Table of Contents
Definition / general | Essential features | CPT coding | Sites | Etiology | Clinical features | Laboratory | Management | Cytology description | Cytology images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Jager L, Choy B. LSIL (cytology). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/cervixcytologyLSIL.html. Accessed March 30th, 2025.
Definition / general
- Changes in squamous cells associated with human papillomavirus (HPV) infection, encompassing mild dysplasia and cervical intraepithelial neoplasia (CIN) 1
Essential features
- Lesion of intermediate or superficial cells caused by low risk and high risk HPV
- Most are transient infections with little risk for oncogenesis
- Criteria based on the 2014 Bethesda System for Reporting Cervical Cytology (see Bethesda system):
- Nuclear atypia, including nuclear enlargement (> 3x the area of normal intermediate nuclei), hyperchromasia, anisonucleosis, coarsely granular / smudgy / densely opaque chromatin, variable nuclear membranes, binucleation / multinucleation
- Koilocytosis or dense orangeophilia must be accompanied by nuclear abnormalities
CPT coding
- For screening Pap tests (routine and high risk): smear
- For screening Pap tests (routine and high risk): liquid based
- Manual screening only
- ThinPrep Imager assisted screening
- FocalPoint (instrument only)
- FocalPoint (with manual screening)
- For diagnostic Pap tests: smear
- For diagnostic Pap tests: liquid based
- Manual screening only
- ThinPrep Imager assisted screening
- FocalPoint (instrument only)
- FocalPoint (with manual screening)
Sites
- Cervix, vagina, anus
Etiology
- Caused by a number of low risk and high risk HPVs (J Clin Pathol 2002;55:244, N Engl J Med 2003;348:518)
- Low risk HPV: 6, 11, 42, 43, 44, 53, 54, 57, 66
- High risk HPV: 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68
Clinical features
- Accounts for ~2.5% of all Pap test results (Arch Pathol Lab Med 2010;134:331)
