Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1Cite this page: Al Dallal H, Salih ZT. LSIL / CIN I. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/cervixLSIL.html. Accessed April 3rd, 2025.
Definition / general
- Usually transient / self limited infection by human papillomavirus (low risk or high risk HPV)
- This category includes:
- Flat low grade squamous intraepithelial lesion (LSIL) / cervical intraepithelial neoplasia (CIN) I
- Exophytic / papillary LSIL (can be immature or mature)
Essential features
- Low grade squamous lesion caused by low or high risk HPV
- Koilocytes in the upper layers are characteristic
- Majority of LSIL regress spontaneously
Terminology
- Bethesda terminology: low grade squamous intraepithelial lesion (LSIL), use for cytology or cervical biopsies; recommended by LAST project and adopted by the World Health Classification of Female Genital Tumours (IARC 2020) (Arch Pathol Lab Med 2012;136:1266)
- Alternative terminology (no longer recommended): mild squamous dysplasia, cervical intraepithelial neoplasia I (CIN I)
- Exophytic forms: immature condyloma, mature condyloma / giant condyloma) (Am J Surg Pathol 2013;37:300, Hum Pathol 1998;29:641)
ICD coding
- ICD-10: N87.0 - mild cervical dysplasia
Epidemiology
- Young women < 40 years old but can occur in any age group
- LSIL cells are found in about 2% of all Pap smears (Obstet Gynecol Clin North Am 2008;35:599)
Sites
- HPV associated LSIL can involve:
- Cervix
- Vagina
- Vulva
- Anus
- Penis
- Scrotum
Pathophysiology
- LSIL is a heterogenous group caused by
- Low risk HPV: 6, 11, 42 and 44
- High risk HPV: 16, 18, 31, 33, 35, 45, 52 and 58
- HPV is a member of the papovavirus family and consists of a virion containing double stranded, circular DNA surrounded by a protein capsid
- HPV has 6 E (early) genes (E1, E2, E4, E5, E6, E7) and 2 L (late) genes
- Called E and L genes depending on when they are expressed during the cycle
- HPV needs a human host cell to replicate
- HPV infects squamous cells (a population of reserve / metaplastic cells in the transformation zone of the cervix) (Proc Natl Acad Sci U S A 2012;109:10516)
- HPV infection begins in the basal layers of the epithelium with expression of the E genes
