Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Lérias S, Lerwill M. Angiosarcoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/breastmalignantangiosarcoma.html. Accessed March 30th, 2025.
Definition / general
- Malignant vascular neoplasm, which may arise in previously irradiated skin or breast tissue (secondary postradiation angiosarcoma) or in nonirradiated tissue (primary angiosarcoma)
Essential features
- Irregular, infiltrative anastomosing vascular channels with endothelial atypia
- Postradiation angiosarcoma demonstrates amplification of MYC
Terminology
- Alternate terminology: hemangiosarcoma, lymphangiosarcoma
ICD coding
- ICD-O: 9120/3 - angiosarcoma, postradiation angiosarcoma
- ICD-10: C50 - malignant neoplasm of breast
- ICD-11: 2B56.2 & XH6264 - angiosarcoma of breast & angiosarcoma
Epidemiology
- Rare (0.05% of malignant breast tumors) but is the most common type of mammary sarcoma
- Most often arises after radiation treatment for breast cancer
- Postradiation angiosarcoma
- Incidence of 0.03 - 0.14% after breast irradiation (BMC Cancer 2018;18:463, J Am Acad Dermatol 2006;54:499)
- Median age of 70 years (Cancer 2005;104:2682)
- Arises within the radiation field with a median latency of 6 - 7 years (Br J Surg 2021;108:388, Ann Surg Oncol 2013;20:1267)
- Rare cases may develop within a shorter latency period of 1 - 2 years
- Primary angiosarcoma
- Median age of 40 years (Am J Surg Pathol 2008;32:1896)
Sites
- Postradiation angiosarcoma
- Typically arises in irradiated skin and may secondarily extend into the breast parenchyma (Breast J 2020;26:458)
- Less commonly arises in breast parenchyma
