Table of Contents
Leiomyosarcoma | Low grade myofibroblastic sarcoma | Osteosarcoma | Rhabdomyosarcoma | Stromal sarcoma | Undifferentiated pleomorphic sarcomaCite this page: Reisenbichler ES. Other sarcomas. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/breastmalignantRMS.html. Accessed April 2nd, 2025.
Leiomyosarcoma
Definition / general
Essential features
Etiology
Clinical features
Radiology description
Prognostic factors
Case reports
Treatment
Gross images
Images hosted on other servers:
Microscopic (histologic) description
Microscopic (histologic) images
Contributed by Emily S. Reisenbichler, M.D., Mark R. Wick, M.D. and AFIP
Cytology description
Cytology images
Images hosted on other servers:
Positive stains
Negative stains
Molecular / cytogenetics description
Differential diagnosis
- Malignant smooth muscle neoplasm of the breast
Essential features
- Rare, < 1% of all breast malignancies
- < 50 primary leiomyosarcomas of the breast reported in the literature
- Should be distinguished from metastatic tumor
Etiology
- Primary tumors likely arise from smooth muscle of the nipple or vascular wall
- Have been reported to occur secondary to radiation (Surg Case Rep 2015;1:76)
Clinical features
- Occur most frequently in the fourth and seventh decades of life, typically in postmenopausal women (Case Rep Pathol 2012;2012:491984)
- Average size of 5 cm
Radiology description
- Mammographically presents as a mass or architectural distortion
- By ultrasound, lesions are homogenously hypoechoic, lobular or oval with microlobulated or indistinct margins (Acta Radiol 2011;52:597)
Prognostic factors
- Type of surgery does not affect prognosis as long as the tumor is excised with an adequate (2 - 3 cm) margin (Breast 2011;20:389)
- Due to the rare nature of this tumor, no specific prognostic features are established in primary leiomyosarcoma arising in the breast
- If the tumor is cutaneous and limited to the dermis of the breast skin (i.e., atypical intradermal smooth muscle neoplasm), rather than arising in the mammary parenchyma, prognosis is excellent without metastases
Case reports
- 18 year old woman with leiomyosarcoma invading the breast skin (Breast 2011;20:389)
- 19 year old woman with primary leiomyosarcoma clicinally suspected to be fibroadenoma (Case Rep Pathol 2012;2012:491984)
