Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Rana C. Squamous cell carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/breastmalignantscc.html. Accessed April 2nd, 2025.
Definition / general
- Breast neoplasm with greater than 90% squamous differentiation with variable degrees of keratinization (Eur J Surg Oncol 2003;29:386, Acta Cytol 1989;33:201)
- The following criteria are also required to establish a firm diagnosis:
- Tumor is centered in the breast parenchyma, independent of the overlying skin and nipple of adnexal elements (exclusion of primary cutaneous neoplasm)
- Exclusion of metastasis from an extramammary primary squamous cell carcinoma (SCC) (e.g., lung, cervix, bladder, head and neck)
Essential features
- All or at least 90% of tumor must be composed of malignant squamous cells
- Etiology uncertain; thought to arise as a result of extensive squamous metaplasia in benign conditions (e.g., cysts, chronic inflammatory conditions, abscess, intraductal papillomas)
- Associated with a lower rate of lymph node metastasis and a significant rate of distant metastasis without lymph node involvement
- Aggressive and often refractory to treatment
Terminology
- Pure metaplastic squamous cell carcinoma of the breast
- Primary squamous cell carcinoma of the breast
- Pure squamous cell carcinoma of the breast
ICD coding
- ICD-O: 8575/3 - metaplastic carcinoma, NOS
