Table of Contents
Definition / general | Essential features | Terminology | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Radiology description | Radiology images | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Javadi T, Ai D. Benign breast implant related changes . PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/breastimplantchanges.html. Accessed April 2nd, 2025.
Definition / general
- Saline and silicone breast implants are suitable for use in augmentation mammaplasty and breast reconstruction following mastectomy
- Soft tissue surrounding breast implants can display various benign histological findings over time, including dense fibrosis (capsule), chronic inflammation, granulomatous reaction, calcification and synovial metaplasia (Aesthetic Plast Surg 2010;34:481)
- Implant associated reactions vary based on the implant composition, duration and mechanical forces along the capsule and if violated / ruptured (Biomaterials 2003;24:1101)
Essential features
- Capsules can form around breast implants over time, especially silicone type implants
- Chronic movement and gliding of the implant in its cavity produces benign changes along the implant capsule interface with associated clinical and histological findings (Acta Cytol 2014;58:511)
- Implant related changes include dense fibrosis, chronic inflammation / granulomatous reaction, calcification and synovial metaplasia
- Leaking or rupture of silicone implant leads to silicone granuloma, which consists of amorphous / crystalline material with a foreign body giant cell reaction
- Synovial metaplasia can be noted, which consists of epithelioid cells lining the inner capsular surface with a well developed reticulin network histologically indistinguishable from normal joint synovium
Terminology
- Synovial metaplasia is also referred to as synovial-like reaction or synovial-like metaplasia
Epidemiology
- Occurs in smooth and textured silicone surfaced breast implants as well as in saline filled and polyurethane coated implants (Plast Reconstr Surg 1997;100:1558, Biomaterials 2003;24:1101)
- Risk of implant related changes increases with prolonged implant duration
- Textured surface breast implants with a duration of 0 - 5 years exhibit the highest incidence of synovial metaplasia (Biomaterials 2003;24:1101)
- Risk of rupture increases with duration, with a minimum of 15% estimated to rupture between the third and tenth year after implantation in a cohort followed by MRI (Arch Surg 2003;138:801)
Sites
- Breast implant capsule interface
Pathophysiology
- Inflammatory changes
- Immune recognition of breast implants as foreign results in inflammatory response, leading to the formation of scar (capsule) around the implant, which may contract and cause the implant to feel hard or change shape
