Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Preston PA, Skala SL. Adenoid basal carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/cervixadenoidbasal.html. Accessed April 1st, 2025.
Definition / general
- Epithelial tumor composed of small, basaloid cells forming nests or cords
- It typically has an infiltrative growth pattern, although desmoplasia should not be present (Am J Surg Pathol 1988;12:134, Arch Pathol Lab Med 2021;145:891)
Essential features
- Nests of basaloid cells with low grade features
- No desmoplastic stromal response
- Associated with high risk human papillomavirus (HPV)
- p16 block positivity
- No known metastatic potential when occurring in pure form
Terminology
- Adenoid basal epithelioma, low grade adenoid basal tumor (Oncol Rep 2019;41:1769)
ICD coding
- ICD-O: 8098/3 - adenoid basal carcinoma
- ICD-11: 2C77.1 & XH70J2 - adenocarcinoma of cervix uteri & adenoid basal carcinoma
Epidemiology
- This lesion occurs most frequently in postmenopausal women (mean: 64.6 years); however, the lesion has been reported in patients as young as 20 years old (Oncol Rep 2019;41:1769, Hum Pathol 2005;36:82, Int J Gynecol Pathol 2002;21:327, Diagn Pathol 2006;1:20)
- In studies with HPV PCR results, the vast majority of cases are positive for high risk HPV, most commonly HPV 16 (Hum Pathol 2005;36:82, Int J Gynecol Pathol 1997;16:301, Hum Pathol 2000;31:740)
- The vast majority of reported invasive adenoid basal carcinomas (as opposed to low grade noninvasive adenoid basal tumors or adenoid basal hyperplasia) are positive for p16 and high risk HPV ISH (Hum Pathol 2012;43:2255, Int J Gynecol Pathol 2016;35:82)
Sites
- Cervix, usually transformation zone, similar to other high risk HPV related lesions
Pathophysiology
- Typically associated with, although not arising from, high grade squamous intraepithelial lesion (HSIL)
- There has been speculation that basal cell hyperplasia may be a precursor lesion (Obstet Gynecol 1971;37:807, Int J Gynecol Pathol 2002;21:327)
- Theorized to arise from cervical reserve cells (Am J Surg Pathol 1999;23:448, Int J Gynecol Pathol 2002;21:327, Int J Gynecol Pathol 2016;35:82)