- ICD-11: 2C6Y & XH0RD4 - other specified metaplastic carcinoma of breast & metaplastic carcinoma, NOS
Epidemiology
- First described by Troell in 1908
- Very rare and constitutes < 0.1% of primary invasive breast cancer (Hum Pathol 1984;15:526)
- Prevalence is uncertain due to rarity of the disease; a limited number of cases have been reported thus far
- Usually known to affect postmenopausal females
Sites
- Can affect any anatomical area of breast
Pathophysiology
- Histogenesis remains unclear and many theories have been postulated
- Commonly proposed theories are:
- Extreme form of squamous metapalsia developing in adenocarcinoma (Ann Surg Oncol 1996;3:367)
- Squamous cell metaplasia developing in cysts, chronic inflammations, abscesses and adenofibromas (Eur J Surg Oncol 2003;29:386)
Etiology
- No single specific etiological factor identified or described; no association with familial cancer syndromes reported
- Chronic inflammation resulting in squamous metaplasia may represent a predisposing factor (e.g., implant associated squamous cell carcinoma) (Hum Pathol 2017;67:94, Cancer 1994;73:1449)
Clinical features
- Most patients present with a well circumscribed palpable mass
- Tends to be somewhat larger at presentation than other types of breast carcinoma
- Mean age of primary squamous cell carcinoma reported between 52 and 64 years old (Cancer 1994;73:1449)
- 20 - 40% of the reported cases in excess of 5 cm in diameter (Anticancer Res 2007;27:547, Hum Pathol 1984;15:526)
