Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Ismail A, Sanders MAG. Axillary lymph nodes. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/breastmalignantaxillary.html. Accessed April 2nd, 2025.
Definition / general
- Extent of axillary lymph node involvement is important for breast cancer stage, clinical management and prognosis
Essential features
- Evaluation of axillary lymph nodes for pathologic staging of invasive breast cancer requires sentinel lymph node biopsy with or without axillary lymph node dissection
- Axillary lymph node dissection should contain 10 or more lymph nodes
- Primary goal when histologically evaluating axillary lymph nodes is to identify all macrometastases
Terminology
- Macrometastases: > 2.0 mm
- Micrometastases: > 0.2 mm to 2.0 mm, or > 200 cells in a single histologic cross section
- Isolated tumor cells (ITCs): ≤ 0.2 mm or ≤ 200 cells in a single histologic cross section
ICD coding
Clinical features
- Axillary lymph node dissection typically removes level I and level II lymph nodes
- Lymph node dissection of level I and level II of the axilla should contain 10 or more lymph nodes
- If level III lymph nodes are surgically removed, the surgeon should separately identify them for staging purposes
- Regional lymph nodes:
- Axillary (ipsilateral), subdivided as follows:
- Level I (low axilla): lateral to the lateral border of pectoralis minor muscle
- Level II (mid axilla): between medial and lateral borders of pectoralis minor muscle, plus the interpectoral (Rotter) lymph nodes
- Level III (apical axilla or infraclavicular nodes): medial to the medial margin of the pectoralis minor muscle and inferior to the clavicle
- Internal mammary (ipsilateral): lymph nodes in the intercostal spaces along the edge of the sternum in the endothoracic fascia
- Supraclavicular (ipsilateral)
- Axillary (ipsilateral), subdivided as follows:
