Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1Cite this page: Czaja R, Jorns JM. Sparganosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/breastsparganosis.html. Accessed April 2nd, 2025.
Definition / general
- Sparganosis is a parasitic zoonosis caused by spargana, the plercercoid tapeworm larvae of the genera Spirometra (Emerg Infect Dis 2017;23:665)
Essential features
- Sparganosis is caused by the migration of spargana larvae into superficial or visceral anatomic locations
- Infection occurs by drinking contaminated water, eating raw frogs or snakes or applying raw frog or snake poultices to wounds (Clin Infect Dis 2020 Jul 23 [Epub ahead of print])
- Treatment for superficial sparganosis is surgical removal (Lancet Infect Dis 2019;19:465)
ICD coding
Epidemiology
- Spirometra are endemic in Asia, Europe and North America (Parasitol Int 2020;75:102036)
- Most cases of human infection have been reported out of east and southeast Asian countries (Lancet Infect Dis 2015;15:1226)
Sites
- Common sites are the superficial soft tissue and muscle (Parasitol Int 2020;75:102036)
- Less commonly involves internal sites, such as the breast, abdominal wall, pericardium, liver, bone, eye and central nervous system
Pathophysiology
- Dogs; cats are the primary hosts of the adult tapeworms and when eggs are shed in their feces, they mature into coracidia in water and are ingested by copepods or crustaceans (the first intermediate hosts) (Lancet Infect Dis 2015;15:1226)
