Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Clinical features | Interpretation | Uses by pathologists | Prognostic factors | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive staining - normal | Positive staining - disease | Negative staining | Sample pathology report | Board review style question #1 | Board review style answer #1Cite this page: Li JJX, Tse GM. Hormone receptors. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/breastmalignanthormonereceptors.html. Accessed April 1st, 2025.
Definition / general
- The most clinically important hormone receptors in breast cancer are estrogen, progesterone, and to a lesser extent, androgen receptors
- Hormone receptor status is strongly associated with histology, prognosis and treatment response
Essential features
- Clinically used hormone receptor markers for breast cancers include estrogen, progesterone and androgen receptors
- Expression of hormone markers is associated with favorable prognostic features and less aggressive histologic features
- Estrogen and progesterone expression select breast cancer patients for hormone therapy
Terminology
- Estrogen receptor alpha
- ERα is the routinely used marker in a clinical setting
- Predictive value in prognostication and treatment response is better established in ERα compared to ERβ (Biomark Res 2020;8:39)
- ER immunostain usually refers to ERα unless otherwise specified
Pathophysiology
- General
- The hormone receptors most commonly expressed in breast cancers are for sex steroid hormones (estrogen, progesterone and androgen), which are involved in breast cancer behavior and treatment (Breast 2013;22:S38)