- Intramammary nodes are present within breast tissue and are most commonly found in the upper outer quadrant and may rarely be sentinel lymph nodes; these nodes are included with axillary nodes for AJCC N classification
- Side effects of axillary nodal dissection include lymphedema, shoulder restriction, numbness, weakness and pain syndromes (Cancer J 2008;14:216)
Diagnosis
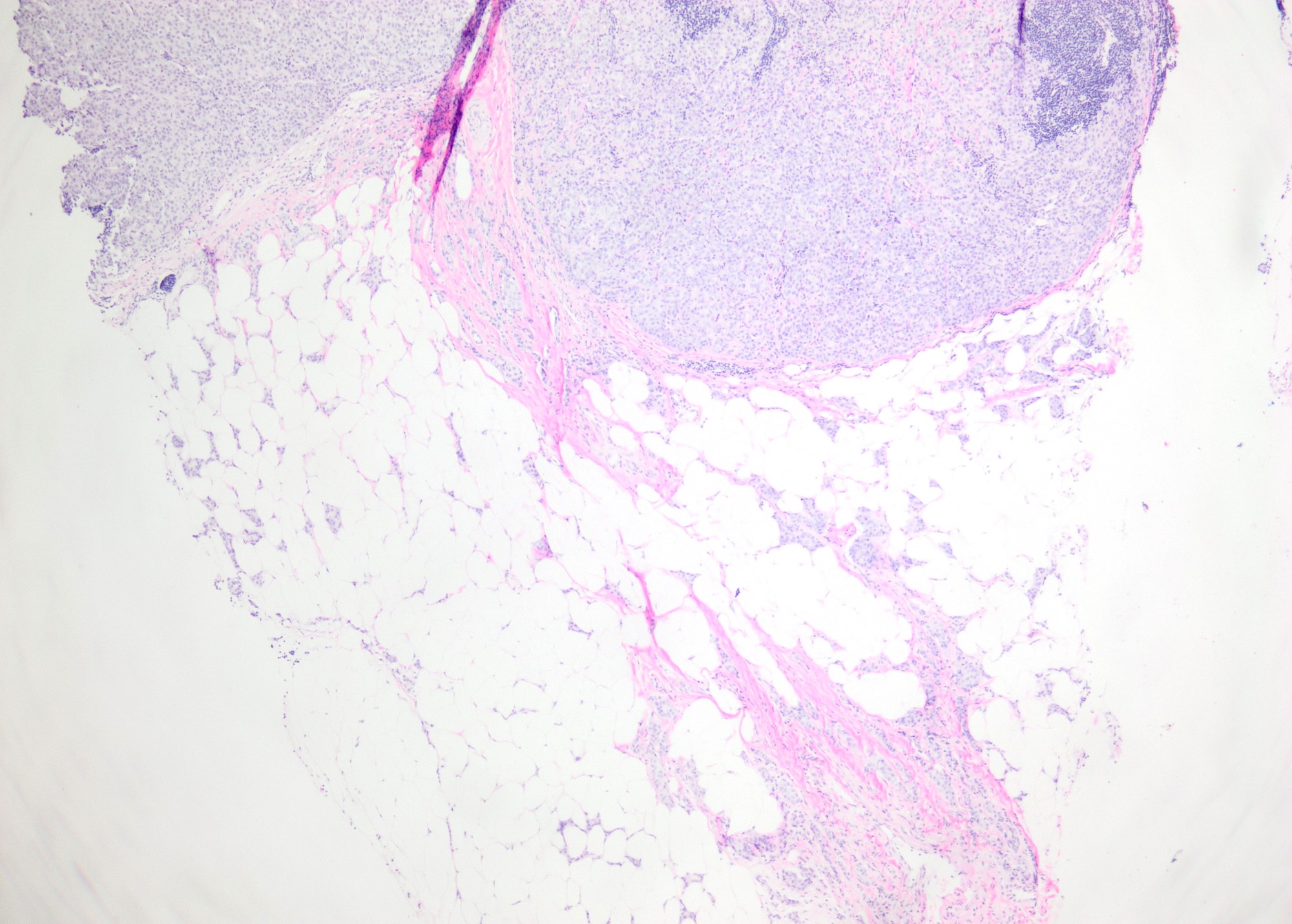
- Lymph nodes are thinly sliced at 2 mm intervals (to detect all macrometastasis)
- All lymph node tissue is submitted for histologic evaluation
- If grossly positive then a representative section (including any possible areas of extranodal extension) is adequate
- Additional evaluation of SLNs to detect occult metastasis, including multiple levels and cytokeratin immunohistochemistry, offers no clinical benefit (N Engl J Med 2011;364:412)
- Intraoperative evaluation of sentinel lymph nodes can be avoided in most patients who are clinically node negative and are undergoing breast conserving surgery (Arch Pathol Lab Med 2016;140:830)
Radiology description
- Axillary ultrasound (US) is the primary modality for evaluating axillary lymph node status prior to surgery
- Cortical thickening, hilar effacement and nonhilar cortical blood flow are more important than size criteria in the identification of metastases (Radiographics 2013;33:1589)
- Preoperative axillary US and fine needle aspiration (FNA) cytology are routine at many breast units, with a sensitivity of 56% (confidence interval: 47 - 64%) and specificity of 90% (84 - 93%) for US alone, and 76% (61 - 87%) and 100% (65 - 100%) when combined with FNA cytology (J BUON 2011;16:454)
- Standard breast MRI is comparable to dedicated axillary US in breast cancer patients; subsequent axillary US can be done on those with suspicious nodal findings (Eur J Radiol 2016;85:2288)
- CT and radionuclide imaging play a lesser role in imaging the axilla (Radiographics 2013;33:1589)
Prognostic factors