- 51 year old woman with primary breast leiomyosarcoma located in the premammary zone / subcutaneous fat (Clin Imaging 2015;39:1105)
- 59 year old woman with leiomyosarcoma arising in irradiated region after breast conserving surgery (Surg Case Rep 2015;1:76)
Treatment
- As no axillary lymph node metastases have been reported with primary breast leiomyosarcoma, sentinel lymph node excision is not indicated (Breast 2011;20:389)
- Wide excision with at least 2 cm margin but 3 cm margin is recommended (Breast 2011;20:389)
- In tumors > 3 cm or with inadequate excision, radiotherapy may be indicated
- Adjuvant chemotherapy may result in greater clinical response in radiation induced sarcomas (Surg Case Rep 2015;1:76)
Gross images
Images hosted on other servers:
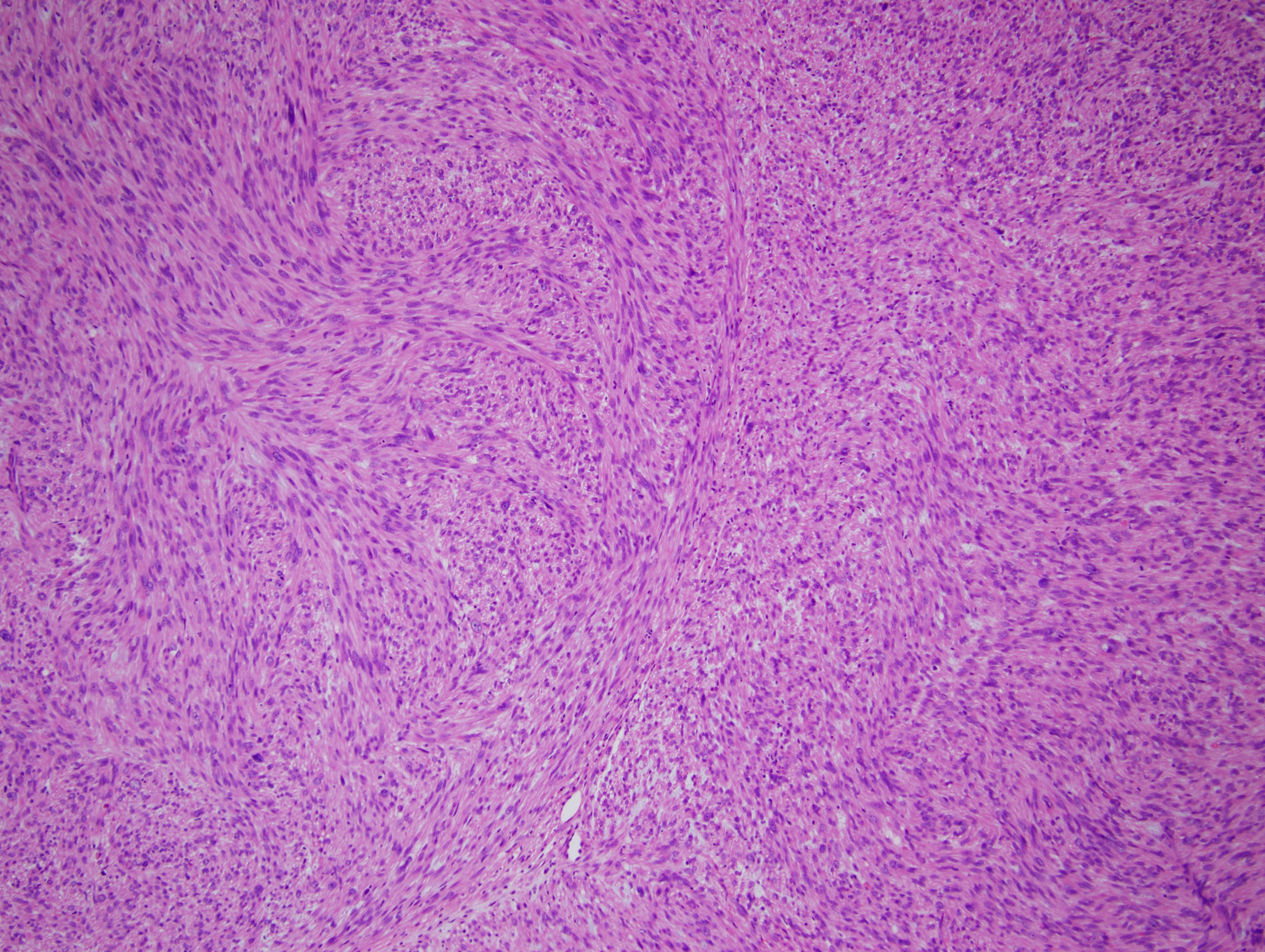
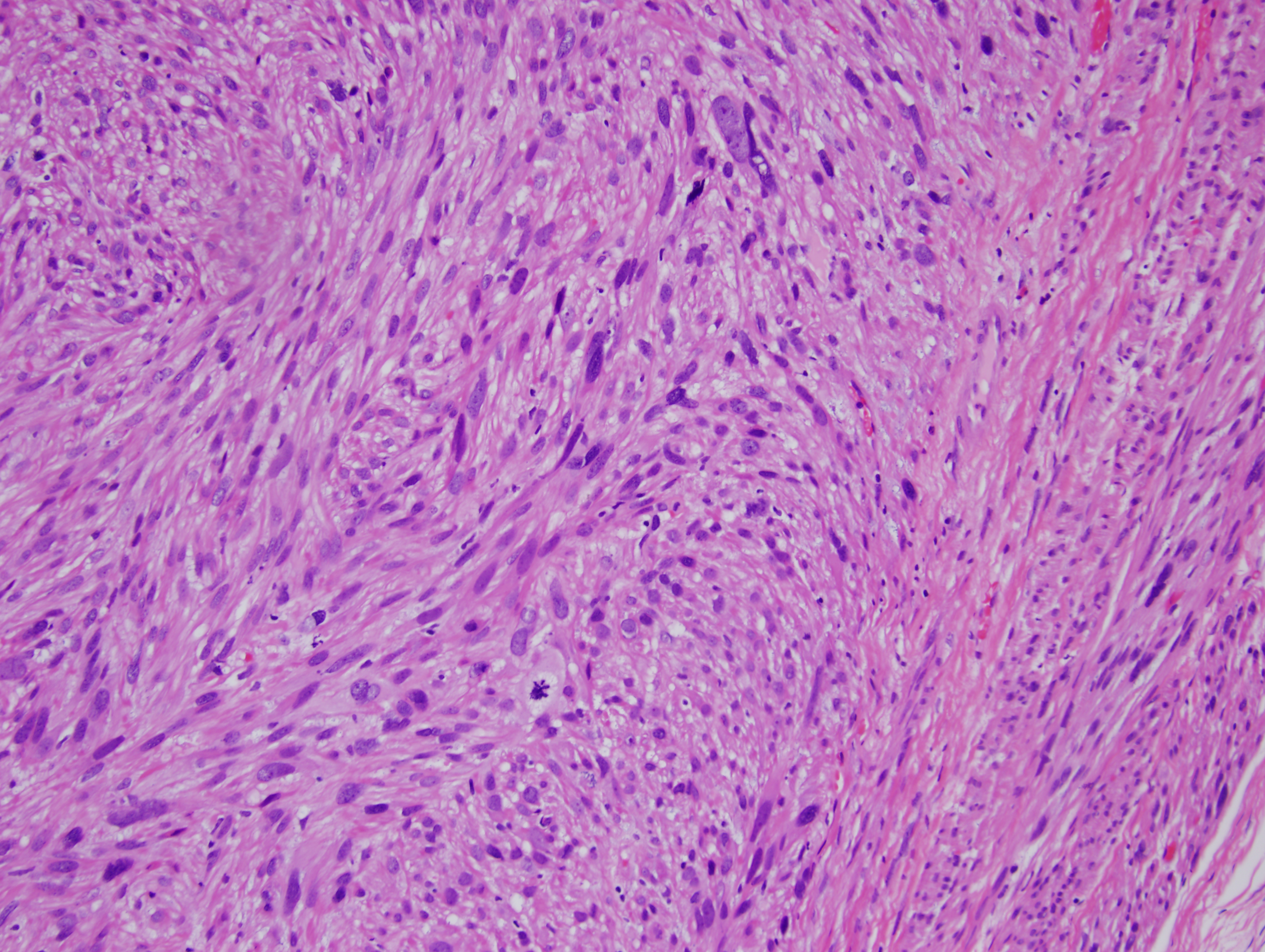
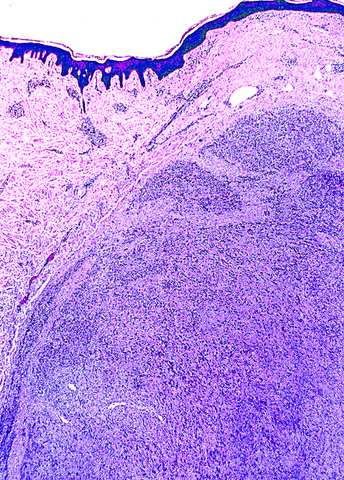
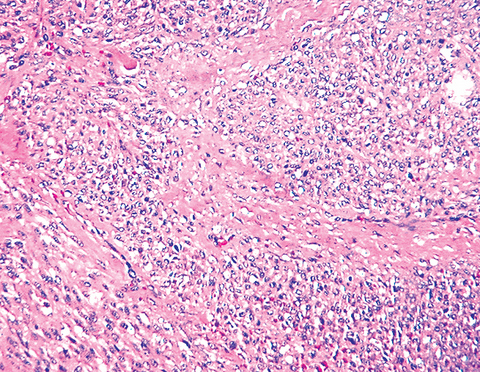
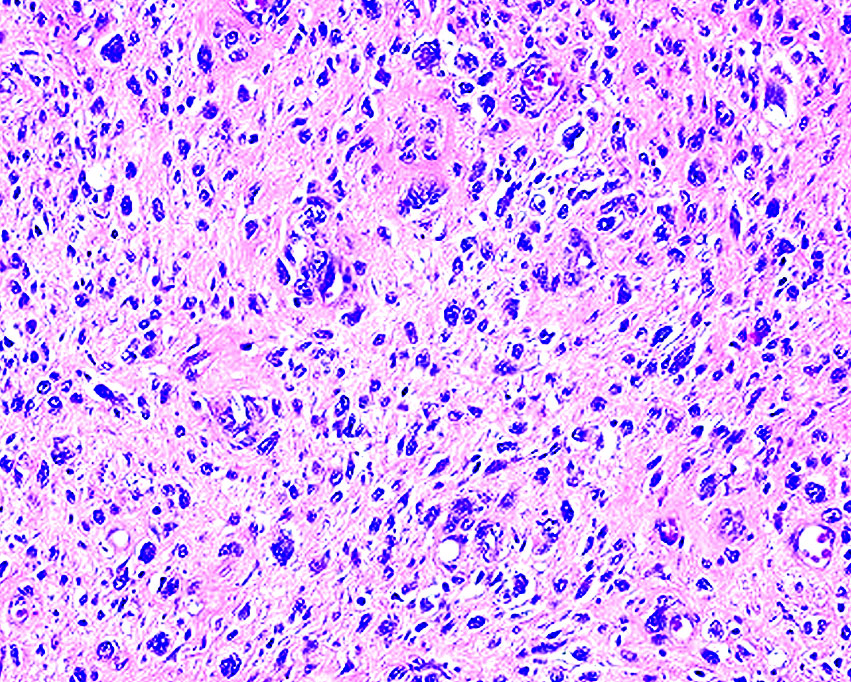
Microscopic (histologic) description
- Intersecting fascicle of spindled cells with abundant eosinophilic cytoplasm and cigar shaped nuclei demonstrating variable pleomorphism, mitotic activity and necrosis
- Tumor borders are typically infiltrative
Microscopic (histologic) images
Contributed by Emily S. Reisenbichler, M.D., Mark R. Wick, M.D. and AFIP
Cytology description
- Large, dissociated round to spindle cells, medium to large, with abundant vacuolated cytoplasm with occasional intranuclear cytoplasmic invaginations
- Mitotic activity, including abnormal forms, nuclear atypia and a necrotic background favor a malignant process
- Immunohistochemistry is typically required to distinguish leiomyosarcoma from other malignant spindle cell tumors of the breast (Diagn Pathol 2006;1:13)
Cytology images
Images hosted on other servers:
Positive stains
Negative stains
Molecular / cytogenetics description
- Loses of 16q and 1p (Oncogene 2010;29:845)
Differential diagnosis
- Leiomyosarcomatous differentiation in a malignant phyllodes tumor
- Metaplastic (spindle cell) carcinoma
- Myofibroblastoma
Low grade myofibroblastic sarcoma
Definition / general
Essential features
Prognostic factors
Case reports
Treatment
Gross description
Microscopic (histologic) description
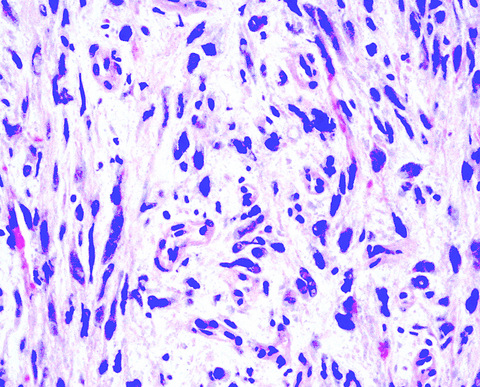
Microscopic (histologic) images
Contributed by Mark R. Wick, M.D.
