Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Pathophysiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Agarwal AN, Valente PT. Clear cell carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/cervixclearcell.html. Accessed January 21st, 2025.
Definition / general
- Malignant glandular neoplasm composed of clear or eosinophilic cells with varying architectural patterns, including solid, tubulocystic or papillary
- Accounts for ~3 - 4% of adenocarcinoma of the cervix
- HPV independent
Essential features
- Multiple architectural patterns with hyalinized stroma and hobnail cells
- Cytoplasm may be clear, eosinophilic or granular and may contain intracytoplasmic hyaline globules
- High nuclear grade, at least focally, contrasting with relatively low mitotic count and mildly increased Ki67
- HNF1β and napsin A positive; ER, PR and p16 negative; normal p53 expression in most cases (Int J Gynecol Pathol 2018;37:388, Am J Surg Pathol 2011;35:633)
- Women with history of in utero exposure to diethylstilbestrol (DES) are at higher risk for developing clear cell adenocarcinoma of the vagina and cervix (Cancer Causes Control 2022;33:1121)
Terminology
- Not preferred: mesonephroid carcinoma
ICD coding
- ICD-O: 8310/3 - clear cell adenocarcinoma, NOS
- ICD-10: C53.0 - malignant neoplasm of endocervix
- ICD-11: 2C77.1 & XH6L02 - adenocarcinoma of cervix uteri & clear cell adenocarcinoma, NOS
Epidemiology
- Accounts for 3 - 4% of adenocarcinoma of cervix
- Bimodal age distribution (J Midlife Health 2015;6:85)
- First peak occurs in women aged 17 - 37 years
- Second peak occurs in women aged 44 - 88 years