- Newer theories suggest origin from the Skene gland (female counterpart of prostate glands) (Am J Surg Pathol 2024;48:238, Pathology 2021;53:193, Int J Gynecol Pathol 2021;40:400)
Etiology
- Infection with high risk HPV
Clinical features
- These lesions are typically found incidentally and do not manifest grossly or clinically unless associated with another, more aggressive tumor (Arch Pathol Lab Med 2021;145:891)
Diagnosis
- Microscopic examination of biopsy, loop electrosurgical excision procedure (LEEP) / cone or hysterectomy
- Pure adenoid basal carcinoma can only be definitively diagnosed in a well sampled excision specimen with negative margins
- In reports for biopsies, it is prudent to include a comment noting that this morphology sometimes co-occurs with other forms of invasive carcinoma (affecting prognosis)
Prognostic factors
- In its pure form, adenoid basal carcinoma does not metastasize and has an excellent prognosis
- Excision is typically curative (Arch Pathol Lab Med 2021;145:891)
- When coexisting with other neoplasms, the prognosis is expected to be that of the more aggressive tumor type (Arch Pathol Lab Med 2021;145:891)
Case reports
- 20 year old woman with HSIL and incidental finding on subsequent LEEP specimen (Diagn Pathol 2006;1:20)
- 22 year old woman with HSIL and incidental finding on subsequent LEEP specimen (J Menopausal Med 2013;19:154)
- 54 year old woman with postmenopausal abnormal uterine bleeding (Balkan Med J 2012;29:453)
- 80 year old woman with uterine prolapse and an incidental finding in the cervix (Int J Clin Exp Pathol 2018;11:1758)
Treatment
- Excision is curative
Gross description
- Typically, grossly unremarkable unless associated with another neoplasm
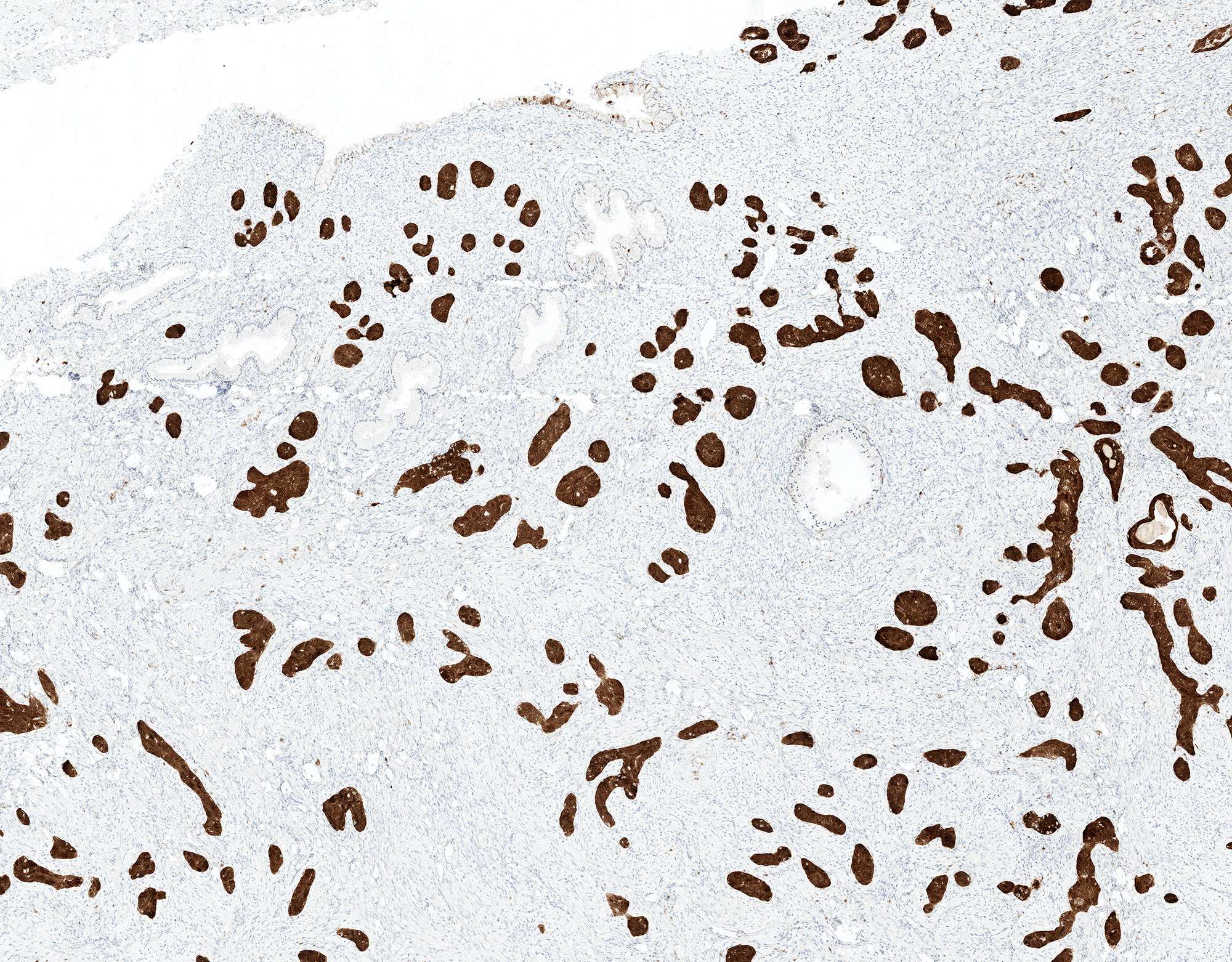
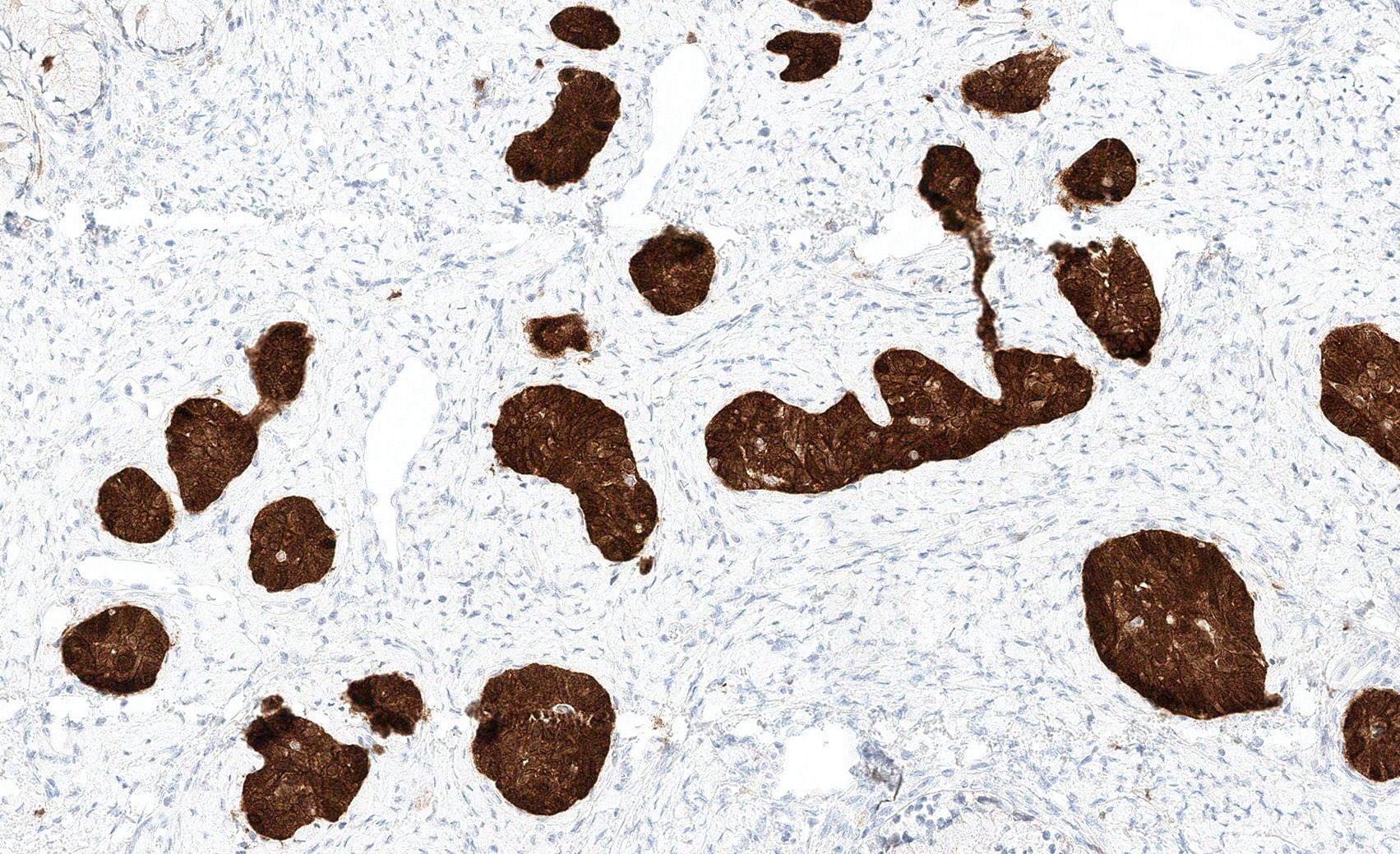
Microscopic (histologic) description
- Generally accepted features of pure adenoid basal carcinoma include absent to minimal mitotic activity, infrequent necrosis and a low degree of cytologic atypia (Arch Pathol Lab Med 2021;145:891)
- ~15% are present as a component of a mixed invasive tumor (Diagn Pathol 2006;1:18)
- Per the 5th edition of the WHO classification of tumors
- Essential
- Non-mass forming lesion
- Infiltrative small nests or cords of morphologically bland basaloid cells
- Absence of stromal reaction