- Massive lesions have also been described; such lesions may displace the nipple and cause skin ulceration
- Associated with a lower rate of lymph node metastasis and a significant rate of distant metastasis without lymph node involvement (J Cancer Res Ther 2019;15:1057, Am J Clin Oncol 2003;26:571)
- Aggressive and often refractory to treatment (Eur J Obstet Gynecol Reprod Biol 2008;137:222, J Clin Oncol 2005;23:7827)
- Due to its rarity, prognosis and optimal diagnostic and therapeutic management are uncertain
Diagnosis
- Squamous component can be diagnosed on cytology or biopsy; however, to diagnose pure squamous cell carcinoma, histopathological evaluation of the excised lesion is recommended
- Primary cutaneous or metastatic squamous cell carcinomas from other sites must be ruled out
Radiology description
- No specific mammography findings
- Solid hypoechogenic masses with complex cystic components (Am Surg 1999;65:1153)
Prognostic factors
- Prognostic information is limited; however, reports suggest an aggressive clinical course, with outcomes comparable to poorly differentiated ductal carcinoma of the breast
- 5 year survival has been reported to be 52% and 63% (Anticancer Res 2007;27:547, Cancer 1990;65:272)
Case reports
- 43 year old Moroccan woman presenting with an infected mass in the left breast associated with ipsilateral axillary lymphadenopathy (Pan Afr Med J 2015;20:152)
