Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Sardana R, Singh K. Micropapillary. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/breastmalignantmicropapillary.html. Accessed March 30th, 2025.
Definition / general
- Micropapillary carcinoma is characterized by pseudopapillary, tubular and morular epithelial structures with inside out growth pattern (WHO Classification of Tumours Editorial Board: Breast Tumours, 5th Edition, 2019)
- Micropapillae are composed of cell clusters with inverted polarity floating in empty spaces and often separated by delicate strands of fibrous stroma (Am J Clin Pathol 2004;121:857)
- First described by Fisher et al. as exfoliative appearance (Am J Clin Pathol 1980;73:313)
- Micropapillary carcinoma terminology first used by Tavassoli (Mod Pathol 1993;6:660)
Essential features
- Pseudopapillae, morulae or tubules with inside out growth pattern characterized by reverse polarity of cells
Terminology
- Invasive micropapillary carcinoma: > 90% of invasive component consists of micropapillary carcinoma
- Also acceptable: micropapillary carcinoma (WHO Classification of Tumours Editorial Board: Breast Tumours, 5th Edition, 2019)
- Invasive breast carcinoma with micropapillary component: micropapillary pattern is present in association with other histologic types (more common)
ICD coding
Epidemiology
- < 2 - 8% of all breast cancers (Mod Pathol 2018;31:956)
- Pure micropapillary carcinoma is rare, 0.9 - 2% of all breast cancers; often admixed with other histologic subtypes
- Reported median age: 50 - 62 years
- Mean age: 59 years; range: 25 - 92 years
