimic this pattern (Am J Surg Pathol 2003;27:1080)
Microscopic (histologic) images
Cytology description
- Site specific data for primary cervical endometrioid adenocarcinoma are lacking but presumably mirror cytologic findings for endometrial endometrioid adenocarcinoma
Positive stains
- Site specific data for primary cervical endometrioid adenocarcinoma are lacking but appear to mirror endometrial endometrioid adenocarcinoma (Int J Gynecol Pathol 2023 Sep 22 [Epub ahead of print])
Negative stains
- p16 is typically patchy, though high grade endometrioid carcinomas may be block positive (Am J Surg Pathol 2019;43:75)
- High risk HPV in situ hybridization
- GATA3, TTF1
Molecular / cytogenetics description
- Site specific data for primary cervical endometrioid adenocarcinoma are lacking but presumably mirror endometrioid adenocarcinoma originating in the endometrium or in endometriosis (Pathol Res Pract 2023;245:154452, Int J Gynecol Pathol 2023 Sep 22 [Epub ahead of print])
Videos
HPV independent glandular lesions
Benign endocervical lesions
Cytology: glandular cervical lesions
Sample pathology report
- Uterus and cervix, hysterectomy:
- Endometrioid adenocarcinoma, FIGO grade 1 (of 3), most consistent with cervical primary site (see comment)
- Comment: Gross examination of the cervix reveals a 1.2 cm solid - cystic lesion. The endometrium is grossly unremarkable. Microscopic examination of the cervical lesion reveals a FIGO grade 1 endometrioid adenocarcinoma, arising in a background of cervical endometriosis. The endometrium was entirely submitted for histologic examination, which revealed no evidence of endometrial hyperplasia or neoplasia. The composite findings are most consistent with primary cervical endometrioid adenocarcinoma. Correlation with clinical and radiographic findings is advised.
Differential diagnosis
- Cervical involvement by endometrial endometrioid adenocarcinoma:
- Features favoring endometrial primary include (Arch Pathol Lab Med 2014;138:453)
- Endometrial based mass
- Atypical hyperplasia / endometrioid intraepithelial neoplasia in endometrium
- Generous (or if feasible, complete) histologic sampling of the uterus should exclude an endometrial primary site
- Rare cases of synchronous primary endometrial and cervical endometrioid carcinomas are reported
- Demonstration of distinct clonal events in the endometrial and cervical tumors supports synchronous primaries (Int J Gynecol Pathol 2023 Sep 22 [Epub ahead of print])
- Histologic continuity or shared molecular alterations supports cervical involvement by a primary endometrial carcinoma
- Key papers on this topic have come to different conclusions but most lack modern molecular methods (Int J Gynecol Pathol 2010;29:146, Am J Surg Pathol 2003;27:1080, Pathology 2021;53:568)
- Rare cases of synchronous primary endometrial and cervical endometrioid carcinomas are reported
- Cervical spread of primary endometrial endometrioid carcinoma may rarely mimic minimal deviation endometrioid adenocarcinoma of the cervix (Am J Surg Pathol 2003;27:1080)
- Some experts posit that a minimal deviation endometrioid adenocarcinoma pattern in the cervix associated with atypical or nonatypical hyperplasia of the endometrium should be designated as stage II endometrial endometrioid carcinoma, though objective data to support this position are lacking (Pathology 2021;53:568)
- Features favoring endometrial primary include (Arch Pathol Lab Med 2014;138:453)
- HPV associated usual type endocervical adenocarcinoma:
- Mesonephric carcinoma of the cervix:
- Often associated with mesonephric remnants / hyperplasia
- GATA3 or TTF1 positive; ER and PR negative
- Mixed architectural patterns, including tubular, ductal (resembling endometrioid glands), papillary, solid, sieve-like, corded, glomeruloid and single cell, among others
- Dense, colloid-like eosinophilic luminal secretions
- Lacks squamous morular or mucinous differentiation