Positive stains
Negative stains
Electron microscopy description
Molecular / cytogenetics description
Differential diagnosis
- Spindle cell sarcoma with myofibroblastic differentiation
- Also called myofibrosarcoma
Essential features
- Uncommon tumor overall, occurring predominantly in the head and neck or extremities with only rare reports within the breast
- At least moderate cytologic atypia must be seen focally
- Not part of WHO breast classification
Prognostic factors
- Frequently recurs, particularly when incompletely excised
- Low rates of metastasis but lung is most common site when it occurs (Am J Surg Pathol 2001;25:219)
Case reports
- 46 year old woman with palpable low grade myofibroblastic sarcoma (J Clin Oncol 2005;23:6249)
- 55 year old woman with diffuse pleuropulmonary metastases (Am J Surg Pathol 1997;21:489)
- 61 year old woman with low grade myofibroblastic sarcoma arising in a fibroadenoma (Diagn Pathol 2016;11:33)
- 81 year old woman with myofibrosarcoma (Breast J 2011;17:300)
Treatment
- Complete local excision with negative margins
- Radiation has been used but its effectiveness is unclear (Laryngoscope 2016 Jul 5 [Epub ahead of print])
Gross description
- Well circumscribed tumor with firm, pale cut surface, despite infiltrative microscopic growth
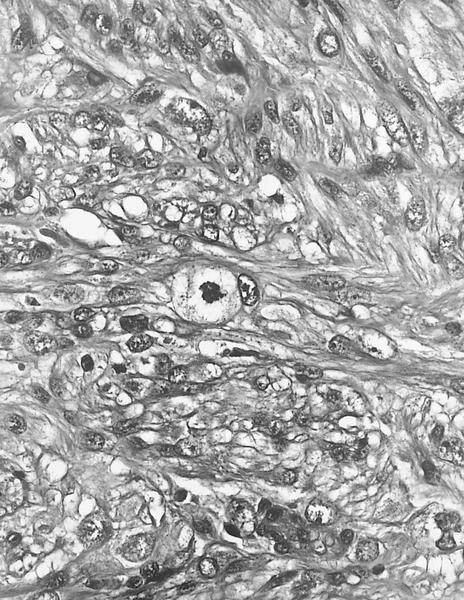
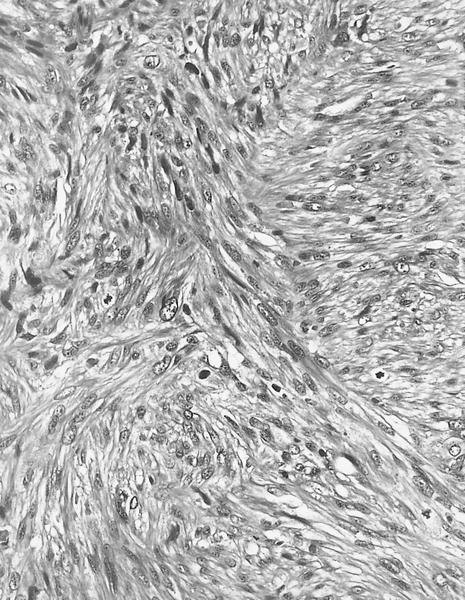
Microscopic (histologic) description
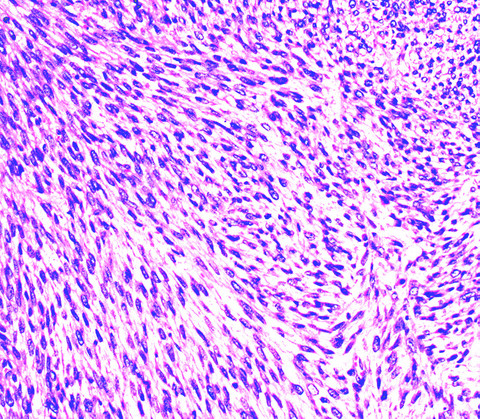
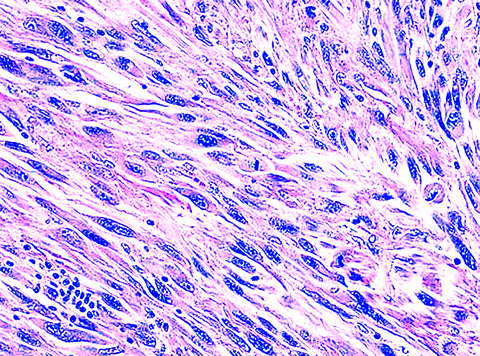
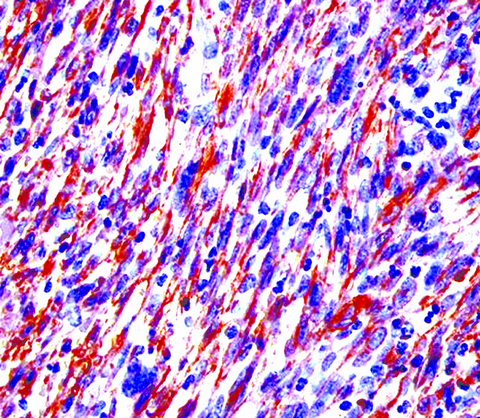
- Spindle cells in a fascicular or storiform growth pattern
- Variable stromal collagen
- Cells demonstrate pale eosinophilic cytoplasm and the nuclei must show at least moderate atypia focally and hyperchromasia
- Diffusely infiltrative borders
Microscopic (histologic) images
Contributed by Mark R. Wick, M.D.
Positive stains
Negative stains
- S100, keratins, EMA, CD34 (focal staining has been reported), h-caldesmon, nuclear beta-catenin
Electron microscopy description
- Prominent rough endoplasmic reticulum, peripheral myofilaments and the fibronectin fibrils of the fibronexus junctions (J Clin Pathol 2009;62:236)
Molecular / cytogenetics description
- Gains at 1p11 → p36.3 (66%), 12p12.2 → p13.2 (45%), 5p13.2 → p15.3 (31%), +22 (28%), loss at 15q25 → q26.2 (24%) (Am J Clin Pathol 2009;131:701)
- Complex DNA copy number changes
- Higher average number of chromosomal aberrations than seen in nodular fasciitis
Differential diagnosis
- Desmoid fibromatosis:
- Long sweeping fascicles with stromal collagen deposition
- Lacks cytologic atypia
- Inflammatory myofibroblastic tumor:
- Variably cellular fascicles
- Background lymphoplasmacytic infiltrate
- Lacks cytologic atypia
- ALK positive in ~50%
- Leiomyosarcoma:
- Shorter fascicles, lacks stromal collagen, h-caldesmon positive
- Myofibroblastoma:
- Myofibromatosis:
- Lacks cytologic atypia
- Biphasic fascicular and pericytoma-like areas
- Nodular growth, protruding into vascular spaces
- Lacks cytologic atypia
- Nodular fasciitis:
- Lacks fascicular growth pattern and cytologic atypia
- Border is typically not infiltrative
- Usually small (< 3 cm)
- Solitary fibrous tumor:
- Spindle cells lacking a fascicular architecture (i.e., patternless pattern)
- Hemangiopericytoma-like vessels
- Spindle cell (metaplastic) carcinoma:
- At least focal keratin positivity
- Spindle cell rhabdomyosarcoma:
Osteosarcoma
Definition / general
Essential features
Etiology
Clinical features
Radiology description
Prognostic factors
Case reports
Treatment
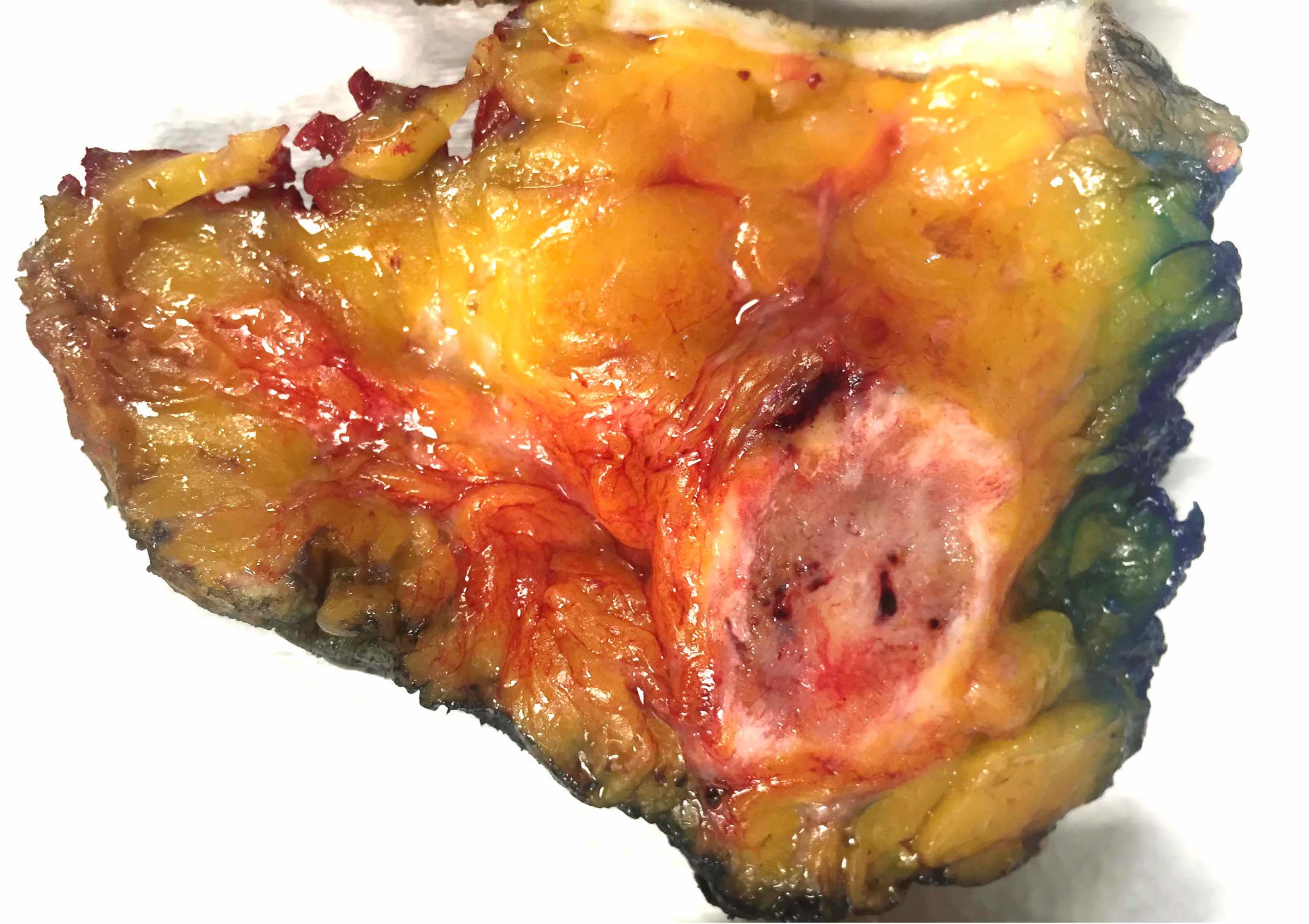
Gross description
Gross images
Contributed by Nitin Marwaha, M.D.
