Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Case reports | Treatment | Clinical images | Gross description | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Rana C. Pubertal macromastia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/breastpubertalmacromastia.html. Accessed December 26th, 2024.
Definition / general
- Rare form of breast hypertrophy that is characterized by an atypical, alarmingly rapid and continual breast growth during puberty or in the peripubertal age group (J Breast Health 2014;10:122)
Essential features
- Rare form of breast hypertrophy characterized by rapid and continual breast enlargement
- Pathogenesis is not clear
- Surgery with or without medical therapy is the treatment of choice
- Breast hypertrophy is defined as a medical condition of the breast connective tissues in which the breasts become excessively large
- There is no universal classification or definition
- Based on the severity, it can be of 2 types (Hoda: Rosen's Breast Pathology, 5th Edition, 2020)
- Gigantomastia: refers to cases with extreme breast enlargement, where excessive tissue is > 2.5 kg
- Macromastia: refers to sustained, steady breast enlargement that develops throughout puberty, where excessive tissue is < 2.5 kg
Terminology
- Also known as
- Juvenile macromastia or juvenile gigantomastia (Case Rep Surg 2017;2017:3491012)
- Virginal breast hypertrophy or virginal mammary hypertrophy (J Breast Health 2014;10:122)
- Adolescent breast hypertrophy, gigantomastia or macromastia (Clin Plast Surg 2016;43:383)
ICD coding
