Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Agarwal AN, Mais DD. Nonproliferative fibrocystic changes. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/breastfcc.html. Accessed April 2nd, 2025.
Definition / general
- Nonspecific, general term to describe a range of common and benign breast conditions, which may occur together or in isolation
- Cause clinical, radiographic (e.g. calcifications, mass or architectural distortion) or histologic changes of the breast tissue that may result in concern for malignancy
- Nonproliferative and nonatypical fibrocystic changes are not associated with increased risk of subsequent breast carcinoma
- Some proliferative fibrocystic changes are associated with a slightly increased risk of subsequent breast carcinoma
Essential features
- Histologically benign structural alterations in epithelial and stromal elements
Terminology
- Fibrocystic disease
- Use in surgical pathology reports is discouraged (N Engl J Med 1982;307:1010, N Engl J Med 1985;312:179)
- Diffuse cystic mastopathy
ICD coding
- ICD-10: N60.19 - diffuse cystic mastopathy of unspecified breast
Epidemiology
- Common, affecting 50% of women (Dtsch Arztebl Int 2019;116:565)
- Occurs during reproductive years, usually presenting between the ages of 25 - 45 years
- Reduced incidence in postmenopausal women (Am J Obstet Gynecol 1986;154:161)
Sites
- Breast
- Can occur in axilla from the accessory breast tissue
Pathophysiology
- Excess estrogen leads to proliferation of epithelium in terminal duct lobular units and induces stromal fibrosis
- Fibrosis and epithelial proliferation may lead to obstruction of ducts and acini, leading to involution or cyst formation
- Some cysts may rupture, inducing adjacent fibroinflammatory stromal reactions
- Reference: J Adv Sci Res 2020;11:30
Etiology
- Associated with hormonal imbalance (increased estrogen to progesterone ratio) (Am J Obstet Gynecol 1986;154:161)
Clinical features
- Breast pain, tenderness, lumpiness, cysts or mass
- Manifestations may be cyclic, reflecting menstrual cycle