- Most are transient infections with little risk for oncogenesis
- ~60% regress spontaneously (Int J Gynecol Pathol 1993;12:186)
- 30% persist
- 10% progress to high grade squamous intraepithelial lesion (HSIL)
- 18% of women with an low grade squamous intraepithelial lesion (LSIL) Pap result prove to have HSIL on biopsy (Am J Obstet Gynecol 2003;188:1406)
- < 1% of untreated progress to invasive cancer (Obstet Gynecol 1998;92:727)
Laboratory
- HPV testing may be used as part of screening, triage and surveillance (J Am Soc Cytopathol 2020;9:291)
- Initially endorsed as triage test for atypical squamous cells of undetermined significance (ASCUS) cytologic result in 2001
- Approved for:
- Cotesting in 2003
- Postcolposcopic / posttreatment follow up and risk stratification using partial genotype (HPV 16 / 18) in 2006
- Primary screening option in 2014
- 5 U.S. Food and Drug Administration (FDA) approved HPV testing platforms
- QIAGEN Hybrid Capture
- Hologic Cervista
- Hologic Aptima
- Roche Cobas: FDA approved for primary screening
- Becton Dickinson Onclarity: FDA approved for primary screening
- Note: HPV result plays no role in the cytologic examination or grading of SIL
Management
- 2019 American Society of Colposcopy and Cervical Pathology (ASCCP) risk based management consensus guidelines for abnormal cervical cancer screening tests and cancer precursors (J Low Genit Tract Dis 2020;24:102)
- Personalized risk based recommendations based on a patient's risk of CIN 3+, as determined by a combination of current results and past history (including unknown history)
Cytology description
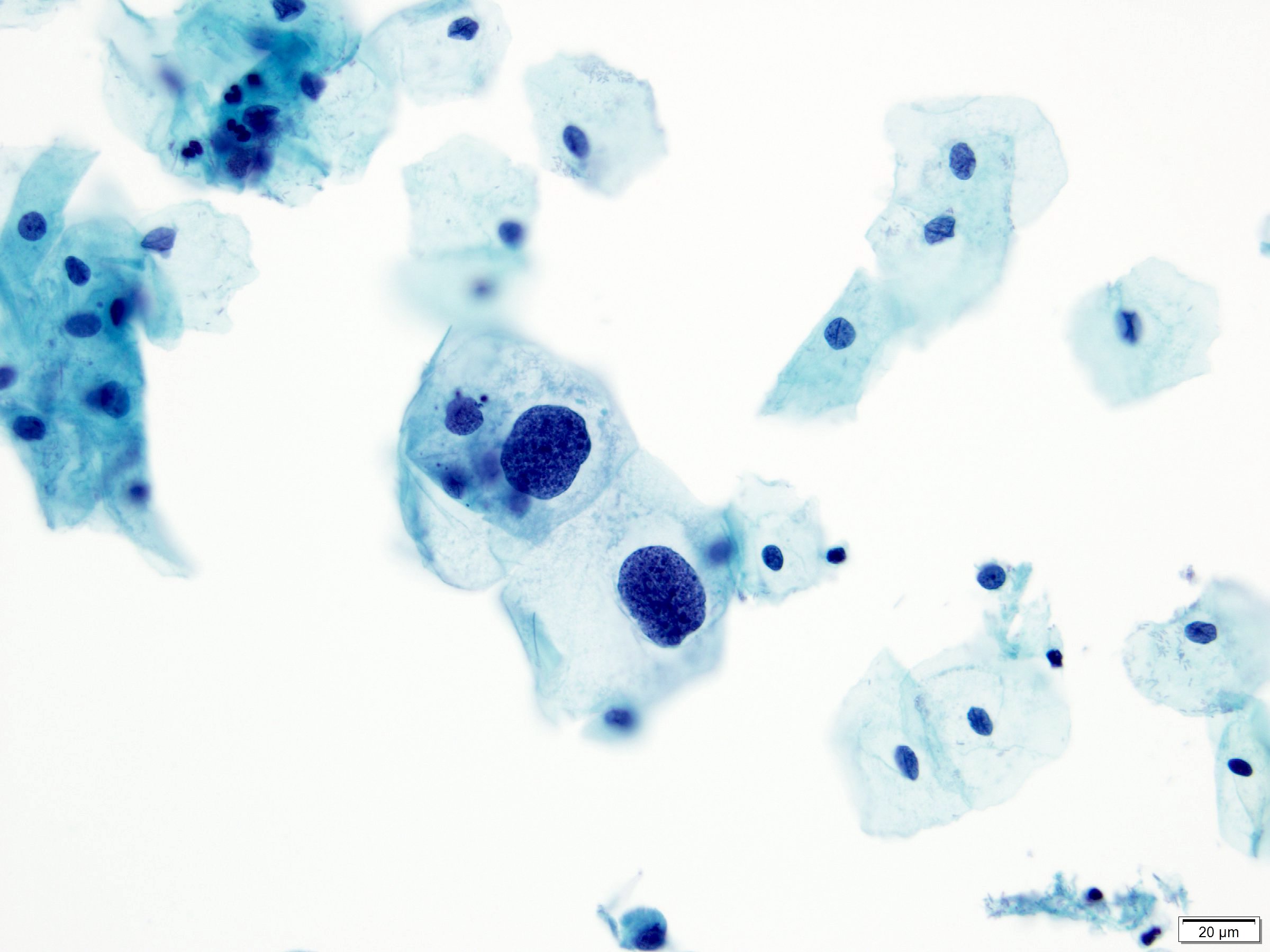
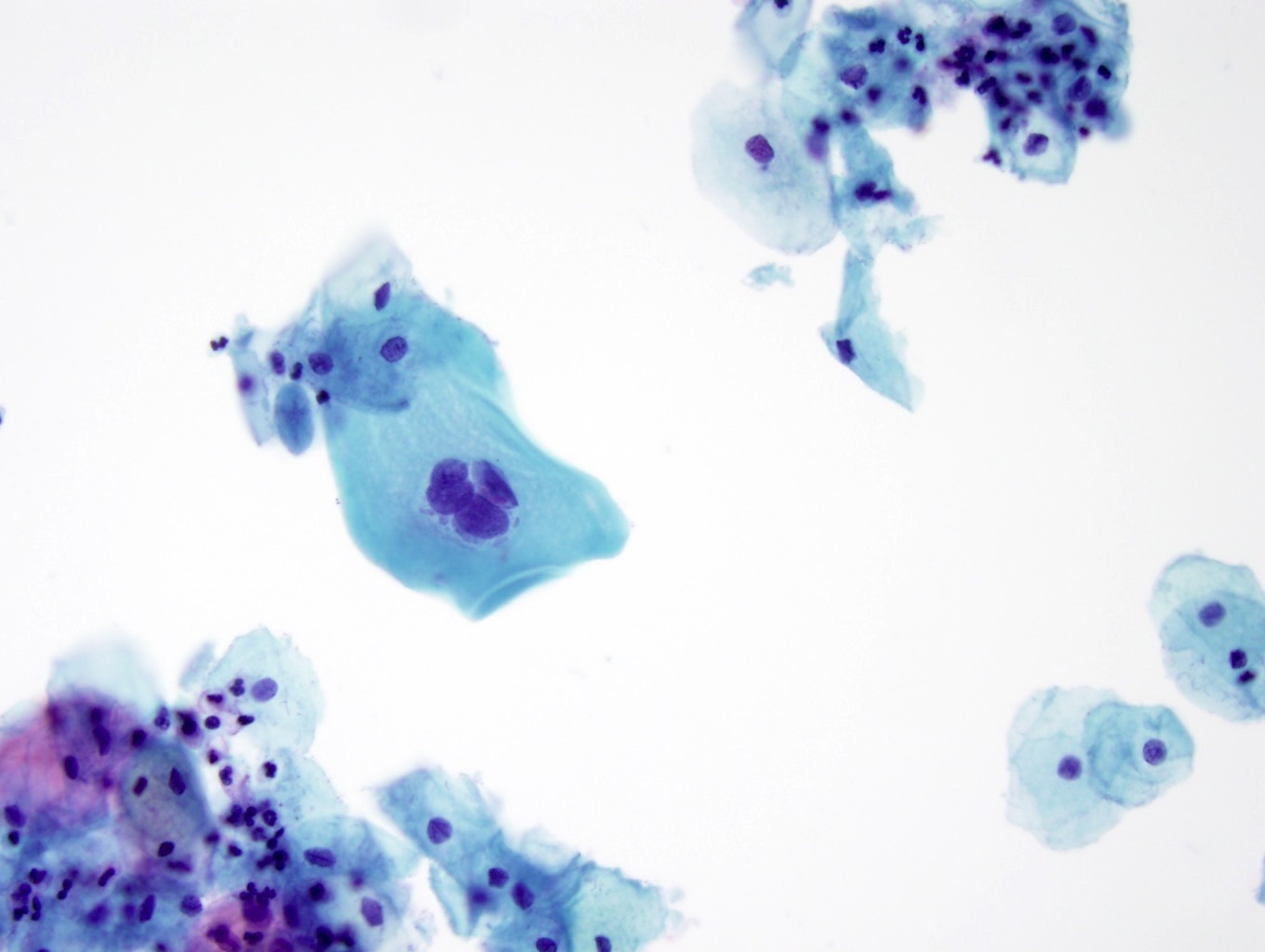
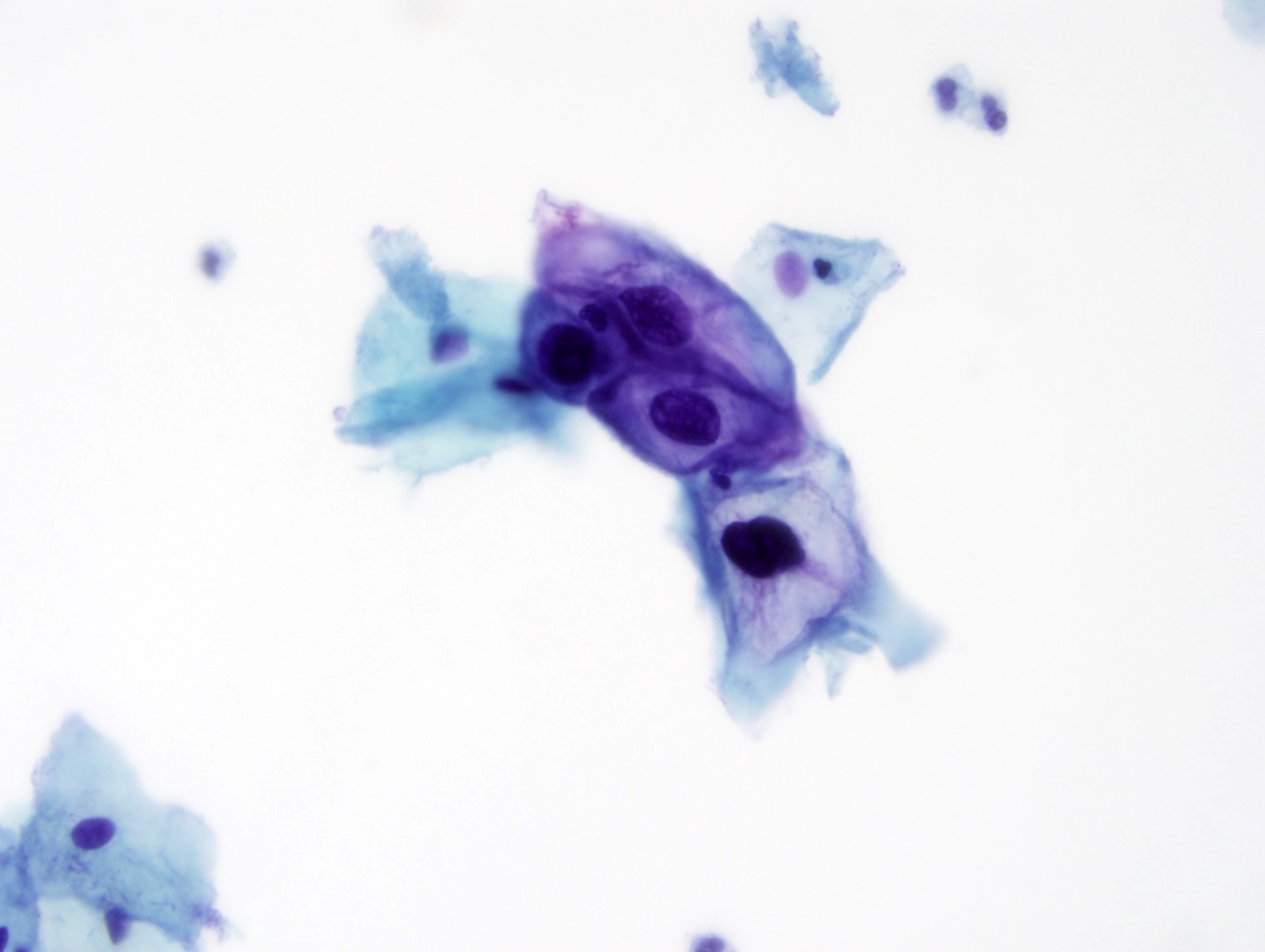
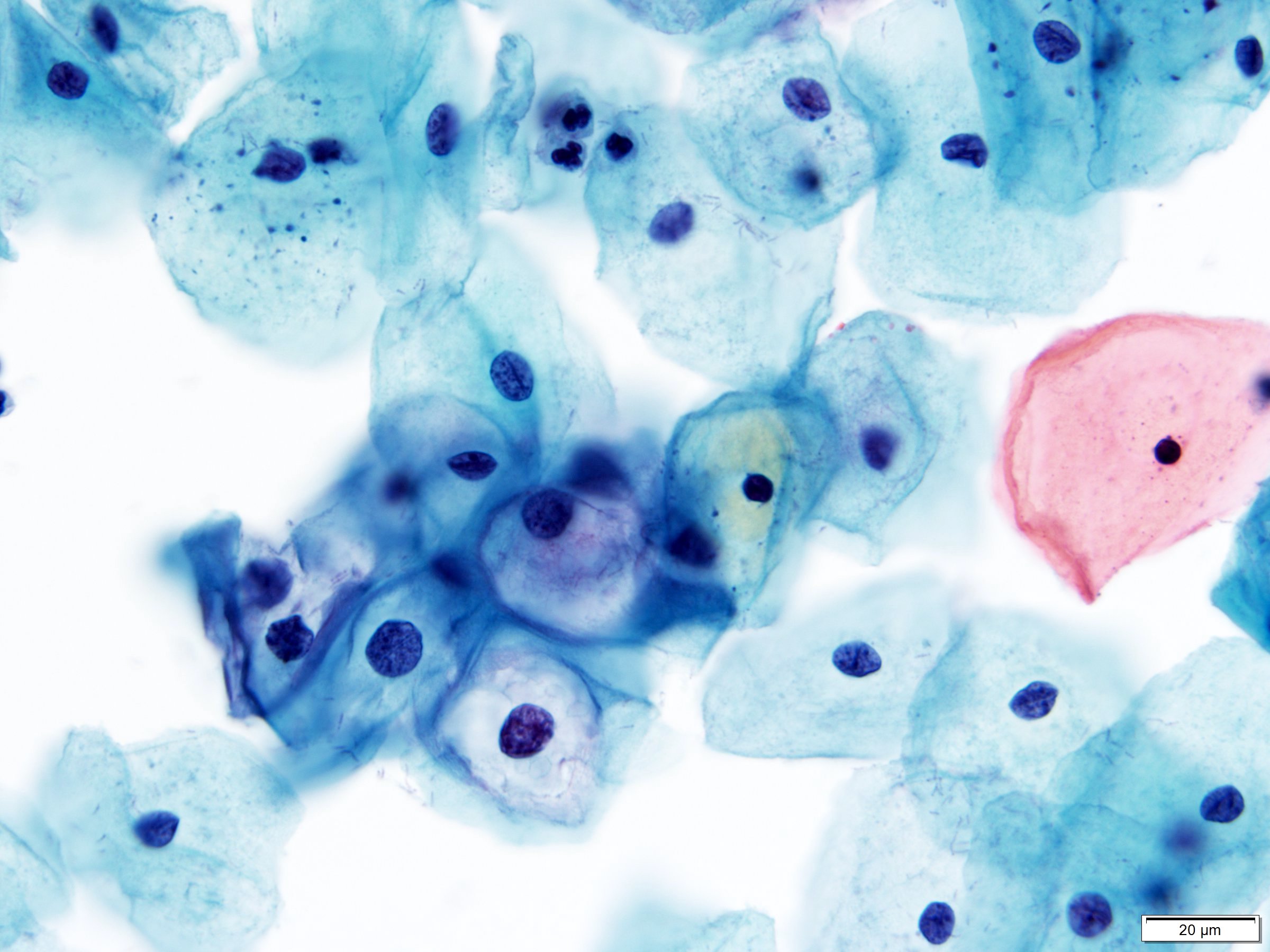
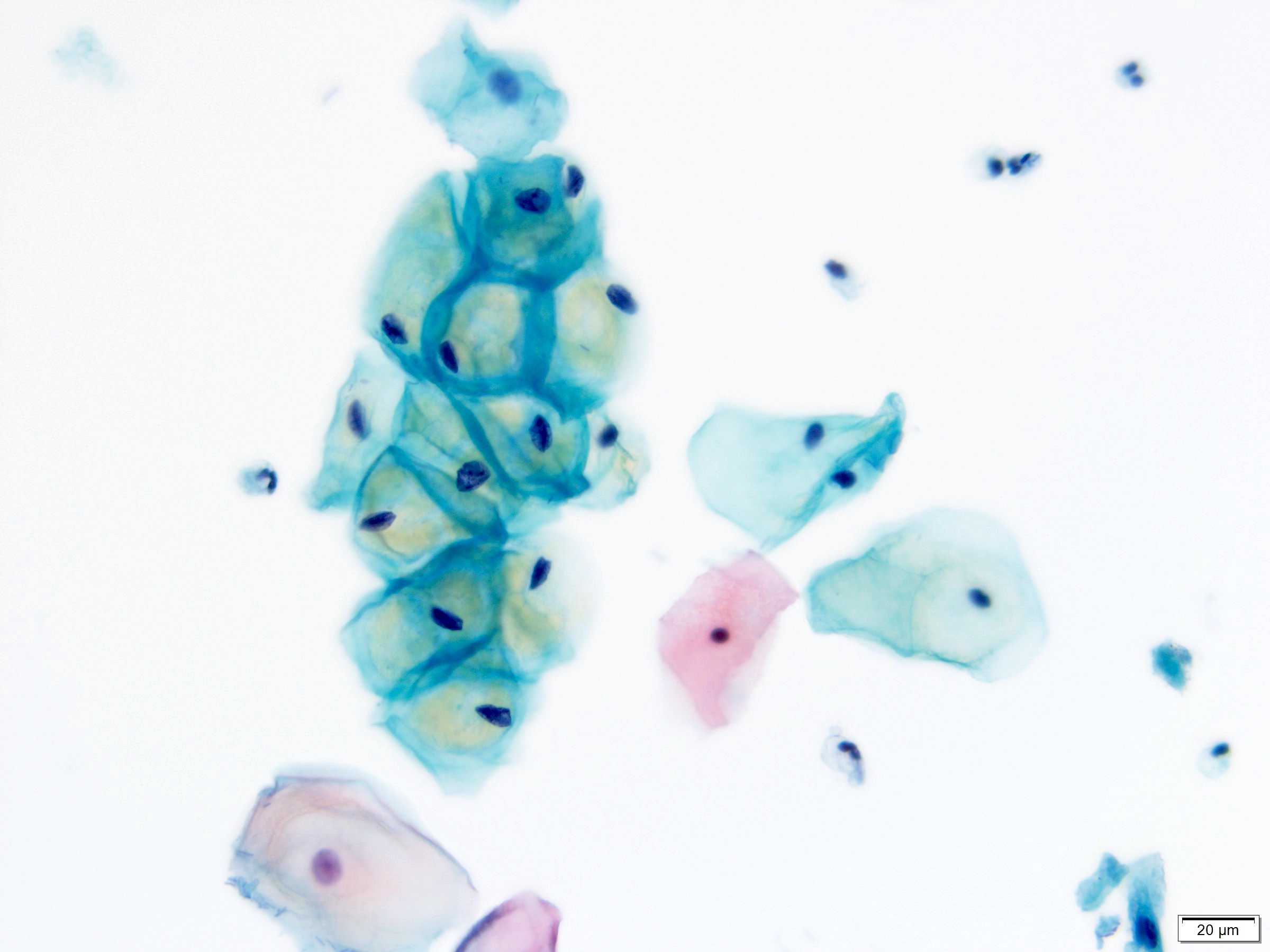
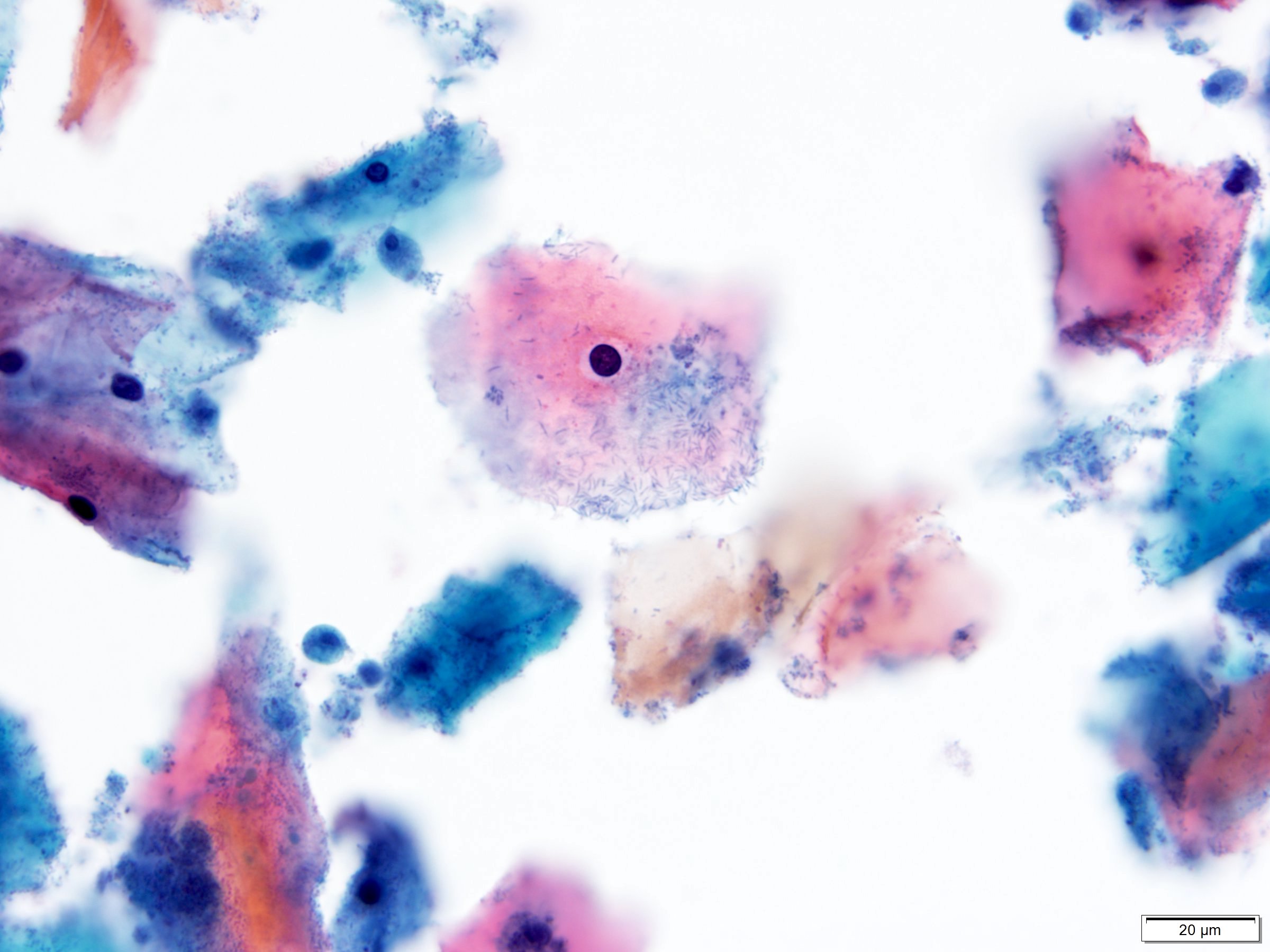