- Primary angiosarcoma
- Usually arises in breast parenchyma
- Stewart-Treves syndrome
- Cutaneous angiosarcoma of the upper limb arising in the setting of chronic lymphedema, typically occurring after mastectomy and axillary dissection (J Am Acad Dermatol 2012;67:1342)
- May secondarily extend to the breast / chest wall
Pathophysiology
- Malignancy of vascular or lymphatic endothelial cells
- Exact lineage remains unclear since endothelial cells may undergo transdifferentiation
Etiology
- Ionizing radiation (postradiation angiosarcoma)
- Longstanding lymphedema (Stewart-Treves syndrome)
- Unknown (primary angiosarcoma)
Clinical features
- Solitary or multiple erythematous to violaceous plaques, papules, nodules or areas of discoloration on the skin (postradiation angiosarcoma) (Am J Clin Pathol 1994;102:757)
- Rapidly growing poorly defined mass, swelling or asymmetry of the breast parenchyma (primary angiosarcoma) (Am J Surg Pathol 2008;32:1896)
Diagnosis
- Histologic examination of tissue obtained by biopsy or surgical excision
Radiology description
- Mammography
- Cutaneous tumors: skin thickening (may be masked by postradiation changes)
- Parenchymal tumors: focal or diffuse asymmetry or an ill defined mass, sometimes with a lobulated or oval shape; a minority are mammographically occult (AJR Am J Roentgenol 2008;190:533, BMC Womens Health 2019;19:73)
- Ultrasonography
- Hyperechoic mass or areas of mixed hyper and hypoechogenicity with architectural distortion (Radiology 2007;242:725)
- Doppler sonography shows hypervascularity
- Magnetic resonance imaging
- High signal intensity in T2 weighted images
