Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1Cite this page: Marotti J. Idiopathic granulomatous mastitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/breastgranulomatousmastitis.html. Accessed April 2nd, 2025.
Definition / general
- Lobulocentric granulomatous inflammation
- Diagnosis of exclusion (excluding other causes of granulomatous inflammation)
Essential features
- Rare, benign inflammatory process affecting women of childbearing age
- Clinical symptoms and radiologic findings concerning for breast cancer
- Reported association with pregnancy, lactation, oral contraceptive pill use, hyperprolactinemia, autoimmunity
- Lobulocentric granulomatous inflammation
- Diagnosis of exclusion
Terminology
- Idiopathic granulomatous mastitis
- Lobular granulomatous mastitis
Epidemiology
- Rare
- Most common in parous women, childbearing age
- Frequent in postpartum and breastfeeding women
- Median age in the 30s
Sites
- Breast, most often unilateral, rarely bilateral
Pathophysiology
- Unknown
Etiology
- Unknown
- Proposed causes or associations: pregnancy, lactation, oral contraceptive pill use, hyperprolactinemia, autoimmunity, infection
Clinical features
- Mimics breast cancer, including inflammatory breast cancer (Breast J 2019;25:1245)
- Palpable breast mass
- Breast pain
- Abscess formation with fistula tract formation
- Nipple retraction
- Peau d'orange
- Rare lymphadenopathy
Diagnosis
- Breast core biopsy or surgical excision with histologic examination
Laboratory
- Microbiology studies to exclude infection
- Serologic markers to exclude autoimmune processes
- Endocrine studies
Radiology description
- Nonspecific imaging findings (Radiographics 2018;38:330)
- Mammography: focal asymmetric density (Clin Imaging 2021;69:126)
- Ultrasound: irregular hypoechoic mass with tubular projections (Clin Imaging 2021;69:126)
- MRI: nonmass-like enhancement; ring enhancing lesions (Acta Radiol 2016;57:796, Clin Imaging 2021;69:126)
Radiology images
Prognostic factors
- Self limiting in approximately 50% of patients (Am J Surg 2015;210:258)
- Can persist or recur, prompting treatment
Case reports
- 33 year old woman with chronic breast wound (Breast J 2020;26:281)
- 36 year old woman with tender breast mass (Int Semin Surg Oncol 2007;4:21)
- 37 year old woman with painless breast mass (J Clin Diagn Res 2017;11:PD14)
- 43 year old woman with tender breast mass and erythema nodosum (JAAD Case Rep 2016;2:125)
Treatment
- No standard treatment guidelines
- Observation (Am J Surg 2015;210:258)
