Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Pors J, Hoang L. Mesonephric adenocarcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/cervixmesonephricadeno.html. Accessed April 2nd, 2025.
Definition / general
- Rare, nonhuman papillomavirus (HPV) associated cervical neoplasm that is thought to derive from mesonephric / Wolffian remnants
Essential features
- Shows a variety of morphologic patterns, presenting a risk of misdiagnosis
- PAX8+, GATA3+, p16-, ER- immunoprofile; TTF1+ in a subset
- Frequently harbors KRAS mutations
Terminology
- Mesonephric carcinoma of the cervix
- Mesonephric carcinosarcoma of the cervix
- Mesonephric adenocarcinoma of the cervix
ICD coding
- ICD-10: C53.9 - malignant neoplasm of cervix uteri, unspecified
Epidemiology
- Rare, accounts for < 1% of all cervical adenocarcinomas (Am J Surg Pathol 2018;42:214)
- Mean age at diagnosis is 52 - 59 (Gynecol Oncol Rep 2016;17:7, Am J Surg Pathol 2021;45:498)
- Unassociated with human papillomavirus (HPV) (Am J Pathol 2000;157:1055, Histopathology 2010;57:342)
Sites
- Cervix, more common in lateral walls
Pathophysiology
- Unknown at this time
Etiology
- Thought to derive from mesonephric duct remnants / hyperplasia (Mod Pathol 2015;28:1504)
- Mesonephric remnants are found in the lateral cervical wall in up to 22% of adult uterine cervices (Int J Gynecol Pathol 2002;21:327)
Clinical features
- Most common clinical presentation is abnormal vaginal bleeding