- Low grade tumors show progressive enhancement
- High grade tumors show rapid enhancement and washout
Radiology images
Prognostic factors
- Poor prognostic features include older age, large tumor size, high histological grade, tumor spread and incomplete initial resection, although results differ among studies (Ann Surg Oncol 2013;20:1267, BMC Cancer 2017;17:295, BMC Cancer 2018;18:463, Breast Cancer Res Treat 2019;178:523)
- Correlation between histologic grade and outcome is debated (Am J Surg Pathol 2008;32:1896)
- Primary and postradiation angiosarcomas appear to have a similar prognosis after adjustment for clinicopathological variables (BMC Cancer 2017;17:295)
Case reports
- 32 year old woman with Li-Fraumeni syndrome and postradiation angiosarcoma (Sao Paulo Med J 2015;133:151)
- 39 year old woman with primary angiosarcoma (Int J Clin Exp Pathol 2019;12:664)
- 62 year old woman with bilateral postradiation angiosarcoma (Case Rep Oncol Med 2020;2020:5768438)
Treatment
- Complete surgical excision is the primary treatment modality
- Radical resection of all previously irradiated skin may improve recurrence rate and disease specific survival in cases of postradiation angiosarcoma (Ann Surg 2017;265:814)
- Role of chemotherapy is poorly defined but it may improve survival in patients with tumors > 5 cm (Breast Cancer Res Treat 2019;175:409)
- Radiation therapy remains controversial, particularly in cases of postradiation sarcoma
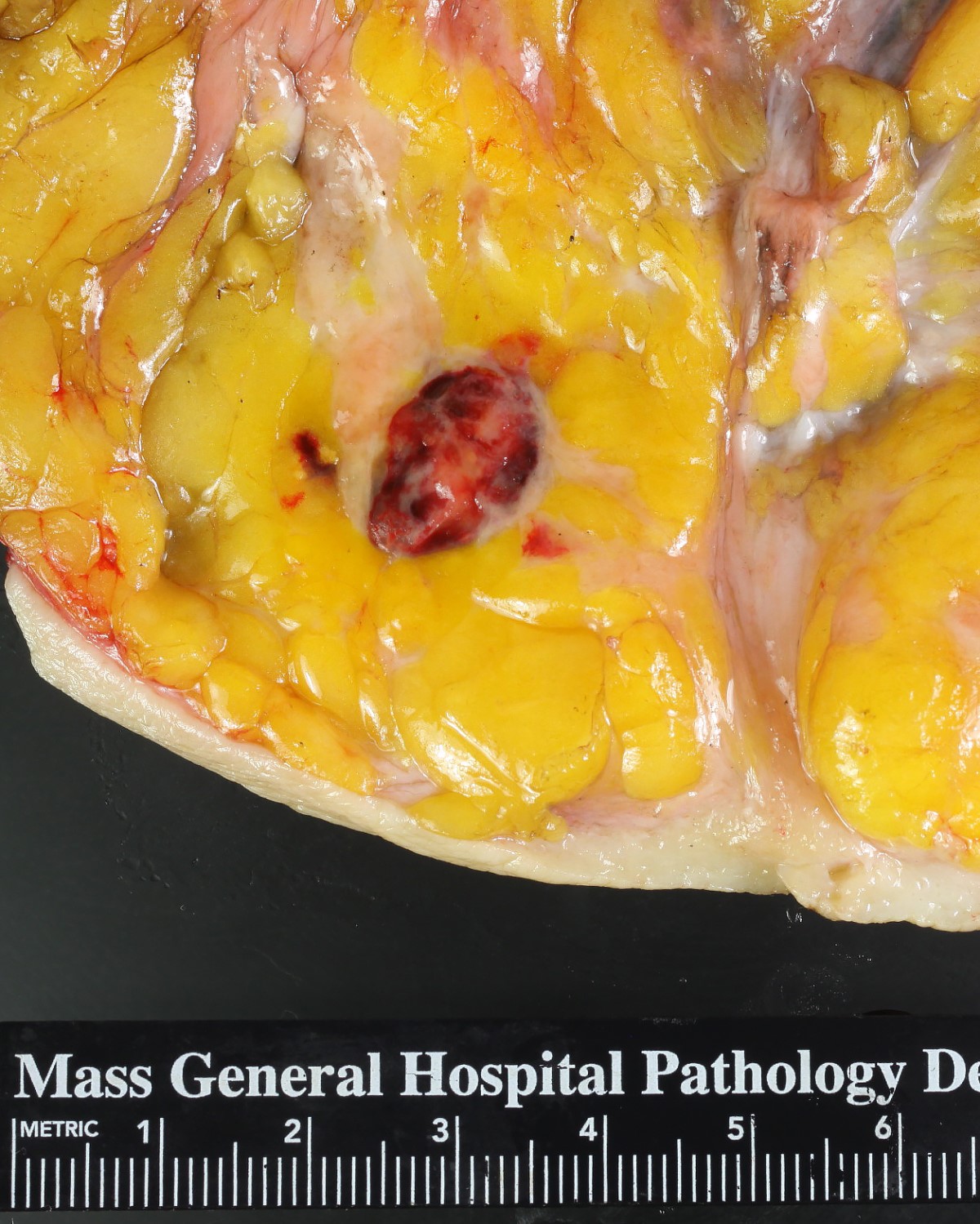
Gross description
- Average size of 4 - 6 cm (Breast Cancer Res Treat 2019;178:523)
- Multifocality is more common in postradiation than in primary angiosarcoma
