Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Clinical features | Diagnosis | Radiology description | Radiology images | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Tozbikian G. Secretory. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/breastmalignantjuvenile.html. Accessed December 26th, 2024.
Definition / general
- Rare subtype of low grade, translocation associated invasive breast carcinoma
- Tumor with microcystic, solid and tubular architecture, composed of vacuolated tumor cells producing intracellular and extracellular secretions
- Generally triple negative with basal-like phenotype (Mod Pathol 2012;25:567)
- First described by McDivitt and Stewart in 1966 (JAMA 1966;195:388)
Essential features
- Rare, < 1% of breast cancers
- Most common primary pediatric breast cancer but can occur at any age
- Circumscribed margins, solid nests, cysts and gland formation with PAS+ intraluminal secretions
- Tumor cells with abundant vacuolated or granular cytoplasm, low nuclear grade
- Generally triple negative for estrogen receptor, progesterone receptor and HER2
- Most tumors have translocation yielding ETV6-NTRK3 fusion gene
- Associated with a favorable prognosis in younger patients
Terminology
- Originally named juvenile breast carcinoma, the terminology was changed to secretory carcinoma after reports of the tumor occurring in adults
ICD coding
- ICD-O: 8502/3 - secretory carcinoma of breast
Epidemiology
- Rare, < 0.02% of all breast cancers (Breast 2012;21:350, J Surg Oncol 2016;113:721)
- Initially described in children; most common childhood breast cancer (JAMA 1966;195:388)
- Wide age range, bimodal age distribution with peaks in second and seventh decades (Breast 2012;21:350, Diagn Histopathol 2020;26:51)
- M:F = 1:6 to 1:31 (World J Surg Oncol 2005;3:35, Mod Pathol 2012;25:567, J Surg Oncol 2016;113:721, Ann Oncol 2000;11:1343)
Clinical features
- Tumor size, rates of axillary lymph node involvement, AJCC stage at presentation and surgical treatment are similar to invasive ductal carcinoma (J Surg Oncol 2016;113:721)
- Generally associated with indolent clinical behavior, excellent prognosis (Cancer 1980;45:2404, Clin Cancer Res 2004;10:5367)
- 5 year overall survival: 87%