- Median age of diethylstilbestrol (DES) related clear cell carcinoma is 19 years, while median age of sporadic (non-DES associated) clear cell carcinoma is 51 years (Gynecol Oncol 2000;76:147)
- Majority of cervical clear cell carcinoma (~60%) is associated with in utero exposure to diethylstilbestrol (DES) (JAAPA 2017;30:49)
Pathophysiology
- Historically associated with intrauterine DES exposure; use declined after U.S. FDA warning in 1971 (NCI: Diethylstilbestrol (DES) Exposure and Cancer [Accessed 16 February 2023])
- Cervical endometriosis might contribute to the occurrence of clear cell carcinoma of the cervix in women without DES exposure (Br J Radiol 2009;82:e20, Int J Gynecol Pathol 2018;37:88)
- Observation of tuboendometrioid metaplasia adjacent to clear cell carcinoma lesions suggests it as a potential precursor lesion (Int J Gynecol Pathol 2022;41:105)
- Not related to high risk HPV infection (Int J Gynecol Cancer 2013;23:1084)
- Clear cell carcinoma in situ may be a precursor lesion to invasive clear cell carcinoma of the cervix (Int J Gynecol Pathol 2023;42:217)
Clinical features
- Abnormal uterine bleeding
- Abdominal pain
- Postcoital bleeding
- Abnormal vaginal discharge
- Physical examination shows polypoid / exophytic lesion, barrel shaped cervix or normal appearing cervix
- Rarely pelvic mass
- Abnormal pap smear
- Reference: Onco Targets Ther 2014;7:111
Diagnosis
- Can be made on a biopsy with classic morphologic patterns, which can be supported by napsin A immunohistochemical stain positivity
Prognostic factors
- Traditional prognostic factors include the following (Gynecol Oncol 2008;109:335)
