Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Gill HK, Harmon BE. Microinvasive. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/breastmalignantmicroinvasion.html. Accessed December 26th, 2024.
Definition / general
- Microinvasive carcinoma is defined by invasive carcinoma measuring ≤ 1 mm in size
- Classified as American Joint Committee on Cancer (AJCC) T1mi
Essential features
- Microinvasive carcinoma is defined by single or multiple foci of invasive tumor cells measuring ≤ 1 mm in size
- It is usually an invasive breast carcinoma of no special type (ductal) present in periductal stroma adjacent to a duct involved by high grade ductal carcinoma in situ (DCIS); more rarely it can be other histologic types such as invasive lobular carcinoma, which has been described in association with lobular carcinoma in situ (LCIS) (particularly pleomorphic LCIS)
- Microinvasive carcinoma can be of any molecular subtype (luminal A-like, luminal B-like, HER2 overexpressing or basal / triple negative category)
- Clinical and radiologic presentation of microinvasive breast carcinoma is similar to the presentation of the associated in situ carcinoma
- World Health Organization (WHO) 5th edition of the classification of tumors published in 2019
- Microinvasive breast carcinoma is the earliest form of invasive breast carcinoma that can be recognized morphologically
- Defined as invasive breast carcinoma that is 1 mm or less in size and is usually associated with DCIS
Terminology
- Microinvasive carcinoma is the preferred terminology
- Carcinoma in situ with microinvasion is not a recommended term
ICD coding
- Microinvasive carcinoma does not have an ICD-10 code; the code for the type of invasive carcinoma it represents can be used (carcinoma of no special type, invasive lobular carcinoma, etc.)
Epidemiology
- Accounts for < 1% of all breast cancers
- Median age of 59 years of age but has a wide range (J Surg Res 2020;254:378)
Sites
- Can be found in any site of the breast
Pathophysiology
- Main pathogenesis of the transition to stromal invasion are likely the alteration in normal cells, loss of basement membrane maintenance and the microenvironment (Clin Cancer Res 2020;26:3682)