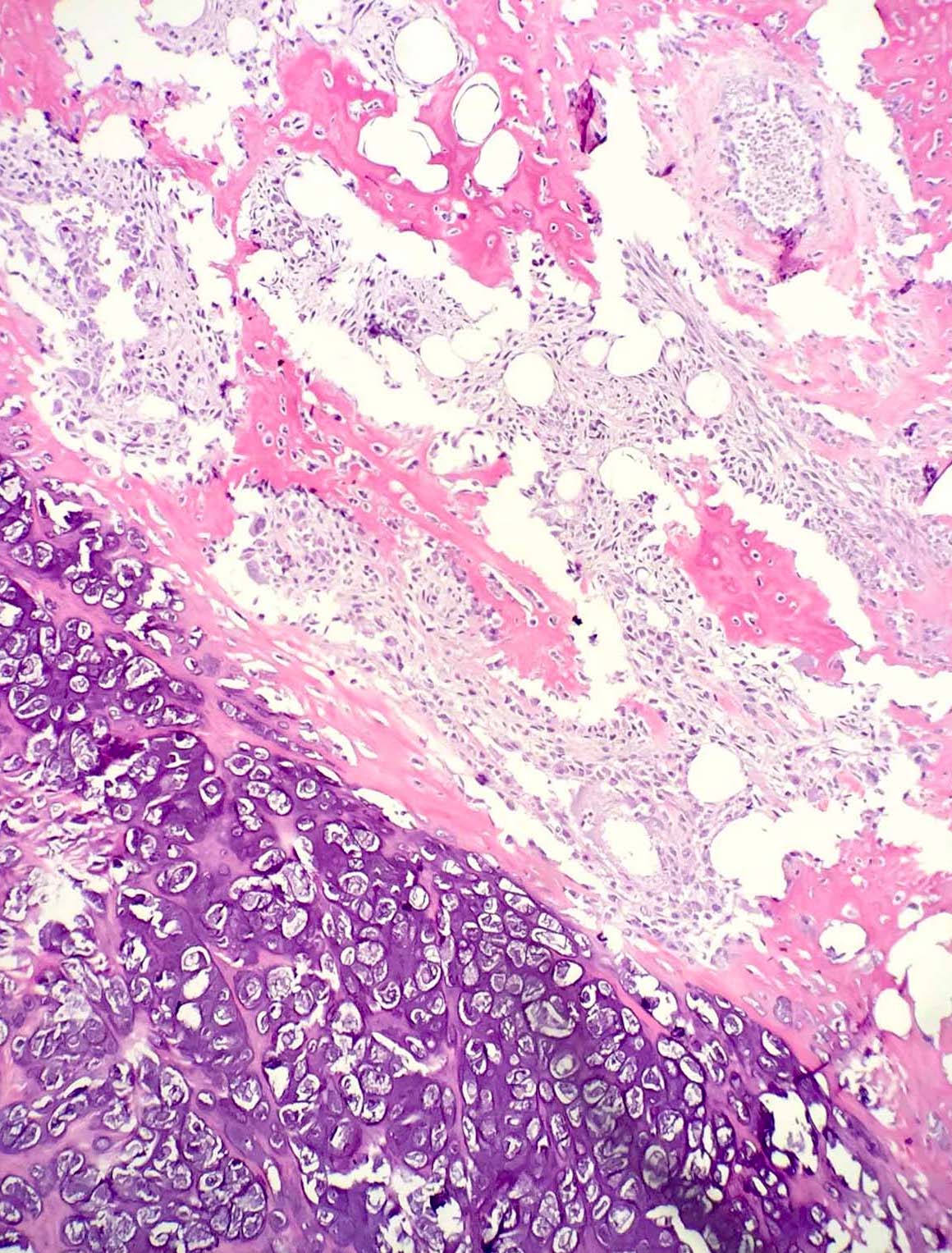
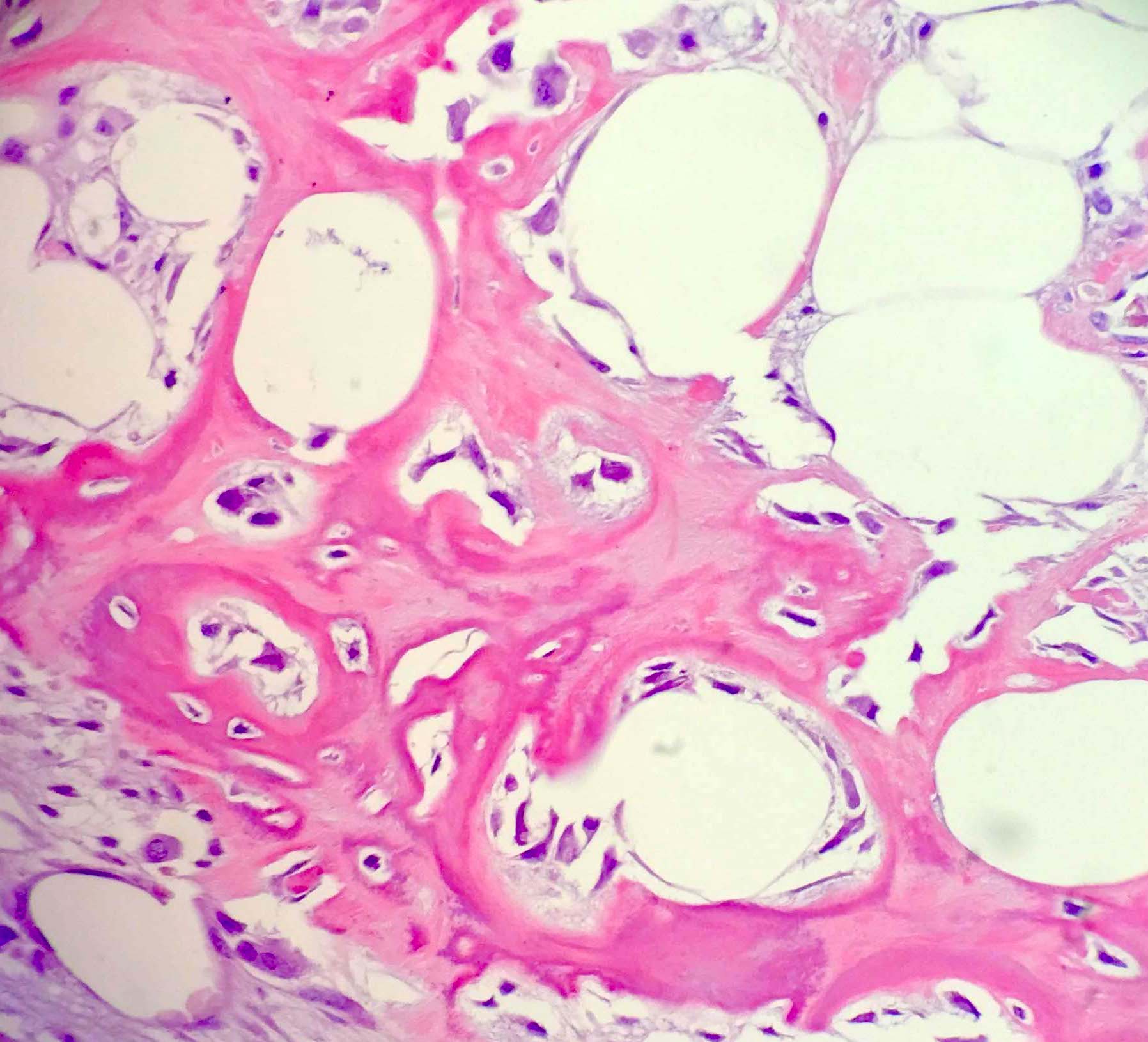
Microscopic (histologic) description
Microscopic (histologic) images
Contributed by Emily S. Reisenbichler, M.D. and Nitin Marwaha, M.D.