- Presence of axillary lymph node metastases is the most important prognostic factor for disease free and overall survival in the absence of distant metastasis and is important for determining treatment for breast cancer
- Macroscopic extranodal extension presents clinically as palpable matted lymph nodes and is a risk factor for local regional recurrence
- Microscopic extranodal extension measuring > 2 mm is associated with greater axillary nodal burden (Ann Surg Oncol 2014;21:2897)
- Tumor deposits and intravascular tumor emboli in extranodal axillary fat are associated with greater axillary nodal burden (Ann Surg Oncol 2020;27:3585)
- Presence of treatment effect (fibrosis with or without macrophages or hemosiderin) after neoadjuvant chemotherapy is an important prognostic factor
Case reports
- 49 year old man with axillary lymph node metastasis as first manifestation of occult breast cancer (Medicine (Baltimore) 2018;97:e13706)
- 55 year old woman with DCIS arising in intraductal papilloma in axillary lymph node (Arch Pathol Lab Med 2008;132:1940)
- 63 year old woman with nevus cell aggregate in axillary lymph node mimicking metastatic breast carcinoma (Breast J 2019;25:726)
- 70 year old woman with sentinel lymph node involvement by epithelial inclusions mimicking metastatic carcinoma (Am J Case Rep 2020;21:e926094)
- 81 year old woman with contralateral axillary lymph node metastasis in second primary breast cancer (Int J Surg Case Rep 2017;40:47)
Treatment
- Sentinel lymph node biopsy (SLNB) at time of breast surgery for early stage breast cancer with clinically negative axillary nodes (J Clin Oncol 2017;35:561):
- If no sentinel lymph node (SLN) metastasis, then no axillary lymph node dissection (ALND)
- If 1 or 2 SLNs with metastases are present and patient is undergoing breast conserving surgery with whole breast radiotherapy, then no ALND
