Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1Cite this page: Zhang H. Metaplastic. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/breastmalignantmetaplastic.html. Accessed April 1st, 2025.
Definition / general
- Heterogeneous group of invasive breast carcinomas characterized by differentiation of the neoplastic epithelium towards squamous cells or mesenchymal looking elements, including but not restricted to spindle, chondroid and osseous cells
Essential features
- Invasive breast carcinoma with atypical squamous, spindle cell or mesenchymal / matrix producing differentiation
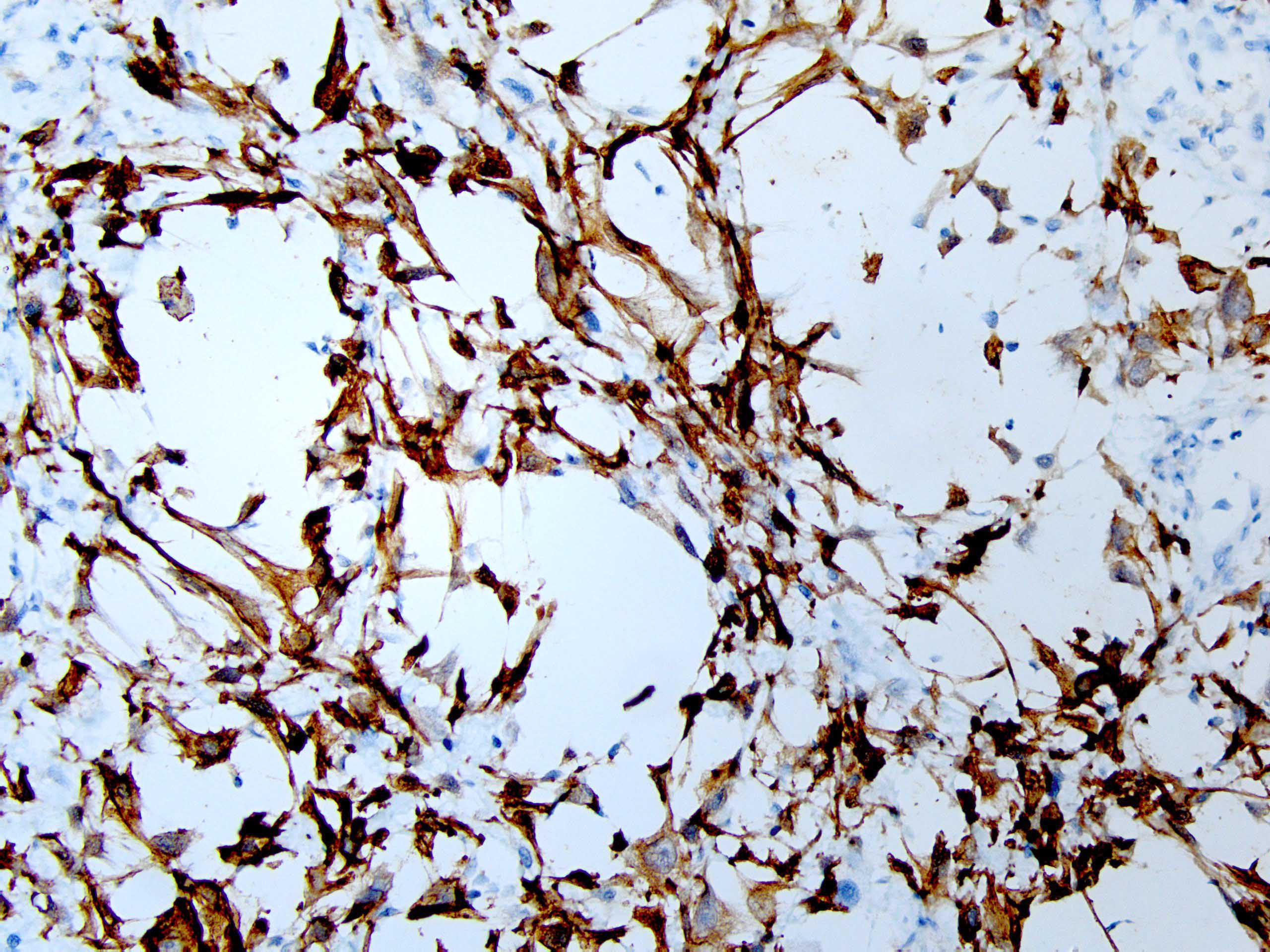
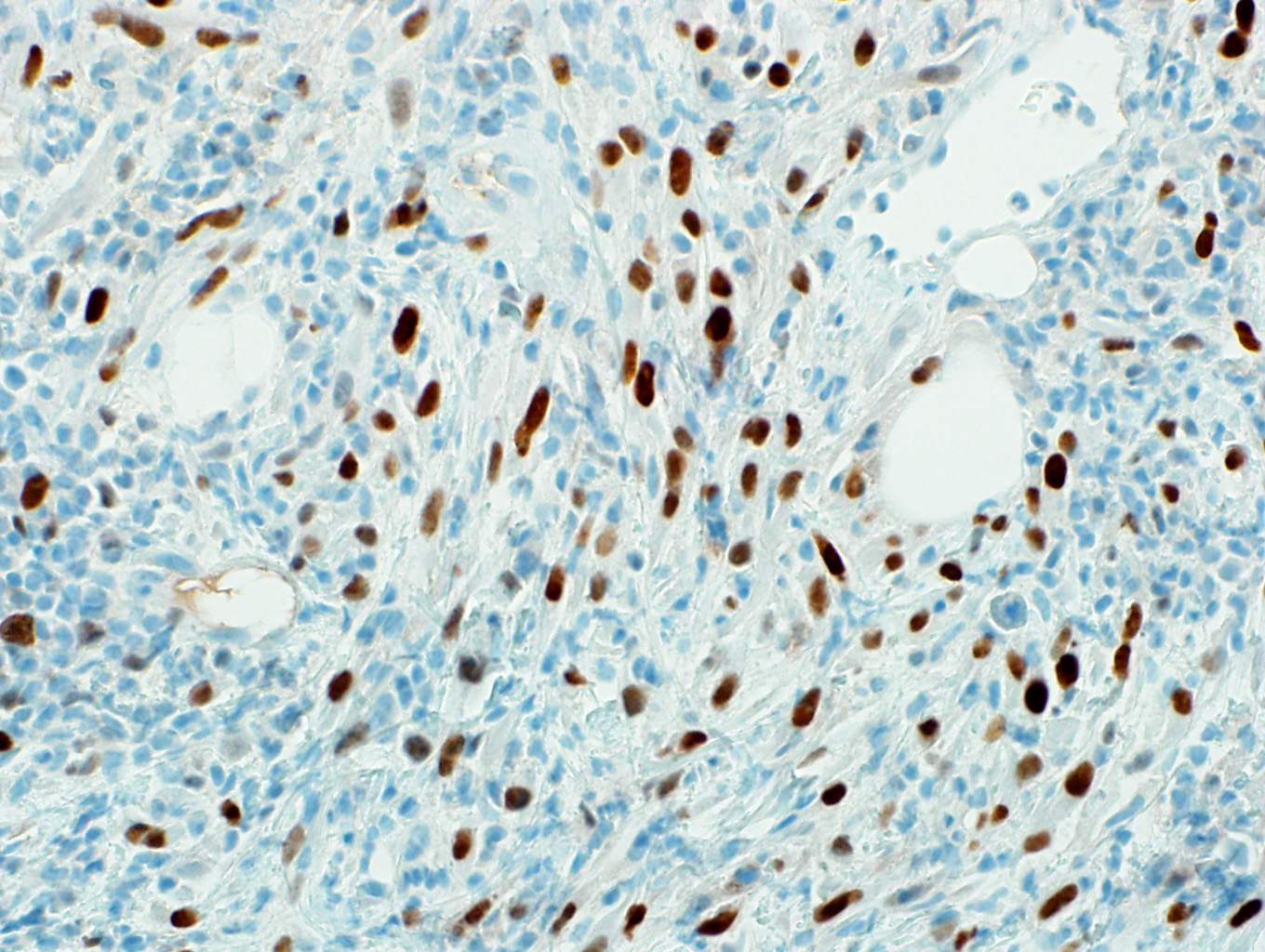
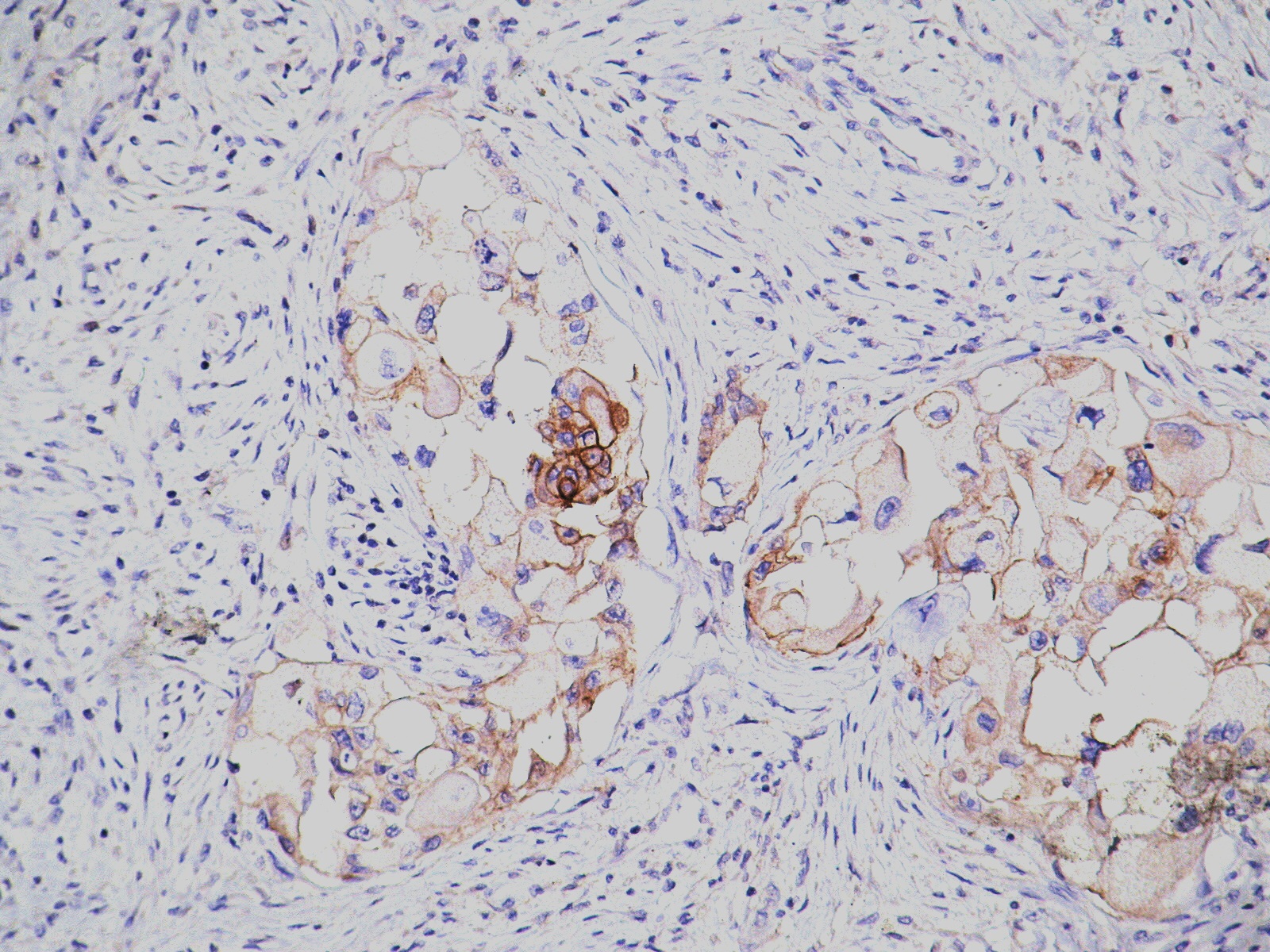
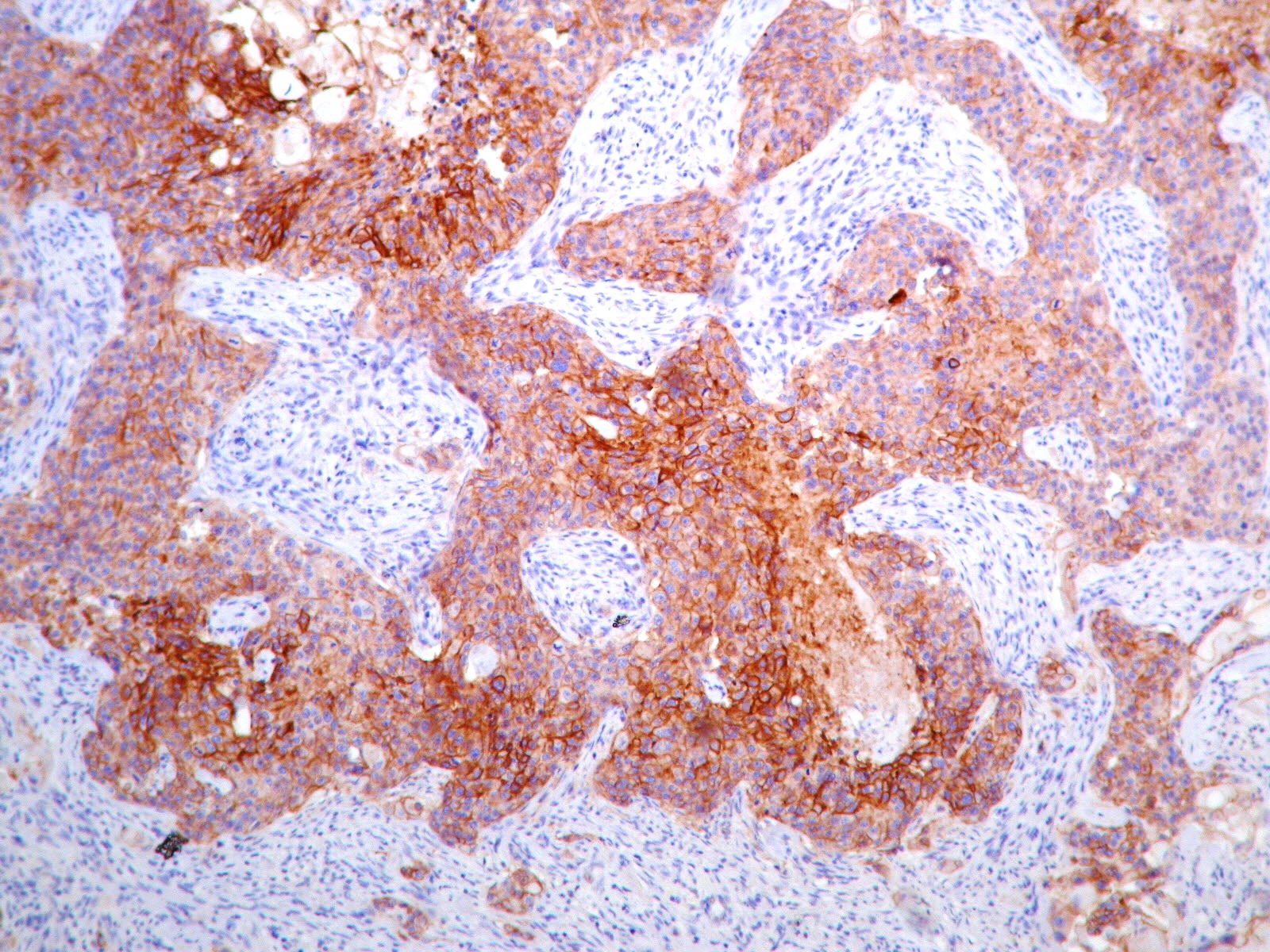
- When lacking a ductal carcinoma in situ or conventual mammary carcinoma component, a panel of immunohistochemical stains (cytokeratins, including high molecular weight and p63) is needed to confirm the presence of epithelial differentiation
Terminology
- Acceptable: metaplastic carcinoma, NOS
- Not recommended: carcinosarcoma, sarcomatoid carcinoma, carcinoma with pseudosarcomatous metaplasia, carcinoma with pseudosarcomatous stroma
ICD coding
- ICD-O: 8575/3 - metaplastic carcinoma, NOS
- ICD-11: 2C6Y & XH0RD4 - metaplastic carcinoma of breast and metaplastic carcinoma, NOS