- 5 year disease specific survival: 94% (Breast 2012;21:350)
- Subsets with aggressive clinical course and distant metastases have been reported (World J Surg Oncol 2005;3:35, Histopathology 2019;75:213)
- Outcome may be better in patients < 20 years old (Hum Pathol 1999;30:1435)
- Limited data regarding patterns of use and analysis of effectiveness of adjuvant radiation and chemotherapy
Diagnosis
- Histologic examination of tissue with immunohistochemistry, demonstration of ETV6-NTRK3 gene fusion by fluorescent in situ hybridization
Radiology description
- Variable, nonspecific, with reports ranging from presentation as a small, round, well circumscribed mass / nodular density to suspicious lesions with spiculated margins and microcalcifications on ultrasound and mammography (J Clin Ultrasound 2003;31:425, Breast J 2003;4:2000, Ann Surg Oncol 2002;9:663)
Case reports
- 6 year old girl treated with mastectomy and sentinel lymph node dissection (Pediatr Surg Int 2015;31:677)
- 13 year old boy with secretory breast carcinoma (Breast Cancer Res Treat 2012;133:813)
- 24 year old man with axillary lymph node metastasis (Int J Clin Exp Pathol 2015;8:3322)
- 41 year old man with long term follow up of secretory breast carcinoma (Future Oncol 2015;11:1767)
- 53 year old woman with papillary predominant pattern (Histopathology 2017;71:488)
- 79 year old woman with a palpable breast mass (Rare Tumors 2016;8:6650)
Treatment
- Surgical treatment, use of antihormonal targeted therapy similar to invasive ductal carcinoma (J Surg Oncol 2016;113:721)
Gross description
- Small, well circumscribed, mobile mass
- Median size 1.9 - 2.4 cm (J Surg Oncol 2016;113:721, Breast 2012;21:350)
- Often central, located near the areola
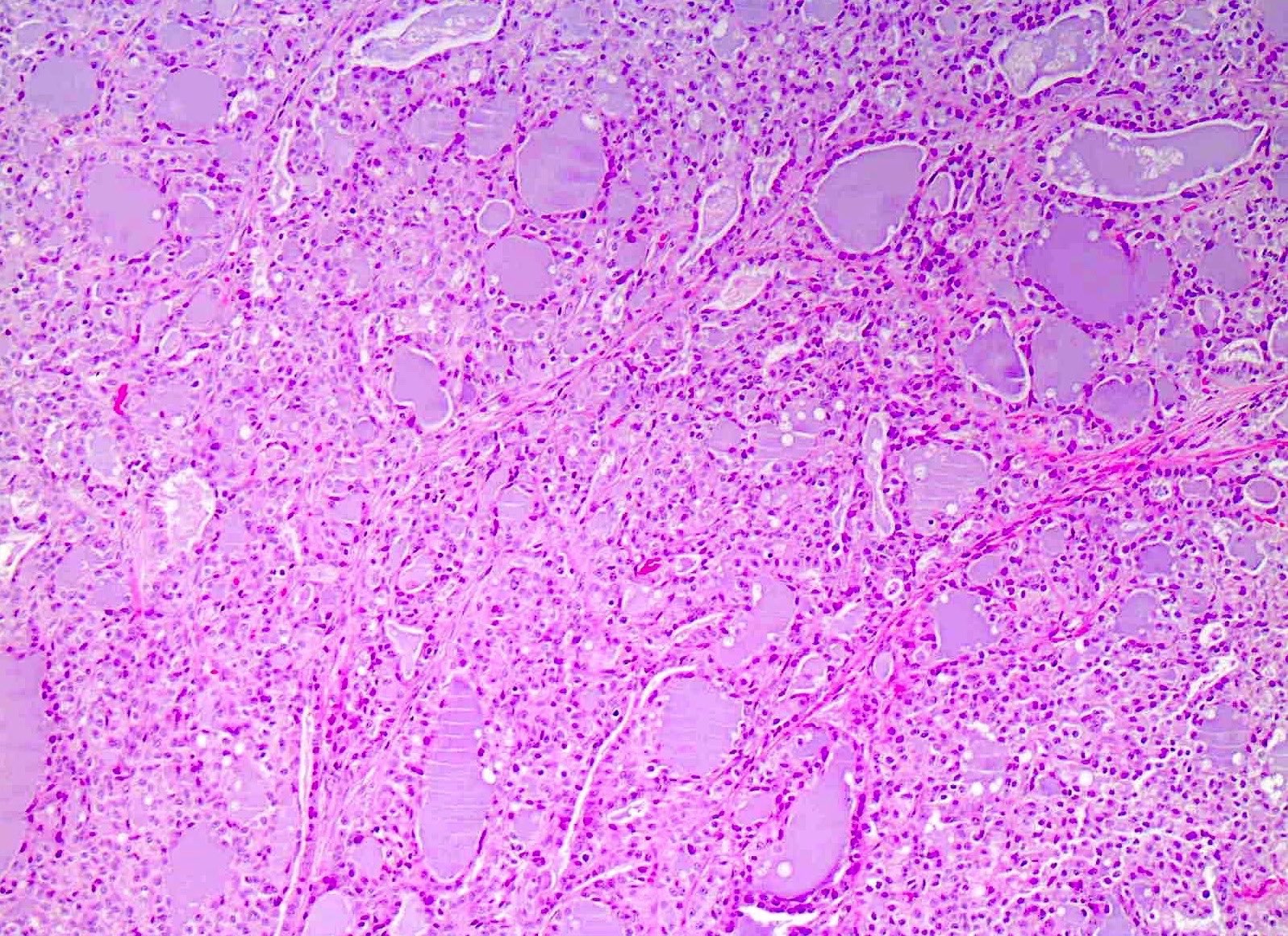
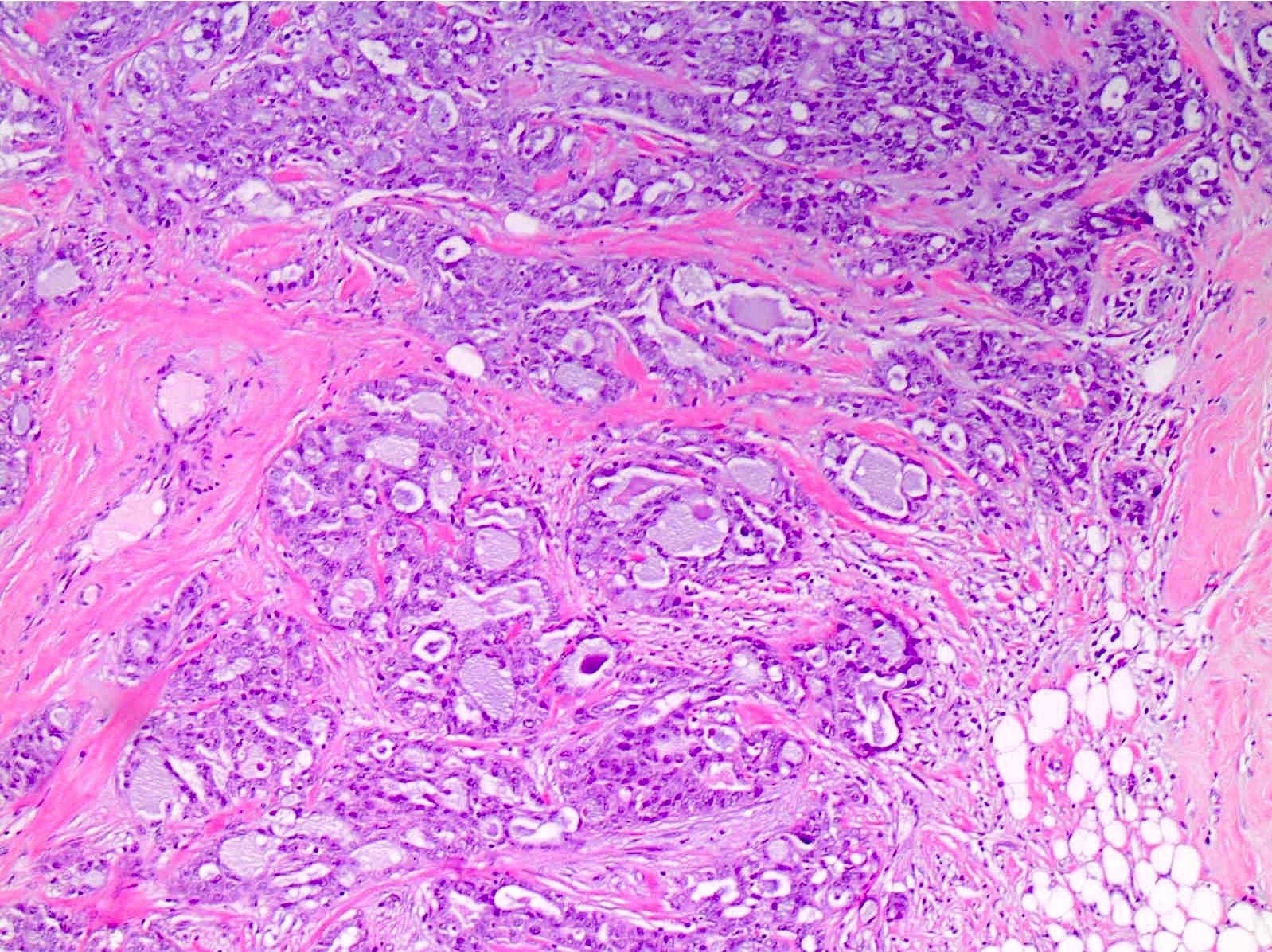
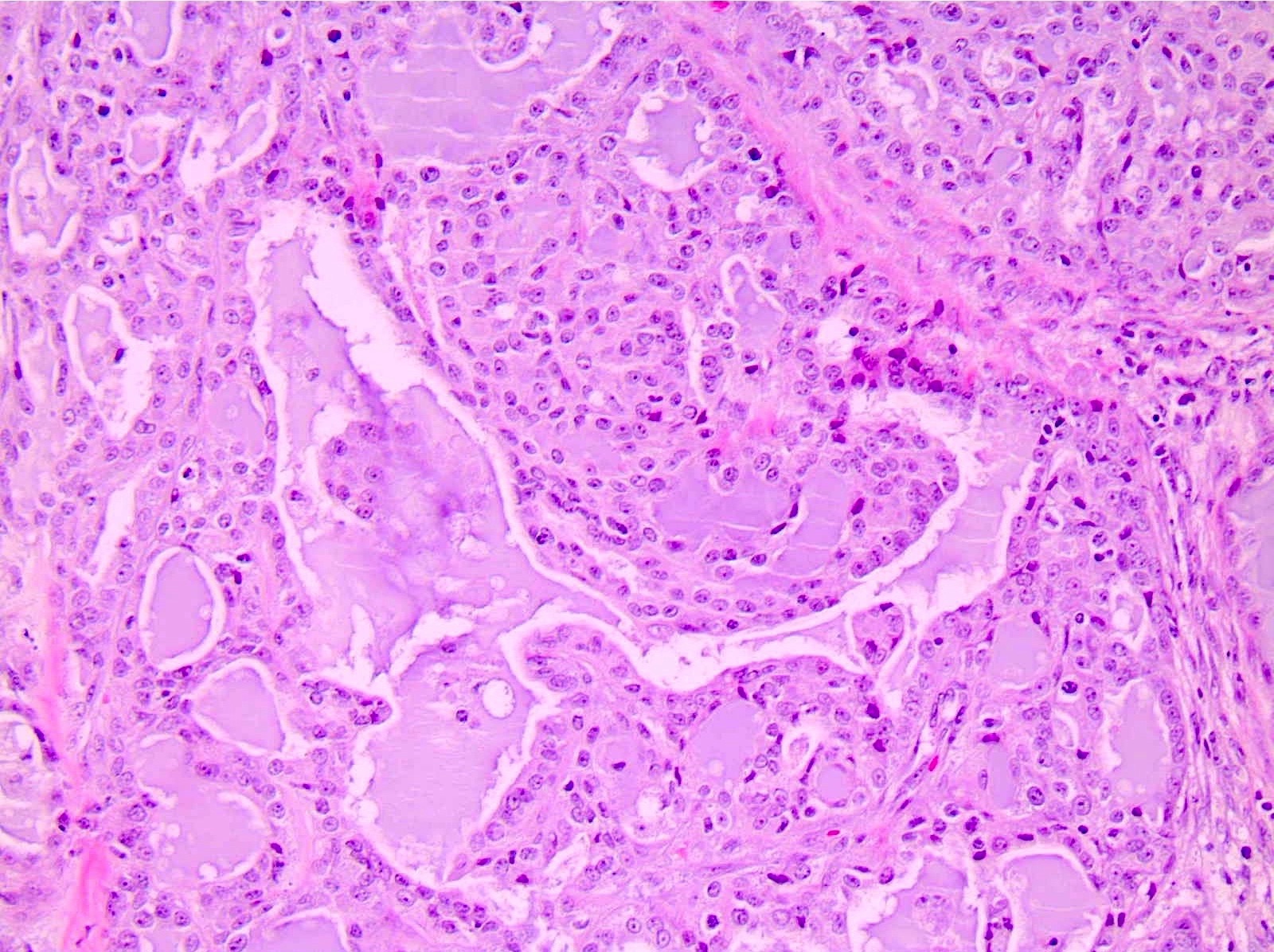
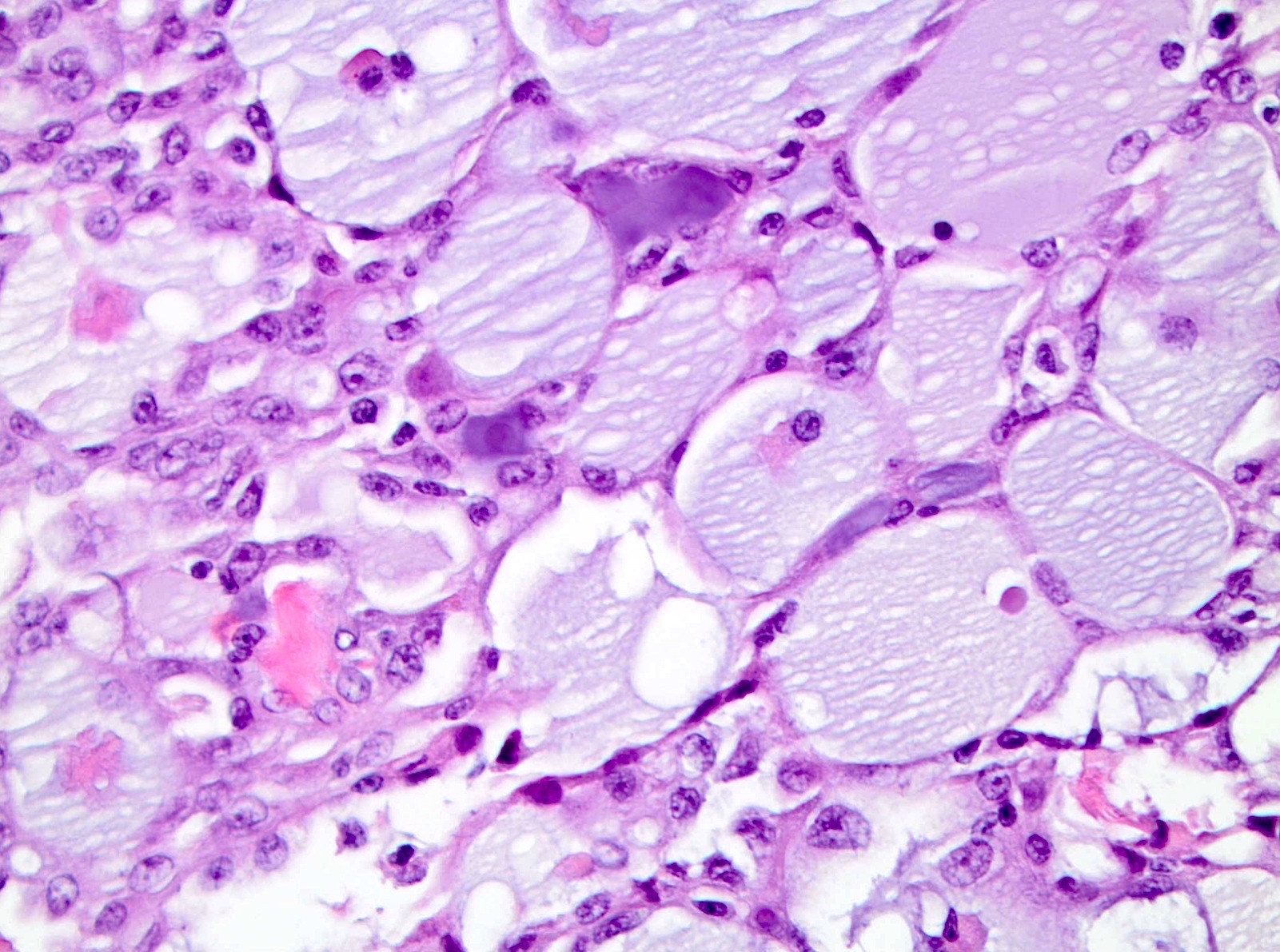
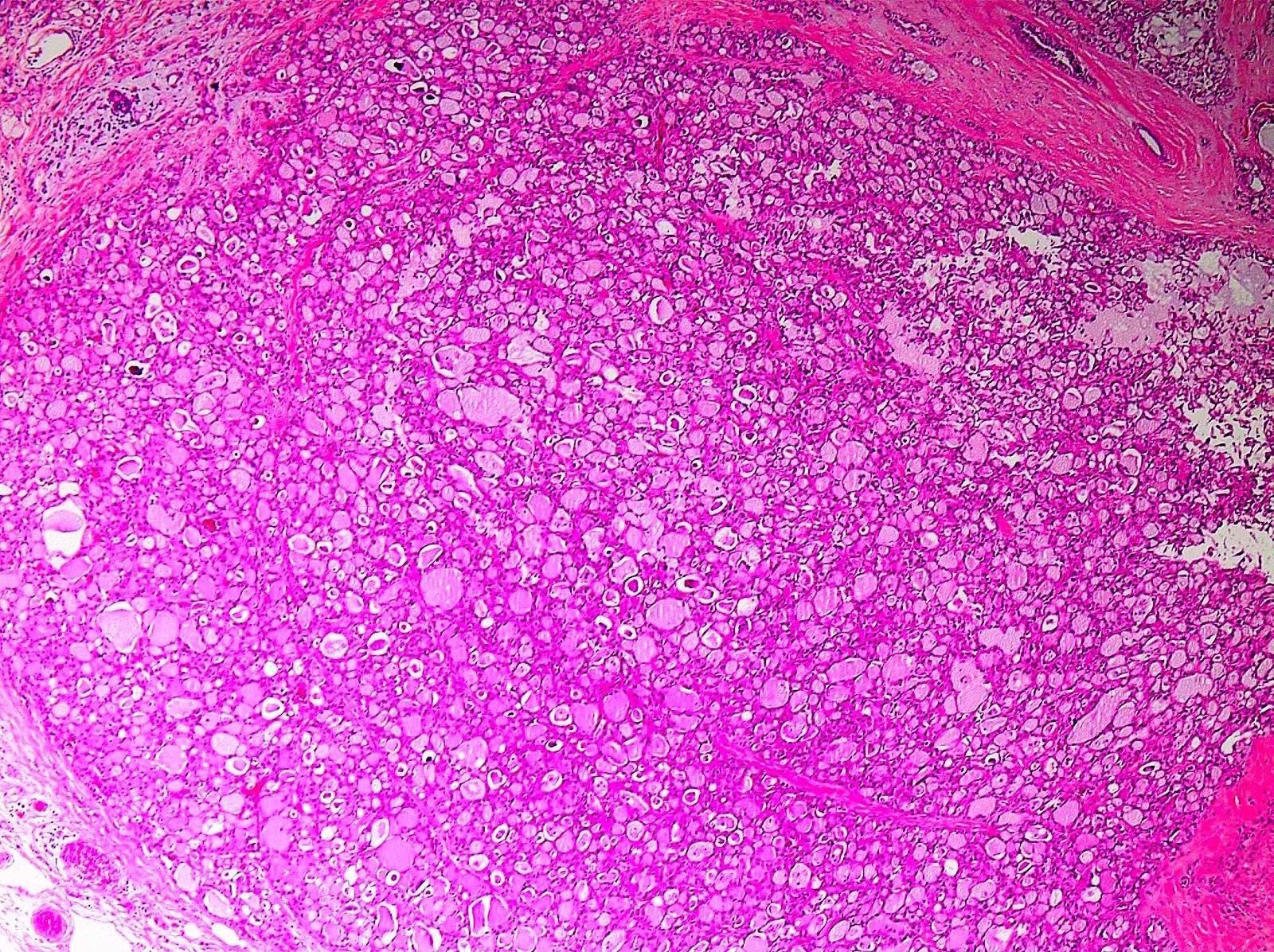
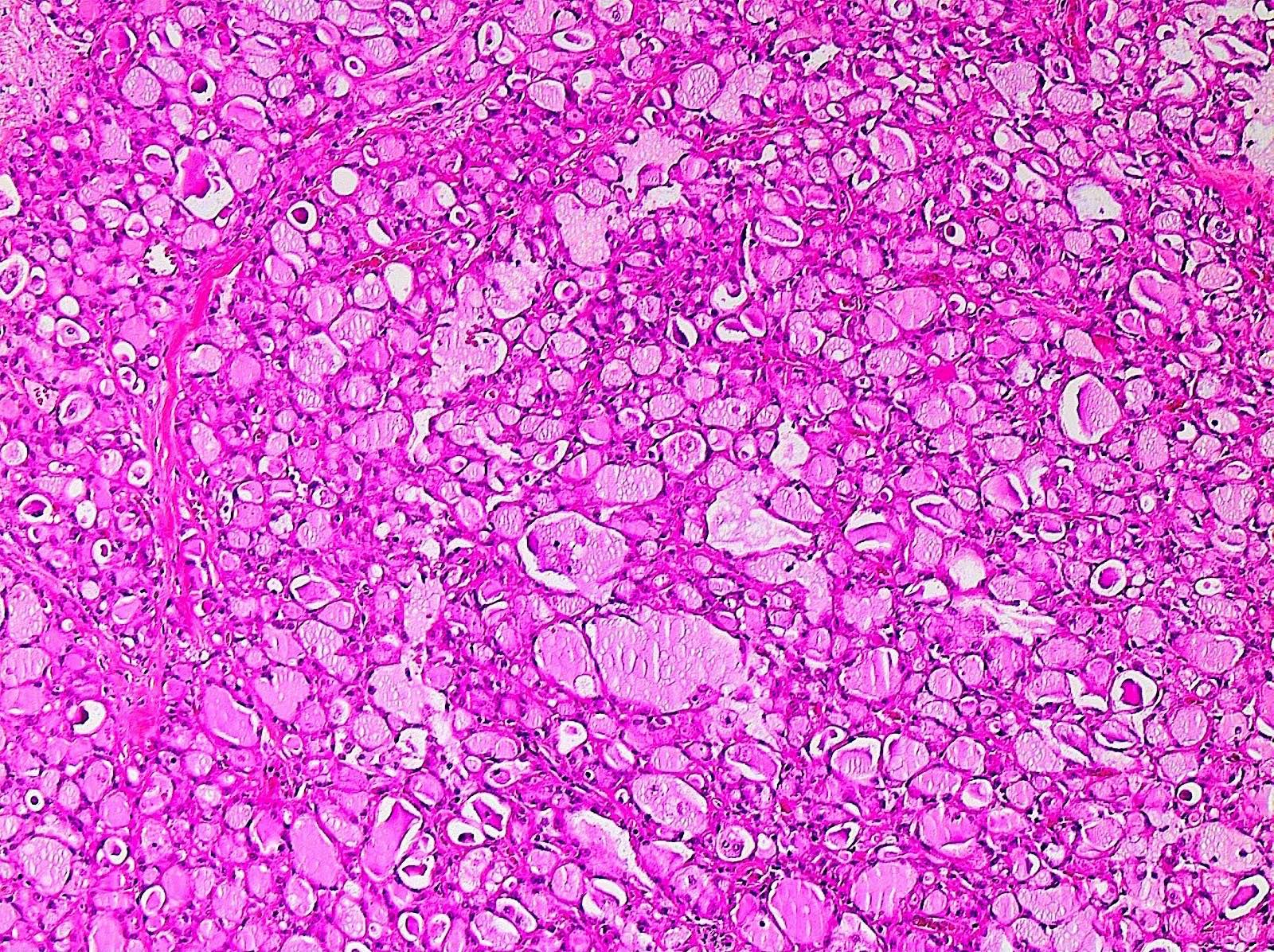
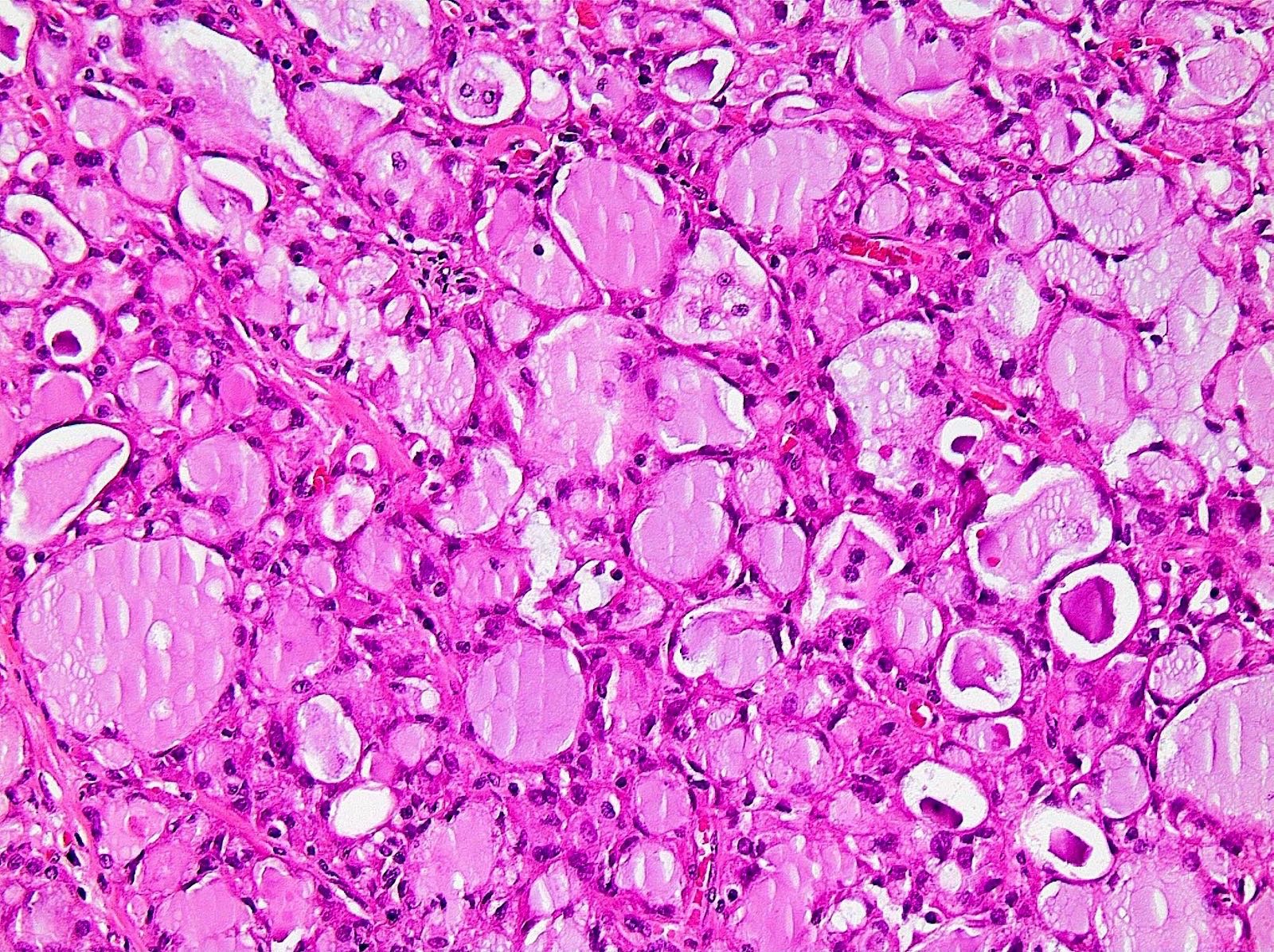
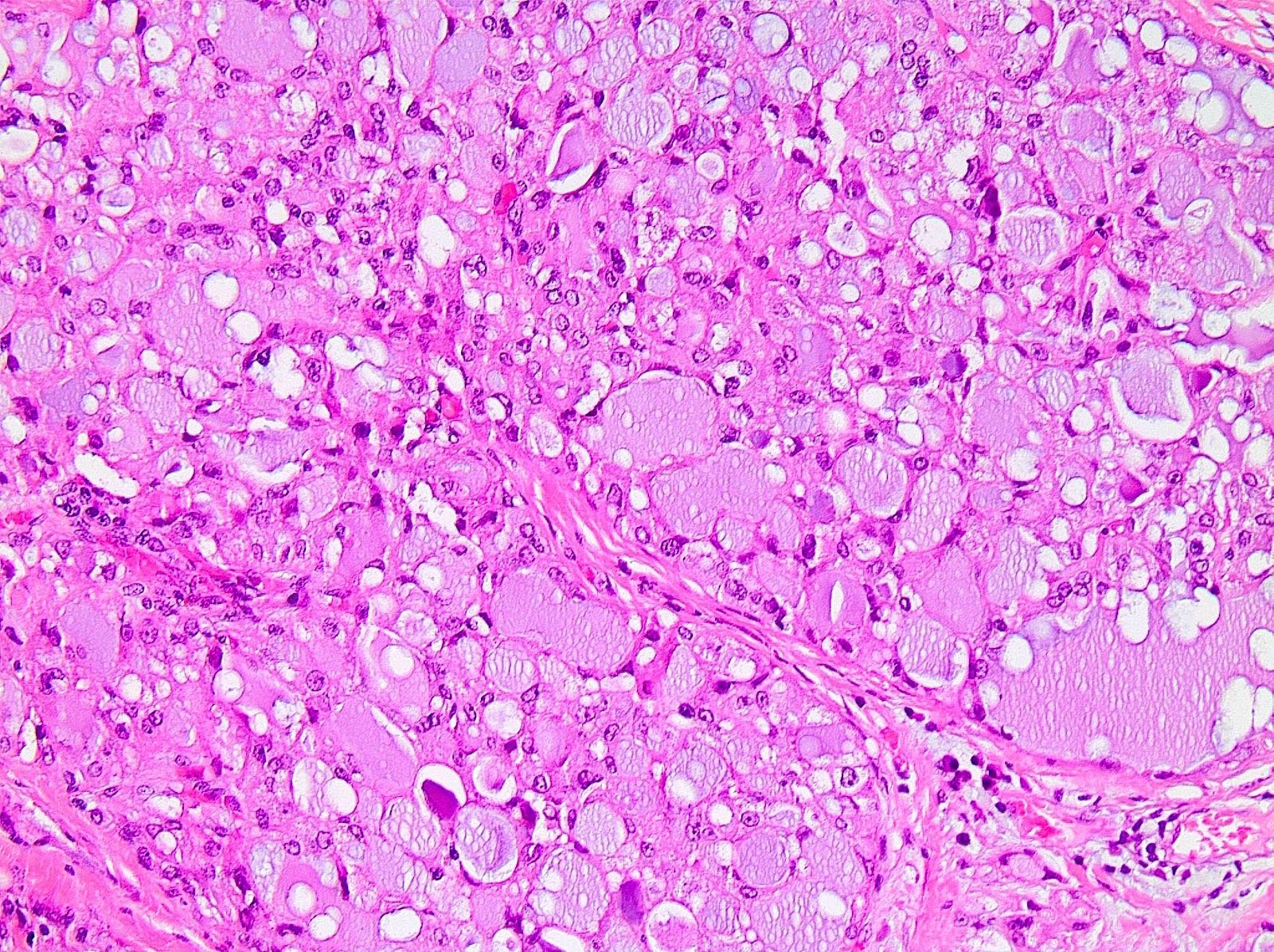
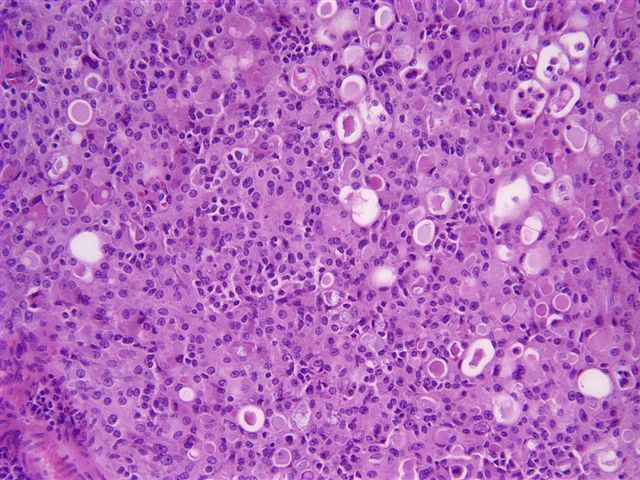
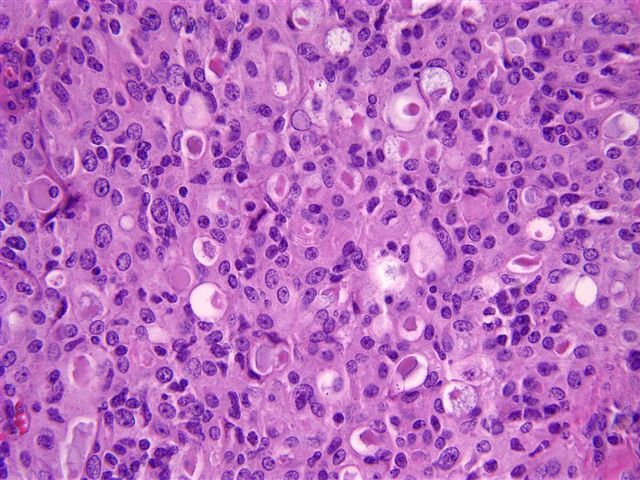
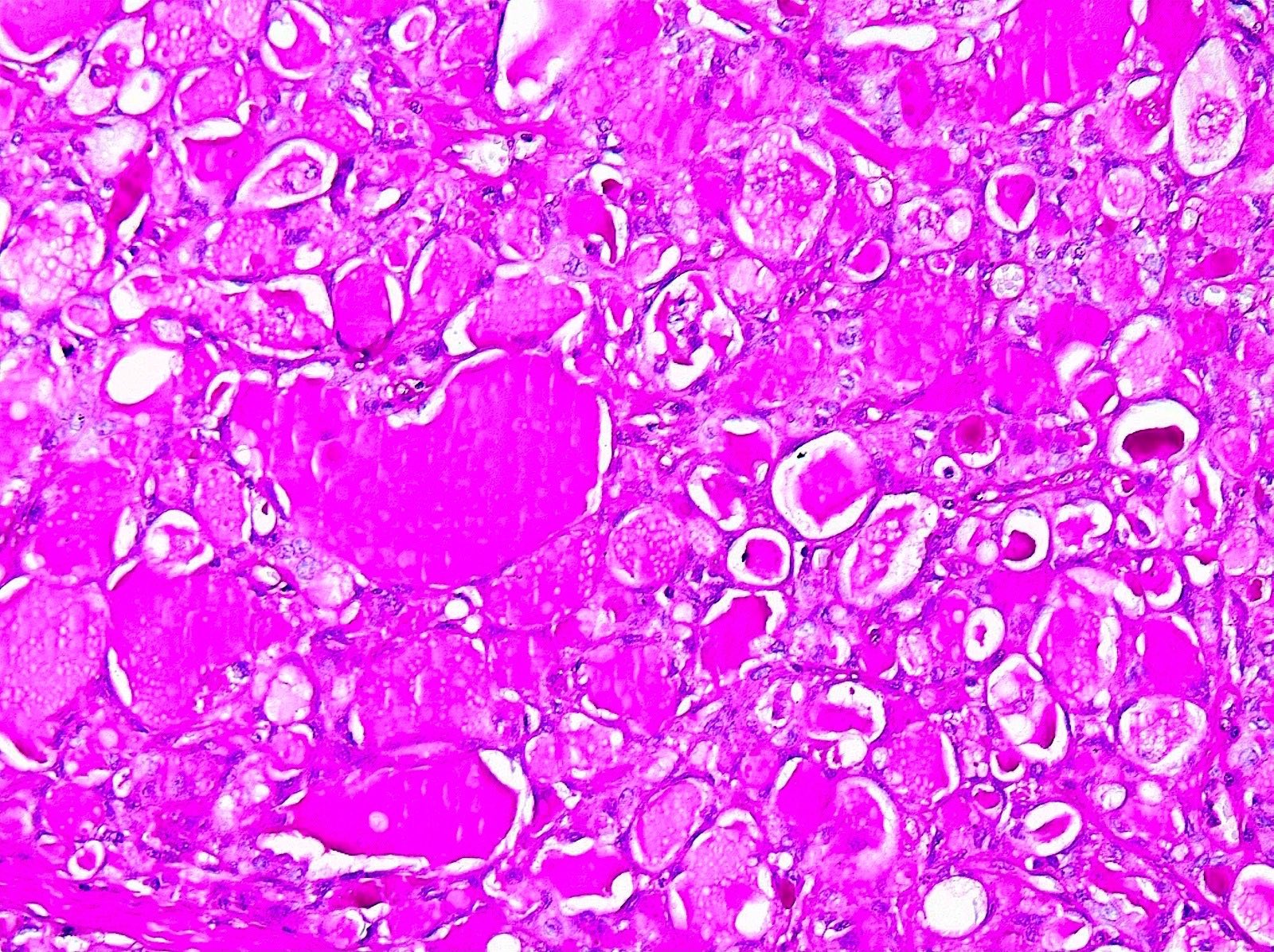
Microscopic (histologic) description