- Associated with polycystic ovary syndrome (Arch Gynecol Obstet 2009;280:249)
- Usually bilateral, although one breast may be affected more than the other
- Symptoms tend to abate after menopause
- Nonproliferative lesions are the most common finding in breast cancer screening biopsies, accounting for about 70% of all cases (N Engl J Med 2005;353:275)
Diagnosis
- Needle biopsy, needle aspiration or excisional biopsy
Radiology description
- Ultrasound: may be a solid mass, cyst, heterogeneous echogenic tissue or no visible abnormality (Invest Radiol 2005;40:436)
- MRI: mass or a nonmass-like regional enhancing lesion with benign enhancement kinetics (Invest Radiol 2005;40:436)
- Can also present as densities with associated calcifications, areolar skin thickening alone or normal dense fibroglandular tissue with no abnormality on mammogram (Invest Radiol 2005;40:436)
Prognostic factors
- Risk of breast cancer (Am J Surg Pathol 2003;27:836)
- Nonproliferative lesions: no increased risk
- Proliferative lesions without atypia: 1.5 - 2 fold risk
Case reports
- 2 year old girl with an ill defined lump (Fetal Pediatr Pathol 2021;40:535)
- 35 year old woman with left breast lump that was diagnosed as cystic fibroadenoma (Breast Dis 2015;35:49)
- 38 year old woman with left breast enlargement (Am J Case Rep 2018;19:1550)
- 43 year old woman with right breast lump that was diagnosed as cystic fibroadenoma (Turk Patoloji Derg 2011;27:254)
Treatment
- Close clinical follow up of patients with high risk for breast cancer, including physical examination (every 4 - 6 months) and mammography (every 1 - 2 years) in most patients (Am J Obstet Gynecol 1986;154:161, N Engl J Med 2005;353:275)
- Nonsteroidal anti-inflammatory drugs, aspirin or hormonal manipulation with low estrogen oral contraceptive, cyclic progestogen or danazol therapy is used less commonly in women with cyclical breast pain (Am J Obstet Gynecol 1986;154:161, N Engl J Med 2005;353:275)
Gross description
- Breast tissue is heterogeneously fibrous and indurated
- Cysts ranging from 1 - 20 mm, clear or blue domed, may be seen