Epidemiology
- Uncommon (0.2 - 1% of breast carcinomas)
- Average 55 years
Sites
- Any anatomical part of breast
Pathophysiology
- Unclear
- Some studies indicate a monoclonal origin of the heterogeneous components (J Pathol 2010;220:562, J Pathol 2004;204:131, Clin Cancer Res 2017;23:4875)
Etiology
- Multifactorial
- Same as invasive breast carcinoma of no special type, especially triple negative breast carcinomas
Clinical features
- Presents like invasive breast carcinoma of no special type
- Biological behavior variable from low to high grade
- Tends to have large tumor size, less nodal involvement and higher American Joint Committee on Cancer (AJCC) stage (Ann Surg Oncol 2014;21:3497, Ann Surg Oncol 2018;25:2249)
- Poor response to neoadjuvant systemic therapy with pathology complete response (pCR) rate of ~ 10% - 17% (Breast Cancer Res Treat 2019;176:709, Mod Pathol 2019;32:807, Ann Oncol 2006;17:605)
Diagnosis
- By histopathological examination
Radiology description
- Similar to invasive breast carcinoma of no special type
- Most appear as a mass on mammography with a mean size of 32 mm
- Microcalcification is uncommon but may be present, especially in a carcinoma in situ component
- Reference: Br J Radiol 2016;89:20140644
Prognostic factors