- Well circumscribed with pushing borders but may be infiltrative at periphery
- Central sclerosis may be observed
- Architecture is usually microcystic, solid or tubular or admixture of all 3 patterns
- Can display peripheral papillary architecture
- Low grade cytologic atypia, bland uniform nuclei, low mitotic rate
- Histologic hallmark is the presence of tumor cells with vacuolated, foamy cytoplasm and abundant intracellular and extracellular pale blue to dense pink secretions, which are periodic acid Schiff (PAS) positive and diastase resistant (JAMA 1966;195:388, Mod Pathol 2012;25:567)
- Often an in situ component (Mod Pathol 2009;22:291)
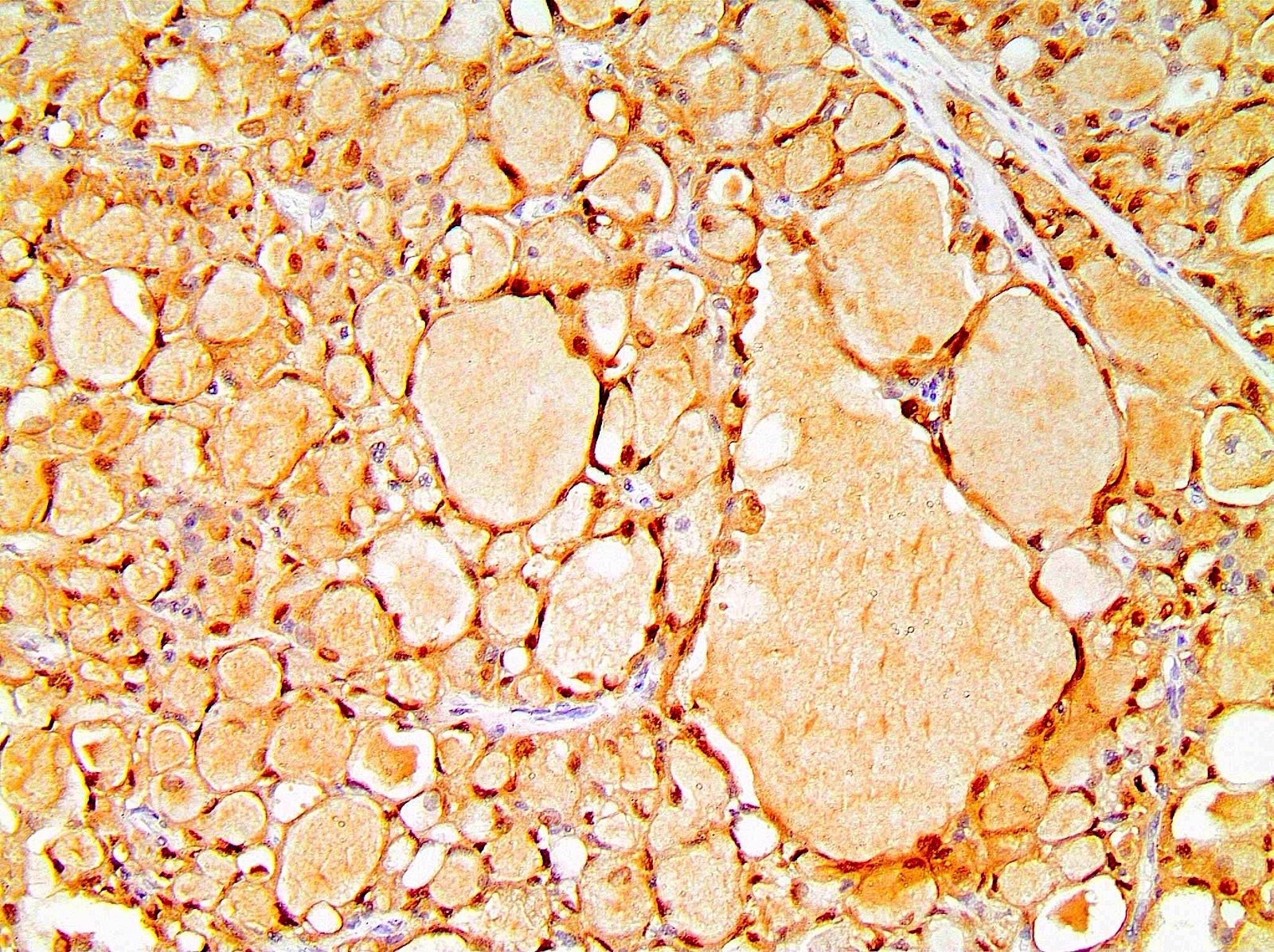
Microscopic (histologic) images
Positive stains
- S100, although expressed frequently in acinic cell carcinoma and in 30% of invasive ductal carcinoma, NOS, so not useful for these differentials (Mod Pathol 2012;25:567, Mod Pathol 2009;22:291)
- CK5/6, EGFR (Mod Pathol 2012;25:567, Mod Pathol 2017;30:1086)
- CK14 in 33% (Mod Pathol 2009;22:291)
- CD117 (focal) (Mod Pathol 2009;22:291)
- MUC4, SOX10 (Mod Pathol 2017;30:1086)