- 46 year old woman with unusual case of implant associated SCC of the breast post silicone gel breast implant (Cureus 2018;10:e3405)
- 54 year old woman with primary pure squamous cell carcinoma of the breast in the form of an intracystic tumor (Cancer Rep (Hoboken) 2021;4:e1391)
- 57 and 60 year old women with acantholytic variant of squamous cell carcinoma (Cesk Patol 2011;47:184)
- 61 year old woman with breast abscess as the initial manifestation of primary pure squamous cell carcinoma (Breast Dis 2011;33:125)
- 68 year old woman with primary squamous cell carcinoma of the breast presenting as a right breast mass (J Surg Case Rep 2019;2019:rjz182)
- 72 year old woman with primary squamous cell carcinoma of the breast with pathologic complete response after neoadjuvant chemotherapy (Curr Probl Cancer 2019;43:308)
Treatment
- Surgical resection, either mastectomy or wide excision
- Relatively resistant to conventional chemotherapy with no documented substantial role of neoadjuvant chemotherapy (Onco Targets Ther 2016;9:3181)
- Hormonal therapy is not indicated, as these tumors are triple negative
- Adjuvant radiotherapy frequently provided with limited available response data (J Clin Oncol 2005;23:7827, Cancer 1994;73:1449)
- Recent study has shown remarkable response to immunotherapy (anti-PDL1) (NPJ Breast Cancer 2017;3:8)
- Usually managed by surgical excision followed by chemotherapy (cisplatin based); radiotherapy is followed as for other invasive carcinomas of breast (Gan To Kagaku Ryoho 2007;34:443, J Surg Oncol 1995;59:199)