- FIGO stage, in particular related to
- Lymph node status
- Parametrial involvement
- > One - third cervical stromal involvement
- Positive surgical margins
- Tumor diameter > 4 cm
- Lymph vascular space involvement
- FIGO stage, in particular related to
- DES independent cervical clear cell carcinoma does not seem to have a worse prognosis than squamous cell carcinoma of the cervix, when matched for stage (Gynecol Oncol 2000;76:331, Onco Targets Ther 2014;7:111)
- However, a large study of ~25,000 patients indicated that adenocarcinoma histology negatively impacts survival for both early and advanced stage carcinomas (Gynecol Oncol 2012;125:287)
- Though not statistically significant, patients with DES independent clear cell carcinoma had a worse 5 year survival rate (67%) compared to squamous cell carcinoma (80%) and non-clear cell carcinoma (77%) (Gynecol Oncol 2000;76:331)
- Cervical clear cell carcinoma has similar overall survival and recurrence free survival to gastric type endocervical adenocarcinoma; it also has poorer outcomes than HPV associated endocervical adenocarcinoma (Am J Surg Pathol 2022;46:1317)
- Median time to recurrence is 12 months overall (Gynecol Oncol 2008;109:335, Gynecol Oncol 2000;76:147)
- Common sites of relapse include pelvis, para-aortic lymph nodes and distant sites (Int J Gynecol Cancer 2014;24:S90)
- 3 year overall survival: 91% stage I and II versus 22% advanced stage (Gynecol Oncol 2008;109:335)
- 5 year progression free survival: 85% stage I - IIA and 42% stage IIB - IV
- 5 year overall survival: 90% stage I - IIA and 63% stage IIB - IV (Gynecol Oncol 2008;109:335)