- These hormones activate nuclear receptors involved in gene transcription and directly control cellular functions (Cold Spring Harb Perspect Biol 2013;5:a016709)
- Glucocorticoid receptor also expressed in breast cancers but is not commonly used in clinical settings (Int J Mol Sci 2021;22:4446)
- Estrogen receptor (ER)
- 2 subtypes: ERα and ERβ
- ERα
- ER subtype that is assessed in breast cancer typing, prognostication and treatment decision
- ER immunostain usually refers to ERα unless specified
- Expressed in breast epithelium and > 70% of breast cancers (Clin Cancer Res 2019;25:1970)
- Promotes carcinogenesis through oxidative damage and induces proliferation and inhibits apoptosis in breast cancer (N Engl J Med 2006;354:270)
- ERβ
- Discovered after ERα, as the second estrogen receptor (Proc Natl Acad Sci U S A 1996;93:5925)
- Expressed in breast epithelium, myoepithelium and 20 - 30% of breast cancers (Breast Cancer Res Treat 2020;179:241)
- Isoforms ERβ1, ERβ2 and ERβ5 are important in breast cancer with prognostic associations (Clin Cancer Res 2008;14:5228)
- ERβ inhibits epithelial to mesenchymal transition and exerts antiproliferative effects in breast cancers (Mol Cell Endocrinol 2014;382:665)
- Progesterone receptor (PR)
- PR is dependent on estrogen for its expression, upregulated by ER and modulates the behavior of ER (Nature 2015;523:313)
- > 80% of ER positive breast cancers are PR positive; > 95% of PR positive breast cancers are ER positive (Breast Cancer Res 2007;9:R6)
- PR activity is implicated in tumor differentiation and chemotherapy resistance (Womens Health (Lond) 2008;4:151)
- Androgen receptor (AR)
