Table of Contents
Definition / general | Essential features | Terminology | Diagrams / tables | Clinical features (clinicoanatomical correlation) | Radiology description | Radiology images | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Videos | Additional references | Board review style question #1 | Board review style answer #1Cite this page: Mohamed N, Asirvatham JR. Anatomy. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/cervixanatomy.html. Accessed April 1st, 2025.
Definition / general
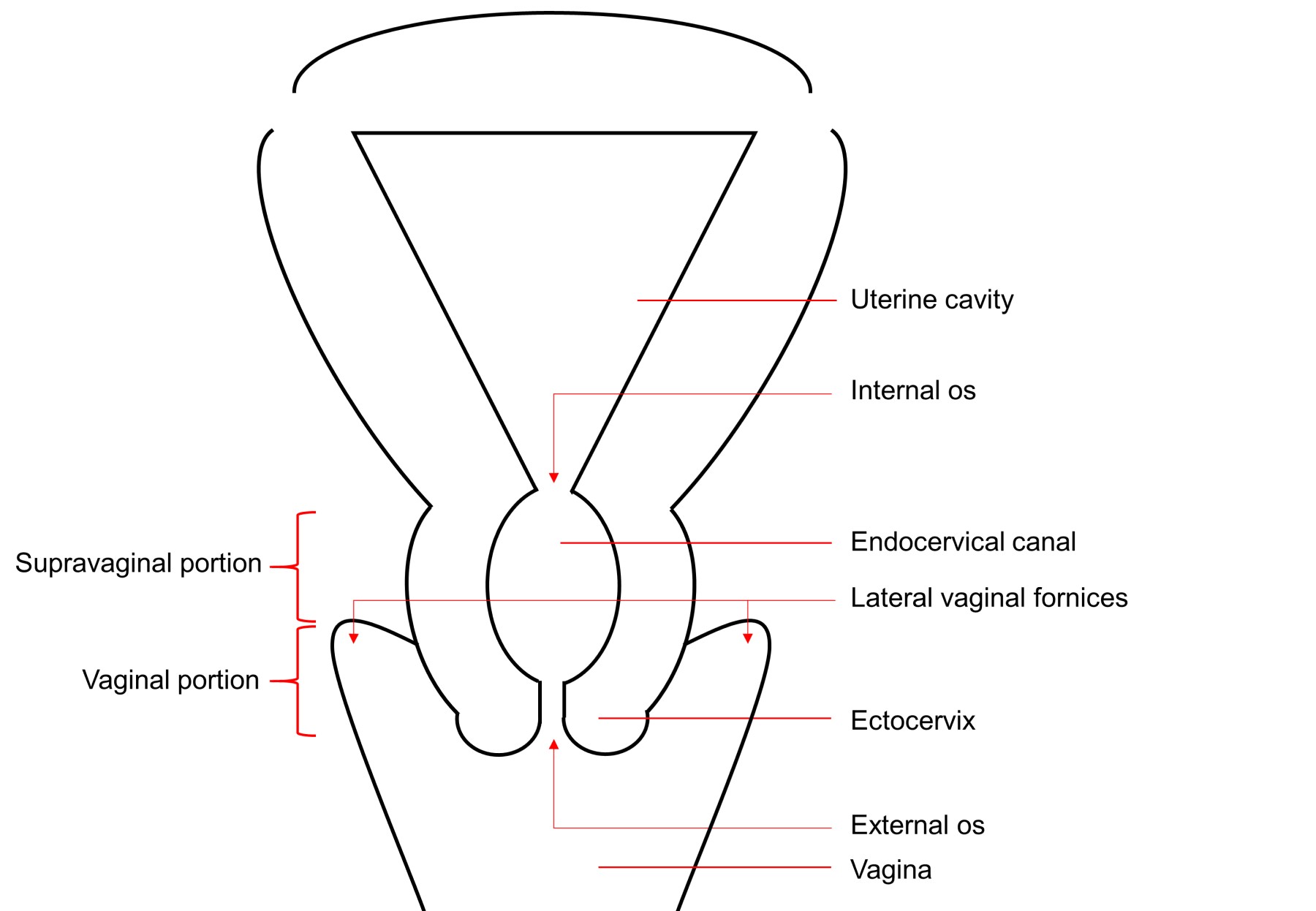
- The cervix is the lowest, cylindrical / fusiform part of the uterus that connects the body of uterus (corpus uteri) to the vagina and is composed of 2 regions, the endocervical canal and ectocervix
Essential features
- Internal os connects the uterine cavity to the endocervical canal
- Endocervical canal is lined by columnar mucinous epithelium
- External os connects the endocervical canal to the vagina
- Ectocervix is distal (exterior to the external os), projects into the vagina and is lined by stratified squamous epithelium
- Squamous epithelium meets the glandular epithelium at the squamocolumnar junction (SCJ); at birth the SCJ is usually near the external os and is identifiable as a sharp line
- SCJ is dynamic and migrates during the lifespan of the woman
- Epithelium between the 2 sites of the SCJ is called the transformation zone (TZ); cervical cancer mostly originates from this region
Terminology
- Cervix uteri (Latin: neck of uterus)
Diagrams / tables
Clinical features (clinicoanatomical correlation)
- Identification of the transformation zone (TZ) is very important during colposcopy