- GATA3 (Mod Pathol 2017;30:1086)
- PAS (periodic acid Schiff) positive and diastase resistant
Negative stains
- Triple negative or focal / weak (44 - 64%) for ER, PR and HER2 (Mod Pathol 2012;25:567, Mod Pathol 2017;30:1086, J Surg Oncol 2016;113:721, Am J Surg Pathol 2015;39:1458, Hum Pathol 2003;34:1299)
- p63 (Mod Pathol 2009;22:291)
Molecular / cytogenetics description
- Associated with chromosomal translocation t(12;15)(p13;q25), resulting in ETV6-NTRK3 fusion gene in 95% of cases (J Pediatr Surg 2000;35:765, Cancer Cell 2002;2:367, Genes Chromosomes Cancer 2004;40:152, World J Surg Oncol 2005;3:35, Mod Pathol 2017;30:1086, Histopathology 2019;75:213)
- Lacks the complex genomic alterations such as high mutational burden, frequent copy number alterations or TP53 mutations seen in conventional basal-like triple negative breast cancers (Mod Pathol 2017;30:1086, Am J Surg Pathol 2015;39:1458)
- Lacks chromosomal alterations 1q gains and 16q losses seen in low grade neoplasia pathway (Mod Pathol 2017;30:1086)
- Amplification of 16p13.3, TERT promoter mutation, loss of 9p21.3 locus, reported in cases with aggressive clinical course (Histopathology 2019;75:213)