- Thick, fibrous capsule is formed as a host reaction to foreign material (implant) or possibly as a form of repair
- Breast implant related changes can lead to other complications, such as implant rupture or displacement and breast implant associated anaplastic large cell lymphoma (BIA-ALCL) in the context of textured implants (Plast Reconstr Surg 2017;140:645)
- Synovial metaplasia
- Persistent movement of the implant induces a local cellular response along the inner capsular surface that evolves into an organized synovial-like structure resembling normal joint synovium (Plast Reconstr Surg 1995;96:1747)
Clinical features
- Usually delayed onset of symptoms
- Pain with or without swelling
- Distortion / capsular contracture
- Excessive firmness of breast
- Infection
- Reference: Plast Reconstr Surg 1997;100:1558
Diagnosis
- History of breast implant
- Clinically presents in the setting of suspected silicone leak or implant rupture
- Nonspecific imaging findings, including fibrous capsule thickening
- Can mistakenly raise suspicion for breast implant associated anaplastic large cell lymphoma (BIA-ALCL) or infection (Clin Imaging 2020;59:144)
- Capsulectomy, with histopathologic evaluation
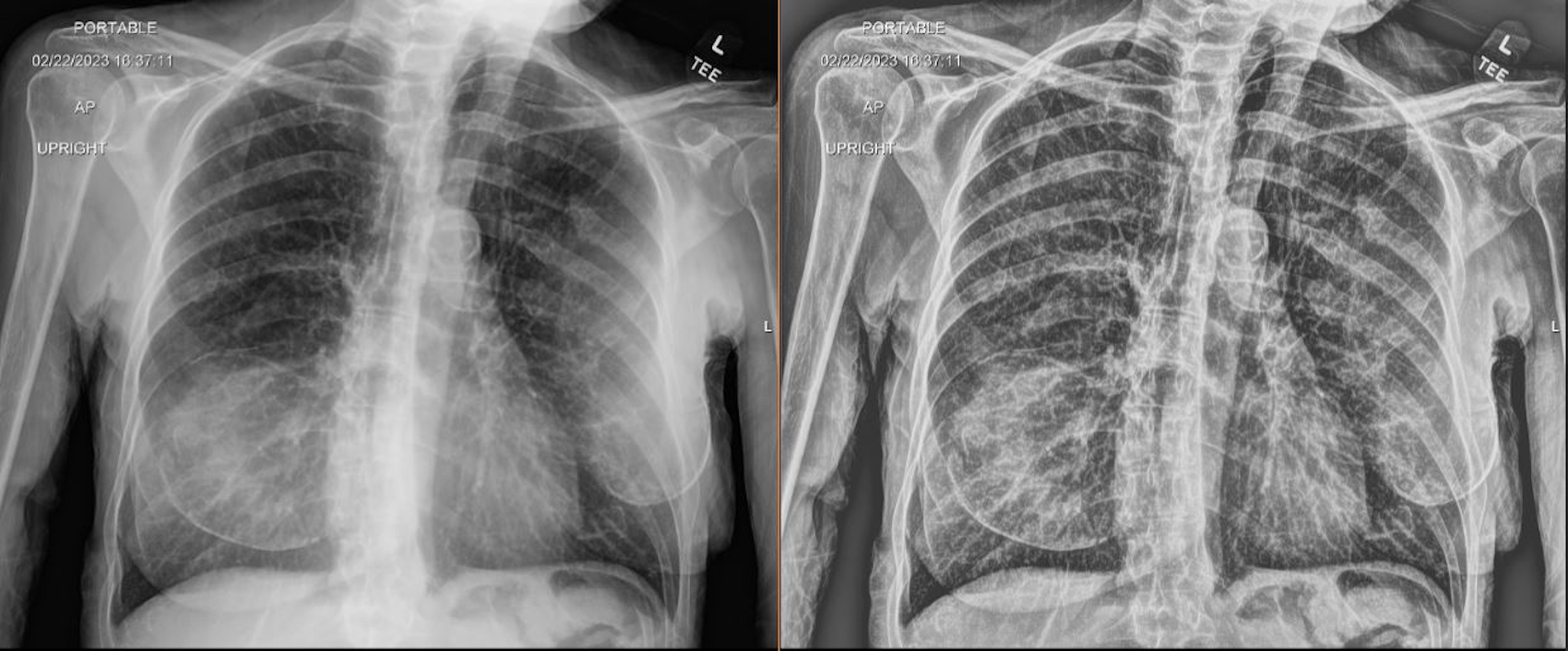
Radiology description
- Capsular thickening with or without peri-implant fluid on breast ultrasound / MRI (Clin Imaging 2020;59:144)