- Firm to spongy hemorrhagic mass
- Cystic necrosis can occur in higher grade tumors
- Tumors are often larger than is grossly evident
Gross images
Frozen section description
- See Microscopic (histologic) description section
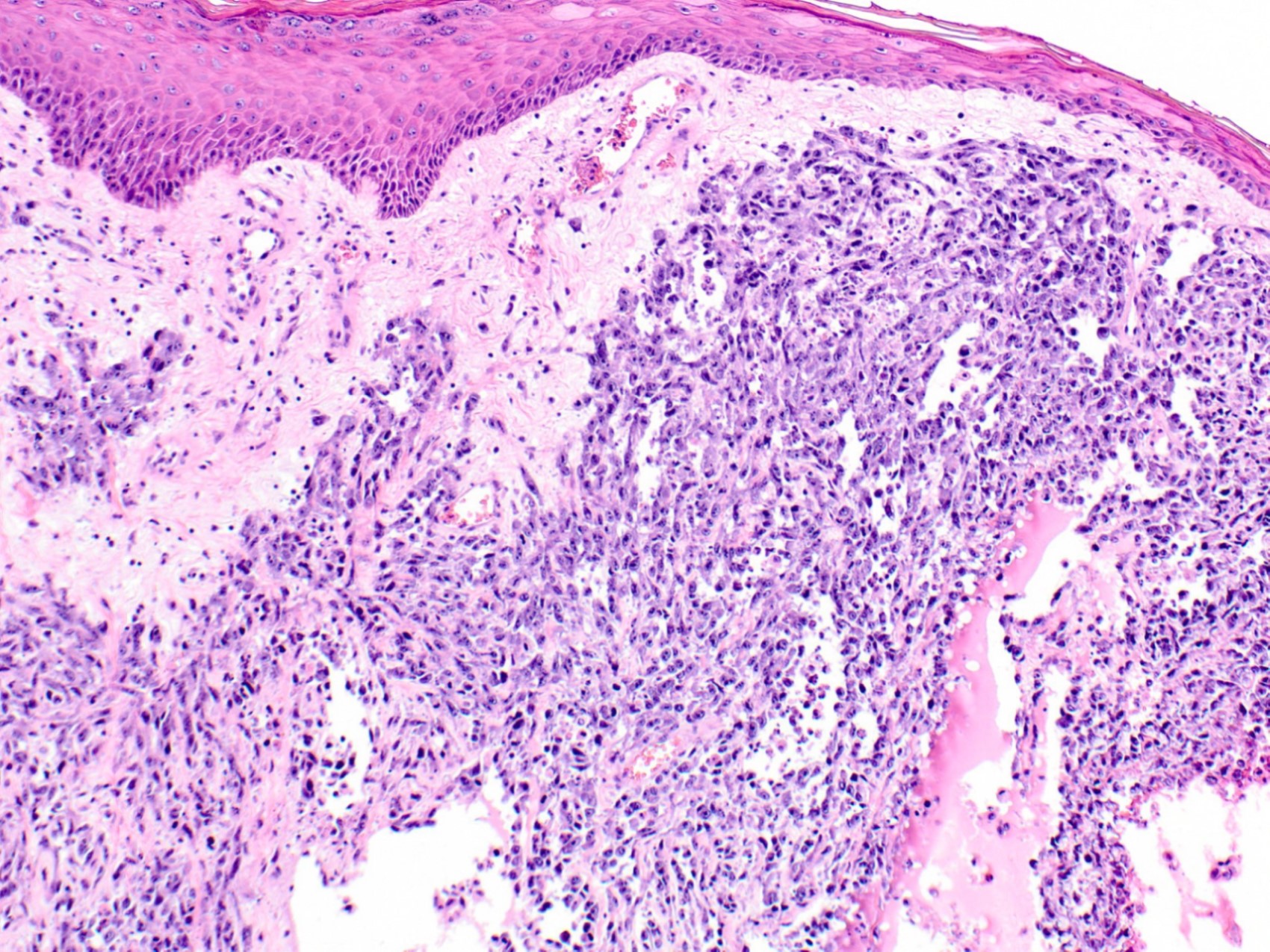
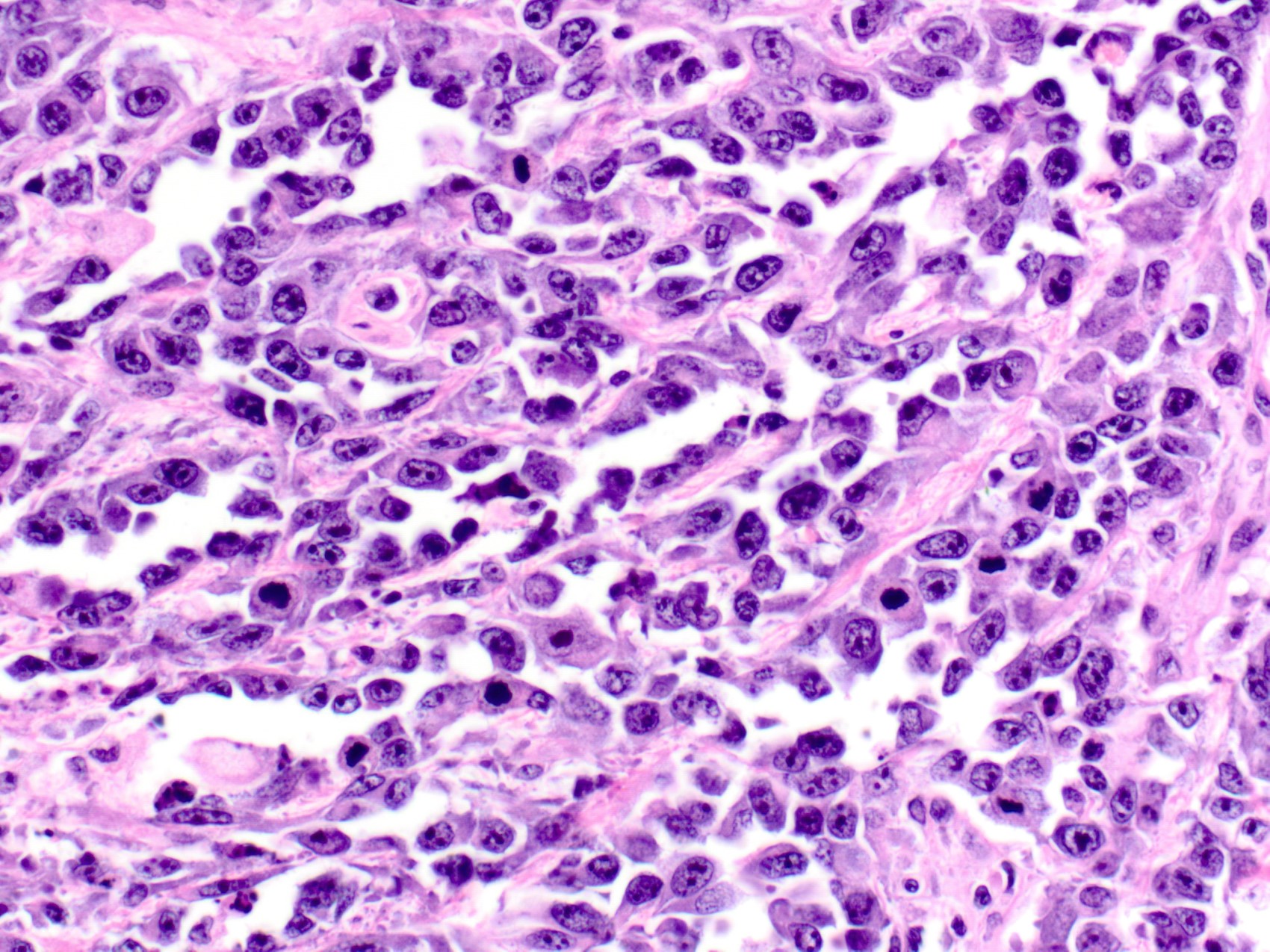
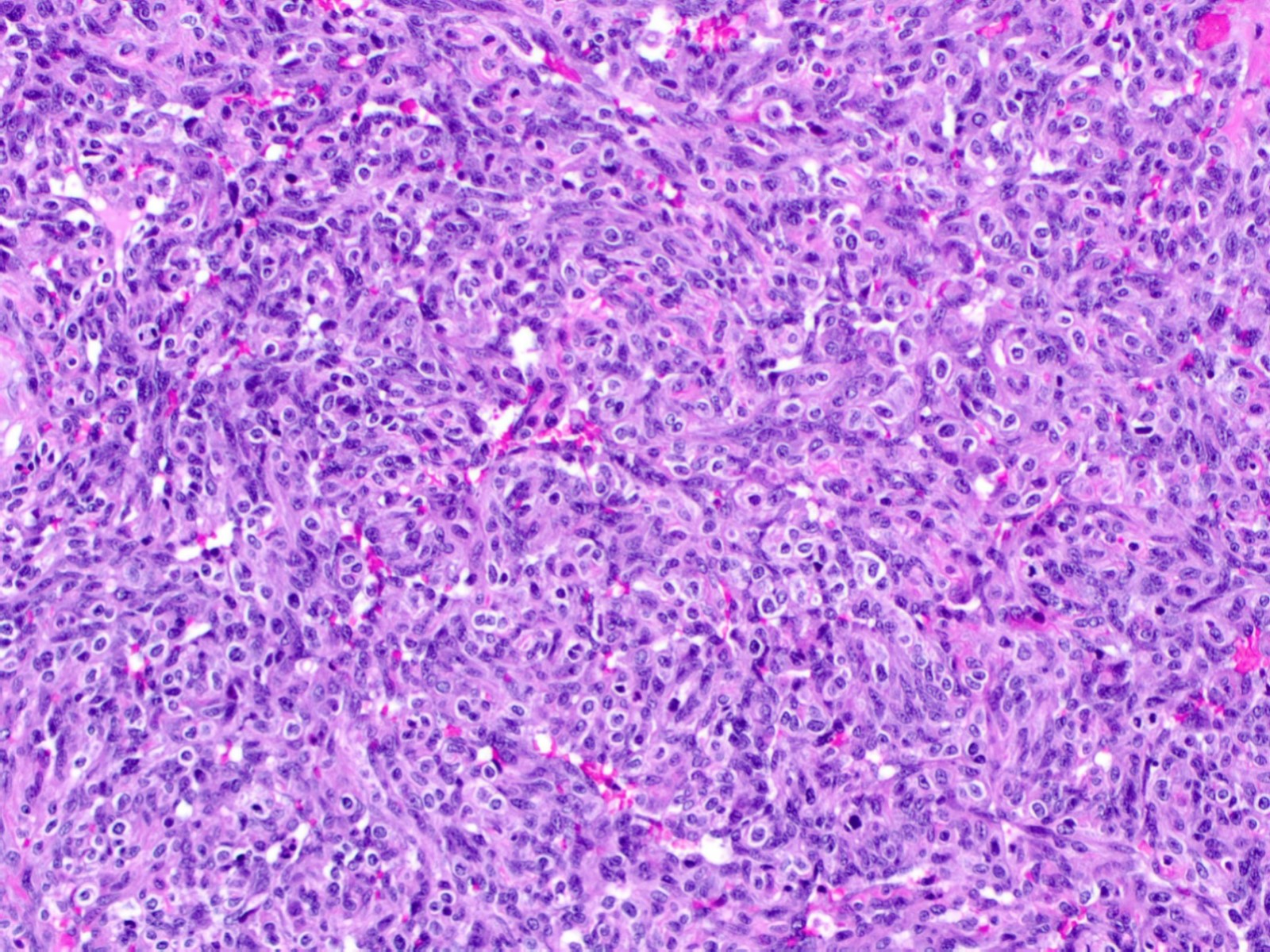
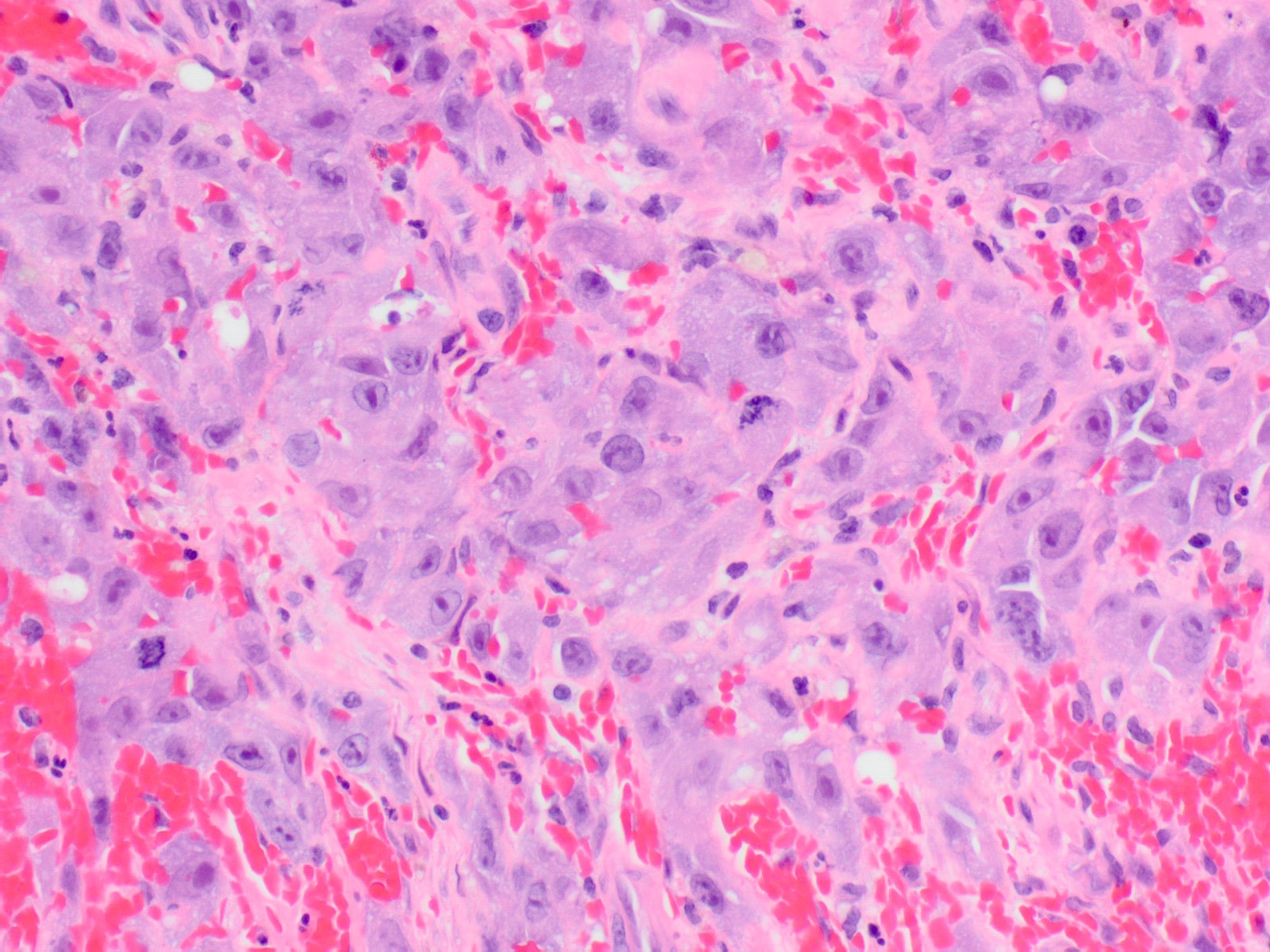
Microscopic (histologic) description
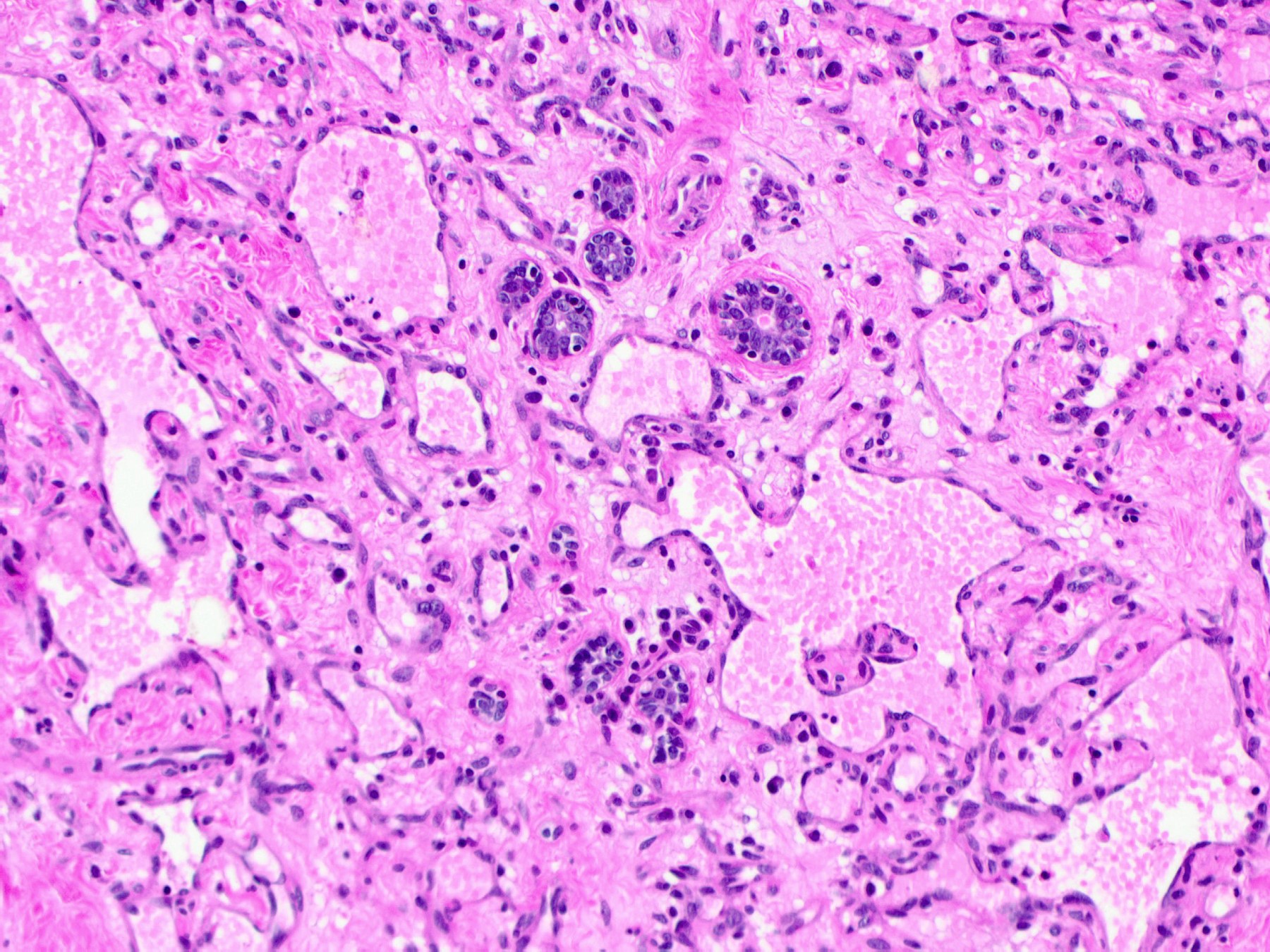
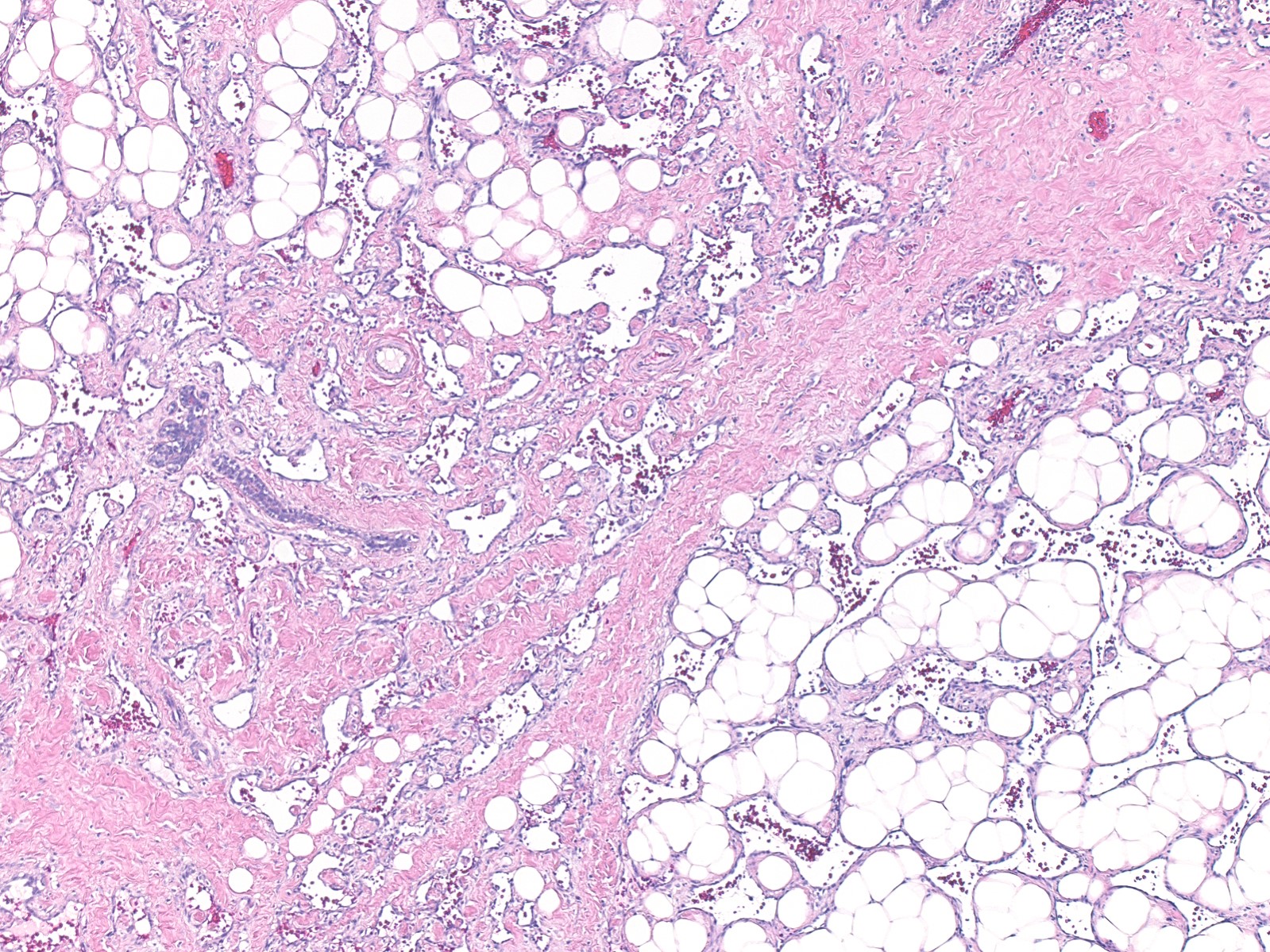
- Morphologic heterogeneity is typically present within individual tumors
- Irregular anastomosing vascular channels dissect through the stroma
- Infiltrative growth through normal structures (e.g., terminal duct lobular units)
- Poorly differentiated tumors often show solid growth of spindle or epithelioid cells with limited vasoformative features
- Necrosis and blood lakes can be seen in poorly differentiated tumors
- Endothelial cell atypia can range from minimal to marked
- Endothelial tufting and papillary formations are common
- Mitotic activity increases in proportion to grade
- Grading is based on a combination of histologic features (Table 1) (Am J Surg Pathol 1981;5:629)
- Low grade features are more common as a dominant finding in primary angiosarcomas
- Majority of postradiation angiosarcomas are high grade (Ann Surg Oncol 2013;20:1267, Ann Surg Oncol 2020;27:1002)
- All histologic grades of angiosarcoma may contain low grade areas, especially at the periphery of the tumor
Table 1. Histologic characteristics of different grades of mammary angiosarcoma
| Histologic features | Low grade | Intermediate grade | High grade |