- DCIS is a nonobligate precursor of invasive ductal carcinoma, no special type (IDC, NST), whose mechanisms of progression to invasive breast cancer are diverse and vary from case to case (Clin Cancer Res 2020;26:3682)
Etiology
- Transition from carcinoma in situ (CIS) to stromal invasion is similar to invasive breast carcinoma
- Incidence and risk factors vary in the literature
- Size of DCIS may be associated with presence of microinvasion (3% risk for DCIS < 5 mm increasing to 23% risk for DCIS > 50 mm) (Cancer 1990;66:102)
- CIS associated with invasion has the following features (Ann Surg Oncol 2014;21:3330)
- Higher proliferative rate and enhanced apoptosis
- Higher levels of matrix metalloproteases expression
- Less likely to be ER+
- More likely to be HER2+
Clinical features
- No specific clinical features; clinical and imaging features are those of the associated in situ carcinoma
- Not palpable
- Commonly found by chance during microscopic evaluation for in situ carcinoma
- In rare cases, microinvasive carcinoma can be seen arising from Paget disease of nipple and skin changes (Hum Pathol 2014;45:2480)
Diagnosis
- Histologic examination of involved tissue
Radiology description
- Imaging features of in situ carcinoma; majority present with mammographic calcifications
Prognostic factors
- Overall prognosis is excellent (Hum Pathol 2013;44:2684)
- Sentinel lymph node positivity rate of 3.2% for macrometastasis and 4% for micrometastasis (Eur J Surg Oncol 2014;40:5)
- Prognosis of microinvasive carcinoma has been shown by some studies to be equivalent to DCIS (Am J Surg 2013;206:478)
- Other studies have shown it to be closer to that of very small invasive carcinoma (Breast Cancer Res Treat 2018;167:787, Oncotarget 2016;7:64182)
- Large systematic review and meta analysis found only lymph node status to be associated with prognosis and disease free survival (DFS) (ER, PR, HER2, multifocality, grade of microinvasion, patient’s age and lymph node status evaluated) (Cancers (Basel) 2023;15:3007)
- Microinvasion is associated with the following, although none were found to be an independent predictor of microinvasion
- More extensive DCIS
- Higher grade
- Comedo or solid histologic pattern