- Also described in male breast (Breast Care 2018;13:192)
Sites
- Breast parenchyma
Pathophysiology
- Upregulation of several nutrient transporters, such as glucose transporter 1 (GLUT1) via the activation of a transcription factor, hypoxia-inducible factor (Histol Histopathol 2019;34:1009)
- Frequent overexpression of MUC4 (cytoplasmic) (BMC Cancer 2017;17:895)
- Plakoglobin, a key component in cell adhesion, promotes metastasis and downregulates apoptosis in the cell clusters through activation of PI3K / Akt / BCL2 signaling (J Cancer 2019;10:2800)
- Tumor infiltrating lymphocytes usually lack cytotoxic phenotype (Mod Pathol 2008;21:1101)
- Low expression of Fas and FasL in lymphocytes (Mod Pathol 2008;21:1101)
- Increased expression of CD146 and microvessel density (Pathol Res Pract 2011;207:739)
- Overexpression of beta1 integrin and the resultant upregulation of Rac1 contribute to polarity reversal and metastasis (Mod Pathol 2004;17:1045, Oncotarget 2017;9:4338)
- Increase in CD44+ / CD24-/low tumor cells (Pathol Res Pract 2010;206:828, Arch Pathol Lab Med 2016;140:799)
- Sialyl Lewis X / CD15s, the ligand of E-selectin, also exhibits reversed cell polarity in these tumors (Int J Surg Pathol 2010;18:193)
Etiology
- Unknown
Clinical features
- Almost 90% present as a palpable mass
- Radiologic findings, locations and gross features similar to conventional invasive breast carcinoma (BMC Cancer 2017;17:839)
- Aggressive clinical presentation with large tumor size (often T2), frequent positive lymph nodes at initial presentation and advanced stage when compared with invasive ductal carcinoma (Cancer Med 2017;6:2775)