- AR is positive in 73 - 88% of breast cancers and 41 - 55% of triple negative breast cancers (Ann Oncol 2011;22:1288, Am J Cancer Res 2014;4:353, PLoS One 2018;13:e0197827)
- AR exhibits tumor suppressive effects in ER positive breast cancers but may assert protumor effects in triple negative breast cancers (Nat Med 2021;27:310, Breast Cancer Res Treat 2010;123:139)
- Not currently used in routine breast marker assessment since an independent prognostic value has not been established and lacks approved androgen related therapy for breast cancers (Molecules 2020;25:358)
Clinical features
- Estrogen receptor
- Older average age of presentation in ER positive breast cancers (Breast Cancer Res Treat 2002;74:199)
- ER positivity is associated with smaller tumor size and lower risk of lymph node metastasis (Breast Cancer Res 2007;9:R6)
- Expression of AR and PR are correlated with ER and demonstrate similar associations with demographic and disease parameters (Asian Pac J Cancer Prev 2012;13:5047, Appl Immunohistochem Mol Morphol 2016;24:550)
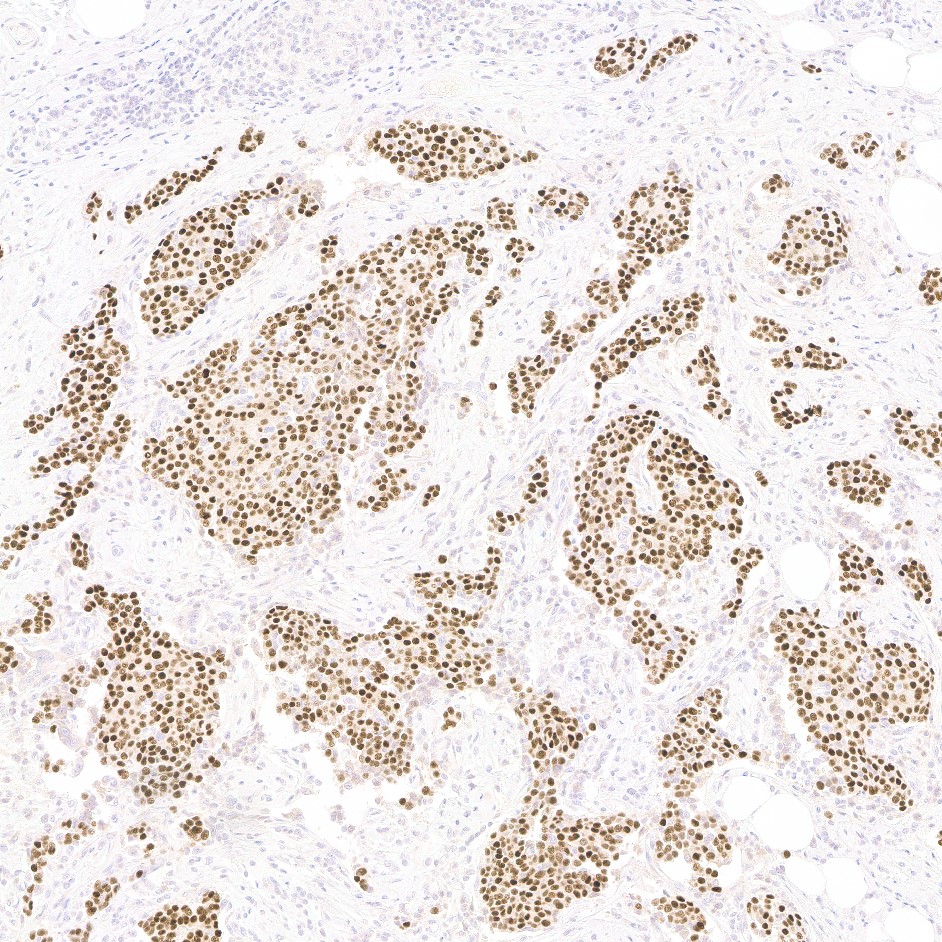
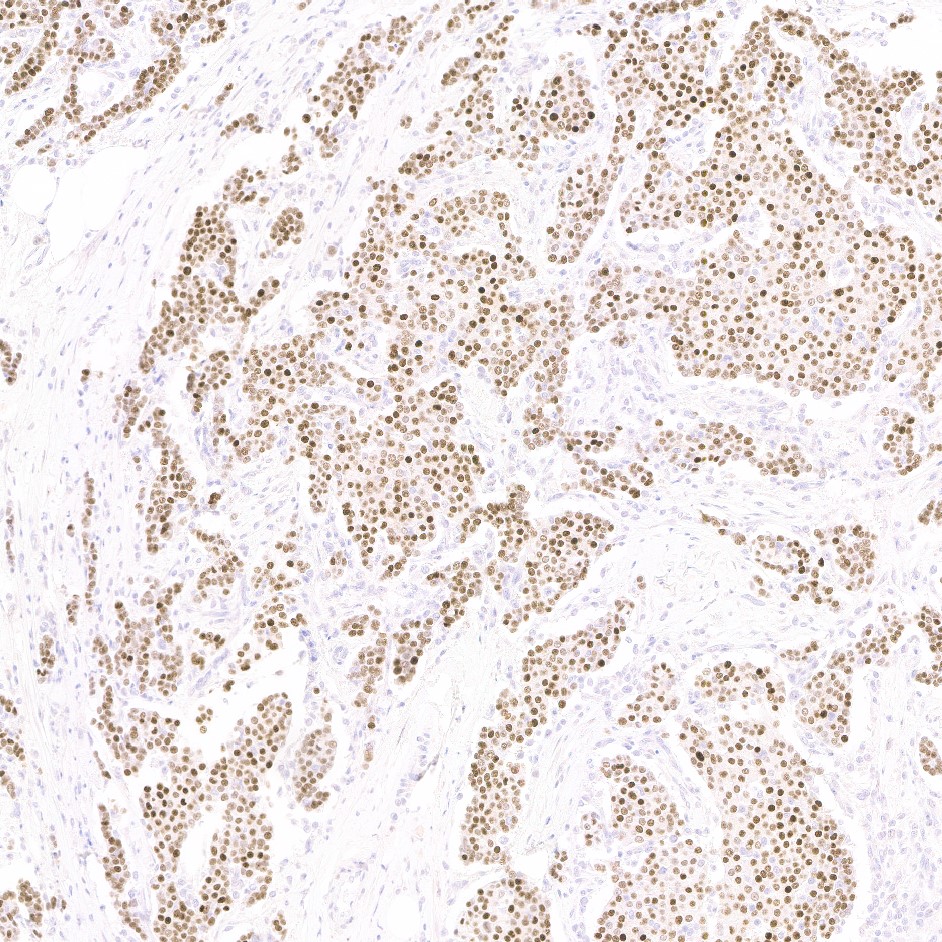
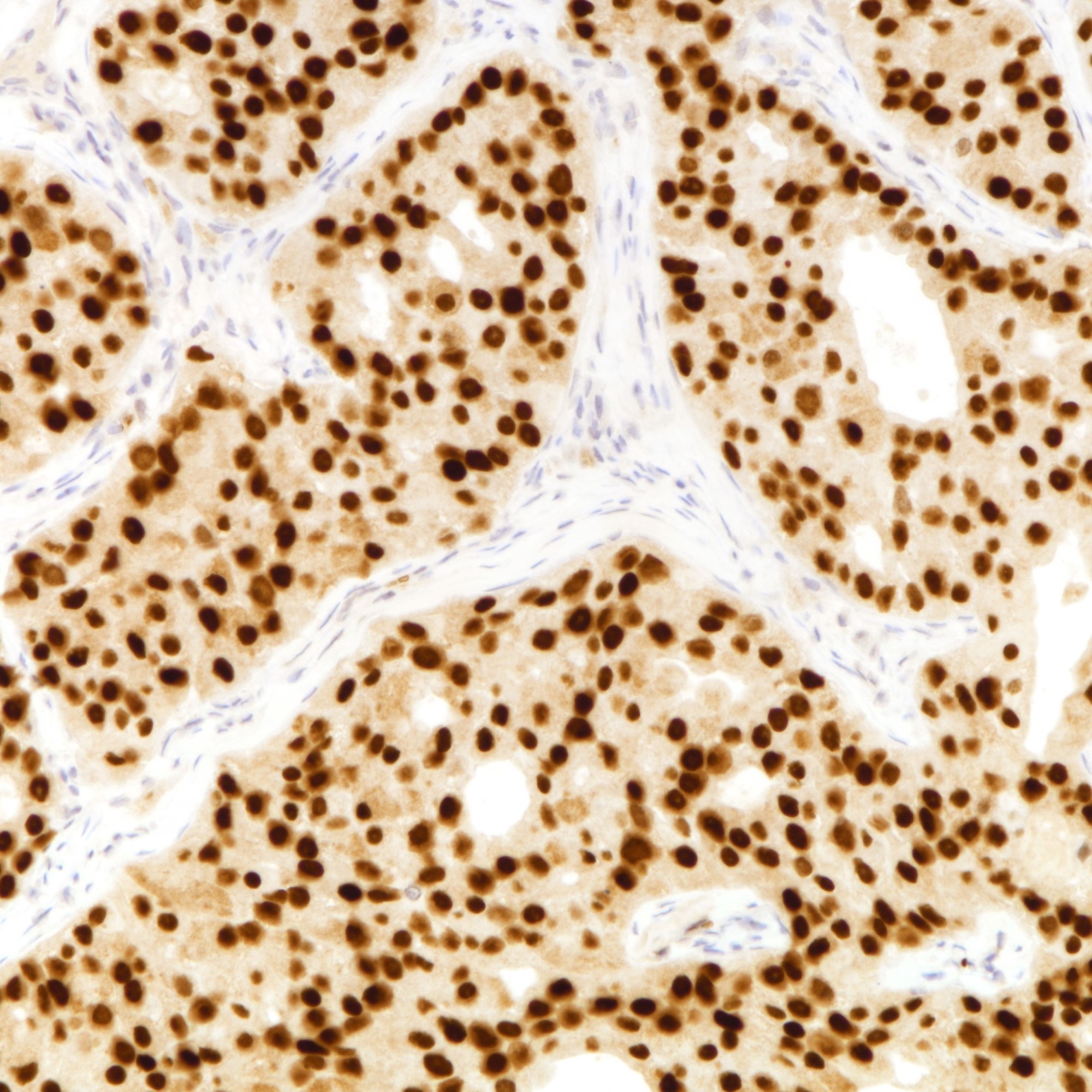
Interpretation
- Estrogen, progesterone and androgen receptors are nuclear stains
- Interpretation of ER and PR outlined by ASCO / CAP guideline on estrogen and progesterone receptor testing in breast cancer (J Clin Oncol 2020;38:1346)
- Staining is considered positive regardless of intensity
- Reported as percentage of tumor nuclei positive (0 - 100%)
- 1 - 100% staining considered as positive, < 1% staining considered as negative
- ER low positive category (1 - 10% staining) introduced in the latest ASCO / CAP Guideline
- Other scoring methods (Ann Oncol 2013;24:47)
- Allred score