- Diagnostic criteria (Nayar: The Bethesda System for Reporting Cervical Cytology, 3rd Edition, 2015)
- Large, mature cells (equal in size to a normal superficial or intermediate squamous cell) with abundant cytoplasm
- Cells seen singly, in clusters, as well as in sheets
- Nuclear atypia
- Nuclear enlargement > 3x the area of normal intermediate nuclei
- Low but slightly increased N/C ratio
- Generally hyperchromatic but may be normochromatic
- Anisonucleosis
- Coarsely granular, smudgy or densely opaque chromatin
- Variable nuclear contours ranging from smooth to very irregular with notches
- Binucleation and multinucleation common
- Absent or inconspicuous nucleoli
- Cytoplasmic cavities (koilocytes): characteristic viral cytopathic feature
- Broad, sharply delineated clear perinuclear zone and a peripheral rim of densely stained cytoplasm
- Dense, eosinophilic cytoplasm of increased keratinization with little or no evidence of koilocytosis
- Koilocytosis or dense orangeophilia must be accompanied by nuclear abnormalities
- Large, mature cells (equal in size to a normal superficial or intermediate squamous cell) with abundant cytoplasm
Cytology images
Contributed by Lucy Jager, M.D. and Bonnie Choy, M.D.
Images hosted on other servers:
Sample pathology report
- Statement of adequacy:
- Satisfactory for evaluation
- Transformation zone component present
- Final interpretation:
- Epithelial cell abnormality, squamous cell
- Low grade squamous intraepithelial lesion (LSIL)
Differential diagnosis
- Pseudokoilocytosis:
- Small perinuclear halo without any significant nuclear abnormality
- Seen in association with reactive / inflammatory conditions like Trichomonas infection
- Glycogen cytoplasmic vacuolization appears yellow, refractile and cracked
- Small perinuclear halo without any significant nuclear abnormality
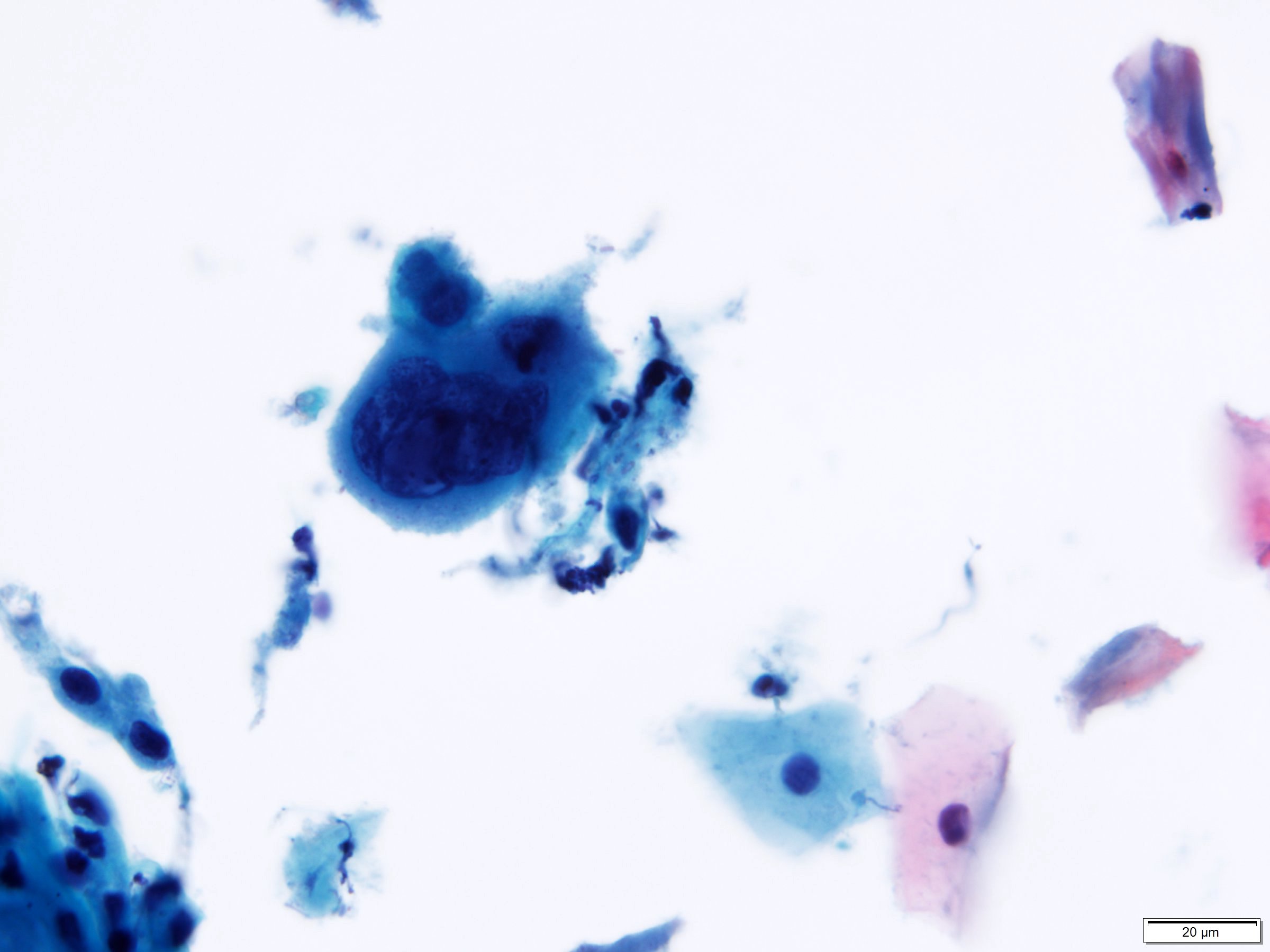
- Herpes cytopathic effect:
- Early herpes cytopathic effect shows nuclear enlargement and degenerative chromatin but lack other changes of HPV cytopathic effect (koilocytosis)
- Cells with classic features of herpes (multinucleation, nuclear molding, margination of chromatin and clear, ground glass nuclei) will also be present
- Radiation changes:
- Large, bizarre cells with normal N/C ratio
- Binucleation and multinucleation common
- Cytoplasmic vacuolization and polychromasia (2 toned) without perinuclear clearing and peripheral condensation
- Atypical squamous cells of undetermined clinical significance (ASCUS):
- Nuclei approximately 2.5 - 3x the area of the nucleus of a normal intermediate squamous cell or 2x the size of a squamous metaplastic cell nucleus
- Slightly increased N/C ratio
- Minimal nuclear hyperchromasia and irregular chromatin distribution or nuclear shape
- Nuclear abnormalities associated with dense orangeophilic cytoplasm (atypical parakeratosis)
- Cytoplasmic changes suggestive of HPV cytopathic effect (incomplete koilocytosis)
- Reactive endocervical cells:
- Enlarged, polygonal shaped cell with prominent nucleolus and granular cytoplasm
Board review style question #1
Which of the following is the correct interpretation of the cervical cytology shown above from a 32 year old woman?
- Atypical glandular cells, NOS
- Atypical squamous cells of undetermined significance (ASCUS)
- Benign reactive squamous cells
- High grade squamous intraepithelial lesion (HSIL)
- Low grade squamous intraepithelial lesion (LSIL)
Board review style answer #1
Board review style question #2
This routine cervical cytology specimen was obtained from a 33 year old woman. What is the correct interpretation?
- Atypical squamous cells cannot exclude HSIL (ASCH)
- Atypical squamous cells of undetermined significance (ASCUS)
- High grade squamous intraepithelial lesion (HSIL)
- Low grade squamous intraepithelial lesion (LSIL)
- Negative for intraepithelial lesion or malignancy (NILM)
Board review style answer #2