- E4 protein of HPV interact with filaggrin (a cytokeratin binding protein), which leads to loss of specific cytokeratin from the cell and collapse of matrix
- As the cells mature and move toward the surface, L1 and L2 genes are expressed, which are necessary for the viral capsid proteins' transcription
- In LSIL, the HPV DNA does not integrate into the host DNA and remains in free episomal form; this allows for replication of the virus
- Koilocytes are filled with complete virions, ready to be discharged
Etiology
- Low risk HPV in most cases
- Exophytic LSIL, both immature and mature, is caused by HPV types 6 and 11 (Am J Surg Pathol 2013;37:300, Hum Pathol 1998;29:641)
- High risk HPV: 25 - 30% of the LSIL cases (Mod Pathol 2016;29:1501)
Clinical features
- Asymptomatic
- Found incidentally on Pap smear screening, cervical biopsy or hysterectomy
Diagnosis
- Pap smear (cervical cytology screening)
- Cervical biopsy
Prognostic factors
- 85.3% of LSILs regress, 7.3% persist, 7.3% progress to HSIL and 0.15% progress to invasive cancer (Mod Pathol 2016;29:1501)
- p16+ LSIL has a higher risk of progression to HSIL (Cancer Cytopathol 2016;124:58, Am J Obstet Gynecol 2009;201:488.e1)
Treatment
- Women 30 years of age and older
- Pap+ and no HPV test or HPV+ → colposcopy
- Pap+ and HPV- → repeat Pap or cotesting in 1 year → if Pap+ or HPV+ → colposcopy; if both negative, repeat cotesting in 3 years
- Women aged 21 - 24 years
- Colposcopy is not recommended; follow up in 1 year
- Pregnant women
- Deferring colposcopy until 6 weeks postpartum is acceptable
- Postmenopausal women
- HPV testing, repeat cytologic testing at 6 months and 12 months or colposcopy
- Types of available vaccines
- HPV bivalent vaccine (Cervarix) will only protect against HPV 16 and 18
- HPV quadrivalent vaccine (Gardasil) will protect against HPV types 6, 11, 16 and 18
- HPV 9 valent vaccine, recombinant (Gardasil 9) can protect against HPV types 6, 11, 16, 18, 31, 33, 45, 52 and 58
- Reference: Obstet Gynecol 2013;121:829, National Comprehensive Cancer Network: NCCN Guidelines [Accessed 2 June 2021]
Gross description
- Flat lesions usually do not produce a grossly identifiable lesion
- Appears white after application of 3% acetic acid (acetowhite) on colposcopy examination