- Necrosis and microcalcifications
Case reports
- 44 year old woman with an enlarged axillary mass (Jpn J Clin Oncol 1998;28:47)
- 47 year old woman with HER2+ microinvasive breast carcinoma with an aggressive course (BMC Res Notes 2014;7:325)
- 51 year old woman with microinvasive carcinoma arising within a fibroadenoma (Acta Radiol 2006;47:643)
- 80 year old woman with left sided breast lump (J Cytol 2016;33:98)
- Case series of 121 cases of breast microinvasive carcinoma with different morphologies (Breast Cancer (Auckl) 2020;14:1178223420948482)
Treatment
- Surgical
- Microinvasive carcinoma with DCIS requires surgical excision with negative margins (> 2 mm) (Ann Surg Oncol 2013;20:811)
- Axillary sentinel lymph node biopsy should be strongly considered, as additional foci of invasion may be detected on excision
- Radiation therapy after breast conserving excisional procedures to reduce rates of local recurrence
- Adjuvant hormonal therapy (such as tamoxifen or aromatase inhibitor) in cases that are ER+
- Anti-HER2 therapy can be considered in HER2 positive cases but present literature is conflicting on the benefits in the setting of microinvasive carcinoma (Cancers (Basel) 2021;13:5836)
Gross description
- Gross features of in situ carcinoma
- Gross breast tissue is usually firm but without discrete mass and it is usually white or gray in color, so careful examination of the entire breast specimen should be done
- There may be necrotic debris extruded from ducts if the DCIS has associated comedonecrosis
- Reference: Hum Pathol 1998;29:1412
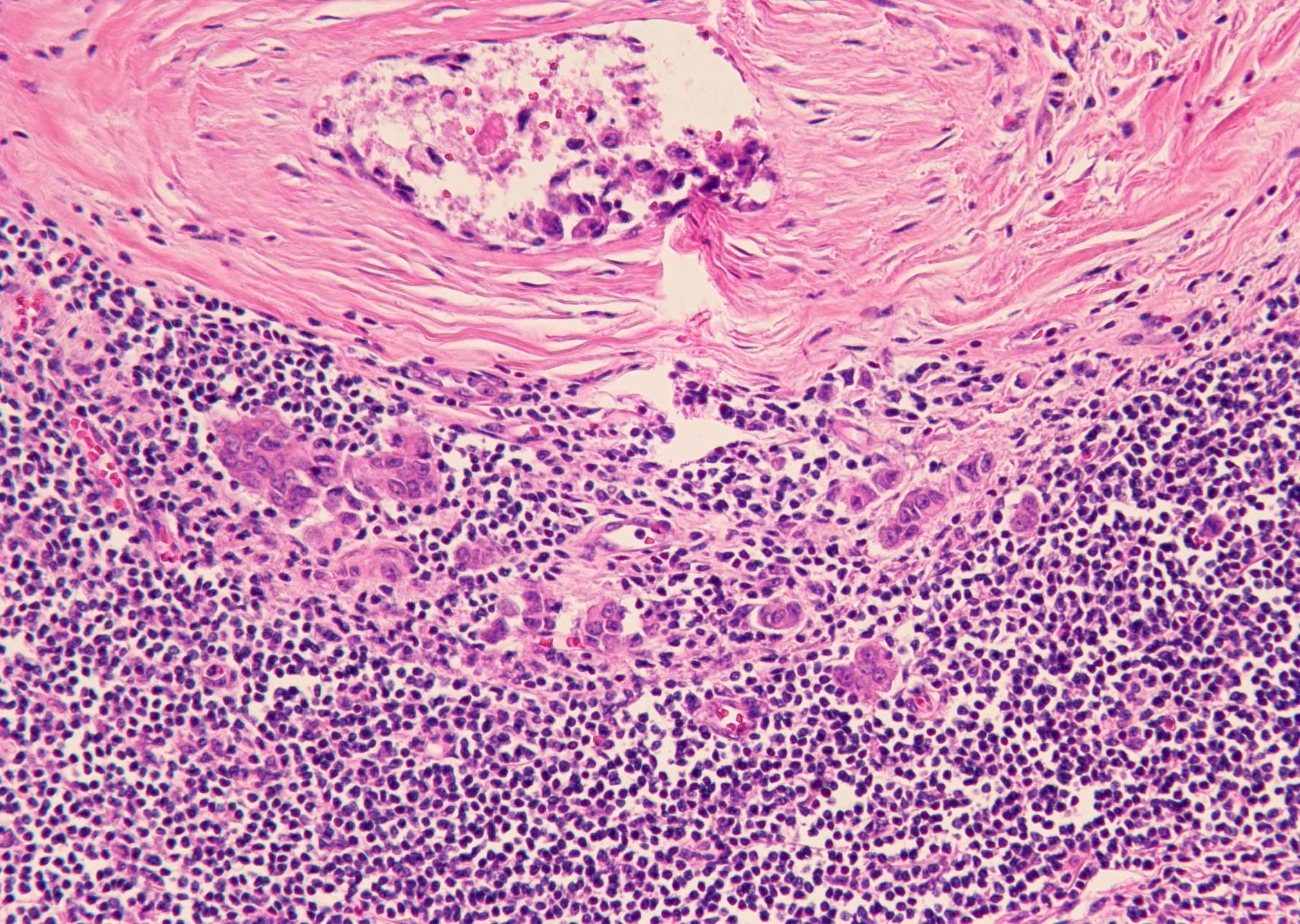
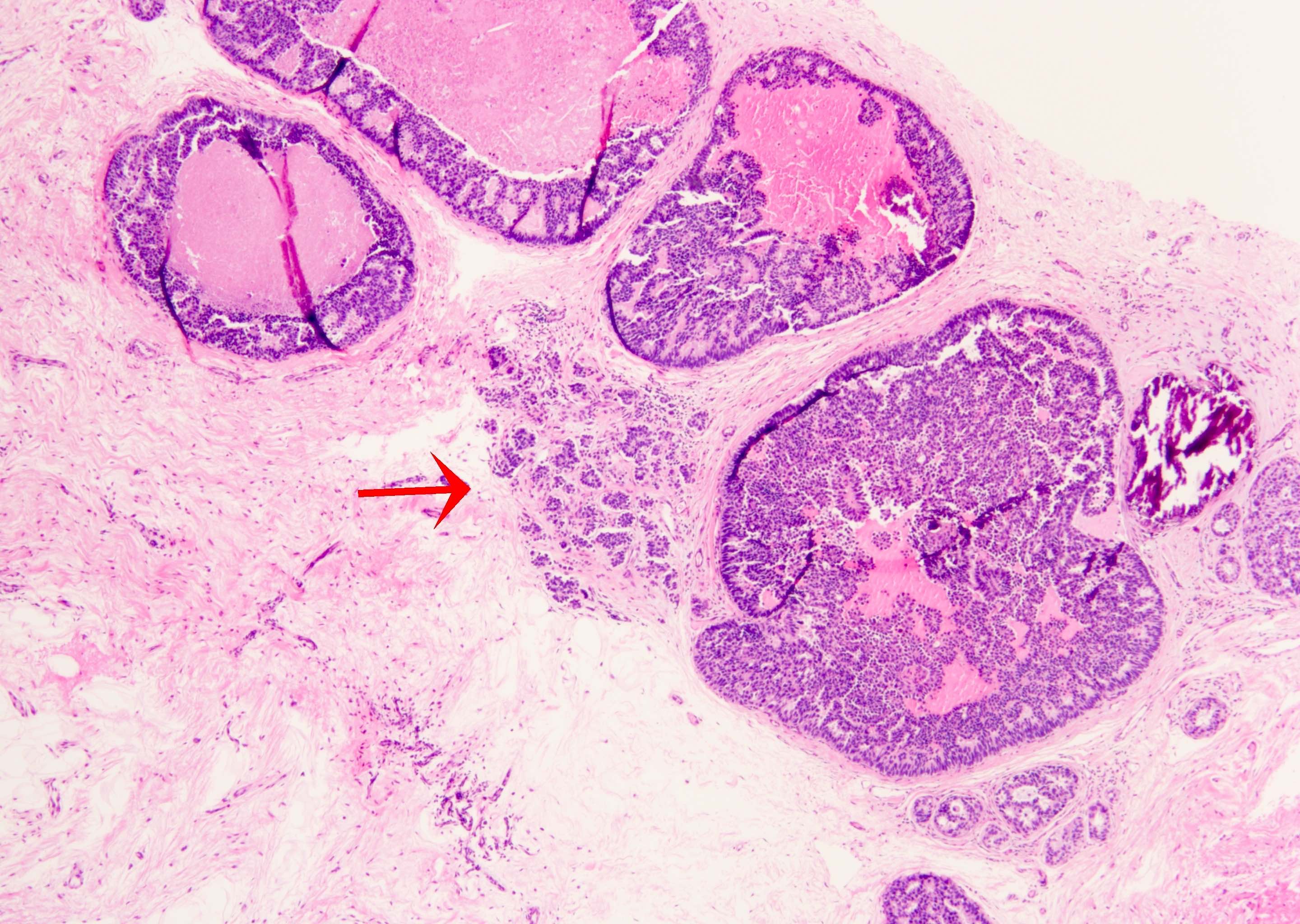
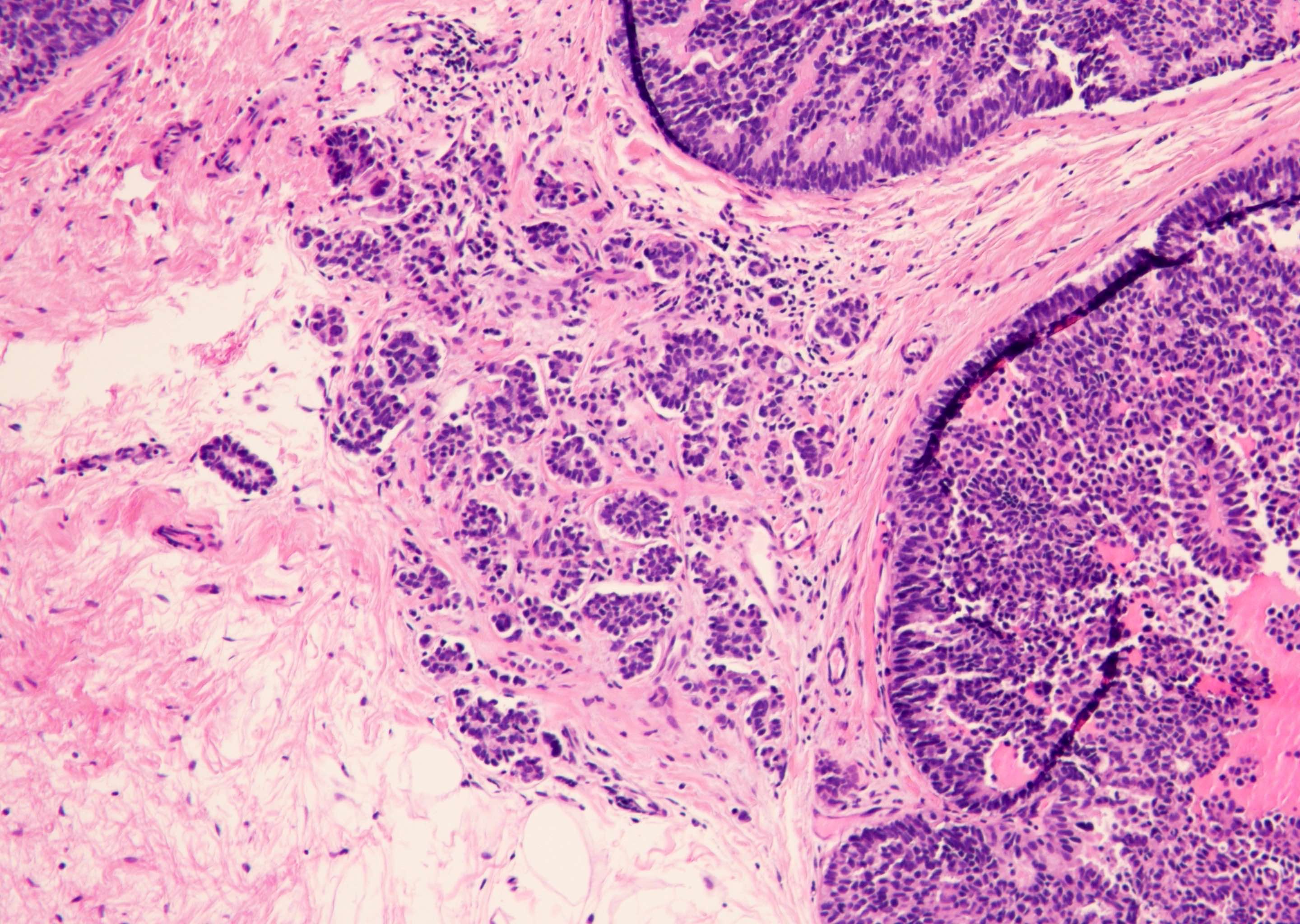
Microscopic (histologic) description
- Tumor cells in stroma measuring ≤ 1 mm
- Usually directly adjacent to DCIS, rare cases are associated with LCIS (J Breast Cancer 2018;21:197)
- Tumor cells must not appear to be attached to an adjacent focus of DCIS
- Associated DCIS usually has high grade nuclei, rarely low grade
- Multiple foci may be present; it is still considered microinvasive carcinoma as long as all foci are ≤ 1 mm in size
- Foci should not be added together to determine size