- Summation of proportion (0 - 5) and intensity (0 - 3) of ER positive tumor cells into a score of 0 to 8 out of 8
- Proportion
- 0: 0%
- 1: < 1%
- 2: 1 - 10%
- 3: 11 - 33%
- 4: 34 - 66%
- 5: > 66%
- Intensity
- 0: negative
- 1: weak
- 2: moderate
- 3: strong
- Scores 0 and 2 interpreted as negative; scores 3 to 8 interpreted as positive
- H score
- Score of 0 to 300 from multiplying proportion as percentage (0 - 100) and intensity (0 - 3) of ER positive tumor cells
- % of tumor cells with weak staining x 1 + % of tumor cells with moderate staining x 2 + % of tumor cells with strong staining x 3
- Allred score
- Pitfalls in ER and PR assessment are not uncommon and should be avoided (Pathobiology 2022 Mar 4 [Epub ahead of print])
- Positive staining in nonneoplastic or entrapped breast tissue, proliferative and in situ lesions should be excluded
- Prolonged cold ischemia time can decrease ER and PR expression
- ER and PR antigenicity are also sensitive to tissue processing, fixation protocol and decalcification
Uses by pathologists
- Routine assessment of breast cancer
- For prognostication of breast cancers
- Selecting ER positive breast cancers for hormonal therapy
- ER and PR are components of the surrogate classification for breast cancer subtyping (Breast 2016;29:181)
- ER / PR positivity indicates luminal-like breast cancers
- Differentiating hyperplastic and neoplastic breast lesions
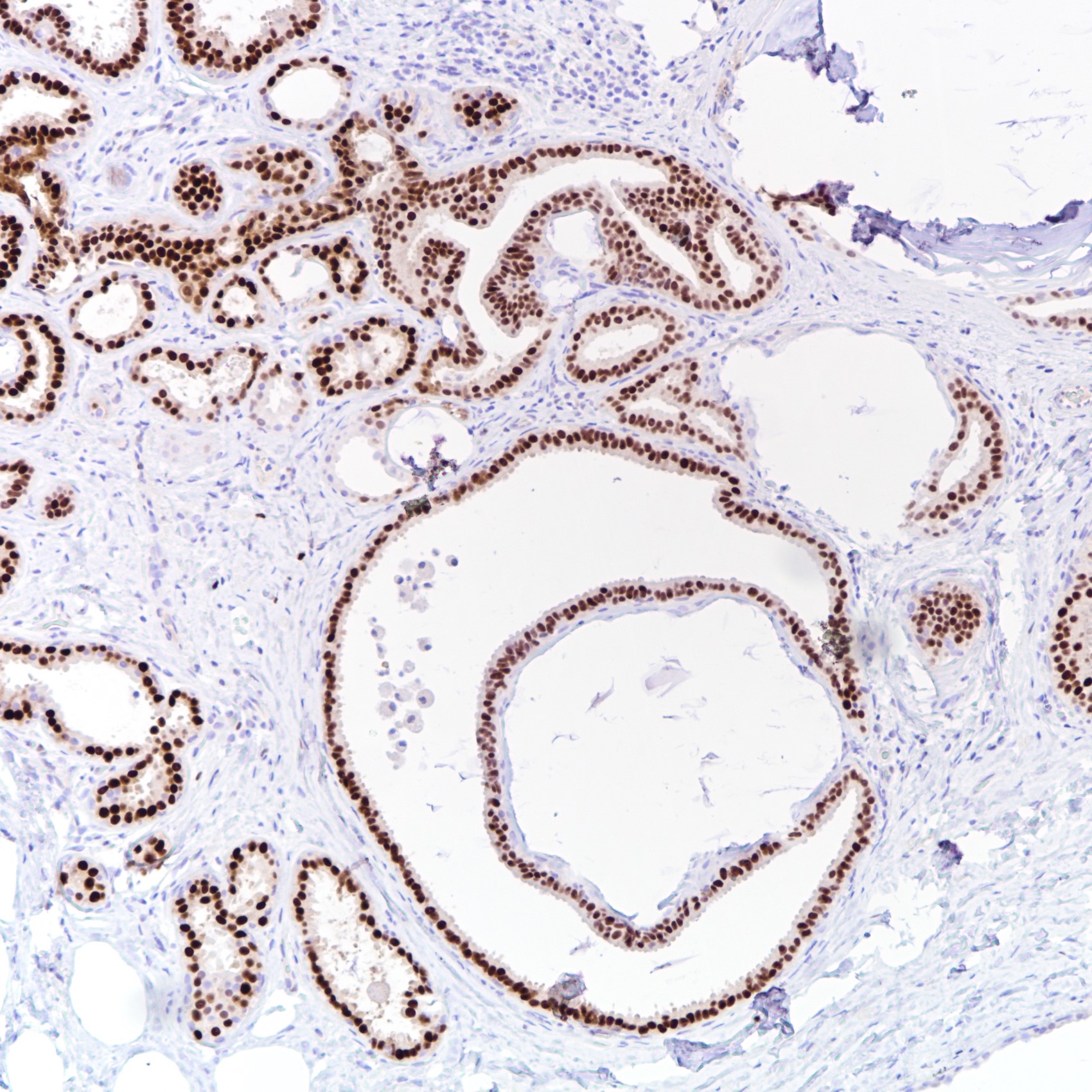
- Homogenous uniform ER staining indicates clonality and favors a neoplastic process (Mod Pathol 2010;23:S1)
- Homogenous uniform ER staining: columnar cell change, columnar cell hyperplasia, flat epithelial atypia, atypical ductal hyperplasia and carcinoma in situ