Gross images
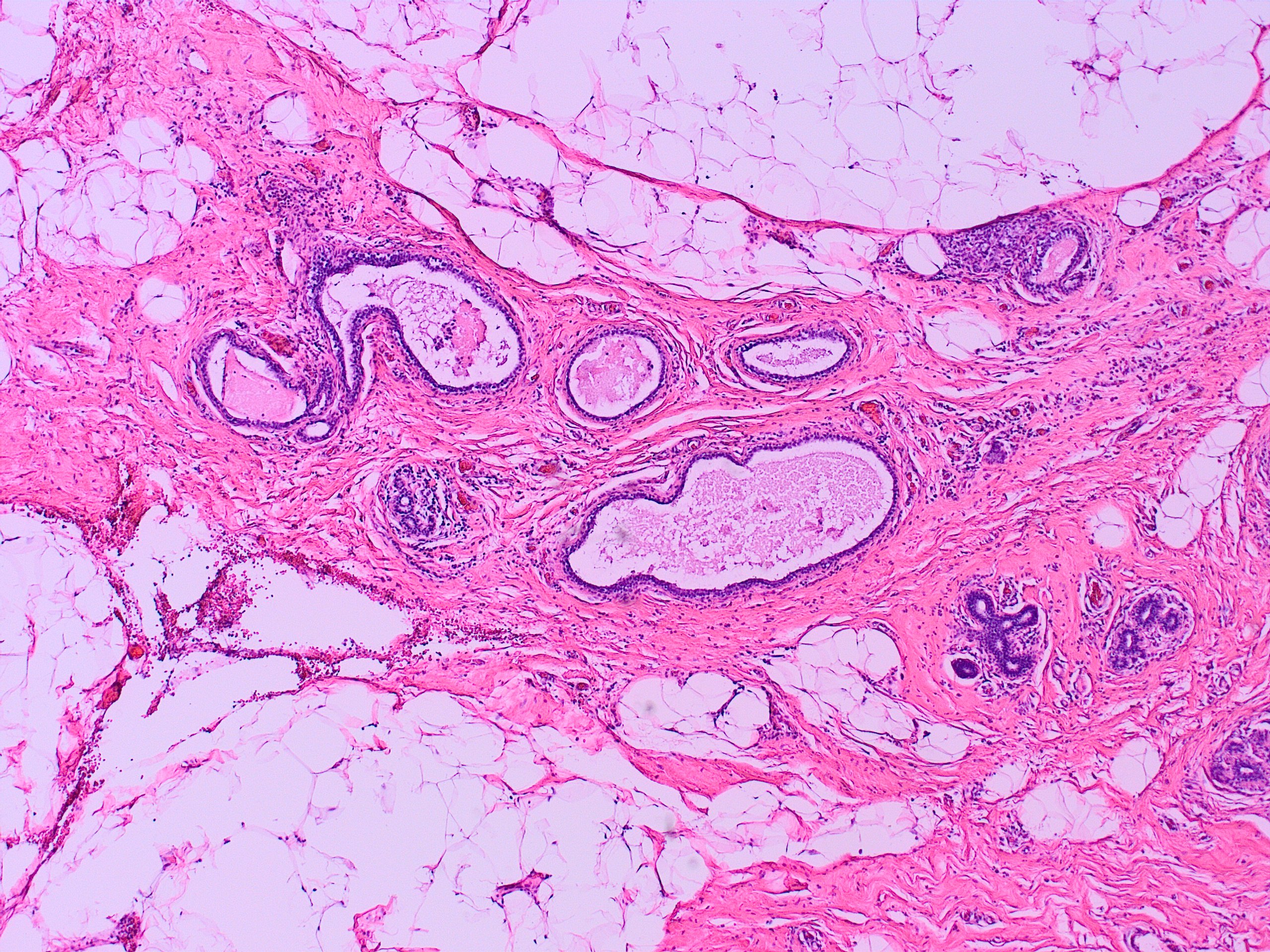
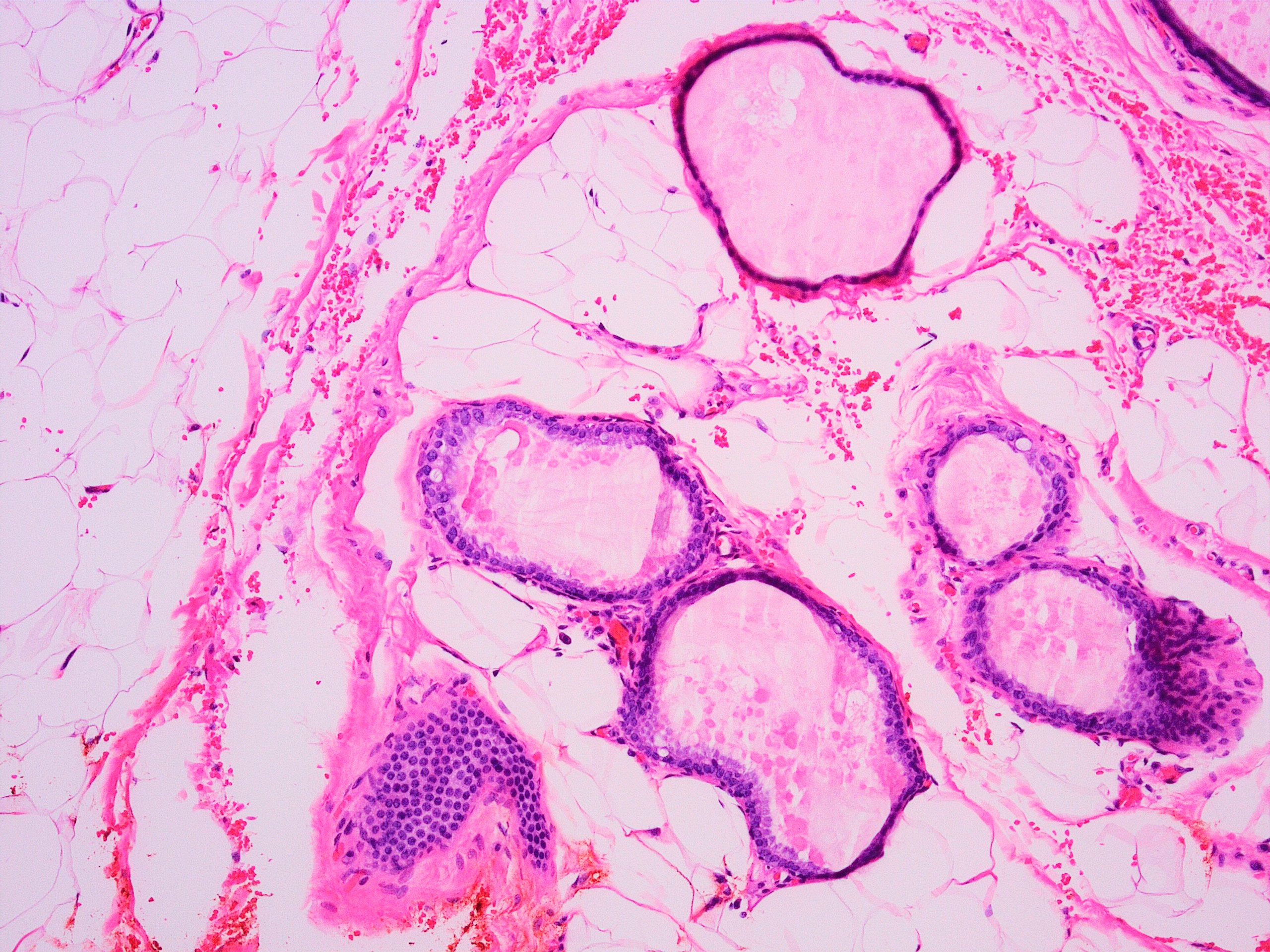
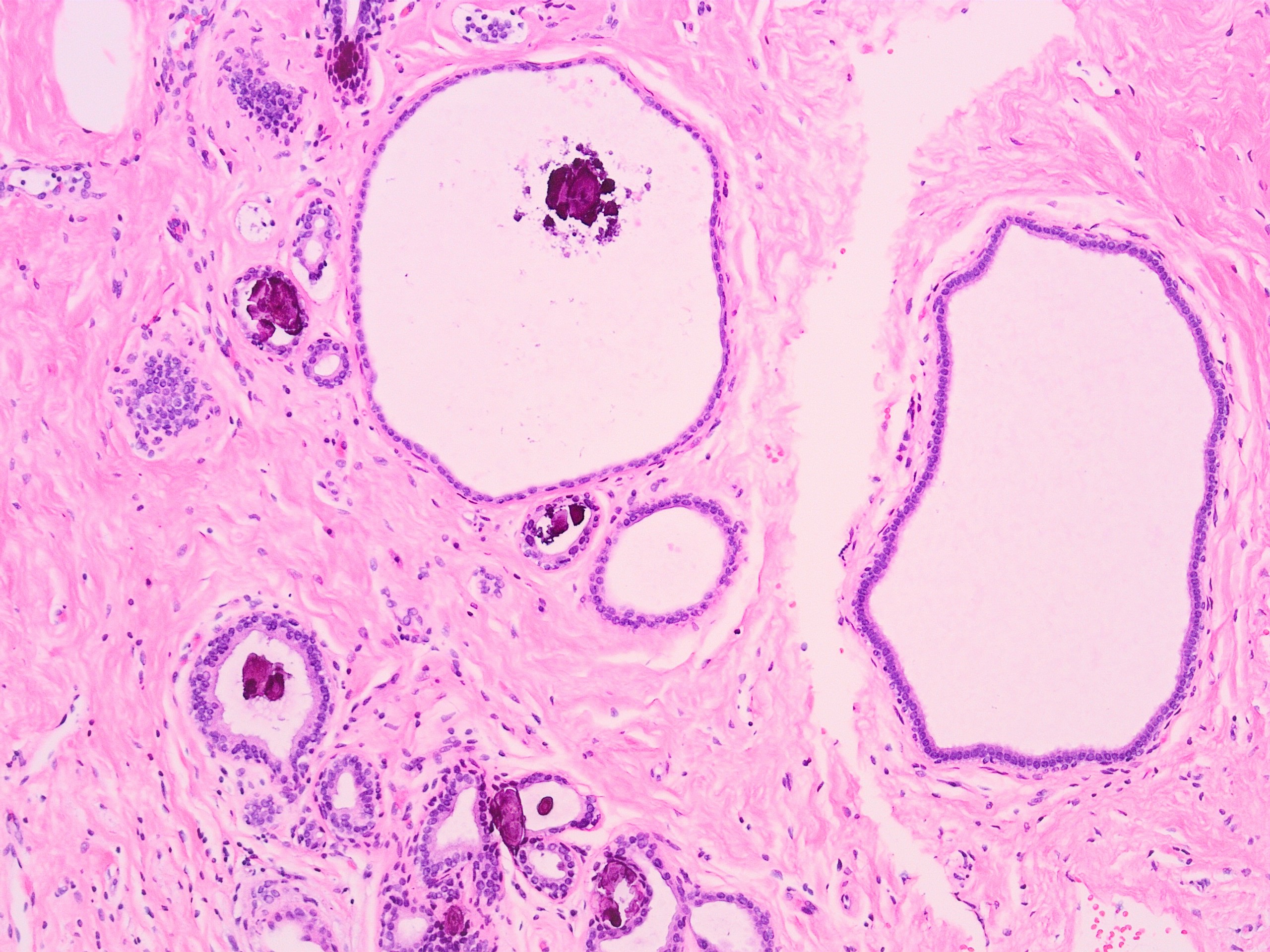
Microscopic (histologic) description
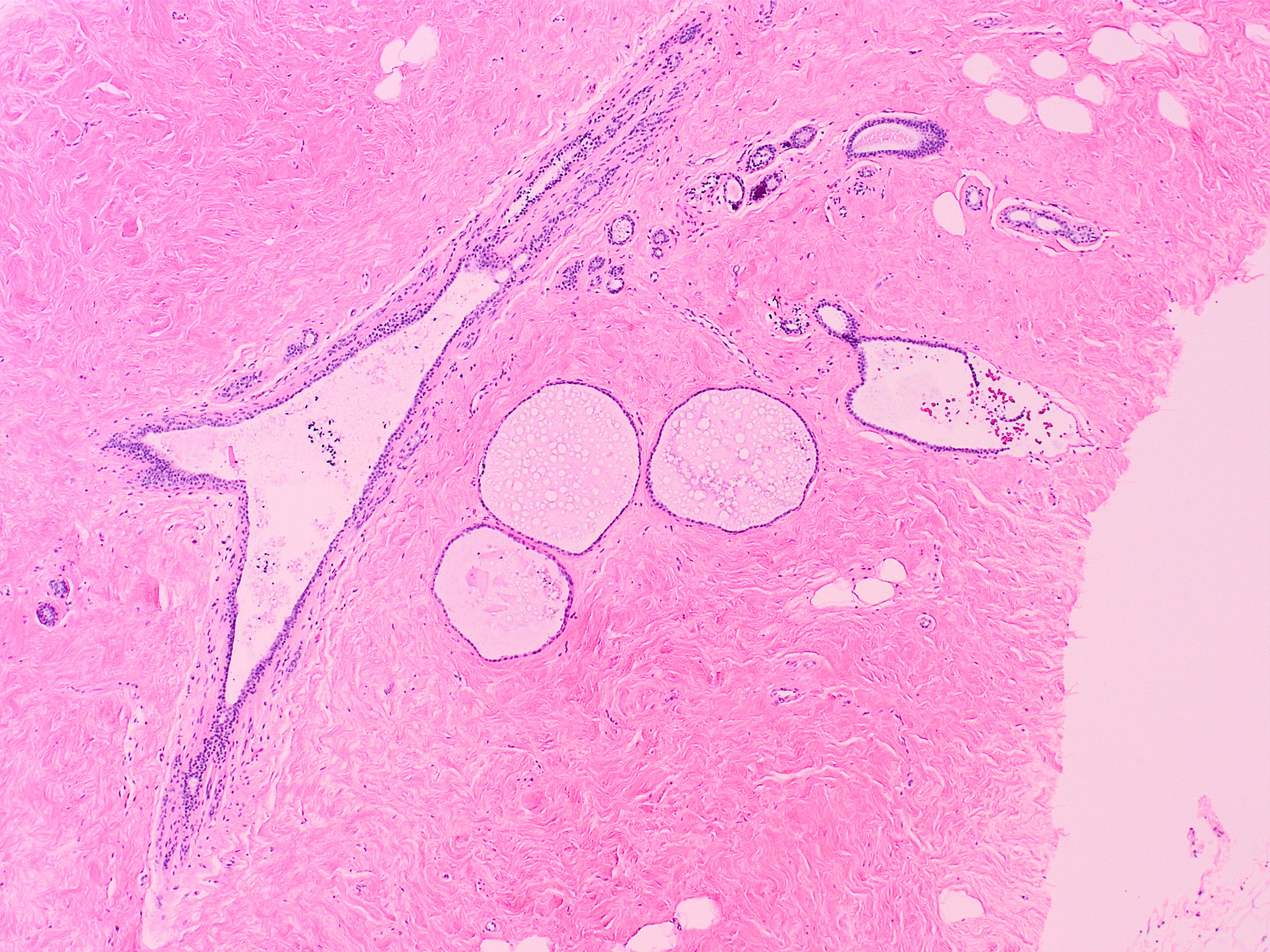
- Nonproliferative fibrocystic changes; characterized by 3 features: adenosis, fibrosis and cyst formation
- Adenosis:
- Increased number of acini per lobule
- Acini are lined by columnar cells, which may be benign or have atypia
- Adenosis is frequently seen in pregnancy and may be focal in nonpregnant women
- Fibrosis:
- Stromal fibrosis
- Cyst rupture may result in chronic inflammation, prominent histiocytic reaction and fibrosis
- Causes increased density observed on imaging and nodularity observed on palpation
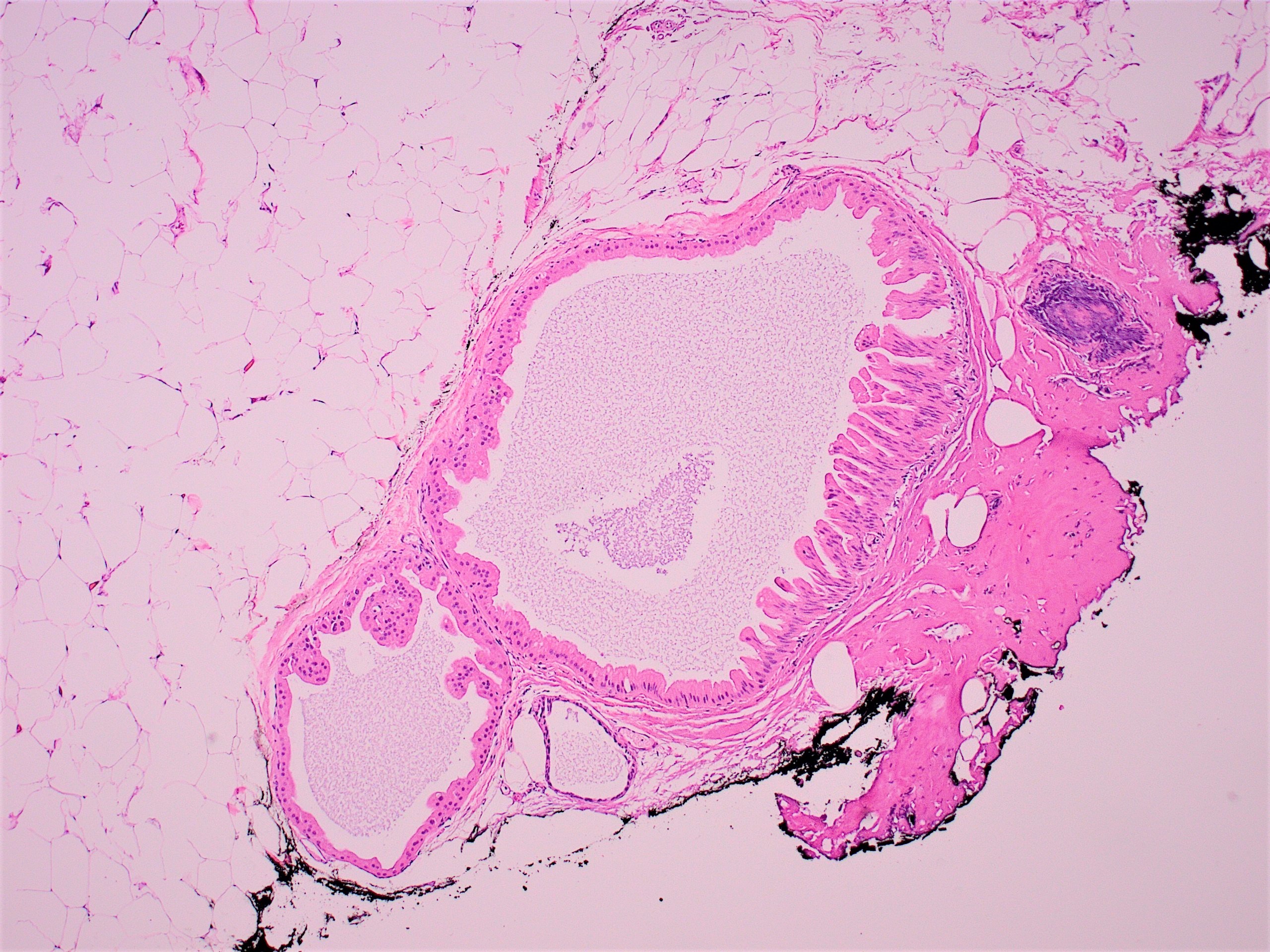
- Cyst formation:
- Cystically dilated ducts or lobules
- May contain eosinophilic secretions, foamy macrophages and calcifications
- Lined by cuboidal epithelium or may have apocrine metaplasia
- Outer myoepithelial layer present but may be attenuated