Positive stains
Negative stains
Differential diagnosis
- Malignant osteoid producing neoplasm
Essential features
- Exceedingly rare tumor in the breast with < 150 reported cases in the literature
- Comprised of cytologically malignant cells with osteoid production, lacking morphologic or immunohistochemical evidence of an epithelial / carcinomatous component
- Must extensively sample tumors to exclude diagnoses of malignant phyllodes with osteosarcomatous differentiation and metaplastic carcinoma with osteogenic matrix production
- Some experts believe that most, if not all, reported osteosarcomas of the breast actually represent matrix producing carcinomas (Breast 2013;22:13)
Etiology
- Has been reported to occur following radiation therapy (Case Rep Oncol 2013;6:367)
Clinical features
- Typically presents in the fifth or sixth decade of life
- Large, palpable mass
Radiology description
- Irregular hyperdense mass by mammography
- Hypoechoic mass by ultrasound
Prognostic factors
- Tumor size is the single most reliable prognostic factor in primary breast sarcomas (Br J Cancer 2004;91:237)
Case reports
- 63 year old woman with primary osteosarcoma of the breast 3 years following surgical excision of metaplastic ossification (J Med Case Rep 2016;10:231)
- 65 year old woman with osteosarcoma of the breast developing 1 year following the identification of a calcified fibroadenoma (Clin Case Rep 2015;4:62)
- 69 year old woman with a 10 cm primary osteosarcoma of the breast (Rev Assoc Med Bras (1992) 2015 ;61:497)
- 87 year old with breast osteosarcoma 29 years after radiation therapy for breast carcinoma (Case Rep Oncol 2013;6:367)
Treatment
- Complete resection with negative margins
- Routine axillary lymph node dissection not necessary due to tendency to metastasize to lungs rather than regional lymph nodes
- Utility of adjuvant radiation or chemotherapy is unclear due to rarity of this tumor type in this location
Gross description
- Well circumscribed large tumor with firm to gritty cut surface
- Difficulty in sectioning possible if abundant osteoid production present
Gross images
Contributed by Nitin Marwaha, M.D.
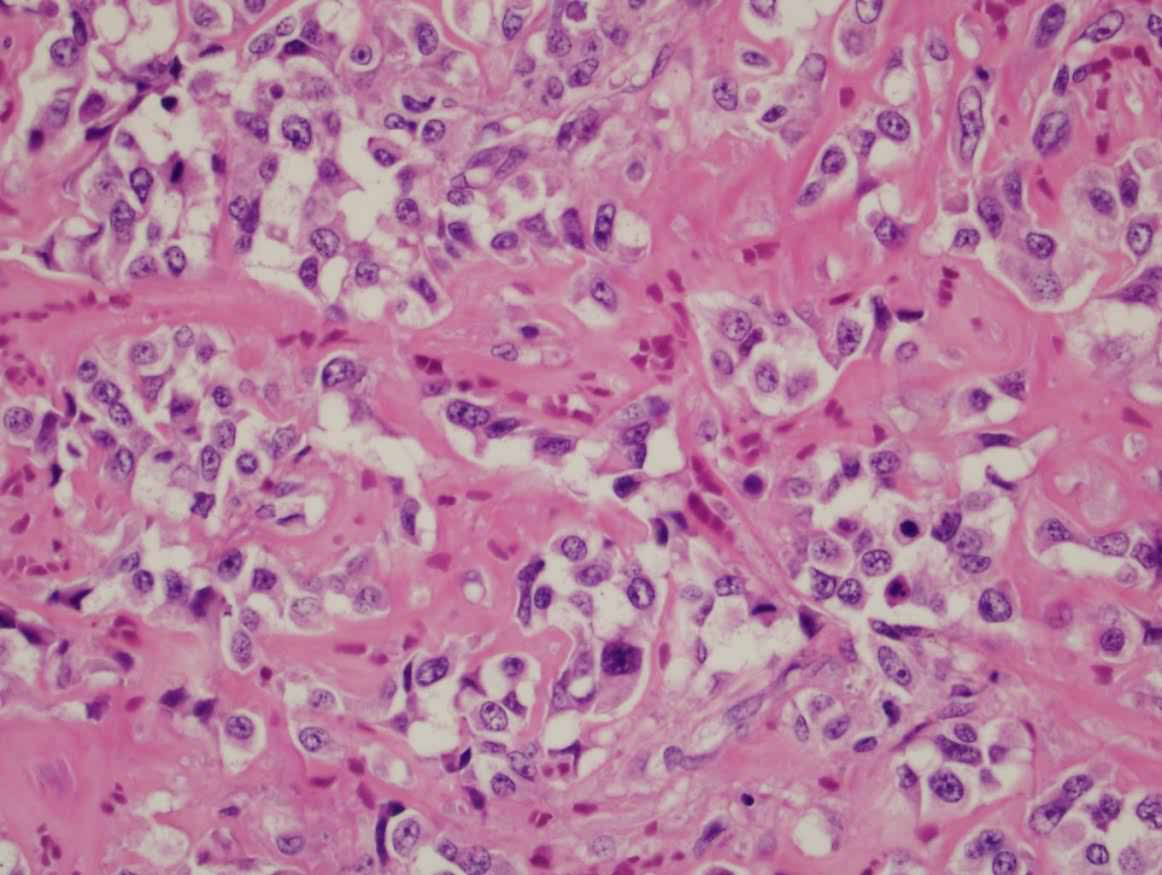
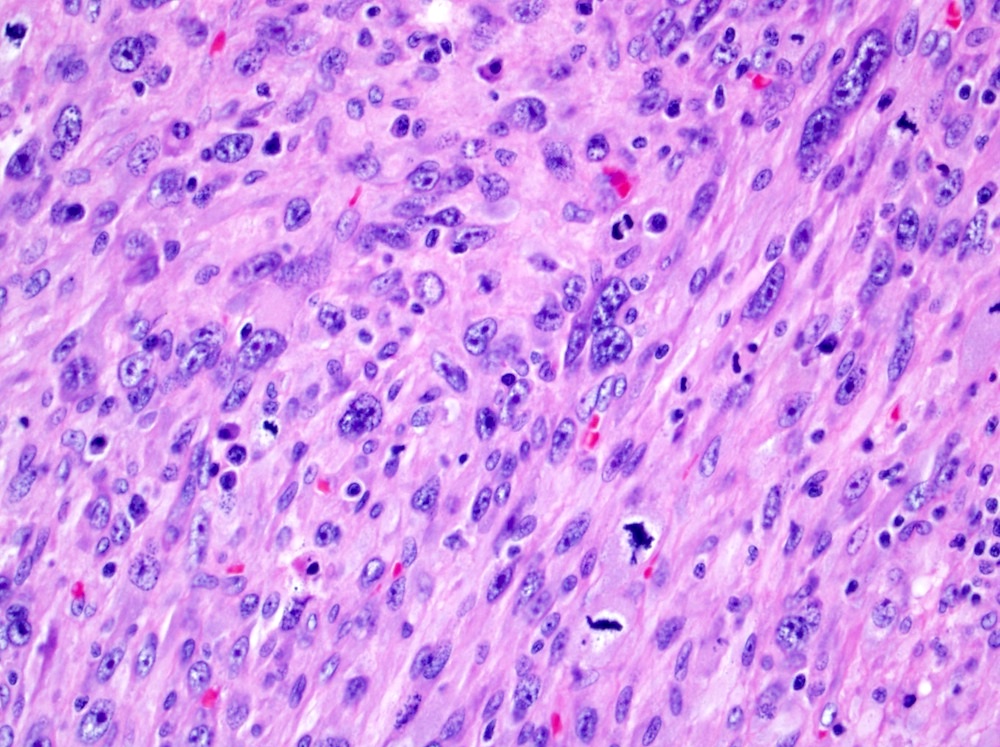
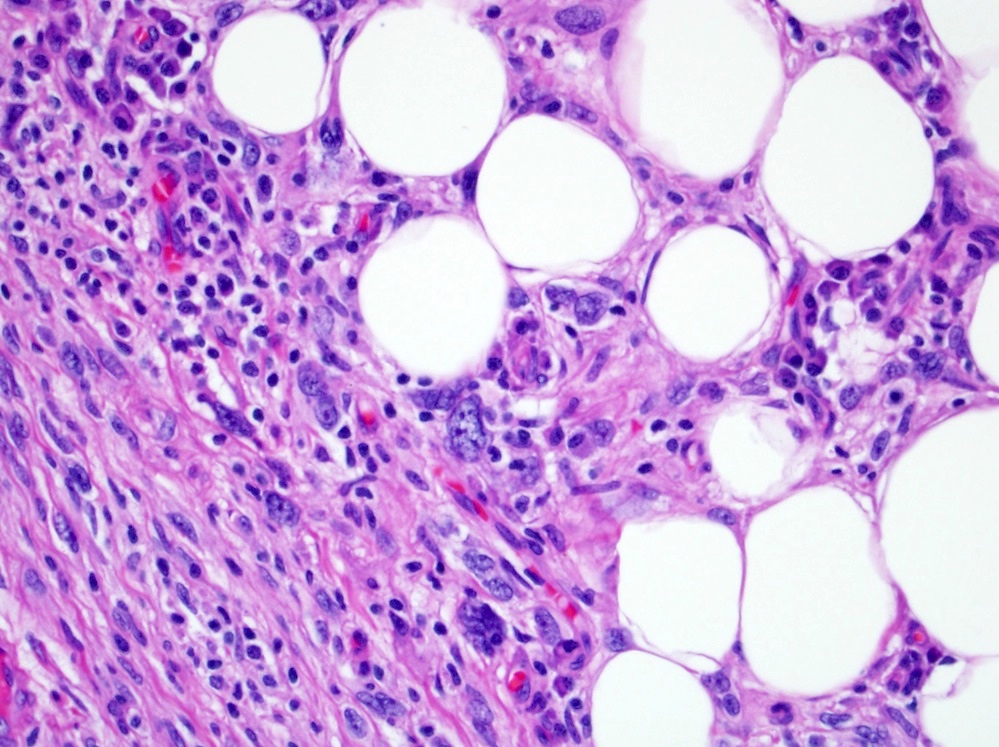
Microscopic (histologic) description
- Spindle to epithelioid cells with nuclear atypia, hyperchromasia and mitotic activity, including atypical forms
- Lace-like osteoid production
- Absence of an in situ carcinoma component
Microscopic (histologic) images
Contributed by Emily S. Reisenbichler, M.D. and Nitin Marwaha, M.D.