- Corticosteroids after infection excluded
- Antibiotics might not be effective
- Immunosuppressants (methotrexate, azathioprine) in persistent or recurrent disease (Surgeon 2021 Apr 6 [Epub ahead of print])
- Surgery
Clinical images
Gross description
- Gray-tan firm mass
- Size variable; average 5 - 6 cm
- Ill defined margins
- Subtle nodularity
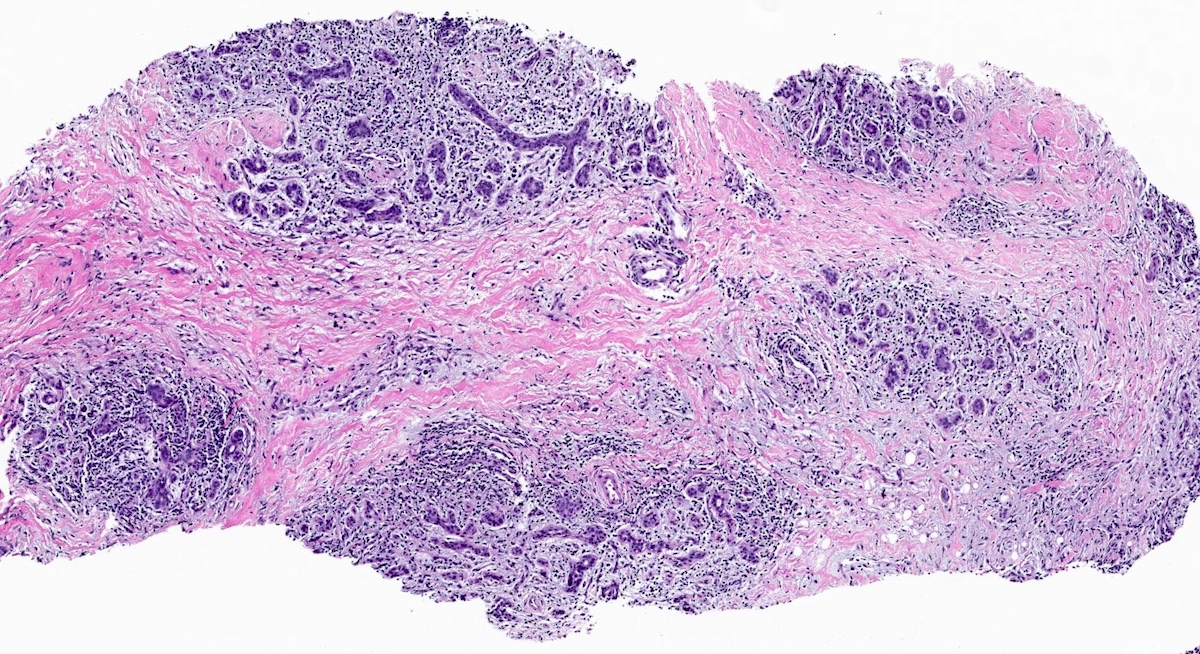
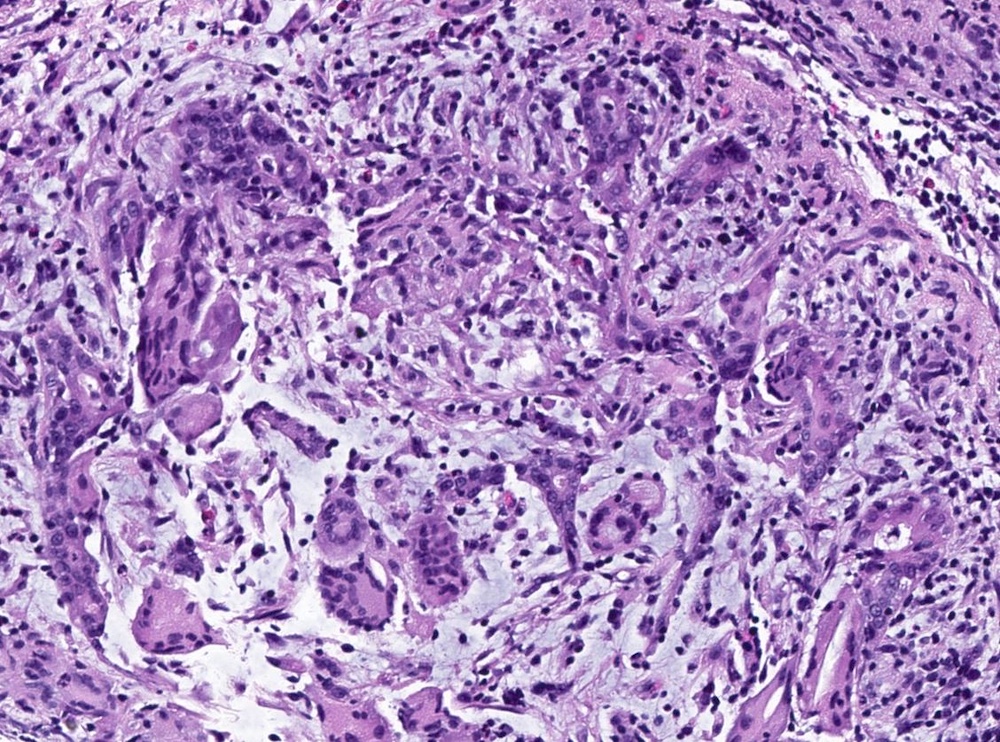
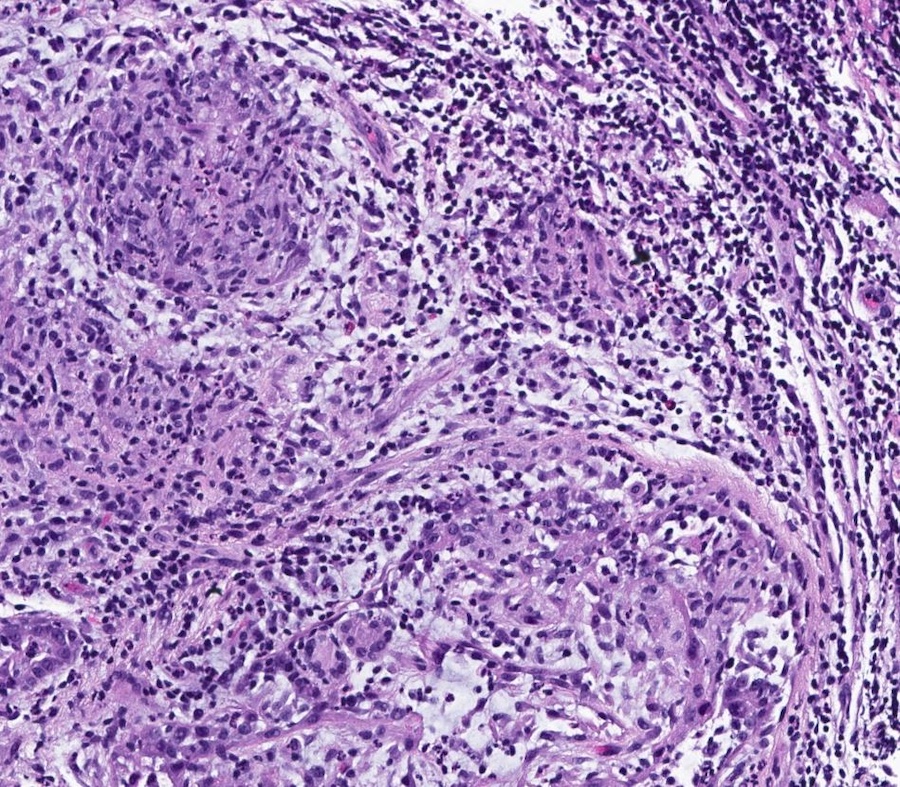
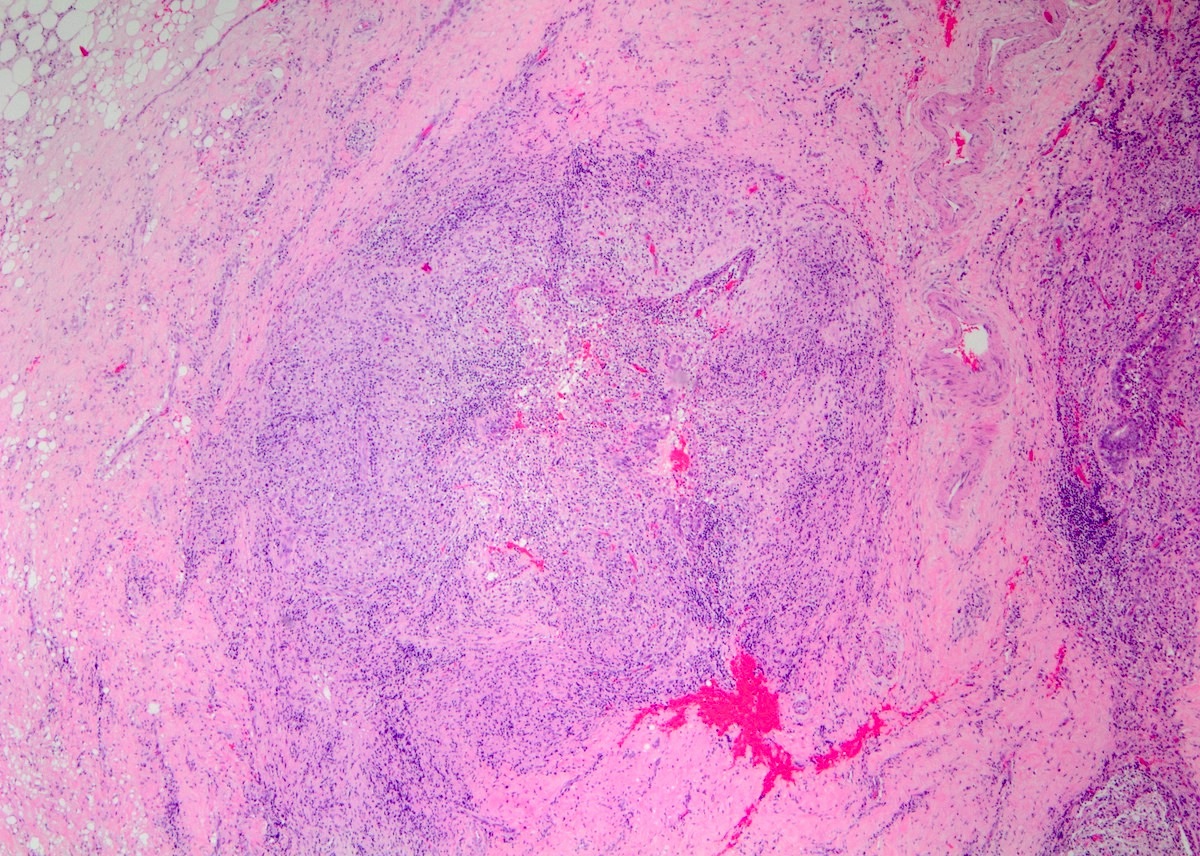
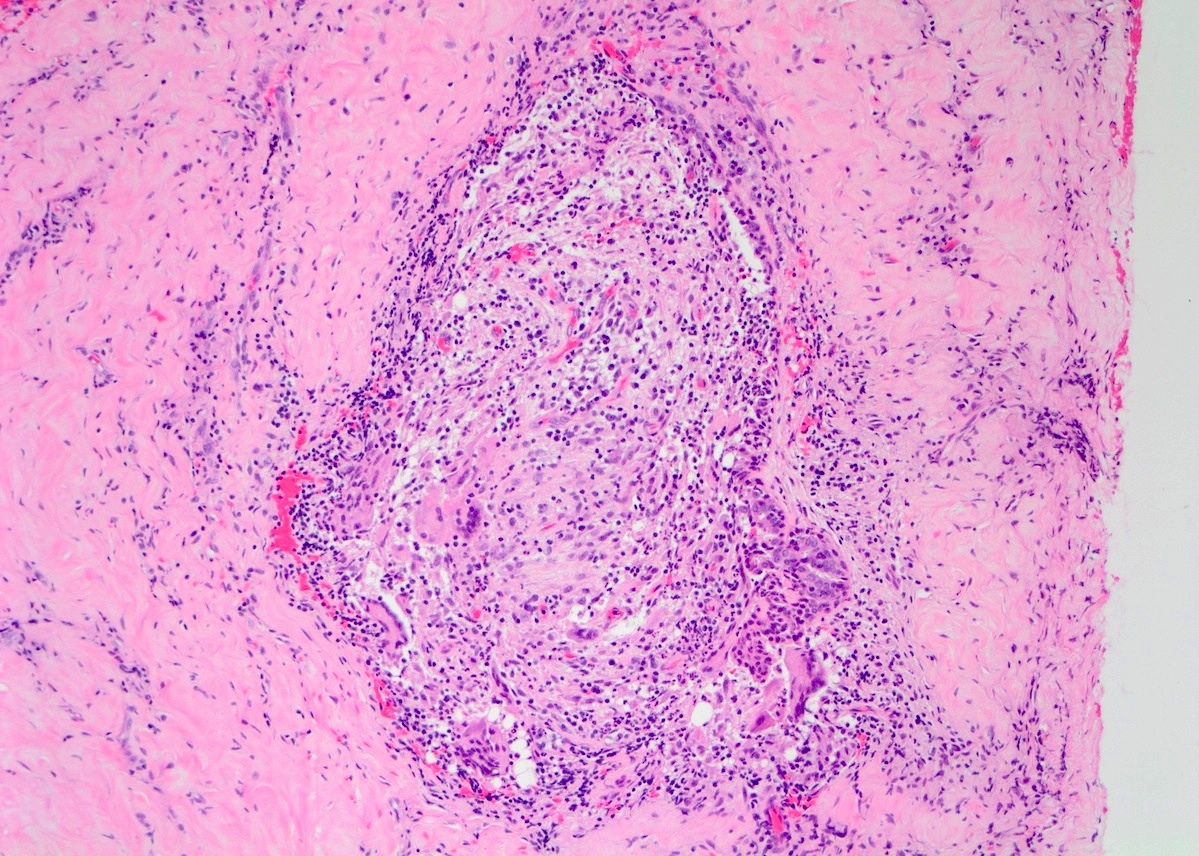
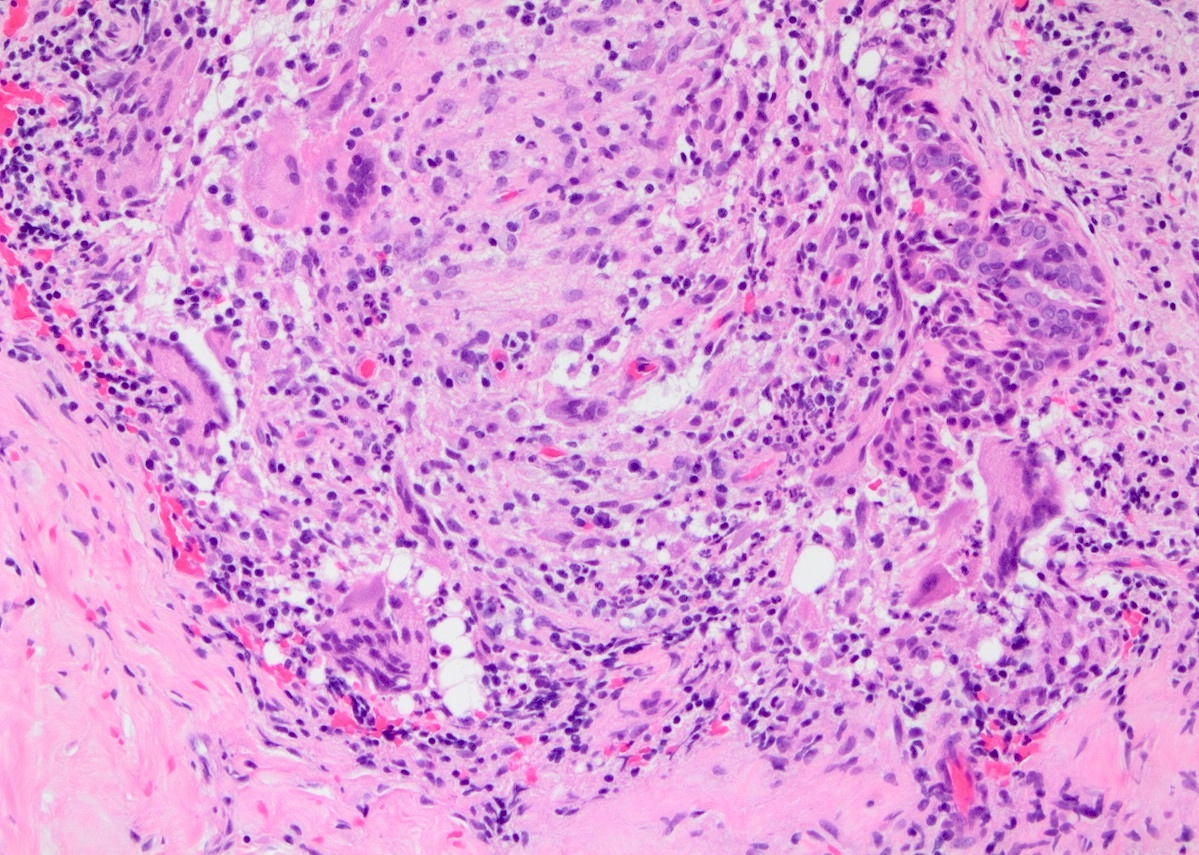
Microscopic (histologic) description
- Lobulocentric granulomatous inflammation (Pathology 2004;36:254)
- Granulomas often contain neutrophils
- Neutrophils can create microabscesses; overlapping features with cystic neutrophilic granulomatous mastitis
- Multinucleated giant cells, lymphocytes, plasma cells and eosinophils within and around lobules
- Extensive inflammation might obliterate lobulocentric distribution
- Caseous necrosis not present
- Schauman and asteroid bodies not common
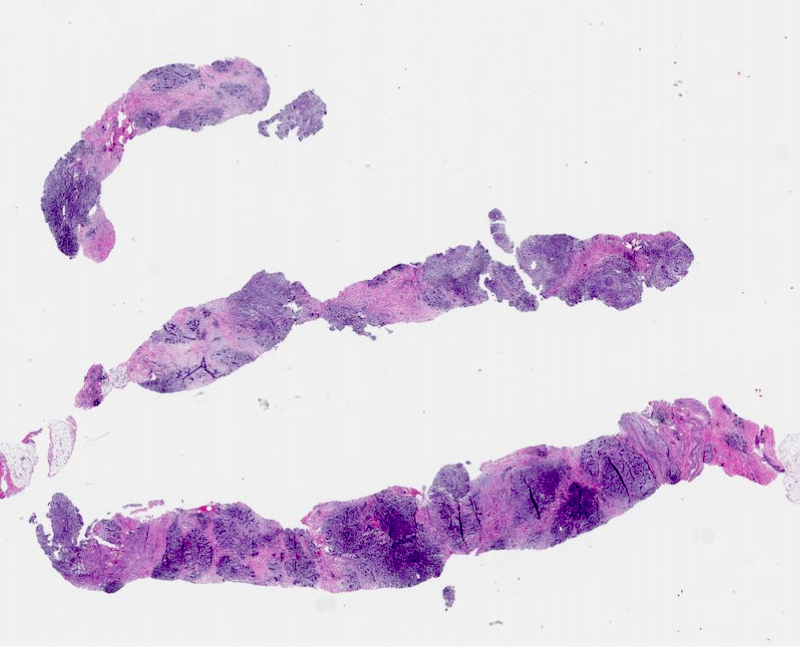
Microscopic (histologic) images
Cytology description
- Nonspecific cytologic findings (J Clin Pathol 2003;56:519, Acta Cytol 2009;53:667)