- Apocrine metaplasia: single or multilayered ductal epithelium with abundant granular eosinophilic cytoplasm, apical snouts, enlarged nuclei and prominent nucleoli
- Columnar cell changes / columnar cell hyperplasia: enlargement of terminal duct lobule with variably dilated lumens and irregular contours, lined by cuboidal to columnar cells, lacking cytologic atypia, frequently with apical snouts
- Adenosis:
Microscopic (histologic) images
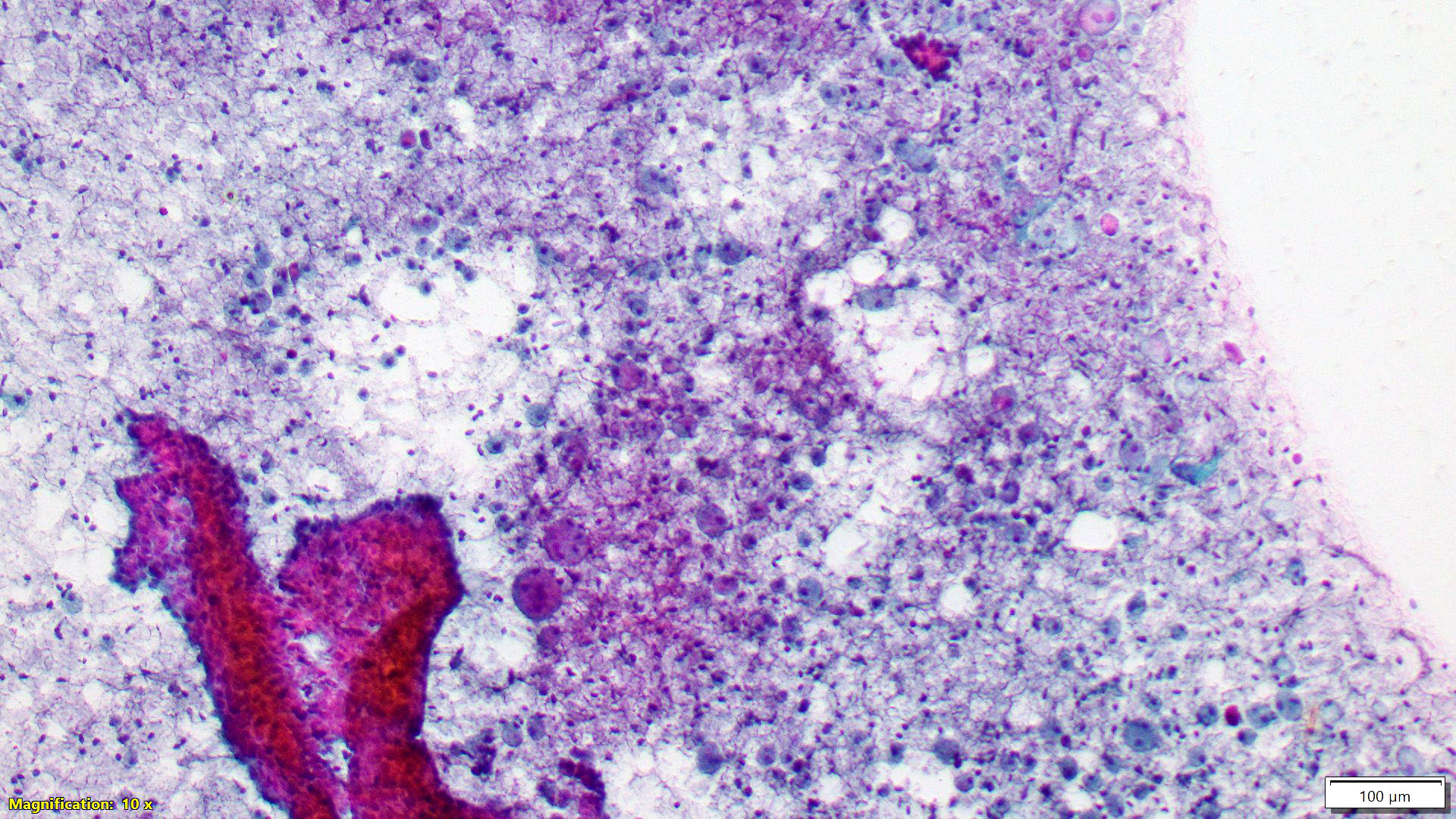
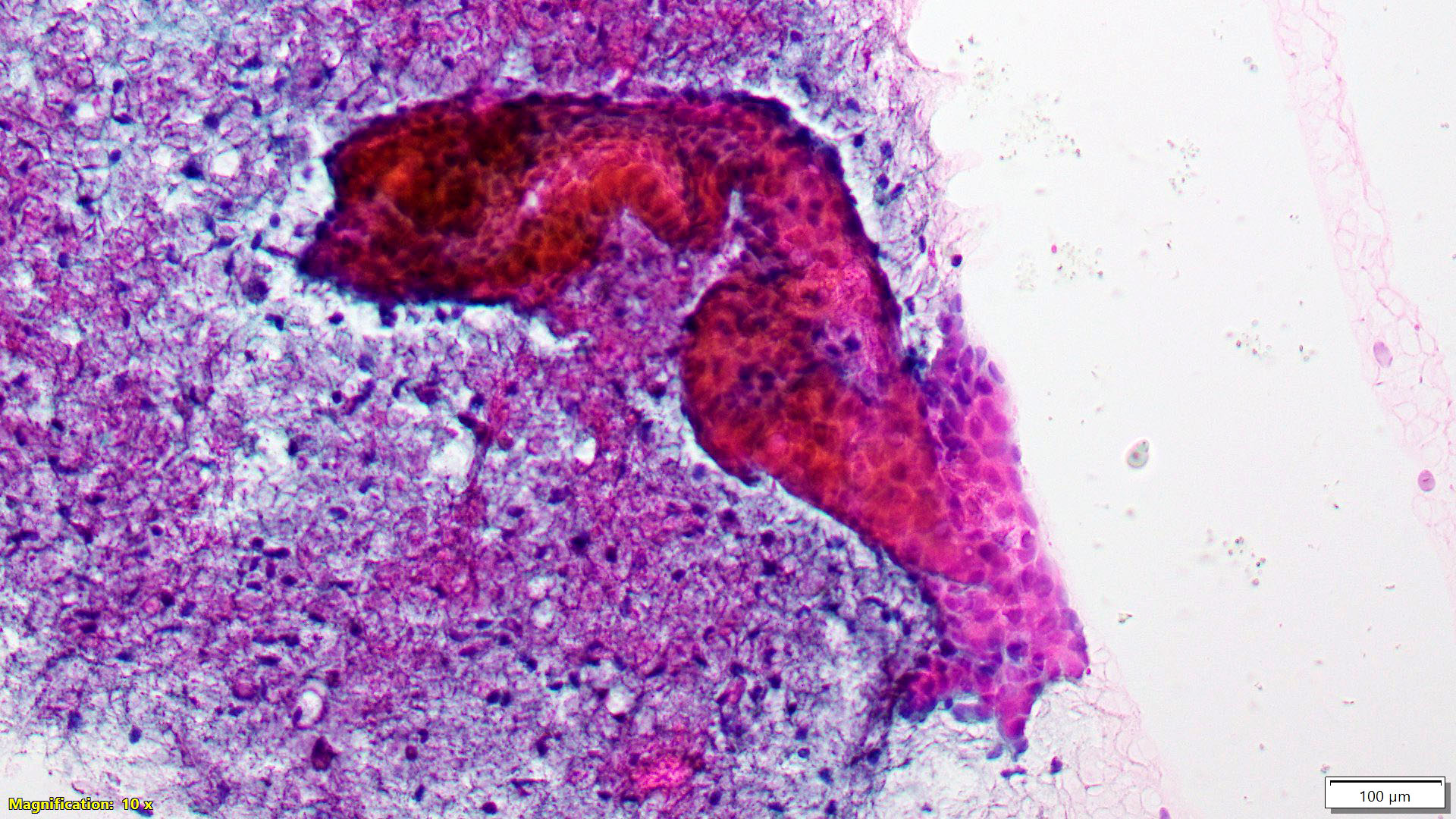
Cytology description
- Nonproliferative breast lesions
- Apocrine cells, foam cells and small, uniform, evenly spaced ductal epithelial cells
- Proliferative breast lesions
- Sheets and tight clusters of cells without significant nuclear overlap
- Reference: Clin Lab Med 2005;25:713
Sample pathology report
- Breast, 12:00, microcalcifications, stereotactic core needle biopsy:
- Benign breast parenchyma with fibrocystic changes, including florid usual type ductal hyperplasia and apocrine metaplasia