- Copepods / crustaceans are consumed by amphibians, reptiles or fish (second intermediate hosts) and the coracidia develop into plerocercoids (larvae)
- Cycle is completed when the primary hosts consume the secondary and the larvae mature into adult tapeworms in the hosts intestinal tracts
- Humans may consume the first or second intermediate hosts or use them as part of a poultice and the larvae migrate into tissue sites outside of the gastrointestinal tract
- Once in a site, the larvae form a nodular cyst or mass
- Sparganum proliferum larvae may proliferate and present with multiple plerocercoids in a single site
Etiology
- Consumption of contaminated water, raw snakes / frogs and cultural practices such as placing raw poultices of snakes / frogs in wounds (Lancet Infect Dis 2015;15:1226)
Clinical features
- Incubation period and clinical presentation depend on the route of infection and final location of the migrating larvae (Lancet Infect Dis 2015;15:1226)
- Incubation period is typically 6 - 11 days but may take several years to present symptoms
- Presents with localized erythema or slowly growing, itchy, nodules in the breast (Clin Infect Dis 2020 Jul 23 [Epub ahead of print])
- Patients infected by Sparganum proliferum show symptoms associated with the spread of proliferating larvae to various organs in the body over the course of years (Lancet Infect Dis 2015;15:1226)
Diagnosis
- Histologic evaluation of surgically removed sparganum