- ICD-10: N62 - hypertrophy of breast
- Applicable to
- Hypertrophy of breast, NOS
- Gynecomastia
- Massive pubertal hypertrophy of breast
- Applicable to
Epidemiology
- Affects girls in pubertal and peripubertal age group (10 - 17 years old) (Semin Plast Surg 2013;27:49)
- Incidence is increasing in general population; however, true incidence is not known (Semin Plast Surg 2013;27:49)
Sites
- Can affect unilateral or bilateral breasts (Semin Plast Surg 2013;27:49)
Pathophysiology
- Underlying mechanism not yet elucidated (Case Rep Surg 2017;2017:3491012)
- Most accepted hypothesis is end organ sensitivity to normal levels of hormones (estrogen, progesterone and prolactin) or growth factor (hepatocyte growth factor, insulin-like growth factor 1 and epidermal growth factor) (Arch Med Sci 2019;18:1016, Case Rep Surg 2017;2017:3491012)
Etiology
- Some suggest association with unhealthy lifestyle and hormone laden diet
- ~66% of women with macromastia are obese (Plast Reconstr Surg 2002;109:64)
- Macromastia is also known to be associated with hypercalcemia, systemic lupus erythematosus and pseudoangiomatous stromal hyperplasia (Plast Reconstr Surg Glob Open 2015;3:e501, Scuderi: International Textbook of Aesthetic Surgery, 1st Edition, 2016)
- Familial virginal breast hypertrophy is seen in association with Cowden syndrome (Ann Intern Med 1963;58:136)
- PTEN gene abnormalities can be a possible factor for precocious puberty and has been postulated as genetic basis of this disease (Development 2002;129:4159)
Clinical features