- MRI has high accuracy in diagnosing silicone implant rupture (Eur Radiol 2014;24:1167)
- Ruptured implant: asymmetric circumferential increased density can be seen on mammography
Radiology images
Contributed by Di Ai, M.D., Ph.D., Kristen E. Muller, D.O. and Samantha A. Stephen, D.O. (Case #530)
Case reports
- 25 year old woman with peri-implant fluid collection mimicking implant rupture / silicone leak, 1 year after bilateral breast augmentation (J Med Case Rep 2008;2:277)
- 53 year old woman undergoing surgery for capsular contracture of textured, silicone breast implants (Diagn Cytopathol 2018;46:769)
- 55 year old HIV+ transgender woman with sudden onset breast skin thickening and swelling, 9 years after bilateral saline breast implant mammoplasty (Clin Imaging 2020;59:144)
- 66 year old woman with a history of invasive lobular carcinoma and bilateral mastectomy with breast implant reconstruction developed rib pain (Case of the month #530)
Treatment
- Surgical excision is the choice of treatment for capture contracture (Breast J 2003;9:428)
- Implant replacement is the choice of treatment for silicone implant leakage (Hoda: Rosen's Breast Pathology, 5th Edition, 2020)
Gross description
- Silicon implant rupture
- Implant ruptures may be intracapsular or extracapsular
