Table of Contents
Definition / general | Essential features | Terminology | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3Cite this page: Wu JM, Turashvili G. Cystic neutrophilic granulomatous mastitis . PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/breastcysticgranulomatousmastitis.html. Accessed December 22nd, 2024.
Definition / general
- Inflammatory process of the breast usually due to Corynebacterium species
Essential features
- Most patients are women, parous or currently pregnant
- Characteristic morphologic features include granulomas comprised of epithelioid histiocytes and giant cells with central lipid vacuoles containing gram positive bacteria and rimmed by neutrophils
- Association with Corynebacterium species, especially Corynebacterium kroppenstedtii, although microbiologic evidence can be difficult to obtain
- Prolonged antibiotic therapy required for complete resolution
Terminology
- Not recommended: granulomatous mastitis, idiopathic granulomatous mastitis, granulomatous lobular mastitis, idiopathic lobular granulomatous mastitis
Epidemiology
- Rare, with at least 141 cases reported since 2002 (J Clin Pathol 2020;73:445)
- Female patients, parous or currently pregnant
- Mean age 35 years (range 19 - 57)
Sites
- Usually unilateral (J Clin Pathol 2020;73:445)
- Approximately 8.5% present with bilateral disease
Etiology
- Strong association with Corynebacterium infection (Am J Clin Pathol 2016;145:635)
Clinical features