- Heterogenous ER staining: normal breast epithelium, usual ductal hyperplasia and florid epithelial hyperplasia
- AR can be used to demonstrate apocrine differentiation, usually with coexpression of GCDFP15 (Pathol Res Pract 1997;193:753, BMC Cancer 2014;14:546)
- Homogenous uniform ER staining indicates clonality and favors a neoplastic process (Mod Pathol 2010;23:S1)
- There are many other uses to ER and PR, including assessment of metastatic carcinomas and gynecological lesions
- These uses are not in the scope of this topic; please refer to estrogen receptor
Prognostic factors
- ERα
- ER is the primary marker used in selection of patients for hormone therapy and its expression is correlated with response to endocrine therapy (Tumori 2008;94:370)
- ER expression is an independent favorable prognostic factor for overall and disease specific survival (Cancer 2005;103:2241)
- Late recurrences, although uncommon, are more frequent in ER positive breast cancers (J Natl Cancer Inst 2022;114:391)
- ER low positive breast cancers behave more similarly to ER negative breast cancers, with worse outcomes and inferior response to hormonal therapy
- ERβ
- ERβ1 and ERβ2 associated with improved disease free and overall survival but no independent prognostic value over ERα (Oncotarget 2016;7:10373)
- Potential for selecting ERα negative breast cancers for ERβ selective agonists (Clin Breast Cancer 2016;16:256)
- Progesterone receptor
- PR expression is associated with improved clinical outcomes, independent from ER (Br J Cancer 2014;110:565)
- Androgen receptor