- Laboratory testing with polymerase chain reaction (PCR) for species level identification (Lancet Infect Dis 2015;15:1226)
- Imaging with CT, MRI and ultrasonography depending on the site
Laboratory
- Antisparganum IgG antibody in peripheral blood or cerebrospinal fluid (CSF) by enzyme linked immunosorbent assay (ELISA) (Lancet Infect Dis 2015;15:1226)
- DNA sequencing and nucleic acid amplification (Lancet Infect Dis 2019;19:465)
Radiology description
- Well defined serpiginous hypoechoic radio-opaque tubular structures are present, usually in subcutaneous fat (World J Surg 2011;35:573)
- Can mimic malignancy on mammogram: multiple, lobular, marginated, amorphic and solid masses without calcifications, which may mimic circumscribed breast cancer or fibroadenoma
- Migration of larvae induces inflammation and increased eosinophil response, which can cause increased F-18 fluorodeoxyglucose (FDG) uptake
Radiology images
Prognostic factors
- Prognosis is dependent on the site of infection
- Infection of the breast has an excellent prognosis and is curative with surgery
Case reports
- 46 and 69 year old women with palpable breast mass (Korean J Parasitol 2019;57:179)
- 57 year old woman with a palpable breast mass (J Parasit Dis 2018;42:442)
- 77 year old woman with palpable breast nodules (J Clin Aesthet Dermatol 2018;11:26)
Treatment
- Primary prevention by avoidance of contaminated food, water and poultices
- Complete surgical removal of superficial sparganum is the most effective therapy (Lancet Infect Dis 2015;15:1226)