| Endothelial cell atypia | Minimal | Moderate | Marked |
| Endothelial tufting | Minimal | Present | Prominent |
| Papillary formations | Absent | Focally present | Present |
| Solid and spindle cell foci | Absent | Absent or minimal | Present |
| Mitotic figures | Absent or rare | Present | Numerous and present in structurally low grade areas |
| Blood lakes (pools of extravasated erythrocytes) | Absent | Absent | Present |
| Necrosis | Absent | Absent | Present |
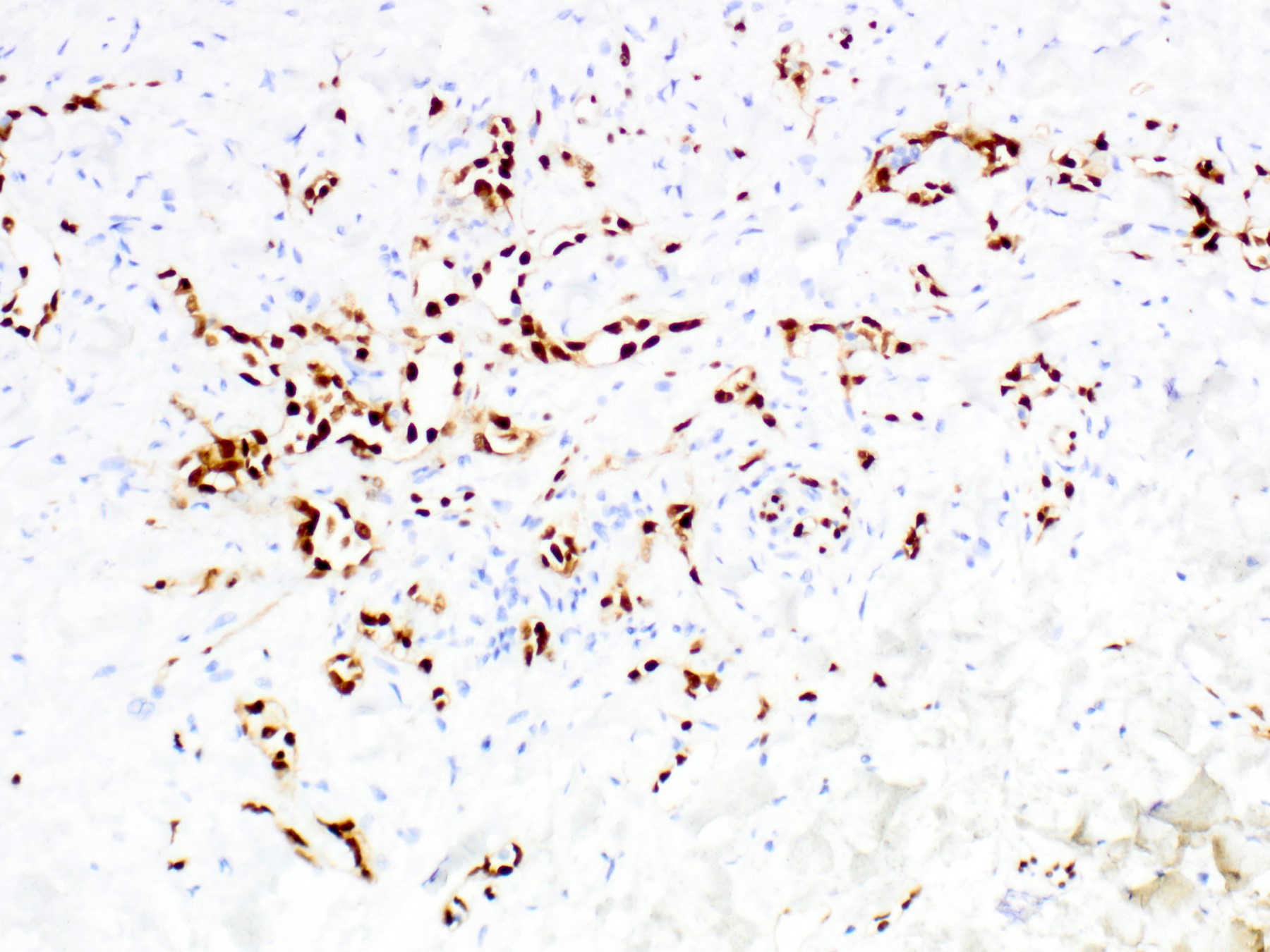
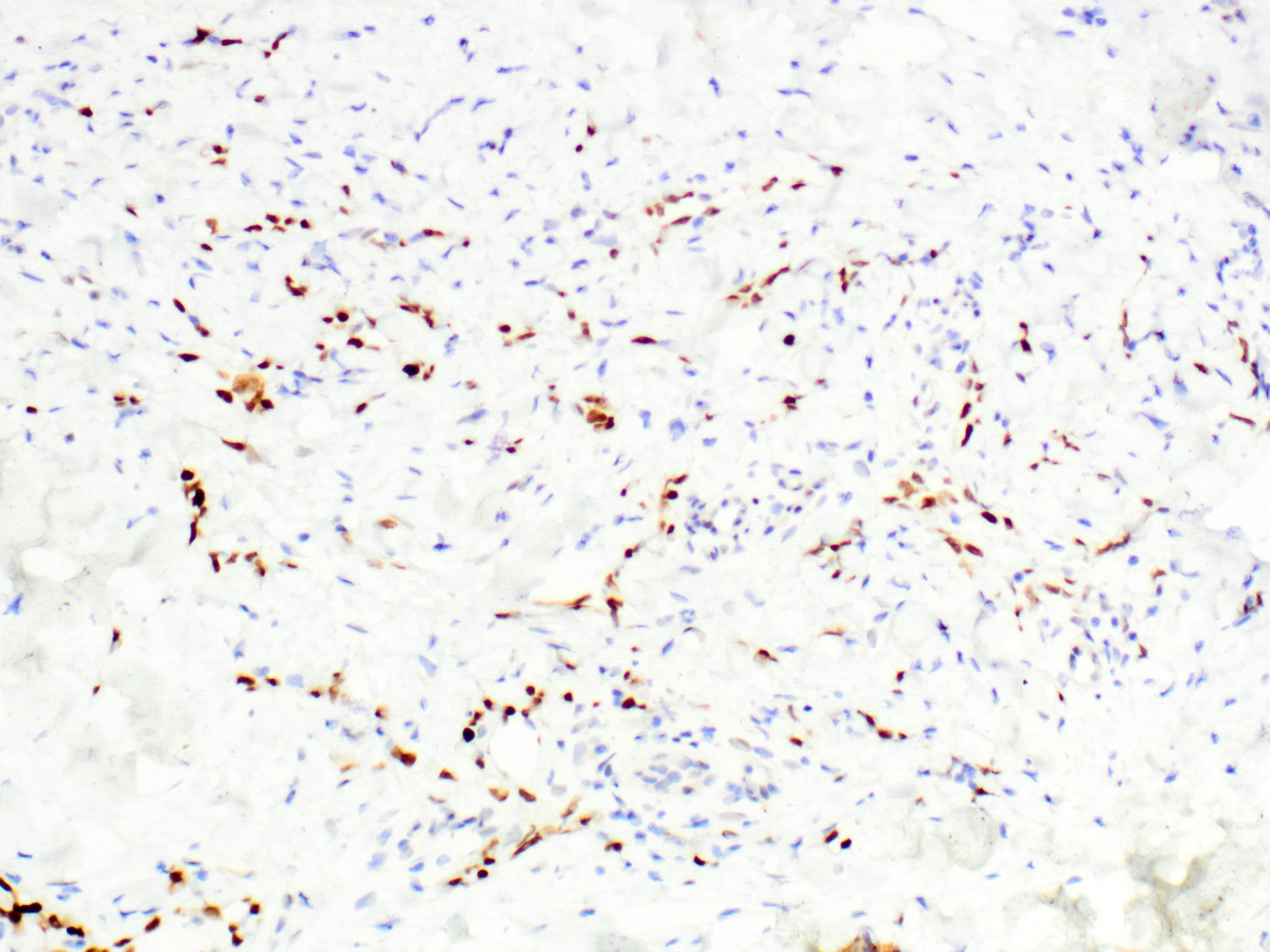
Microscopic (histologic) images
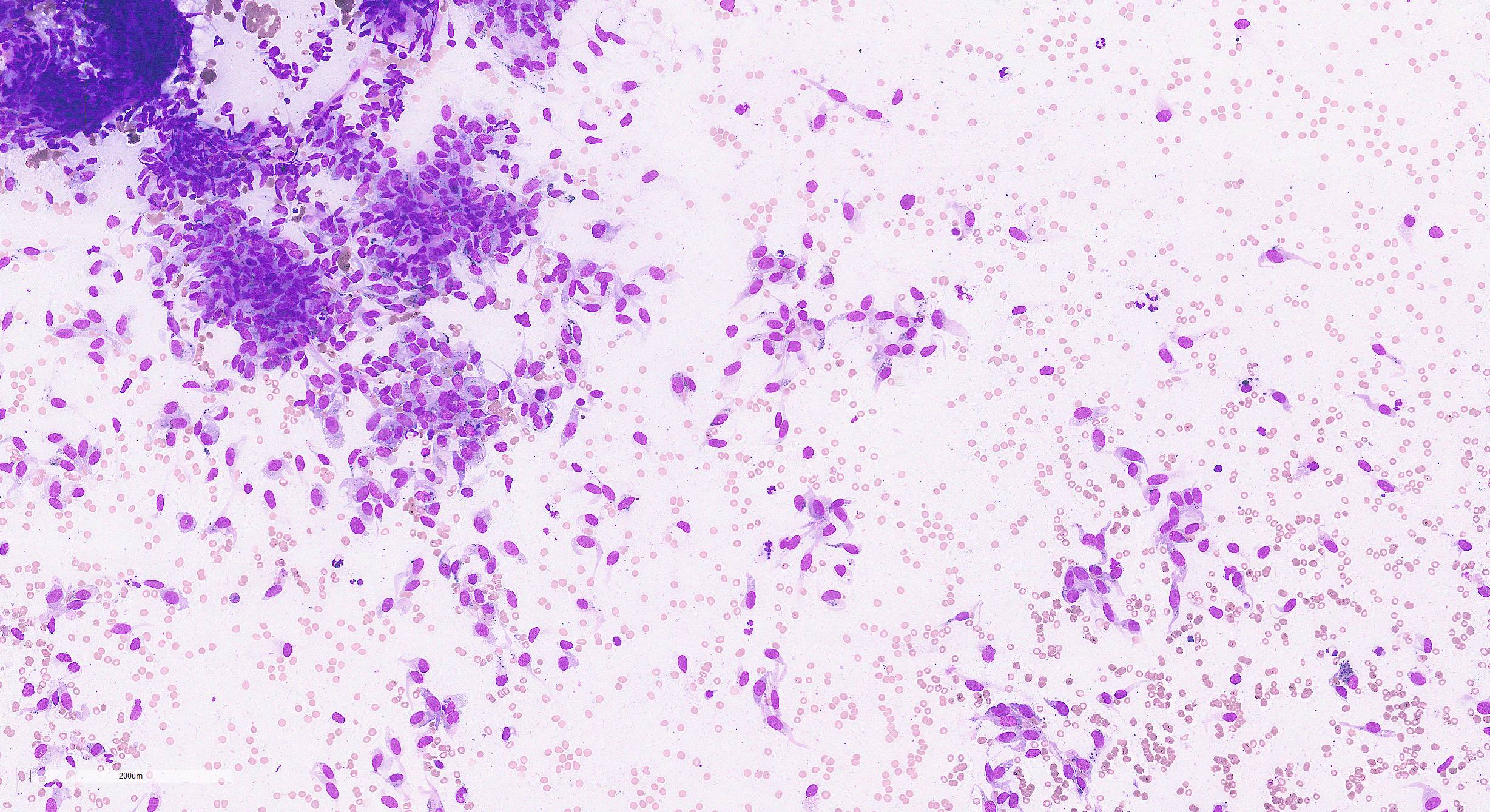
Cytology description
- Variable cellularity: specimens from well differentiated tumors tend to be hypocellular and bloody, while those from poorly differentiated tumors are usually more cellular
- Dispersed cells, cells in loose or cohesive groups or focal papillae with fibrovascular cores (Cancer Cytopathol 2016;124:659)
- Variable cellular morphology (spindle, epithelioid or mixed)
- Prominent epithelioid cells can mimic carcinoma
- Oval to spindled nuclei with variable pleomorphism
- Multiple nucleoli and bar or bullet shaped nucleoli are common; chromatin stranding may be seen (delicate radiating chromatin strands connecting the nucleolus to the nuclear membrane)
- Vasoformative features (hemophagocytosis, cytoplasmic lumina / vacuoles with red blood cells or neutrophils, endothelial wrapping) are often present but their prominence and extent vary
Positive stains
- CD31, ERG: strong and diffuse
- CD34, D2-40, Factor VIII, FLI1: variable, often strong and diffuse
- Cytokeratins and EMA: focal expression in epithelioid variants