- Characterized by 6 months of extreme breast enlargement followed by longer period of slower and sustained breast growth
- Breast weight exceeds ~3% of the total body weight (J Plast Reconstr Aesthet Surg 2011;64:160)
- May be associated with neck, shoulder and back pain (J Breast Health 2014;10:122)
- Shoulder grooving, skin irritation or intertrigo may be present due to brassiere straps
- Often accompanied with skin hyperemia, dilated subcutaneous veins and skin ulceration (J Breast Health 2014;10:122)
- Emotional distress due to dissatisfaction with body image and poor self esteem (J Adolesc Health 2004;35:151)
Diagnosis
- Physical examination typically reveals normal sexual development
- Breasts are generally enlarged, pedunculated, ptotic with widened areolas
- Often firm on palpation and diffusely tender
- Discrete nodules may be present
- Breast growth, velocity and stability should be evaluated along with pubertal development and onset of thelarche (Semin Plast Surg 2013;27:49)
- Family history regarding breast disorders particularly related to breast hypertrophy should be noted (Semin Plast Surg 2013;27:49)
Laboratory
- Endocrinology profile, specifically estradiol, progesterone, luteinizing hormone (LH), follicle stimulating hormone (FSH) and prolactin, does not reveal any abnormalities and is not routinely indicated (Semin Plast Surg 2013;27:62)
Radiology description
- Breast imaging is of limited value owing to the dense breast tissue
- May be required if mass lesion is present
Case reports
- 11 year old girl with virginal breast hypertrophy associated with Beckwith-Wiedmann syndrome (Clin Case Rep 2018;6:484)