- An intracapsular rupture occurs when the shell of the implant ruptures but the formed fibrous capsule remains intact; silicone does not extravasate freely
- An extracapsular rupture occurs when the formed capsule ruptures, which can lead to a change in the implant contour
- Implant ruptures may be intracapsular or extracapsular
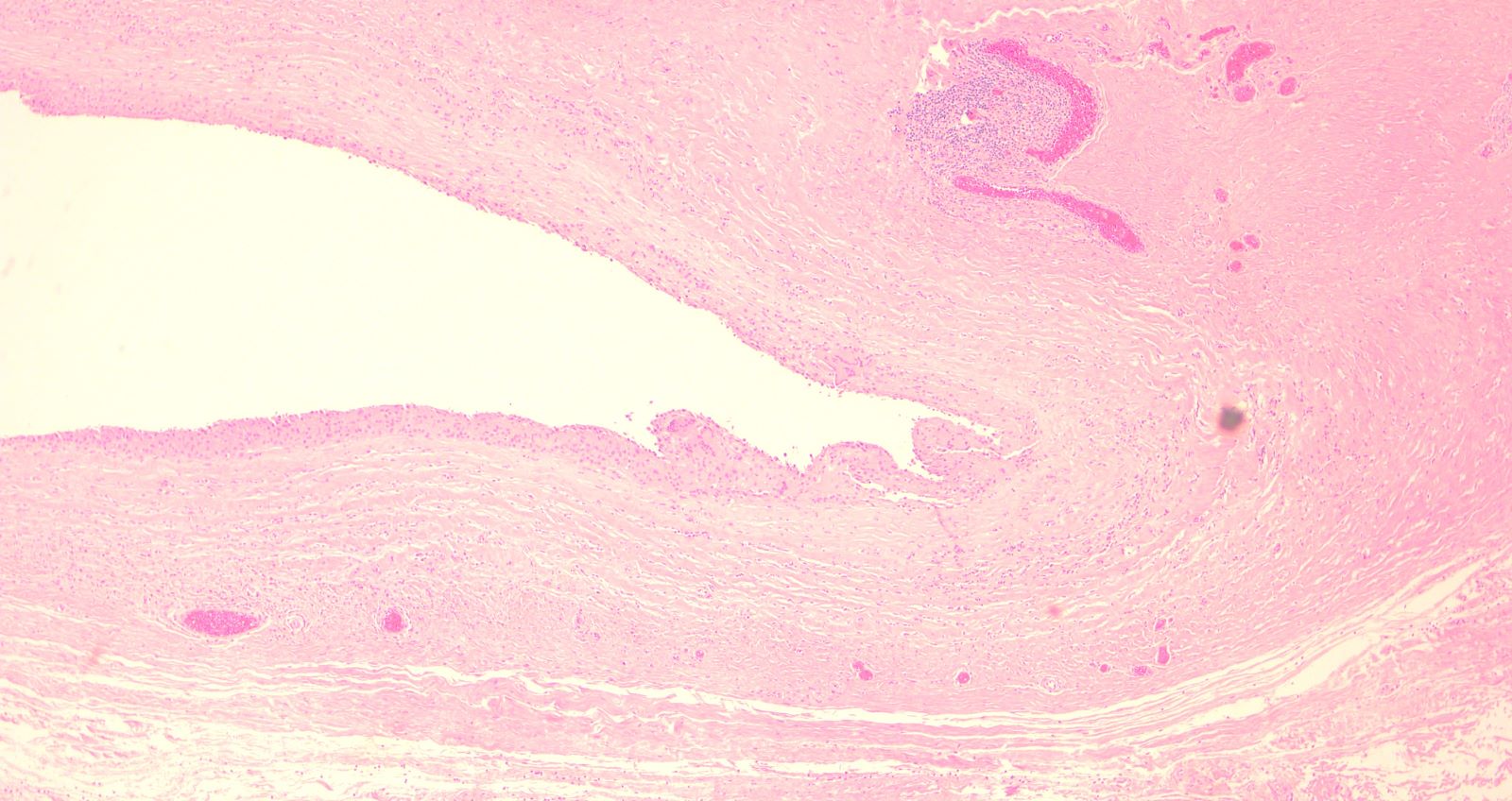
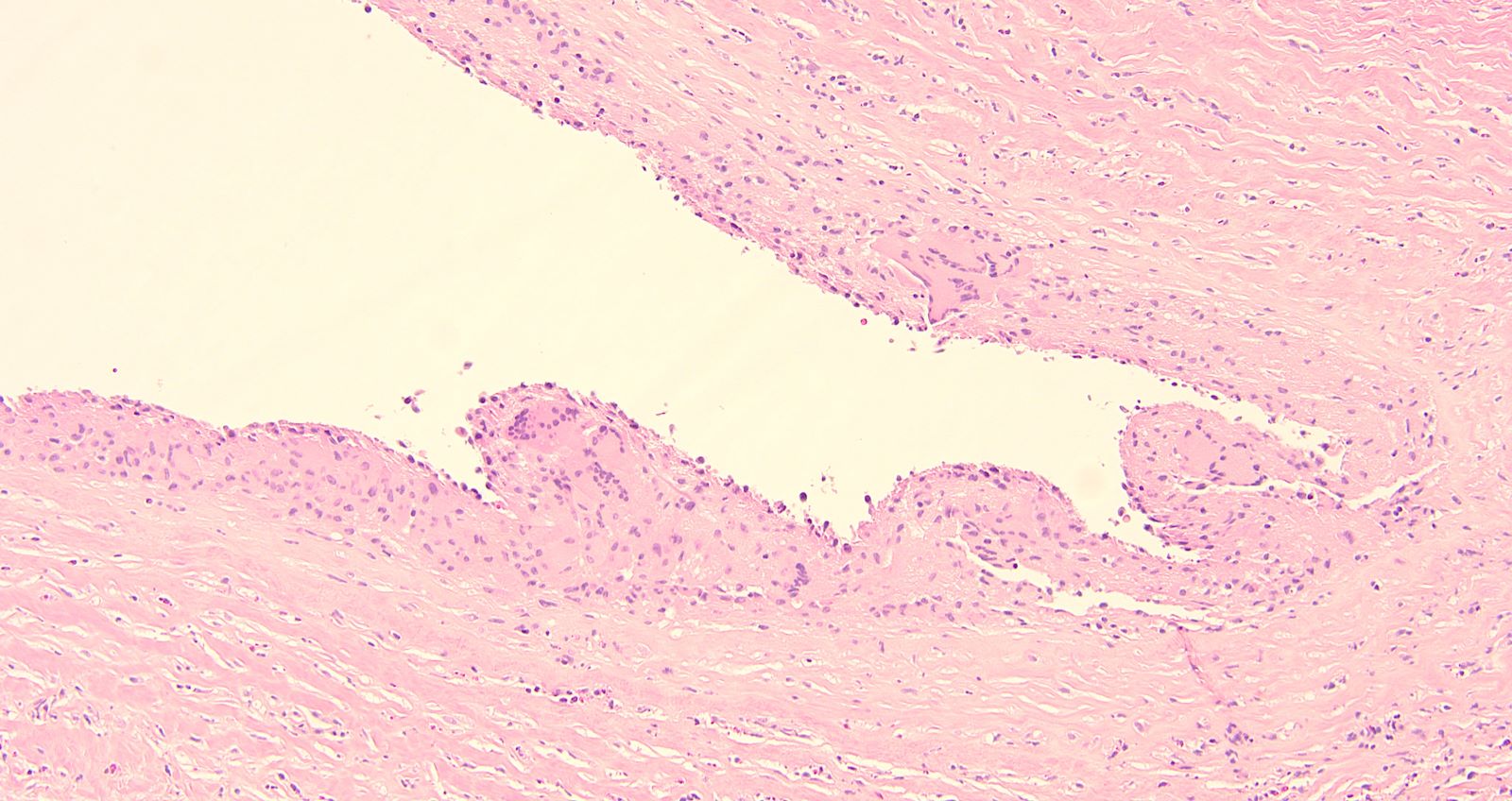
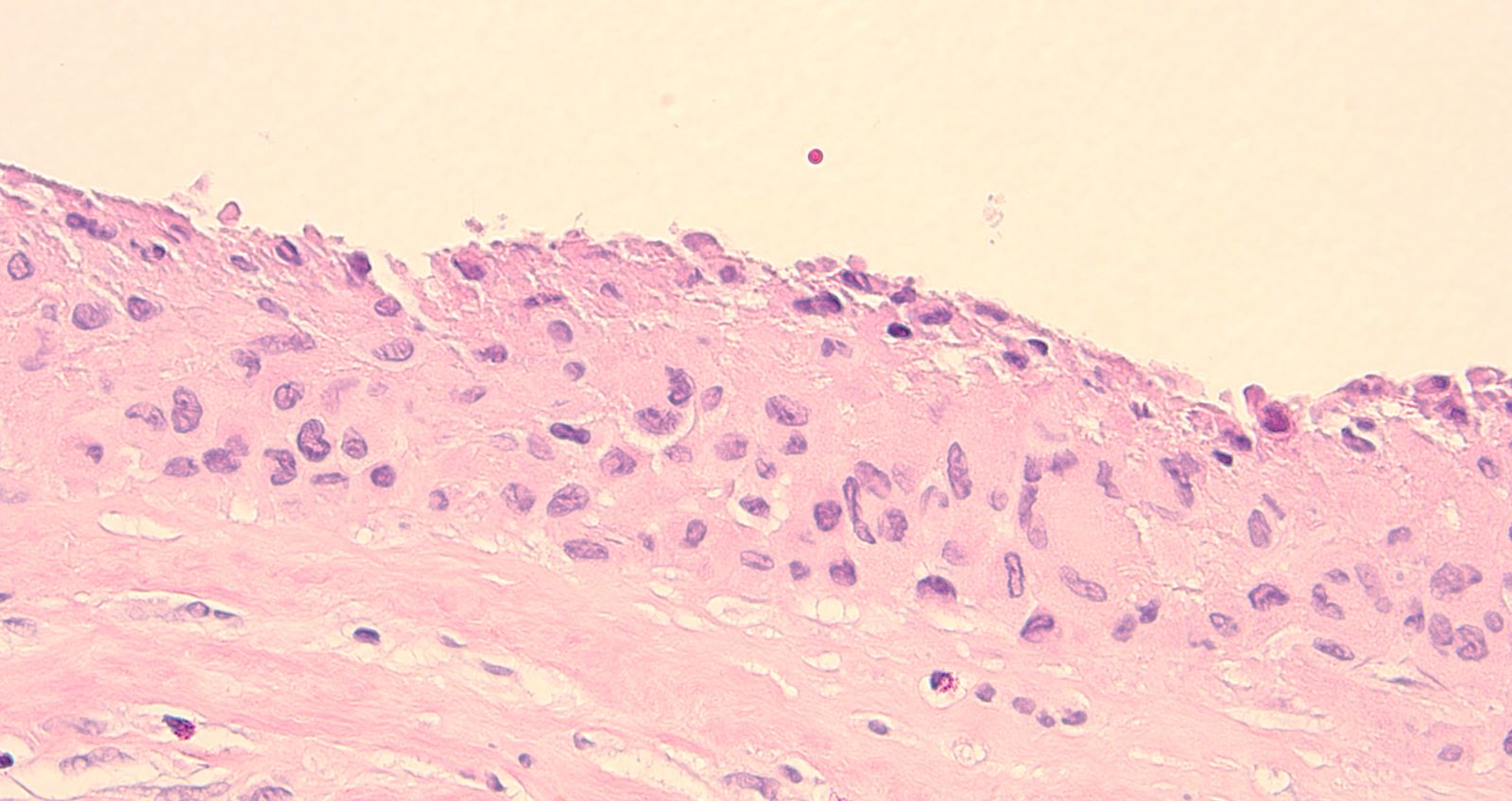
Microscopic (histologic) description
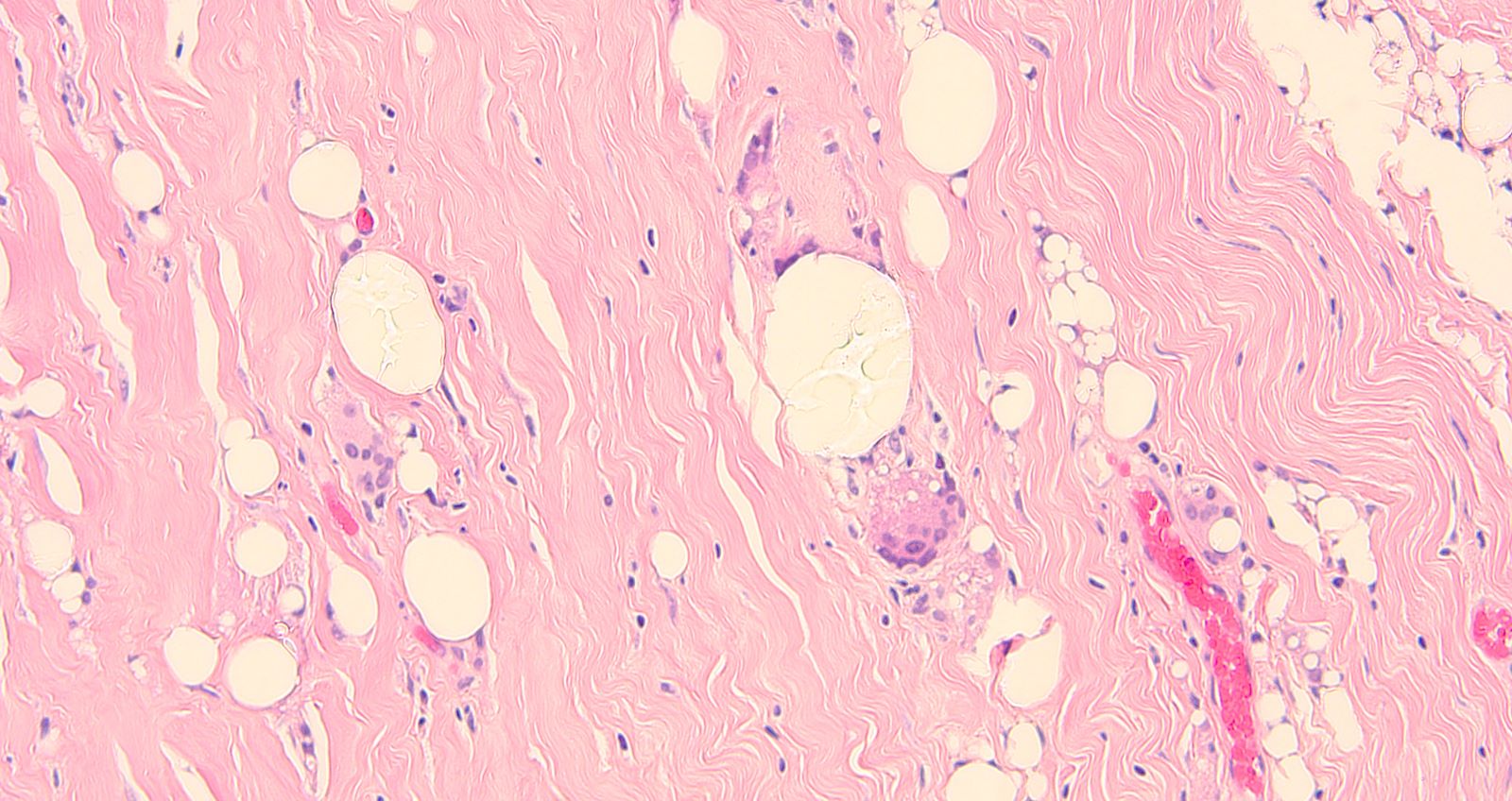
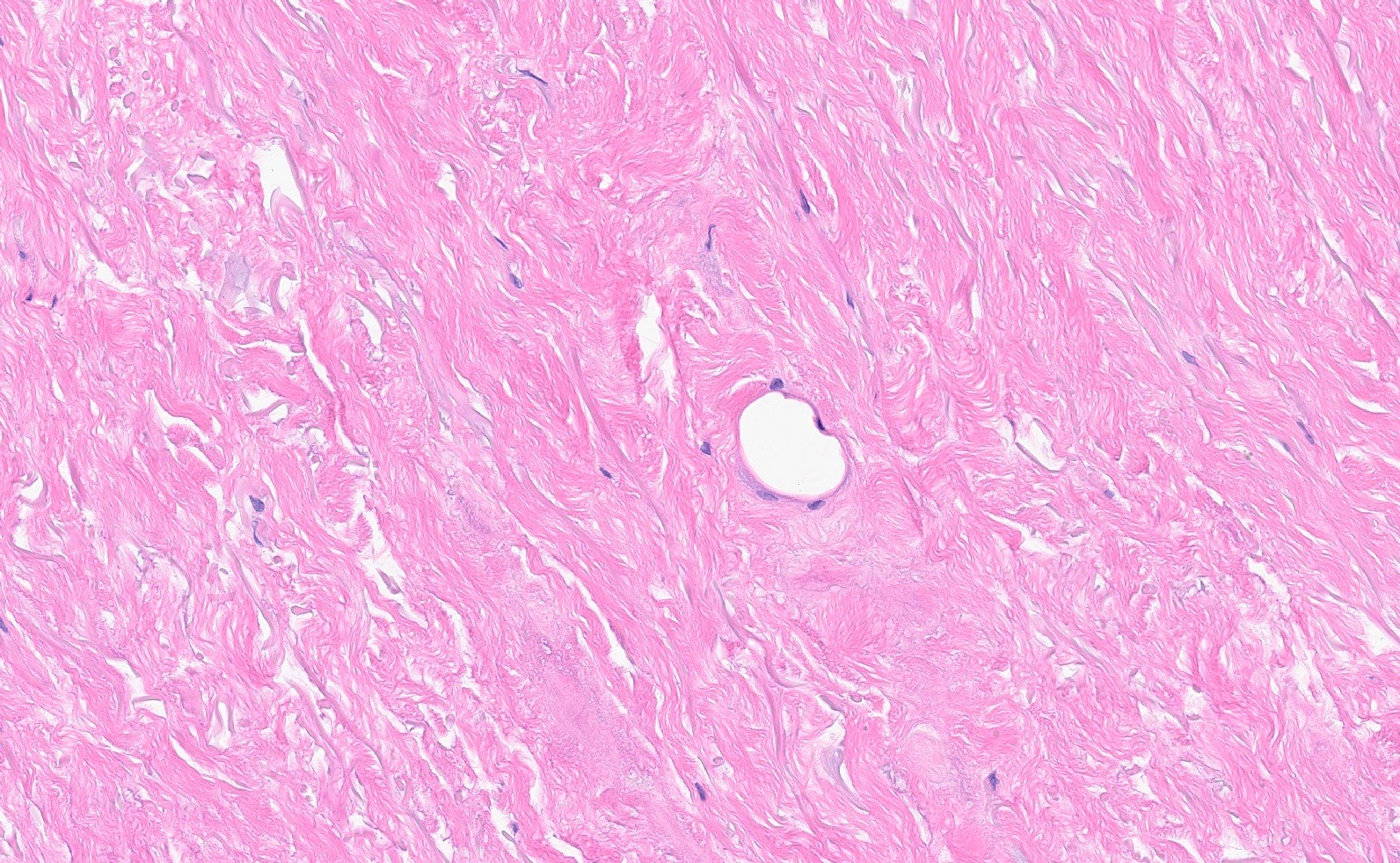
- Thickened fibrosis (capsule) with varying degrees of chronic inflammation, fat necrosis, foreign body giant cell reaction, hemosiderin laden macrophages, calcifications
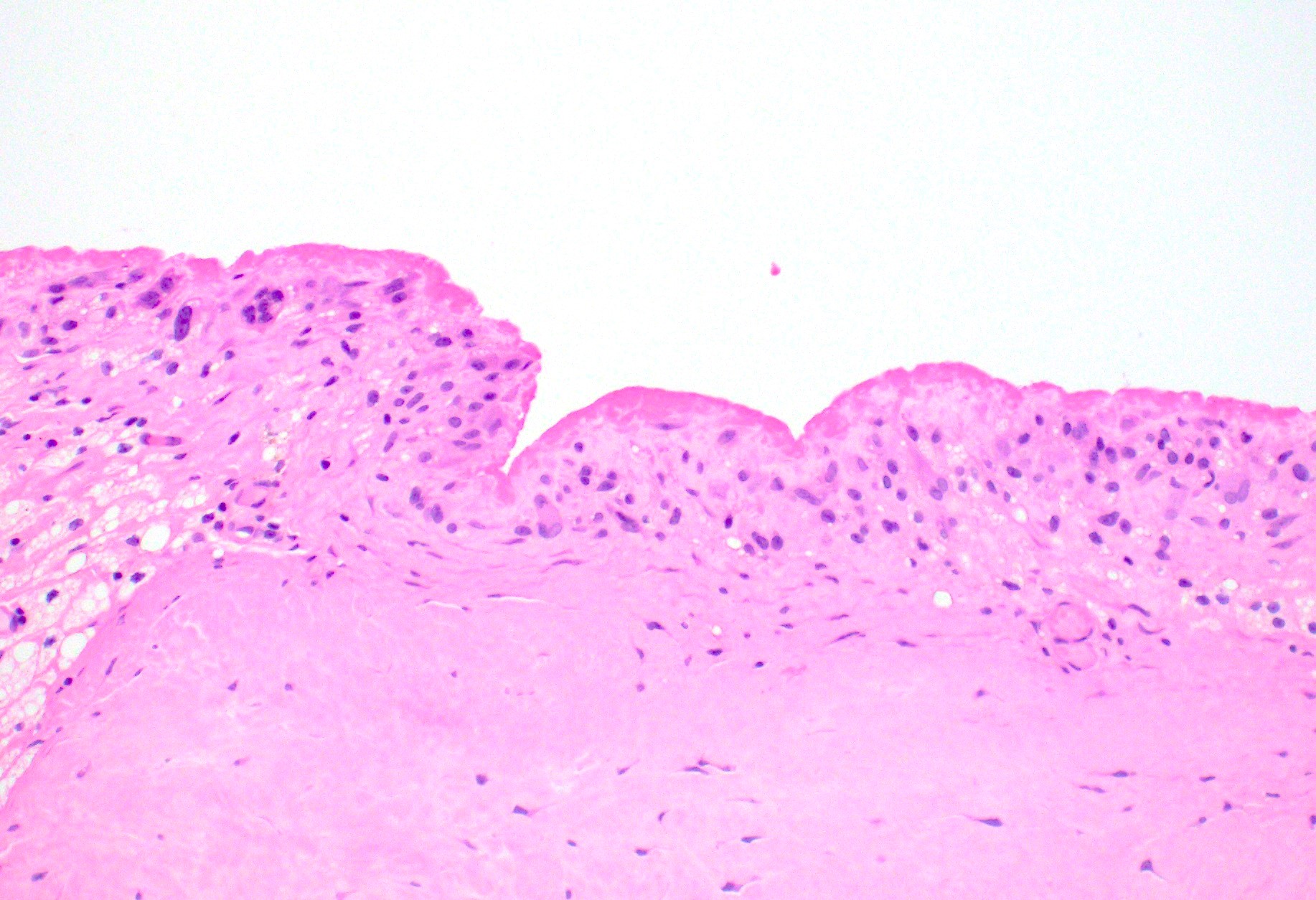
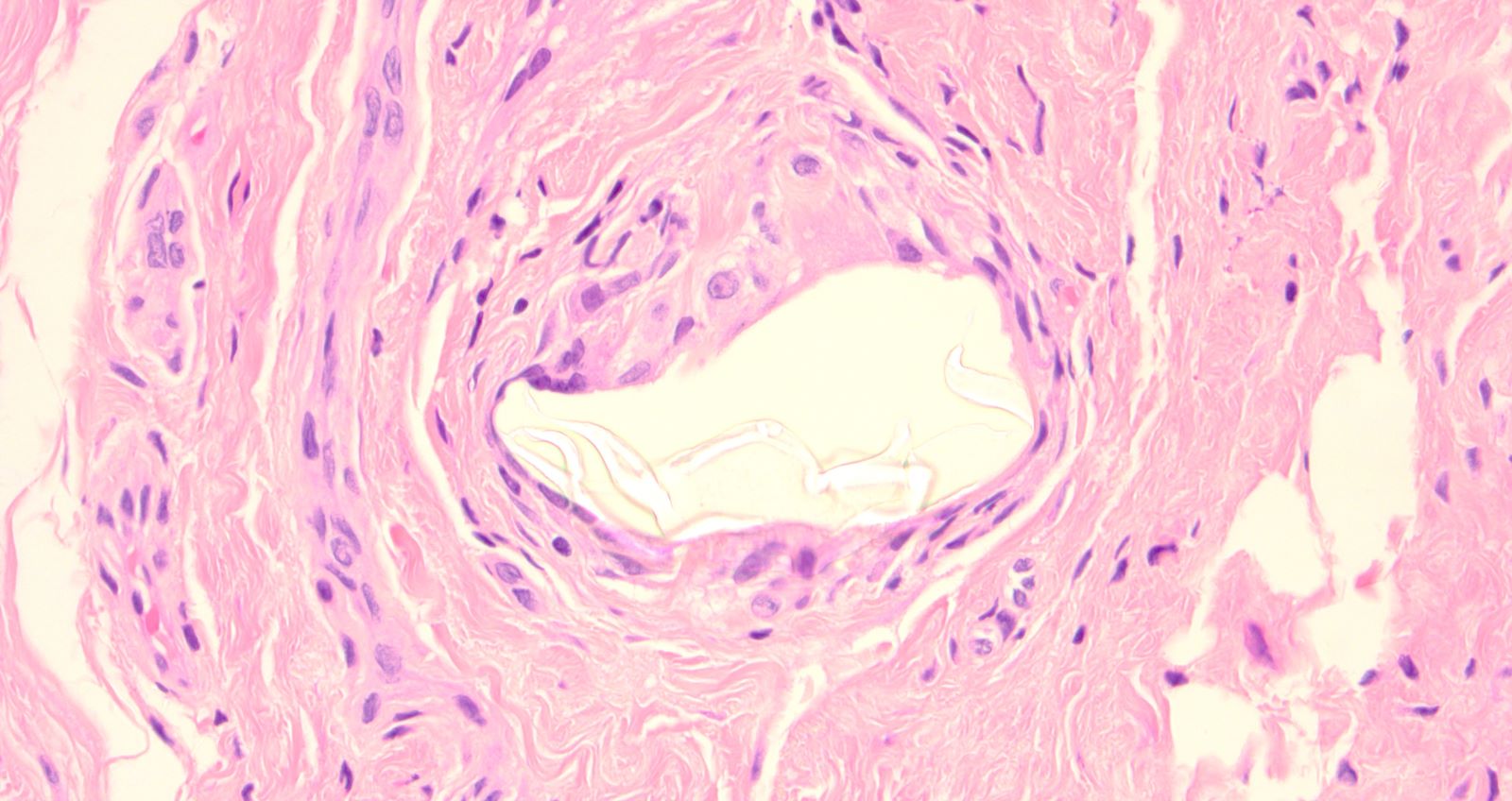
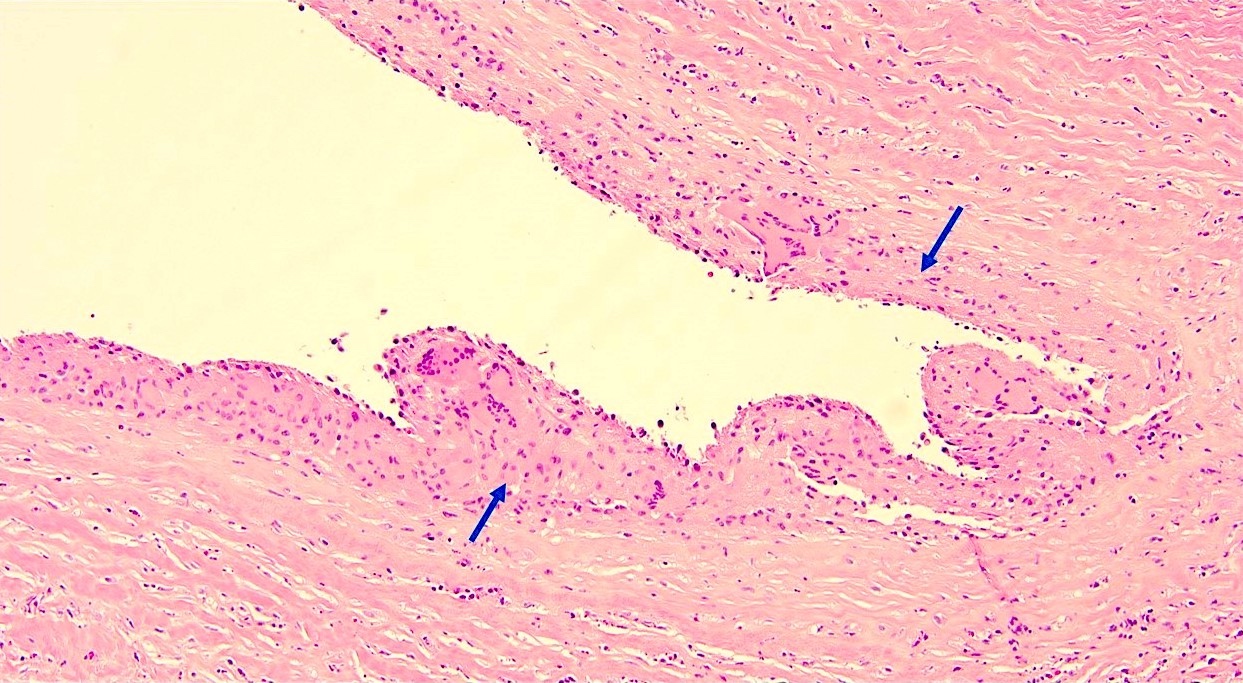
- Synovial metaplasia
- Consists of a layer that is 1 - 7 cells thick, lined by epithelioid cells arranged in a palisading pattern and embedded in a well developed reticulin network
- Cells are perpendicularly oriented with round to oval fibroblast-like nuclei, inconspicuous nucleoli and abundant eosinophilic cytoplasm
- No atypia
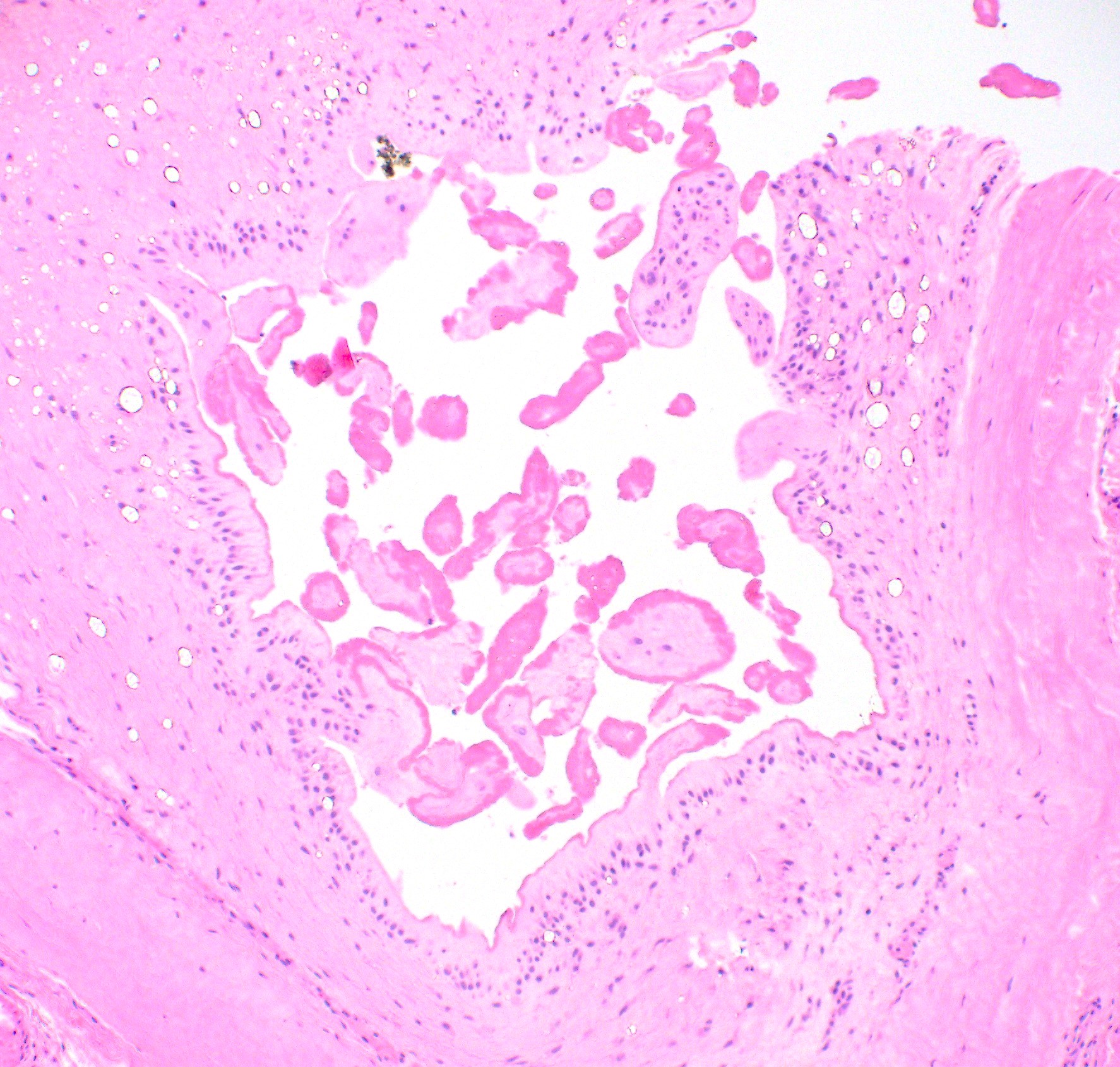
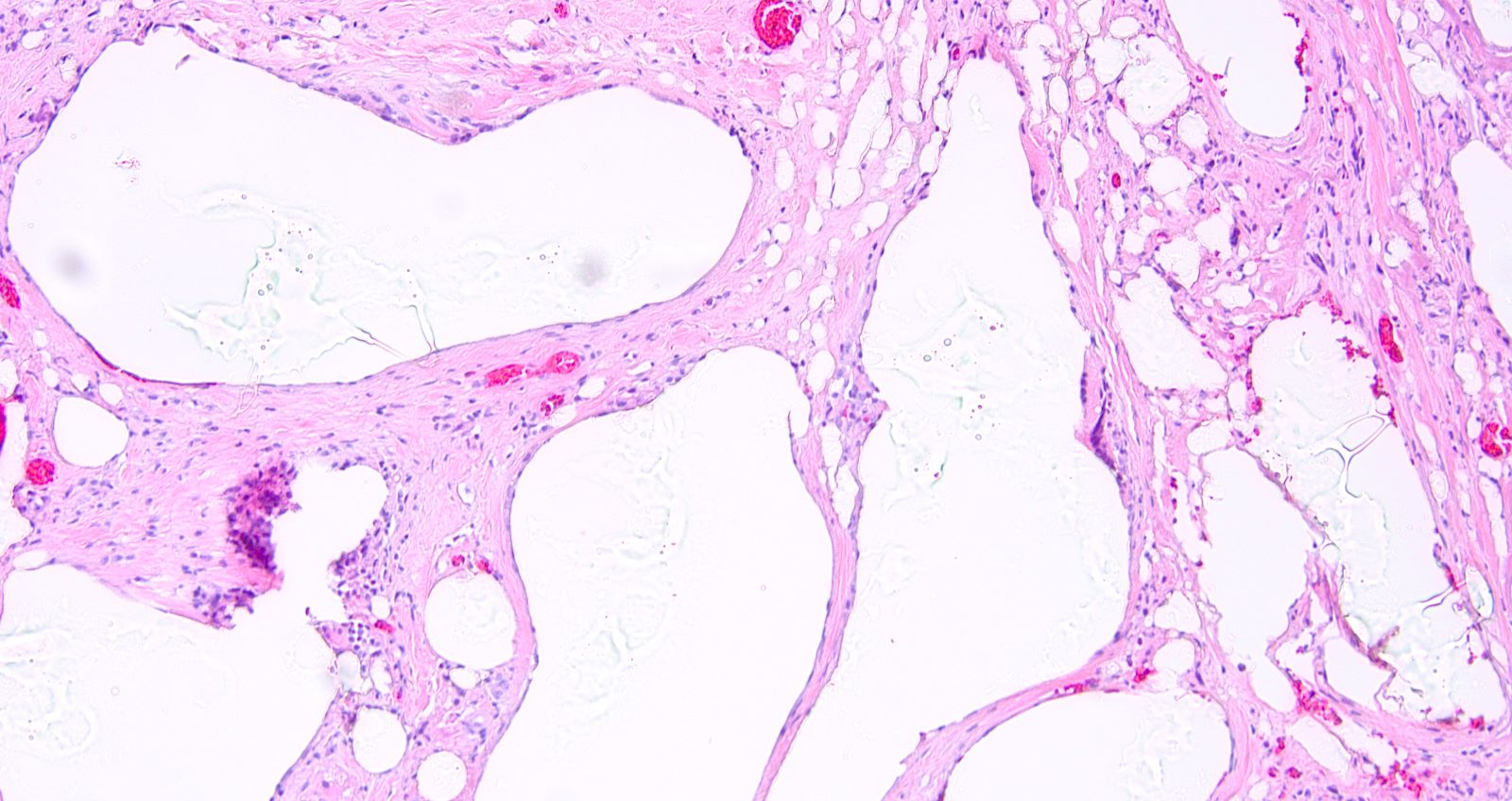
- Silicone granuloma
- Multiple cystic spaces and vacuoles partially filled with silicone granules and surrounded by fibrosis with accompanying local foreign body giant cell reaction, foamy histiocytes and lymphocytes (J Clin Pathol 1998;51:493)