Positive stains
- SATB2: may also be focally positive in a subset of breast carcinomas (Adv Anat Pathol 2015;22:149)
Negative stains
- Cytokeratins (typically high molecular weight keratins such as CK5 / 6) and myoepithelial markers (such as p63): to rule out a metaplastic carcinoma
Differential diagnosis
- Metaplastic carcinoma:
- Presence of an epithelial / carcinomatous component, associated DCIS or demonstration of epithelial differentiation with immunohistochemistry (i.e., cytokeratins, myoepithelial markers, EMA)
- Malignant phyllodes with osteosarcomatous differentiation:
- Thorough sampling of the tumor reveals an epithelial component
- Benign heterotopic ossification / fasciitis ossificans:
- Mature lamellar bone formation lacking the zonation seen in myositis ossificans
- Intervening cells lack significant pleomorphism, hyperchromasia and mitotic activity
- Metastatic osteosarcoma:
- Clinical history of primary osteosarcoma elsewhere
Rhabdomyosarcoma
Definition / general
Essential features
Clinical features
Radiology description
Prognostic factors
Case reports
Treatment
Clinical images
Contributed by Mark R. Wick, M.D.
Gross description
Gross images
Images hosted on other servers:
Microscopic (histologic) description
Microscopic (histologic) images
Contributed by Mark R. Wick, M.D.
Cytology images
Contributed by Mark R. Wick, M.D.
Positive stains
Negative stains
Electron microscopy description
Molecular / cytogenetics description
Differential diagnosis
- Malignant neoplasm with skeletal muscle differentiation
Essential features
- Comprises < 3% of all adult primary soft tissue sarcomas and exceedingly rare as a primary breast tumor
- Primary rhabdomyosarcoma of the breast is most commonly alveolar subtype and is seen more frequently in the pediatric / adolescent population (Med Pediatr Oncol 1997;29:181)
- Typically composed of small, round to spindled cells, with eosinophilic cytoplasm, some of which show cytoplasmic cross striations (embryonal and alveolar subtypes); larger cells with greater degree of atypia seen in pleomorphic subtype
- Must exclude other tumor types with heterologous rhabdomyosarcomatous differentiation (such as malignant phyllodes)
Clinical features
- Primary rhabdomyosarcoma of the breast is seen most frequently in the pediatric / adolescent population and therefore is not typically identified by routine screening mammography
- Presents as a palpable, circumscribed, rapidly growing mass
- Presentation as a metastasis from a primary rhabdomyosarcoma elsewhere in the body occurs in 3 - 6% cases and portends a very poor prognosis (J Pediatr Hematol Oncol 2017;39:62)
Radiology description
- Due to the breast density of the pediatric and adolescent population, ultrasound is the imaging modality of choice for radiographic characterization of this tumor type (Eur J Radiol 2003;48:282)
- Hypoechoic, round or lobulated nodule / mass by ultrasound
Prognostic factors
- Patients with primary breast alveolar rhabdomyosarcoma have a poor prognosis, frequently dying of disease with disseminated metastases (J Pediatr Hematol Oncol 2017;39:62)
- Embryonal subtype portends much better prognosis than alveolar or pleomorphic subtypes
Case reports
- 13 year old girl with primary alveolar rhabdomyosarcoma of the breast (Surg Today 2007;37:38)
- 19 year old woman with primary mammary rhabdomyosarcoma (Indian J Cancer 2015;52:295)
- 49 year old woman with primary pleomorphic rhabdomyosarcoma of the breast (J Res Med Sci 2014;19:1200)
Treatment
- As with all primary breast sarcomas, wide excision without axillary dissection is the mainstay of treatment
- Adjuvant or neoadjuvant radiation often used in large or incompletely resected tumors
- Utility of chemotherapy is unclear due to the rarity of this tumor type
Clinical images
Contributed by Mark R. Wick, M.D.
Gross description
- Circumscribed, nonencapusulated mass
Gross images
Images hosted on other servers:
Microscopic (histologic) description
- 3 microscopic subtypes:
- Alveolar: sheets of small, round cells clustered with variable amounts of fibrous septa; may contain scattered giant cells
- Embryonal: cytologically round to spindle cells with scant cytoplasm in a myxoid background; elongated cells with more abundant eosinophic cytoplasm referred to as strap cells or tadpole cells
- Pleomorphic: sheets of large cells demonstrating marked nuclear atypia or "anaplasia" with eosinophilic cytoplasm
Microscopic (histologic) images
Contributed by Mark R. Wick, M.D.
Cytology images
Contributed by Mark R. Wick, M.D.
Positive stains
- MyoD1 (nuclear)
- Myogenin (nuclear); stronger, diffuse staining seen in alveolar than in embryonal subtype
- Desmin
- Muscle specific actin
Negative stains
Electron microscopy description
- Skeletal differentiation, as evidenced by ultrastructural specific myofilament arrays, focal density, Z band material and pinocytotic vesicle, is suggestive of rhabdomyosarcomatous differentiation but is not specific for the diagnosis of rhabdomyosarcoma (J Pathol Transl Med 2015;49:93)
- Features may not be evident in solid variants of the alveolar subtype
Molecular / cytogenetics description
- Alveolar: t(2;13)(q35;q4), PAX3::FOXO1 fusion more frequent than t(1;13)(p36;q14), PAX7::POXO1 fusion
- Embryonal: chromosome loss, deletion or uniparental disomy resulting in loss of chromosome 11 loci
- Pleomorphic: complex karyotype
Differential diagnosis
- Ewing sarcoma:
- Heterologous rhabdomyosarcomatous differentiation in a malignant phyllodes tumor or in malignant peripheral nerve sheath tumor:
- Extensive sampling to find diagnostic features of these tumor types
- Invasive lobular carcinoma:
- Metastatic rhabdomyosarcoma:
- Clinical history of primary rhabdomyosarcoma elsewhere
Stromal sarcoma
Definition / general
Essential features
Clinical features
Prognostic factors
Case reports
Treatment
Clinical images
Contributed by Mark R. Wick, M.D.