- Lymph node status is a strong predictor of overall survival (80%) and progression free survival (31%) (Gynecol Oncol 2008;109:335, Gynecol Oncol 2000;76:331)
Case reports
- 12 year old girl with vaginal bleeding and no prior exposure of diethylstilbestrol with clear cell carcinoma of cervix (Sichuan Da Xue Xue Bao Yi Xue Ban 2021;52:534)
- 26 year old woman with cesarean radical hysterectomy in a triplet pregnancy complicated by clear cell carcinoma of the cervix (Int J Gynecol Cancer 2012;22:1198)
- 47 year old woman with synchronous invasive squamous cell carcinoma and clear cell carcinoma of the uterine cervix (Gynecol Oncol 2005;97:976)
- 52 year old woman with obstructed hemivagina and ipsilateral renal agenesis (OHVIRA) syndrome with uterine didelphys and clear cell carcinoma of the cervix (World J Oncol 2021;12:34)
- 52 year old woman with clear cell carcinoma of the cervix exhibiting choriocarcinomatous differentiation and mismatch repair protein abnormality (Int J Gynecol Pathol 2017;36:323)
- 56 year old woman with clear cell carcinoma of the uterine cervix and cervical endometriosis (Int J Gynecol Pathol 2018;37:88)
Treatment
- Due to rarity of the tumor, treatment guidelines are based on common cervical cancers (e.g., squamous cell carcinoma)
- Early stage (IA, IB1 and selected IIA1): surgery or radiation therapy or concurrent chemoradiation (NCCN: Clinical Practice Guidelines in Oncology - Cervical Cancer, Version 3.2019 [Accessed 17 February 2023])
- Surgery
- Fertility sparing: cone biopsy or radical trachelectomy with or without pelvic lymph node dissection