- Often associated with periductal fibrosis and dense lymphocytic infiltrate
- No myoepithelial cells are present
- Invasion into dermis can occur from DCIS involving nipple skin (Paget disease) (Breast Cancer (Auckl) 2020;14:1178223420948482)
Microscopic (histologic) images
Positive stains
- Keratin stains to highlight the microinvasive carcinoma (particularly helpful if the microinvasive carcinoma is associated with a dense inflammatory response)
- E-cadherin to identify ductal carcinoma
- Typically shows the identical ER, PR and HER2 expression to adjacent in situ carcinoma
- References: World J Clin Oncol 2014;5:382, Mod Pathol 2021;34:62
Negative stains
- Myoepithelial immunostains (p63, SMMS, calponin, etc.); a panel is recommended as DCIS can lose expression of 1 or more markers, muscle markers can also stain myofibroblasts and vessels and p63 is more specific but can be positive in carcinoma cells and in some cases of high grade DCIS
- Lack of E-cadherin expression to identify lobular carcinoma
- References: World J Clin Oncol 2014;5:382, Mod Pathol 2021;34:62
Molecular / cytogenetics description
- Microinvasive carcinoma can be of any molecular subtype (luminal A-like, luminal B-like, HER2 overexpressing or basal / triple negative category)
Sample pathology report
- Breast, left, 5 o'clock, stereotactic core biopsy with calcifications:
- Focus of microinvasive carcinoma in a background of ductal carcinoma in situ (see comment)
- The ductal carcinoma in situ is high grade with cribriform and papillary patterns, as well as associated comedonecrosis and calcifications.
- Comment: The presence of microinvasive carcinoma is confirmed with myoepithelial stains (p63 and SMMS), which are negative in the area of microinvasion.
Differential diagnosis
- Small invasive carcinoma:
- Foci of invasion measuring > 1 mm
- Classified as invasive breast cancer (T1a)
- Size of the focus should not be rounded down to 1 mm; a 1.1 mm focus should be considered T1a
- DCIS with cancerization of lobules:
- DCIS involving small acinar spaces in lobules
- Myoepithelial immunostains should be positive around involved acini
Additional references
Board review style question #1