- Mean size: 1.5 - 3.9 cm
- Frequent and higher number of axillary nodal metastasis (44 - 85%) at initial diagnosis
Diagnosis
- Tissue biopsy or surgical resection
Radiology description
- Multiple lesions, accompanying nonmass enhancement and axillary lymph node enlargement
- Irregular spiculated mass on mammogram
- Irregular hypoechoic mass with spiculated margins and posterior acoustic shadowing on ultrasound
- Irregular mass with washout kinetics and diffuse heterogeneous mass-like enhancement in MRI
- Radiologists to consider axillary sonography if this entity is found in a core needle biopsy specimen (AJR Am J Roentgenol 2013;200:689)
Prognostic factors
- Traditionally, presence of micropapillary carcinoma component has been considered a poor prognostic factor; however, the data has been controversial
- Meta analysis of 14 published studies showed that presence of micropapillary carcinoma histology is an unfavorable prognostic factor for recurrence free survival and locoregional recurrence free survival (BMC Cancer 2017;17:839)
- Micropapillary carcinoma component did not significantly impact overall survival, disease specific survival and distant metastasis free survival (BMC Cancer 2017;17:839)
- Similar overall survival and better disease specific survival has been described when compared with invasive ductal carcinoma (PLoS One 2014;9:e106564)
- Other studies have reported poorer relapse free survival and overall survival with micropapillary carcinoma when compared with invasive ductal carcinoma (Int J Surg Pathol 2008;16:155, Clin Breast Cancer 2015;15:353, BMC Cancer 2017;17:839)