- Most commonly painful breast mass, nipple inversion or sinus formation (J Clin Pathol 2020;73:445)
- Nipple discharge, skin erythema and abscess
- Fever and leukocytosis
- Axillary lymphadenopathy
Diagnosis
- Microscopic examination and Gram stain with or without microbiologic culture
Laboratory
- Corynebacteria may be difficult to detect and culture
- Corynebacterium species require culture medium containing 1% polysorbate (Tween) 80 and longer incubation periods (Lett Appl Microbiol 2018;66:472)
- Alternative methods include matrix assisted laser desorption / ionization time of flight mass spectrometry (MALDI-TOF MS) or 16S rRNA and rpoB gene sequencing (J Thorac Dis 2017;9:3239, J Clin Microbiol 2005;43:1934, Int J Surg Pathol 2020;28:371)
Radiology description
- Seldom reported (Am J Surg Pathol 2015;39:1440, Breast J 2019;25:80, Clin Case Rep 2018;6:2208)
- Mammography: mass or asymmetry, most commonly BI-RADS 4 (suspicious of malignancy)
- Ultrasound: mass, dilated ducts, abscesses, edema or fluid collection
Prognostic factors
- Prolonged (weeks to months) antibiotic therapy required for complete resolution
- May recur with inadequate therapy
Case reports
- 30 year old woman with a fluctuant mass-like lesion (Case #462)
- 33 year old woman with recurrent breast abscess (Clin Infect Dis 2014;59:410)
- 37 year old woman with abscess and skin ulceration (Clin Microbiol Infect 2020 Jul 9 [Epub ahead of print])