- 12 year old girl with complaint of rapid growth in bilateral breast with symptomatic treatment (J Pediatr Surg 1988;23:1014)
- 12 year old girl with gigantomastia and giant fibroadenomas (BJR Case Rep 2021;8:20210181)
- 14 year old girl with rapid growth of bilateral breast (Clin Case Rep 2020;9:198)
- 22 year old woman with gigantomastia as a cause of pulmonary hypertension (Arch Plast Surg 2022;49:369)
Treatment
- No standard treatment; treated on a case by case basis
- Usually treated with surgical procedures, like reduction mammoplasty or subcutaneous mastectomy with implant application, with or without medical therapy (Case Rep Surg 2017;2017:3491012)
- Higher recurrence rates after reduction mammoplasty but better cosmetic results (J Pediatr Surg 1988;23:1014, Plast Reconstr Surg 2011;127:2224)
- Subcutaneous mastectomy has fewer cosmetic satisfaction rates, no reserve for lactation and lifetime risk of implant but has the lowest risk of recurrence (Plast Reconstr Surg 2011;127:2224, J Pediatr Surg 1988;23:1014)
- Medical therapy includes use of tamoxifen, bromocriptine, medroxyprogesterone, danazole, chorionic gonadotropin hormone and thyroid extracts (Plast Reconstr Surg 2011;127:2224)
Clinical images
Gross description
- No specific gross findings; only fibrofatty tissue seen
Frozen section description
- No role of frozen in these cases
- May be used whenever there is preoperative suspicion of cancer
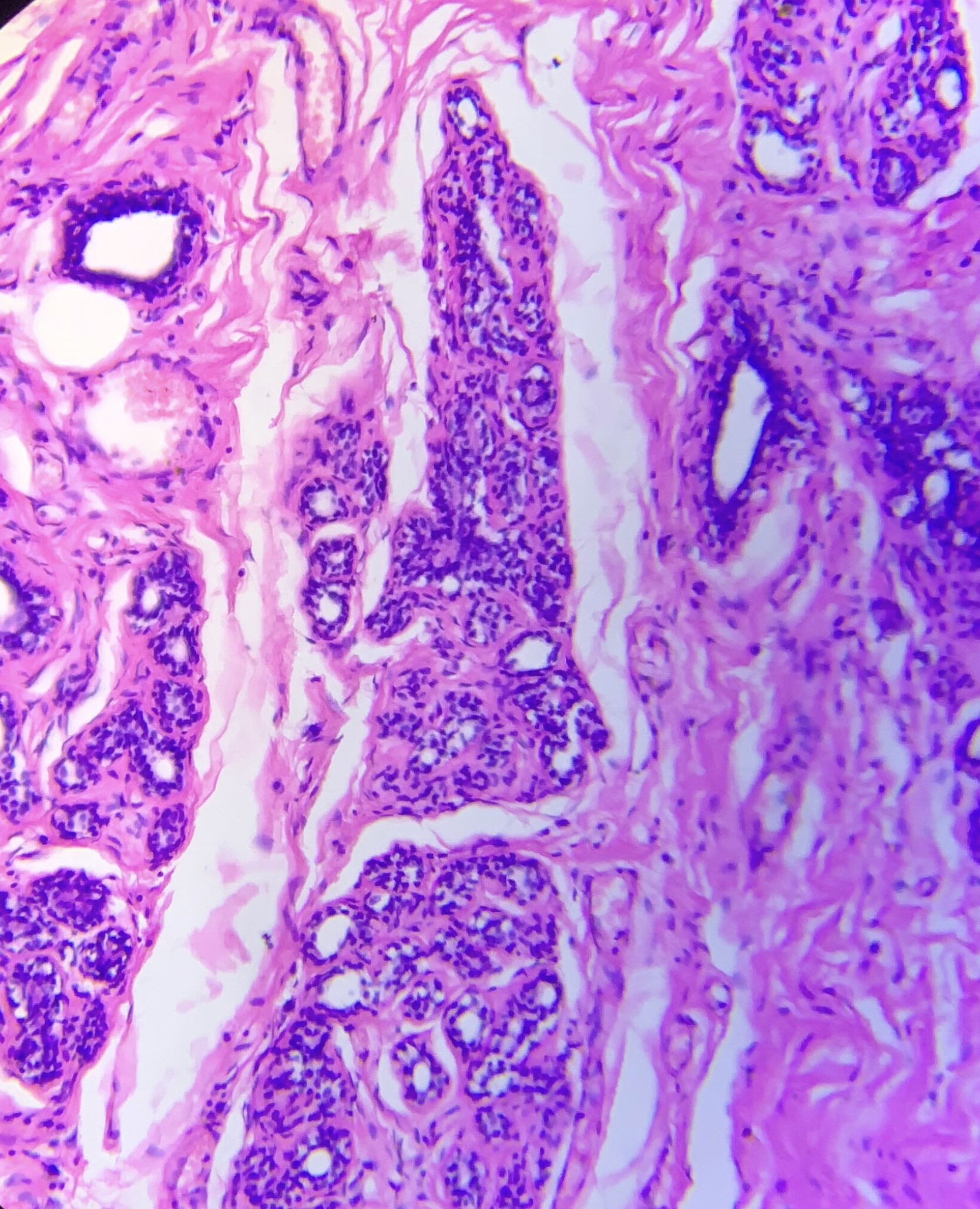
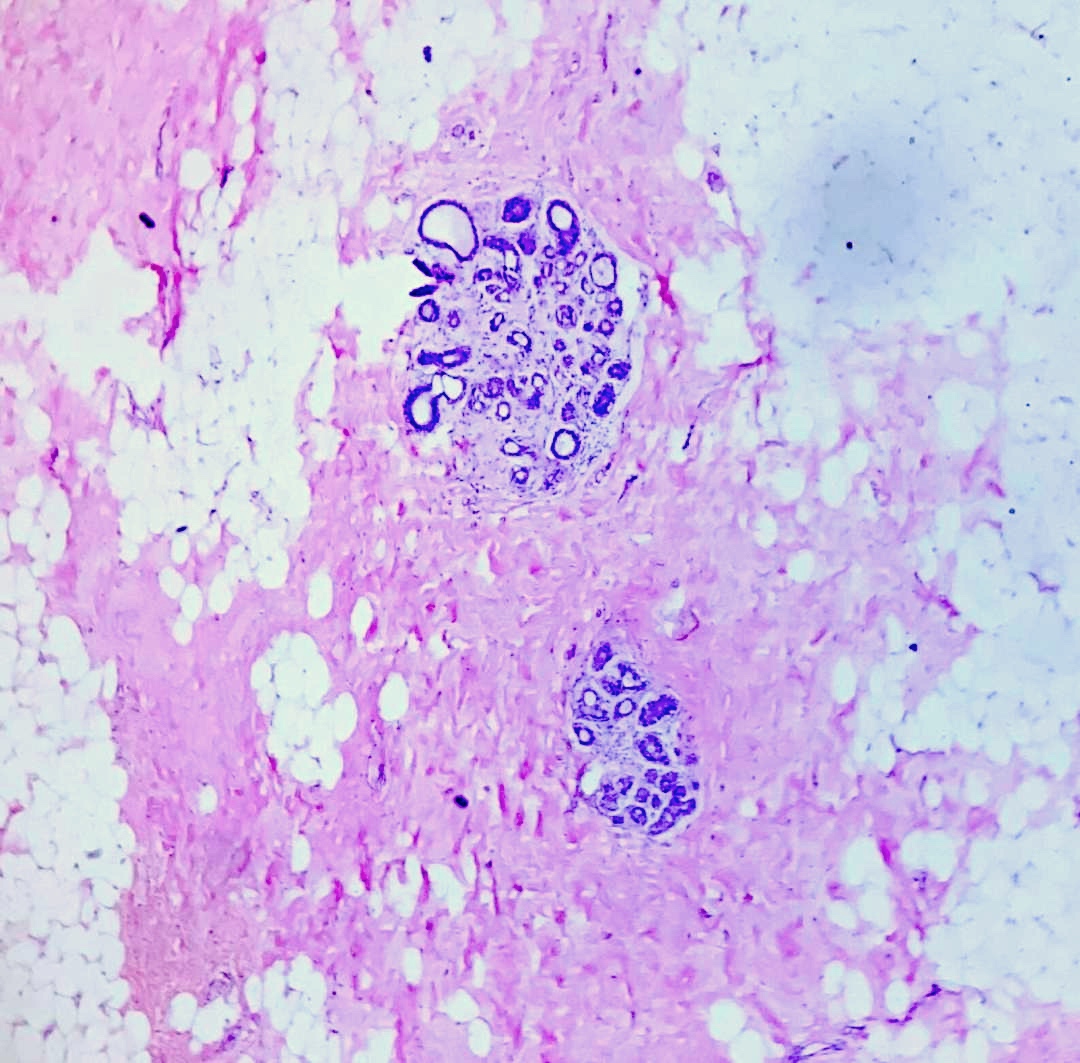