- Similar prognosis as other breast carcinoma subtypes if node status, tumor size and other classic prognostic markers are considered (Hum Pathol 1999;30:1459)
- Focal component found in 6% of all breast carcinomas - these cases have same poor prognosis regardless of amount of micropapillary component (Mod Pathol 2001;14:836, Am J Clin Pathol 2006;126:740)
- Exception is that presence of micropapillary pattern in mucinous / colloid carcinoma of breast may have no clinical significance (Int J Surg Pathol 2008;16:251)
- Presence of micropapillary features and retraction artifact in core biopsies predicts nodal metastases (Am J Surg Pathol 2009;33:202)
Case reports
- 35 year old woman with multifocal grade 3 invasive micropapillary carcinoma associated with metaplastic breast carcinoma (Int J Surg Pathol 2012;20:488)
- 51 year old woman with myoepithelial carcinoma and contralateral invasive micropapillary carcinoma of the breast (J Korean Surg Soc 2011;81:211)
- 60 year old man with triple positive micropapillary carcinoma with axillary lymph node involvement (Breast Care 2018;13:192)
- 66 year old man with pure invasive micropapillary carcinoma (Can J Surg 2005;48:156)
- 69 year old woman with micropapillary carcinoma associated with osteoclast giant cells (Int J Surg Pathol 2015;23:654)
Treatment
- Tumors are typically ER positive and are eligible for antiestrogen treatment
- Treatment varies depending on clinical stage (tumor size and lymph node metastasis)
Gross description