- Conflicting results on prognostic value of AR in breast cancers but unlikely to have independent predictive value over ER (Breast Cancer Res 2019;21:30, J Clin Med 2020;9:1083, Appl Immunohistochem Mol Morphol 2016;24:550)
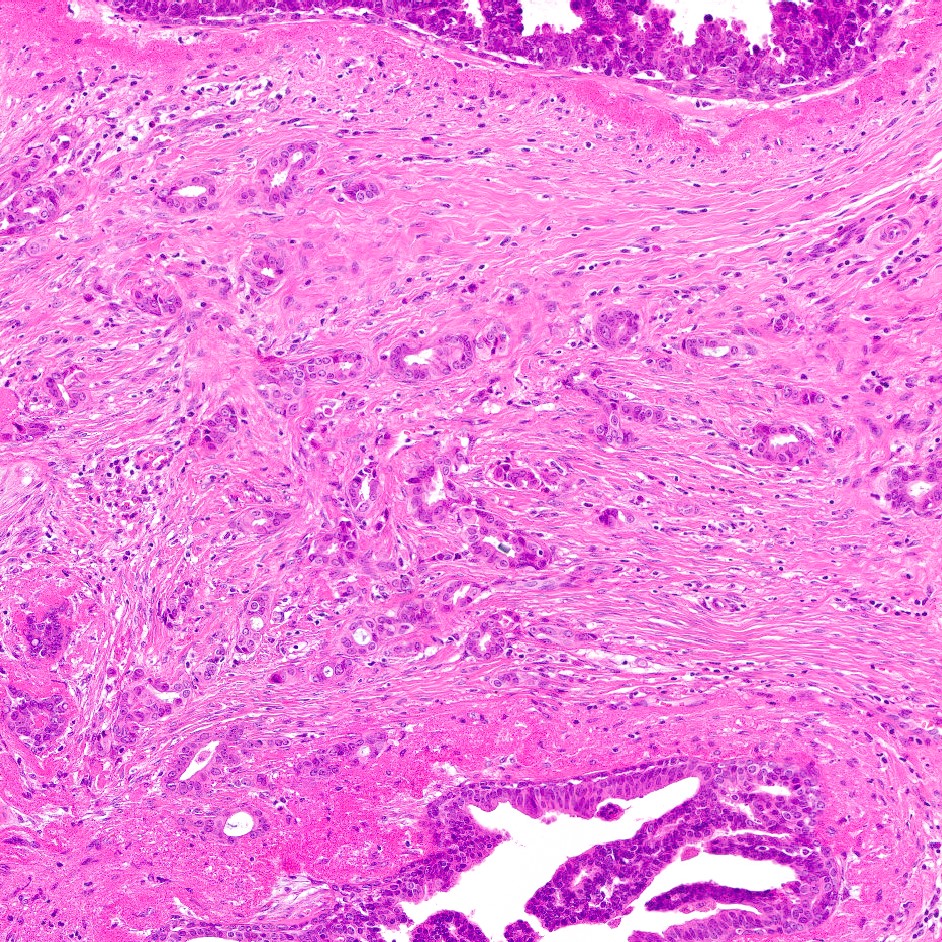
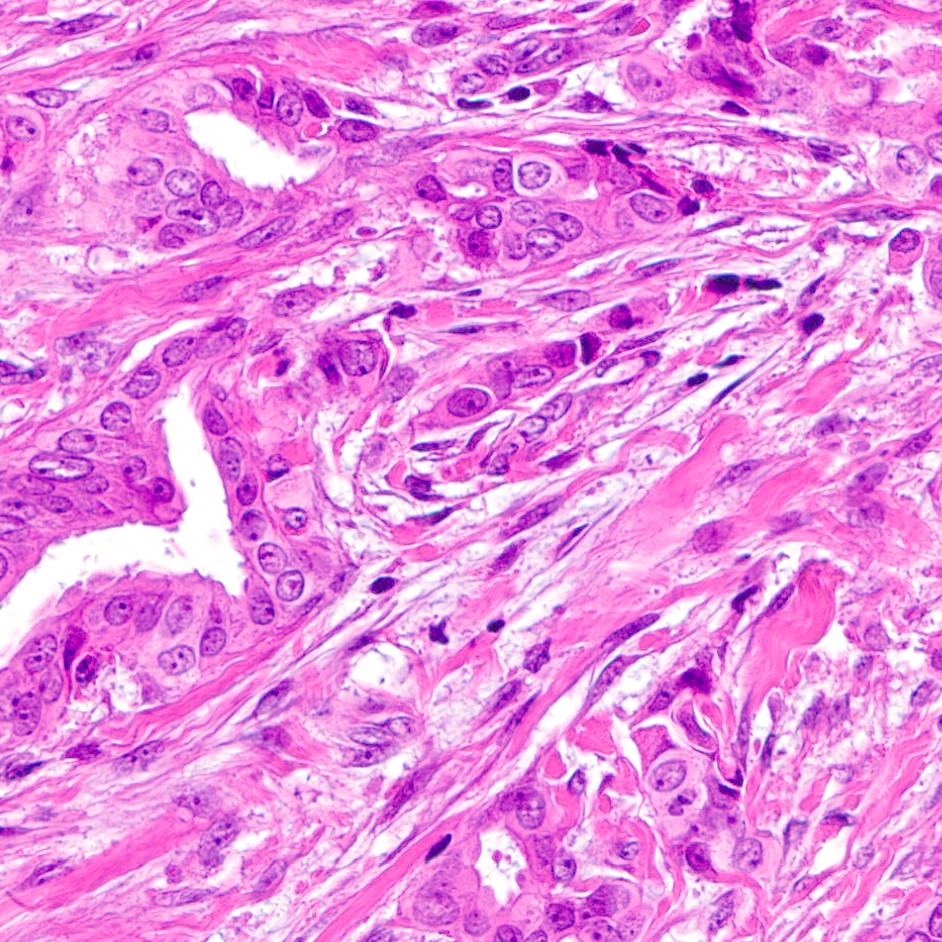
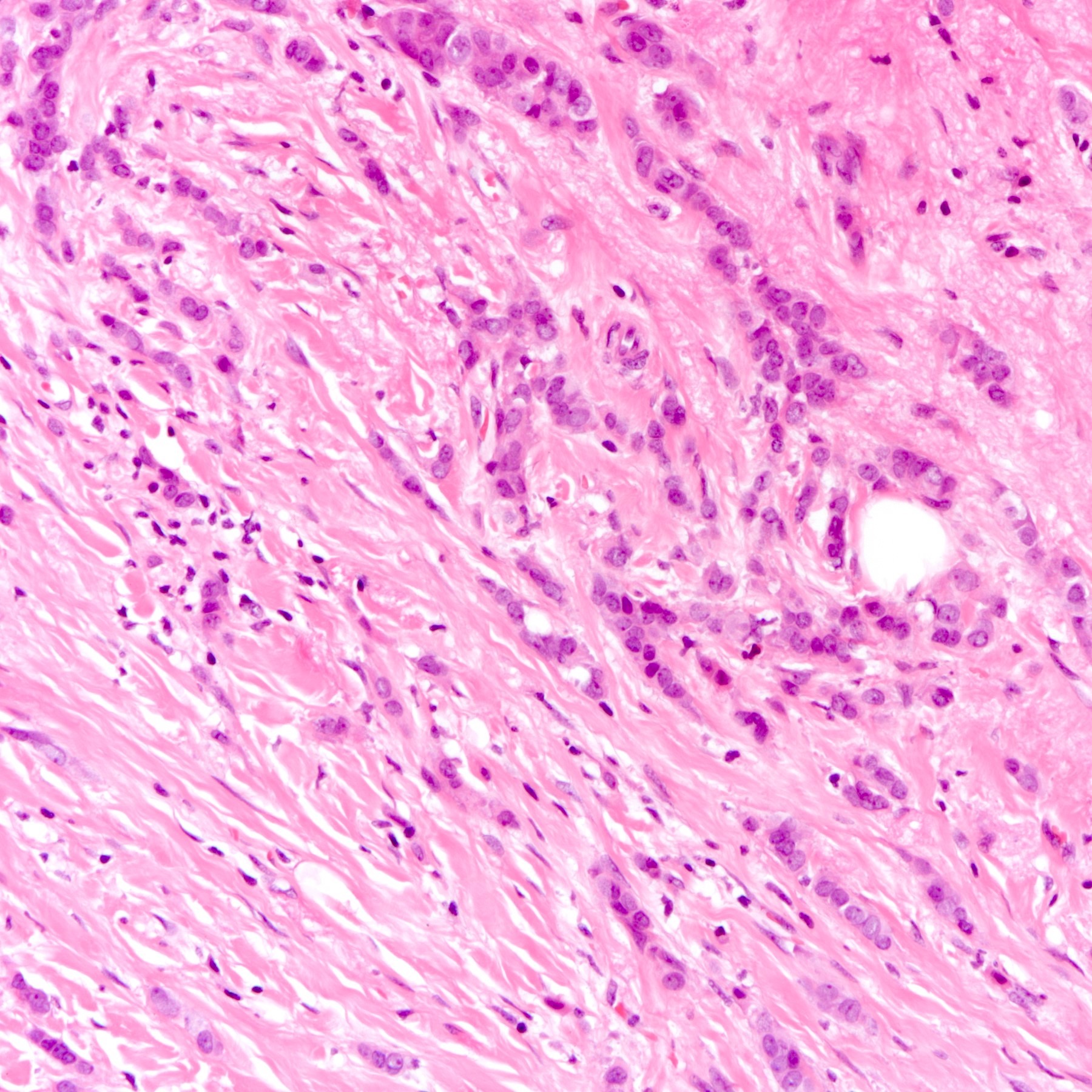
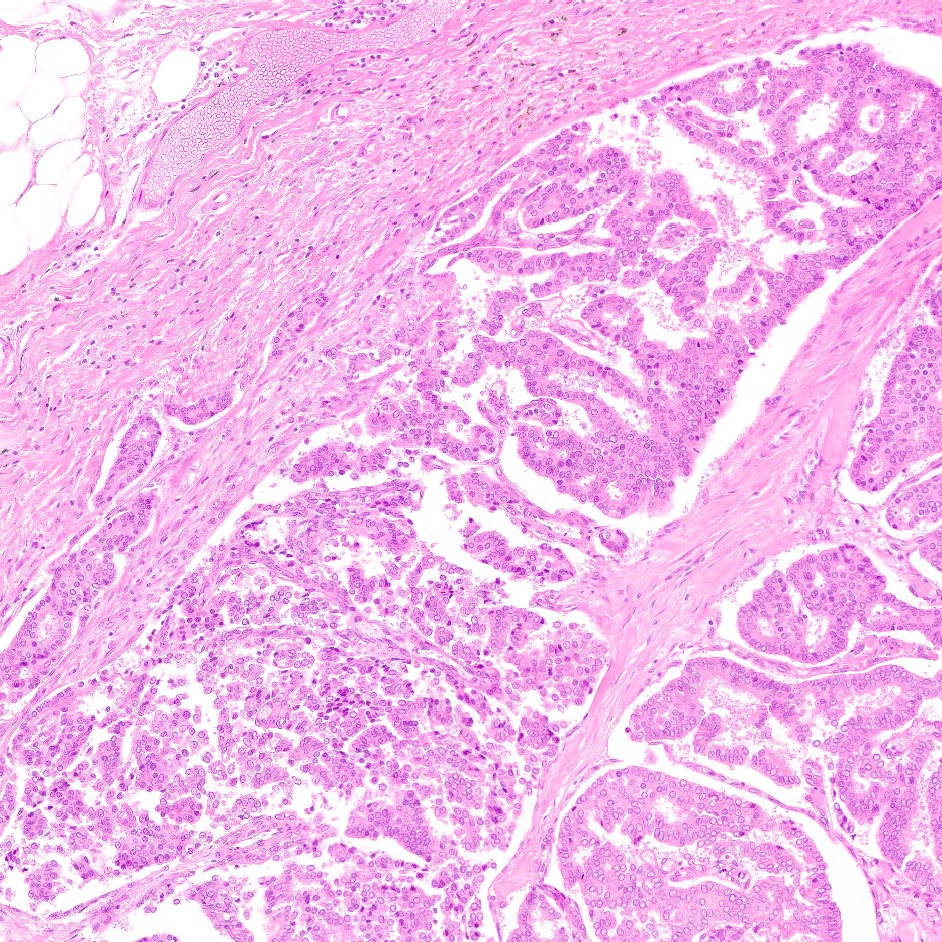
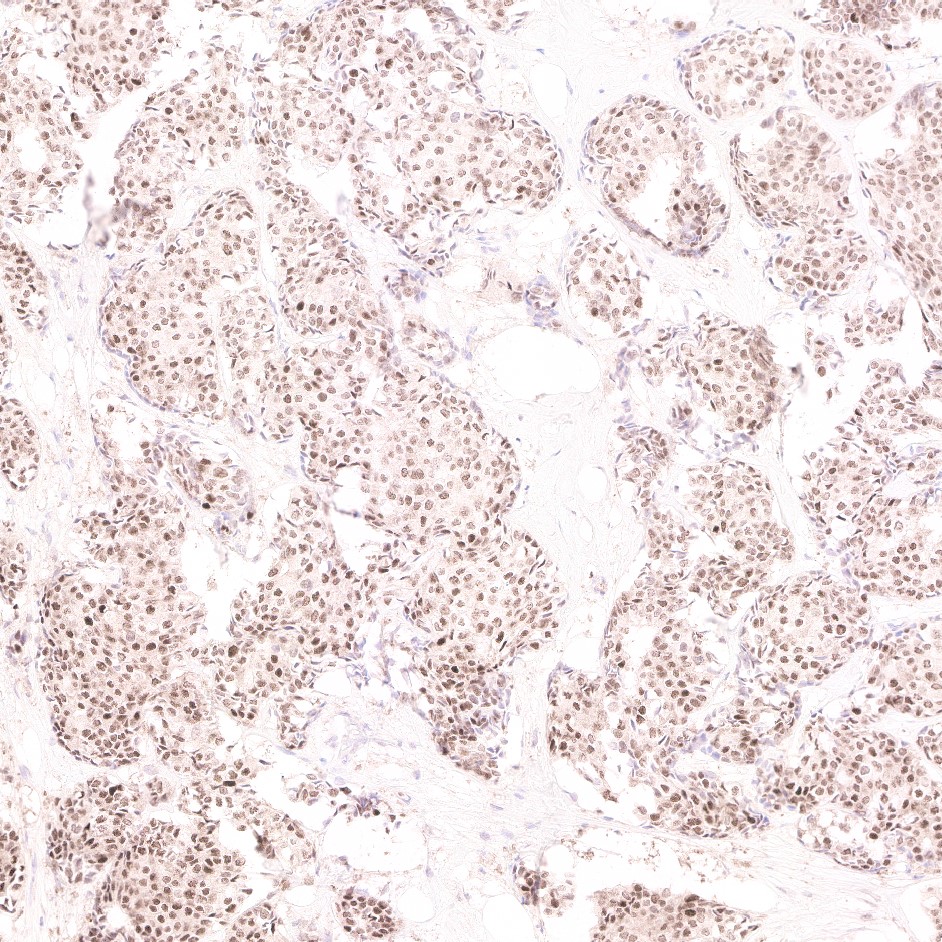
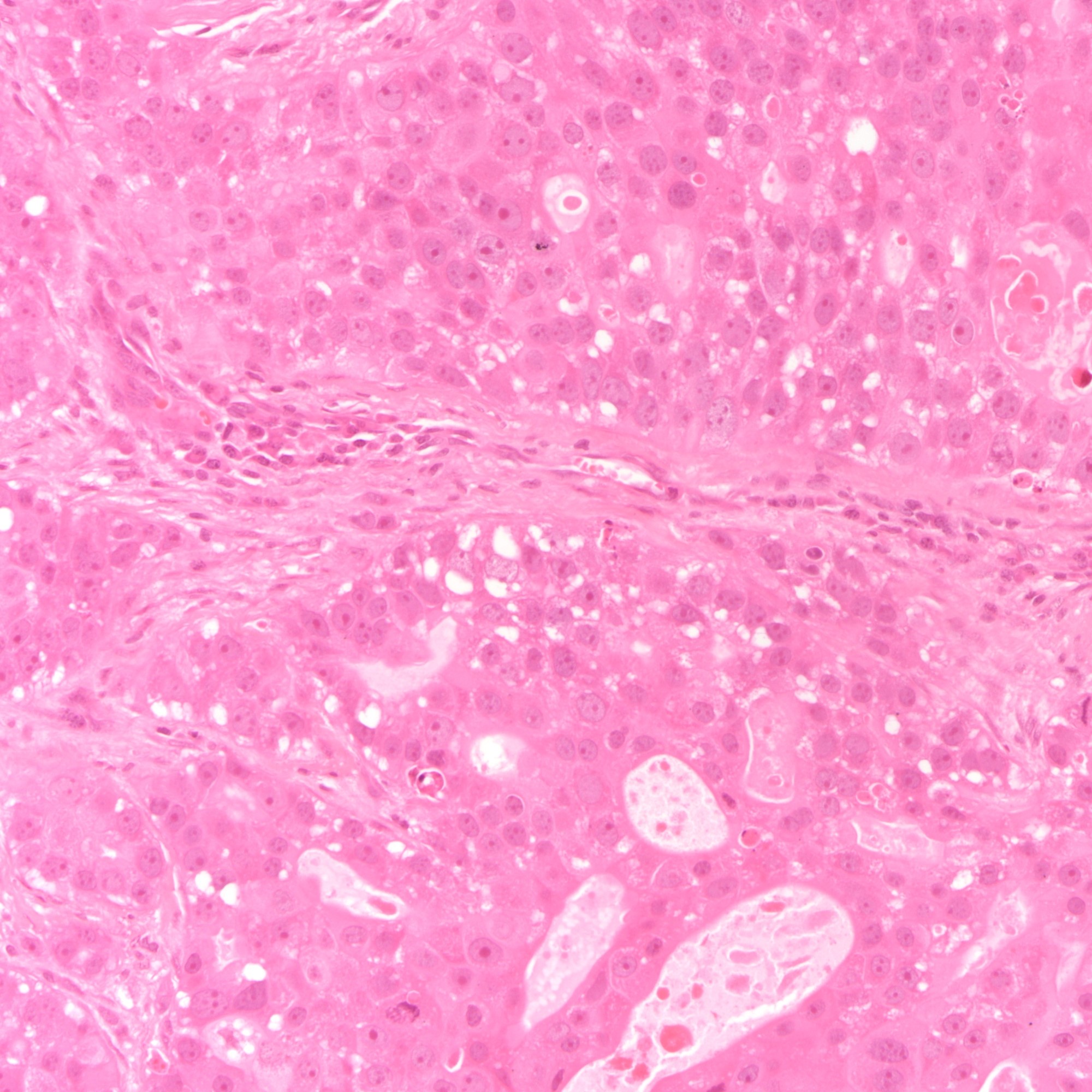
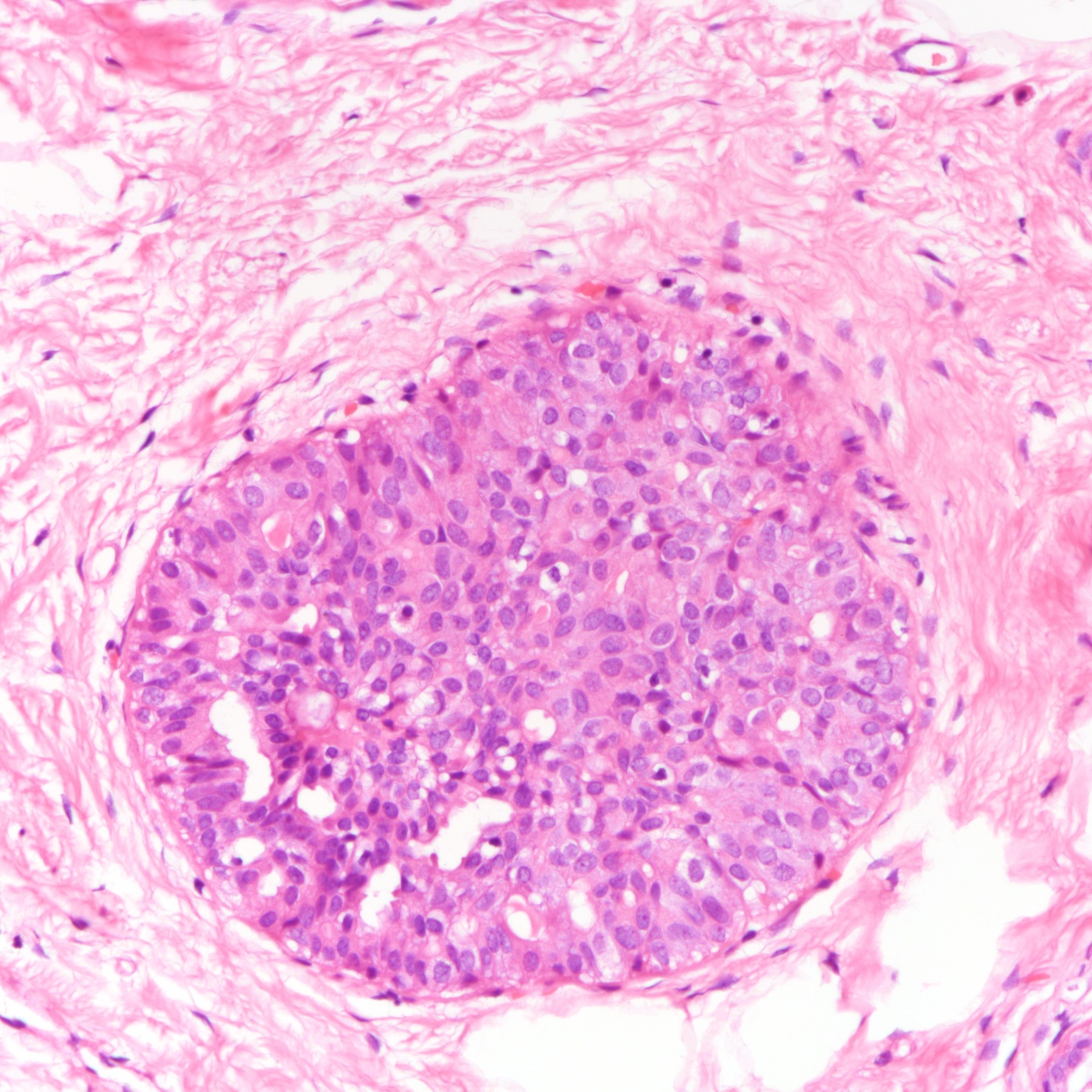
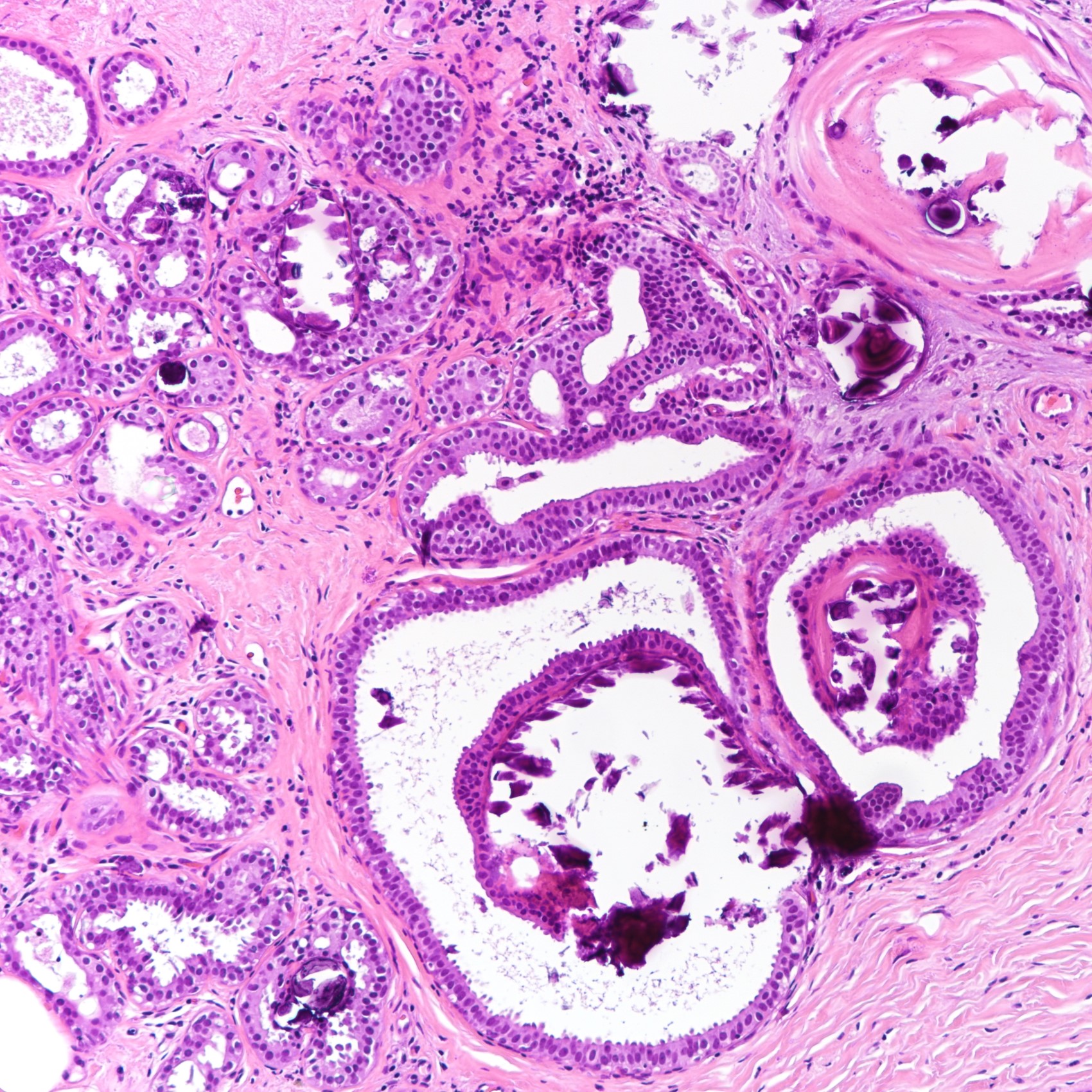
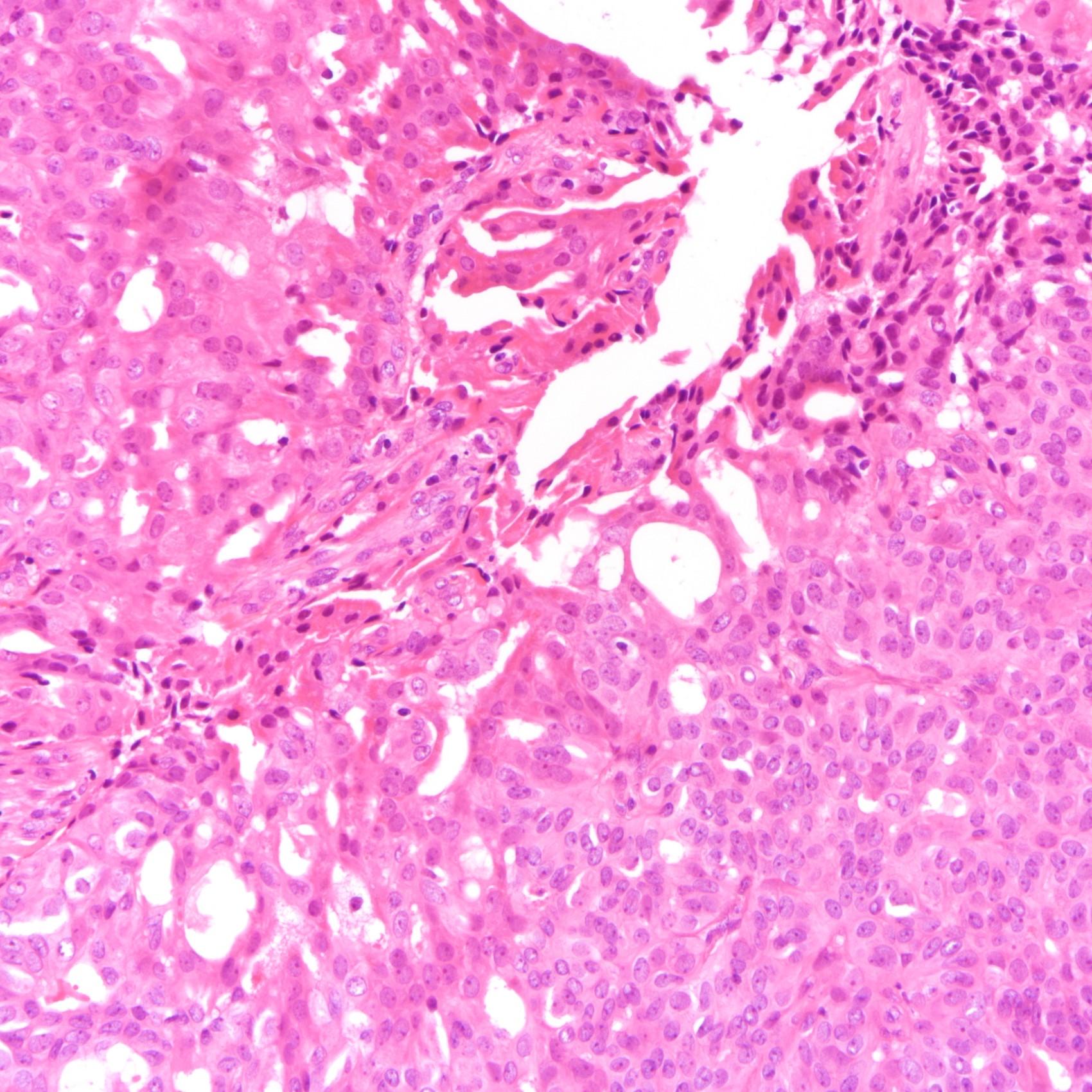
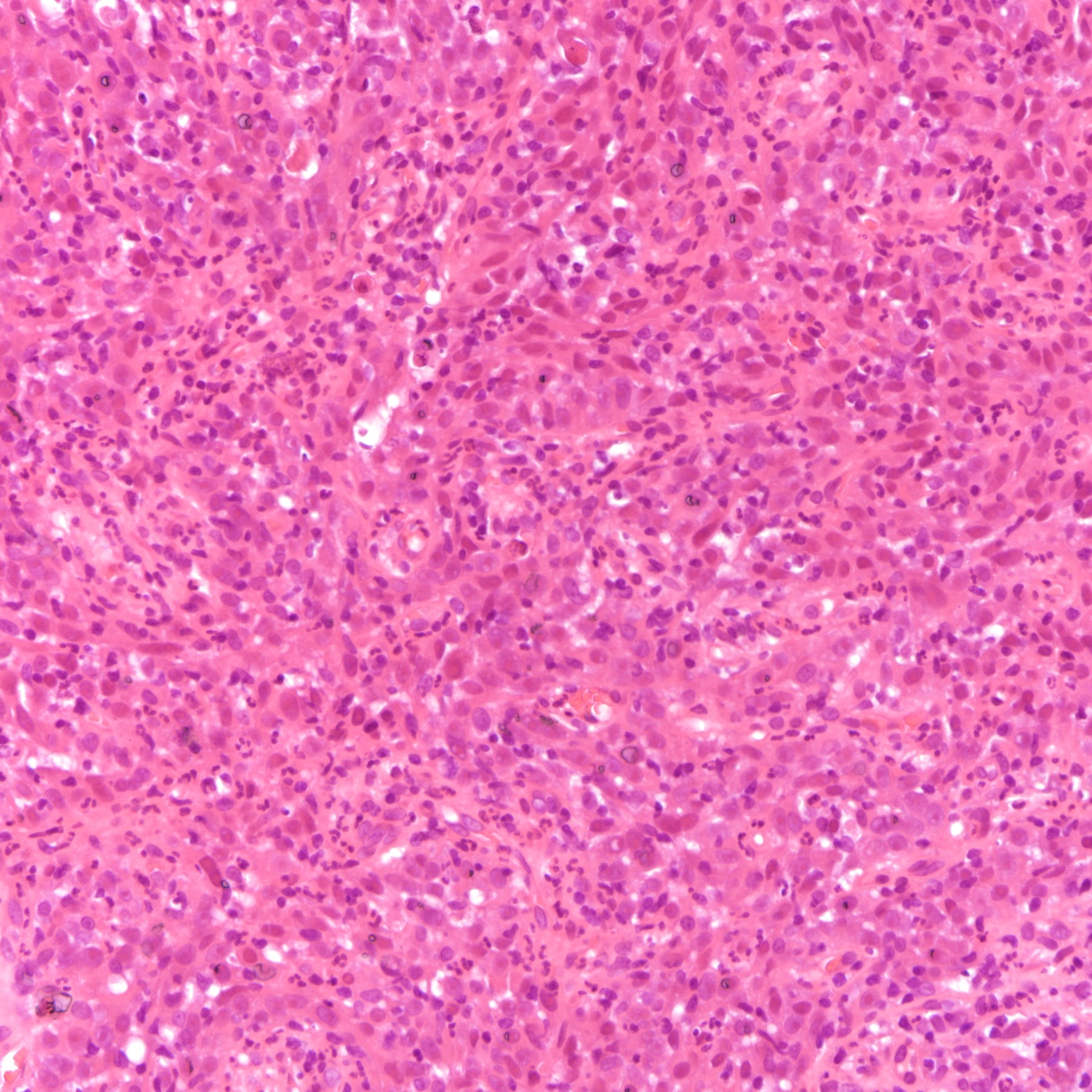
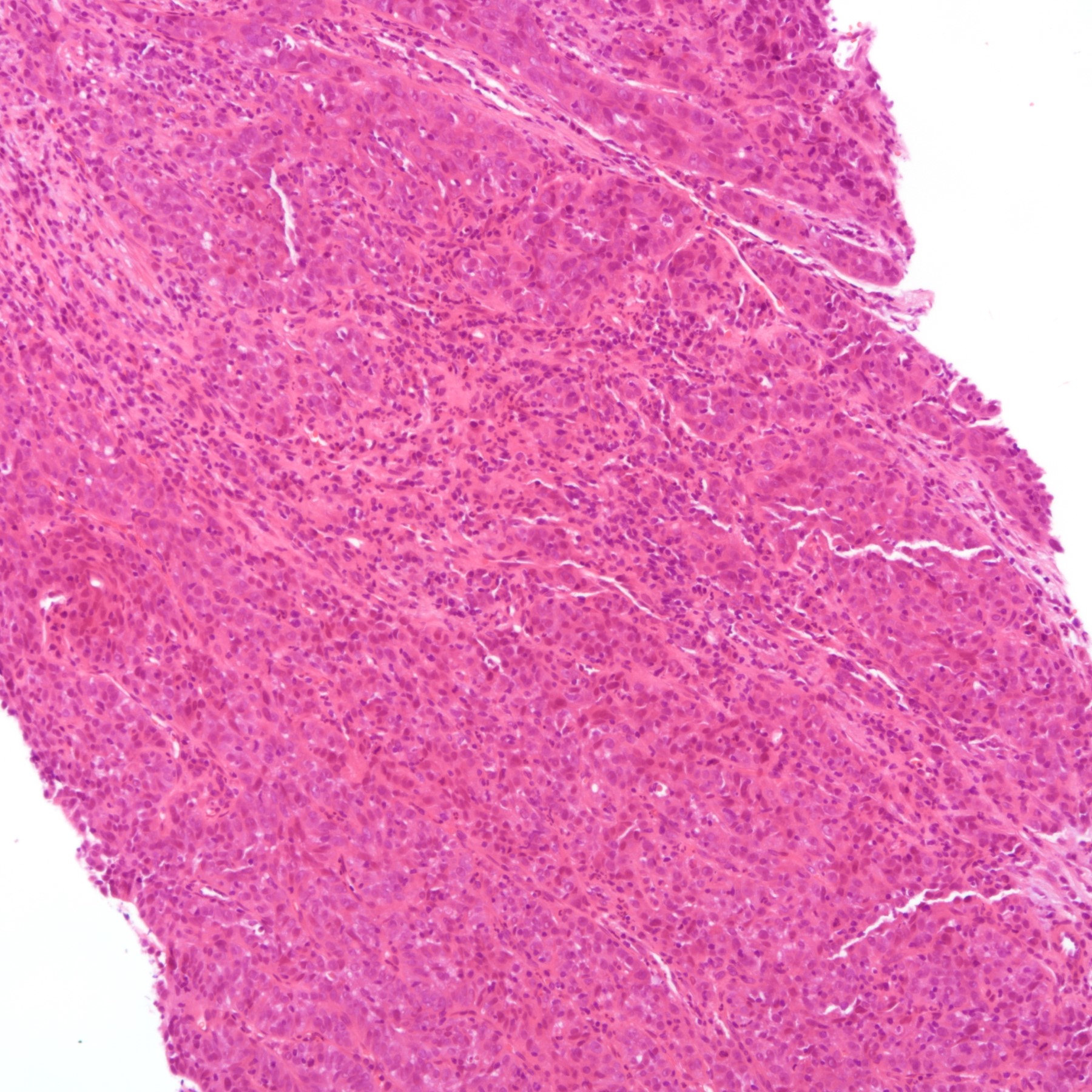
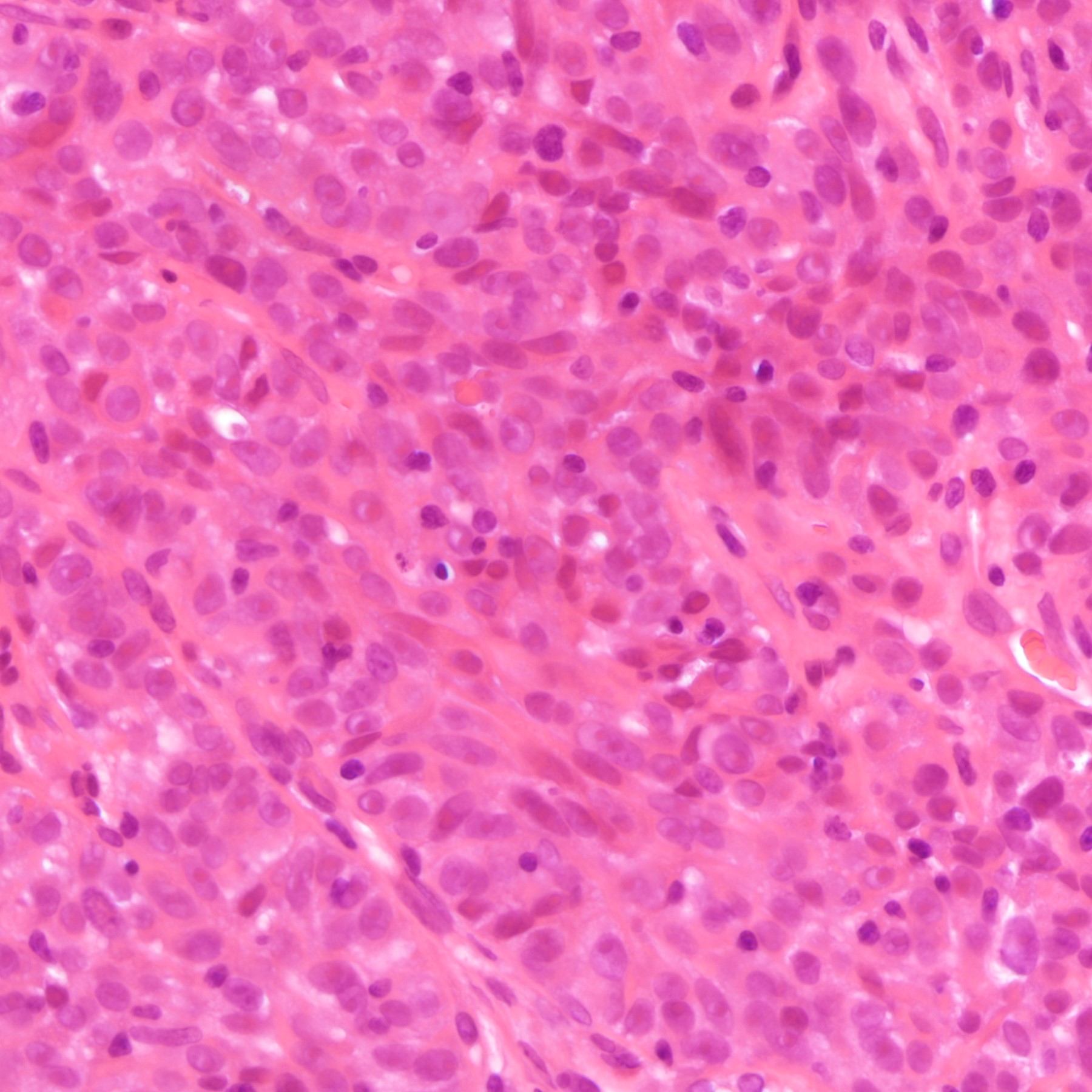
Microscopic (histologic) description
- The most common type of ER positive (and PR, AR positive breast cancers which are correlated with ER expression) breast cancer is low grade invasive breast carcinoma of no special type (IBC, NST) (Breast Care (Basel) 2020;15:327)
- Features include prominent tubule formation, mild nuclear pleomorphism and a low mitotic count
- Other histological features include fewer tumor infiltrating lymphocytes, less lymphovascular invasion and more fibrotic foci (Br J Cancer 2020;123:1223, Ann Surg Oncol 2013;20:2842)
- Special types of breast cancer which are commonly ER positive include lobular, micropapillary, mucinous, papillary and tubular carcinomas (Breast Care (Basel) 2020;15:327)
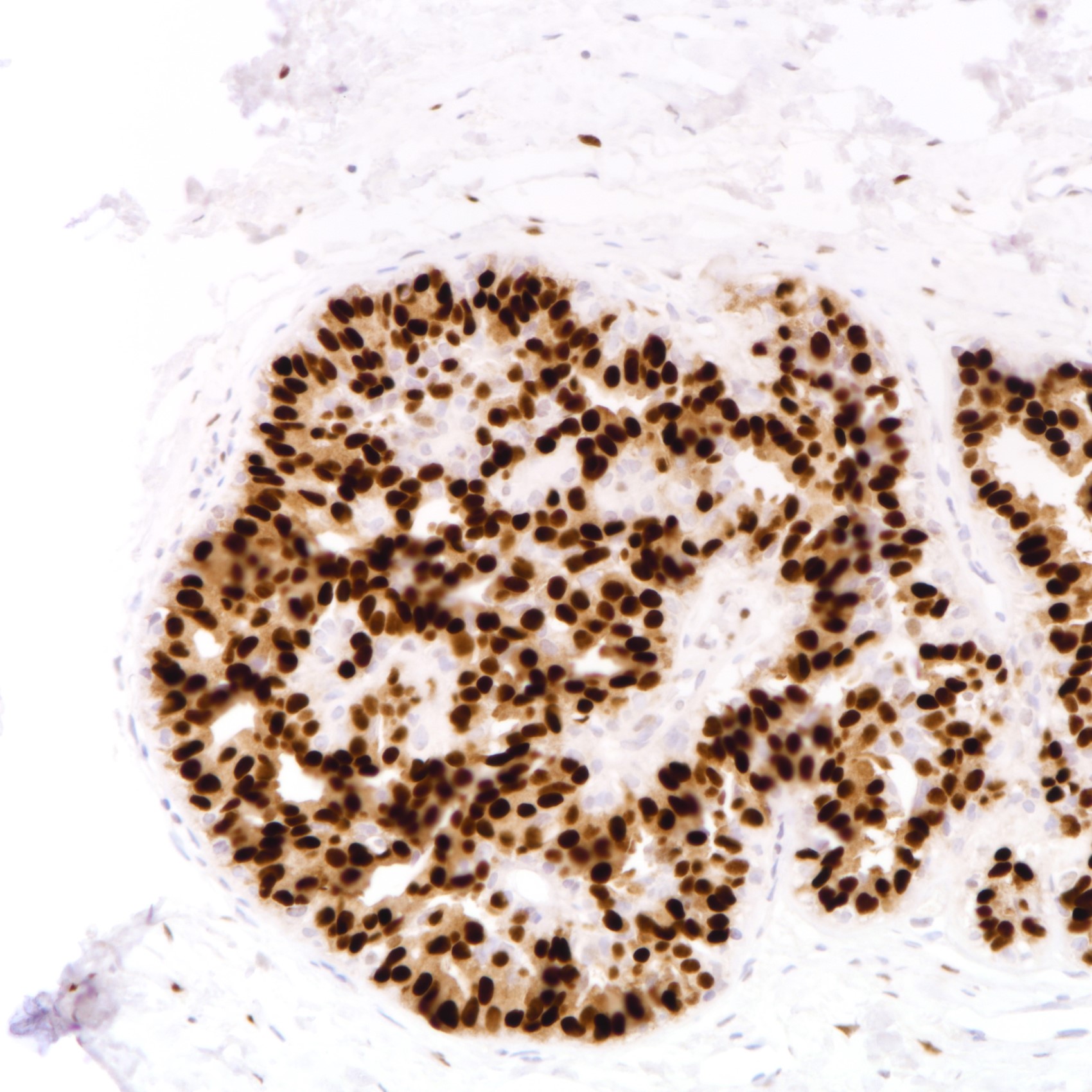
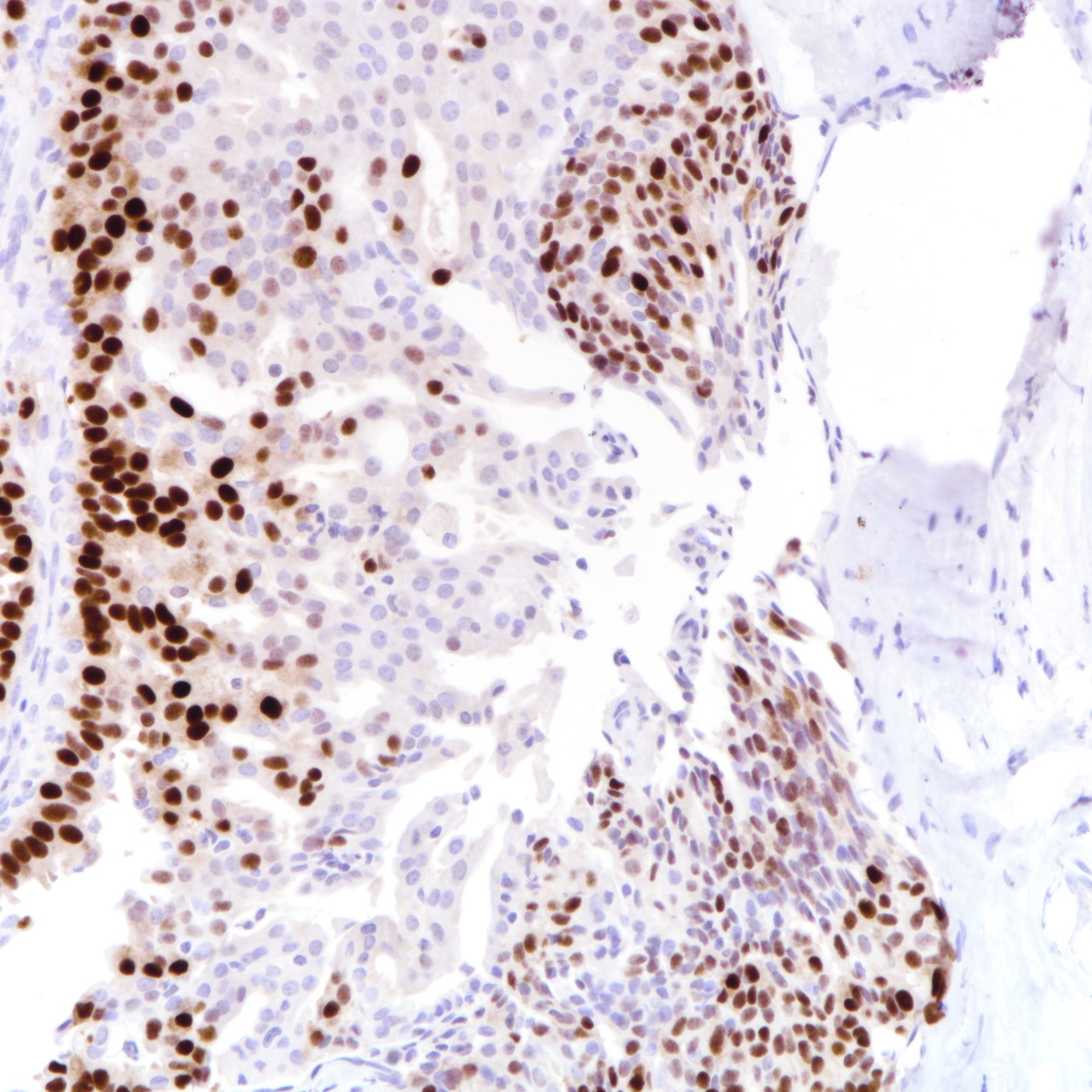
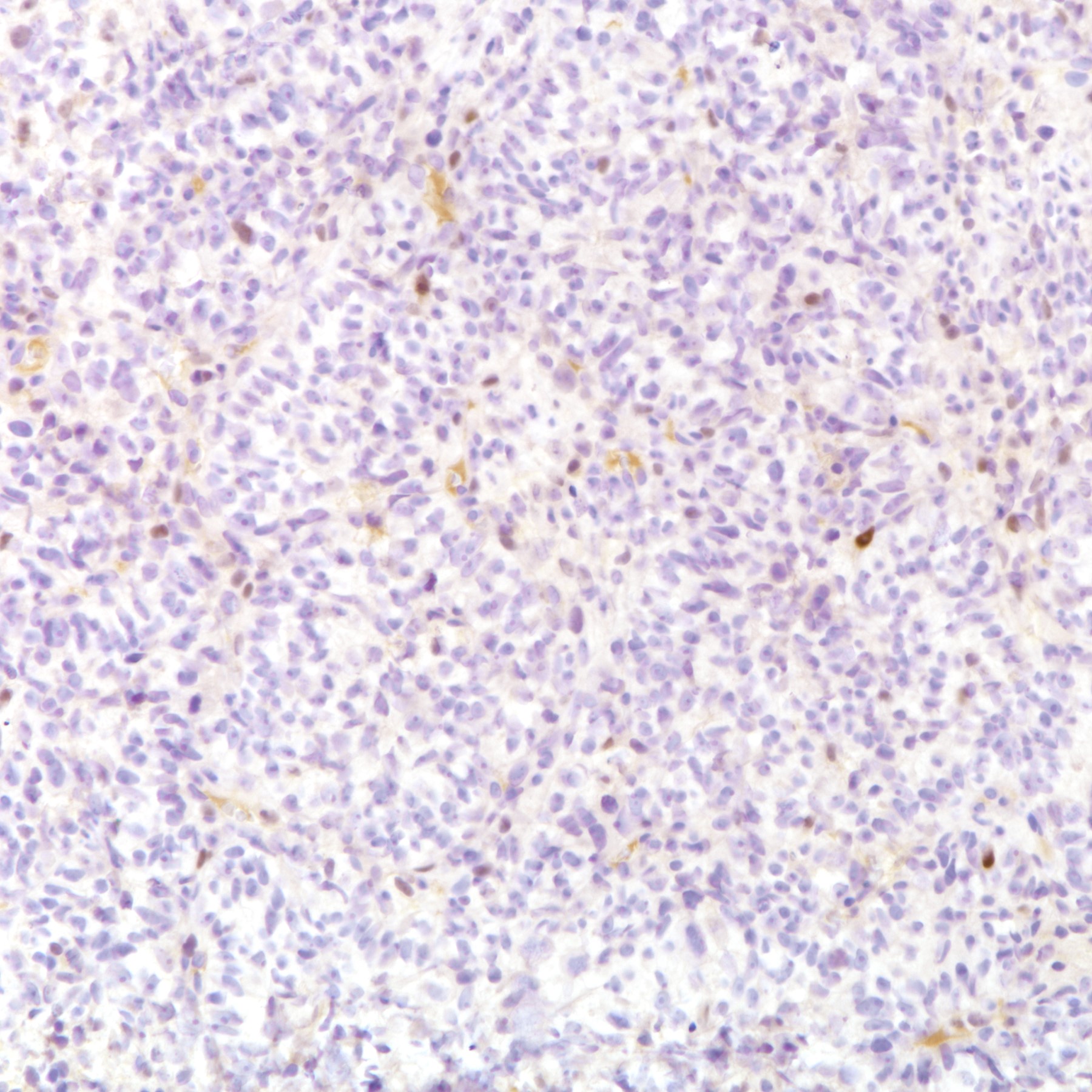
Microscopic (histologic) images
Contributed by Joshua J.X. Li, M.B.Ch.B. and Gary M. Tse, M.B.B.S.
Virtual slides
Positive staining - normal
- Estrogen receptor:
- Breast epithelium and stromal fibroblasts (Int J Cancer 2002;102:334, Breast Cancer Res Treat 2013;142:211)
- Breast myoepithelium expresses ERβ but not ERα (J Mammary Gland Biol Neoplasia 2005;10:231)
- Progesterone receptor:
- Breast epithelium (J Mammary Gland Biol Neoplasia 2004;9:3)
- Androgen receptor:
- Breast epithelium, stromal fibroblasts and adipocytes (Mol Endocrinol 2012;26:1252)
- Apocrine and sebaceous glands (J Endocrinol 1992;133:467)
- For staining in tissue other than the breast, please refer to estrogen receptor, progesterone receptor, androgen receptor
Positive staining - disease
- Estrogen receptor (ERα):
- Clonal proliferative lesions: columnar cell change, columnar cell hyperplasia and flat epithelial atypia (Breast J 2005;11:326)
- Malignant and premalignant lesions: ductal carcinoma in situ (low grade is diffusely positive, intermediate and high grade lesions can be positive or negative), lobular carcinoma in situ, low grade invasive breast carcinoma of no special type; special types of breast cancer - cribriform, lobular, micropapillary, mucinous, neuroendocrine, papillary and tubular carcinomas (Arch Pathol Lab Med 2016;140:686, Histopathology 2007;50:875, Breast Care (Basel) 2020;15:327)
- Cancer associated fibroblasts (Breast Cancer Res Treat 2013;142:211)
- Progesterone receptor:
- Expression of PR is highly associated with and similar to ER in most breast lesions (J Clin Pathol 2007;60:1307, Br J Cancer 2020;123:1223)
- Androgen receptor:
- Apocrine lesions: apocrine metaplasia, apocrine ductal carcinoma in situ and apocrine carcinoma (Pathol Res Pract 1997;193:753)
- Expression of AR in ductal carcinoma in situ and invasive carcinomas is associated with ER expression (J Clin Pathol 2002;55:14, Mod Pathol 2010;23:205)