- Exophytic lesions can occasionally be seen grossly as small and friable frond-like lesions
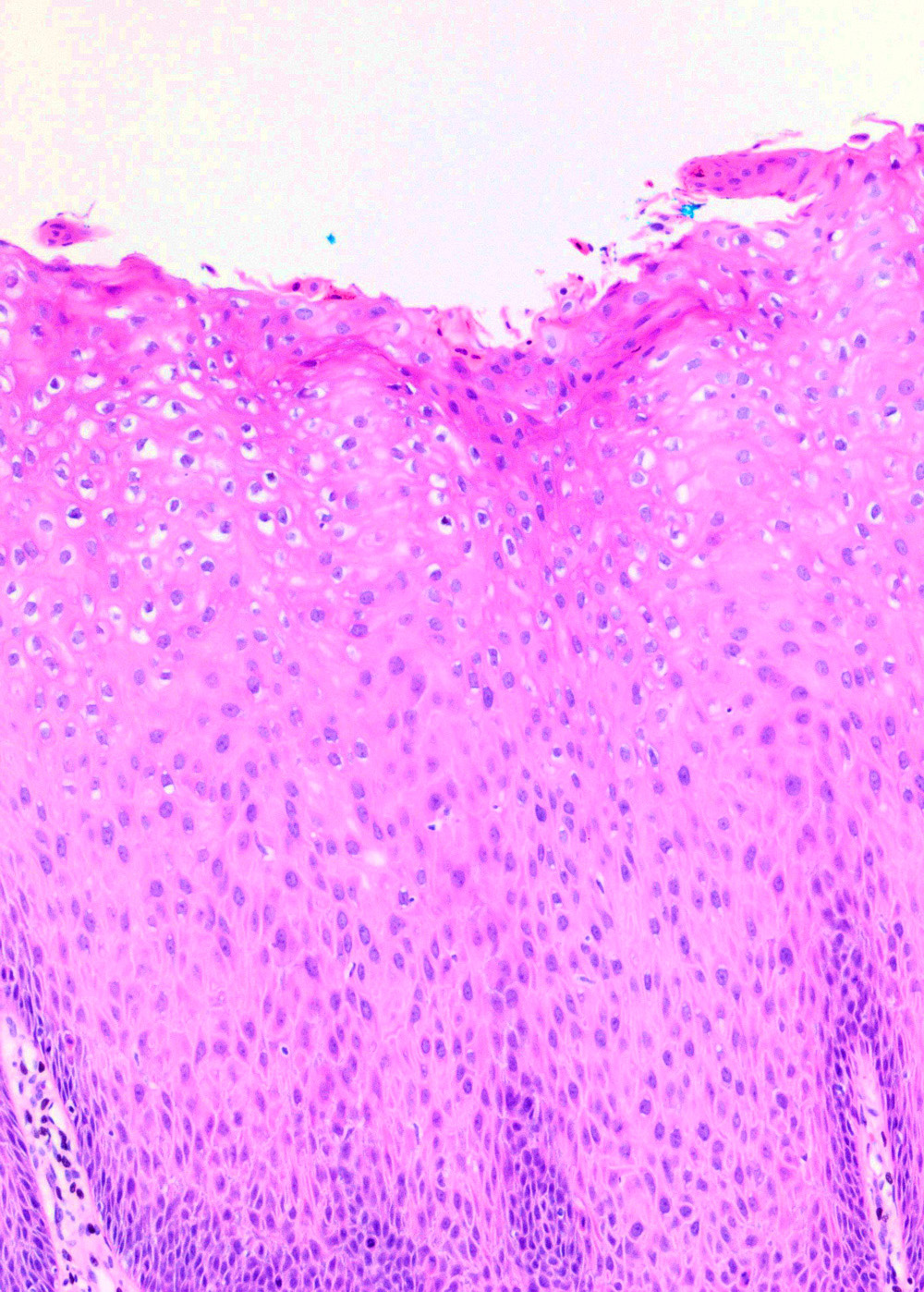
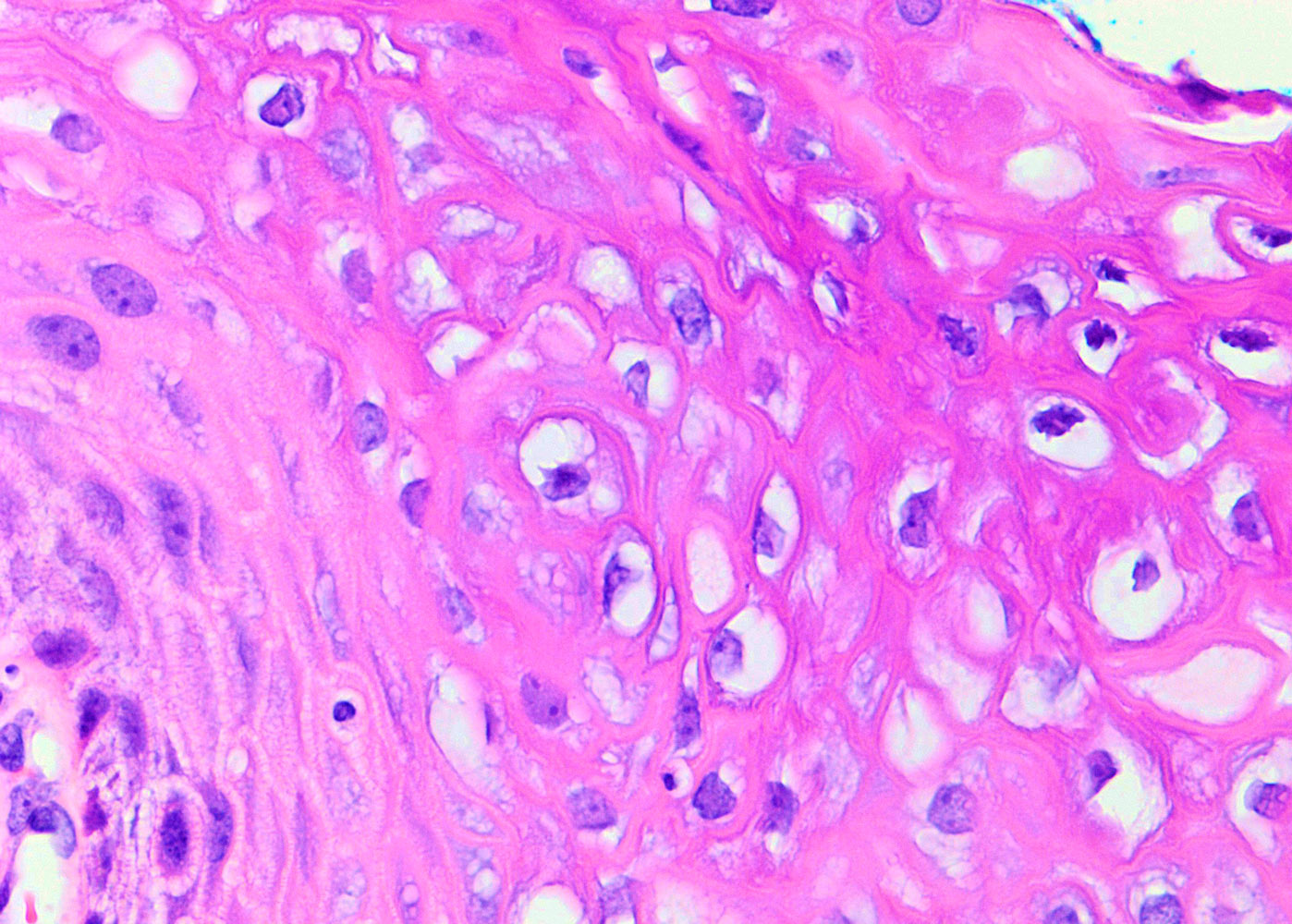
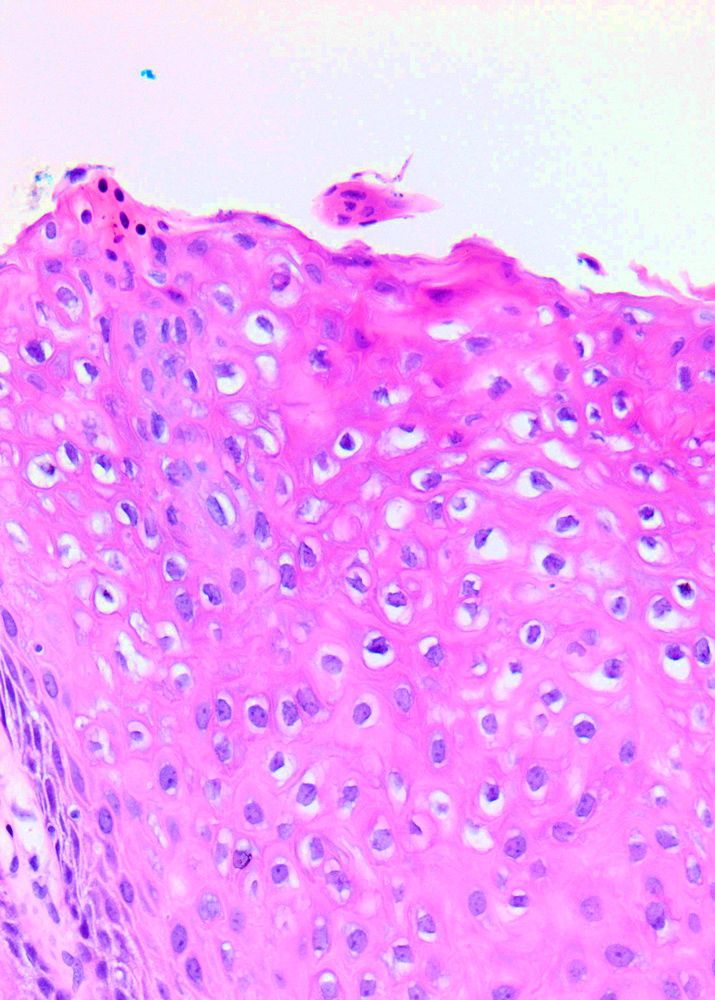
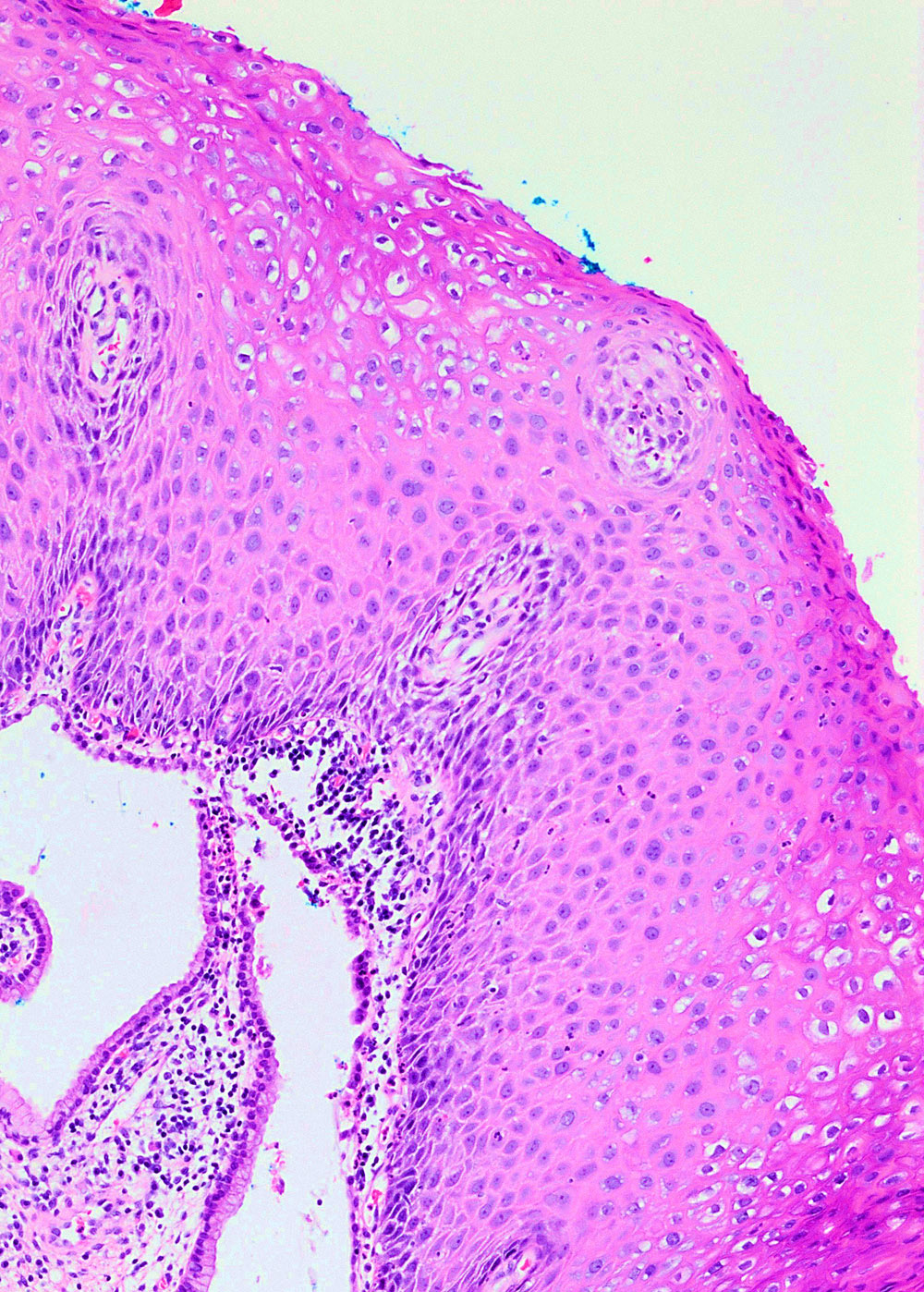
Microscopic (histologic) description
- Flat LSIL
- Preserved maturation
- Basal layer preserves polarity while intermediate to superficial cells lose polarity
- Nuclei in the superficial layer are large, hyperchromatic and irregular with perinuclear halos (koilocytosis / koilocytotic atypia)
- May show mitotic activity
- Exophytic LSIL
- Mature: papillomatosis with preserved maturation and koilocytic atypia
- Immature: slender papillae with metaplastic immature squamous epithelium and mild koilocytic atypia
Microscopic (histologic) images
Virtual slides
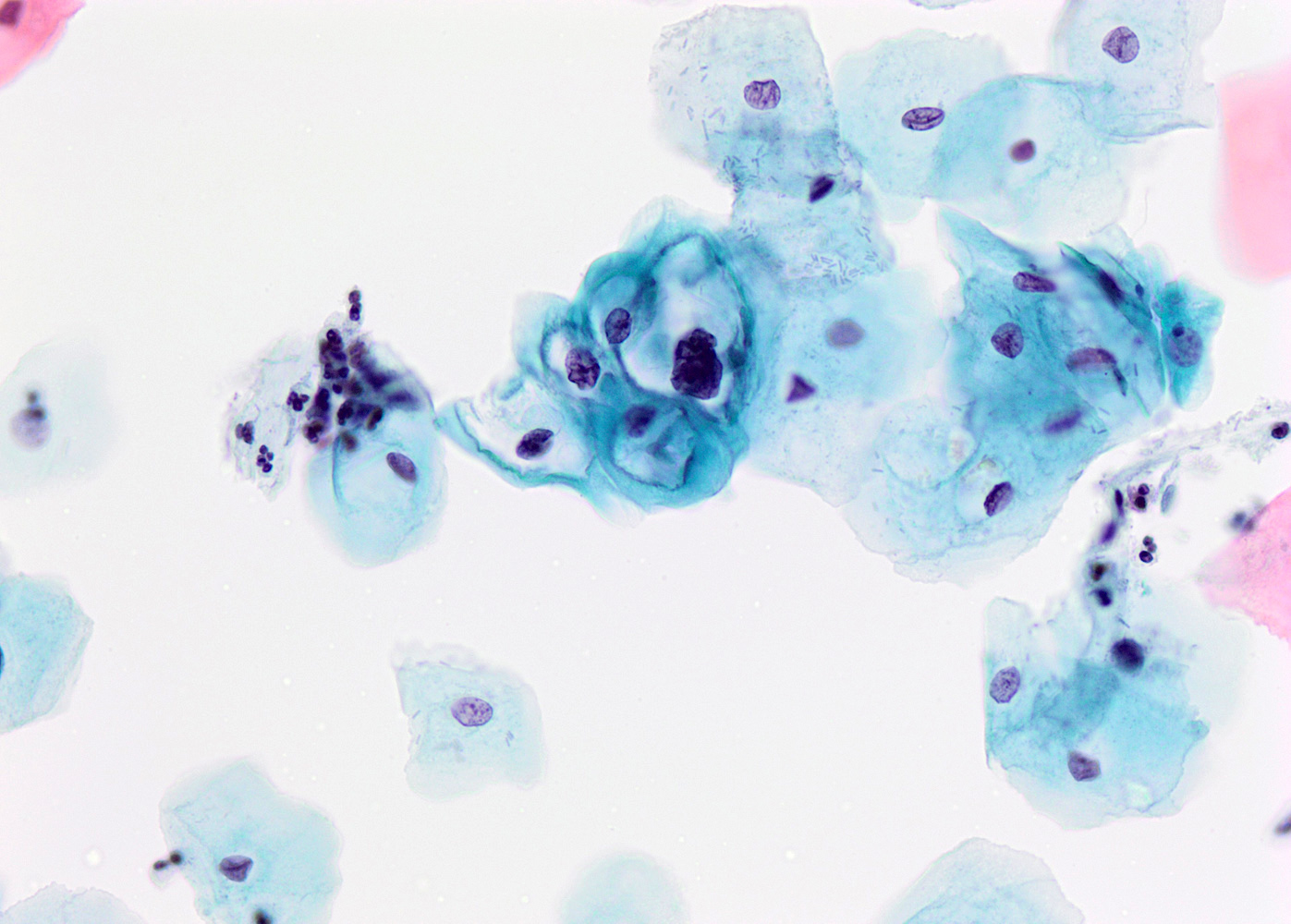
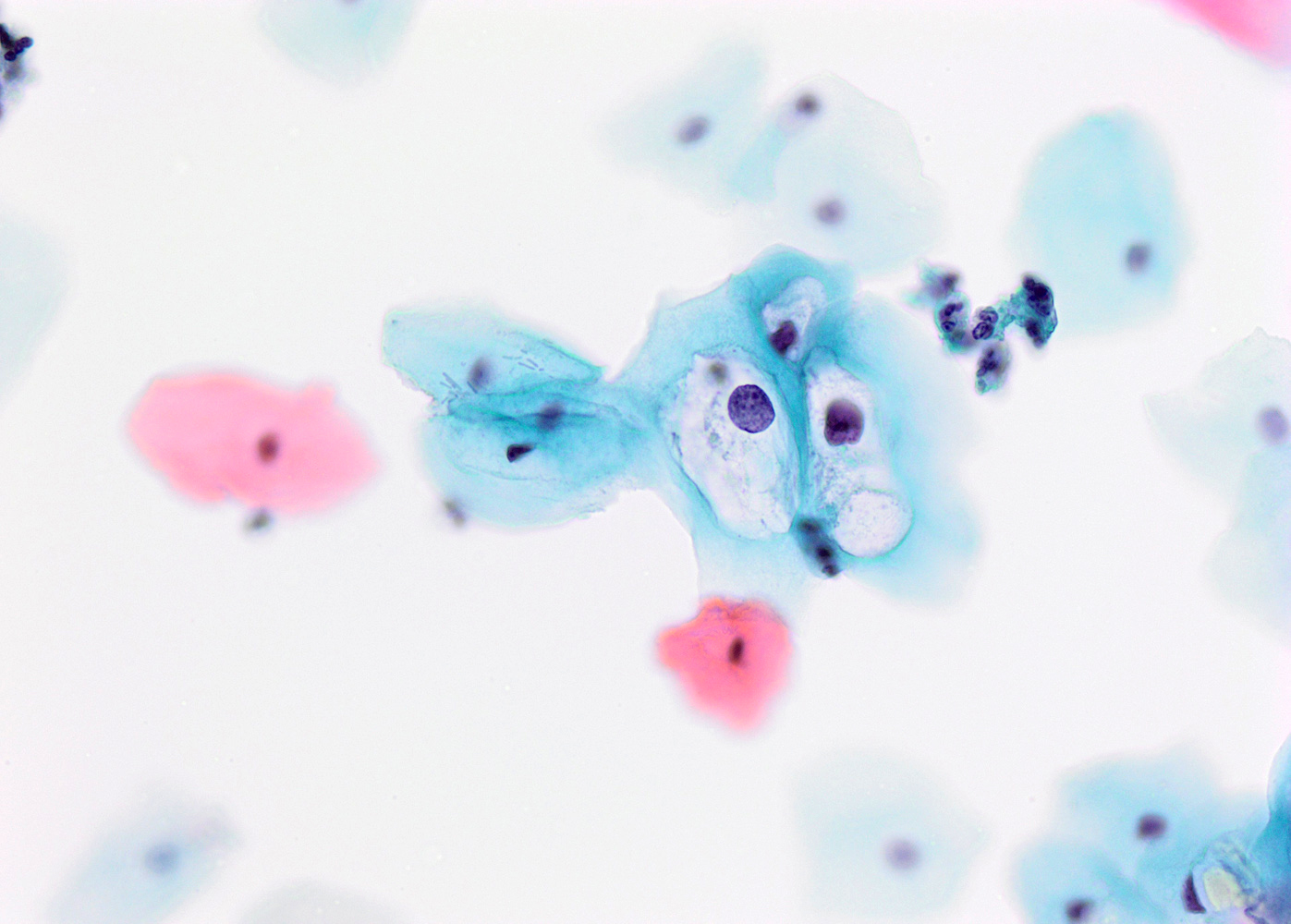
Cytology description
- Presence of koilocytes: intermediate squamous cell with enlarged hyperchromatic nuclei (1 or multiple nuclei) surrounded by perinuclear halo
- Nuclear features:
- Nuclear enlargement comparted to intermediate squamous cell (increased N/C ratio)
- Dense hyperchromatic chromatin
- Irregular nuclear membranes
- Perinuclear clear halo with a well defined, thick cytoplasmic rim
- See LSIL / CIN I cytology
Negative stains
- p16 is usually negative or weak and patchy, although lesions caused by high risk HPV will show overexpression (~33% of cases), limiting its use as a biomarker (Int J Surg Pathol 2012;20:146)
Molecular / cytogenetics description
- Molecular assays available based on RNA ISH include:
- HPV E6 / E7 mRNA in situ hybridization (ISH) assay covering 18 common high risk types (HR-RISH, aka HR-HPV RNA18 ISH)
- HR-RISH was also positive in 78% of anogenital low grade squamous intraepithelial lesion, including 81% of CIN1 (Am J Surg Pathol 2017;41:607)
- Molecular assays based on the detection of HPV DNA include:
- Nonamplified hybridization assays, such as Southern transfer hybridization (STH), dot blot hybridization (DB) and in situ hybridization (ISH)
- Signal amplified hybridization assays, such as hybrid capture assays (HC2)
- Target amplification assays, such as polymerase chain reaction (PCR) and in situ PCR (Int J Biol Markers 2009;24:215)
Videos
Squamous lesions of the cervix and their differential diagnosis
by Carlos Parra-Herran, M.D.
Sample pathology report
- Cervix, biopsy:
- Low grade squamous intraepithelial lesion (LSIL) / CIN I (see comment)
Differential diagnosis
- Inflammatory changes / repair:
- Nuclei are round, uniform and lack hyperchromasia
- Squamous metaplasia:
- Cells with mucin vacuoles, nuclei lack hyperchromasia
- Radiation and chemotherapy effects:
- Previous history, low N/C ratio
- High grade squamous intraepithelial lesion (HSIL):
- Shows hyperchromatic crowded squamous cells with high N/C ratio, present throughout the epithelium
- Mitotic figures are seen above the basal layer
- p16 shows block type staining in most HSILs; however, about 33% of LSILs also show p16 overexpression; therefore, p16 helps only if it is negative or patchy (not overexpressed), as it excludes HSIL and would be supportive of LSIL in the right diagnostic context
Additional references
Board review style question #1
Board review style answer #1