- Fibromatosis-like carcinomas and low grade adenosquamous carcinomas are associated with more indolent behavior (Histopathology 2016;68:45, Tumori 2009;95:264, Am J Surg Pathol 1993;17:248)
- Matrix producing metaplastic carcinomas have relatively better prognosis (Br J Cancer 2015;112:283)
- High grade spindle cell carcinomas, squamous cell carcinomas, high grade adenosquamous carcinomas and higher numbers of morphologies within mixed metaplastic carcinomas are associated with a worse prognosis (Br J Cancer 2015;112:283)
Case reports
- 39 year old woman with a recurred, 3.5 cm breast mass (Case Rep Pathol 2020;2020:4806342)
- 41 year old woman with neurofibromatosis type 1 and breast mass (Cold Spring Harb Mol Case Stud 2018;4:a002352)
- 47 year old man with a 2.4 cm spiculated nodule and associated nipple retraction (BMJ Case Rep 2018;2018:bcr2017222033)
- 47 year old woman with pleomorphic liposarcoma diagnosis on core biopsy (Pathobiology 2018;85:261)
- 48 year old woman with painless calcified breast mass (Int J Surg Case Rep 2017;34:100)
- 60 year old woman with metaplastic carcinoma arising in microglandular adenosis (J Pathol Transl Med 2017;51:418)
- 88 year old woman with huge bleeding tumor (J Med Invest 2020;67:365)
Treatment
- Mastectomy or local excision, with or without radiation and chemotherapy