- Epithelioid histiocytes, multinucleated giant cells, granulomas
- Necrosis usually absent
Positive stains
- CD68: positive in histiocytes
Negative stains
- Gram stain for gram positive bacilli (Corynebacterium)
- Acid fast stain for mycobacteria
- GMS or PAS stains for fungi
- IgG4 in plasma cells for IgG4 related sclerosing mastitis
Sample pathology report
- Left breast, needle core biopsy:
- Breast tissue with lobulocentric granulomatous inflammation (see comment)
- Comment: Sections show a lobulocentric mastitis with histiocytes, granulomas, neutrophils and lymphocytes. The histologic findings are nonspecific but the main differential diagnosis includes idiopathic granulomatous mastitis, cystic neutrophilic granulomatous mastitis (typically caused by Corynebacterium), other infection, sarcoidosis and reaction to foreign material, among others. Given the lobulocentric nature of the granulomatous inflammation and lack of currently identifiable microorganisms, idiopathic granulomatous mastitis is favored. However, clinical and microbiologic correlation is required. Special stains for bacteria, acid fast bacilli and fungi are negative. Foreign material is not identified. There is no evidence of malignancy in this sample.
Differential diagnosis
- Cystic neutrophilic granulomatous mastitis (CNGM) (J Clin Pathol 2020;73:445):
- Small cystic spaces lined by neutrophils with cuff of epithelioid histiocytes
- Cysts contain rare gram positive bacilli (Corynebacterium)
- Granulomatous mastitis due to infection:
- Tuberculosis mastitis:
- Necrotizing granulomas
- Inflammation affects ducts and lobules
- Acid fast stain, culture or polymerase chain reaction to identify Mycobacterium
- Fungal mastitis:
- Tuberculosis mastitis:
- Foreign body reaction:
- Foreign body type granulomas and giant cells
- Presence of foreign material
- Granulomatosis with polyangiitis:
- Necrotizing vasculitis
- c-ANCA positive
- Sarcoidosis:
- Well formed granulomas not confined to the lobules
- Squamous metaplasia of lactiferous ducts (SMOLD):
- Associated with smoking
- Keratinizing squamous metaplasia of nipple ducts with foreign body inflammatory response
- IgG4 related sclerosing mastitis (J Clin Pathol 2020 Dec 16 [Epub ahead of print]):
- Storiform fibrotic process with eosinophils and increased IgG4 positive plasma cells
- Obliterative phlebitis
- Granulomas typically absent
Additional references
Board review style question #1
A 33 year old woman presents with a painful breast lump concerning for breast cancer. A core biopsy is performed. Which histologic finding is most characteristic of idiopathic granulomatous mastitis?
- Keratin debris with associated foreign body inflammatory response
- Large necrotizing granulomas
- Lobulocentric granulomatous inflammation
- Microcysts with gram positive bacilli
- Well formed granulomas within interlobular stroma
Board review style answer #1
C. Lobulocentric granulomatous inflammation. Although not specific, the most characteristic histologic finding of idiopathic granulomatous mastitis is granulomatous inflammation centered on lobules (lobulocentric inflammation). Idiopathic granulomatous mastitis can have overlapping histologic features with cystic neutrophilic granulomatous mastitis (CNGM); however, microcysts with gram positive bacilli (Corynebacterium) are identified in CNGM. Keratin debris with an associated foreign body inflammatory response is usually seen in squamous metaplasia of lactiferous ducts (SMOLD). Large necrotizing granulomas are more typical of an infectious processes, such as mycobacterial infection. The presence of well formed granulomas within the interlobular stroma suggests sarcoidosis.
Comment here
Reference: Idiopathic granulomatous mastitis
Comment here
Reference: Idiopathic granulomatous mastitis