- Skin adnexal lesions: Paget disease (mammary and extramammary), sebaceous lesions (sebaceous hyperplasia, sebaceous adenoma, sebaceoma and sebaceous carcinoma) (Mod Pathol 2005;18:1283, Mod Pathol 2010;23:205)
- For staining in tissue other than the breast, please refer to estrogen receptor, progesterone receptor, androgen receptor
Negative staining
- Estrogen receptor:
- Microglandular adenosis
- Invasive breast carcinoma of no special type of high grade or with medullary features (Mod Pathol 2005;18:26)
- Special types of breast cancer: acinic cell carcinoma, adenoid cystic carcinoma, apocrine carcinoma, metaplastic carcinomas (fibromatosis-like, monophasic and biphasic) (Diag Histopathol 2020;26:76, Cancer Biol Med 2020;17:293)
- Progesterone receptor and androgen receptor expression is closely related to estrogen receptor expression in most breast lesions, with the exception of apocrine lesions (see Positive staining - disease)
Sample pathology report
- Left breast, biopsy:
- Invasive breast carcinoma of no special type (see comment)
- Comment: Immunostaining shows that the invasive tumor cells are ER positive (strong [3+] intensity, 70%) and PR positive (strong [3+] intensity, 70%).
Board review style question #1
Board review style answer #1
E. Prominent tubule formation. ER positivity is associated with low grade features (Breast Care (Basel) 2020;15:327). Lymphovascular invasion, medullary features and tumor infiltrating lymphocytes are associated with ER negativity (Br J Cancer 2020;123:1223, Cancer Biol Med 2020;17:293).
Comment Here
Reference: Hormone receptors
Comment Here
Reference: Hormone receptors