- If SLN metastases are present and patient is undergoing mastectomy, then ALND should be offered
- ALND can be omitted in patients who undergo mastectomy for early stage clinically node negative breast cancer with 1 or 2 SLN metastases, if treated with axillary radiotherapy (Pract Radiat Oncol 2016;6:e219)
- ALND can be avoided in patients with early stage breast cancer and only micrometastasis in the SLNs (Lancet Oncol 2013;14:297)
- SLNB may be considered optional for elderly patients, particularly if axillary staging will not affect selection of adjuvant systemic or radiotherapy
- ALND at time of breast surgery, if clinically palpable lymph nodes or ≥ 3 suspicious nodes by imaging with axillary nodal metastasis confirmed on core biopsy or FNA; SLNB may be considered if clinically node negative after neoadjuvant therapy
Frozen section description
- Axillary SLN are identified by the surgeon by determining uptake of radioisotope technetium 99 sulfur colloid, methylene blue dye or both
- Intraoperative frozen section or imprint cytology may be performed on the SLN to determine need for axillary lymph node dissection (World J Surg Oncol 2008;6:69, Eur J Surg Oncol 2009;35:16)
- Frozen section (FS) had an overall mean sensitivity of 73% (macrometastasis: 94%; micrometastasis 40%) and mean specificity of 100% (meta-analysis of 47 studies, Cancer 2011;117:250)
- SLN FS may be safely omitted in patients who meet ACOSOG Z11 criteria (Clin Breast Cancer 2018;18:276, J Clin Pathol 2016;146:57)
- False negative rate of intraoperative frozen section, post neoadjuvant chemotherapy, was 5.4% in a single institution study of 711 cases (Am J Surg Pathol 2019;43:1377)
- Atypical cases on FS are usually negative on permanent sections (Mod Pathol 2005;18:58)
- In most cases, if metastases are present, the SLN will be involved; in rare cases, only nonsentinel nodes contain metastases