- No specific gross features; tumors with > 50% of micropapillary growth tend to be larger (mean: 6 cm) than those with lesser amount of this pattern (mean: 3.5 cm)
- Mean tumor size: 2 cm; range: 0.1 - 10 cm
- Lobulated outline
Microscopic (histologic) description
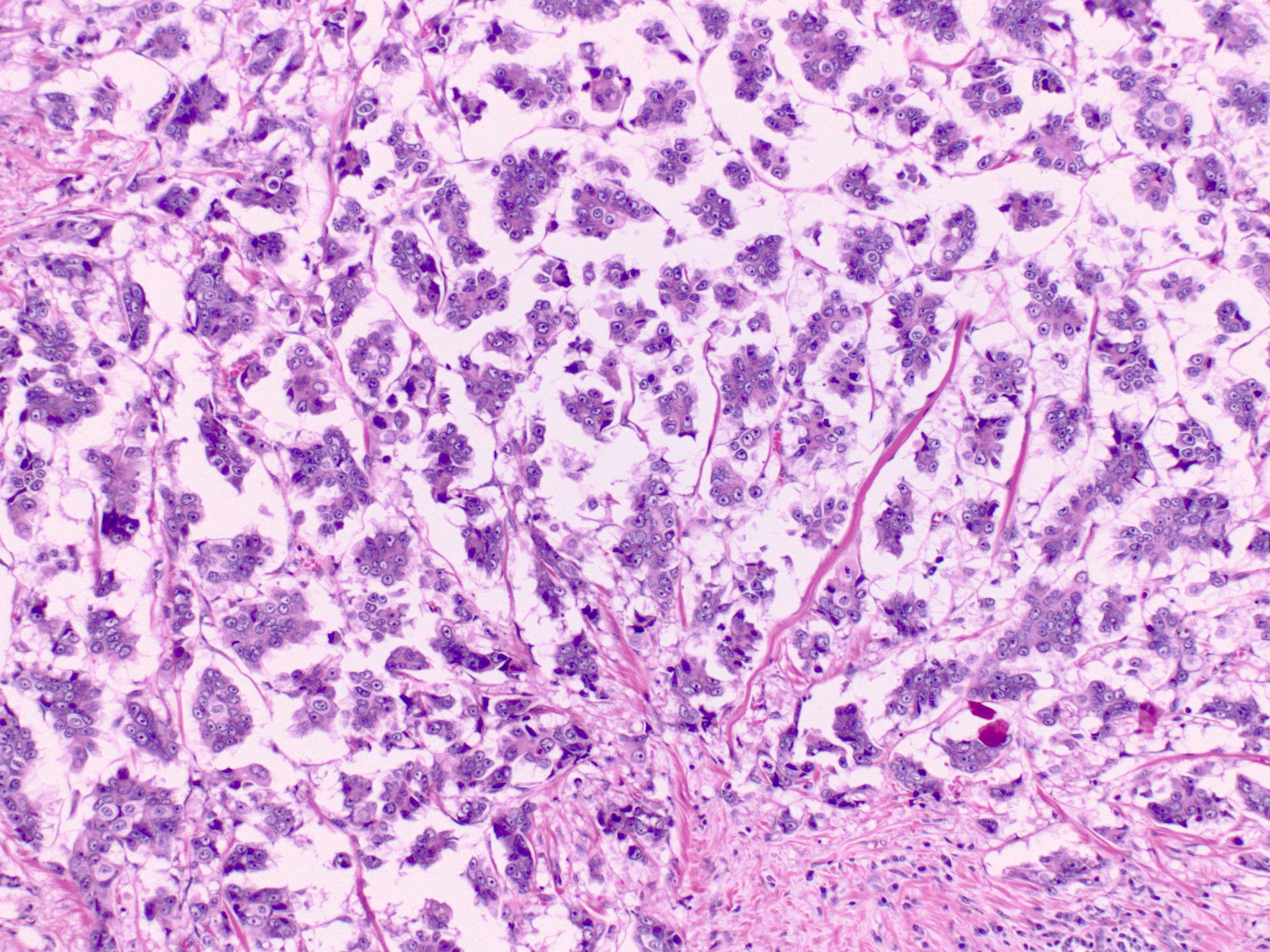
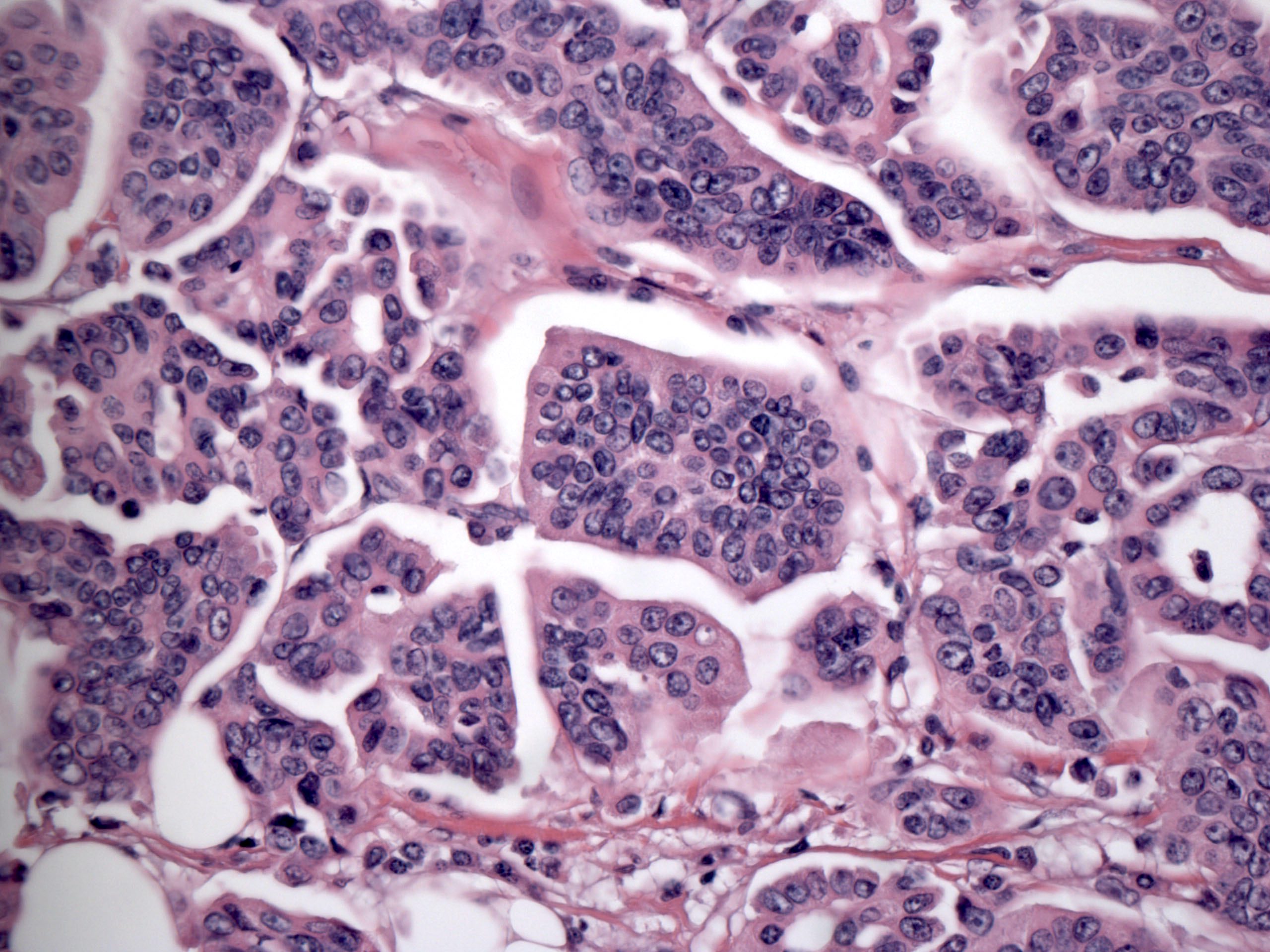
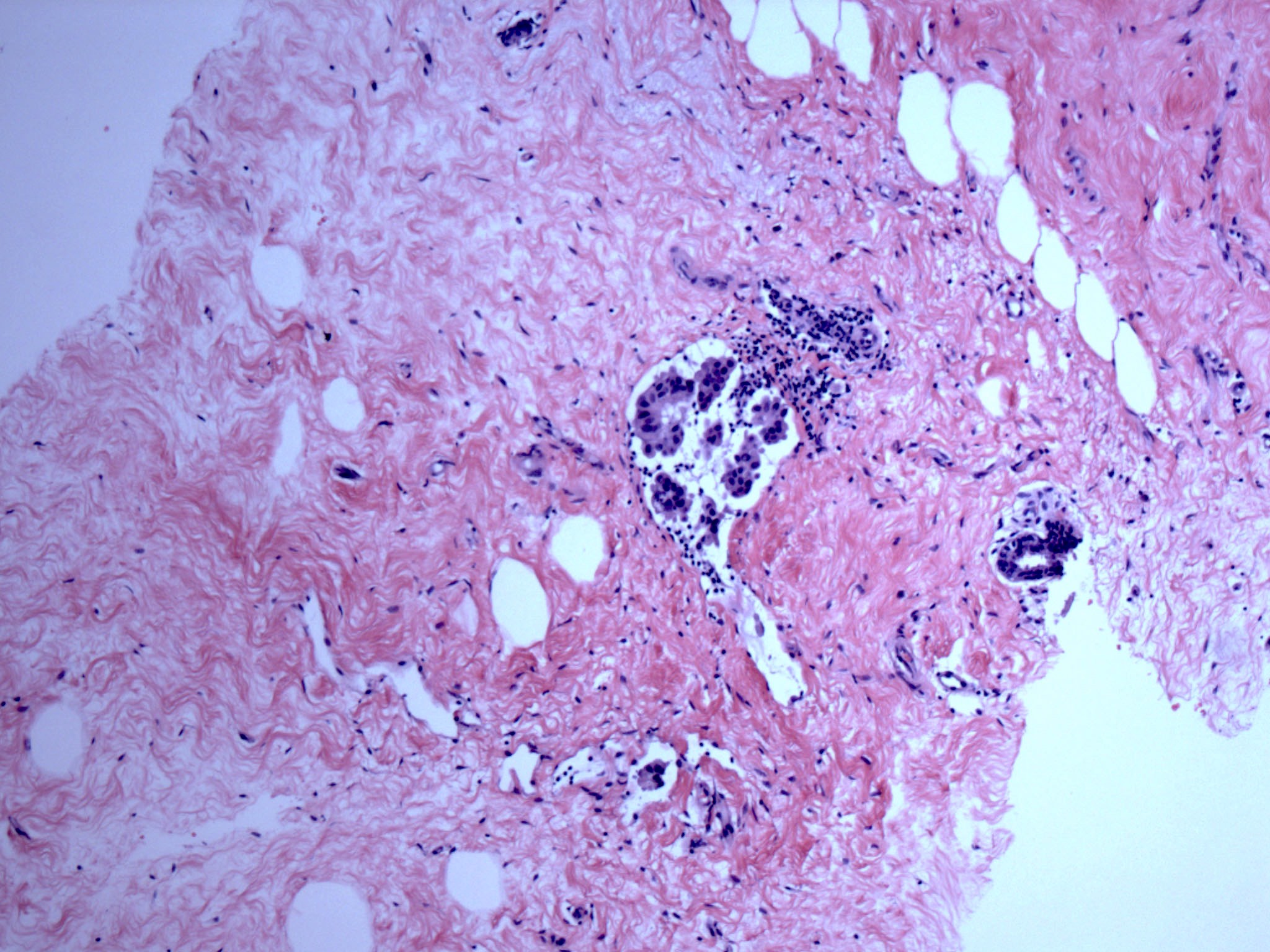
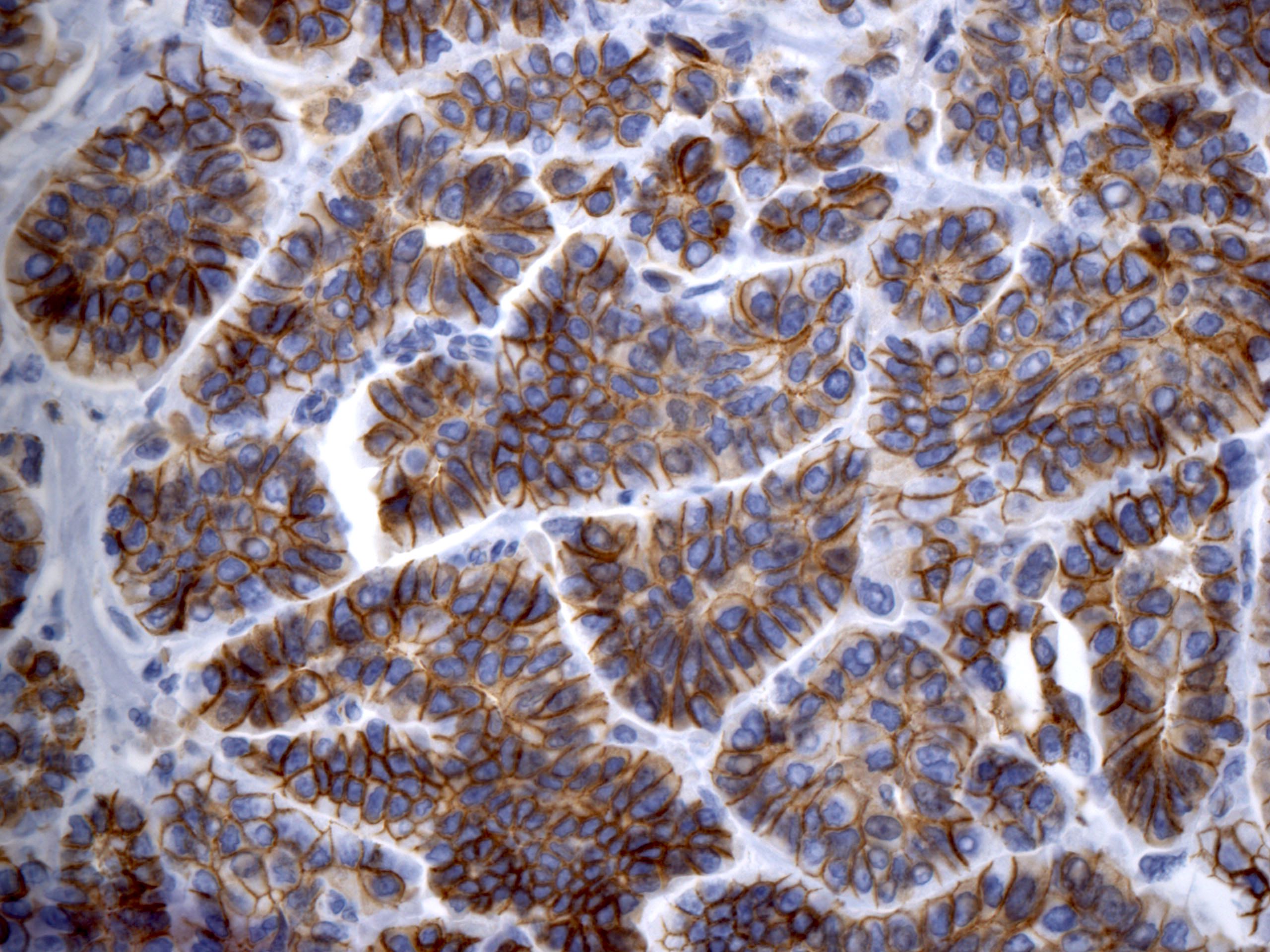
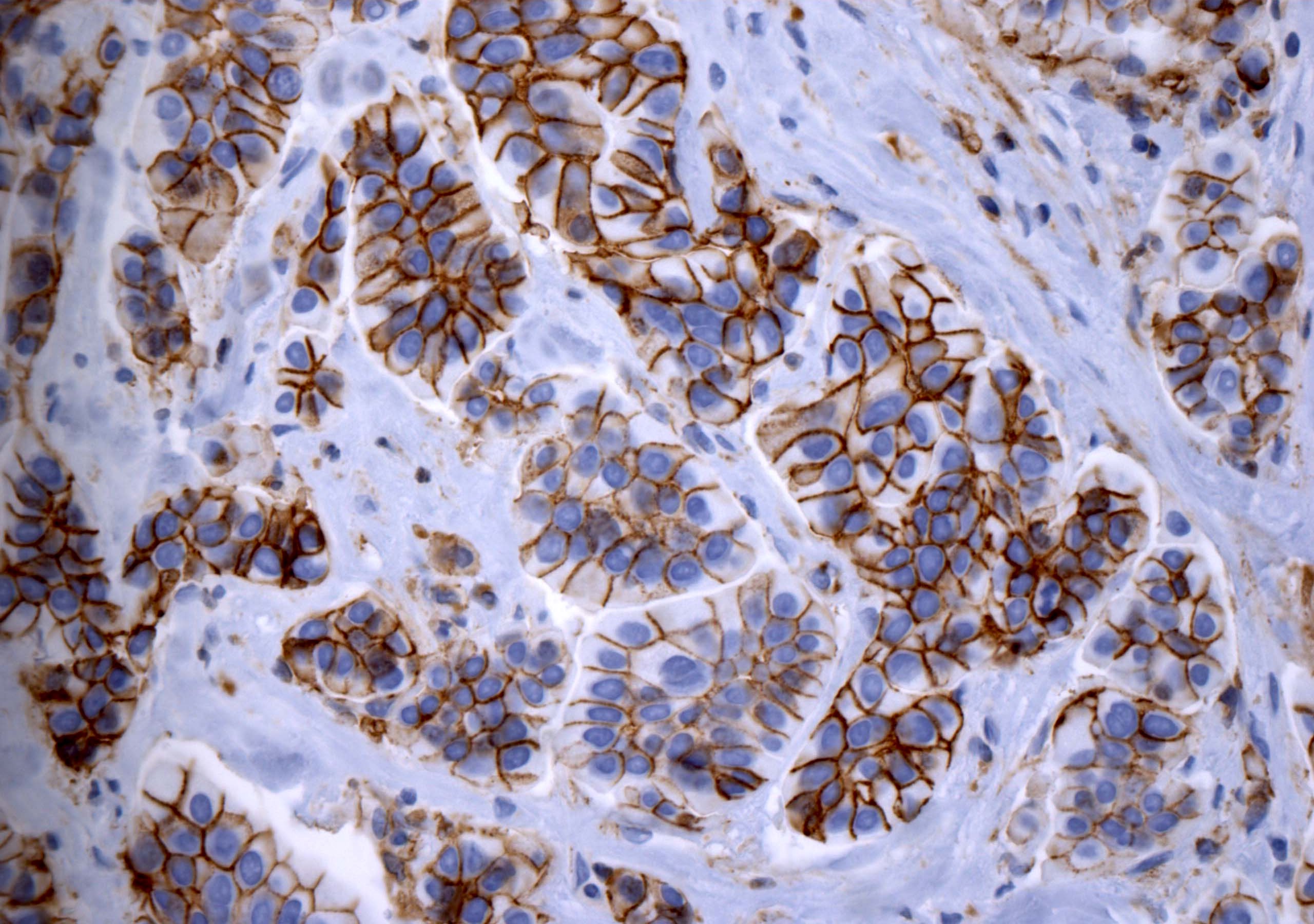
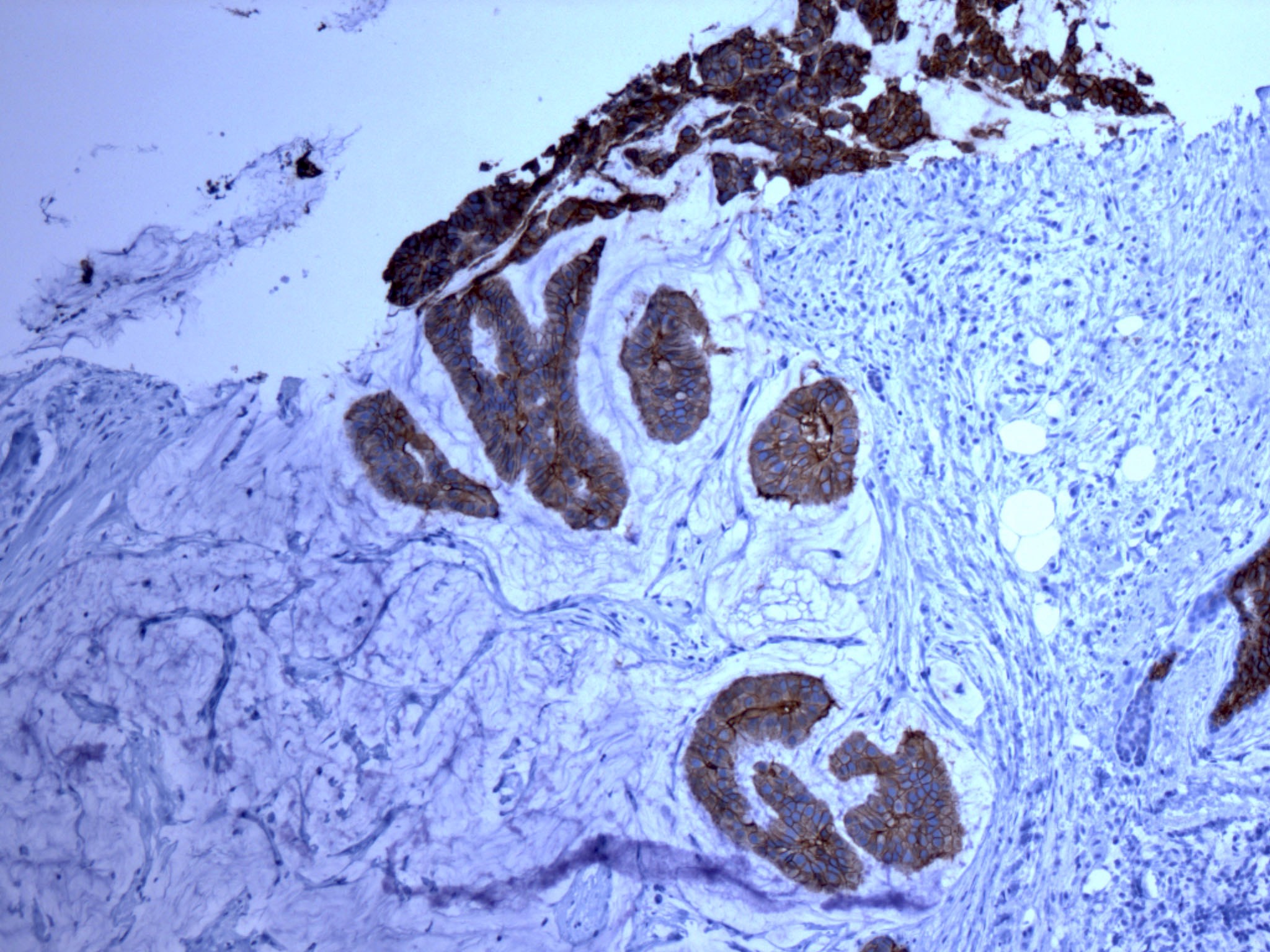
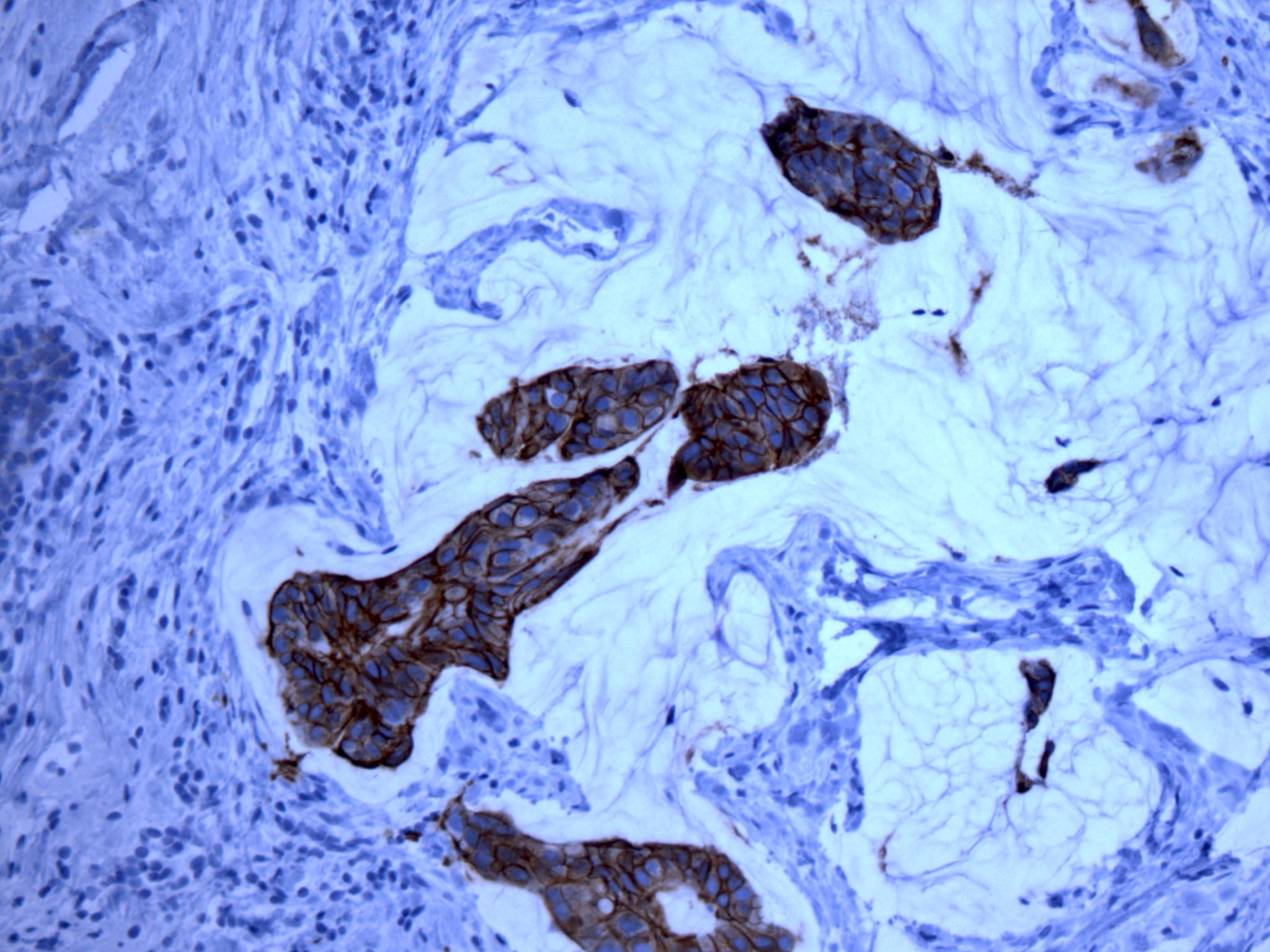
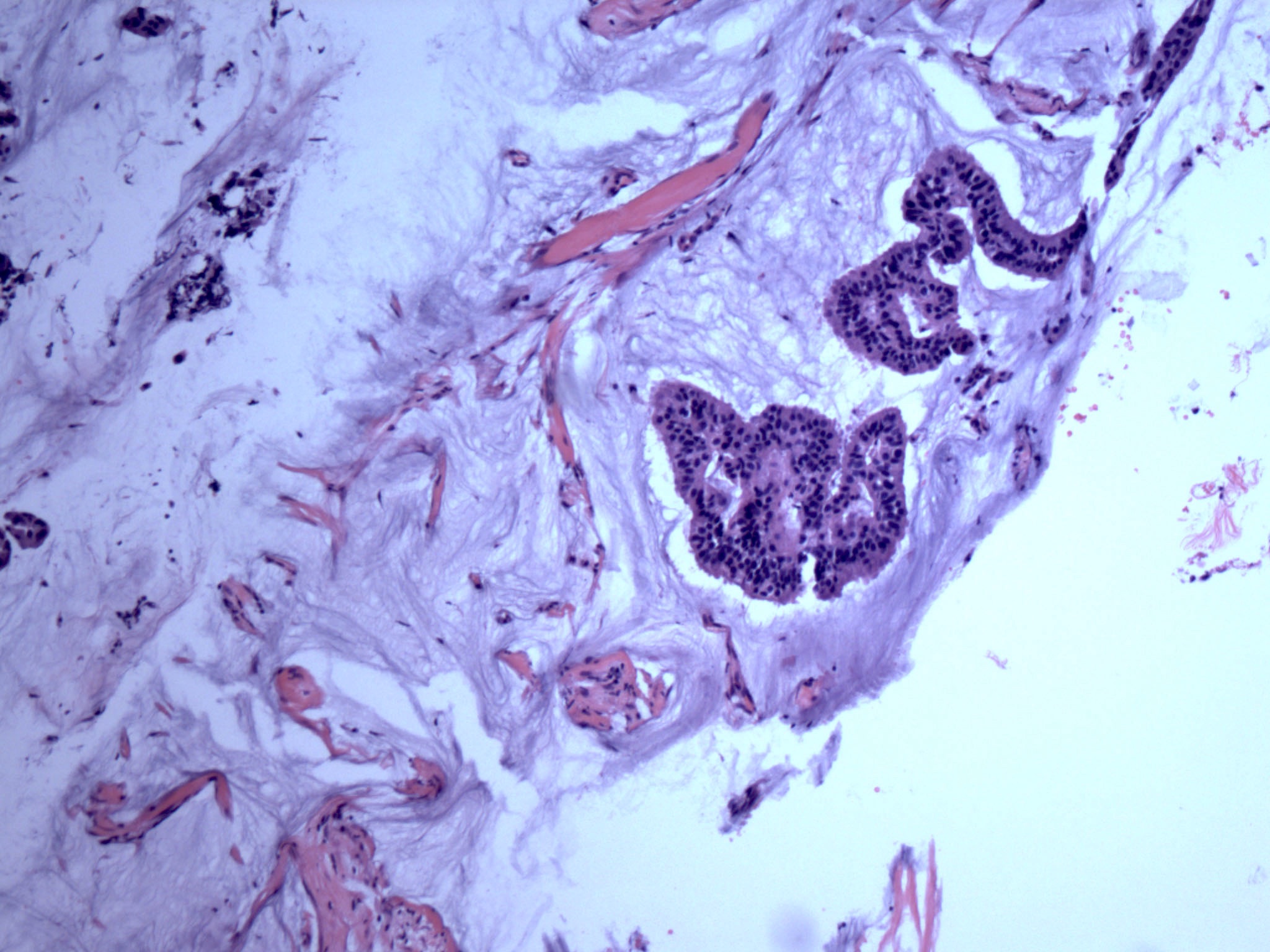
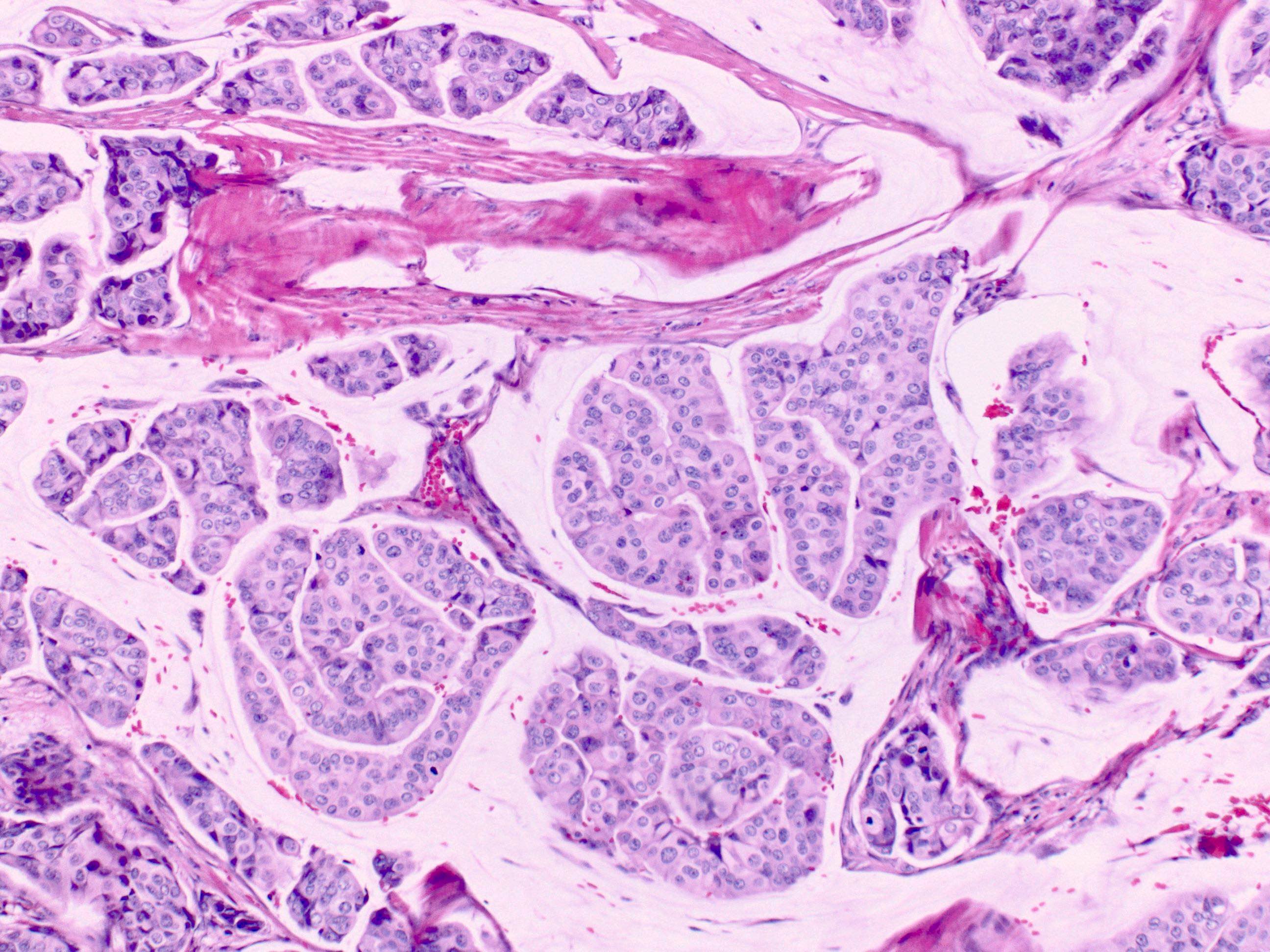
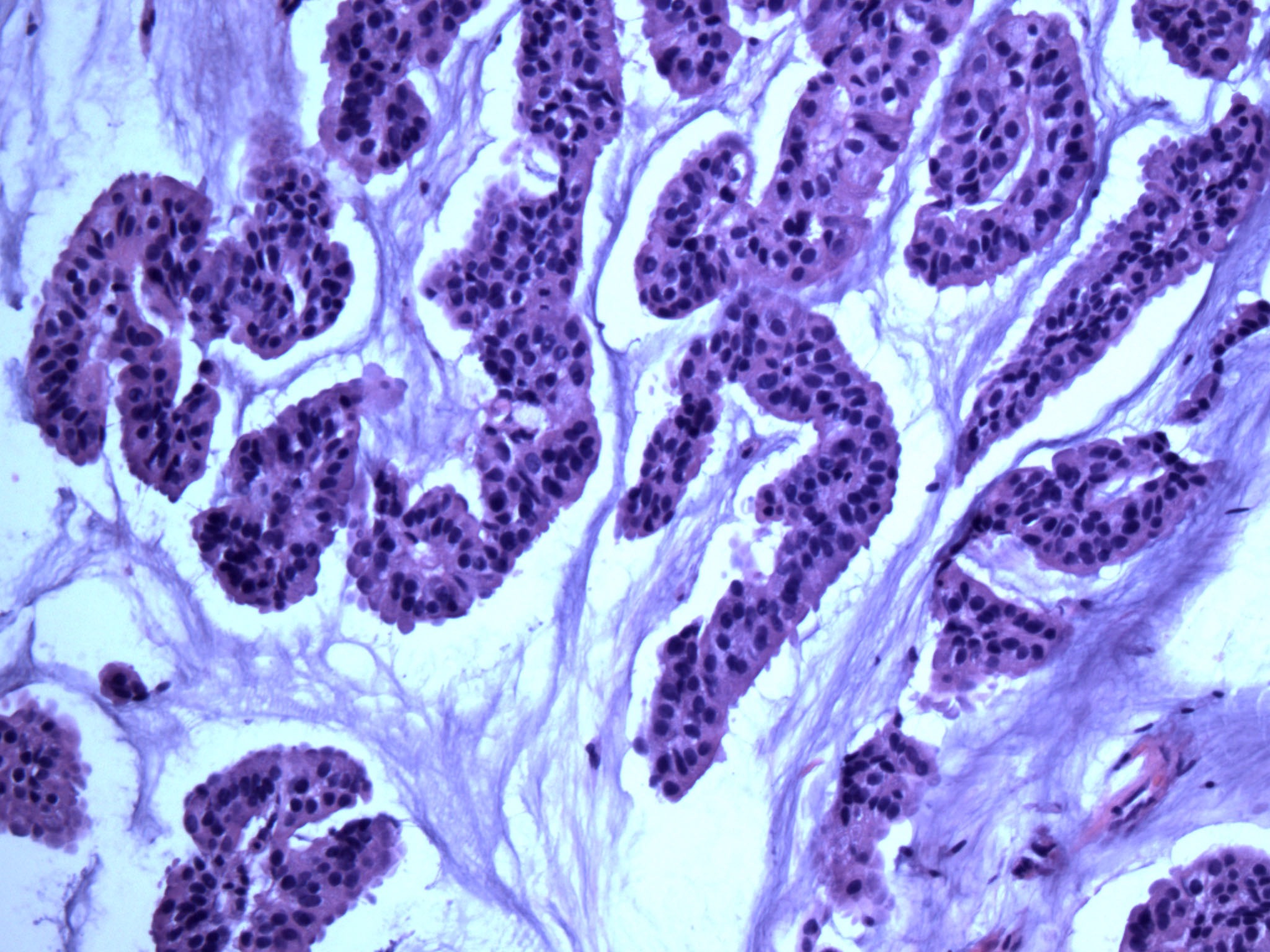
- Tufts of cells arranged in pseudopapillae, hollow tubules and morula that are surrounded by empty clear spaces formed by fibrocollagenous stroma (Arch Pathol Lab Med 2016;140:799)
- Cells show characteristic reverse polarity, also called inside out pattern, with apical surface abutting the epithelial stromal interface
- Densely cellular, with minimal stroma
- Abundant eosinophilic cytoplasm
- Nuclei around the periphery bulge with knobby / serrated appearance
- Extensive true angiolymphatic invasion (78%)
- Foci of necrosis may be present
- May have intracytoplasmic mucin
- Uncommon variant feature: psammoma bodies, microcystic dilation of lumens with cell clusters, apocrine differentiation, multinucleated giant cells (e.g. osteoclast)
- Variable histologic grade, usually grade 2 or 3
- Mucinous carcinoma can contain micropapillary component, also called mucinous micropapillary carcinoma