- Childhood to early reproductive period: original SCJ is located near external os
- Reproductive period: SCJ moves outward to ectocervix (ectropion or ectopy)
- Caused by elongation of the endocervix under the effect of estrogen
- Reproductive period to perimenopause: formation of a new SCJ
- Caused by squamous metaplasia of the endocervical epithelium
- Metaplasia begins at original SCJ and moves toward external os
- New SCJ moves towards the external os
- TZ is the epithelium between original and new SCJ
- Peri to postmenopausal: accelerates migration of new SCJ towards external os
- Lack of estrogen causes the cervix to shrink
- Vaginal portion (portio vaginalis):
- Most visible portion of the cervix upon speculum examination and colposcopy
- Divided into anterior and posterior lips (Indian J Radiol Imaging 2021;31:454)
- Supravaginal portion:
- Anteriorly abuts and is separated from bladder by connective tissue
- Posteriorly is covered by peritoneum that forms lining of cul de sac
- Fornices (anterior, posterior, right, left):
- Recesses formed by reflection of upper vagina (vault) around vaginal portion of the cervix
- Blood supply:
- Uterine artery (branch of internal iliac) (StatPearls: Lower Genitourinary Trauma [Accessed 21 December 2022])
- Lymphatics:
- Most commonly through supraureteral paracervical pathway to interiliac, external iliac and common iliac lymph nodes (Eur J Surg Oncol 2010;36:298)
- Supporting ligaments (apical support) (Int Urogynecol J 2012;23:1483)
- Cardinal / Mackenrodt / lateral cervical ligaments:
- Fibromuscular bands from lower uterine segment / cervix to lateral pelvic walls
- Provide main support for cervix
- Uterosacral ligaments:
- Connective tissue surrounding cervix and vagina that extends towards vertebrae
- Cardinal / Mackenrodt / lateral cervical ligaments:
- SCJ frequently disappears up into the endocervical canal in the postmenopausal period and may no longer be visible on colposcopic examination
Radiology description
- MRI (T2W) can show 4 distinct anatomical zones of the cervix (listed from inner cervix outward): 1) central hyperintense mucous in cervical canal, 2) high signal intensity endocervical mucosa and glands, 3) hypointense fibrous stroma, 4) outer intermediate signal intensity of loose stroma (Indian J Radiol Imaging 2021;31:454)
Clinical images
Gross description
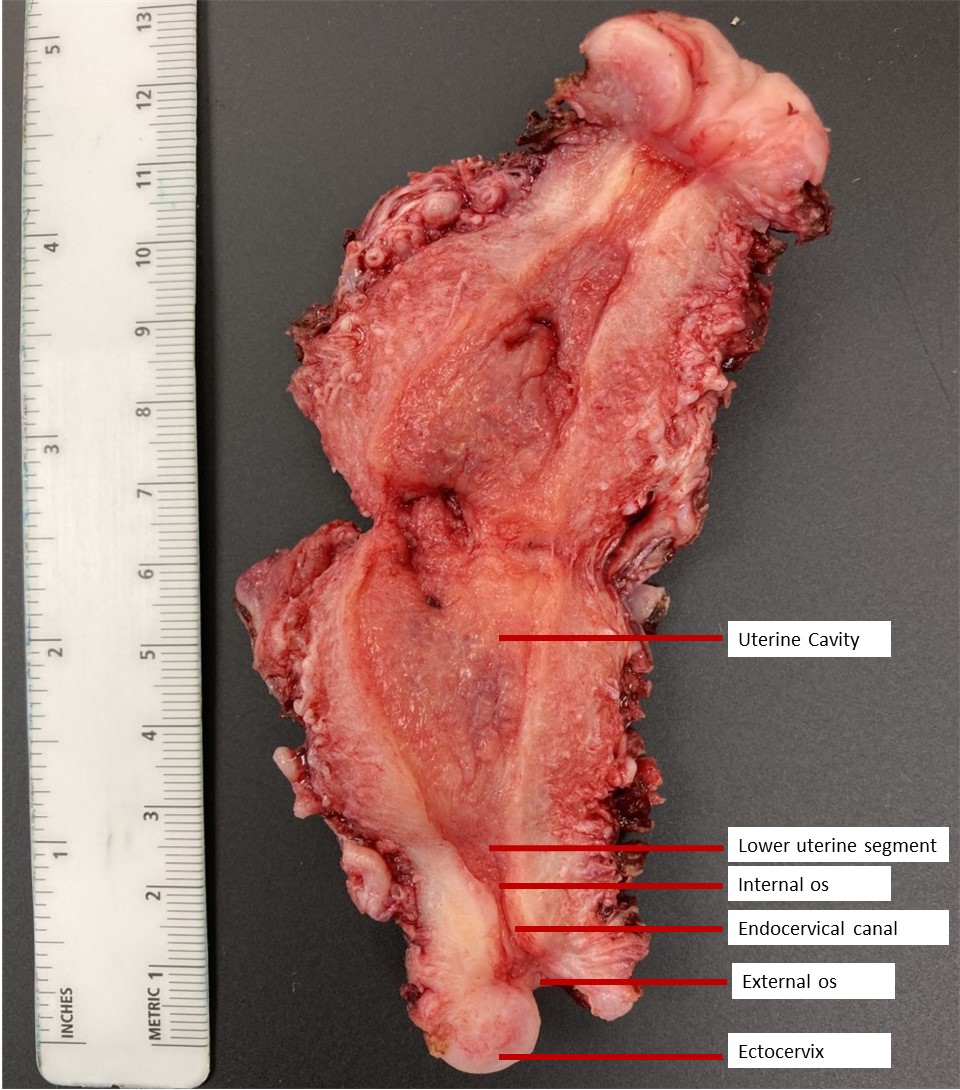
- Cervix is the lower fibromuscular portion of the uterus
- Usually described as cylindrical but the anterior and posterior walls may oppose
- Size and shape of the cervix depends on age, parity and hormonal status (Indian J Radiol Imaging 2021;31:454)
- In the prepubertal state, the cervix is approximately half to one - third of the uterus
- In nonpregnant adult women, the cervix is approximately one - third of the uterus
- In postmenopausal women, the cervix is approximately half of the uterus
- Average size is 3 - 4 cm in length x 2 cm in diameter
- Internal os (isthmus):
- Opening of endocervical canal into uterine cavity
- Usually a narrowing between the uterine corpus and supravaginal portion
- External os:
- Opening of endocervical canal into vagina
- Bound by anterior and the posterior lips