- Nonfertility sparing: simple or radical hysterectomy with sentinel lymph node mapping / pelvic lymph node dissection + para-aortic lymph node dissection
- Radiation therapy (RT): pelvic beam external beam RT (EBRT) with brachytherapy
- Surgery
- Advanced disease (IB2, II, III and IVA): platinum containing chemotherapy and EBRT
Gross description
- In non-DES exposure cases, the tumor arises in ectocervix or endocervix
- In DES exposure cases, the tumor most commonly arises in the ectocervix
- Tumor median size is 3.4 cm (Obstet Gynecol Int 2019;2019:9465375)
- Variable presentation: exophytic mass, barrel shaped cervix or normal appearing cervix (Onco Targets Ther 2014;7:111)
Gross images
Frozen section description
- Variable mix of patterns: tubulocystic, papillary and solid forms seen with clear to eosinophilic cytoplasm
Frozen section images
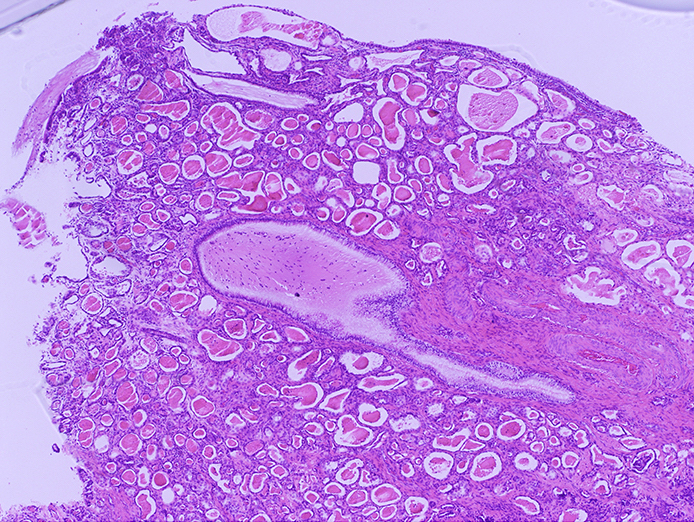
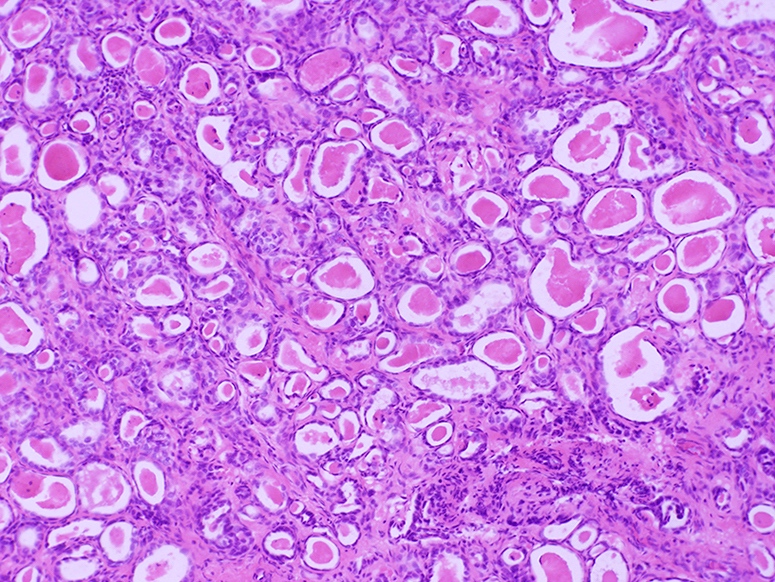
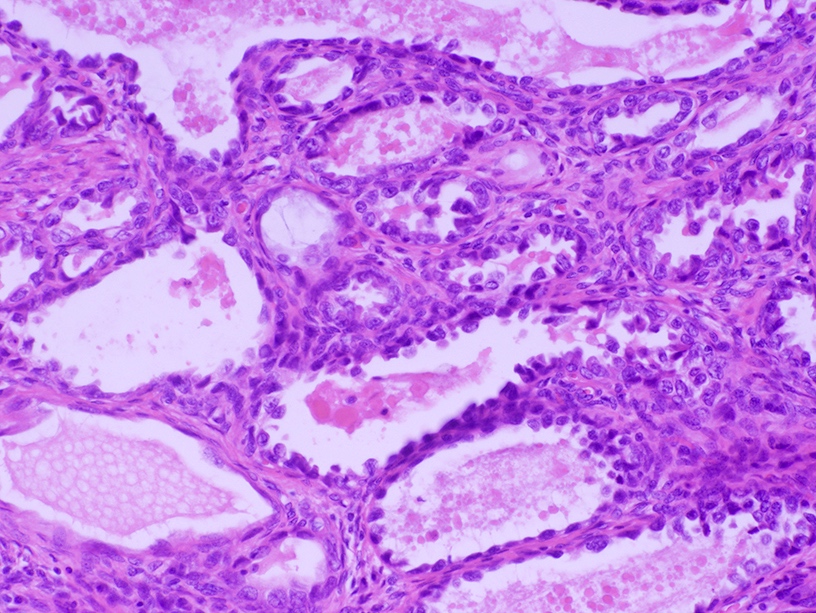
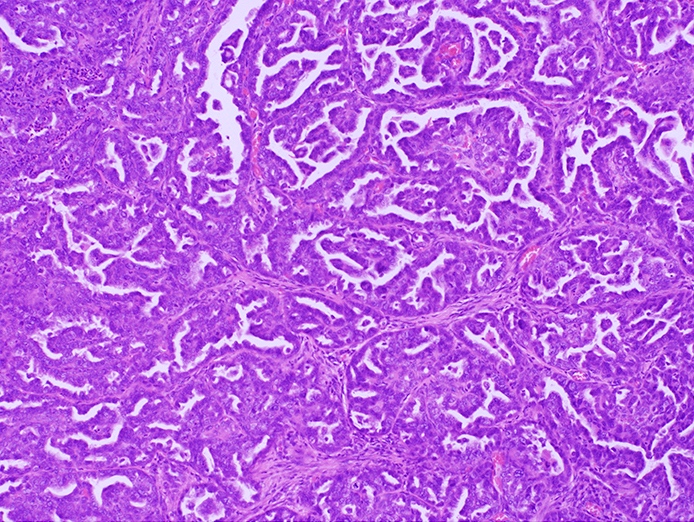
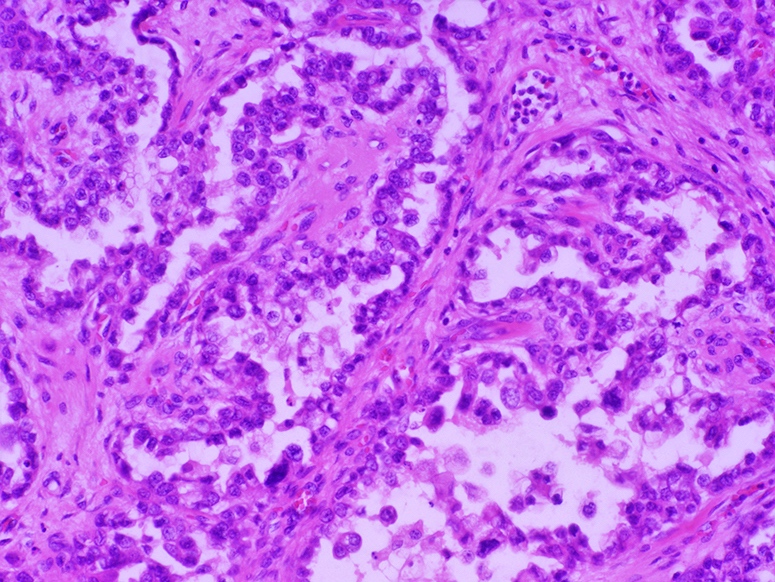
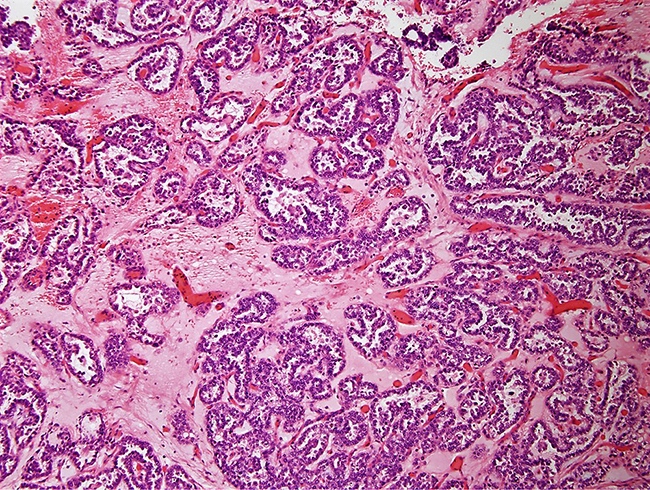
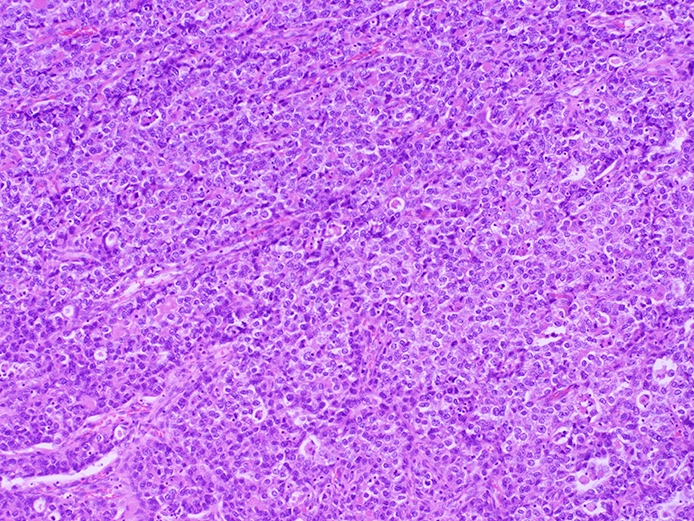
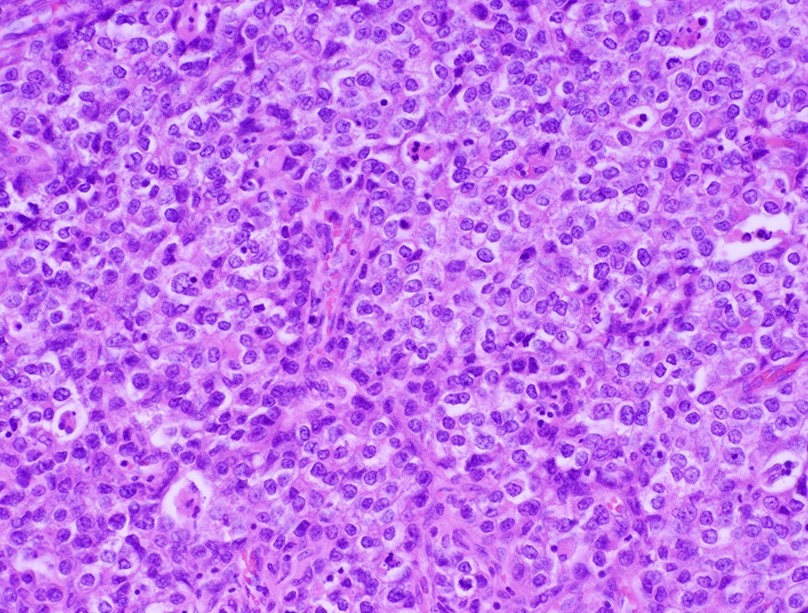
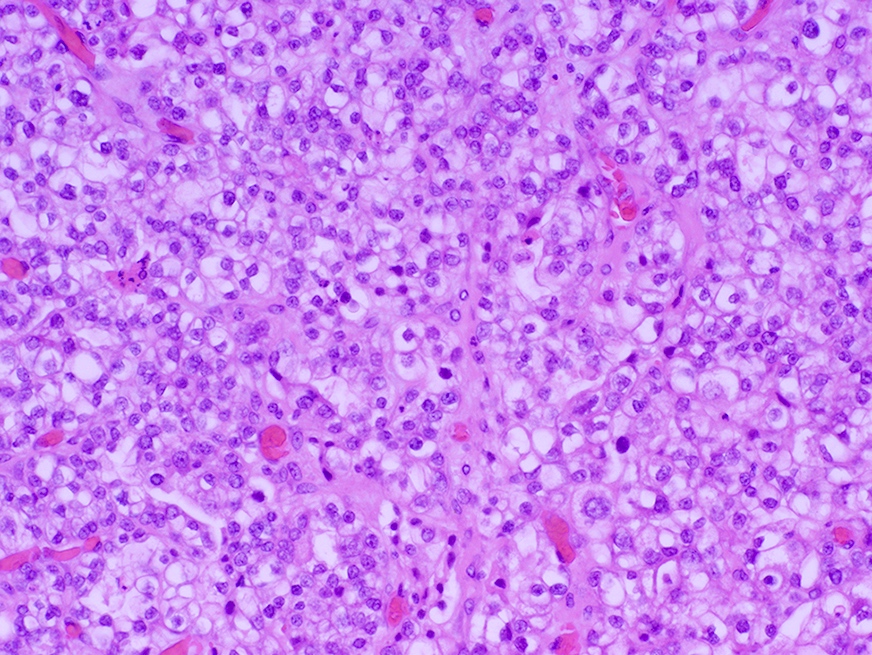
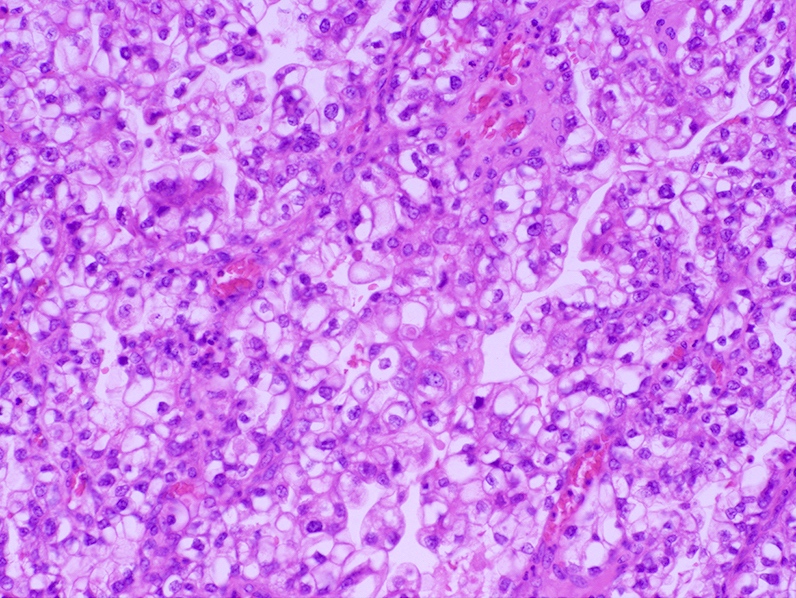
Microscopic (histologic) description
- 3 major patterns
- Tubulocystic pattern (most common): tubules lined by a single layer of bland cells or prominent hyperchromatic nuclei project into the apical cytoplasm forming hobnail appearance
- Papillary pattern (least common): papillae with central hyaline fibrous tissue cores lined by hobnail cells with hyperchromatic nuclei