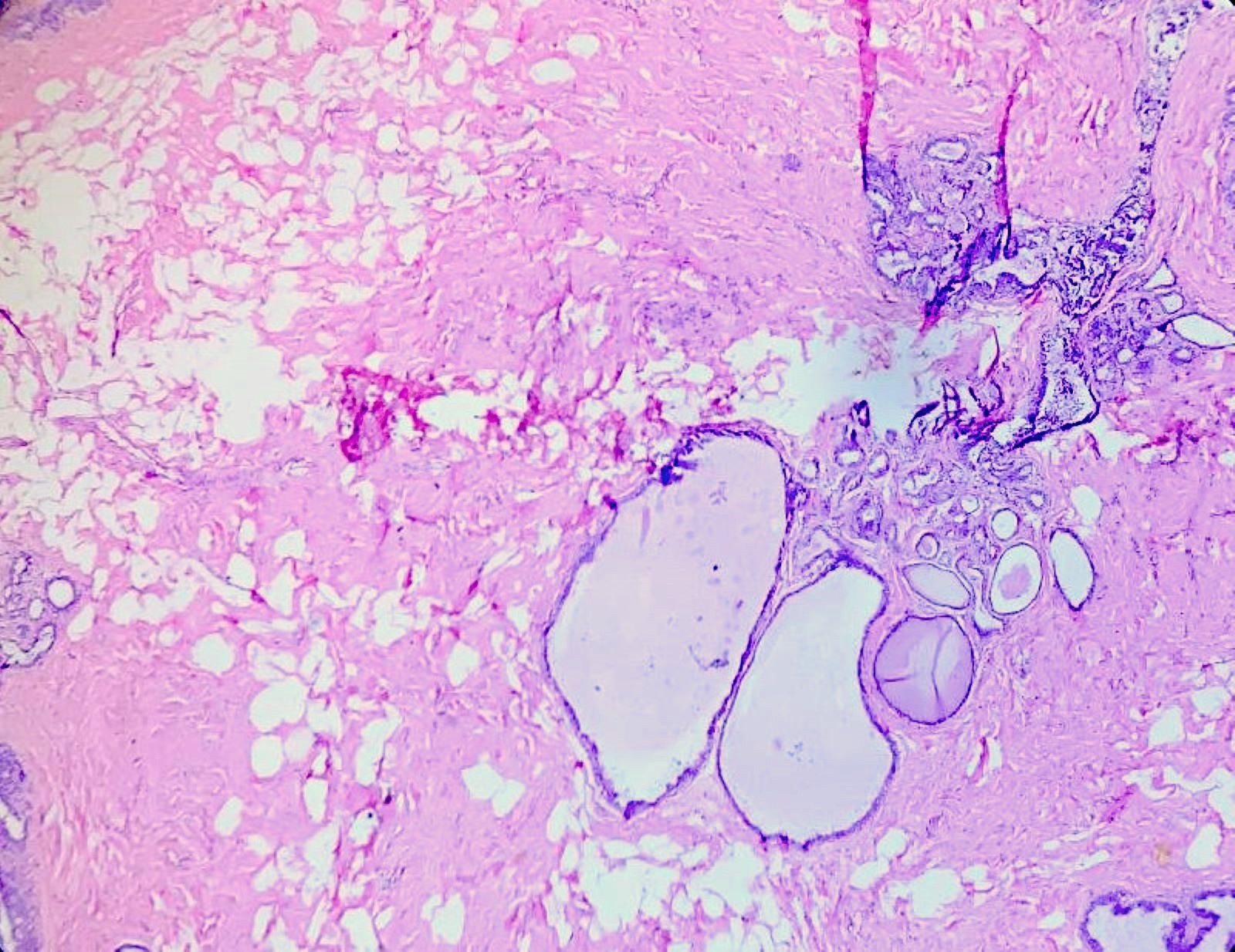
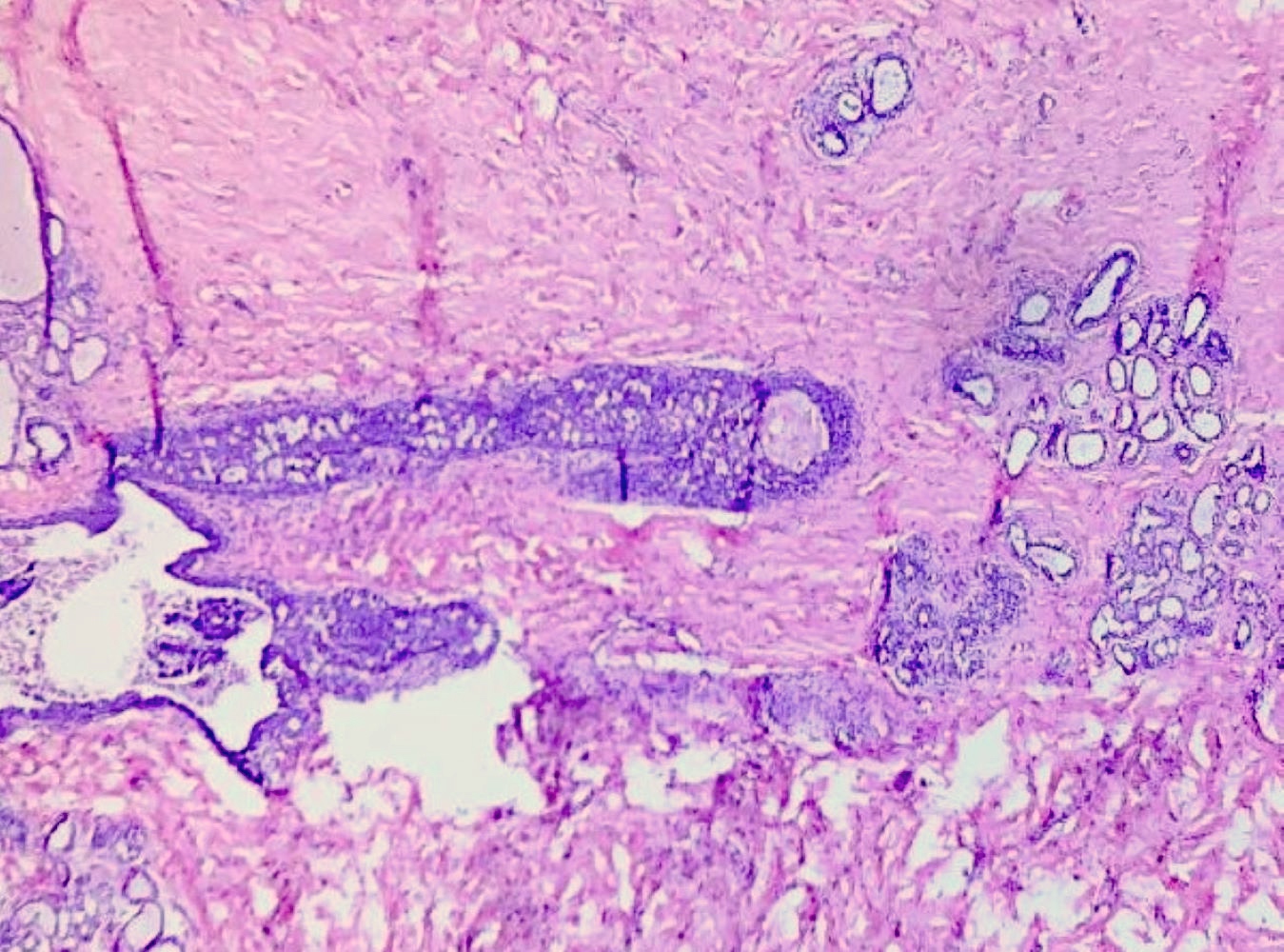
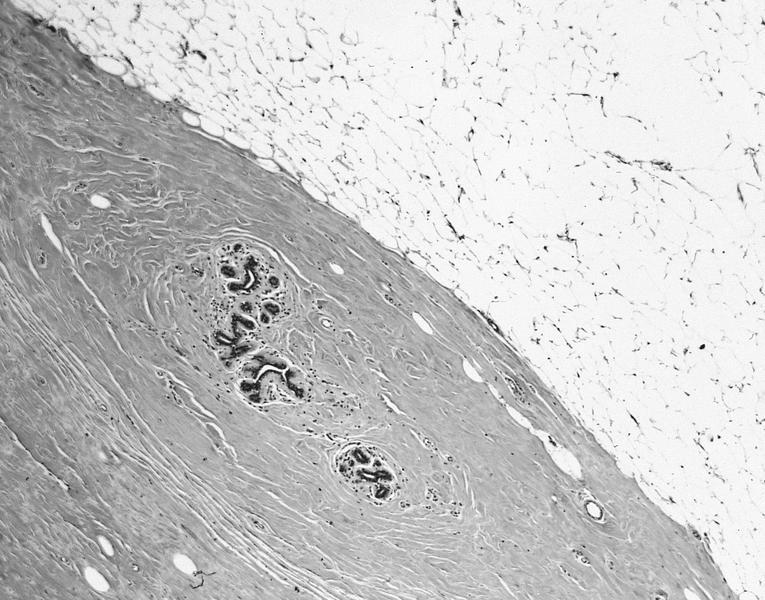
Microscopic (histologic) description
- Clinical diagnosis
- Histomorphological findings resemble gynecomastia
- Increased stromal collagenization and fibrosis
- Poorly developed or reduced lobules
- Sometimes usual ductal hyperplasia is also seen
- Reference: Case Rep Surg 2017;2017:3491012
Microscopic (histologic) images
Cytology description
- It is a clinical diagnosis, which does not require use of fine needle aspiration cytology
- Findings are nonspecific
- Smears may be paucicellular
- Resembles benign breast disease characterized by sheets of benign ductal and myoepithelial cells with bare nuclei in the background
Sample pathology report
- Bilateral breast, reduction mammoplasty:
- Consistent with clinical diagnosis of bilateral breast hypertrophy
- No evidence of malignancy
- Bilateral breast, subcutaneous mastectomy:
- Consistent with clinical diagnosis of bilateral breast hypertrophy
- No evidence of malignancy
Differential diagnosis
- Clinical diagnosis
- Need to exclude other causes of breast hypertrophy
- Breast hypertrophy associated with endocrine disorder:
- Histology is similar but also associated with laboratory abnormalities like aromatase excess, hyperprolactinemia and excessive production of parathyroid hormone
- Drugs:
- Penicillamine, ciclosporin, prednisolone, indinavir, etc.
- There is a history of drug intake followed by development of hypertrophy
- Obesity
Board review style question #1
Board review style answer #1