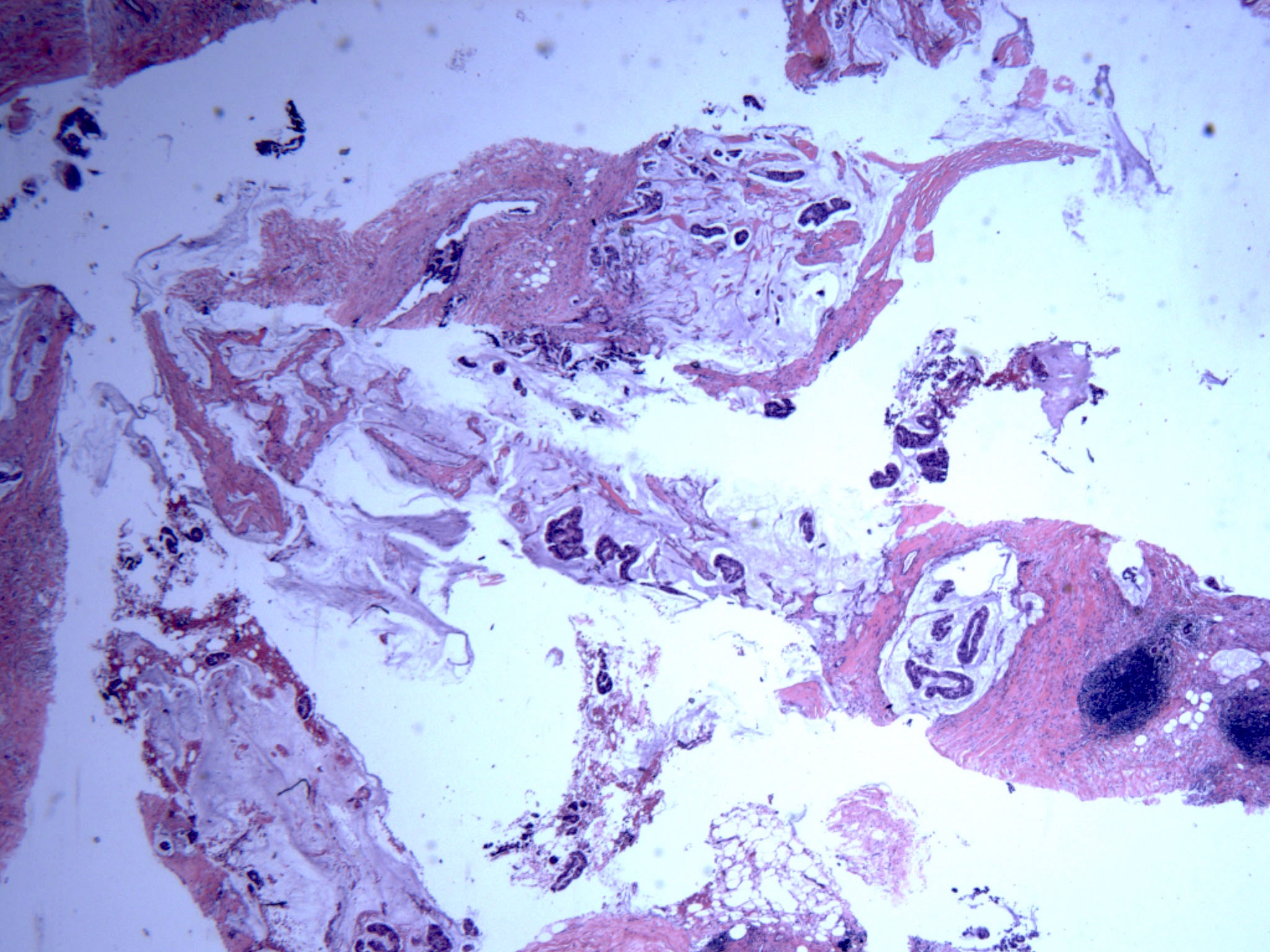
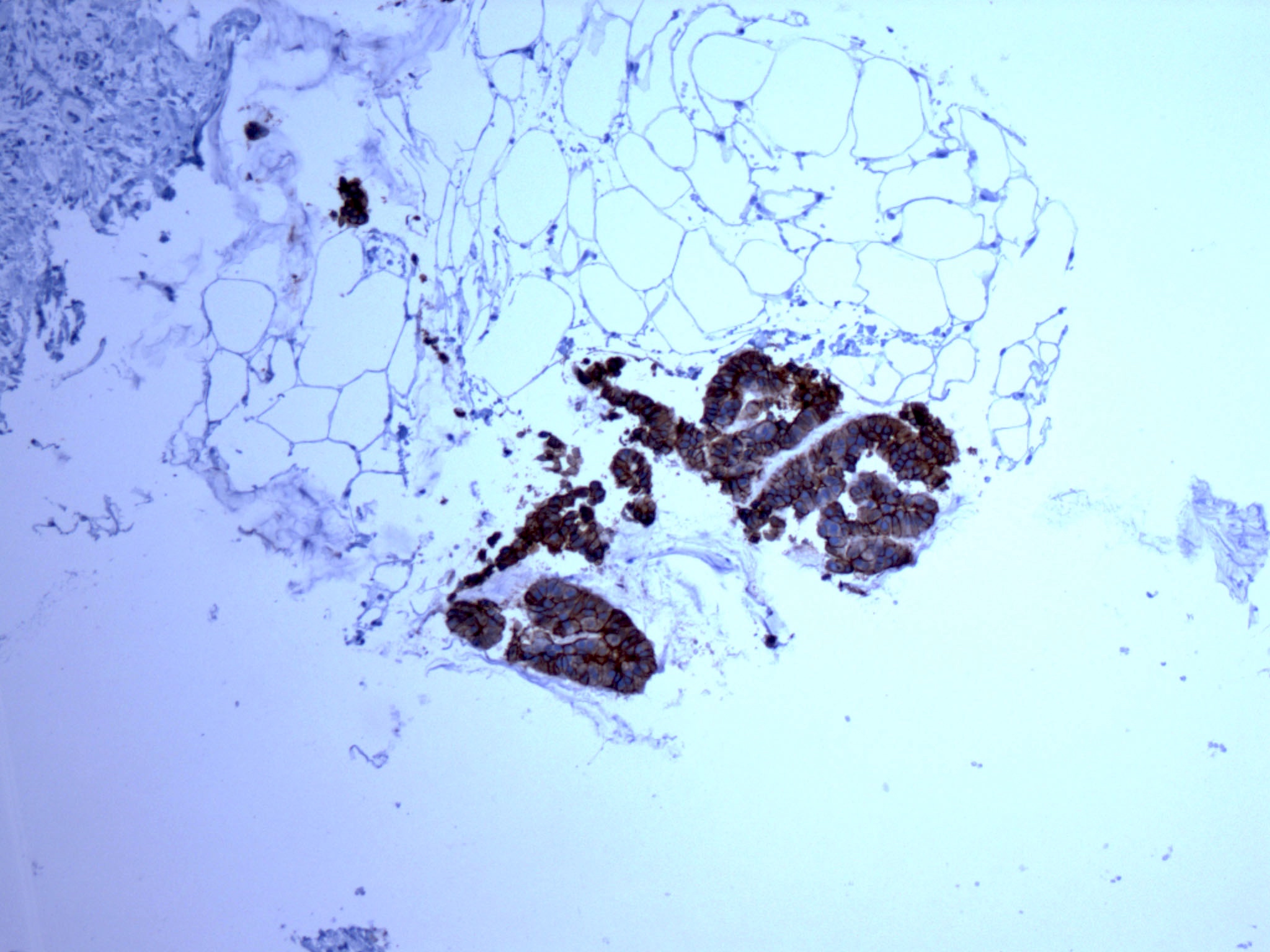
Microscopic (histologic) images
Cytology description
- Increased cellularity, angulated clusters, abortive papillae and isolated malignant cells
- Staghorn epithelial structures in 35%, giving serrated border (Pathology 2007;39:401)
- May have few malignant appearing multinucleated giant cells or focal mucin (Acta Cytol 2009;53:463)
- No fibrovascular cores (Cancer 2002;96:280)
Positive stains
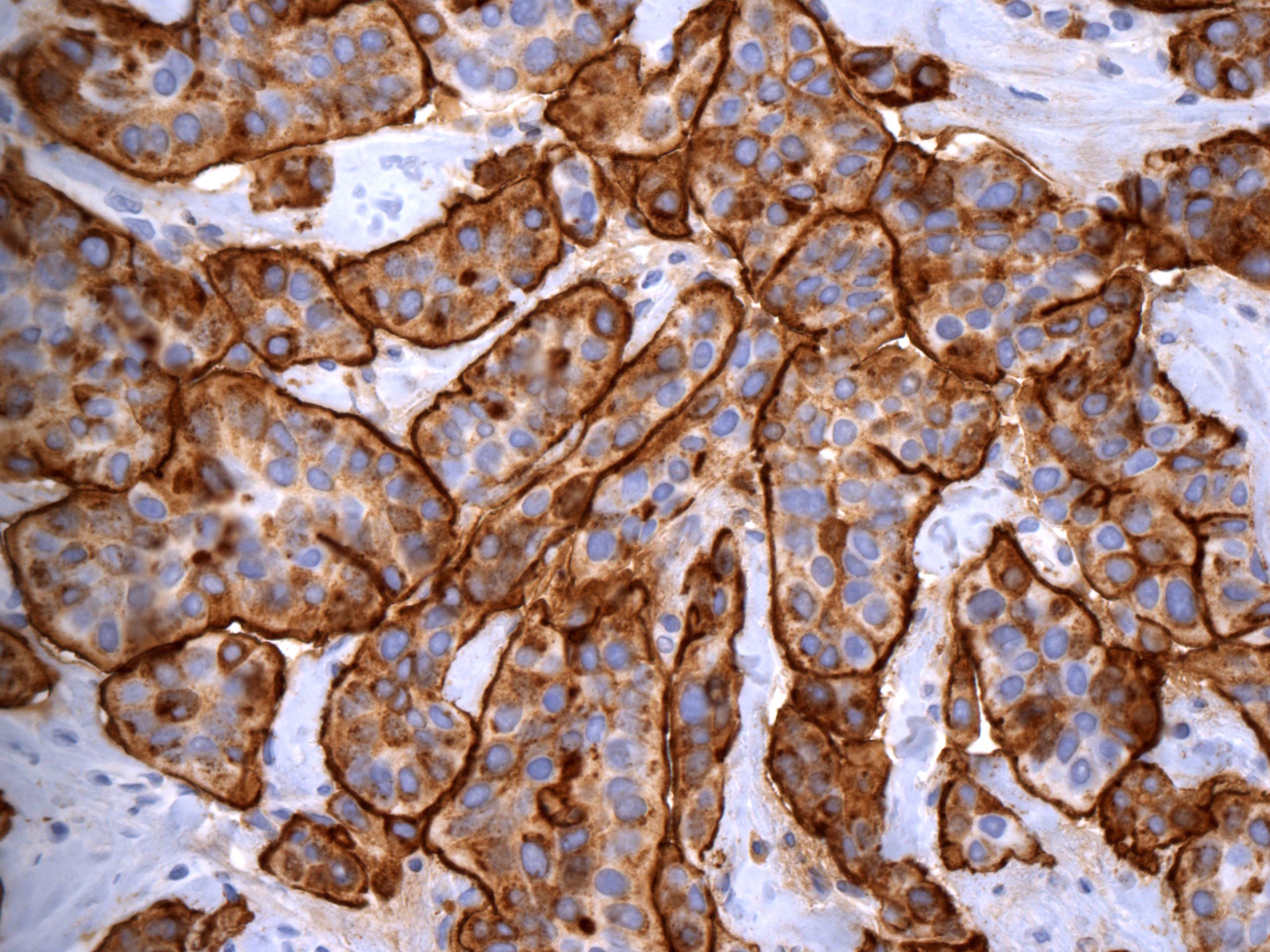
- EMA, CD15s, E-cadherin and p120 catenin: inside out pattern (Arch Pathol Lab Med 2016;140:799)
- EMA and CD15s: membranous staining of tumor cells abutting stroma
- E-cadherin and p120 catenin: cup shaped basolateral membranous staining with sparing of the apical surface
- ER (70 - 94%)
- PR (50 - 84%)
- HER2:
- Reported positivity varies in different studies ranging from 10 - 30% to up to 50 - 80%
- Incomplete basolateral (cup shaped) staining (similar to E-cadherin and p120 catenin)
- GATA3
Negative stains
Electron microscopy description
- Microvilli on their cell membranes lining the outer surfaces of the cell clusters
- Secretory activity in stroma facing surface of tumor cells
Molecular / cytogenetics description
- BC-1514 (C21orf118) is commonly upregulated in the micropapillary area (BMC Cancer 2019;19:76)
- CAMK2N1, CD1d, PJA2, RPL5, SAMD13, TCF4 and TXNIP are commonly downregulated in the micropapillary area (BMC Cancer 2019;19:76)
- Gains of 1q, 8q, 17q, 20q and losses of 1p, 8p, 13q, 16q and 20q (J Pathol 2008;215:398, J Pathol 2014;232:553)