- Lower response rates to conventional chemotherapy (Breast J 2019;25:418)
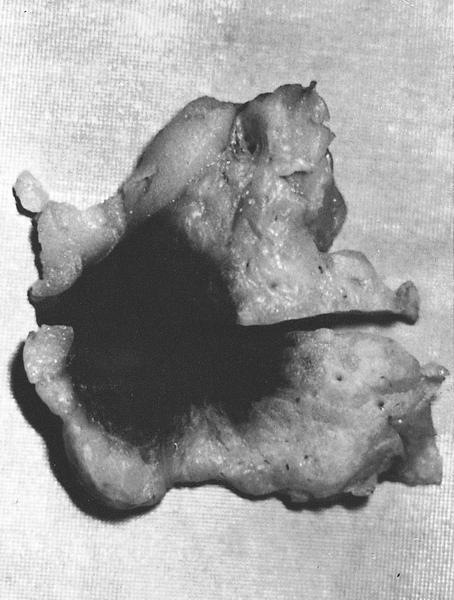
Gross description
- Often firm, well circumscribed and solid
- Pearly, white to grayish and glistening cut surface in areas of squamous and chondroid differentiation
- Mean 3.9 cm, ranging from 2 cm to > 10 cm
Gross images
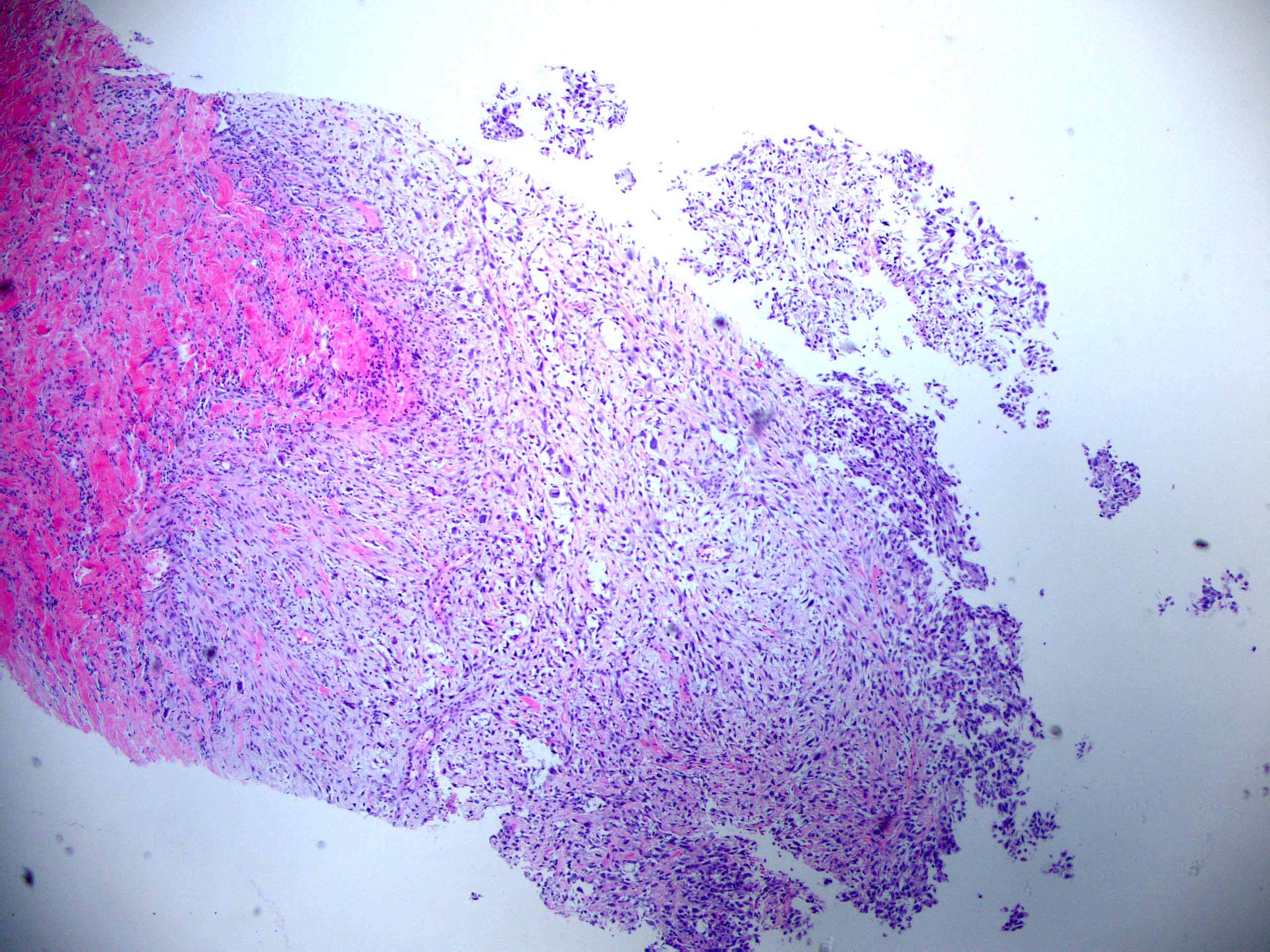
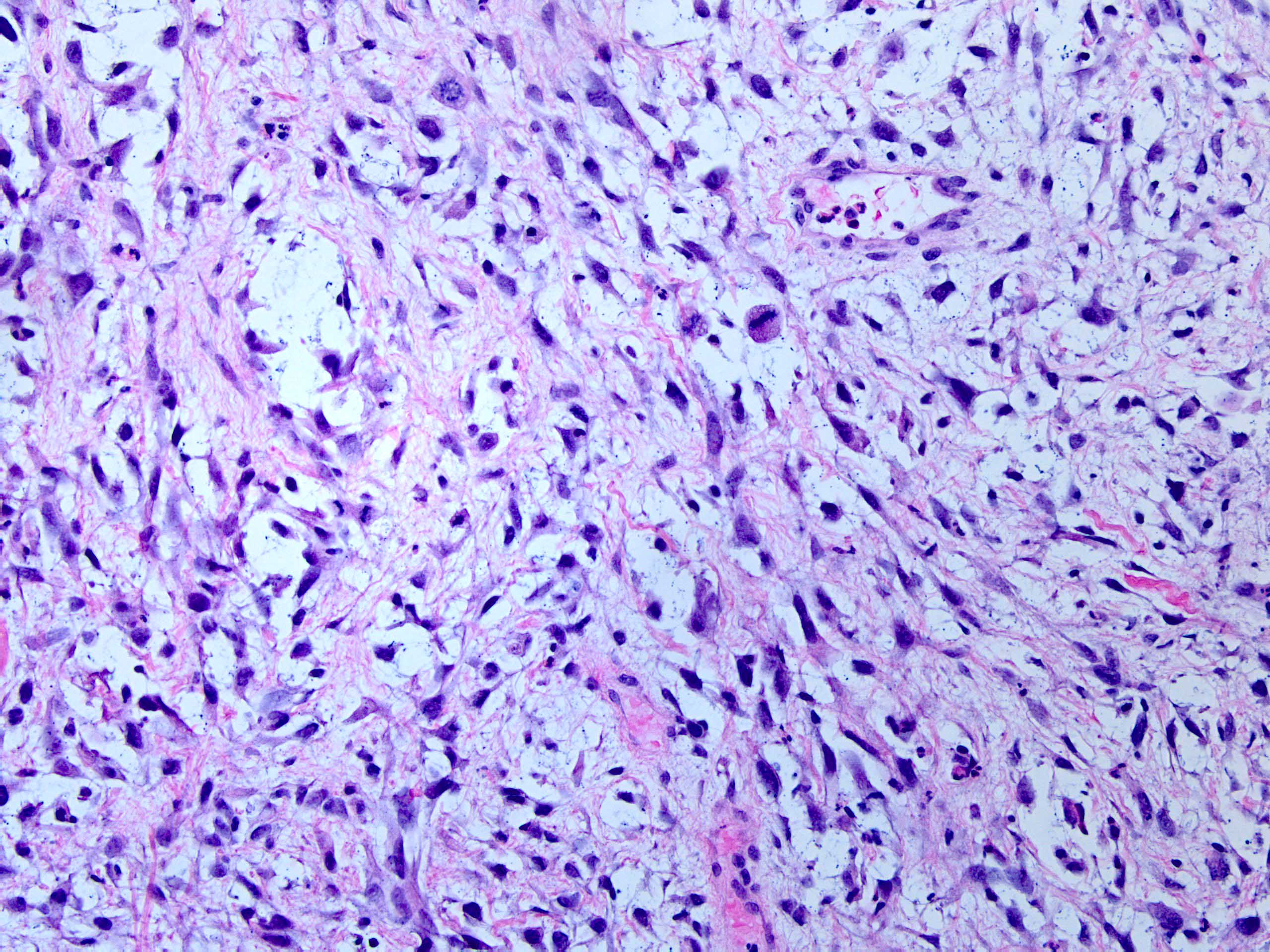
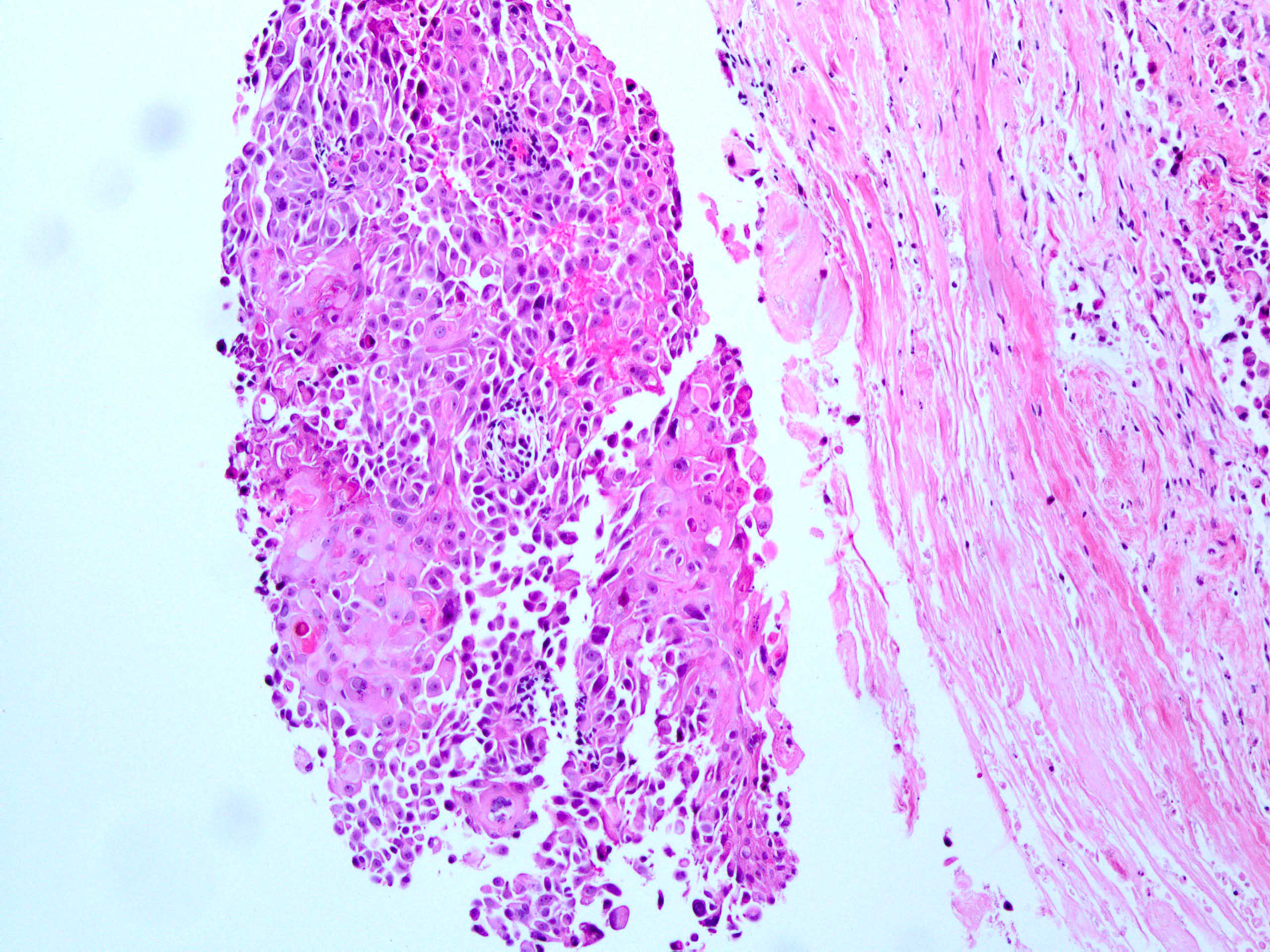
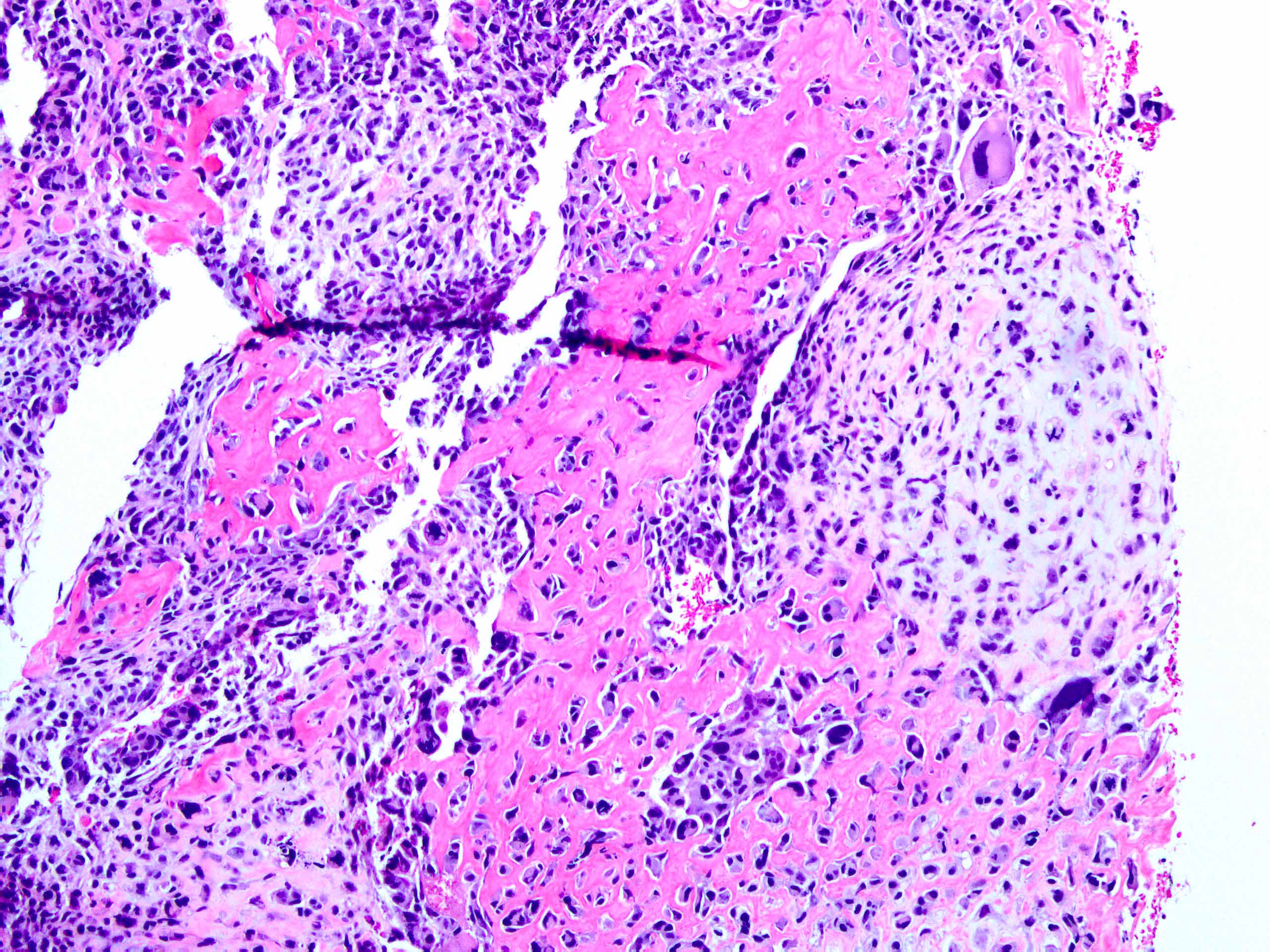
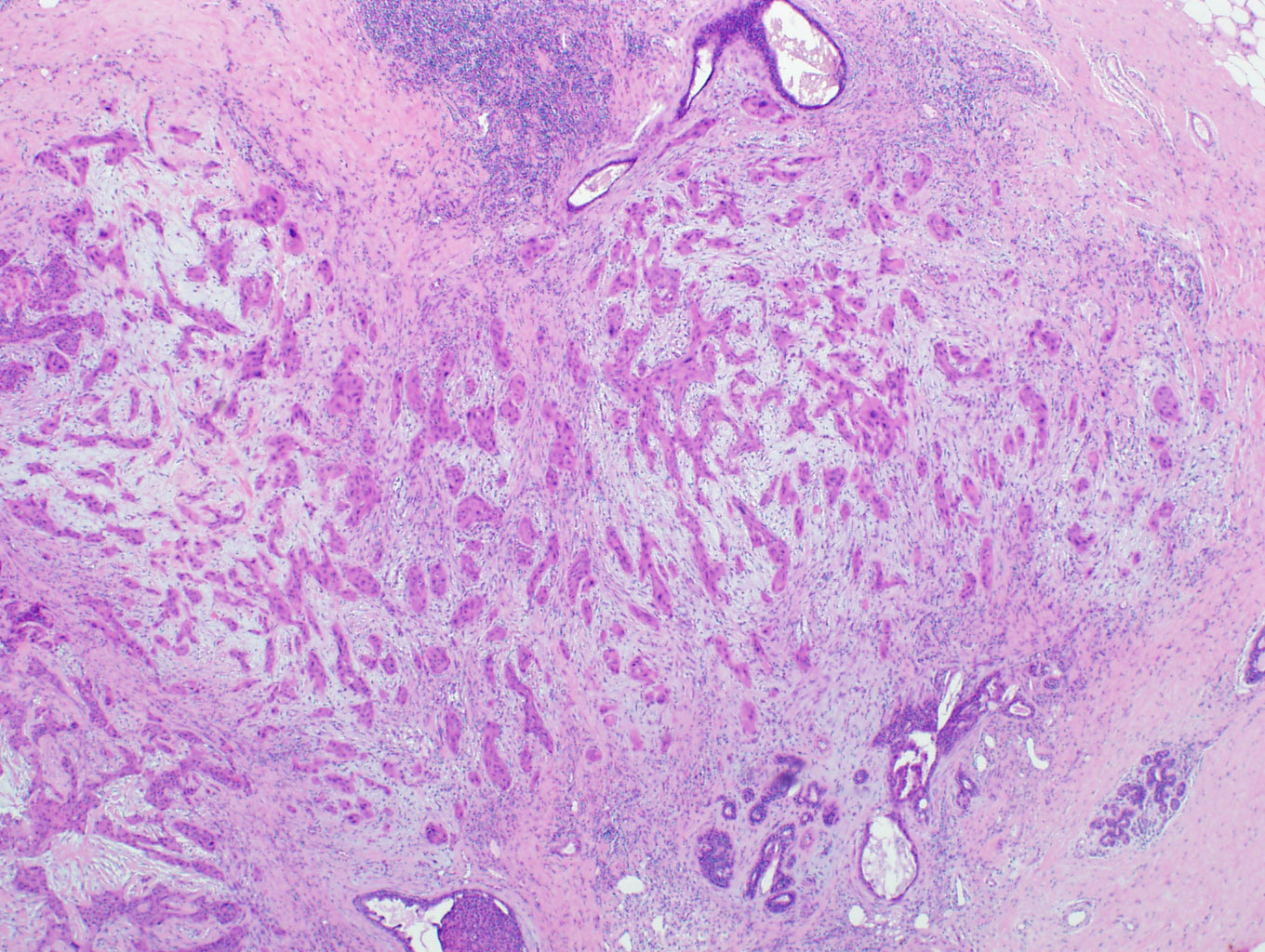
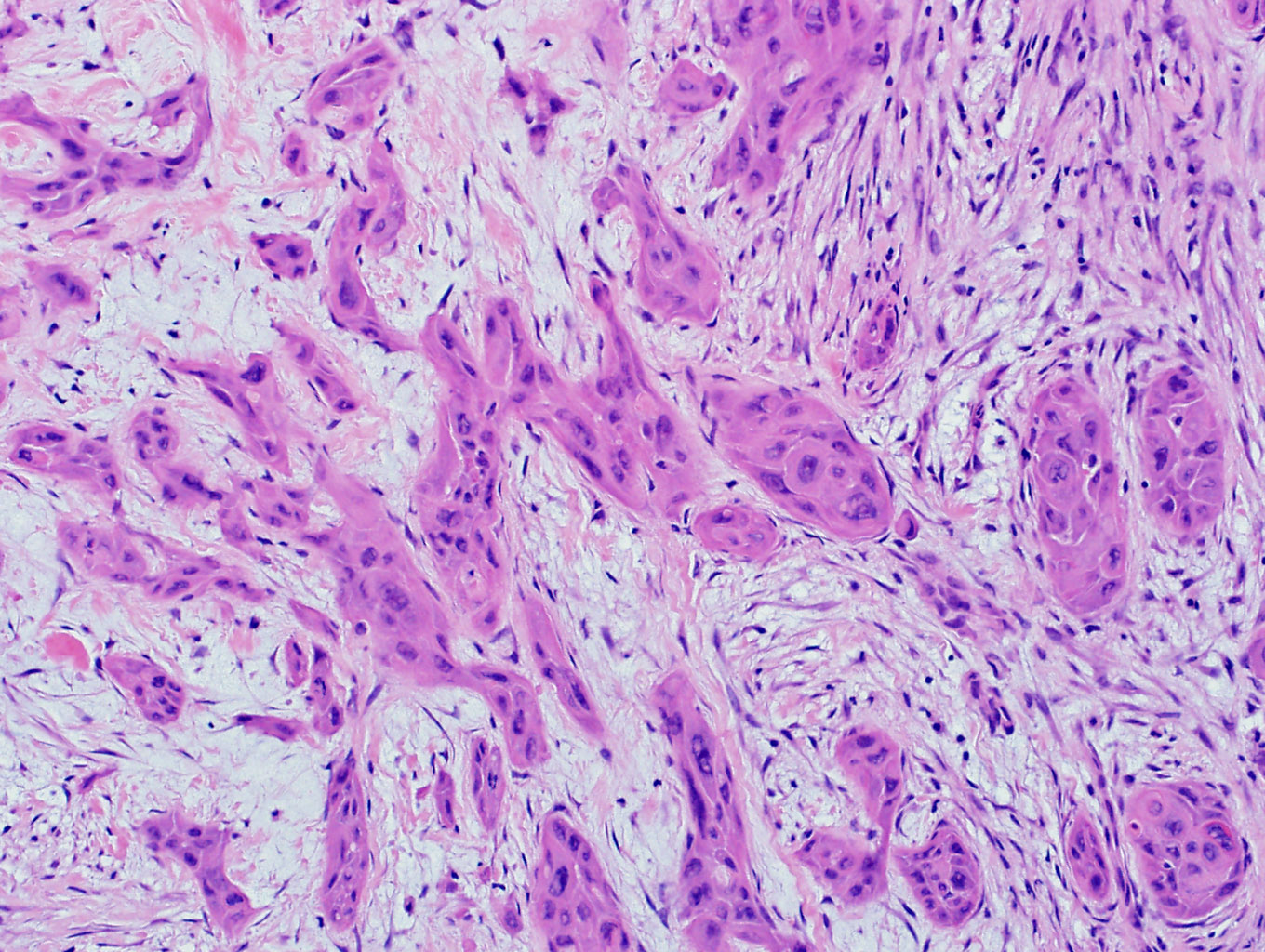
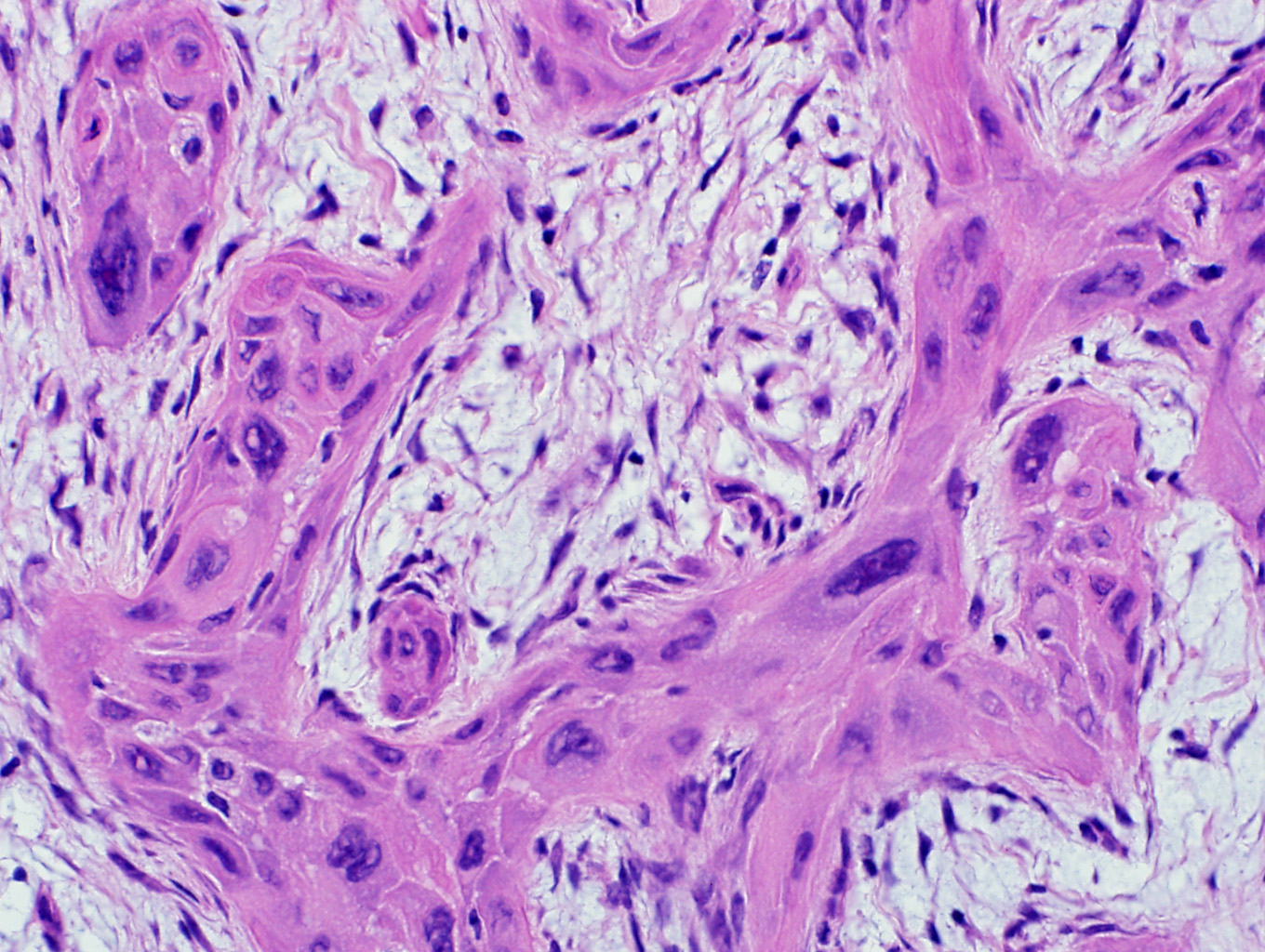
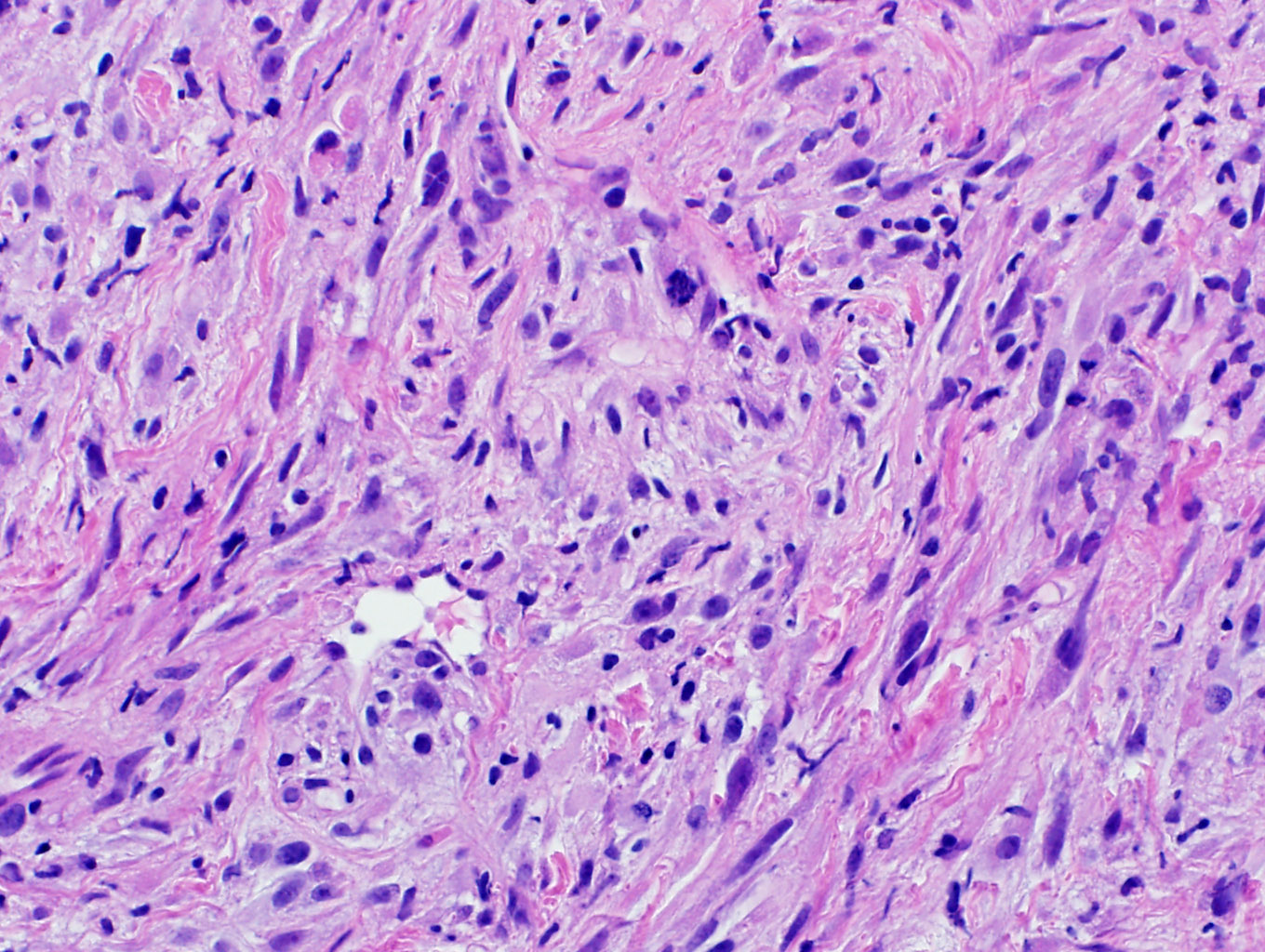
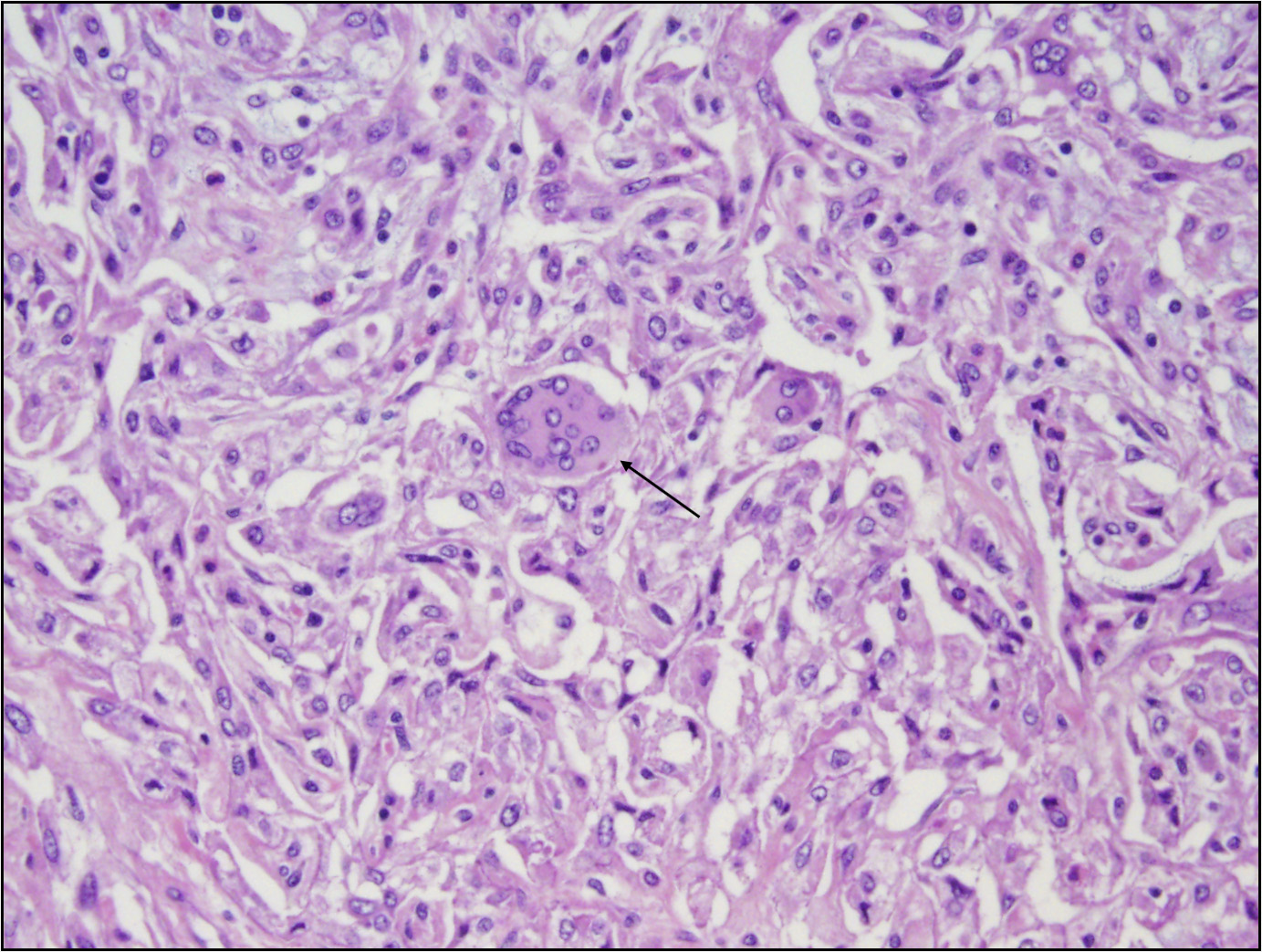
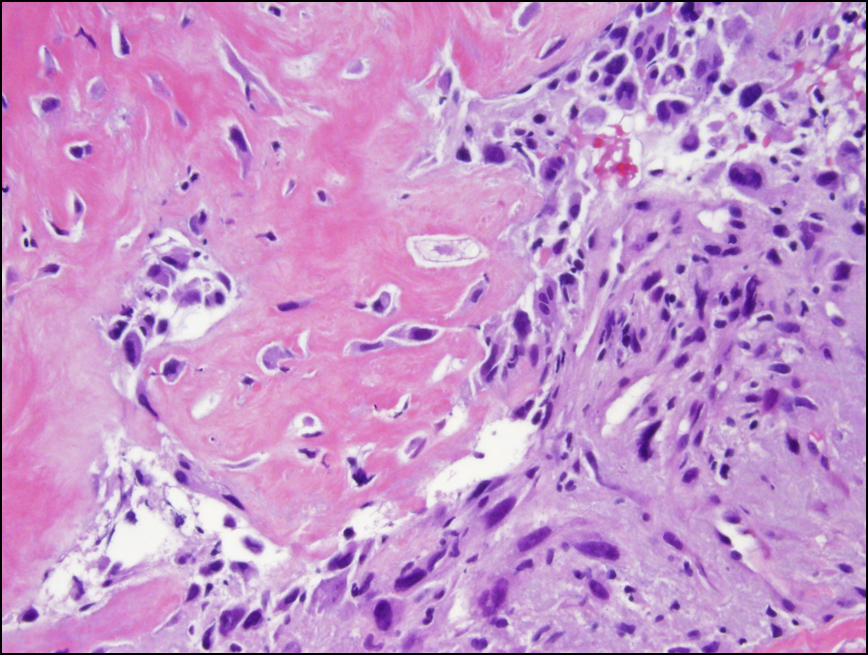
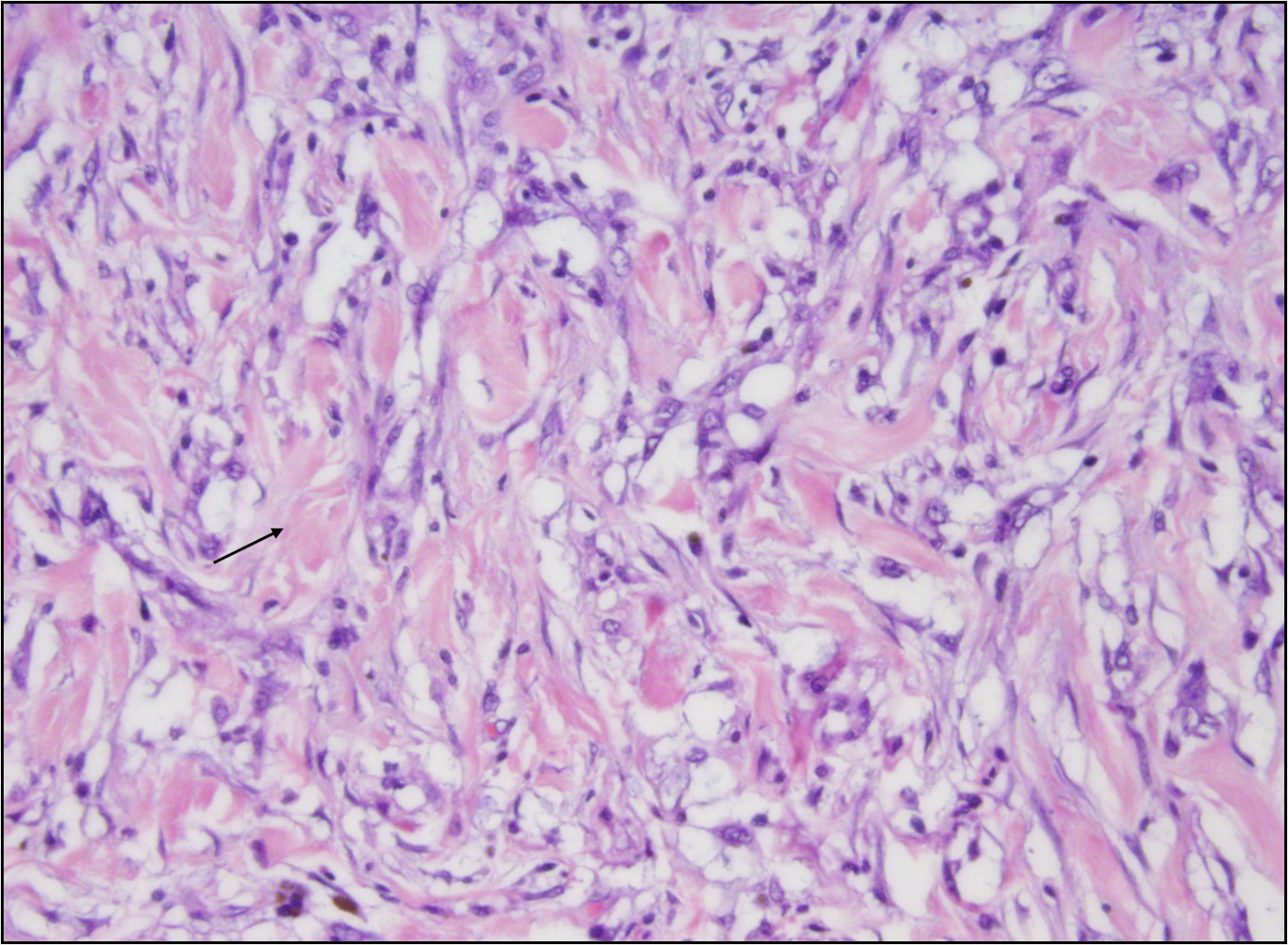
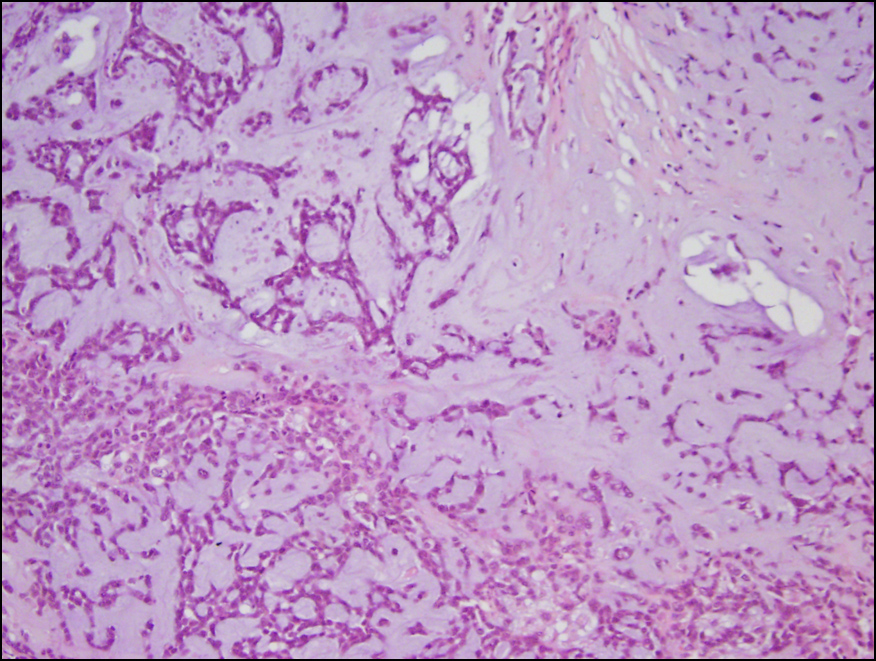
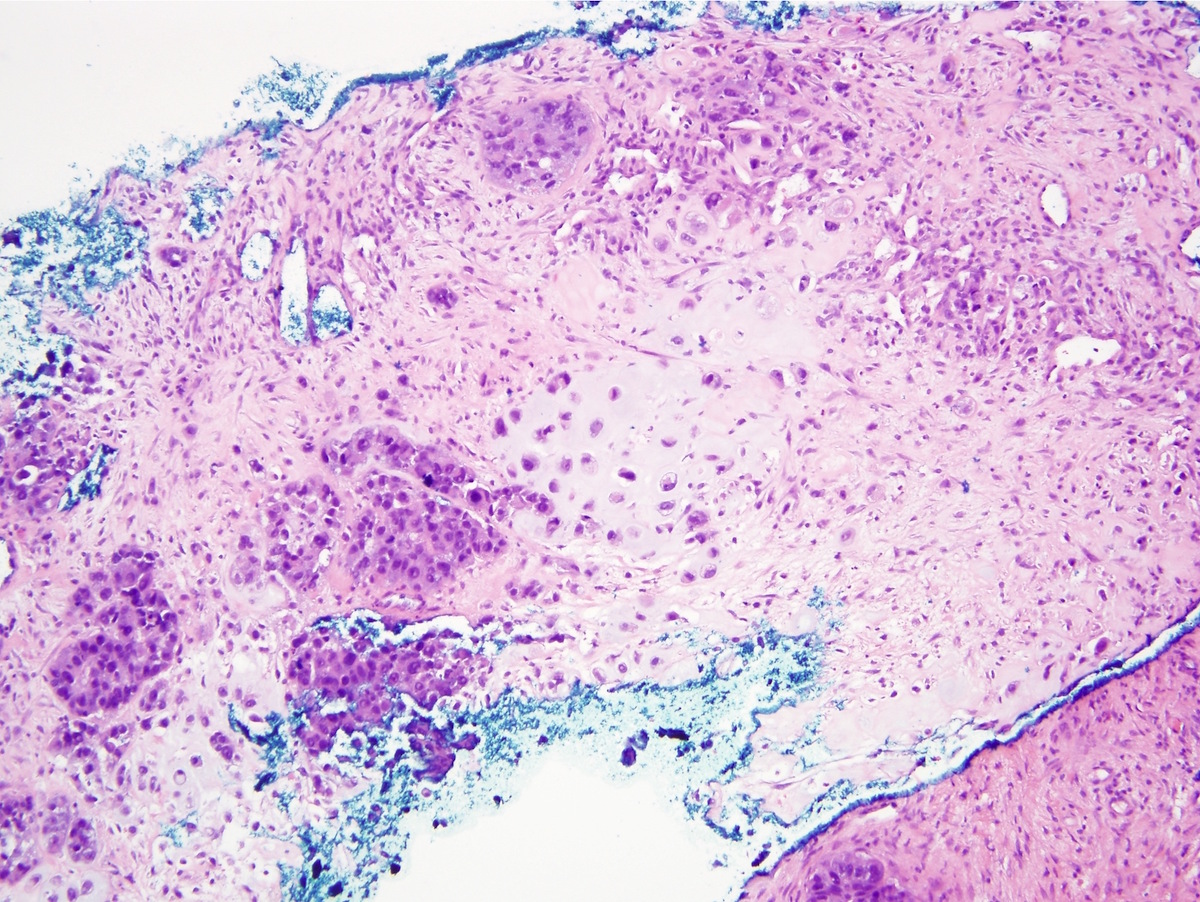
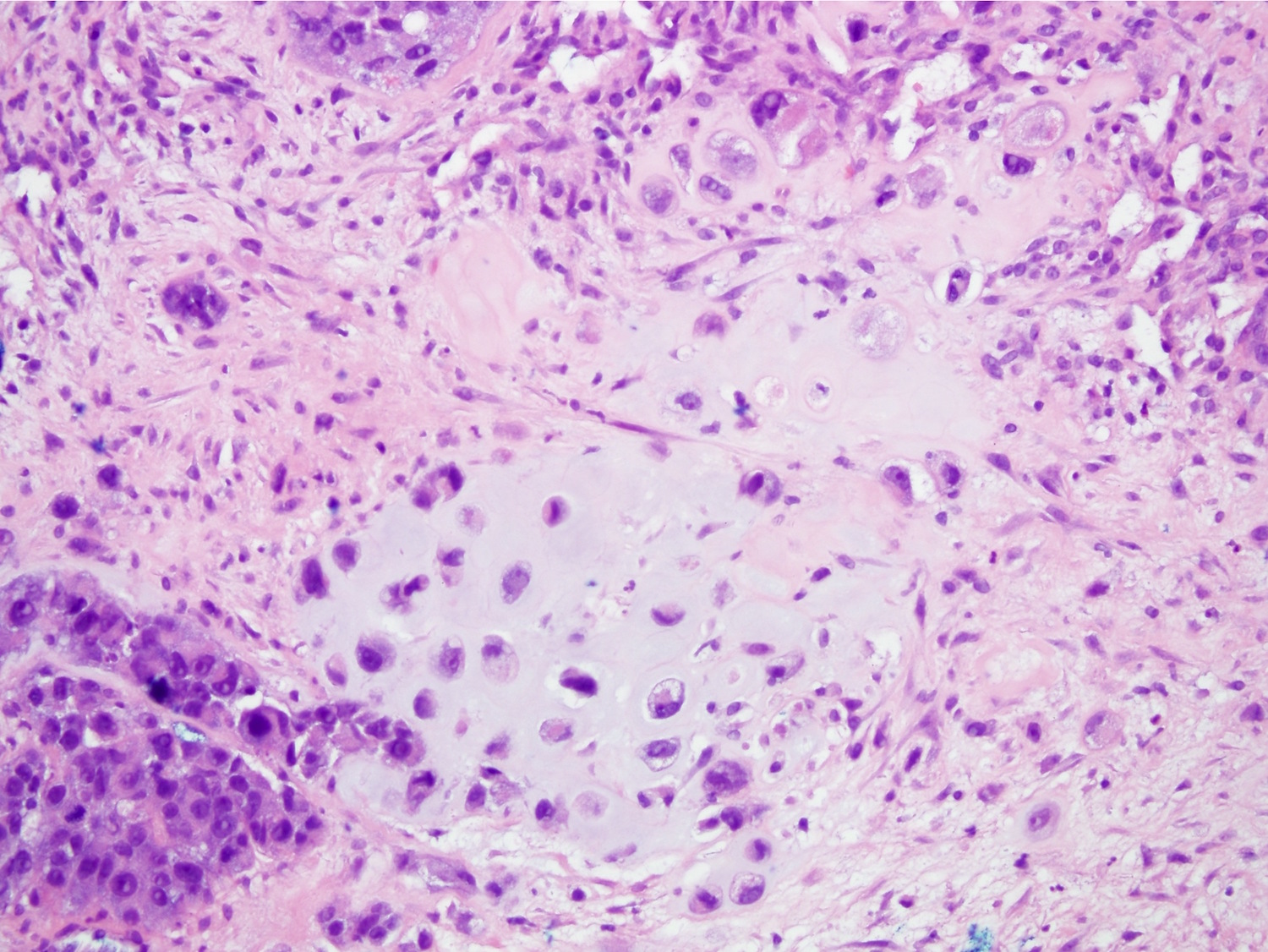
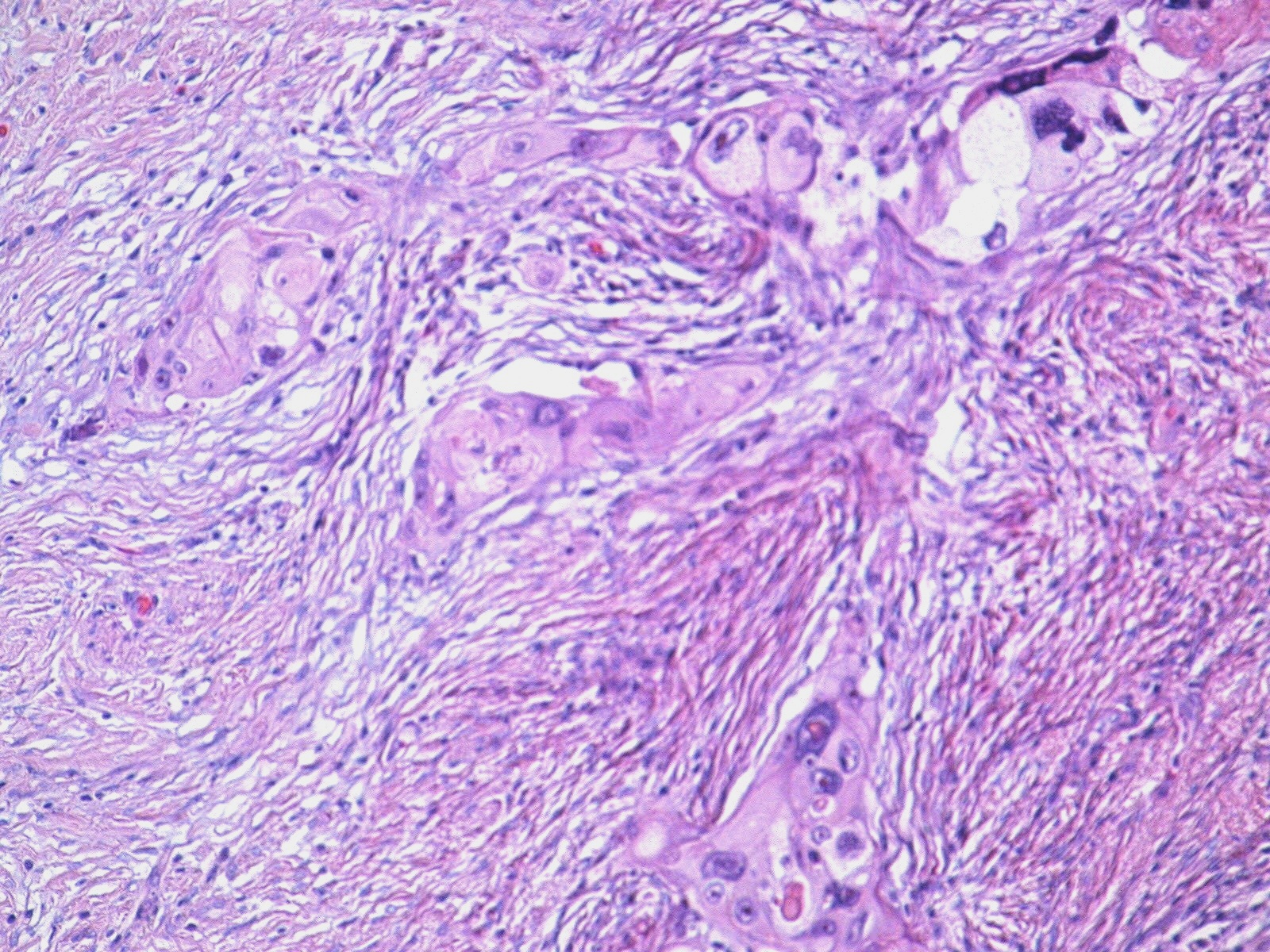
Microscopic (histologic) description
- Morphologically heterogenous
- Can be epithelial only carcinomas, pure (monophasic) sarcomatoid carcinomas and biphasic epithelial and sarcomatoid carcinomas
- Epithelial only carcinomas include low grade adenosquamous carcinoma, high grade adenosquamous carcinoma and squamous cell carcinoma