- Localized chemotherapy or anthelmintic drugs if the site is not suitable for surgery
Gross description
- Sparganum larvae are white, ribbon-like parasites that typically range from 3 - 30 cm in length and 1 - 2 mm in width (Lancet Infect Dis 2015;15:1226)
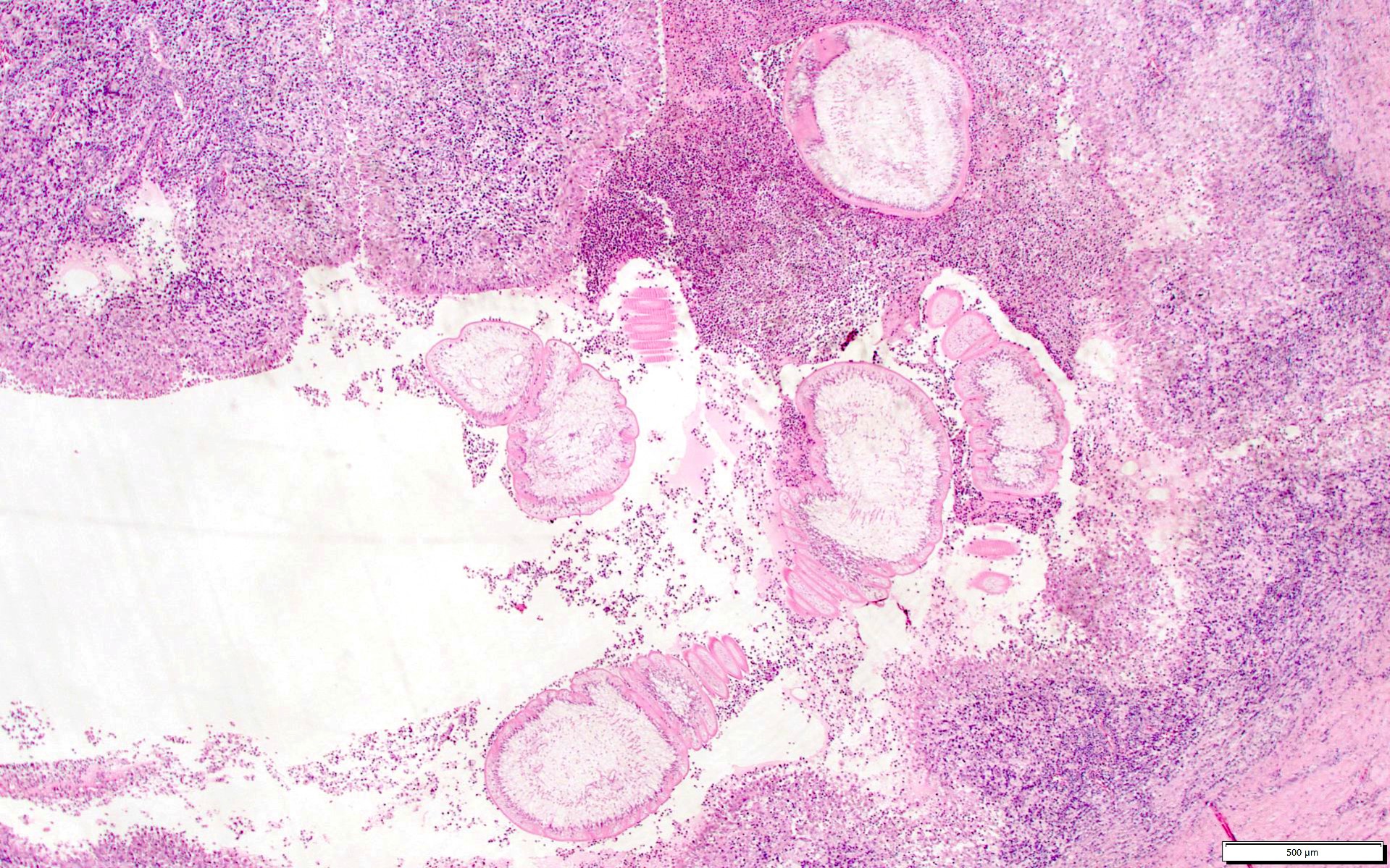
Microscopic (histologic) description
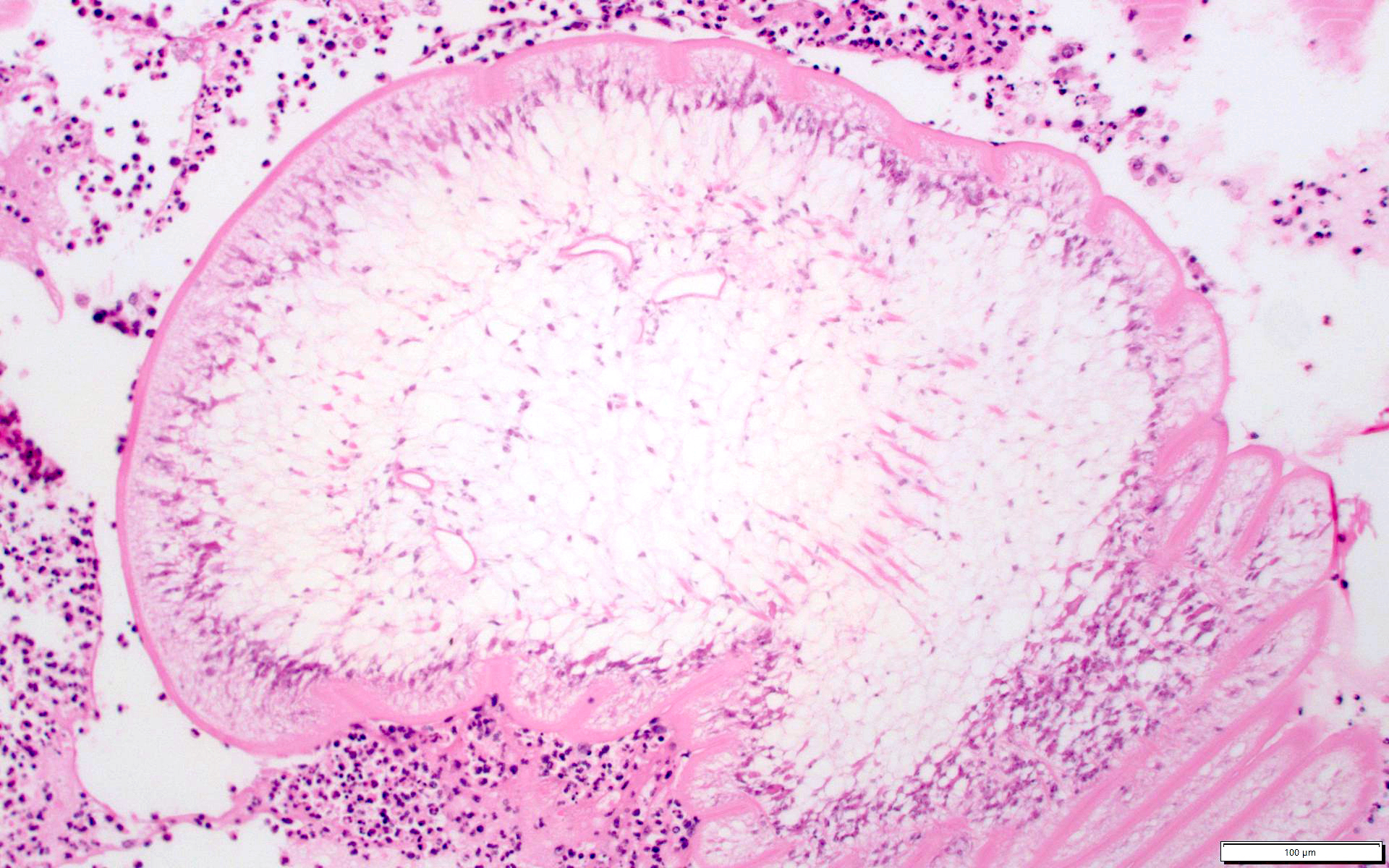
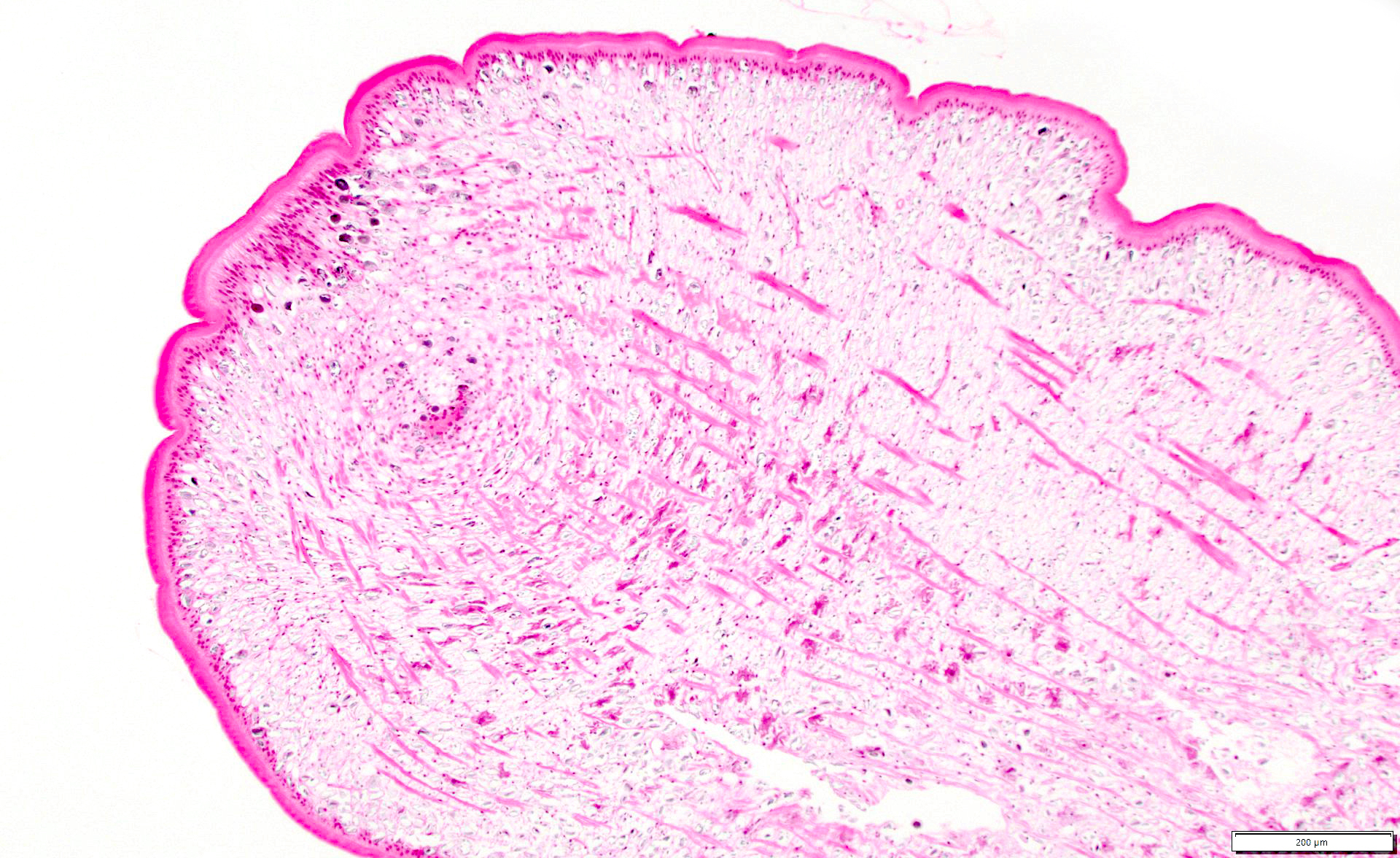
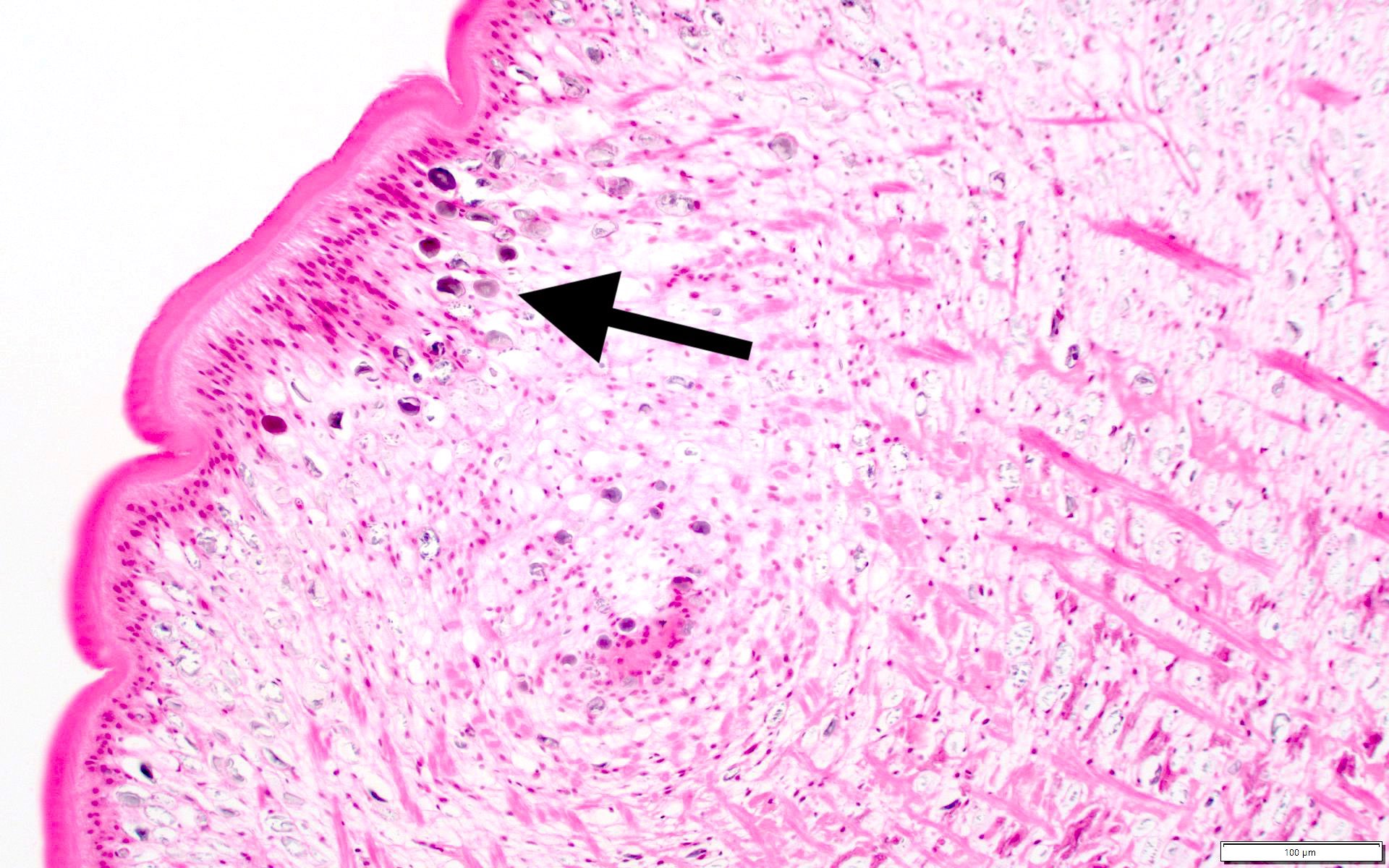
- Cestode shows a pale myxoid matrix with longitudinal smooth muscle fibers and calcareous corpuscles (mineralized concretions), surrounded by a noncellular eosinophilic tegument (Breast J 2014;20:92)
- Thin longitudinal smooth muscle fibers within myxoid matrix of the cestode larva area is the distinguishing feature for organism identification
- Scolex is absent (in contrast to cysticerci)
- Surrounding tissue may show chronic inflammation, cyst formation, granulomatous inflammation
Microscopic (histologic) images
Positive stains
- Periodic acid-Schiff (PAS) highlights tegument
Sample pathology report
- Left breast, excisional biopsy:
- Foreign body reaction to larval organisms showing a myxoid matrix with longitudinal grooves and calcareous corpuscles, consistent with sparganosis
Differential diagnosis
- Cysticercosis:
- Clinically presents with multiple lesions
- Classically involves the brain, skeletal and cardiac muscle
- Caused by larval cysts of the tapeworm Taenia solium