- Metastasis to nonsentinel lymph nodes can occur if the true SLN is completely replaced by tumor (and therefore is not detected by radioactive tracer or dye), if there is unusual lymphatic drainage or if there is failure of the technique to identify the node
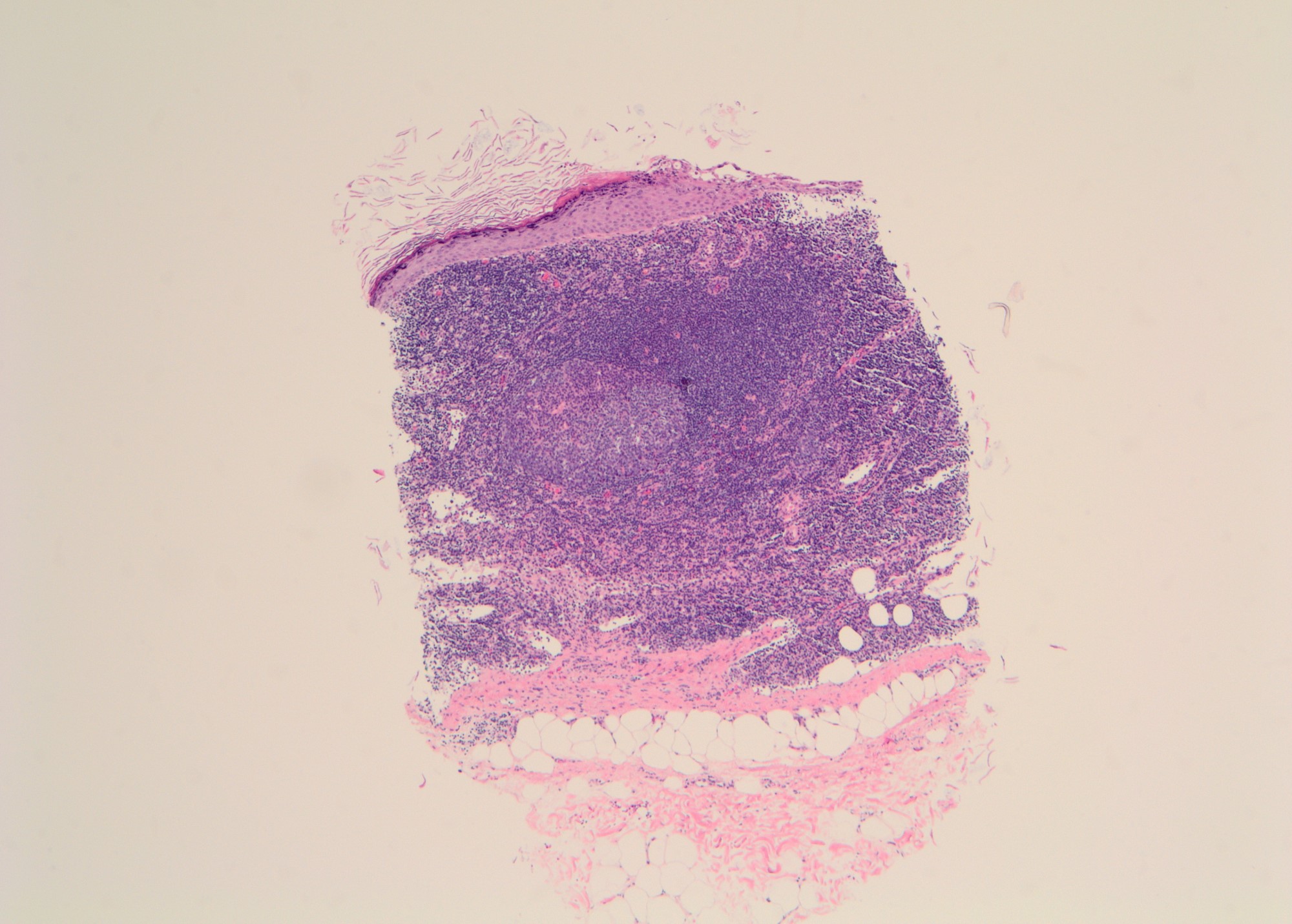
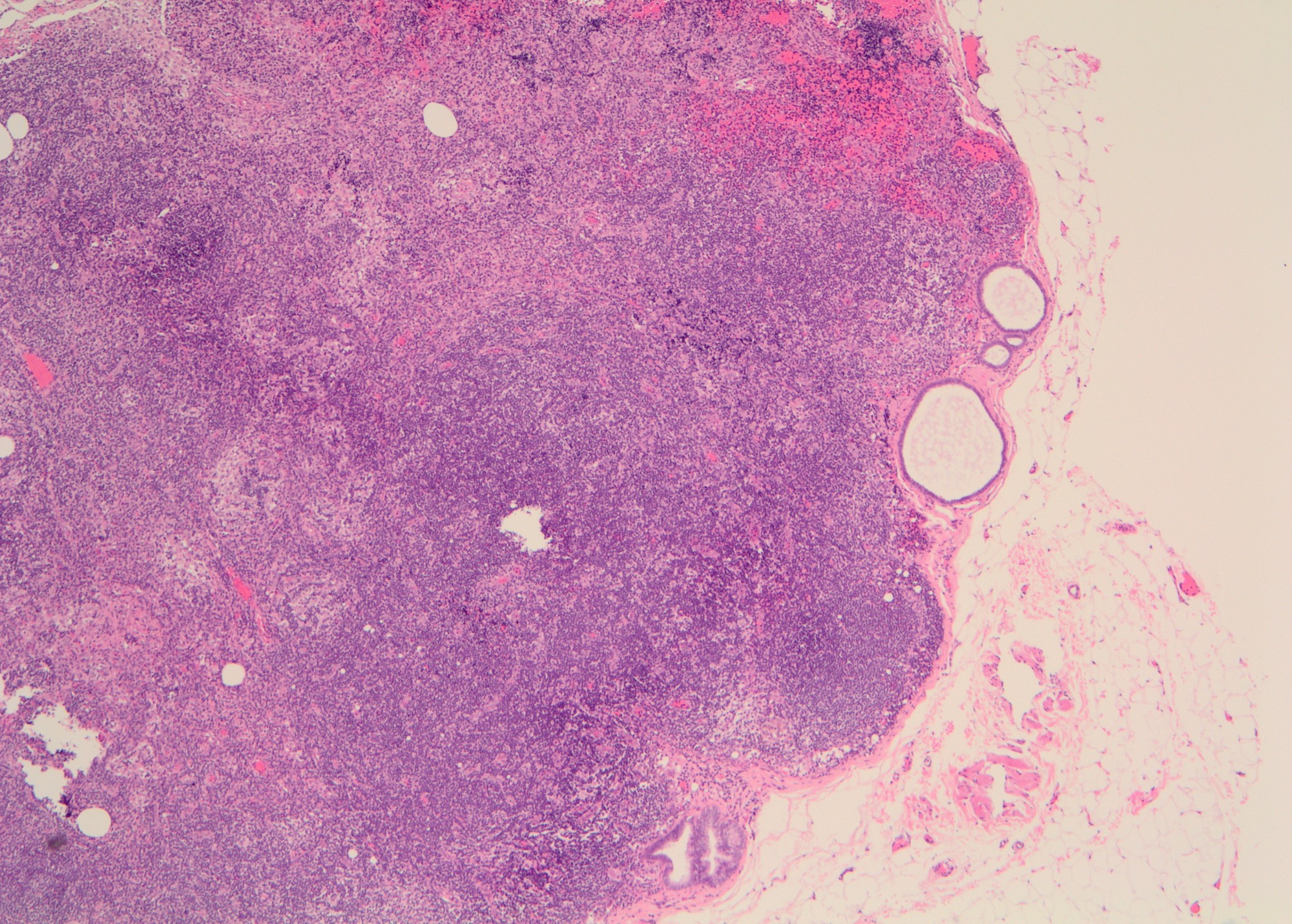
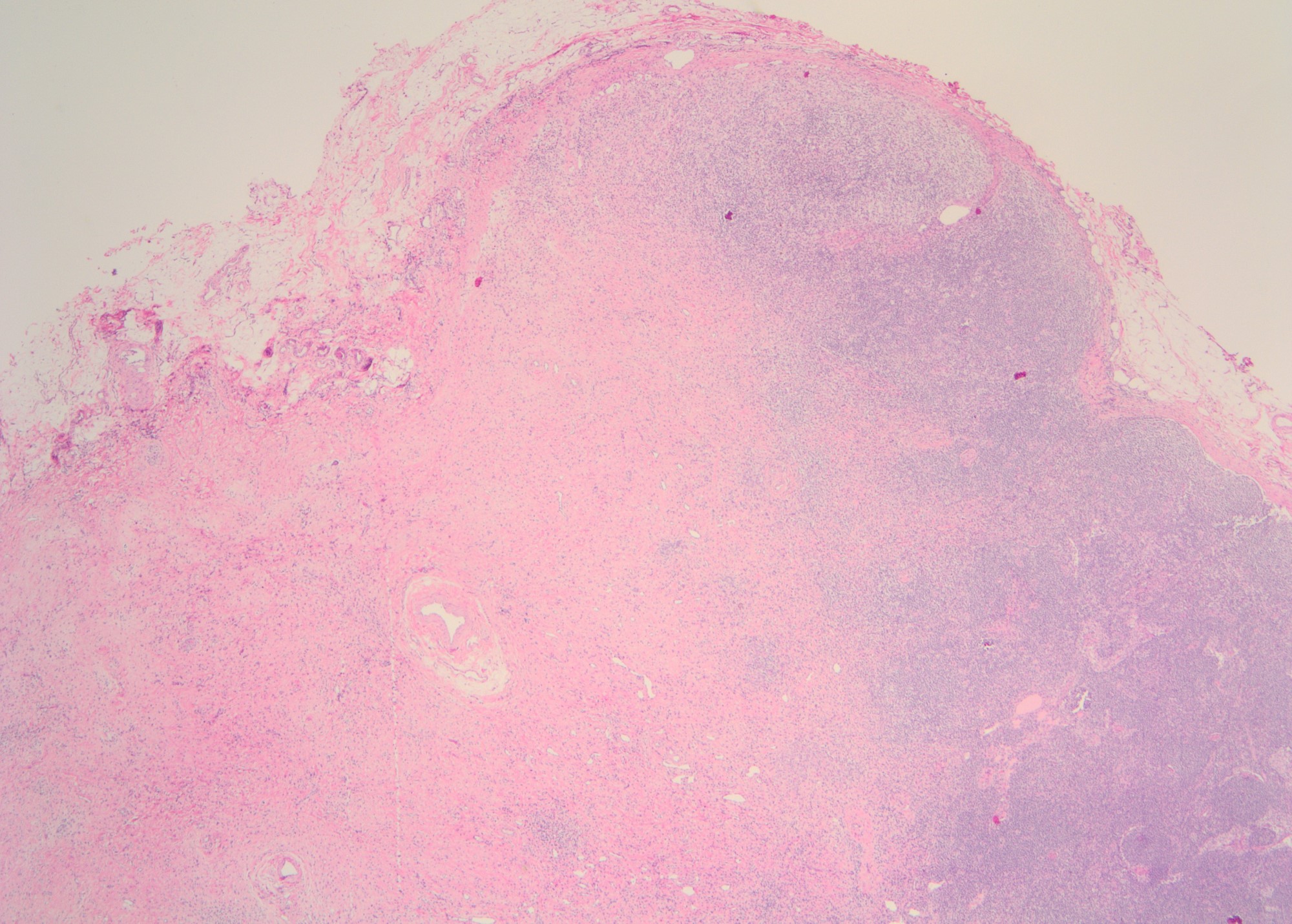
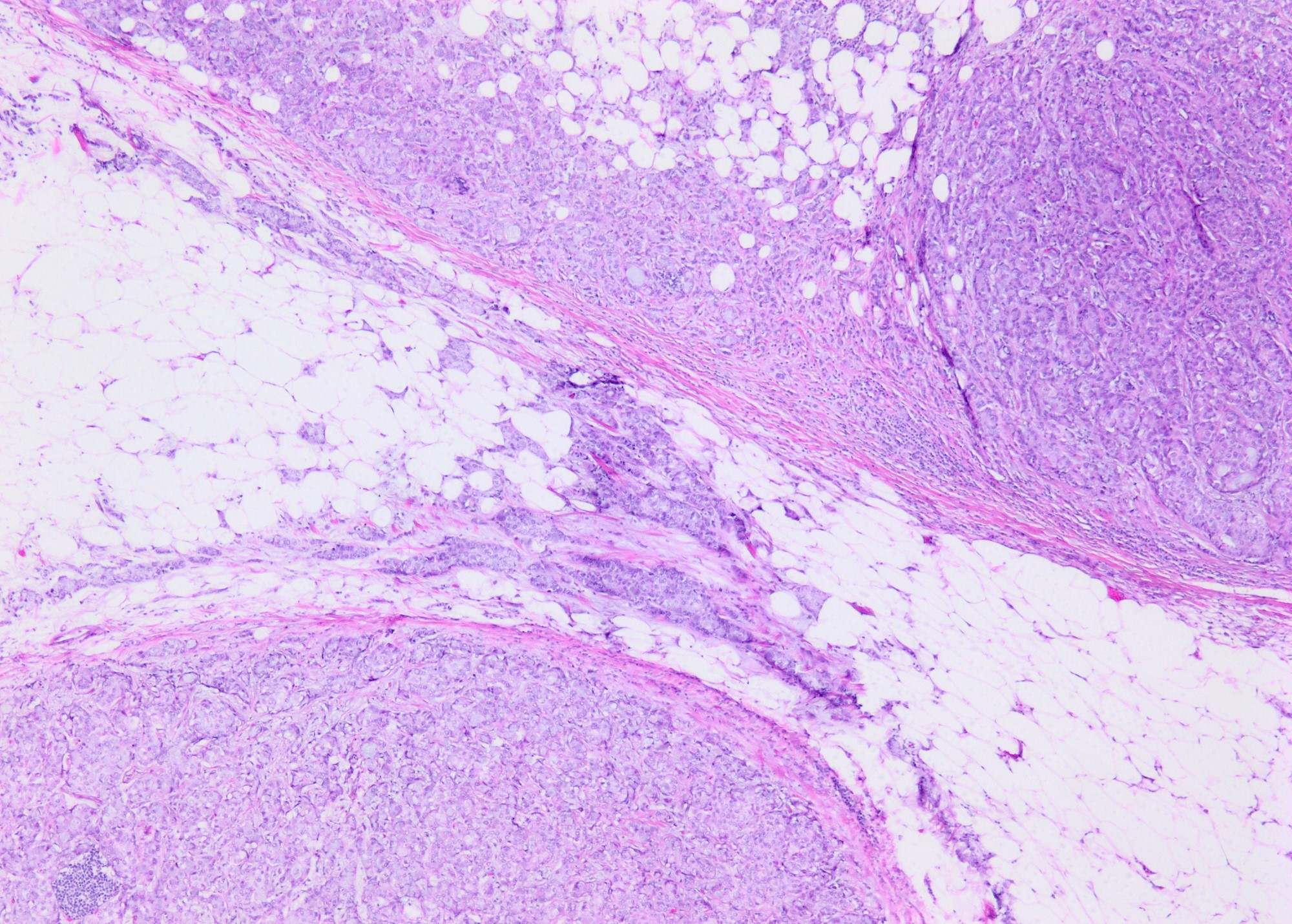
Microscopic (histologic) description
- Size of a metastatic deposit consists of a contiguous focus of tumor cells, including any intervening desmoplasia (for post neoadjuvant treatment, do not include intervening fibrous tumor bed for deposit size)
- Tumor cells of metastatic lobular carcinoma are often dispersed and not contiguous
- 200 cell cutoff helps to determine if dispersed cells in a lymph node should be classified as isolated tumor cells
- Extranodal extension (ENE) is included in the size of the metastatic deposit
- ENE is defined as carcinoma invading into fat outside of a lymph node, either via invasion through the capsule of the node or invasion into fat outside the node at the hilum
- Invasion into fat located within the contours of the lymph node is not ENE
- Carcinoma located within lymphatics or blood vessels in axillary fat is not ENE
- ENE is reported as present or not present; If present, the amount of ENE can be reported as ≤ 2 mm or > 2 mm or the measurement of the largest dimension
- Nodular tumor deposits in axillary fat without evidence of residual lymph node are counted as positive axillary lymph nodes
- pN: see staging topic
- (sn) modifier for pN stage is used when 5 or fewer lymph nodes are sampled / evaluated
- Intramammary lymph nodes are included in the axillary lymph node count
- Metastasis to an ipsilateral level III axillary lymph node is staged as pN3a
- Metastasis to a contralateral axillary lymph node is staged as pM1
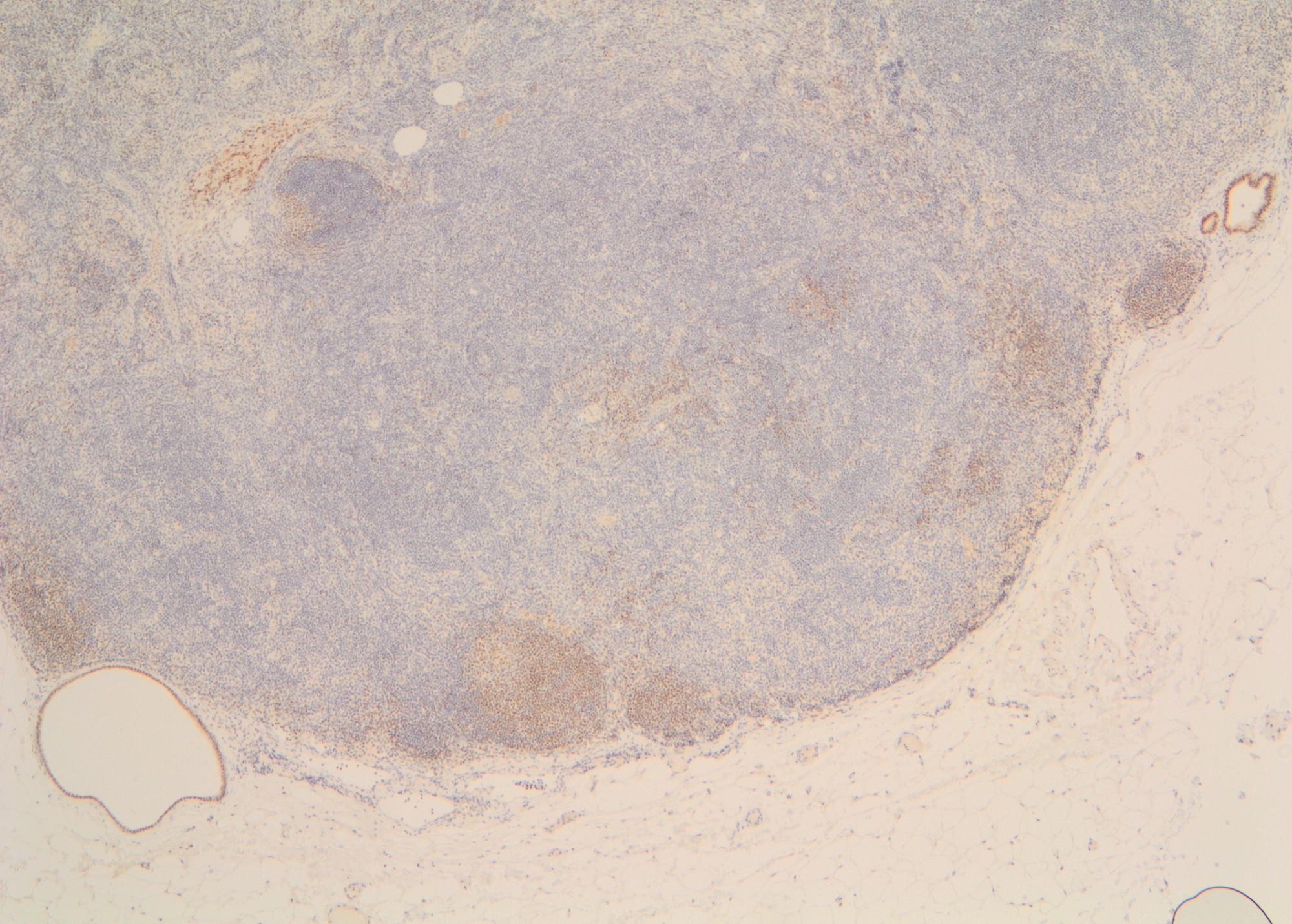
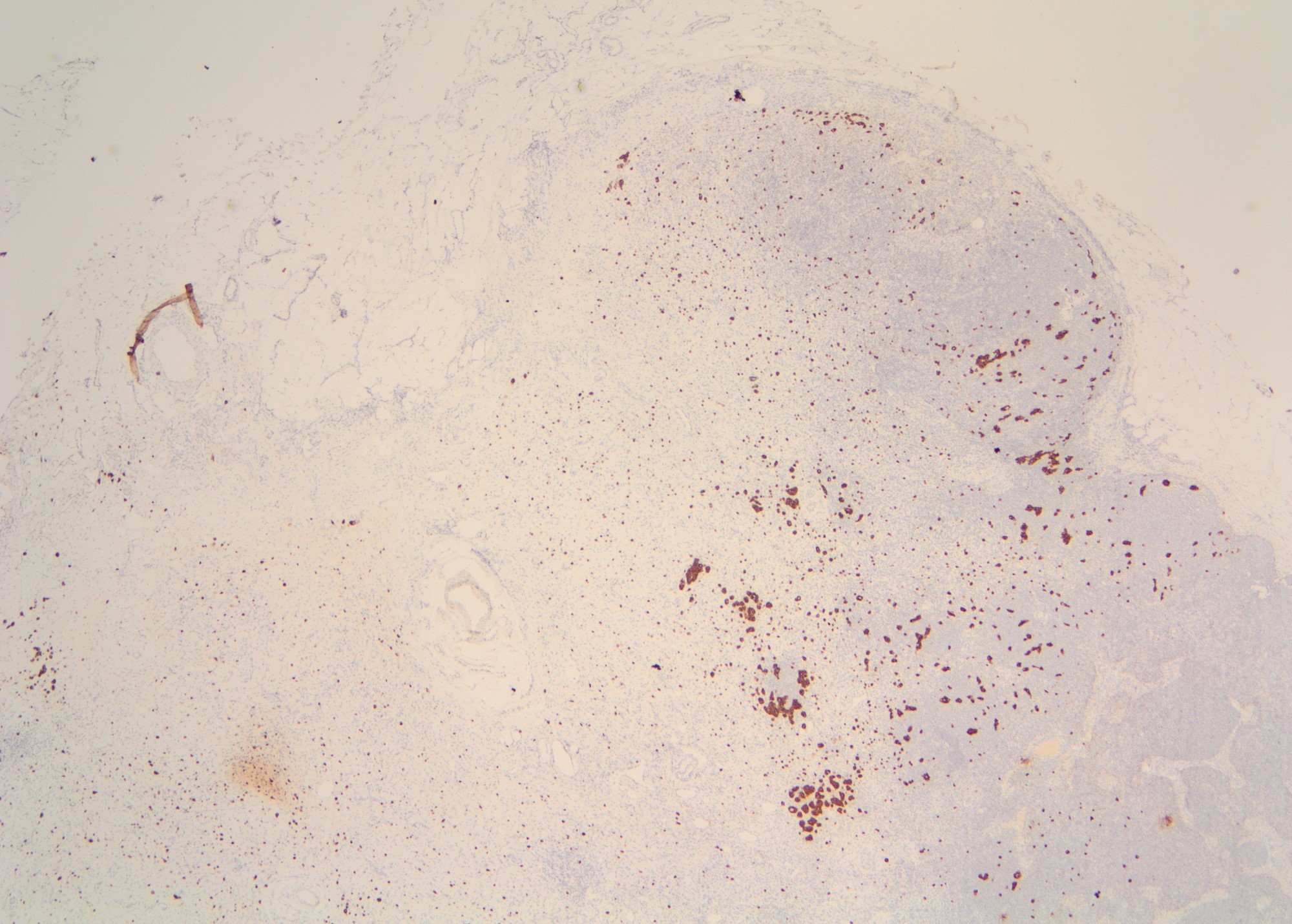
Microscopic (histologic) images