Gross description
Microscopic (histologic) description
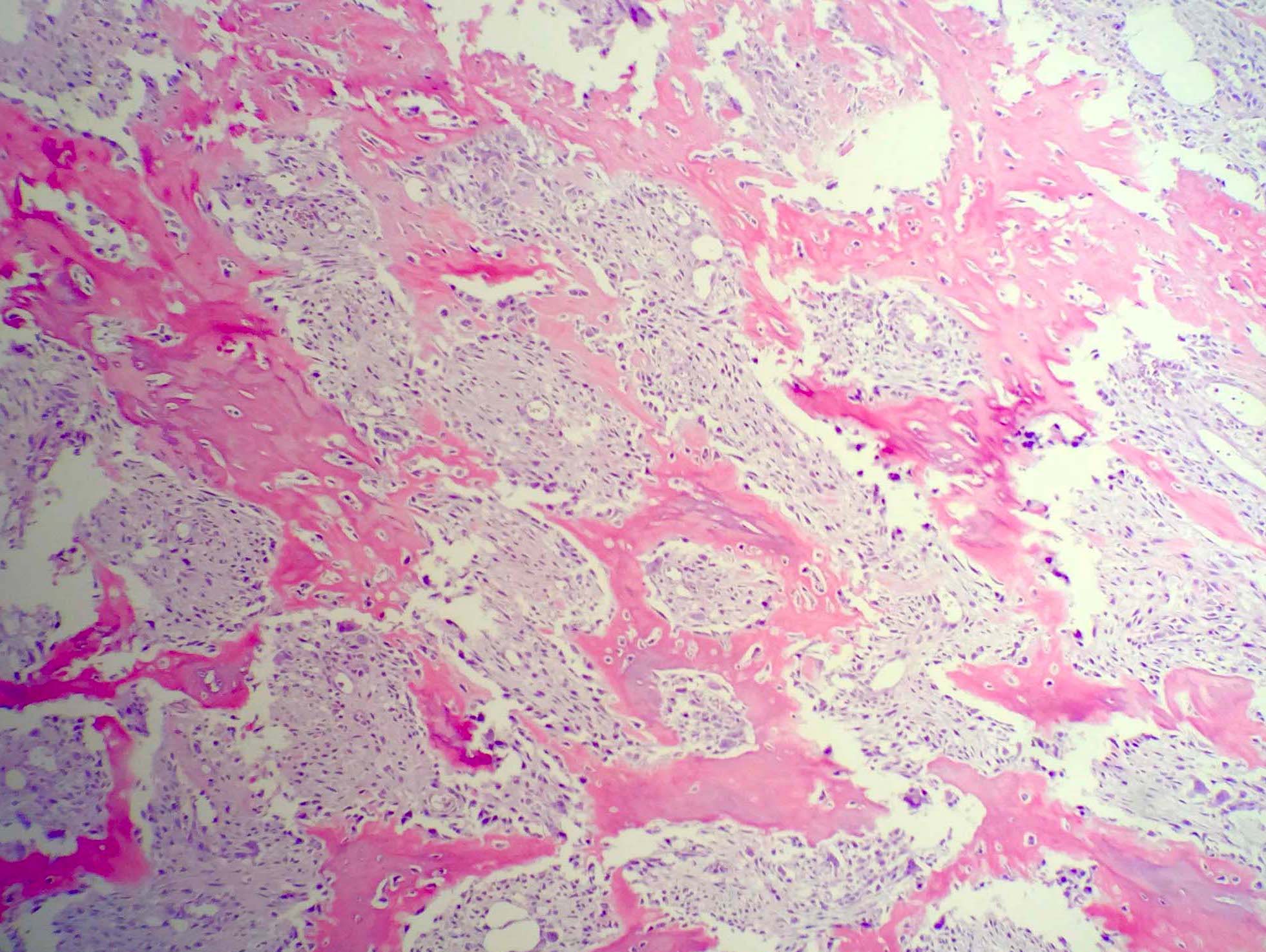
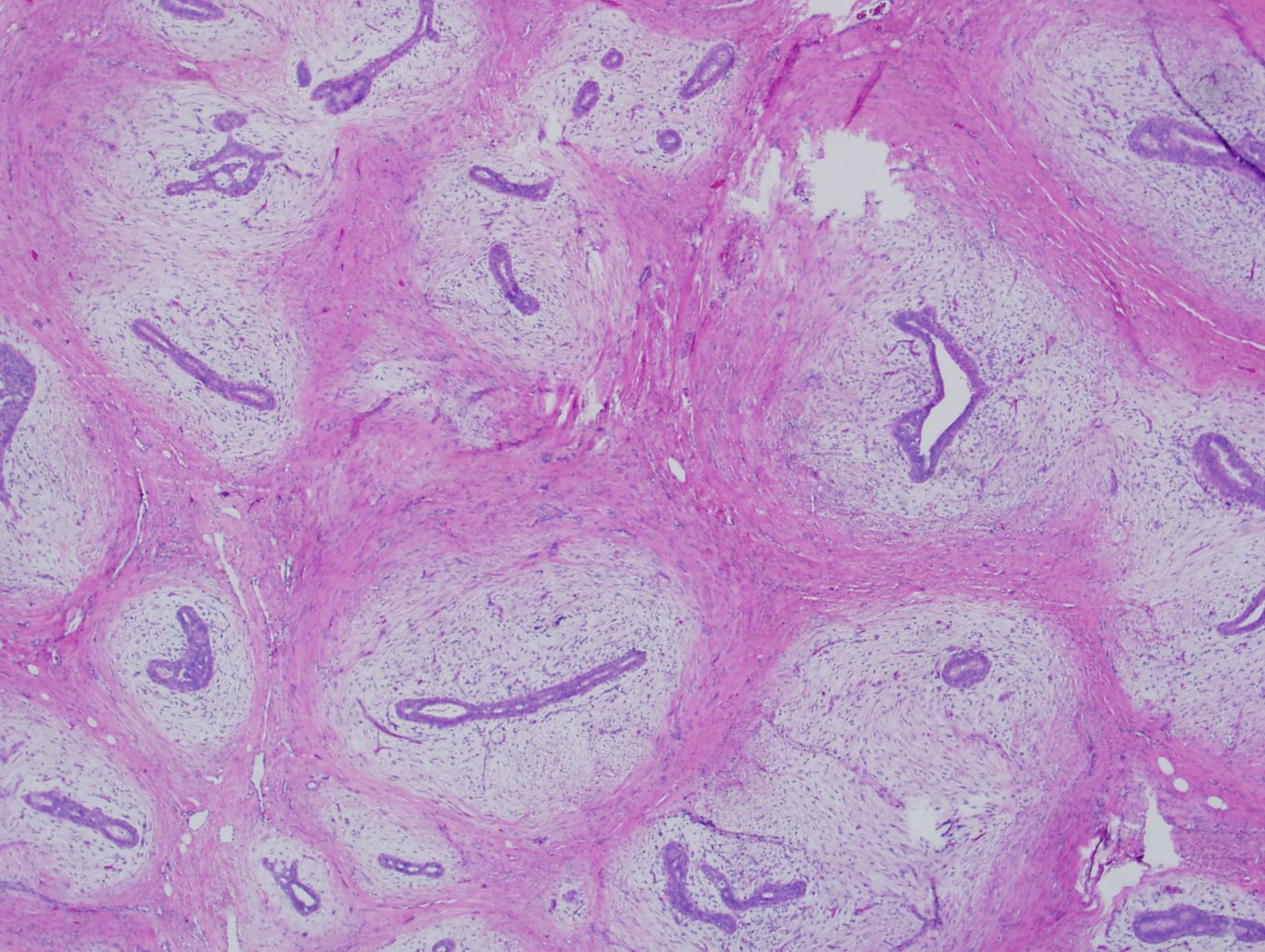
Microscopic (histologic) images
Contributed by Emily S. Reisenbichler, M.D. and Mark R. Wick, M.D.
Positive stains
Negative stains
Electron microscopy description
Differential diagnosis
- The 4th WHO edition (2012) reclassified this periductal stromal tumor as the preferred neutral term in the family of fibroepithelial tumor
- Stromal proliferation around open, benign tubules
Essential features
- Considered a type of fibroepithelial tumor lesion with stromal proliferation around benign tubules
- Lacks the defined tumor borders and compressed tubules of fibroadenoma and leaf-like architecture of phyllodes tumor
- Must demonstrate stromal atypia and mitotic activity to be considered a sarcoma
Clinical features
- Occurs in peri and postmenopausal women (median 55.3 years), ~10 years older than the median phyllodes presentation (Am J Surg Pathol 2003;27:343)
- Variable clinical presentation
Prognostic factors
- Good overall prognosis
- Low recurrence risk, ~10% (Am J Surg Pathol 2003;27:343)
Case reports
- 14 year old boy with periductal stromal sarcoma (J Med Case Rep 2011;5:249)
- 35 year old woman with periductal stromal sarcoma of the breast with liposarcomatous differentiation (Int J Surg Pathol 2015;23:221)
- 43 year old woman with periductal stroma sarcoma 5 months following excision of a phyllodes tumor (Oncol Lett 2014;8:1181)
- 45 year old woman with periductal stromal tumor and synchronous bilateral breast cancer (Anticancer Res 2014;34:3635)
- 52 year old woman with low grade periductal stromal sarcoma of the breast with myxoid features (Pathol Int 2009;59:588)
Treatment
- Given the likely relationship to fibroepithelial lesions, treatment is similar to that of phyllodes tumor
- Wide excision with negative margins
- As with primary breast sarcoma, assessment of axillary sentinel lymph nodes is not necessary
- Adjuvant chemotherapy and radiation are not typically warranted unless presenting with a higher grade sarcomatous component
Clinical images
Contributed by Mark R. Wick, M.D.