- Pure (monophasic) sarcomatoid carcinomas include fibromatosis-like metaplastic carcinoma and spindle cell carcinoma
- Heterologous mesenchymal components include chondroid, osseous, rhabdomyosarcomatous, angiosarcomatous, liposarcomatous and neuroglial differentiation or in combination
- Mesenchymal component can show a wide spectrum of atypia, ranging from minimal atypia to frankly malignant
- May need to look carefully, extensive sampling or performing immunohistochemistry (a combination of several stains) for identification of epithelial component
Microscopic (histologic) images
Contributed by Huina Zhang, M.D., Ph.D. and Julie M. Jorns, M.D.
Contributed by Indu Agarwal M.D. and Semir Vranić, M.D., Ph.D.
Cytology description
- Moderate to marked cytologic atypia
- Large, pleomorphic and spindle shaped cells or malignant squamous cells
- Isolated or clusters of malignant cells
- Rarely, malignant cartilage or bone or osteoclastic-like giant cells
- Dual components usually not identified
- Reference: Cibas: Cytology - Diagnostic Principles and Clinical Correlates, 5th Edition, 2020
Positive stains
- Broad spectrum keratin AE1 / AE3, CAM5.2, OSCAR, 34 beta E12, MNF116: 75 - 90% (Appl Immunohistochem Mol Morphol 2020 Aug 28 [Epub ahead of print])
- High molecular weight keratin CK5/6, CK14: 70 - 77%
- p63: 77%
- Low molecular weight keratin CK8/18, CK7, CK19: 36 - 61%