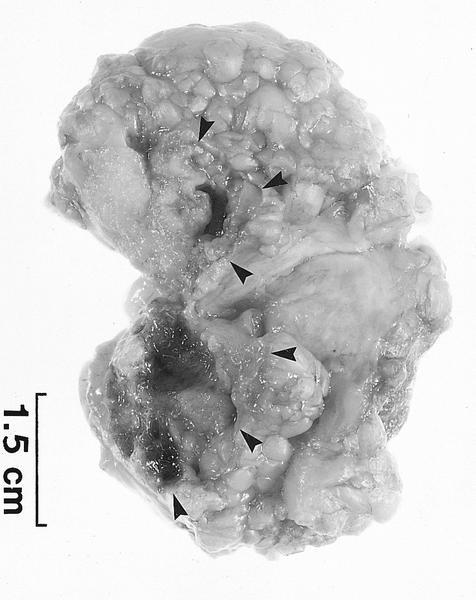
Gross description
- Often presents as large tumors (> 4 cm) at diagnosis (Int J Surg Case Rep 2011;2:194)
- Associated with cystic changes in half of the cases (Int J Surg Case Rep 2011;2:194)
Gross images
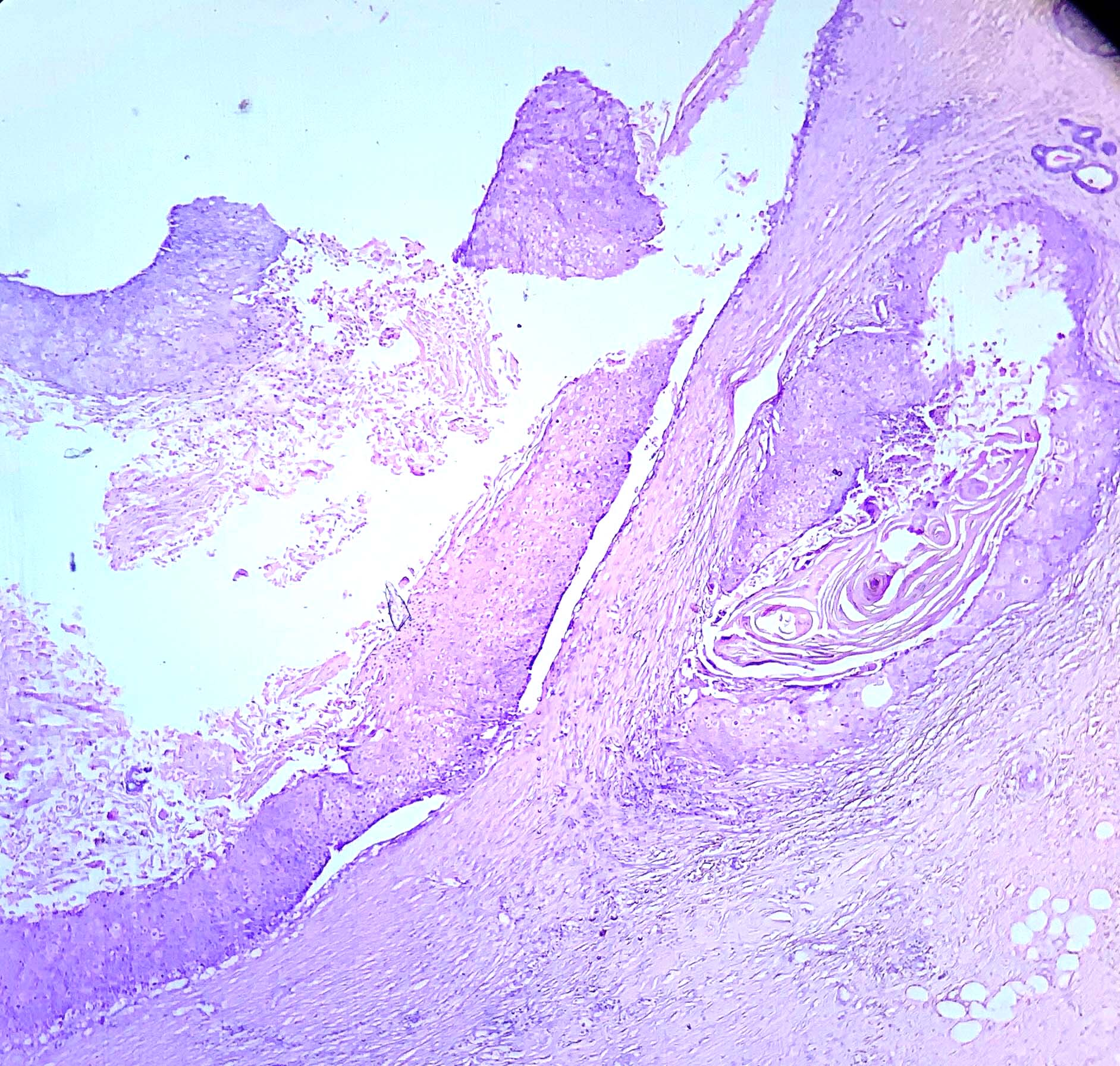
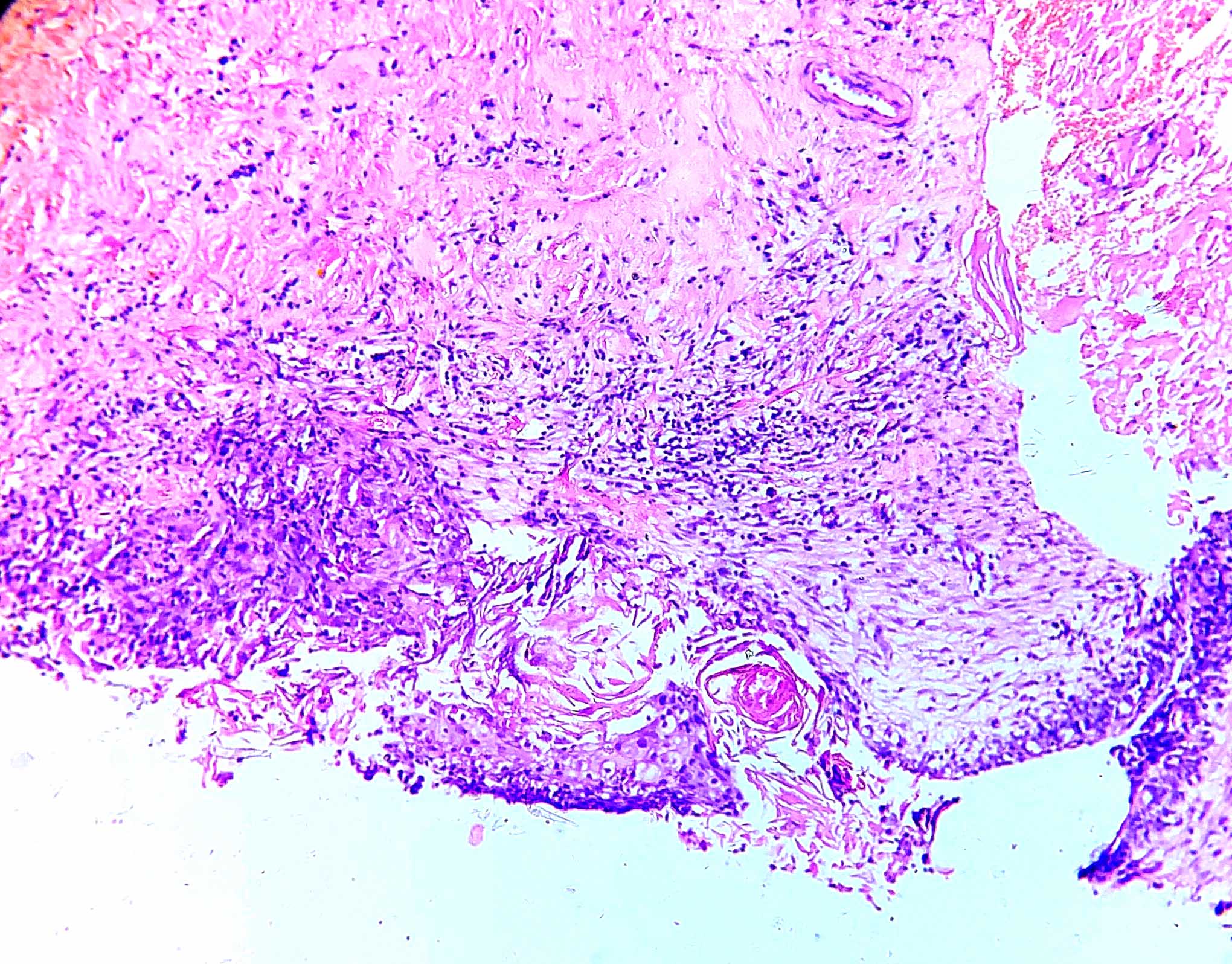
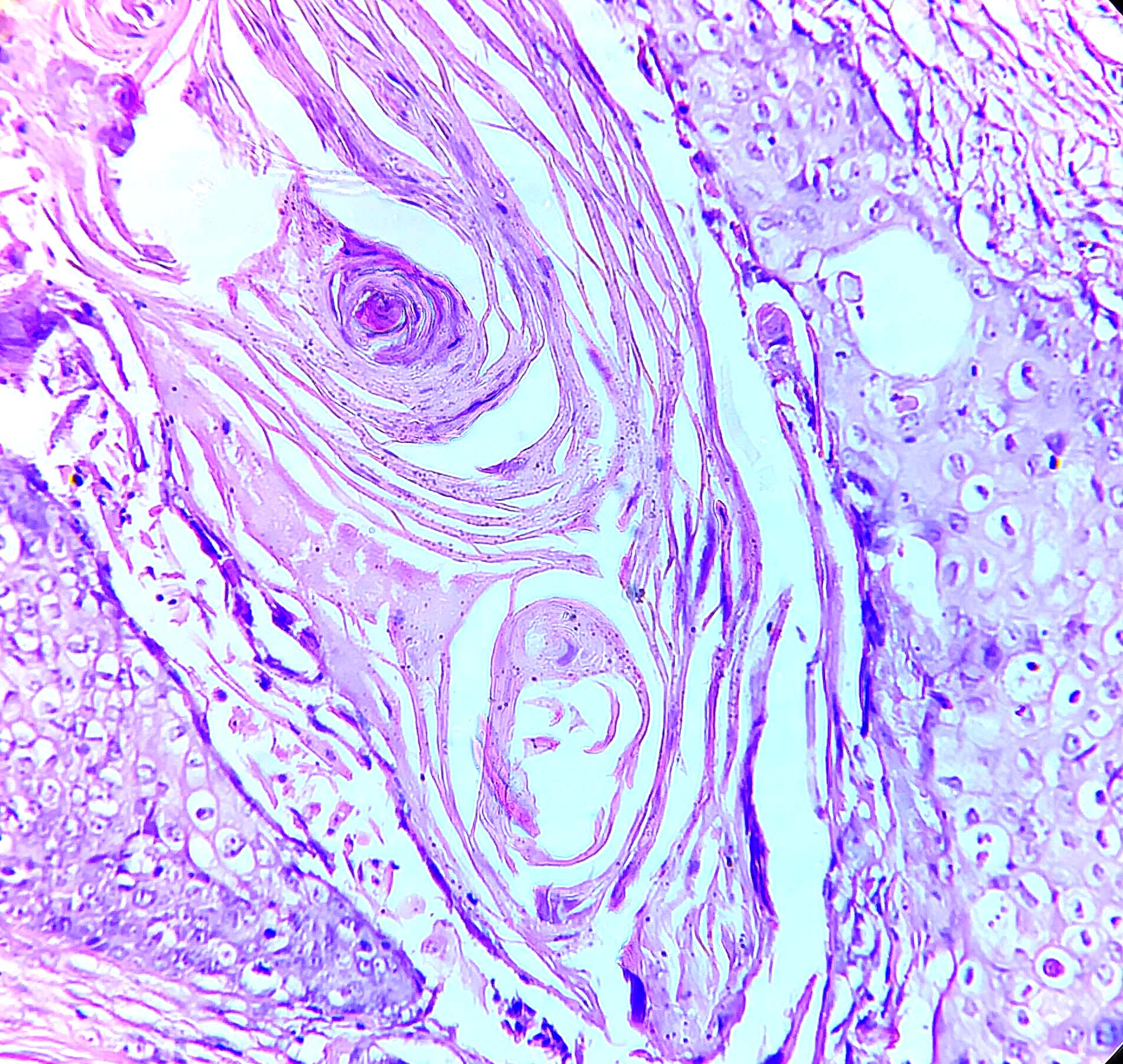
Microscopic (histologic) description
- Considered pure squamous cell carcinoma when squamous component comprises > 90% of the tumor
- Usually presents as a cystic lesion with cavity lined by squamous cells with variable nuclear atypia (Int J Surg Case Rep 2011;2:194)
- Infiltration in surrounding parenchyma as sheets, cords and nests
- Often elicits a significant stromal reaction with prominent inflammatory infiltrates (Cancer 1990;65:272)
- Variable keratinization and spindle cell transformation may be seen
- Acantholytic subtype has pseudovascular or pseudoglandular appearance due to tumor cell discohesiveness, with lining composed of squamous epithelium and spaces with necrotic debris and keratin (Cesk Patol 2011;47:184)
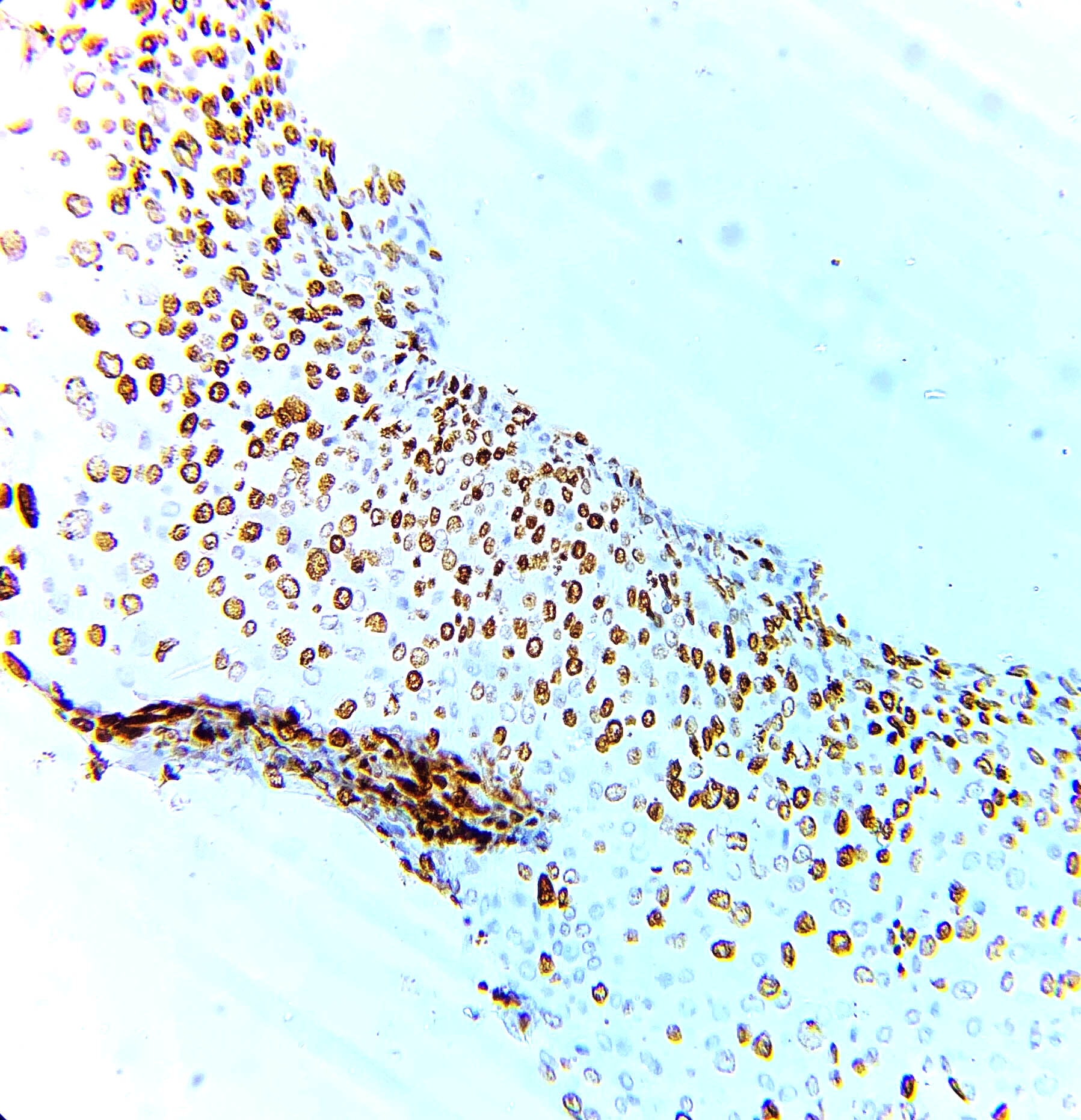
Microscopic (histologic) images
Cytology description
- Squamous cells, isolated and in aggregates, at various stages of maturation (Diagn Cytopathol 2007;35:429)
Cytology images
Positive stains