- Can be detected by abnormal cervical cytology but less frequently than cervical squamous cell carcinoma (BMJ Case Rep 2012;2012:bcr0120125632, Am J Surg Pathol 2021;45:498)
- Can also present as cervical mass or incidentally
Diagnosis
- Cervical biopsy, endometrial curettage or hysterectomy specimen
Radiology description
- MRI demonstrates cervical mass with extension to the uterus, parametrium and upper vagina
Prognostic factors
- Worse overall survival, disease specific survival, and progression free survival compared to HPV endocervical adenocarcinoma (Am J Surg Pathol 2021;45:498)
- Majority present at FIGO stage IB or higher (Gynecol Oncol Rep 2016;17:7, Gynecol Oncol Rep 2020;34:100652, Am J Surg Pathol 2021;45:498)
- Many cases (half in one study) are associated with recurrence, commonly to distant sites (Am J Surg Pathol 2021;45:498)
- Stage I: recurrence rate 32%, mean recurrence interval of 24 months, mean overall survival of 50 months (Gynecol Oncol Rep 2016;17:7)
- Spindle component may portend a worse outcome (Gynecol Oncol Rep 2016;17:7)
Case reports
- 40 year old woman with FGFR2 mutation (Int J Gynecol Pathol 2020;39:452)
- 46 year old woman who presented with abnormal uterine bleeding and an enlarged cervix and was initially diagnosed with mesonephric hyperplasia (Iran J Pathol 2021;16:227)
- 48 year old woman with lung metastasis; tumor showed mutations in KRAS and CTNNB1 and gain of 1q (Diagn Pathol 2019;14:71)
- 60 year old woman initially diagnosed with endometrial carcinoma (Rev Bras Ginecol Obstet 2021;43:329)