- In principle, a mesonephric-like adenocarcinoma could arise in cervical endometriosis; immunostains should resolve this differential
- Tuboendometrioid metaplasia:
- Criteria favoring a diagnosis of minimal deviation endometrioid adenocarcinoma of the cervix over tuboendometrioid metaplasia include (Arch Pathol Lab Med 2014;138:453)
- Deep cervical wall involvement (outer third)
- Haphazard arrangement of glands
- Irregularly sized, branched or cystic glands
- At least focal desmoplastic stromal response
- Criteria favoring a diagnosis of minimal deviation endometrioid adenocarcinoma of the cervix over tuboendometrioid metaplasia include (Arch Pathol Lab Med 2014;138:453)
Additional references
Board review style question #1
A 68 year old obese woman presents with 6 months of postmenopausal bleeding. She has no history of diethylstilbestrol (DES) exposure. Colposcopy reveals an ulcerated 2.0 cm nodular lesion at the cervical os. A Pap test shows atypical glandular cells and human papillomavirus (HPV) testing is negative. Pelvic magnetic resonance imaging (MRI) reveals a cervical based tumor. A hysterectomy is performed. The endometrium and lower uterine segment are entirely submitted for histologic examination and are negative for hyperplasia or neoplasia. A representative image of the cervical mass is shown above. By immunohistochemistry, the tumor is positive for PAX8, ER, PR and vimentin. p16 is patchy. An RNA in situ hybridization assay for high risk HPV is negative. What is the most likely diagnosis?
- Endometrial endometrioid adenocarcinoma with cervical stromal involvement
- Endometrioid adenocarcinoma of the uterine cervix, HPV independent
- Mesonephric carcinoma of the uterine cervix, HPV independent
- Metastatic adenocarcinoma of the bladder
- Usual type endocervical adenocarcinoma, HPV associated
Board review style answer #1
B. Endometrioid adenocarcinoma of the uterine cervix, HPV independent. This is a cervical based tumor, with no evidence of a concurrent endometrial carcinoma. The tumor morphology and immunophenotype are characteristic of endometrioid adenocarcinoma and an HPV assay is negative. These features are diagnostic of primary cervical endometrioid adenocarcinoma.
Answer A is incorrect because a complete histologic examination of the endometrial cavity revealed no evidence of an endometrial tumor. Answer C is incorrect because while mesonephric carcinoma can show ductular architecture that mimics endometrioid neoplasia, it characteristically shows other admixed architectural patterns (tubular, solid, papillary, corded, etc.). Mesonephric carcinoma is also characteristically ER and PR negative. Answer D is incorrect because bladder carcinoma is not expected to be positive for PAX8, ER and PR. Answer E is incorrect because usual type HPV associated endocervical adenocarcinoma shows brisk apical mitoses and basal apoptotic bodies, which are not present in this case. Usual type HPV associated endocervical adenocarcinoma also shows strong diffuse p16 and a high risk HPV assay would be positive.
Comment Here
Reference: Primary endometrioid adenocarcinoma (HPV independent)
Answer A is incorrect because a complete histologic examination of the endometrial cavity revealed no evidence of an endometrial tumor. Answer C is incorrect because while mesonephric carcinoma can show ductular architecture that mimics endometrioid neoplasia, it characteristically shows other admixed architectural patterns (tubular, solid, papillary, corded, etc.). Mesonephric carcinoma is also characteristically ER and PR negative. Answer D is incorrect because bladder carcinoma is not expected to be positive for PAX8, ER and PR. Answer E is incorrect because usual type HPV associated endocervical adenocarcinoma shows brisk apical mitoses and basal apoptotic bodies, which are not present in this case. Usual type HPV associated endocervical adenocarcinoma also shows strong diffuse p16 and a high risk HPV assay would be positive.
Comment Here
Reference: Primary endometrioid adenocarcinoma (HPV independent)