How do you differentiate ductal carcinoma in situ (DCIS) with cancerization of lobules from microinvasive breast carcinoma?
- Stain with ER
- Stain with HER2
- Stain with p63
- Stain with PR
Board review style answer #1
C. Stain with p63. p63 will stain positive for DCIS with cancerization of the lobules, while microinvasive breast cancer will have a negative stain since there are no myoepithelial cells surrounding the carcinoma. A keratin stain such as AE1 / AE3 can be helpful in highlighting the microinvasive carcinoma cells. A panel of myoepithelial immunostains is recommended. Answers A, B and D are incorrect because these can stain positive or negative for both and will not differentiate them.
Comment Here
Reference: Microinvasive carcinoma
Comment Here
Reference: Microinvasive carcinoma
Board review style question #2
You encounter a case of microinvasive carcinoma and you see there are multiple foci. If you see this, how do you approach it?
- Add them together and give the aggregate measurement as overall tumor size
- Do not add them and still report as microinvasive carcinoma if all sizes are ≤ 1 mm
- If one of the foci measures 1.1 mm, it can be rounded down to 1 mm and included as microinvasive carcinoma
- Include the total area spanned by the microinvasive foci including uninvolved intervening tissue in the overall tumor size
Board review style answer #2
B. Do not add them and still report as microinvasive carcinoma if all sizes are ≤ 1 mm. Multiple foci may be present; it is still considered microinvasive carcinoma as long as all foci are ≤ 1 mm in size (the foci should not be added together to determine size). Answer A is incorrect because this will lead to an incorrect size for staging if a measurement of > 1 mm is calculated. Answer D is incorrect because only the sizes of the individual foci should be used for staging and the intervening tissue should not be included. Answer C is incorrect because any focus measuring > 1 mm in greatest dimension no longer meets the criteria for classification as microinvasive carcinoma and measurements > 1 mm cannot be rounded down to be included as microinvasive carcinoma.
Comment Here
Reference: Microinvasive carcinoma
Comment Here
Reference: Microinvasive carcinoma