- 73 year old woman with FGFR2 mutation (Cureus 2022;14:e25098)
Treatment
- Mainstay of treatment is hysterectomy with or without bilateral salpingo-oopherectomy and pelvic lymph node dissection
- Roles of neoadjuvant or adjuvant chemotherapy and radiation therapy remain unclear
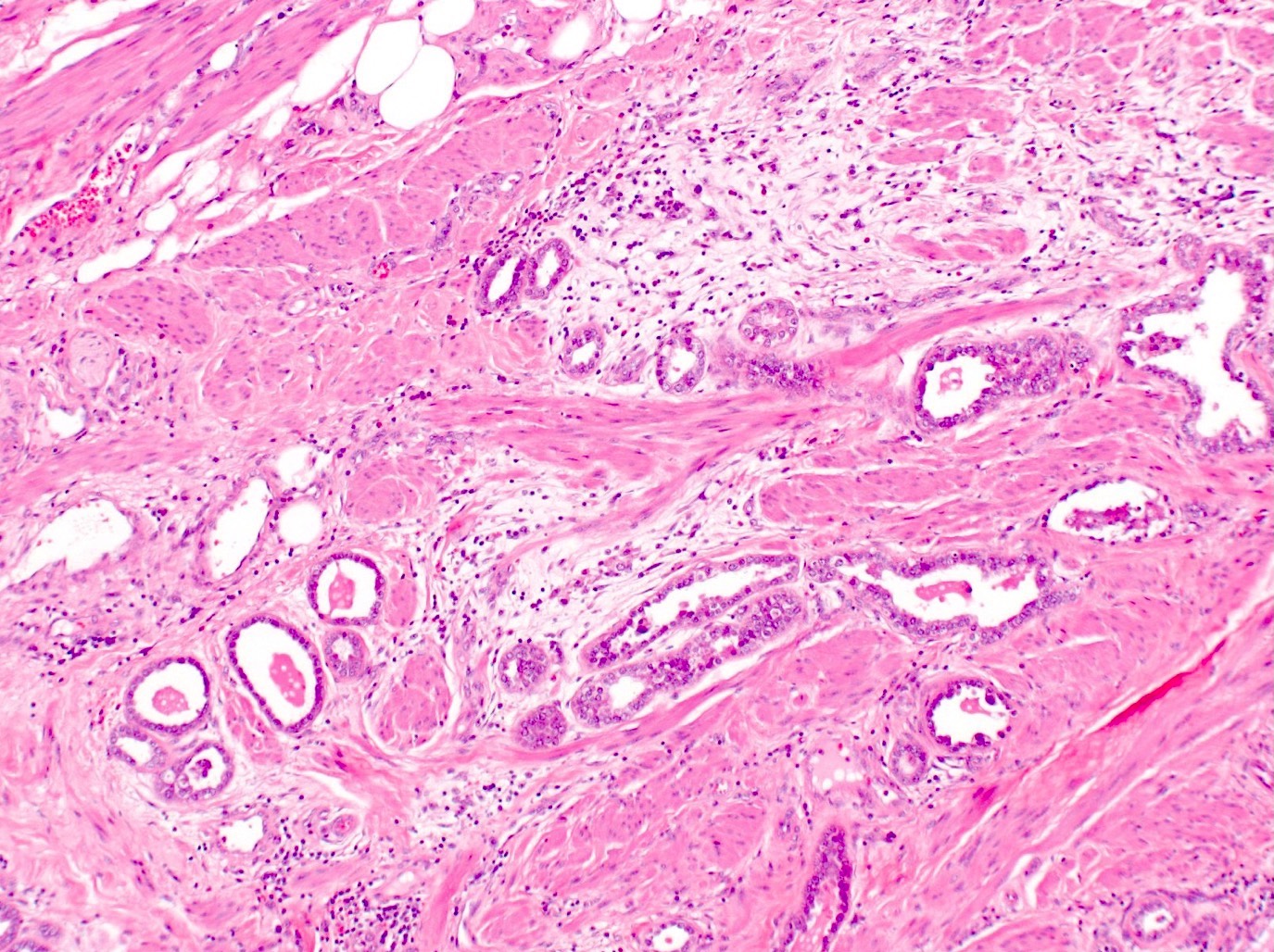
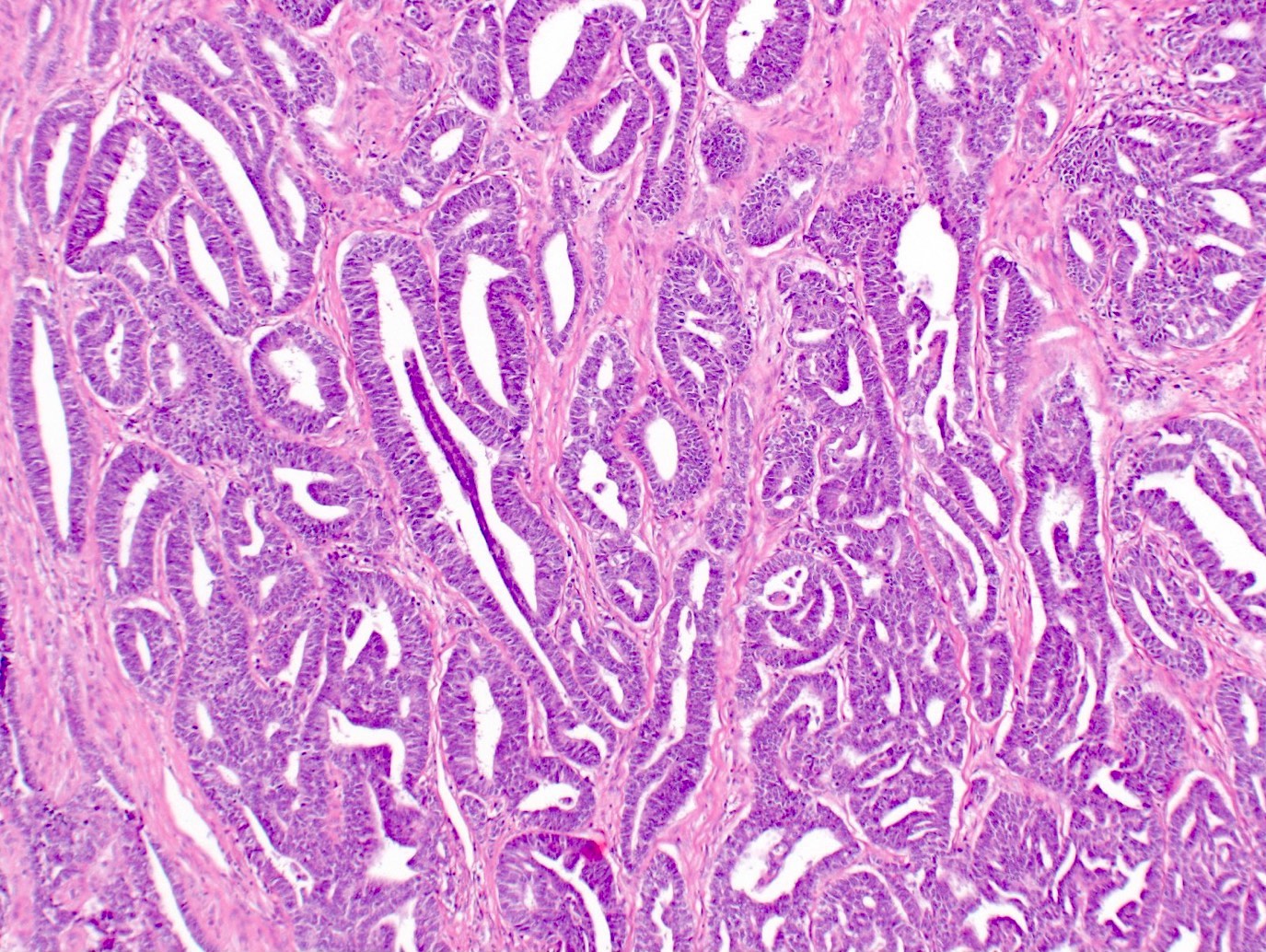
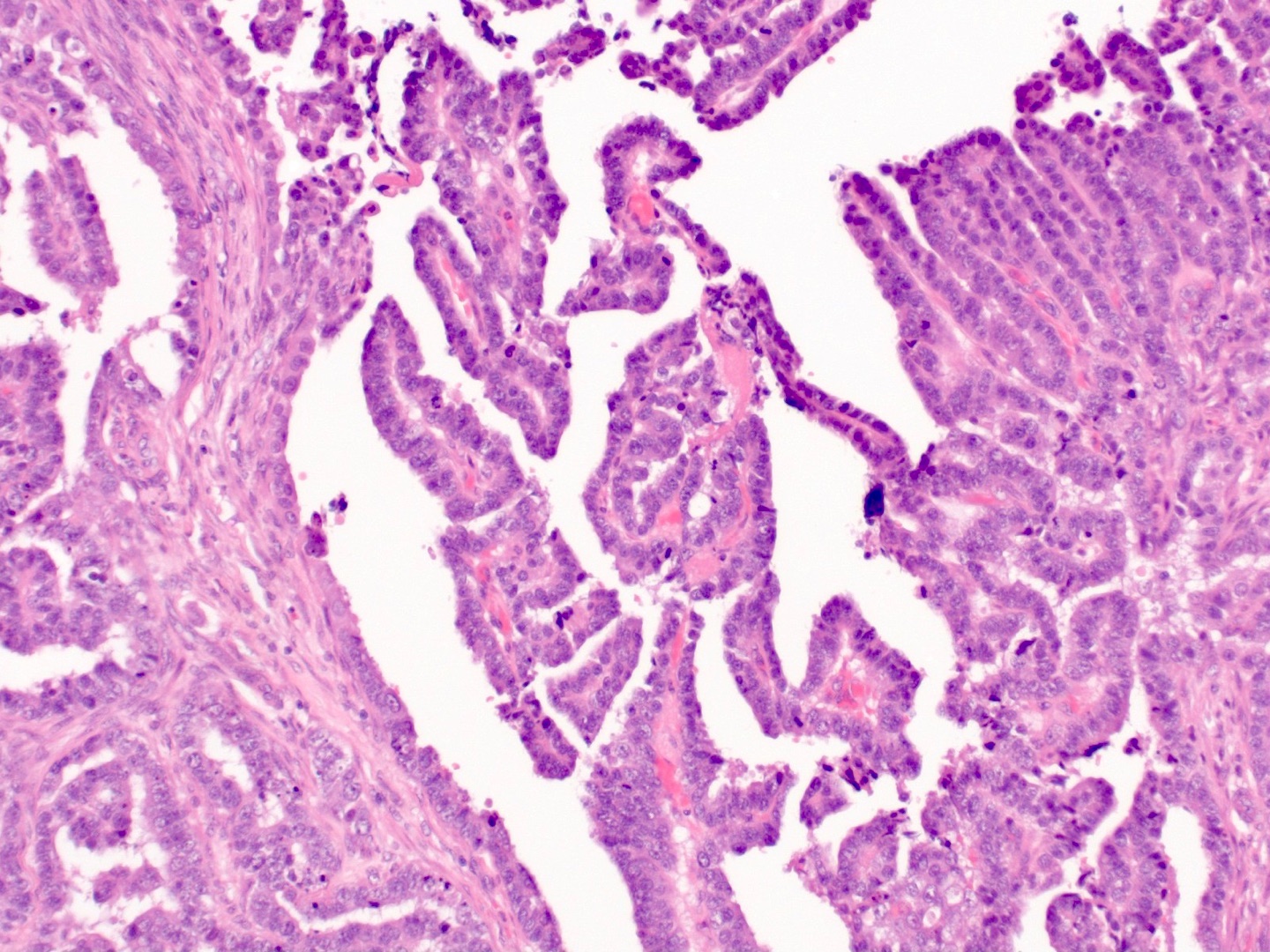
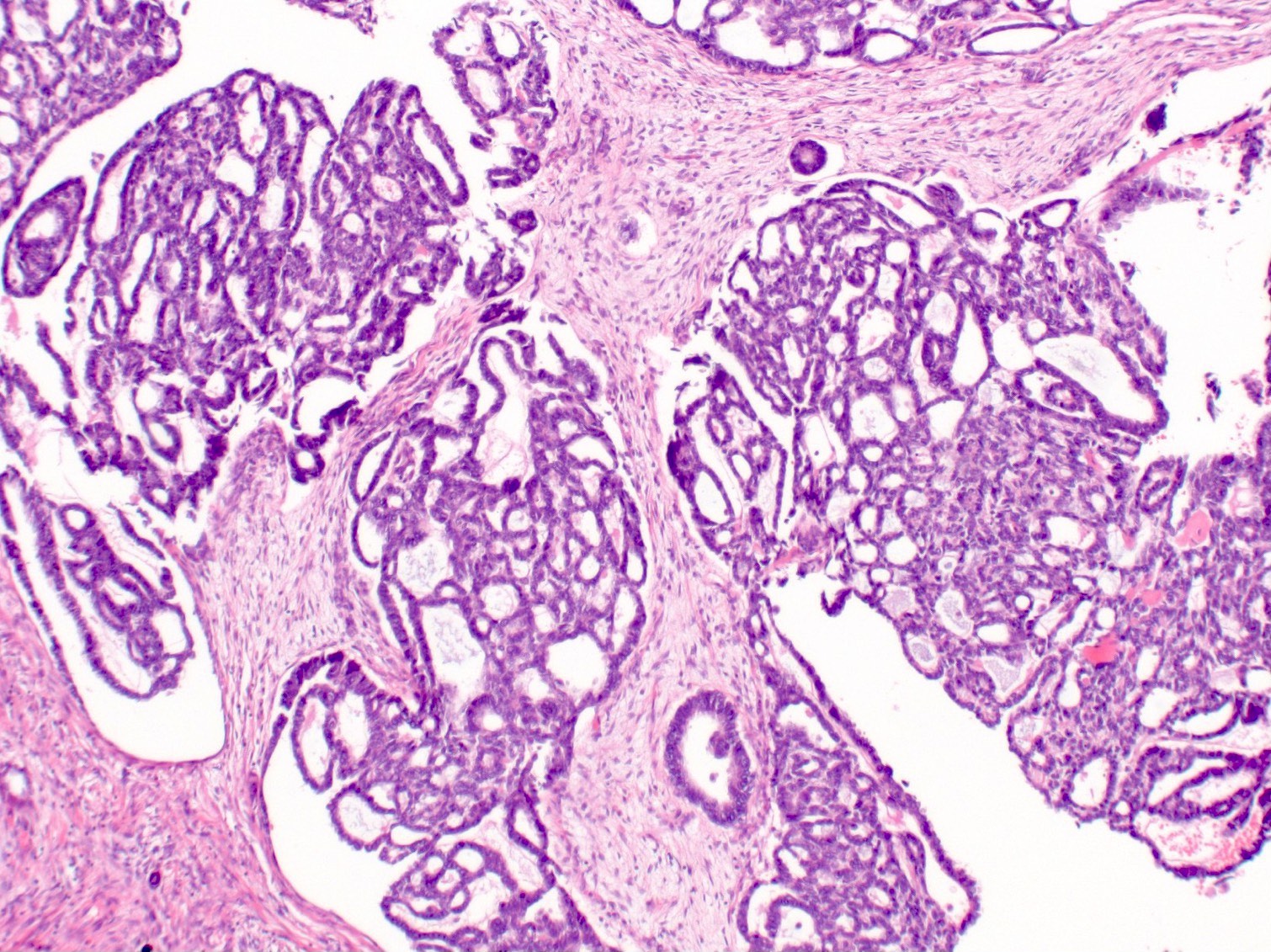
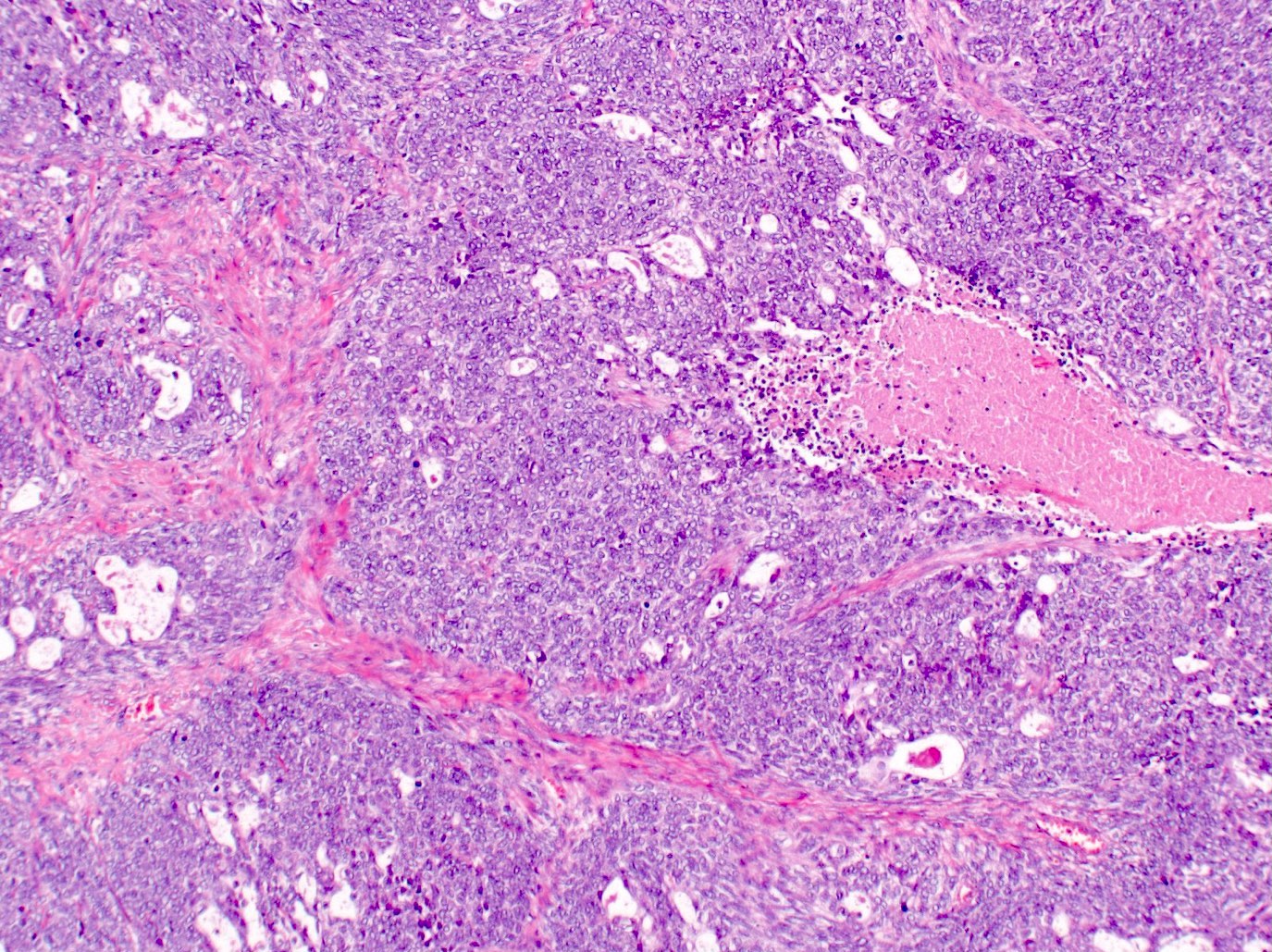
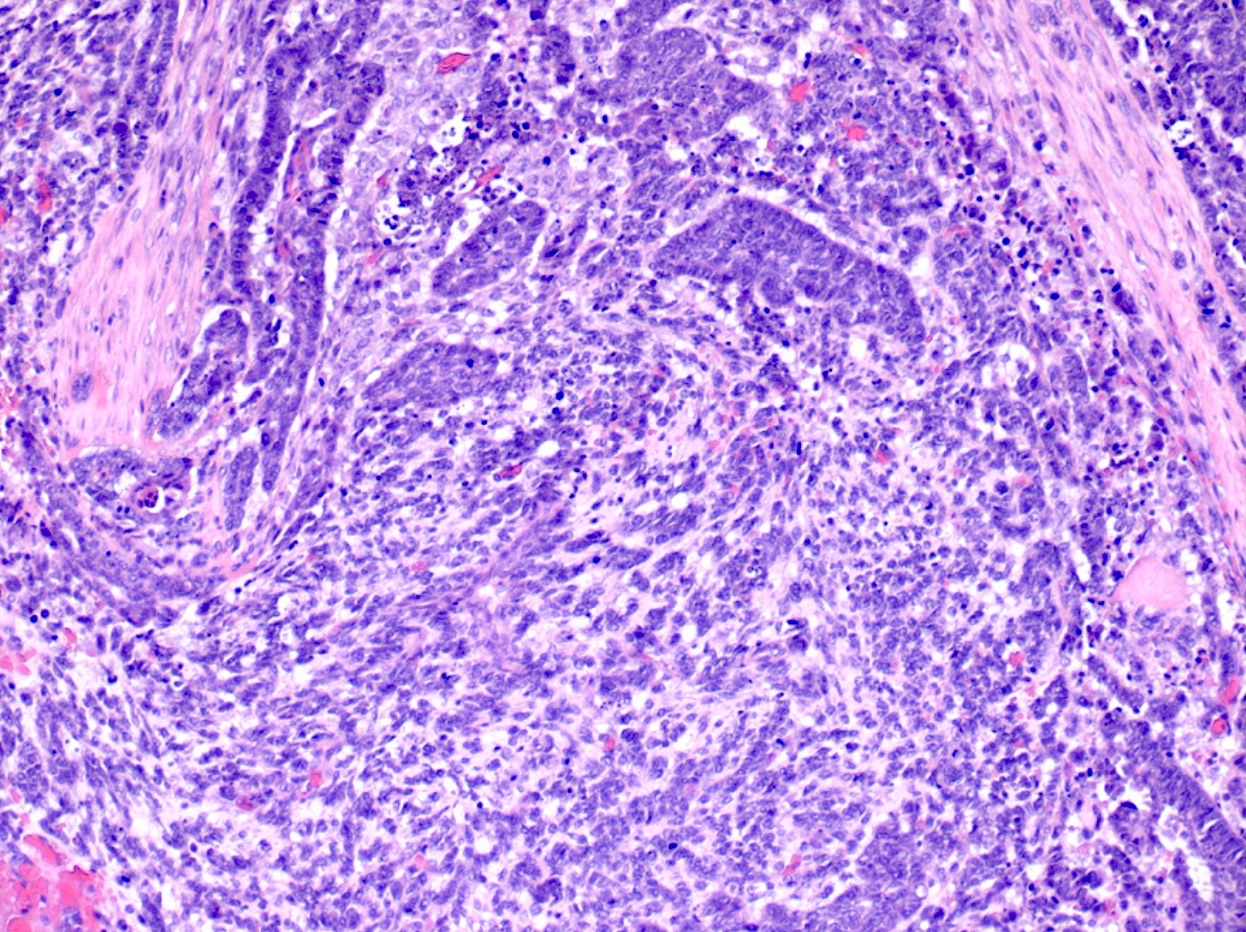
Microscopic (histologic) description
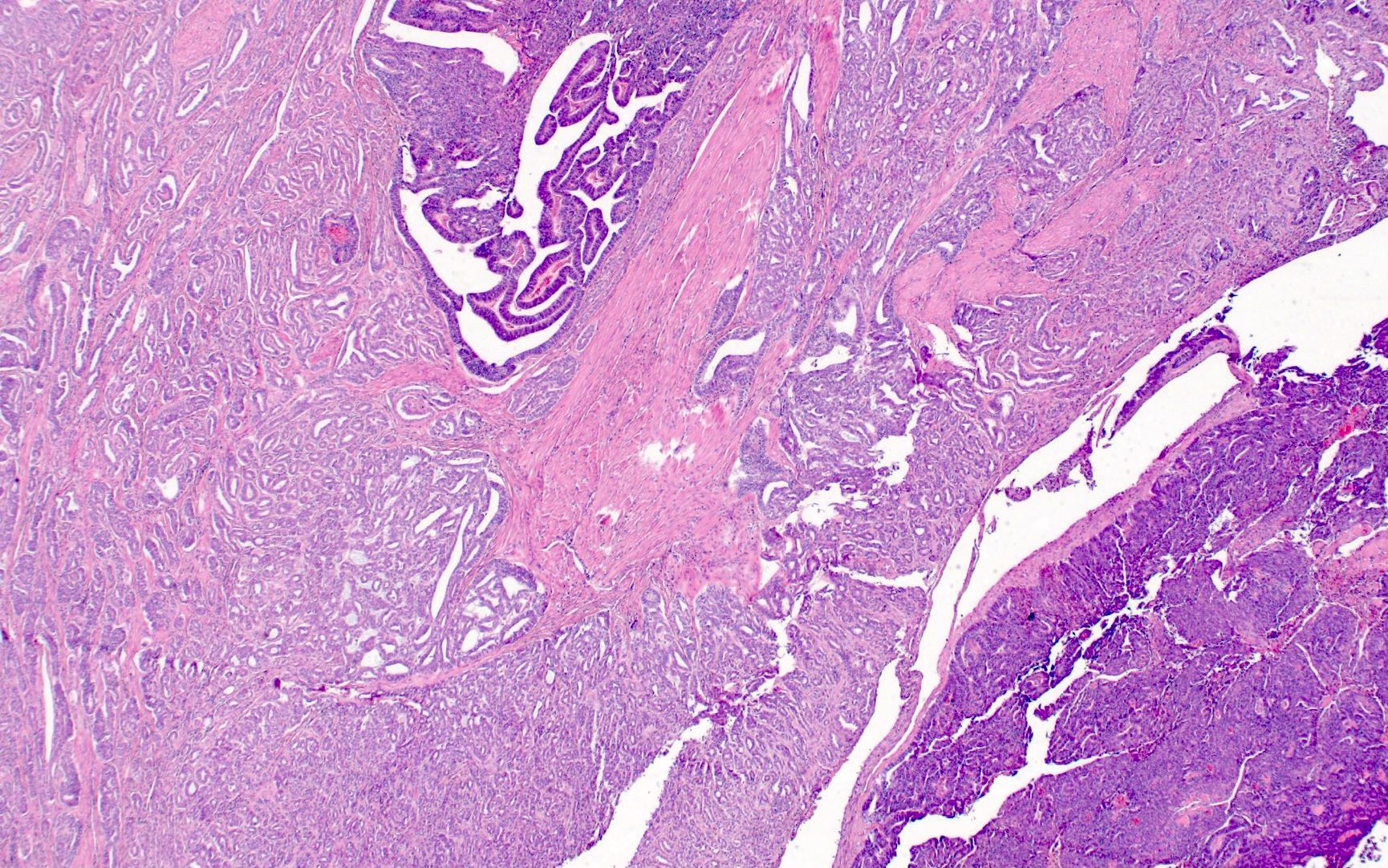
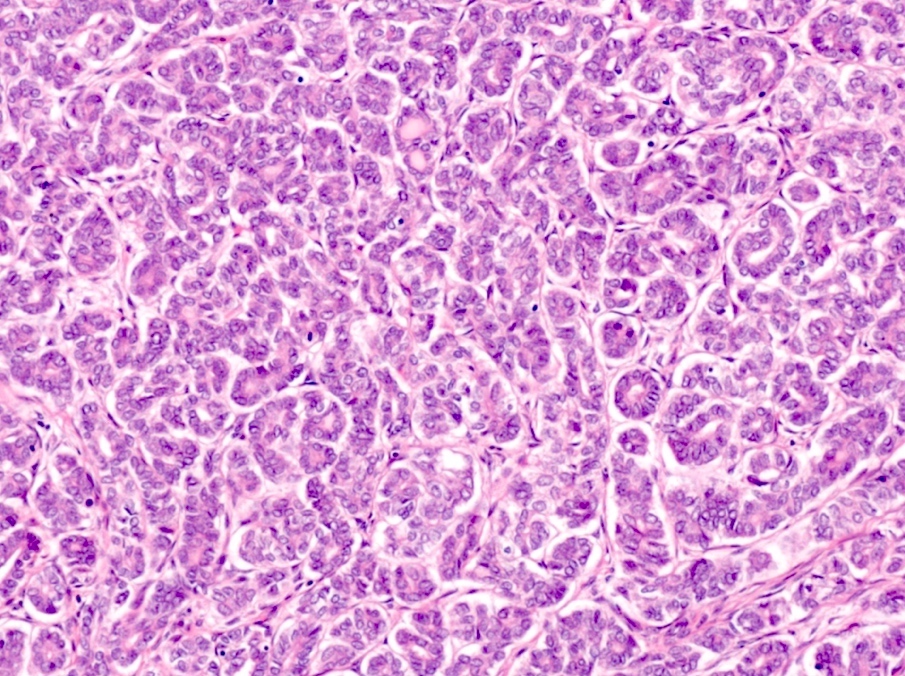
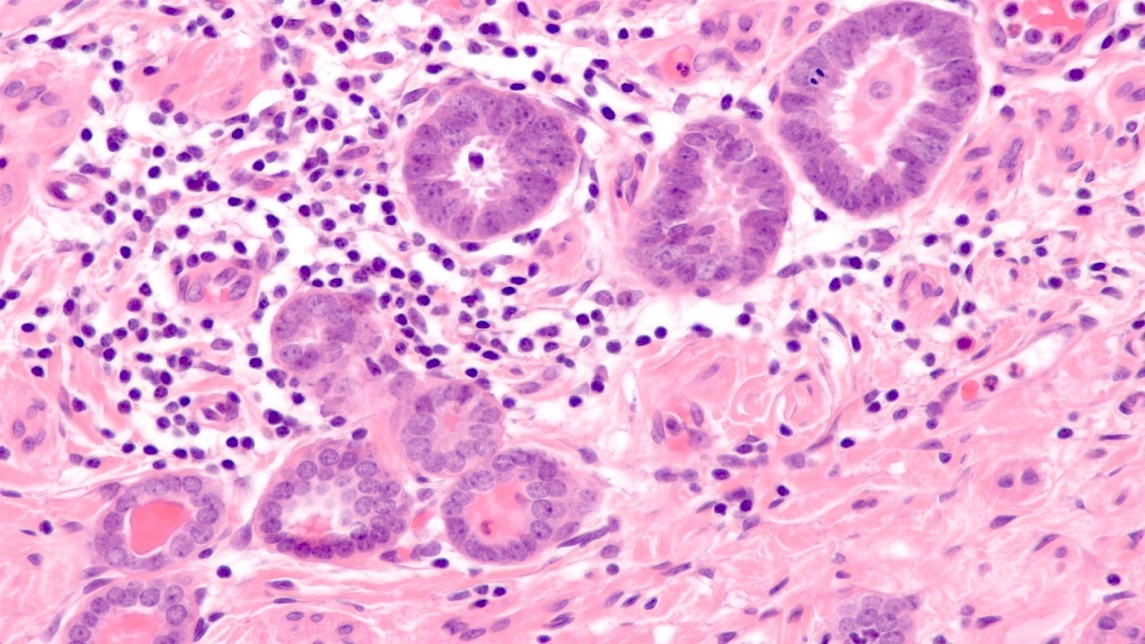