- Desirable: p16 or HPV determination
- Essential
- Infiltrative nests or cords of cytologically bland, basophilic cells with minimal cytoplasm
- Nests may display peripheral palisading, like other basaloid tumors
- May have central squamous differentiation, cystic change, clear cell change
- Deepest point of invasion is typically < 1 cm
- No desmoplastic stromal reaction
- Adenoid basal carcinoma is associated with HSIL in > 90% of cases or may be associated with another type of invasive carcinoma (in which case it should be called mixed carcinoma, with a comment on the additional components present and their relative percentages) (Hum Pathol 2012;43:2255, Hum Pathol 2005;36:82, Int J Gynecol Pathol 2016;35:82)
Microscopic (histologic) images
Cytology description
- While these lesions are seldom diagnosed with cervicovaginal cytology, they have been described as sheets of small, hyperchromatic cells with oval nuclei, fine chromatin and indistinct nucleoli (J Pathol Transl Med 2015;49:396, Diagn Cytopathol 1996;14:172)
Positive stains
- p16: block positivity
- p63: positive in basaloid cells
- NKX3.1: glandular components show at least focal nuclear staining (Am J Surg Pathol 2024;48:238, Pathology 2021;53:193, Int J Gynecol Pathol 2021;40:400)
- References: Diagn Pathol 2006;1:18, Hum Pathol 2012;43:2255, Hum Pathol 2005;36:82, Int J Gynecol Pathol 2016;35:82
Negative stains
- CD117 (Int J Gynecol Pathol 2012;31:25)
- CK17: negative in central areas of squamous metaplasia (J Low Genit Tract Dis 2019;23:77)
Molecular / cytogenetics description
- Studies have employed various methodologies to detect high risk HPV, including RNA in situ hybridization (ISH), DNA ISH and polymerase chain reaction (PCR) (Am J Surg Pathol 1999;23:448, Hum Pathol 2005;36:82, Int J Gynecol Pathol 2016;35:82)
Sample pathology report
- Cervix, loop electrosurgical excision procedure (LEEP):
- Adenoid basal carcinoma (0.8 cm), arising in association with high grade squamous intraepithelial lesion (CIN 3); margins negative (see comment)
- Comment: The adenoid basal carcinoma in this specimen is seen in its pure form, with no features of a more aggressive tumor type. Adenoid basal carcinoma has no known metastatic potential when occurring in its pure form.