- Round (3 - 5 mm) in nullipara
- Slit-like (≈1 cm) in parous women
- Endocervical canal / endocervix:
- Extends from internal os to external os
- Fusiform in shape
- 7 - 8 mm in diameter (widest in reproductive age group)
- Contains longitudinal or oblique mucosal ridges called plicae palmatae / arbor vitae uteri on anterior and posterior walls
- Ectocervix (exocervix):
- Part of the vaginal portion of the cervix that lies external to external os
- Has smooth glistening surface
- The demarcation between the upper endocervix and the lower uterine segment is generally not grossly evident; this demarcation relies on microscopic examination of the gland differentiation and can be challenging, even in that context
- The boundary between the ectocervix and the vagina can be difficult to demarcate, both by gross and microscopic examination; clinical correlation is recommended, especially when dealing with questions of staging
Gross images
Microscopic (histologic) description
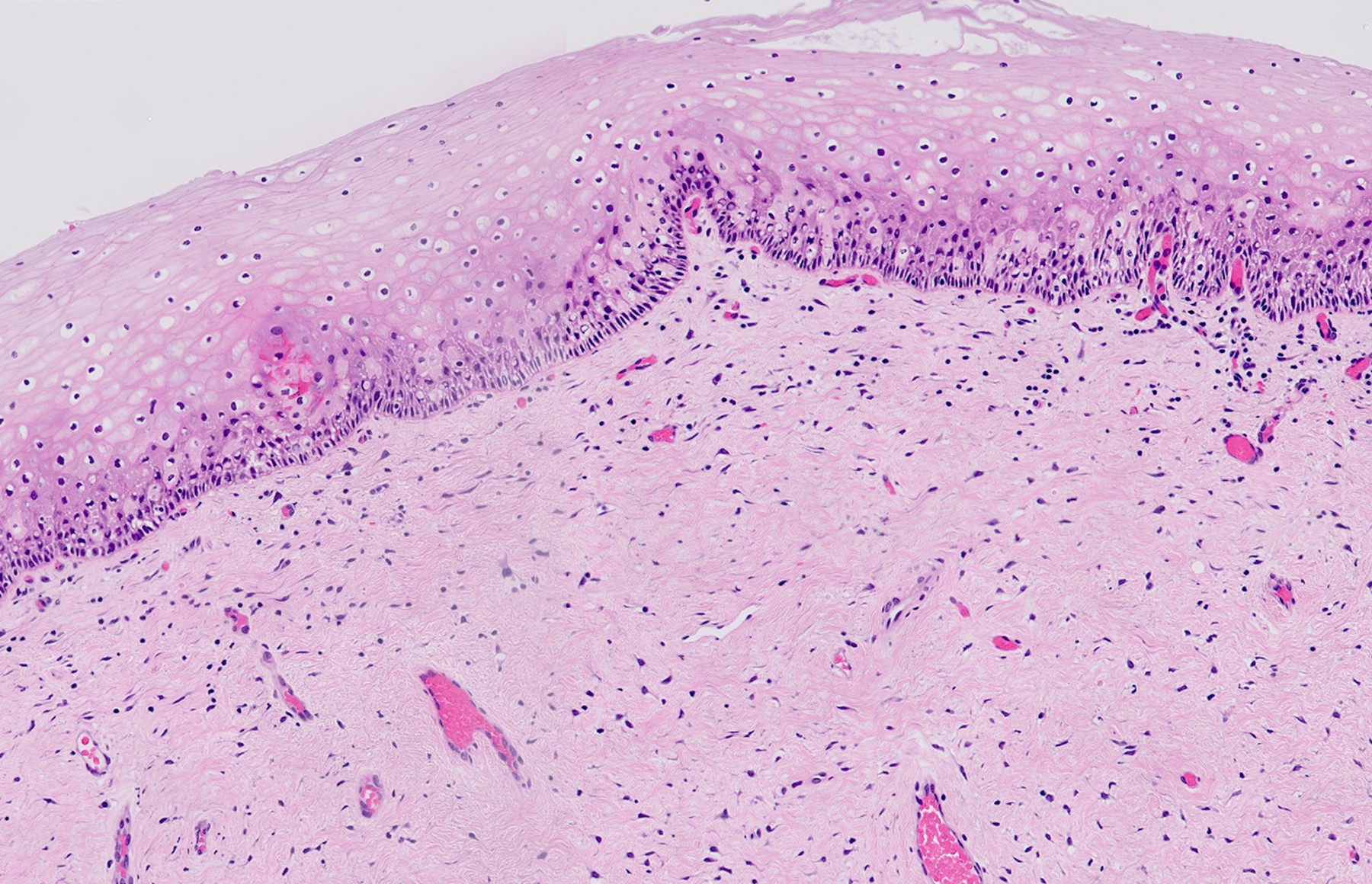
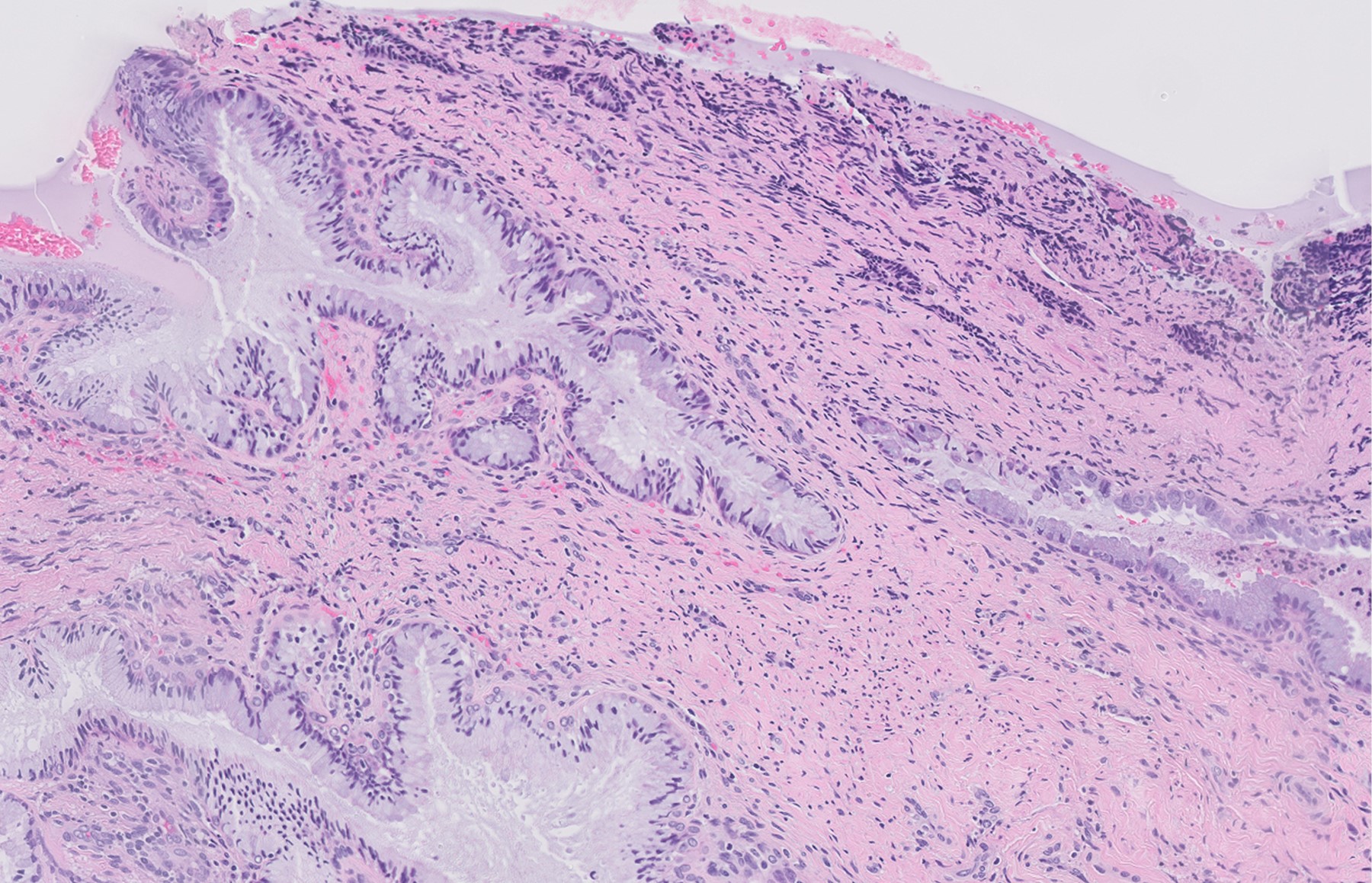
- Cervix is composed mainly of fibromuscular connective tissue (StatPearls: Cervical Squamous Cell Carcinoma [Accessed 21 December 2022])
- Endocervical canal is lined by a single layer of mucus secreting glandular epithelium
- Ectocervix is lined by nonkeratinized stratified squamous epithelium
- Squamous epithelium meets the glandular epithelium at the squamocolumnar junction (SCJ)
- SCJ is dynamic and influenced by hormonal levels
- Original SCJ lies in the endocervical canal, after adolescence and childbirth the SCJ moves to lie in the ectocervix