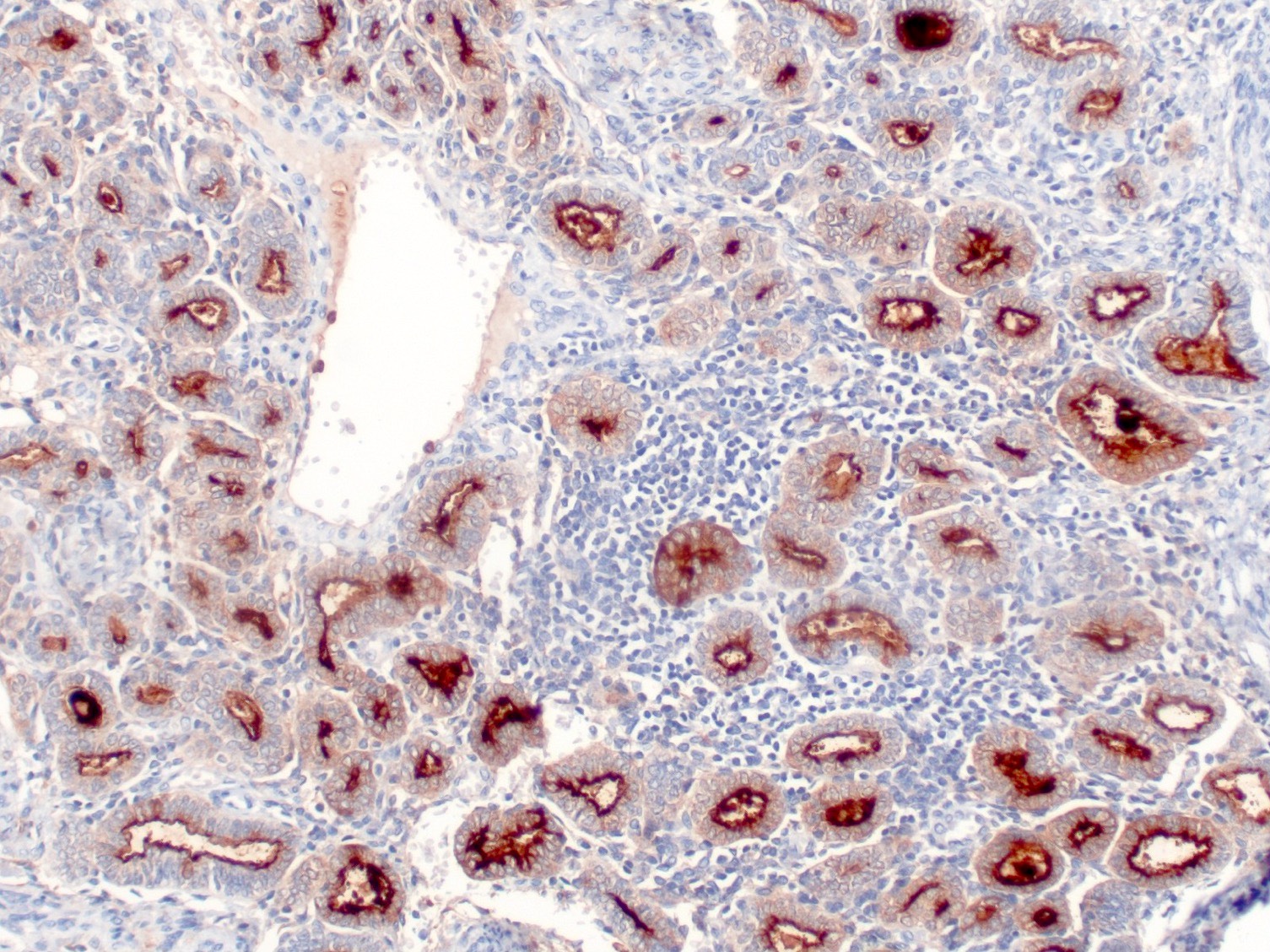
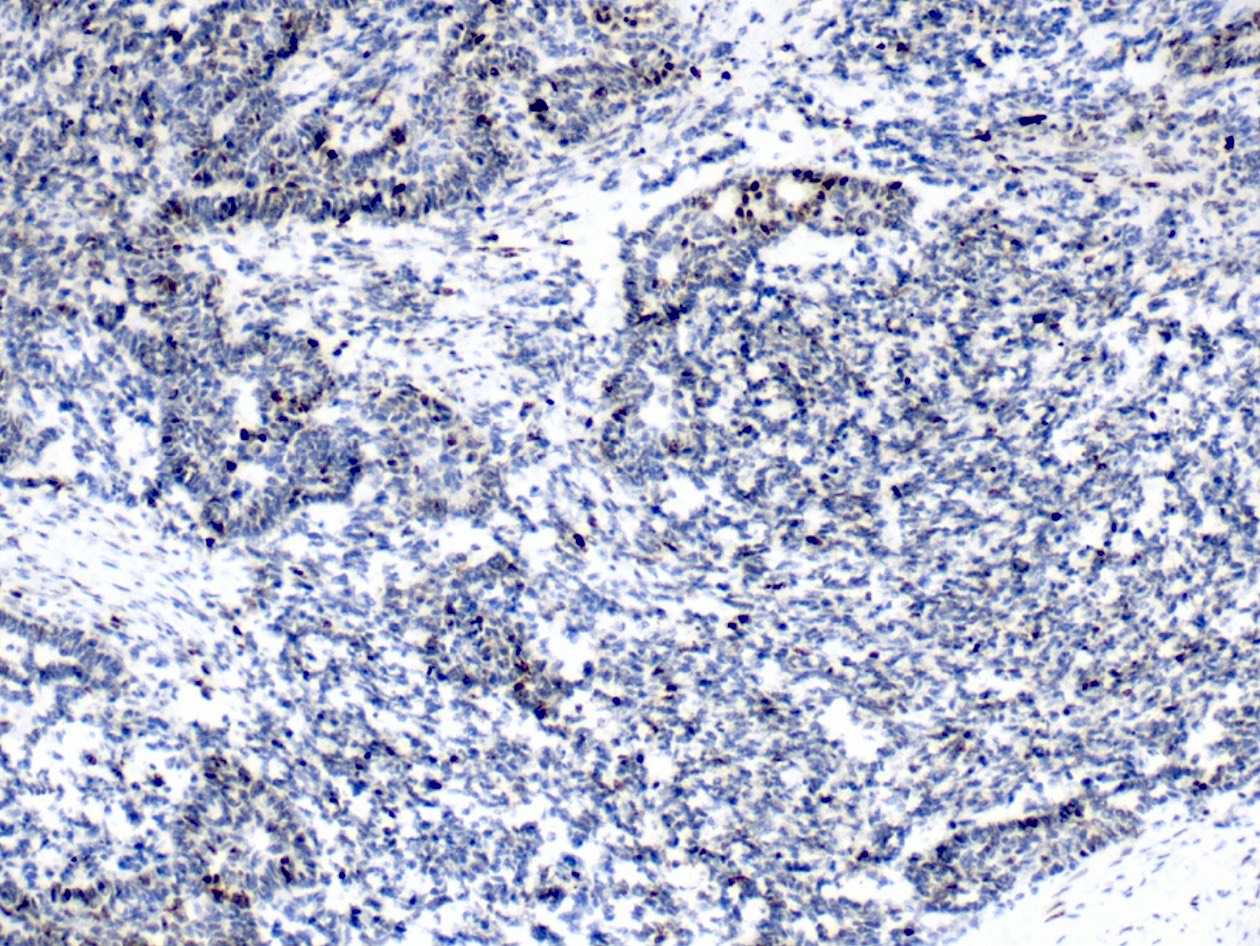
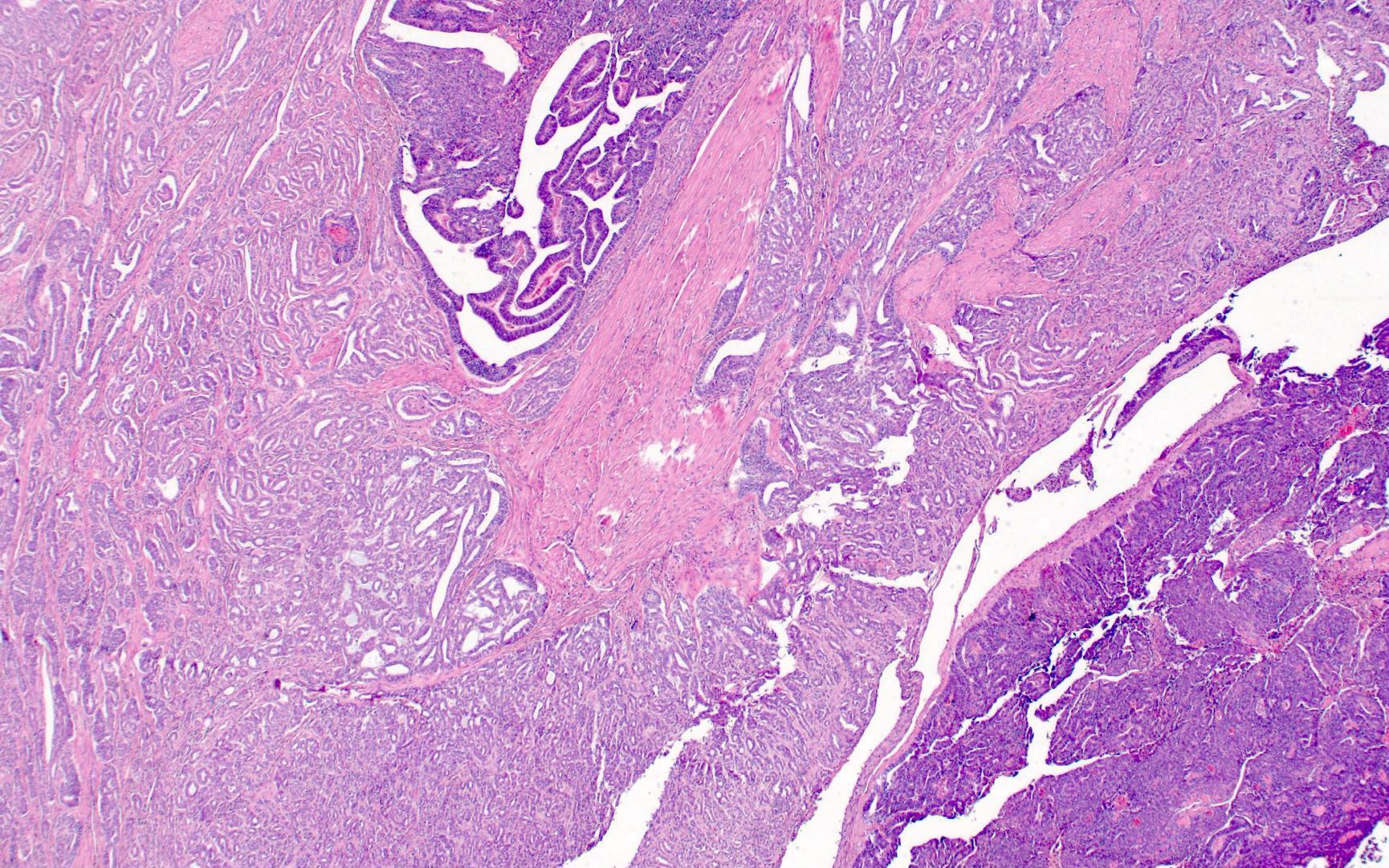
- Many histologic patterns, often varying between tumors and between different microscopic fields of the same tumor (Am J Surg Pathol 1995;19:1158, Int J Gynecol Pathol 2002;21:327)
- Tubular pattern is most common; consists of small back to back tubules lined by cuboidal cells, containing eosinophilic intraluminal colloid-like secretions that stain positive for PASD and mucicarmine
- Ductal (pseudoendometrioid) pattern: glands lined by columnar cells, reminiscent of endometrioid adenocarcinoma
- Other reported histologic patterns: retiform, sex cord-like, papillary, hobnail, glomeruloid, solid, sieve-like, spindled