- Myoepithelial cell markers SMA, CD10: 60 - 70%
Negative stains
Molecular / cytogenetics description
- Basal-like or claudin low molecular subtype
- No uniform molecular profile
- May affect TP53, RB1, TERT promoter genes, chromatin remodeling genes (i.e. ARID1A, KMT2C), genes related to PI3K pathway (i.e. PIK3CA, PIK3R1, PTEN), MAPK pathway (NF1, KRAS, NRAS) or WNT pathway (FAT1, APC, CCN6) (Clin Breast Cancer 2020;20:326, Cancers (Basel) 2020;12:1832, Mod Pathol 2018;31:1661, Clin Cancer Res 2017;23:3859)
Videos
Metaplastic carcinoma by
Dr. Alexander Damron
Sample pathology report
- Breast, left, 3:00 (mass), ultrasound guided core needle biopsy:
- Malignant spindle cell lesion, consistent with spindle cell carcinoma (see comment)
- Comment: H&E sections show a high grade spindle cell lesion with pleomorphic nuclei, irregular nuclear borders and occasional mitotic figures, including atypical mitosis. There is no leaf-like growth pattern. Immunohistochemical staining shows that the neoplastic cells are positive for pancytokeratin, p63, CK5 and AE1 / AE3 and are negative for CD34. The morphology and immunoprofile of this malignant spindle cell lesion are consistent with a spindle cell (metaplastic) carcinoma.
Differential diagnosis
- Phyllodes tumor:
- Primary breast sarcoma:
- Metastatic sarcoma:
- Adenomyoepithelioma:
- Bland epithelial and stromal component
- Stromal only with myoepithelial differentiation
- Lack of squamous differentiation
- Myoepithelial carcinoma:
- Entirely or almost entirely malignant spindle cells with myoepithelial differentiation
- No squamous component or other mesenchymal differentiation
- Pleomorphic adenoma:
- Usually retroareolar region
- Well organized biphasic pattern with inner layer of regular epithelial cells
- Thin, continuous outer layer of myoepithelial cells
- No cytologic atypia, atypical mitosis or necrosis
- See others in variants sections
Additional references
Board review style question #1
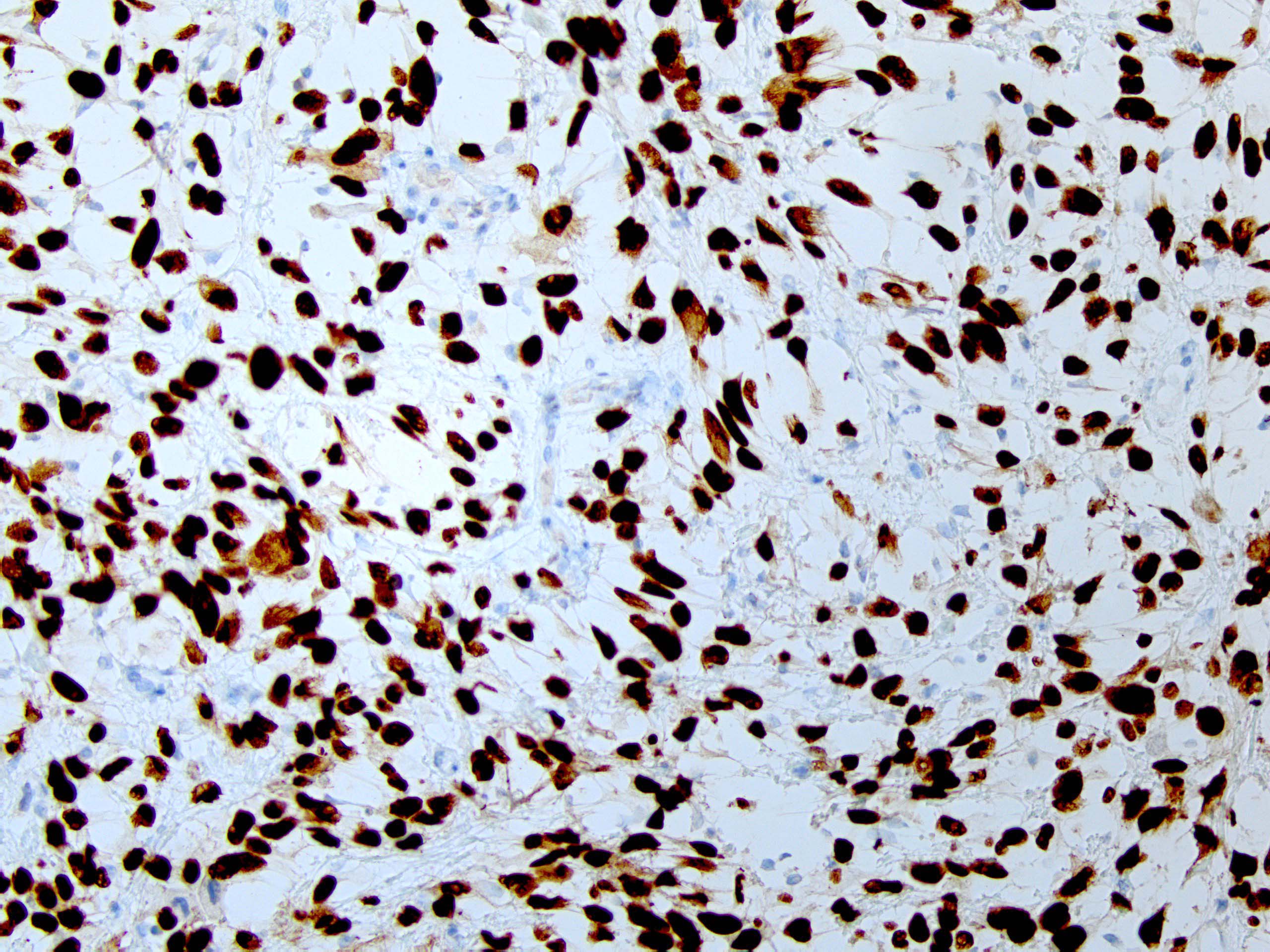
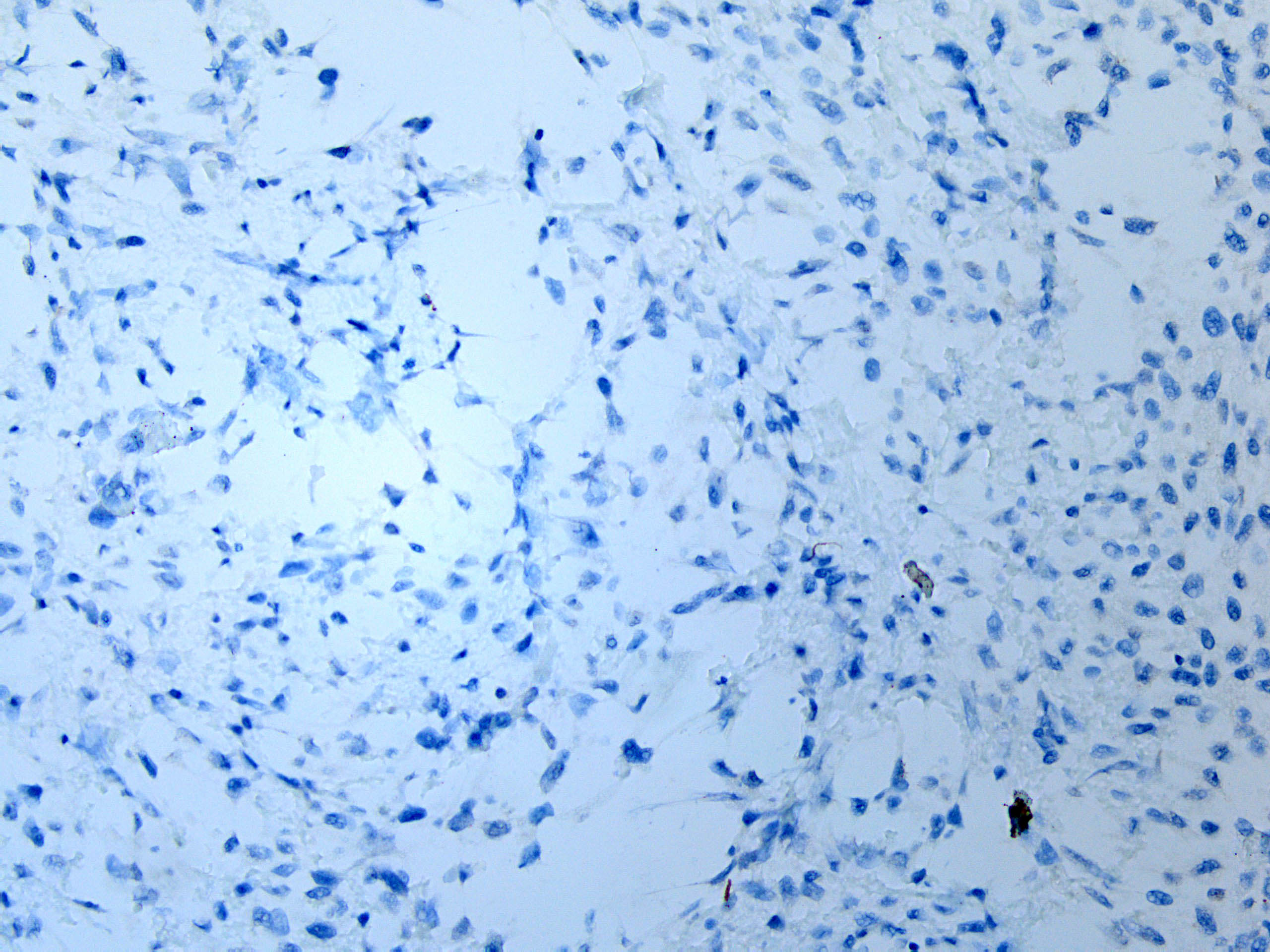
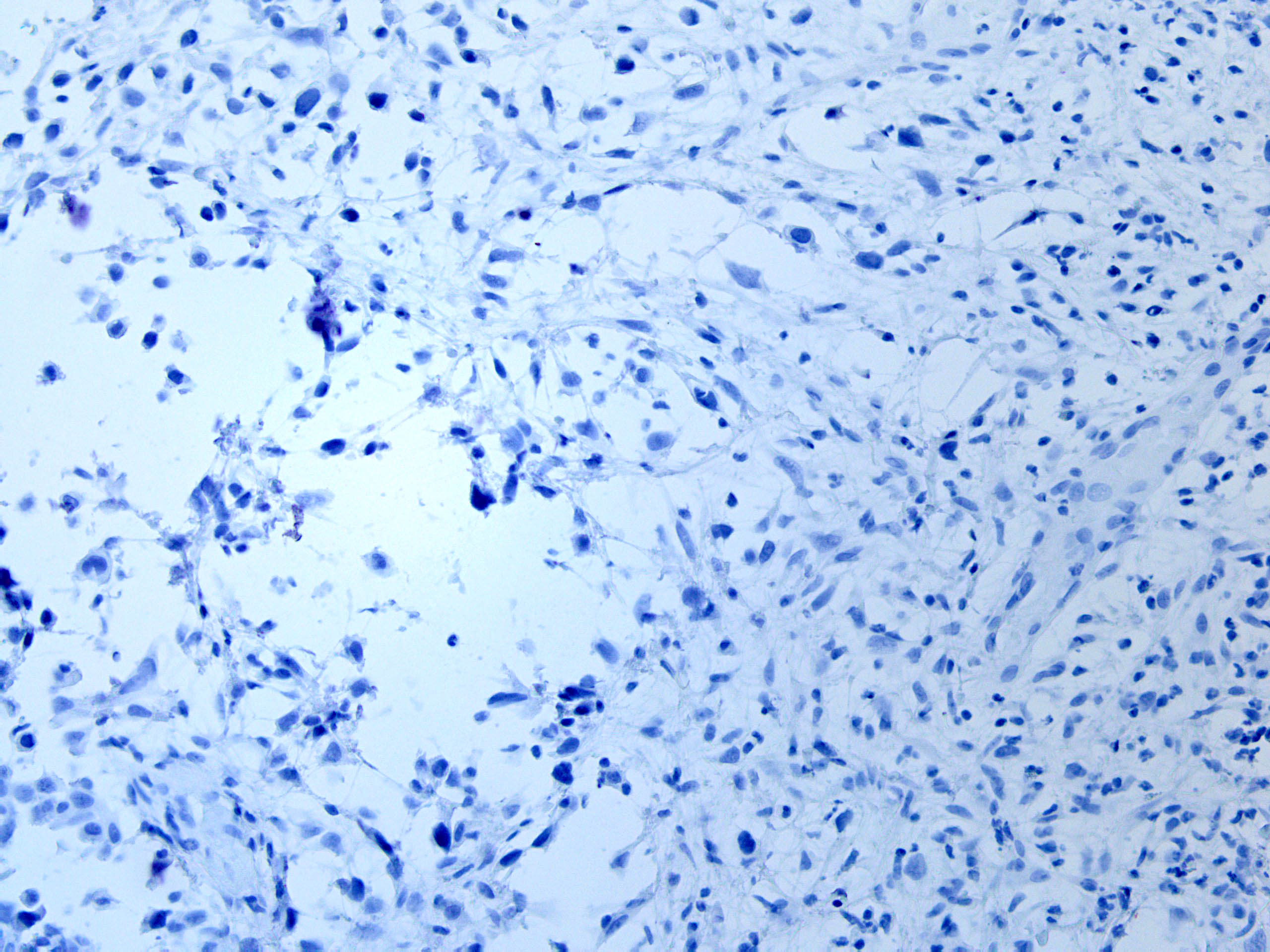
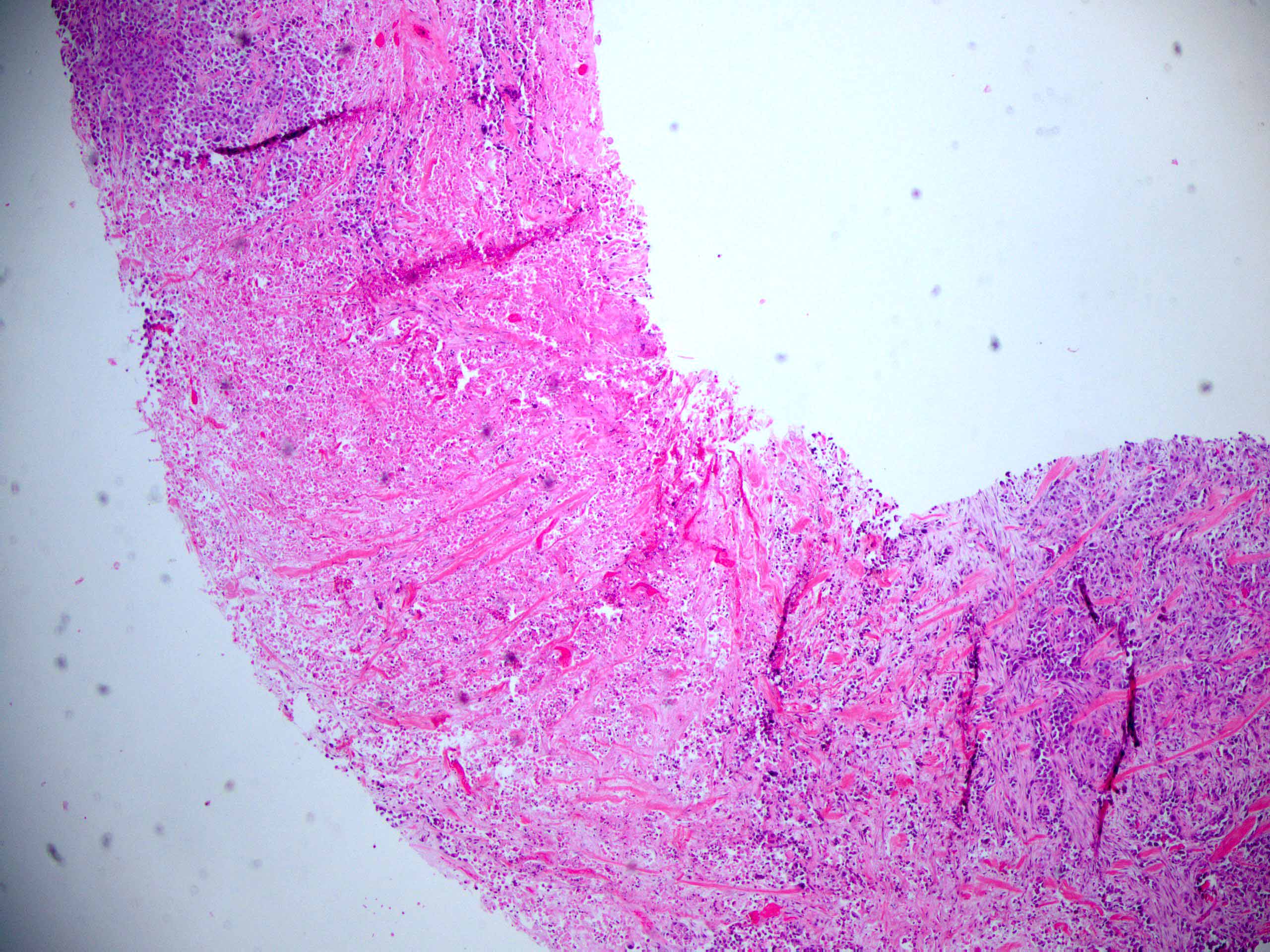
A 55 year old woman without significant medical history was found to have a 2.5 cm mass on mammogram and a biopsy was performed. Histology and immunohistochemical stain for p63 were shown (see images above). What is the likely diagnosis?
- Malignant phyllodes tumor
- Metaplastic carcinoma
- Metastatic sarcoma
- Primary breast sarcoma
Board review style answer #1
B. Metaplastic carcinoma
H&E section shows a high grade spindle cell lesion with pleomorphic nuclei, irregular nuclear borders and occasional mitotic figures, including atypical mitosis. Based on the morphology, all the listed choices should be considered. Performing a panel of immunohistochemical stains including high molecular weight cytokeratin and p63 is very important and helpful. In this case, the positivity for p63 (as well as other cytokeratins, not shown here) supports the diagnosis of spindle cell carcinoma and makes other choices less likely. It needs to be noted that cytokeratins and p63 are often focal and patchy, therefore a panel of immunostains is usually needed.
Comment Here
Reference: Metaplastic carcinoma
H&E section shows a high grade spindle cell lesion with pleomorphic nuclei, irregular nuclear borders and occasional mitotic figures, including atypical mitosis. Based on the morphology, all the listed choices should be considered. Performing a panel of immunohistochemical stains including high molecular weight cytokeratin and p63 is very important and helpful. In this case, the positivity for p63 (as well as other cytokeratins, not shown here) supports the diagnosis of spindle cell carcinoma and makes other choices less likely. It needs to be noted that cytokeratins and p63 are often focal and patchy, therefore a panel of immunostains is usually needed.
Comment Here
Reference: Metaplastic carcinoma