Molecular / cytogenetics images
Sample pathology report
- Breast, right, 3:00, ultrasound guided core biopsy:
- Secretory carcinoma, 0.7 cm in greatest length
- Estrogen receptor: negative (0%)
- Progesterone receptor: negative (0%)
- HER2: negative (score 0)
Differential diagnosis
- Acinic cell carcinoma:
- Cells with clear cytoplasm (hypernephroid pattern)
- Expresses proteins of the salivary gland counterpart of acinic cell carcinoma (e.g. alpha-1-chymotrypsin, salivary gland amylase, lysozyme)
- Lacks the t(12;15) translocation
- Invasive ductal carcinoma, NOS:
- Lacks vacuolated cytoplasm and secretions
- Typically conventional triple negative breast cancer (TNBC) is high grade, not cytologically bland as in secretory carcinoma
- Cystic hypersecretory hyperplasia:
- Cysts containing abundant, homogenous intraluminal secretions resembling thyroid colloid
- Cells lining cysts are bland, flat or cuboidal / columnar cells lacking vacuolated / granular cytoplasm
- Presence of intact myoepithelial cell layer
- Glycogen rich carcinoma:
- PAS positive, diastase sensitive secretions
- Can demonstrate any grade of nuclear atypia
- Lipid rich carcinoma:
Additional references
Board review style question #1
Board review style answer #1
C. Secretory carcinoma of breast is associated with t(12;15)(p13;q25), resulting in ETV6-NTRK3 fusion gene
Comment Here
Reference: Secretory carcinoma of breast
Comment Here
Reference: Secretory carcinoma of breast
Board review style question #2
What histological and immunophenotypic features are most likely to be observed in a breast secretory carcinoma?
- Abundant PAS+, diastase sensitive secretions
- High grade cytologic atypia with brisk mitotic activity
- Irregular clusters of epithelial cells floating in pools of extracellular mucin
- Low grade cytologic atypia, triple negative for ER, PR and HER2
- Negative for basal-like markers CK5/6 or CK14
Board review style answer #2
D. Secretory carcinoma of breast is most likely to show low grade cytologic atypia, triple negative for ER, PR and HER2
Comment Here
Reference: Secretory carcinoma of breast
Comment Here
Reference: Secretory carcinoma of breast