- May show a range of cytologic atypia with inconspicuous to prominent nucleoli (Am J Surg Pathol 1995;19:1158)
- Mitotic figures can be rare or readily apparent (Am J Surg Pathol 1990;14:1100, Am J Surg Pathol 1995;19:1158)
- Often deeply infiltrative but may show little desmoplasia (Am J Surg Pathol 1990;14:1100)
- Often associated with peripheral mesonephric remnants or mesonephric hyperplasia
- Mesonephric carcinosarcoma: high grade spindle cell component; heterologous osteosarcomatous and chondrosarcomatous differentiation have been described (Am J Surg Pathol 1995;19:1158, Am J Surg Pathol 2018;42:1596)
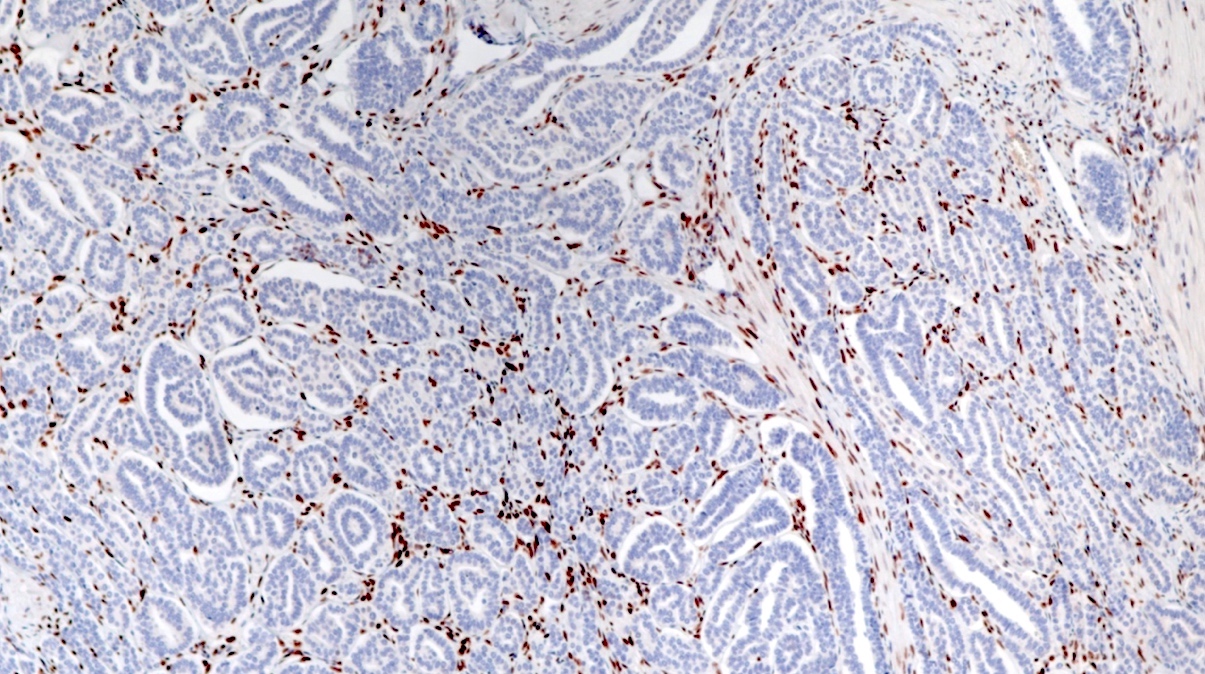
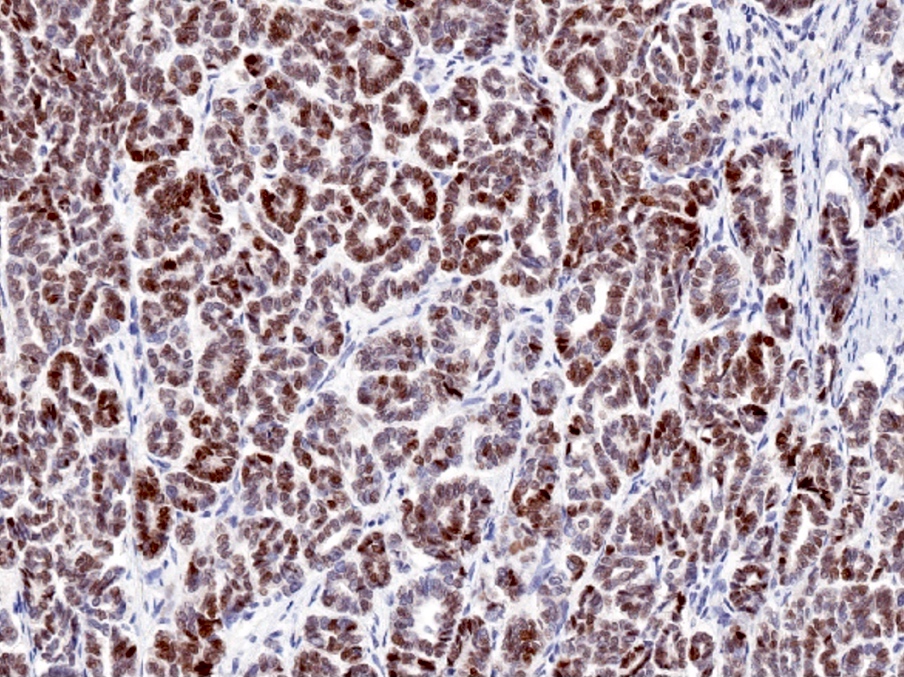
Microscopic (histologic) images
Contributed by Lynn Hoang, M.D.