A. Characterized by increased sensitivity to normal levels of hormone. There is heightened end organ sensitivity with normal hormonal as well as growth factor levels. Answer B is incorrect because cases of pubertal macromastia have normal hormonal levels, only the sensitivity to their levels is increased. Answer D is incorrect because pubertal / virginal / juvenile macromastia is generally treated surgically with or without medical therapy. Answer C is incorrect because recurrence rates are high with reduction mammoplasty.
Comment Here
Reference: Pubertal macromastia
Comment Here
Reference: Pubertal macromastia
Board review style question #2
Which of the following statements about breast hypertrophy is true?
- Drugs such as bromocriptine and tamoxifen are used as a part of medical management
- Medical therapy is never indicated
- Obesity is not one of the major causes
- Subcutaneous mastectomy is never done
Board review style answer #2
A. Drugs such as bromocriptine and tamoxifen are used as a part of medical management. Bromocriptine and tamoxifen are used as medical therapy to reduce breast proliferation. Answer C is incorrect because pubertal / virginal / juvenile macromastia can be associated with obesity. Answer D is incorrect because subcutaneous mastectomy is also one of the surgical management options. Answer B is incorrect because medical management may be given before or after the surgical procedures for breast reduction to prevent further growth.
Comment Here
Reference: Pubertal macromastia
Comment Here
Reference: Pubertal macromastia