- Larvae with similar stroma but containing a scolex, hooks and surrounding fluid filled bladder
- Absence of longitudinal smooth muscle
- Acute mastitis:
- Acute phase shows variable foci of acute inflammatory, necrotic and proteinaceous debris
- May show granulation tissue and chronic inflammatory infiltration in chronic phase
- Multinucleated foreign body cells may be present
- Granulomatous mastitis:
- Shows well formed granulomas within lobules or adjacent to ducts
- May show Langhans giant cells and chronic inflammation
- Microabscesses may be present with lipid vacuoles
Additional references
Board review style question #1
A 36 year old Chinese woman presents with a pruritic, slowly growing erythematous nodule on her left breast over the past 2 weeks. The nodule is surgically removed and shows the images above on review. What histological finding is most diagnostic of sparganosis of the breast?
- Eosinophilic tegument
- Longitudinal smooth muscle fibers
- Presence of a scolex
- Myxoid stroma
Board review style answer #1
B. Longitudinal smooth muscle fibers. Cestodes (tapeworms), including Eichanococcus, Taenia and Spirometra, show calcareous corpustles and a tegument (the outer covering) on histologic evaluation. However, these are not specific for Spirometra. Sparganum are also known for their absence of a scolex. A key histologic feature supportive of sparganosis is the longitudinal smooth muscle fibers.
Comment Here
Reference: Sparganosis
Comment Here
Reference: Sparganosis