Gross description
- Ill defined nodular mass (mean 3 cm)
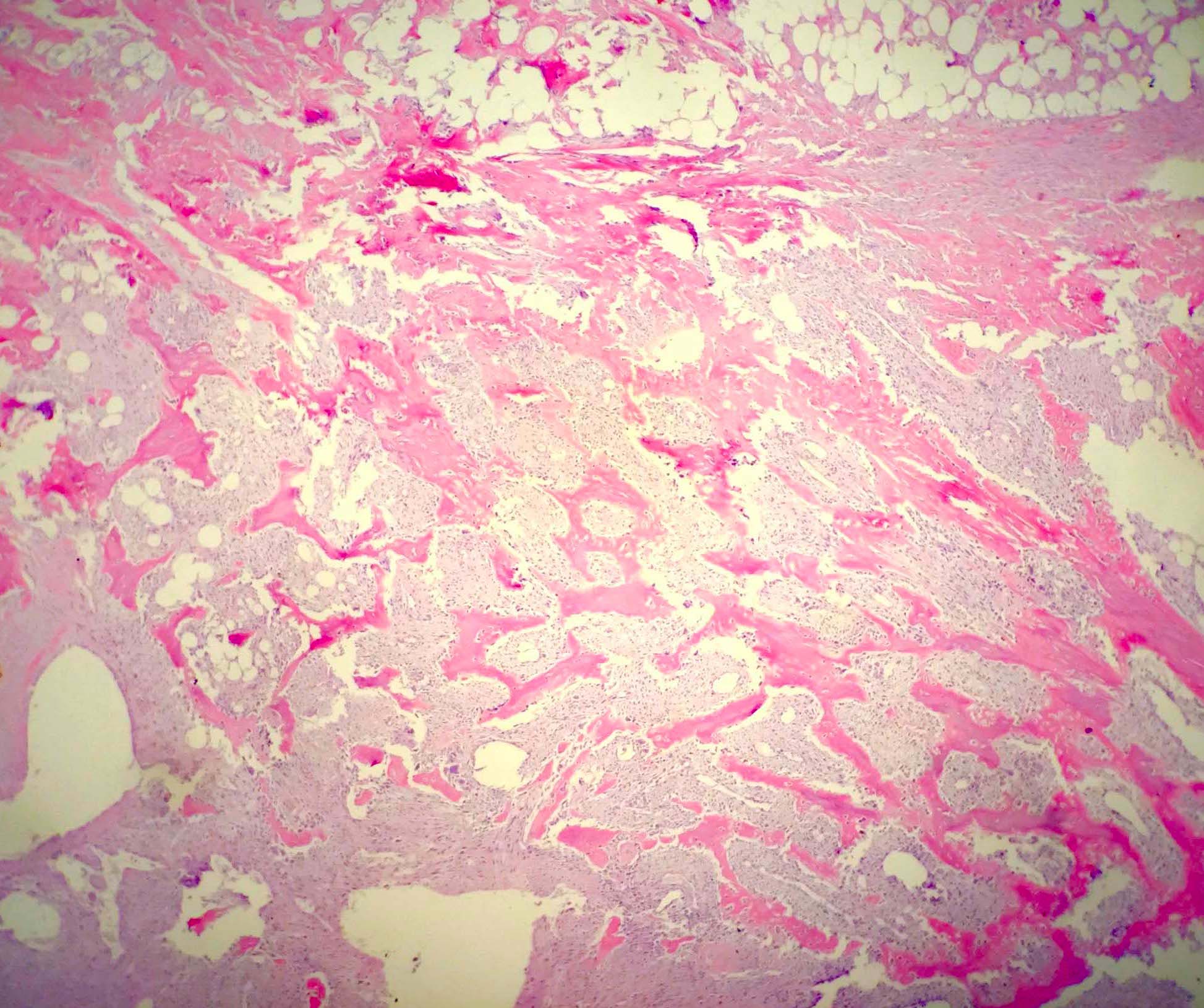
Microscopic (histologic) description
- Increased stromal cellularity of spindled stroma surrounding or cuffing benign ducts in a pericanalicular pattern
- Involved tubules and ducts are not malignant
- Stromal cells demonstrate at least moderate cytologic atypia and mitotic activity
- Infiltrative and often multinodular microscopic border
- May be seen with areas of angiosarcomatous or liposarcomatous components (Am J Surg Pathol 2003;27:343, Int J Surg Pathol 2015;23:221)
Microscopic (histologic) images
Contributed by Emily S. Reisenbichler, M.D. and Mark R. Wick, M.D.
Positive stains
Negative stains
Electron microscopy description
- Undifferentiated mesenchymal cell features such as free ribosomes and irregular profiles of rough endoplasmic reticulum
- Fibroblastic differentiation such as well organized dilated rough endoplasmic reticulum, Golgi complexes, cytoplasmic filaments and pericellular collagen (Cancer 1979;43:209)
Differential diagnosis
- Periductal stromal hyperplasia:
- Nodular growth, lacks the cytologic atypia and mitoses typical of a stromal sarcoma (0 - 2 mitoses per 10 high power fields)
- Phyllodes tumor:
- Has a more defined tumor border with compression and distortion of ductal elements causing a leaf-like architecture
- Abundant stromal overgrowth of intralobular stroma, not limited only to periductal areas
Undifferentiated pleomorphic sarcoma
Definition / general
Essential features
Etiology
Clinical features
Diagnosis
Radiology description
Prognostic factors
Case reports
Treatment
Clinical images
Images hosted on other servers:
Gross images
Images hosted on other servers:
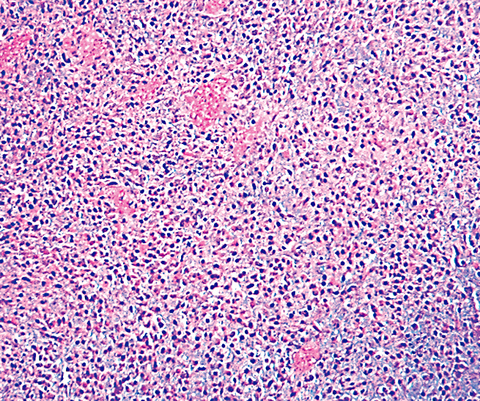
Microscopic (histologic) description
Microscopic (histologic) images
Contributed by Emily S. Reisenbichler, M.D. and Mark R. Wick M.D.
Cytology description
Positive stains
Negative stains
Molecular / cytogenetics description
Differential diagnosis
- See also Soft tissue topic
- A malignant tumor showing no line of differentiation
- Not part of the WHO classification of breast tumors
- Previously known as malignant fibrous histiocytoma (MFH)
Essential features
- High grade sarcoma with no distinctive microscopic, immunohistochemical or molecular features fitting any specific line of differentiation
- Diagnosis of exclusion
- Undifferentiated sarcomas account for ~20% of soft tissue sarcomas in other parts of the body but are exceedingly rare in the breast
Etiology
- May occur as a primary / de novo tumor or in the postradiation setting
Clinical features
- Most occur in fifth to sixth decade of life
- Majority present as rapidly enlarging palpable mass but can be incidental finding at screening
Diagnosis
- A limited core biopsy may underestimate tumor grade as grading systems such as the 3 tier French (FNCLCC) system are dependent on percentage necrosis and mitotic rate
Radiology description
- On mammography, appears as a noncalcified hyperdense mass (Expert Rev Anticancer Ther 2014;14:705)
- By MRI, shows irregular borders and marked inhomogeneous contrast enhancement (AJR Am J Roentgenol 2012;198:W386)
Prognostic factors
- Close / involved margins, large tumor size (> 5 cm) and high grade histology typically indicate a worse prognosis
Case reports
- 29 year old woman with UPS of the breast (World J Surg Oncol 2016;14:186)
- 50 year old man with giant cell variant of MFH of the breast (J Cancer Res Ther 2015;11:657)
- 50 year old woman with breast UPS containing osteoclast-like giant cells (World J Surg Oncol 2013;11:21)
- 72 year old woman with inflammatory MFH of the breast (Pathol Res Pract 2013;209:534)
Treatment
- Surgical resection with a negative margin (R0) is standard treatment
- Sentinel lymph node biopsy is not warranted
- Adjuvant radiation is often utilized in large tumors or following incomplete (R1 / R2) surgical resections
- Response to adjuvant chemotherapy is typically low but may be used in patients with large, unresectable or metastatic tumors
Clinical images
Images hosted on other servers:
Gross images
Images hosted on other servers:
Microscopic (histologic) description
- Cell morphology may be spindle, round / epithelioid or pleomorphic, demonstrating marked cytologic atypia
- Often high mitotic activity
- May be associated with multinucleated giant cells or an inflammatory background
Microscopic (histologic) images
Contributed by Emily S. Reisenbichler, M.D. and Mark R. Wick M.D.
Cytology description
- Single or clustered spindled cells with nuclear pleomorphism
- Absence of an epithelial component
Positive stains
- By definition, no staining to fit a specific line of differentiation
- May show focal staining with keratin, actin, desmin, EMA, CD99, CD34
Negative stains
- Typically negative for most markers
Molecular / cytogenetics description
- Complex karyotypes without specific recurrent aberrations
Differential diagnosis
- Dedifferentiated liposarcoma:
- MDM2 amplified
- Metaplastic (spindle cell) carcinoma:
- Should show at least some keratin or myoepithelial marker expression
- Metastatic sarcoma:
- Must be excluded clinically
- Sarcomatous differentiation in a malignant phyllodes tumor:
- Extensive sampling needed to identify an epithelial component