- Microcalcifications associated with apocrine metaplasia
Differential diagnosis
- Proliferative lesions without atypia:
- Mild usual ductal hyperplasia:
- Proliferation of ductal epithelium no more than 3 or 4 cell layers in thickness
- Moderate to severe (florid):
- Proliferation of ductal epithelium more than 4 cell layers in thickness that may fill and extend the luminal space
- Arrangement of nuclei is haphazard, with cellular heterogeneity, oval nuclei with grooves and small indistinct nucleoli
- Sclerosing adenosis:
- Lobulocentric proliferation of acini within dense hyaline sclerotic stroma
- Intraluminal calcifications may be present
- Mild usual ductal hyperplasia:
- Cystic fibroadenoma:
- Fibroadenoma with extensive cystic changes and cysts that are more than 3 mm (Breast Dis 2015;35:49, Turk Patoloji Derg 2011;27:254)
- Pseudoangiomatous stromal hyperplasia:
- Stroma with prominent slit-like spaces lined by bland spindle cells; the slit-like spaces are empty and have an anastomosing appearance
Additional references
Board review style question #1
Which of the following is true about proliferative fibrocystic changes in the breast?
- Apocrine metaplasia is considered a proliferative fibrocystic change
- Duct ectasia is considered a proliferative fibrocystic change
- Proliferative fibrocystic change has no associated increased lifetime risk of breast cancer
- Proliferative fibrocystic change without atypia has an associated 1.5 - 2 fold increased lifetime risk of breast cancer
Board review style answer #1
D. Proliferative fibrocystic change without atypia has an associated 1.5 - 2 fold increased lifetime risk of breast cancer
Comment Here
Reference: Fibrocystic changes
Comment Here
Reference: Fibrocystic changes
Board review style question #2
Board review style answer #2
B. Columnar cell change. The biopsy shows classic findings of fibrosis, cystic changes and microcalcifications along with the lining epithelium in a couple of cysts lined by columnar epithelium.
Comment Here
Reference: Fibrocystic changes
Comment Here
Reference: Fibrocystic changes