Cytology description
- FNA smears of positive axillary lymph node are characterized by crowded, disorganized groups of cells with enlarged nuclei, nuclear pleomorphism, irregular nuclear membranes and intracytoplasmic vacuoles with or without mucin
- Necrosis or mucin in the background and single intact malignant cells may be present
- Imprint cytology had an overall sensitivity of 63% (macrometastasis: 81%, micrometastasis: 22%) and specificity of 99% (meta analysis of 31 studies) (Br J Surg 2005;92:1068)
- Factors that can affect the outcome of FNA are the size of the metastasis in the lymph node, experience of the person performing image guided FNA and evaluation of the sample for adequacy by a pathologist (at the time of FNA)
Positive stains
- Note: "enhanced methods" of SLN metastasis detection, including routine immunohistochemistry, are not recommended (i.e., should be used on a case by case basis / when necessary for diagnosis) (J Clin Oncol 2014;32:1365)
- AE1 / AE3, CK7, GATA3
- Estrogen receptor / ER (depends on biomarker status)
- Reference: Semin Diagn Pathol 2018;35:143
Negative stains
Molecular / cytogenetics description
- Some studies have reported usefulness of molecular assays, usually reverse transcriptase polymerase chain reaction (RT-PCR) (J Clin Oncol 2008;26:3338)
- False positive and false negative results can occur with RT-PCR
- Significance of a positive RT-PCR result for a histologically negative lymph node is unknown (J Clin Oncol 2008;26:3338)
- Current AJCC cancer staging manual (8th edition) includes positive molecular findings by RT-PCR; no isolated tumor cell clusters detected as pN0 (mol+)
Sample pathology report
- Right axillary lymph nodes, dissection:
- Metastatic carcinoma is present in 3 of 10 lymph nodes, two macrometastases and one micrometastasis, (3/10)
- The largest metastatic deposit measures 8 mm
- Extranodal extension is present (measuring 3 mm)