- MYC: strong and diffuse nuclear positivity in postradiation angiosarcoma (Hum Pathol 2014;45:709)
Negative stains
- H3K27me3: loss or reduced expression in a subset of postradiation angiosarcomas (Histopathology 2021;79:836, Virchows Arch 2018;472:361)
- ER / PR / HER2
Electron microscopy description
- Groups of cells surrounded by basal lamina and closely associated with pericytes, with intercellular and intracellular lumina with or without red blood cells (Am J Surg Pathol 1998;22:683)
- Weibel-Palade bodies may be present (Hum Pathol 1985;16;144)
Molecular / cytogenetics description
- Postradiation angiosarcoma
- High level amplification of MYC at 8q24 in > 90% of cases (Genes Chromosomes Cancer 2011;50:25)
- Coamplification of FLT4 in 25% (Genes Chromosomes Cancer 2011;50:25)
- Angiosarcoma secondary to chronic lymphedema
- Can also show high level amplification of MYC (Am J Pathol 2010;176:34)
- Primary angiosarcoma
- Only rare cases show MYC amplification (Am J Surg Pathol 2016;40:645)
Videos
Postradiation angiosarcoma
Sample pathology report
- Breast, mastectomy:
- Post-radiation angiosarcoma (see comment)
- Comment: The angiosarcoma measures 7.5 x 5 cm and involves the skin and underlying breast parenchyma. The tumor is high grade with pleomorphic spindle and epithelioid cells, a high mitotic rate (up to 30 MF / 10 HPF) and focal areas of necrosis. By immunohistochemistry, the tumor cells are positive for CD31, CD34, D2-40, ERG and MYC and negative for pancytokeratin and S100, supporting the diagnosis. Angiosarcoma extends to 0.5 cm of the superior skin margin, 1 cm from the inferior skin margin and is greater than 2 cm from the remaining margins.