Differential diagnosis
- Squamous cell carcinoma - basaloid and well differentiated (Arch Pathol Lab Med 2021;145:891):
- Desmoplastic stromal response may be seen
- Higher degree of mitotic activity
- More frequent necrosis
- Often positive for CK17
- Adenoid basal hyperplasia / basal cell hyperplasia (Arch Pathol Lab Med 2021;145:891):
- Adenoid cystic carcinoma (Oncol Rep 2019;41:1769, Int J Gynecol Pathol 2012;31:25):
- Not currently listed as a distinct entity in the WHO classification for tumors of the cervix
- Significantly worse prognosis
- More likely to be symptomatic
- Larger cellular nodules, often with cribriform sieve-like pattern
- More nuclear atypia with more frequent mitoses and possible comedonecrosis
- Positive for CD117
- Negative for p16 when present as pure adenoid cystic carcinoma (Am J Surg Pathol 2016;40:529)
- Adenoid cystic morphology is often seen admixed with adenoid basal carcinoma, squamous cell carcinoma or small cell carcinoma; in these cases, p16 and high risk HPV are positive (Am J Surg Pathol 2016;40:529)
- May be prudent to reserve definitive diagnosis of cervical adenoid cystic carcinoma for tumors with MYB fusion
- Ectopic prostate tissue (prostatic metaplasia):
Additional references
Board review style question #1
Which of the following viruses or virus strains is most strongly associated with adenoid basal carcinoma of the cervix?
- Epstein-Barr virus (EBV)
- Human immunodeficiency virus (HIV)
- Human papillomavirus (HPV) 11
- Human papillomavirus (HPV) 16
Board review style answer #1
D. Human papillomavirus (HPV) 16. HPV 16 is a high risk strain of HPV and is the most common high risk strain identified in cases of adenoid basal carcinoma of the cervix.
Answer A is incorrect because Epstein-Barr virus (EBV) is not associated with adenoid basal carcinoma of the cervix, nor is it associated with other gynecologic tumors. Rather, EBV is associated with nasopharyngeal and gastric carcinomas as well as several types of lymphoma (J Cancer Res Clin Oncol 2022;148:31).
Answer C is incorrect because HPV 11 is a low risk strain of HPV and is one of the strains most associated with genital warts. It is not known to be associated with malignancies (Arch Gynecol Obstet 2012;286:1261).
Answer B is incorrect because HIV is not associated with adenoid basal carcinoma. Individuals with HIV are at a greater risk for infection with high risk HPV and subsequent development of high grade squamous intraepithelial lesions (HSIL) and HSIL is commonly associated with adenoid basal carcinoma; however, there is currently no evidence to suggest that infection with HIV is directly associated with development of adenoid basal carcinoma (N Engl J Med 2018;378:1029).
Comment Here
Reference: Adenoid basal carcinoma
Comment Here
Reference: Adenoid basal carcinoma
Board review style question #2
The finding shown above is seen in a cervical loop electrosurgical excision procedure (LEEP) specimen from a 50 year old woman. What is the expected clinical course after complete excision?
- Benign outcome
- Local recurrence
- Metastasis to pelvic lymph nodes
- Progression to invasive squamous cell carcinoma
Board review style answer #2
A. Benign outcome. Adenoid basal carcinoma, in its pure form, has no known metastatic potential and has excellent prognosis.
Answers B, C and D are incorrect because pure adenoid basal carcinoma has an excellent prognosis and complete excision is curative.
Comment Here
Reference: Adenoid basal carcinoma
Comment Here
Reference: Adenoid basal carcinoma