- Solid pattern: nests of cells with clear to pale eosinophilic cytoplasm, notable nuclear atypia, focal gland formation and variable sized cytoplasmic vacuoles, simulating signet ring cell differentiation; appears to be more common in clear cell carcinoma of the cervix (Int J Gynecol Pathol 2018;37:388)
- Intracytoplasmic hyaline globules, especially in solid pattern
- Extensive stromal hyalinization may be present
- May be associated with abundant plasma cells and psammoma bodies
- Morphologic spectrum is comparable to that of endometrial and ovarian counterparts with few differences (Int J Gynecol Pathol 2018;37:388)
- Low mitotic index (0 - 5/10 high power fields) often encountered in cervical (85%) compared to endometrial and ovarian cases (72% and 50%, respectively)
- Necrosis or psammoma bodies are usually absent in endocervical cases (present in 38% and 6% in ovarian clear cell carcinoma and 59% and 5% endometrial clear cell carcinoma, respectively, without statistical significance)
Microscopic (histologic) images
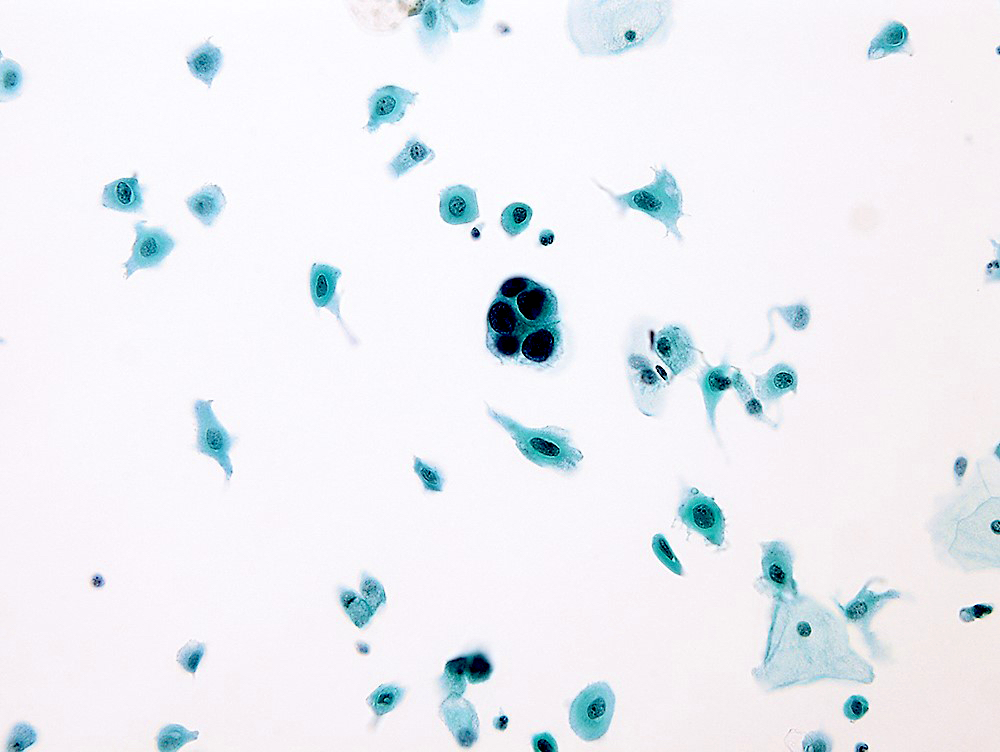
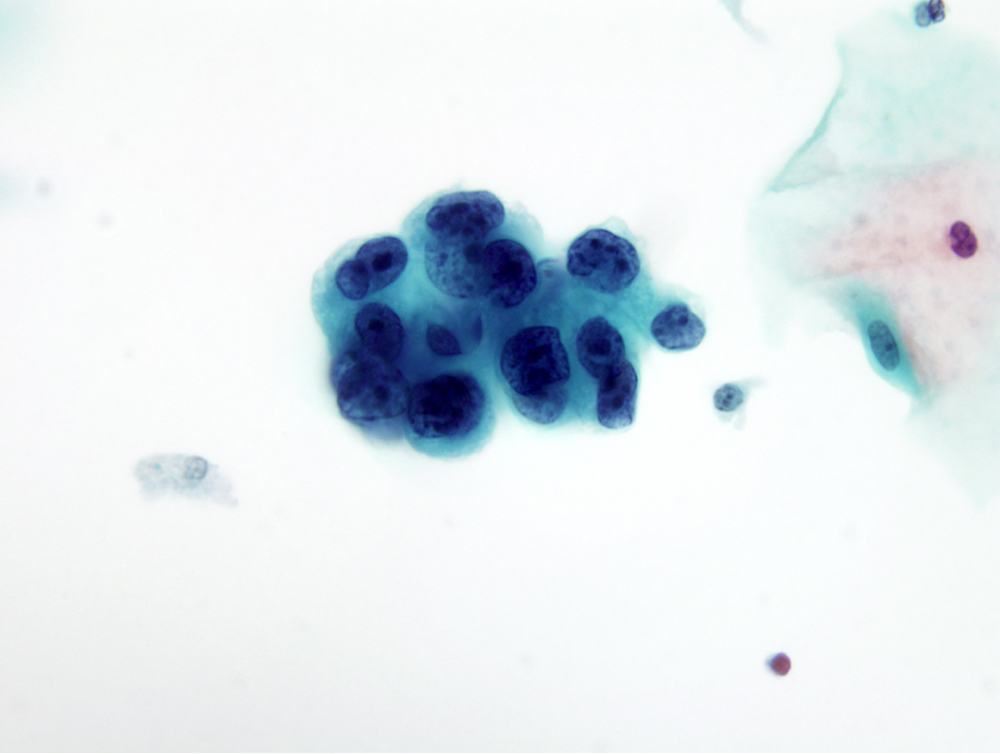
Cytology description
- Pap test
- Cells arranged in sheets, clusters or papillae
- Cells have delicate, vacuolated, glycogen rich cytoplasm or finely granulated cytoplasm, naked nuclei and a tigroid background
- Nuclei are large, pale and round with prominent nucleoli
- Reference: Diagn Cytopathol 2020;48:804
Positive stains
- Pancytokeratin (AE1 / AE3, CAM5.2)
- CK7, CK8, CK18, CK19
- HNF1β (97%)
- Napsin A (74%)
- Racemase / AMACR (diffuse)
- p16 (focally positive in tumor cells)