- Usually secondary to extracapsular implant rupture
- Silicone gel leakage may be seen even in the absence of implant rupture
- References: Biomaterials 2003;24:1101, Aesthetic Plast Surg 2010;34:481
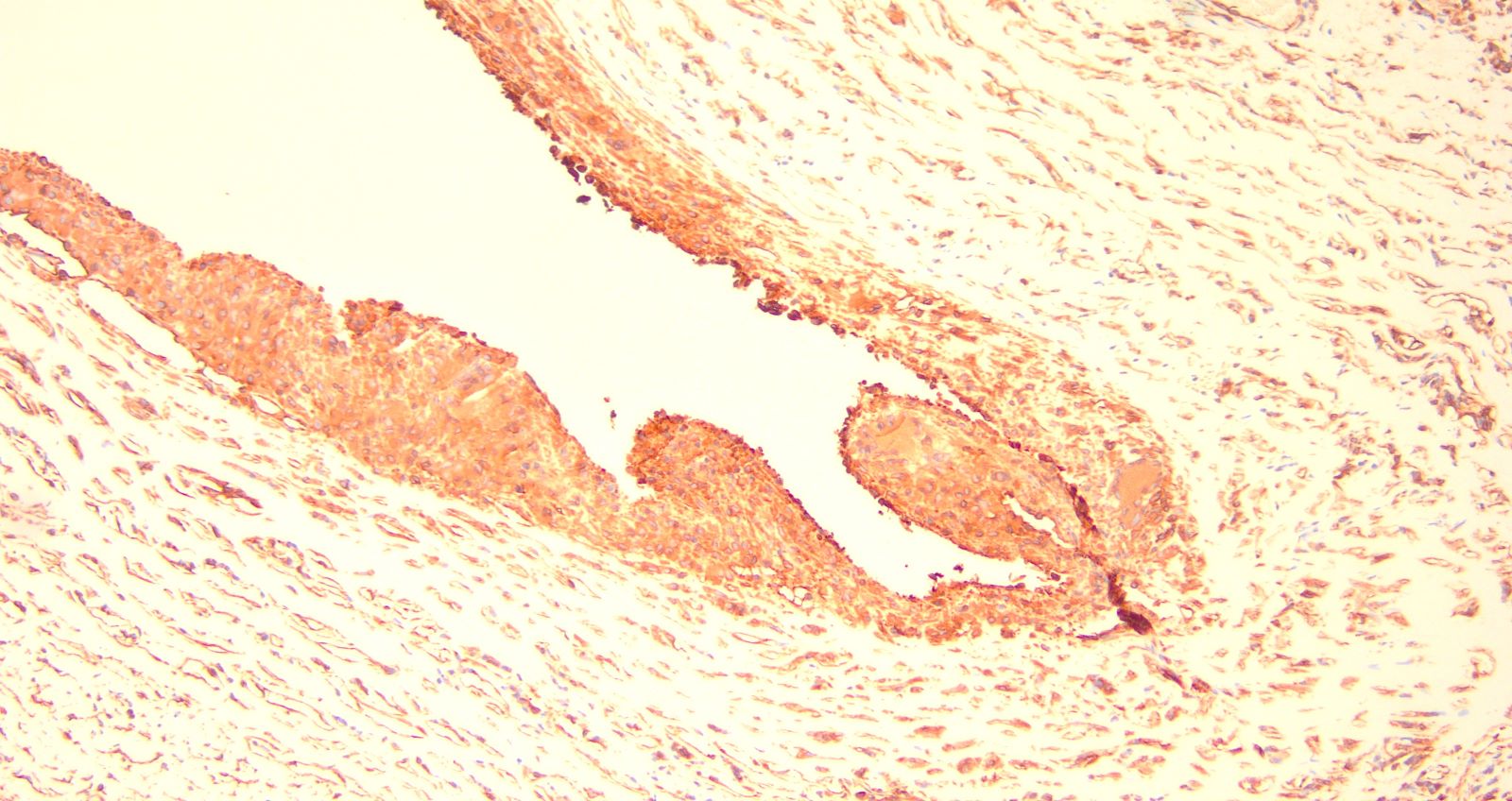
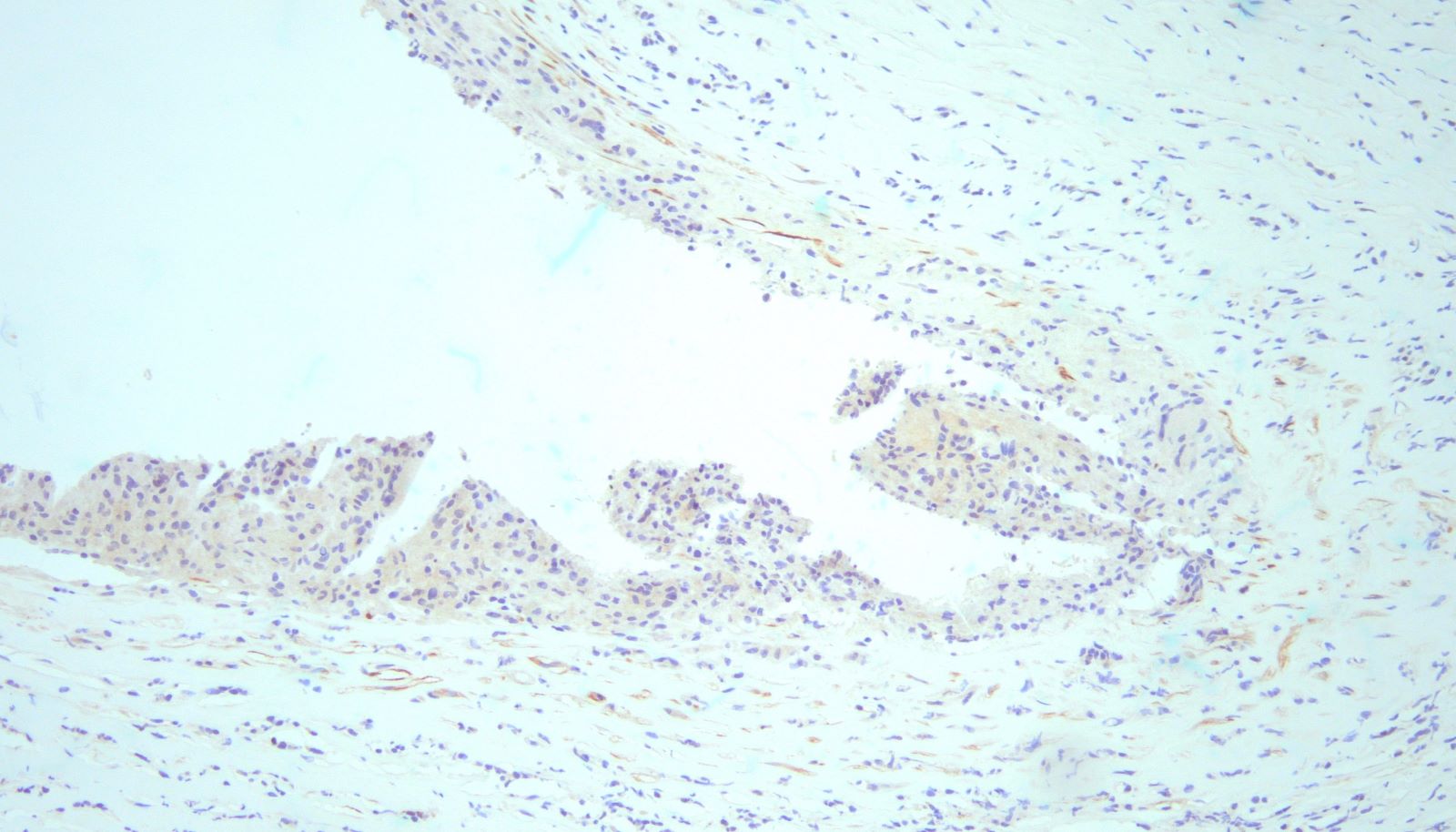
Microscopic (histologic) images
Contributed by Di Ai, M.D., Ph.D., Julie M. Jorns, M.D., Kristen E. Muller, D.O. and Samantha A. Stephen, D.O. (Case #530)
Positive stains
- Vimentin
- CD68
- Reference: Ultrastruct Pathol 1995;19:83
Negative stains
Sample pathology report
- Right breast tissue, capsulectomy:
- Dense fibroconnective tissue with chronic inflammation, fat necrosis, foreign body giant cells and amorphous foreign materials (see comment)
- Comment: Foreign materials are amorphous, transparent and nonpolarized, consistent with silicone leakage.
- Right breast capsule, excision:
- Benign fibrous capsule with chronic (lymphohistiocytic) inflammation and giant cell reaction to silicone
Differential diagnosis
- Breast implant associated fibromatosis (J Surg Case Rep 2018;2018:rjy249):
- Can be locally aggressive, with high rates of recurrence despite adequate excision, while lacking metastatic potential
- Develop from fibroblasts or myofibroblasts, in association with the capsule surrounding a silicone breast implant