- EGFR (85%) (Int J Surg Pathol 2005;13:319, Anticancer Res 2007;27:547)
- CK5/6 (75%), p63 (70%), p40 (Anticancer Res 2007;27:547)
- Ki67 index > 20% (i.e., high proliferative index) (77%) (Anticancer Res 2007;27:547)
Negative stains
- Usually ER and PR; however, a few positive cases have been documented
- HER2 (93%) (Anticancer Res 2007;27:547)
- Mucin, CEA and vascular markers
- Acantholytic variant: EMA, factor VIII, PAS and Alcian blue
Electron microscopy description
- Composed of whorls of squamous epithelial cells that contain numerous cytokeratin filaments and tonofibrils (Am J Surg Pathol 1993;17:248)
- Cells are joined by large number of mature desmosomes (Am J Surg Pathol 1993;17:248)
- May have glandular features ultrastructurally (Arch Pathol Lab Med 1980;104:130)
Molecular / cytogenetics description
- Displays a basal-like molecular phenotype and usually shows poor prognostic features; lack of BRCA1 expression is expected (Anticancer Res 2007;27:547)
Sample pathology report
- Left breast, upper quadrant, core needle biopsy:
- Squamous cell carcinoma (see comment)
- Comment: The tumor shows extensive squamous differentiation. The differential diagnosis includes
- Metaplastic carcinoma of the breast with squamous cell differentiation, primary squamous cell carcinoma breast and metastatic squamous cell carcinoma from a non mammary primary site. Additional clinical and radiologic correlation is recommended.