- Mixed tumors have genetic profiles more similar to pure tumors than to ductal carcinoma (J Pathol 2009;218:301)
- High cyclin D1 expression, high proliferation rates and MYC (8q24) amplification (J Pathol 2008;215:398)
Sample pathology report
- Breast, right, 12:00 mass, core needle biopsy:
- Invasive breast carcinoma with micropapillary component, preliminary Nottingham (or modified Bloom-Richardson) grade 2
- Lymphovascular invasion is present
- Comment: The tumor is ER positive (90%; 3+), PR positive (50%; 3+) and HER2 (score 2+) equivocal for overexpression.
- Microscopic (optional): The sample shows a moderately differentiated carcinoma comprised of invasive ductal carcinoma and micropapillary carcinoma components.
- ±% of subtype components: This may be of particular importance if micropapillary pattern makes up the majority (> 90%) of the biopsy sample and the diagnosis of pure micropapillary carcinoma is of consideration, pending full histologic evaluation at resection.
Differential diagnosis
- Metastatic ovarian papillary serous carcinoma:
- Clinical history of ovarian tumor
- PAX8+, WT1+, GATA3-, GCDFP-15- (Hum Pathol 2008;39:666)
- Metastatic micropapillary carcinoma of nonmammary / nonovarian origin (lung, bladder):
- Breast primaries are GATA3+ and ER+, mammaglobin+, PAX8 / WT1-
- Other primaries have different patterns (Am J Surg Pathol 2009;33:1037)
- Extensive lymphovascular invasion by a primary or metastatic breast carcinoma:
- Tumor clusters do not demonstrate reverse polarity
- Mucinous carcinoma with micropapillary pattern:
- Micropapillary epithelium floating in mucin pools