- Long fascicles of spindle cells with no / minimal cytologic atypia and no mitotic figures
- Focal prominent stromal collagen
- Nuclear staining for beta catenin, while negative for CD34 and p63
- Squamous cell carcinoma (Ann Plast Surg 1992;29:425):
- Poorly differentiated squamous cell carcinoma is rarely seen
- The histologic features of lining of squamous epithelium around a breast implant include: pleomorphic and hyperchromatic nuclei, single cell dyskeratosis, atypical mitotic figures and infiltration into the stroma around the capsule
- Immunostaining positive for cytokeratin
- Squamous metaplasia is bland and lacks the histologic features mentioned above
- Implant associated anaplastic large cell lymphoma (Clin Imaging 2020;59:144):
- Tumor lymphocytes have significant atypia (anaplastic) with horseshoe shaped nuclei, CD30 positive
- High grade sarcoma:
- High grade sarcoma, such as liposarcoma and angiosarcoma, has been reported to be associated with breast implant; also, breast implant associated fibrosarcoma was reported in 35% in a rat model (Plast Reconstr Surg Glob Open 2013;1:e11)
- Histologic features include high grade nuclear atypia, atypical mitotic figures and necrosis
Additional references
Board review style question #1
Board review style answer #1
C. CD68. The lining cells exhibit an immunohistochemical profile similar to synovial cells, including positive staining for CD68 and vimentin. Answers A, B, D and E are incorrect because staining for cytokeratins, CD3, EMA and factor VIII are negative.
Comment Here
Reference: Benign breast implant related changes
Comment Here
Reference: Benign breast implant related changes
Board review style question #2
Which of the following statements is true about acellular dermal matrix?
- Comprised of avascular and acellular collagen fibers after implantation
- Never clinically palpable
- Not commonly used in breast reconstructive surgery
- Shows hypercellular stroma with intermixed breast ducts and lobules
Board review style answer #2
A. Comprised of avascular and acellular collagen fibers after implantation. The histologic features of acellular matrix vary based on the stage of tissue remodeling. After implantation, the tissue is comprised of acellular and avascular disorganized collagen fibers. Eventually, the acellular matrix undergoes neovascularization with the production of small capillaries and proliferation of fibroblasts around the collagen fibers. Once acellular dermal matrix undergoes tissue remodeling and incorporation, the tissue may resemble mature dense fibrous tissue (see Case #530 for more information).
Comment Here
Reference: Benign breast implant related changes
Comment Here
Reference: Benign breast implant related changes