Cytology description
- Clusters of epithelial cells in tubular, cribriform and sheet-like proliferations (Cytopathology 2013;24:129)
- Round to oval, occasionally angulated, small to medium sized nuclei with mild to moderate atypia and increased N:C ratio (Cytopathology 2013;24:129)
- Intraluminal eosinophilic material (Cytopathology 2013;24:129)
- Infrequently detected by cervical cytology compared to cervical squamous cell carcinoma (BMJ Case Rep 2012;2012:bcr0120125632)
Positive stains
- PAX8: nuclear staining, > 88% (Am J Surg Pathol 2012;36:799, Am J Surg Pathol 2018;42:1596)
- GATA3: nuclear staining, > 85% (Am J Surg Pathol 2015;39:1411, Am J Surg Pathol 2018;42:1596)
- Caveat: solid / spindled lesions show loss of GATA3 staining (Am J Surg Pathol 2018;42:1596)
- CD10: luminal staining, > 70% (Am J Surg Pathol 2012;36:799, Am J Surg Pathol 2018;42:1596)
- Calretinin: nuclear and cytoplasmic staining, 57 - 88% (Am J Surg Pathol 2001;25:379, Am J Surg Pathol 2004;28:601, Am J Surg Pathol 2012;36:799, Am J Surg Pathol 2018;42:1596)
- HNF-1B: nuclear staining, 38 - 64% (Am J Surg Pathol 2012;36:799, Appl Immunohistochem Mol Morphol 2020;28:593)
Negative stains
- Estrogen receptor / ER: negative nuclear staining (Am J Surg Pathol 2018;42:1596, Am J Surg Pathol 2001;25:379)
- Caveat: positive in a subset of cases (Am J Surg Pathol 2012;36:799)
- Progesterone receptor / PR: negative nuclear staining (Am J Surg Pathol 2001;25:379)
- p16: usually negative; positive (nuclear and cytoplasmic block staining) in subset of cases but does not correlate with HPV status (Am J Surg Pathol 2012;36:799, Histopathology 2010;57:342)
- Napsin A: usually negative; focally positive (cytoplasmic granular staining) in a subset of cases (Appl Immunohistochem Mol Morphol 2020;28:593)
- AMACR: usually negative; focally positive (cytoplasmic staining) in a subset of cases (Appl Immunohistochem Mol Morphol 2020;28:593)
- TTF1: nuclear staining, 0 - 13% (Am J Surg Pathol 2012;36:799, Am J Surg Pathol 2018;42:1596, Mod Pathol 2021;34:1570)
- Rarely positive in mesonephric carcinoma of the cervix; more frequently positive in mesonephric-like carcinoma of the ovary and uterus
- Can have inverse staining pattern with GATA3 (Am J Surg Pathol 2018;42:1596)
- Androgen receptor: nuclear staining, 33% (Am J Surg Pathol 2001;25:379)
Electron microscopy description
- One case report demonstrated the presence of cytotelolysomes (Pathol Res Pract 2008;204:671)
- A distinctive feature of mesonephric epithelium (Int J Gynecol Pathol 1985;4:245)
Molecular / cytogenetics description
- Majority associated with mutations in KRAS and gain in 1q, in contrast to HPV associated endocervical adenocarcinoma (Mod Pathol 2015;28:1504)
- Some mesonephric carcinomas harbor mutation in actionable gene KRAS G12C (Diagn Pathol 2019;14:71, Gynecol Oncol Rep 2020;34:100652)
- Mutations in NRAS, chromatin remodeling gene mutations (ARID1A, ARID1B, SMARCA4), BCOR, TP53 have also been described (Mod Pathol 2015;28:1504)
- Low tumor mutational burden (Diagn Pathol 2019;14:71)
- Mesonephric hyperplasia does not harbor KRAS or NRAS mutations (Histopathology 2017;71:1003)
Sample pathology report
- Uterus (with cervix), fallopian tubes and ovaries, total hysterectomy and bilateral salpingo-oophorectomy:
- Mesonephric adenocarcinoma (see comment and synoptic report)
- Comment: This tumor demonstrates several distinct histologic patterns (tubular, glandular and papillary) with associated peripheral mesonephric remnants. By immunohistochemistry, this tumor shows diffuse and strong expression of GATA3 and PAX8 and no expression of ER. Taken together, these features are diagnostic of mesonephric adenocarcinoma of the cervix.
Differential diagnosis
- Mesonephric-like adenocarcinoma (MLA) of the endometrium:
- Bulk of tumor in uterine corpus
- No associated mesonephric remnants
- Both are ER-, GATA3+, CD10+
- MLA more commonly TTF1+ than mesonephric adenocarcinoma of the cervix (Am J Surg Pathol 2018;42:1596)
- Endometrioid endometrial adenocarcinoma:
- Also shows a variety of histologic patterns
- ER+, GATA3-, CD10- (Am J Surg Pathol 2018;42:1596)
- Clear cell carcinoma:
- Can also show solid, papillary and tubulocystic morphologic patterns
- Cuboidal cells with clear to eosinophilic cytoplasm, in contrast to relatively blue, basophilic appearance of mesonephric carcinoma
- Both are ER- and variably HNF-1B+
- AMACR+, napsin A+ (Appl Immunohistochem Mol Morphol 2020;28:593)
- Endometrial serous carcinoma:
- Mutant p53 pattern, GATA3-, CD10- (Mod Pathol 2015;28:1504, Int J Gynecol Pathol 2014;33:624, Am J Surg Pathol 2018;42:1596)
- Mesonephric hyperplasia:
- Rarely shows atypia or mitoses and does not have back to back glandular crowding or stromal desmoplasia
- May show a lobulated low power appearance with tubules arranged around a central duct
- Does not harbor KRAS mutations (Histopathology 2017;71:1003)
- Carcinosarcoma:
- Carcinoma component shows endometrioid, serous or mixed features
- Mutant p53 pattern (Am J Surg Pathol 2018;42:1596)
Board review style question #1
Board review style answer #1
B. PAX8+, ER-, GATA3+, napsin A-.
Mesonephric carcinomas of the cervix are typically PAX8+, ER-, GATA3+ and napsin A-. Answers A and D are incorrect because they typically show negative to focal staining for napsin A and AMACR.
Comment Here
Reference: Mesonephric adenocarcinoma
Comment Here
Reference: Mesonephric adenocarcinoma
Board review style question #2
Which mutation is frequently harbored by mesonephric adenocarcinomas of the cervix?
- BRAF
- BRCA
- KRAS
- RET
Board review style answer #2
C. KRAS. Mesonephric adenocarcinomas of the cervix frequently harbor KRAS mutations. Answers A, B and D are incorrect because BRAF, BRCA and RET mutations have not been identified in mesonephric adenocarcinoma of the cervix (Gynecol Oncol Rep 2020;34:100652, Mod Pathol 2021;34:1570, Mod Pathol 2015;28:1504).
Comment Here
Reference: Mesonephric adenocarcinoma
Comment Here
Reference: Mesonephric adenocarcinoma