Differential diagnosis
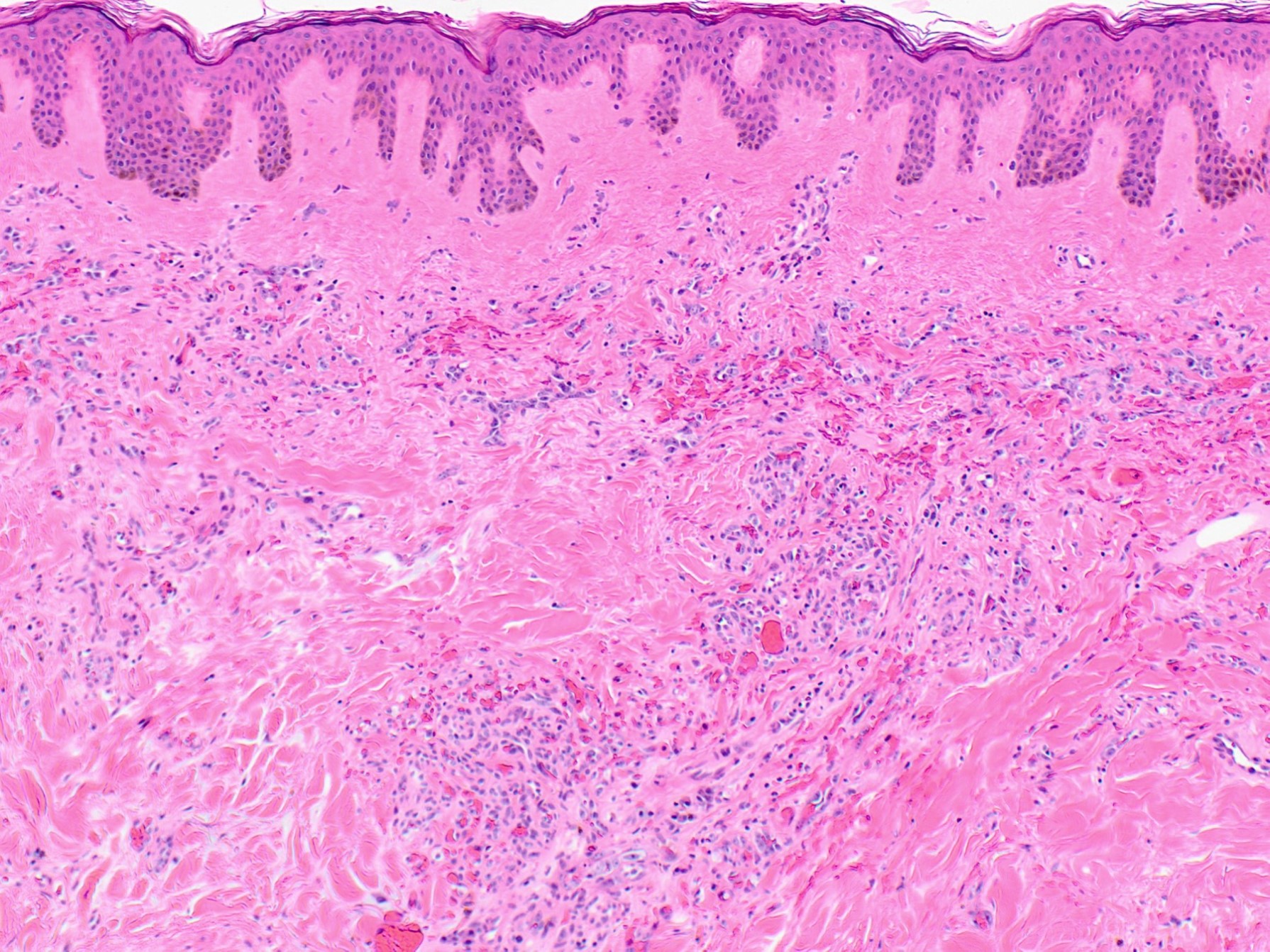
- Atypical vascular lesion:
- Small vascular proliferation occurring in the dermis of irradiated skin
- Most lesions are < 1 cm in size (and often < 0.5 cm)
- Relatively circumscribed, often wedge shaped proliferation of thin walled vessels within the superficial to mid dermis
- Lacks evidence of infiltration
- No significant endothelial atypia or proliferation
- Lacks amplification of MYC and negative or only weakly reactive for MYC by immunohistochemistry
- Clinicopathological correlation is needed to ensure that the biopsy does not represent sampling at the edge of an angiosarcoma
- Hemangioma:
- Well defined
- No destructive invasion of terminal duct lobular units
- Flattened endothelial cells without atypia or significant mitotic activity
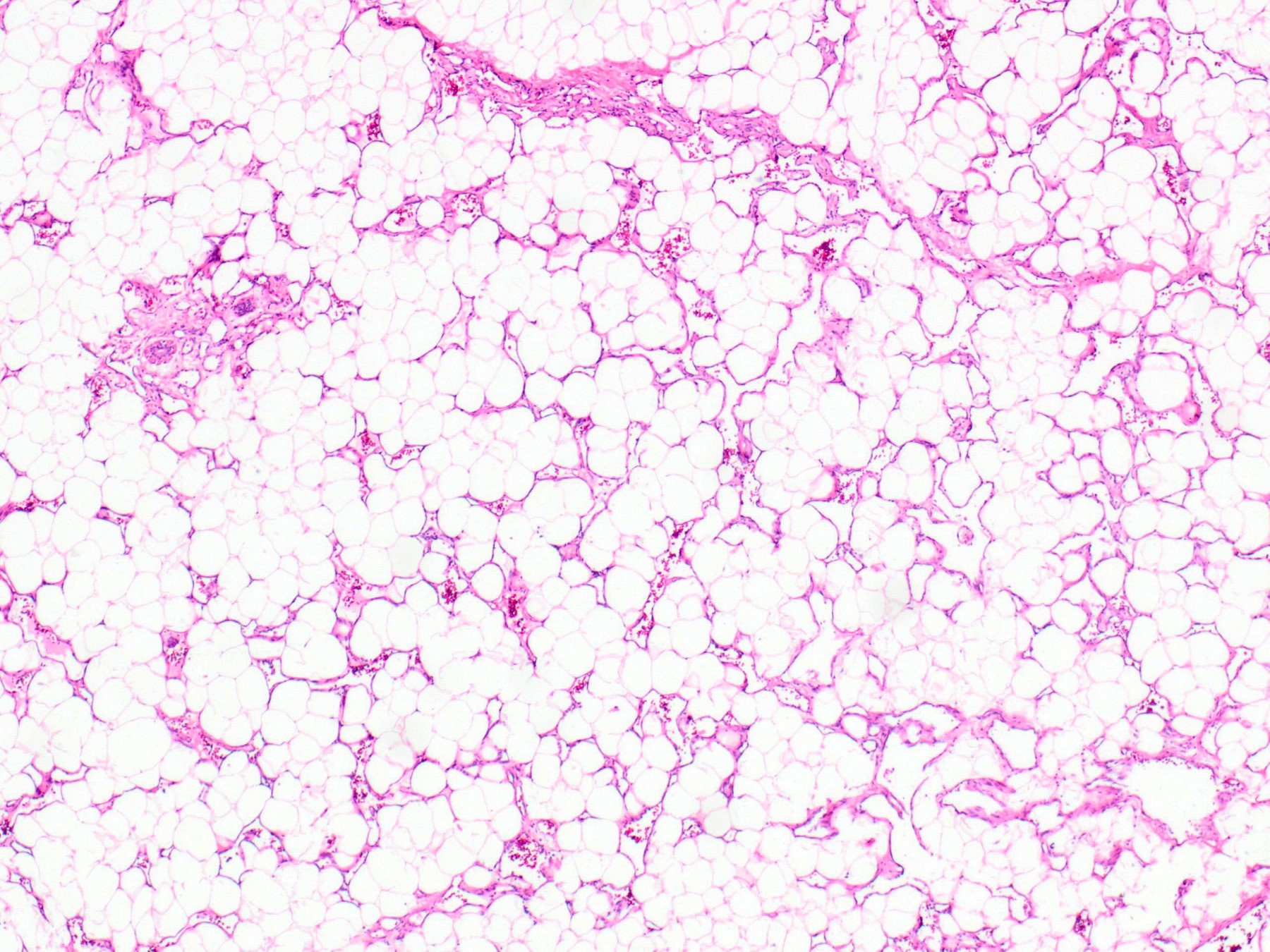
- Angiomatosis:
- Very rare benign vascular proliferation involving large areas of breast parenchyma
- Large dilated vascular channels permeate the breast but show exquisite sparing of the terminal duct lobular units, unlike angiosarcoma
- No endothelial atypia, stratification or notable mitotic activity
- Carcinoma:
- Evidence of epithelial differentiation or in situ carcinoma
- Negative for vascular markers
Additional references
Board review style question #1
Which of the following is true regarding postradiation angiosarcoma of the breast?
- Greater than 90% are low grade
- Incidence of 10% among patients receiving breast irradiation for breast cancer treatment
- Most often arises in the breast parenchyma and then secondarily involves the skin