Differential diagnosis
- Benign epithelial inclusions (Am J Surg Pathol 2011;35:1123):
- Glandular type:
- Breast-like:
- Have myoepithelial cells which are p63+ and smooth muscle myosin+
- Müllerian-like:
- Breast-like:
- Mixed glandular and squamous type
- Squamous type
- Glandular type:
- Benign transport after prior breast biopsy (Am J Clin Pathol 2000;113:259):
- Additional features such as giant cells and hemosiderin are indicative of benign transport rather than true metastases
- Ectopic breast tissue (Breast Cancer 2007;14:425)
- Muciphages:
- Resemble signet ring cell carcinoma
- Associated with prior surgery
- Alcian blue+, CD68+, MAC387+, keratin- (Am J Surg Pathol 1998;22:545)
- Nevus cells (Am J Clin Pathol 1994;102:102, Am J Surg Pathol 2003;27:673, Arch Pathol Lab Med 1985;109:1044)
- Occult breast cancer:
- Axillary nodal metastasis consistent with breast cancer and no evidence of primary breast cancer by physical exam and imaging (Ann Surg Oncol 2017;24:3141)
- Lymphoma:
- Melanoma:
- Keratin-, SOX10+, HMB45+, MelanA / MART1+
- Metastatic carcinoma other than breast:
Additional references
Board review style question #1
The gross image provided is a right axillary sentinel lymph node received from the OR of a patient with stage 1 breast cancer undergoing lumpectomy and sentinel lymph node biopsy. Recommendations provided by the College of American Pathologists (CAP) for evaluating axillary lymph nodes in breast cancer include which of the following?
- Evaluate 3 H&E levels for sentinel lymph nodes
- Submit all lymph node tissue if grossly positive
- Thinly slice each lymph node at 2 mm intervals
- Tumor deposits in axillary tissue are counted as extranodal extension
- Use cytokeratin immunohistochemistry on all negative lymph nodes
Board review style answer #1