- Left breast, upper outer quadrant, wide local excision:
- Primary squamous cell carcinoma breast
Differential diagnosis
- Metastatic squamous cell carcinoma to the breast:
- Radiological or clinical evidence of tumor at other sites, such as oral cavity bronchus, esophagus, renal pelvis, bladder, ovary, cervix and anus
- p16 and HPV genotyping may be useful if known history of HPV driven SCC at another site
- Metaplastic carcinoma with squamous differentiation
- < 90% squamous differentiation, mixed with other types of metaplastic carcinoma or no special type
- Low grade adenosquamous carcinoma
- Low grade glandular component
- Phyllodes neoplasm with cystic / extensive squamous metaplasia:
- Biphasic fibroepithelial lesions with stromal and glandular epithelial components
- Absence of nuclear atypia and significant mitosis in the squamous component
- Other histological features of phyllodes neoplasm, such as leaf-like architecture, stromal growth, etc.
- Extensive metaplasia in benign conditions like fibroadenoma, breast abscess, chronic inflammation and cyst (Eur J Cancer Care (Engl) 2009;18:650):
- Squamous component is benign
- Other histological features pertaining to the primary disease
- Acantholytic variant may mimic angiosarcoma:
- Endothelial cells line spaces and are CD31+, CD34+, keratin- (Am J Surg Pathol 1986;10:855, Head Face Med 2008;4:17)
- Posttraumatic lobular squamous metaplasia (Mod Pathol 1988;1:385):
- Lobular growth pattern with bland cytology
Board review style question #1
A 65 year old woman presented with well defined swelling of the upper inner quadrant of the right breast. Histological details are shown in the figure above. Which of the following statements is true of this entity?
- Commonly presents as a solid homogenous mass
- Has a low proliferative index
- Is never more than 4 cm in greatest dimension
- May metastasize without locoregional lymph node involvement
Board review style answer #1
D. May metastasize without locoregional lymph node involvement. The microphotograph shows a neoplasm with tumor cells arranged in islands. These cells are polygonal and have pleomorphic hyperchromatic nuclei with a moderate to abundant amount of dense eosinophilic cytoplasm. No other type of invasive component is seen. These features are consistent with primary squamous cell carcinoma of the breast.
Primary squamous cell carcinoma of the breast is less likely to be associated with lymph node metastasis and may metastasize even without axillary lymph node involvement. It is usually of larger size at the time of presentation and has a high proliferative index.
Comment Here
Reference: Squamous cell carcinoma of breast
Primary squamous cell carcinoma of the breast is less likely to be associated with lymph node metastasis and may metastasize even without axillary lymph node involvement. It is usually of larger size at the time of presentation and has a high proliferative index.
Comment Here
Reference: Squamous cell carcinoma of breast
Board review style question #2
Which of the following statements about primary squamous cell carcinoma (SCC) of the breast is true?
- Can always be diagnosed on core needle biopsy
- Can arise at any anatomical site in the breast
- Is more commonly encountered in perimenopausal women
- Is very responsive to conventional chemotherapy and radiotherapy
Board review style answer #2
B. Can arise at any anatomical site in the breast. Primary squamous cell carcinoma (SCC) of the breast is commonly encountered in postmenopausal women. It does not have any specific site involvement but can arise at any anatomical location in a breast. All or at least > 90% of the tumor cells should be squamous for diagnosis, which requires evaluation of the entirety of the neoplasm; hence, SCC cannot be diagnosed on core needle biopsy alone. It is an aggressive tumor and is often refractory to conventional treatment options.
Comment Here
Reference: Squamous cell carcinoma of breast
Comment Here
Reference: Squamous cell carcinoma of breast