- Ki67 index (~50%) (Int J Gynecol Pathol 2018;37:388)
- Epithelial membrane antigen (EMA)
- References: Technol Cancer Res Treat 2023;22:15330338221149297, Virchows Arch 2019;475:537, Int J Environ Res Public Health 2022;19:16652
Negative stains
- CK20
- High molecular weight CK 34 beta E12
- GATA3
- ER, PR (rarely focally expressed)
- Vimentin, SMA, desmin
- Chromogranin, synaptophysin, CD56, NSE
- CAIX
- CEA, unlike most other types of cervical adenocarcinoma
- p53 (14% have strong, diffuse mutant pattern staining) (Int J Gynecol Pathol 2018;37:388)
Electron microscopy description
- Continuous lamina densa, numerous mitochondria and rough endoplasmic reticulum, abundant glycogen and blunt microvilli
- Vesicular aggregates in nucleoplasm, perinuclear cytoplasm or between membranes of nuclear envelope (Acta Cytol 1976;20:262)
Electron microscopy images
Molecular / cytogenetics description
- Rare case has been associated with Lynch syndrome (Int J Mol Sci 2018;19:979)
- Rare cases of clear cell carcinomas of endocervical origin may be associated with POLE mutation (Gynecol Oncol Rep 2019;28:15)
- Pathogenic genetic alterations in the Hippo signaling pathway (including recurrent somatic mutations in WWTR1 S89W) have been identified in patients with cervical clear cell carcinoma (J Pathol 2022;257:635)
Videos
Clear cell neoplasms of the gynecologic tract
Sample pathology report
- Cervix, 12:00, biopsy:
- Clear cell adenocarcinoma (see comment)
- Comment: Depth of invasion is at least 2 mm. Immunohistochemical stains for mismatch repair proteins show retained nuclear expression of MLH1, PMS2, MSH2 and MSH6.