C. Thinly slice each lymph node at 2 mm intervals. Per the CAP guidelines, sampling of lymph nodes must be adequate to detect all macrometastasis (> 2 mm deposit). Therefore, all lymph nodes must be thinly sliced at 2 mm intervals. All tissue from grossly negative lymph nodes must be submitted for histologic evaluation. For grossly positive lymph nodes, a representative section including areas suspicious for extranodal extension is adequate. Additional evaluation, including multiple H&E levels and cytokeratin immunohistochemistry, increases detection of isolated tumor cells and micrometastasis (occult metastasis), however this provides minimal clinical benefit. Therefore, the CAP recommends evaluating 1 H&E level from the surface of the tissue block when lymph node tissue has been sliced at 2 mm intervals. Tumor deposits in axillary tissue are counted as positive axillary lymph nodes (lymph node replaced by tumor).
Comment Here
Reference: Axillary lymph nodes
Comment Here
Reference: Axillary lymph nodes
Board review style question #2
A 50 year old woman underwent core needle biopsy of a 10 mm right breast mass detected on ultrasound and diagnosed as invasive ductal carcinoma, grade 2, that was estrogen receptor positive, progesterone receptor positive and HER2 negative. Right axillary ultrasound showed normal appearing lymph nodes. Breast MRI showed no additional lesions. There was no evidence of distant metastasis. What is the appropriate surgical management for this patient?
- Double mastectomy
- Lumpectomy
- Lumpectomy with axillary lymph node dissection
- Lumpectomy with sentinel lymph node biopsy
- No surgery
Board review style answer #2
D. Lumpectomy with sentinel lymph node biopsy. This patient has early stage breast cancer with clinically negative axillary lymph nodes; therefore, she will need sentinel lymph node biopsy to stage the axilla and to determine further axillary management and adjuvant systemic therapy and radiotherapy.
Comment Here
Reference: Axillary lymph nodes
Comment Here
Reference: Axillary lymph nodes