- Patients have a median age of 40 years
- Shows strong positivity for MYC by immunohistochemistry
Board review style answer #1
E. Shows strong positivity for MYC by immunohistochemistry. Greater than 90% of postradiation angiosarcomas of the breast show high level amplification of MYC and corresponding strong overexpression of MYC by immunohistochemistry. Postradiation angiosarcoma develops in 0.03 - 0.14% of patients after radiation therapy for the treatment of breast cancer. Reflective of that cohort, the mean age is 70 years. Most postradiation angiosarcomas arise in the skin (from which they may secondarily involve the breast parenchyma) and the majority are of high histologic grade.
Comment Here
Reference: Angiosarcoma
Comment Here
Reference: Angiosarcoma
Board review style question #2
A 27 year old woman with no significant prior medical history presents with an 8 cm poorly defined left breast mass. A representative histological image is shown above. What is the most likely diagnosis?
- Atypical vascular lesion of the skin
- Capillary hemangioma
- Low grade angiosarcoma
- Pseudoangiomatous stromal hyperplasia
- Spindle cell carcinoma with acantholytic pattern
Board review style answer #2
C. Low grade angiosarcoma. The illustrated lesion is a primary, low grade angiosarcoma of the breast parenchyma. It demonstrates irregularly shaped, anastomosing vascular channels that dissect through the fat and collagen and around normal glandular structures. This pattern of destructive invasion distinguishes it from benign vascular proliferations.
Comment Here
Reference: Angiosarcoma
Comment Here
Reference: Angiosarcoma