Differential diagnosis
- Benign entities:
- Arias-Stella reaction:
- History of intrauterine or ectopic pregnancy, progestin treatment or gestational trophoblastic disease
- Hypersecretory glands; may be striking and produce a papillary or cribriform pattern
- Decidual change in stromal cells
- Focally enlarged, hyperchromatic nuclei that typically protrude into the gland lumen, giving the cell a hobnail appearance; nuclei may be smudged and have pseudoinclusions
- No / rare mitosis (low Ki67 index), no infiltration
- Microglandular hyperplasia:
- Small, markedly crowded glands lined by a single layer of bland cuboidal cells and usually associated with squamous metaplasia
- Has 2 distinct cell layers (luminal and basal / reserve cell); p63 highlights the basal / reserve layer or squamous metaplasia
- May present with sheets of clear cells
- Small bland nuclei and low mitotic activity should distinguish it from clear cell carcinoma
- Arias-Stella reaction:
- Malignant entities:
- Alveolar soft part sarcoma:
- Mesonephric adenocarcinoma:
- Develops deep in the lateral wall of the cervix (corresponding to the location of mesonephric duct remnants); invades the wall of the cervix
- Lacks clear cells and hobnails cells
- Does not display the admixture of tubulocystic, papillary and solid patterns
- Positive for CK7, EMA, CD10, calretinin and GATA3
- Metastatic clear cell renal cell carcinoma:
- Non-clear cell carcinomas of endometrial origin:
- May be difficult to differentiate on biopsy specimens
- Squamous cell carcinoma:
- Urothelial carcinoma:
Additional references
Board review style question #1
Which of the following statements regarding clear cell adenocarcinoma of the cervix is true?
- All cases are linked to perinatal exposure of diethylstilbestrol (DES)
- Histologically, there are cords of cells with abundant eosinophilic cytoplasm
- Immunohistochemical profile of this neoplasm includes positivity for CK7, AE1 / AE3, CAM 5.2, HNF1β and napsin A
- Median age of diagnosis is 5 years
Board review style answer #1
C. Immunohistochemical profile of this neoplasm includes positivity for CK7, AE1 / AE3, CAM 5.2, HNF1β and napsin A. Answer A is incorrect because not all cases are linked to DES exposure. Answer B is incorrect becauase cytoplasm in clear cell carcinoma of the cervix may be clear, eosinophilic or granular. Answer D is incorrect because the median age of diethylstilbestrol (DES) related clear cell carcinoma is 19 years and the median age of sporadic (non-DES associated) clear cell carcinoma is 51 years.
Comment Here
Reference: Cervix - Clear cell carcinoma
Comment Here
Reference: Cervix - Clear cell carcinoma
Board review style question #2
Board review style answer #2
C. p63, napsin A and vimentin. Clear cell carcinoma of the cervix is negative for p63 and vimentin while positive for napsin A. Answer B is incorrect because MelanA, GFAP and S100 are markers for melanoma and glial origin markers. Answer A is incorrect because it includes markers for gastrointestinal tract, pancreatic and lung origin markers. Answer D is incorrect because synaptophysin, chromogranin and Ki67 are neuroendocrine markers.
Comment Here
Reference: Cervix - Clear cell carcinoma
Comment Here
Reference: Cervix - Clear cell carcinoma