Additional references
Board review style question #1
Which of the following is true regarding the pictured special subtype of breast carcinoma?
- Low stage disease is typical presentation
- Pure micropapillary carcinoma is common
- Tumor cells show circumferential HER2 staining
- Tumor cells show inside out pattern with EMA staining
- Tumor is frequently ER negative
Board review style answer #1
D. Tumor cells show inside out pattern with EMA immunostaining. The pictured lesion shows characteristic features of the micropapillary subtype of invasive breast carcinoma, which is frequently ER positive, with cup shaped basolateral HER2 immunostaining. Tumors often present at high stage with lymph node involvement. Tumor cells show reverse polarity, also known as inside out pattern with apical surface placed towards the stroma. Inside out pattern can be demonstrated by EMA staining of the apical surface.
Comment Here
Reference: Micropapillary carcinoma
Comment Here
Reference: Micropapillary carcinoma
Board review style question #2
The HER2 immunohistochemical staining pattern of tumor cells in micropapillary carcinoma of the breast is
- Apical
- Basal
- Basolateral
- Circumferential
- Cytoplasmic
Board review style answer #2
C. Basolateral. The basal and lateral surfaces of tumor cells in the micropapillary variant of invasive breast carcinoma frequently show membranous staining (cup shaped pattern). No staining is noted on the apical surface that stains with EMA.
Comment Here
Reference: Micropapillary carcinoma
Comment Here
Reference: Micropapillary carcinoma