- Epithelium between the 2 sites of SCJ is called the transformation zone (TZ); cervical cancer mostly originates from this region
- See Cervix - Histology for details
Microscopic (histologic) images
Cytology description
Cytology images
Positive stains
- Squamous epithelium: p63, p40, CK5/6, ER (basal, parabasal, intermediate layers)
- Endocervical epithelium: CK7, PAX8, CEA, ER, PR
- Low Ki67 / MIB1 proliferation rate
- Reference: J Clin Pathol 2003;56:164, Arch Pathol Lab Med 2016;140:148
Videos
Histology of the cervix
Additional references
Board review style question #1
Board review style answer #1
C. Prepubertal. After puberty the original squamocolumnar junction migrates due to the elongation of the cervix under the influence of estrogen and is located in the ectocervix. The acidic environment of the vagina is thought to induce metaplasia of the everted endocervical epithelium and formation of a new squamocolumnar junction, which migrates towards the external os and possibly into the endocervical canal during the lifespan of the woman. In postmenopausal women the new SCJ may not be visible on colposcopy. As the original SCJ migrates, it results in ectropion which is seen as a bright red patch on colposcopy. The original SCJ is the junction between the bright red area (endocervical epithelium) and the peripheral pale area (ectocervical epithelium). Nabothian cysts may develop in the transformation zone when the opening of the endocervical gland is obstructed by squamous metaplasia leading to retention of mucus.
Comment Here
Reference: Cervix - Anatomy
Comment Here
Reference: Cervix - Anatomy