- 52 year old woman with a tender left breast mass (Clin Case Rep 2018;6:2208)
Treatment
- Observation
- Antibiotics:
- Empirical antimicrobial therapy may be started prior to histologic diagnosis
- Lipophilic antibiotics such as doxycycline, trimethoprim sulfamethoxazole, clarithromycin and rifampicin may be more effective (J Clin Microbiol 2015;53:2895)
- Antibiotic susceptibility test should be performed
- Steroids
- Surgery including incision and drainage, excision and even mastectomy
- Combination of the above therapies
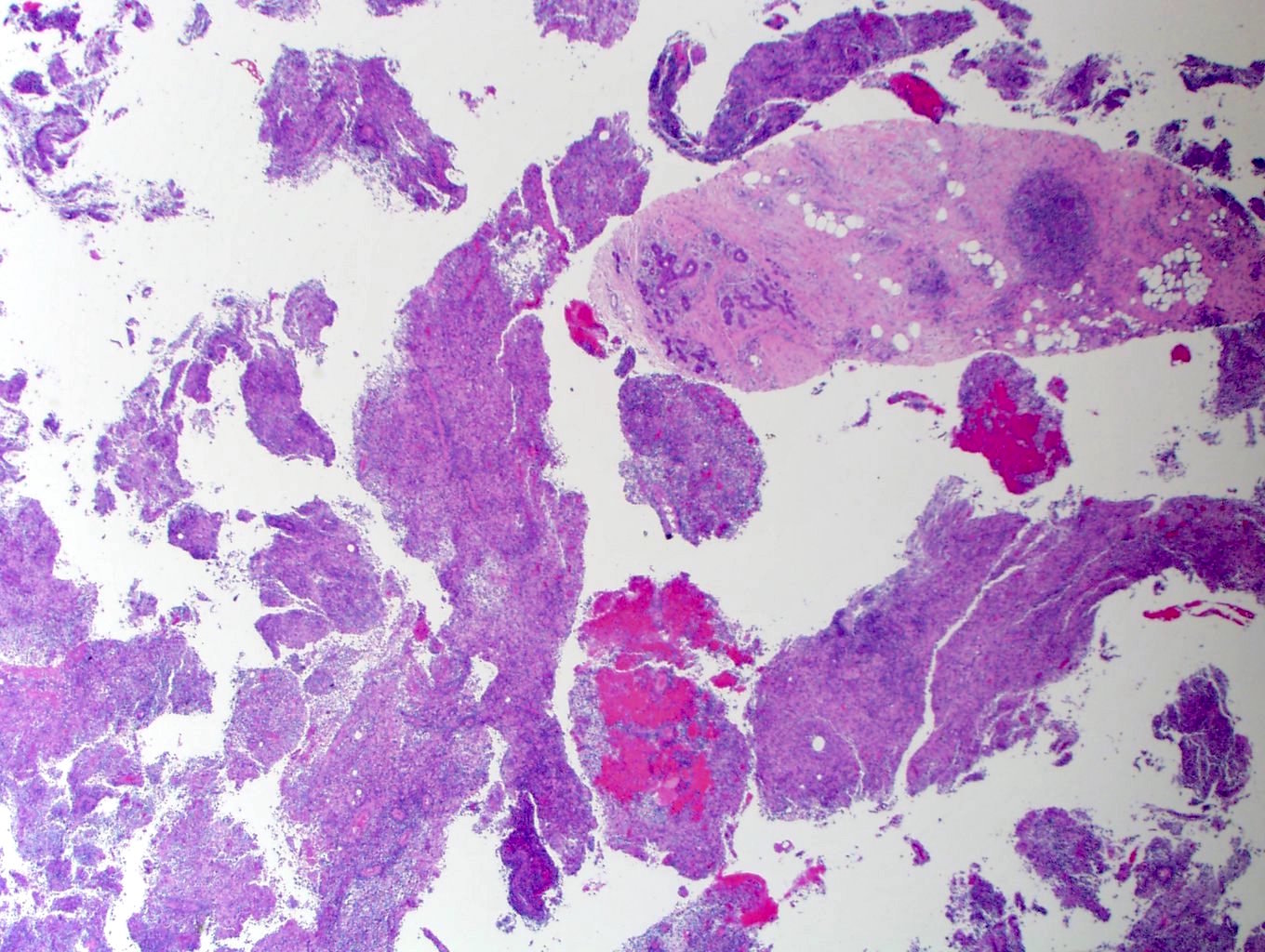
Gross description
- Definitive gross lesions may not be identified
- Solid lesions or masses with abscess cavities (Int J Surg Pathol 2020;28:371)
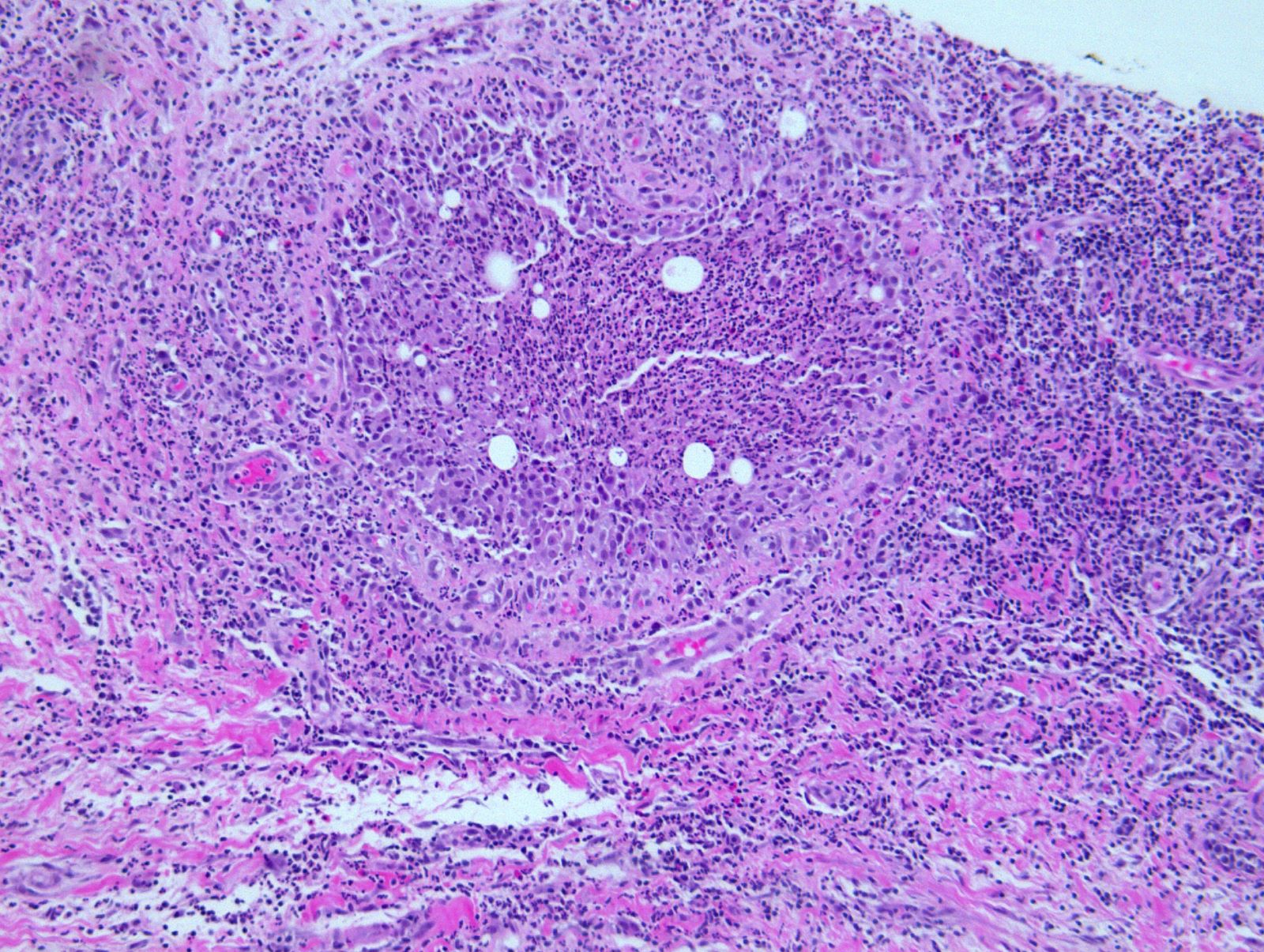
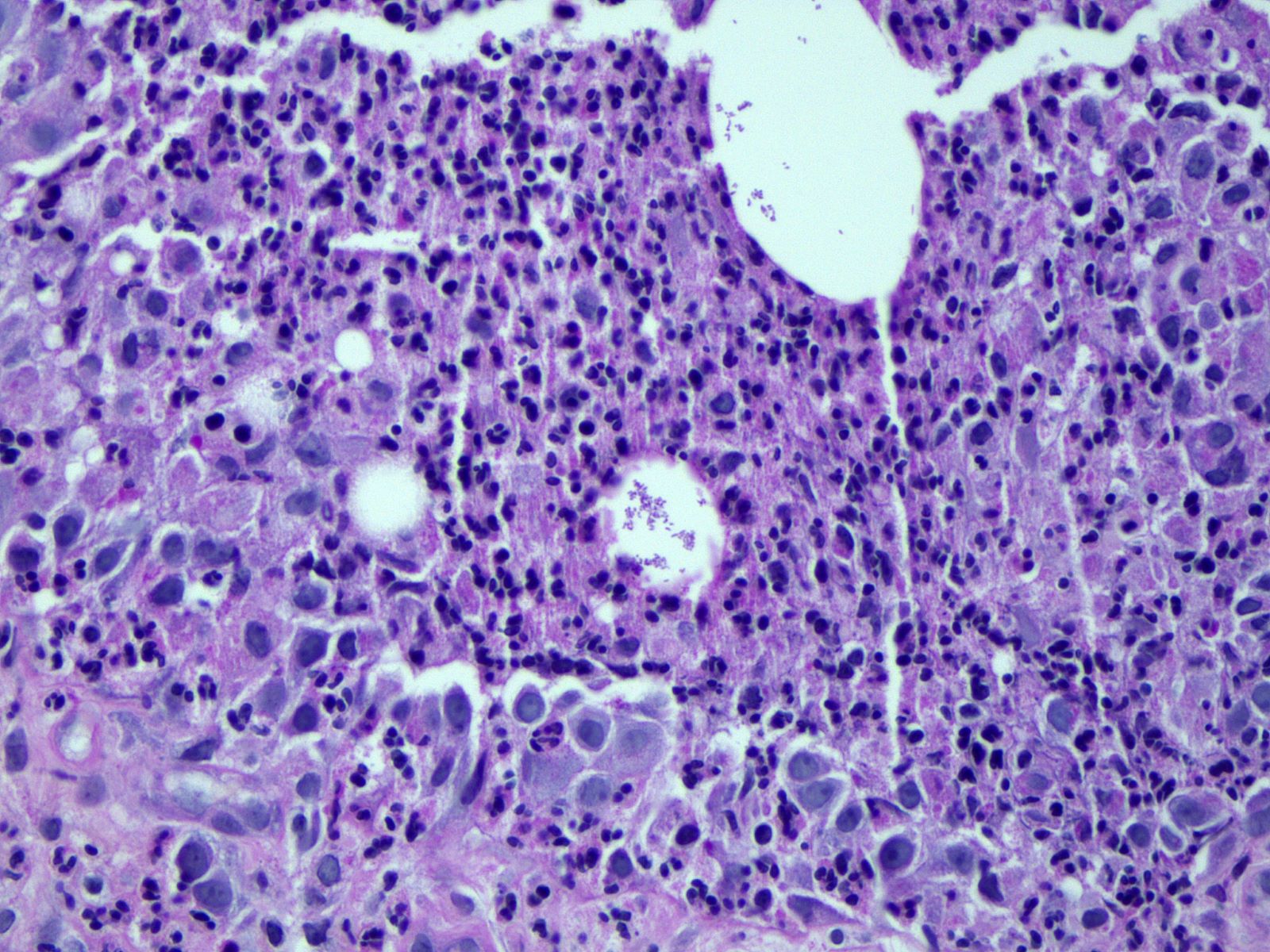
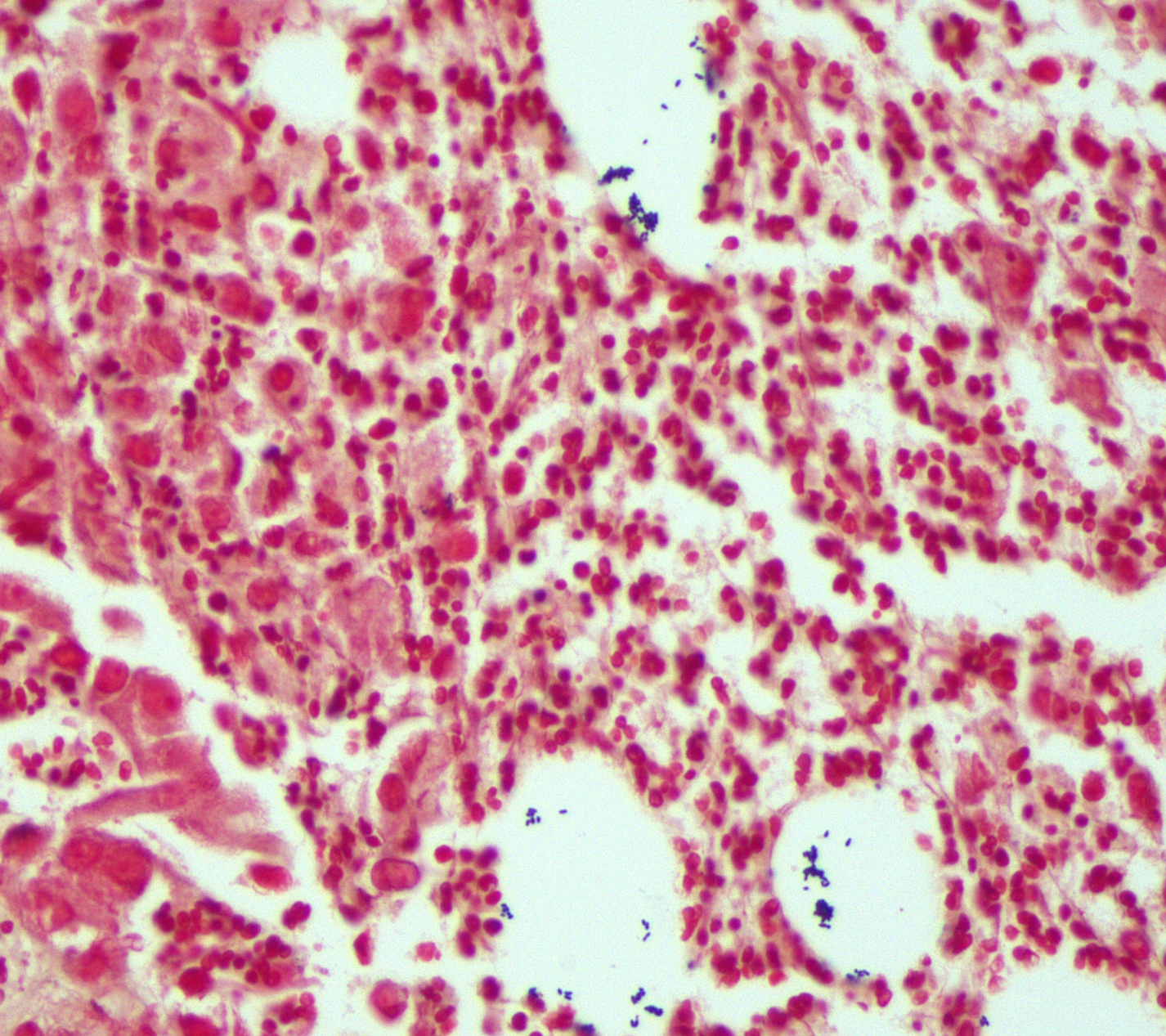
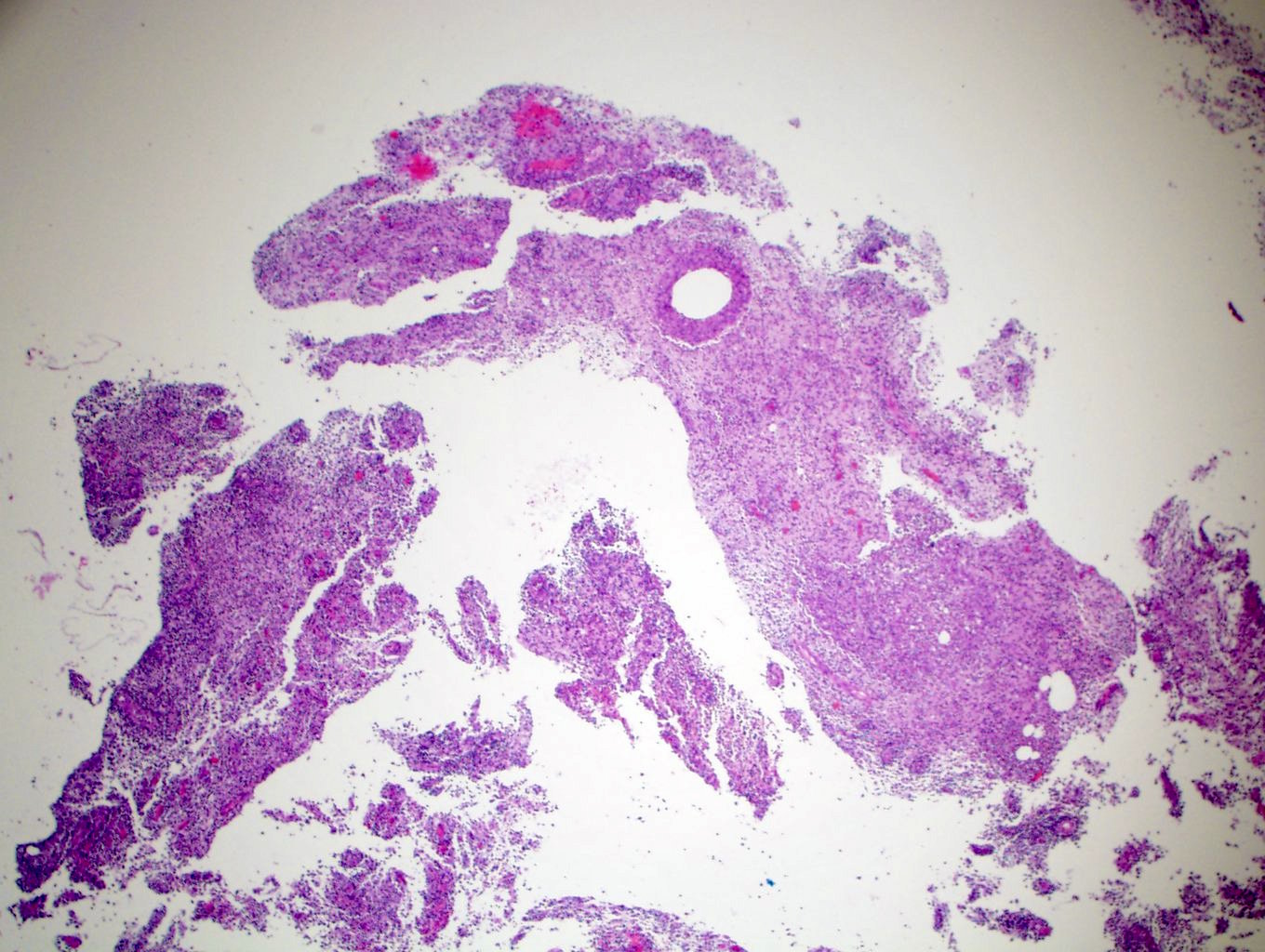
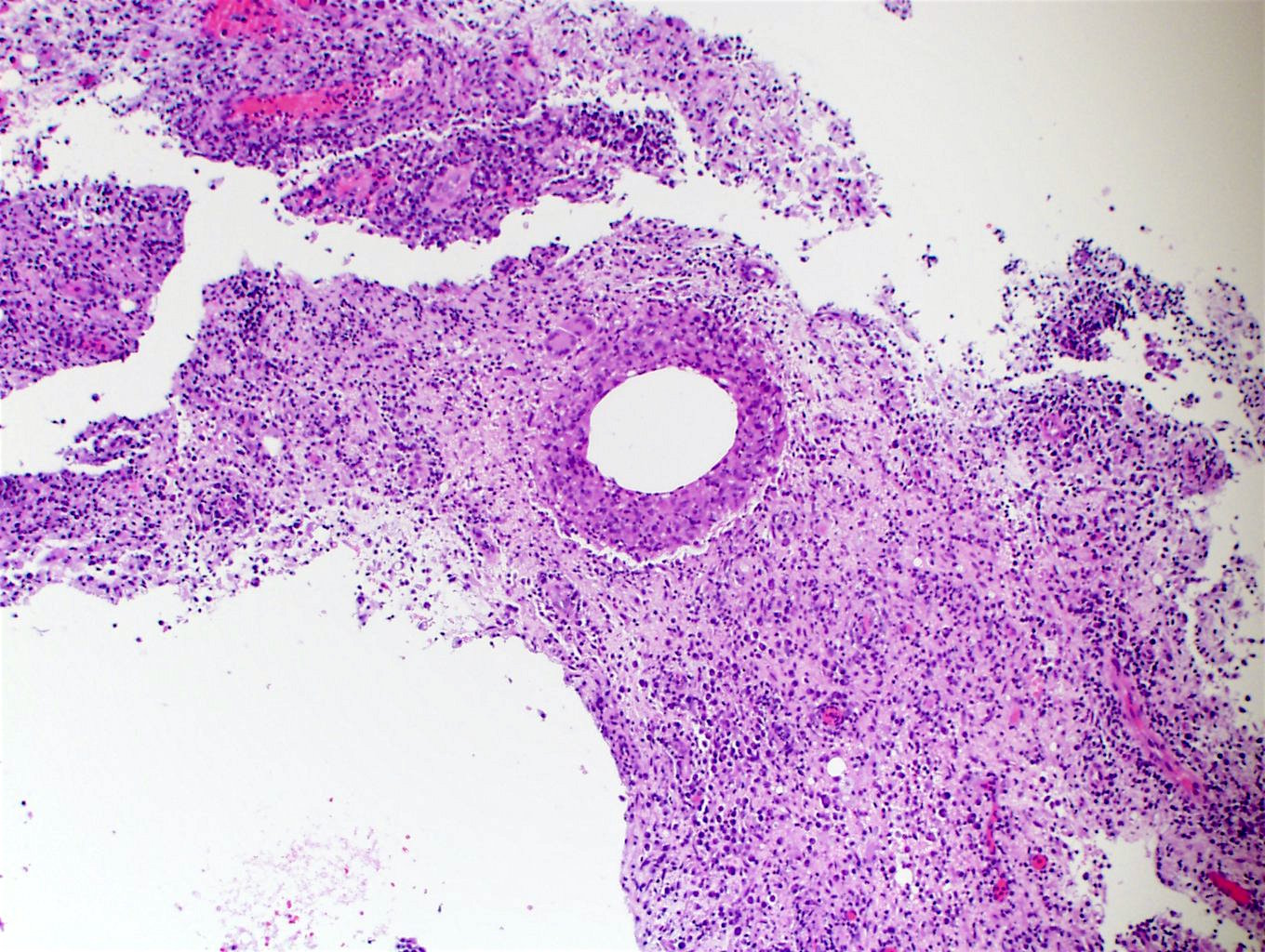
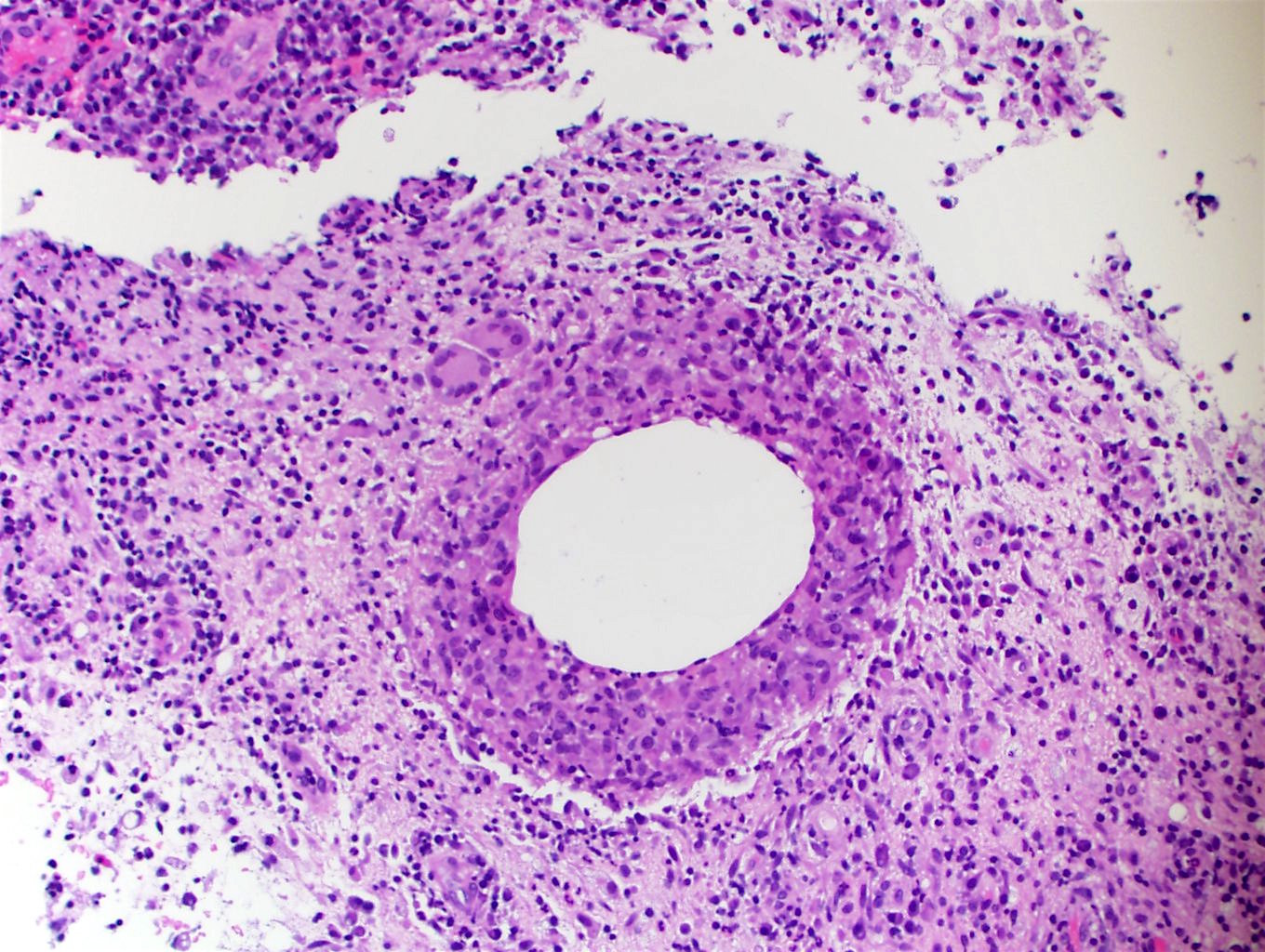
Microscopic (histologic) description
- Presence of 2 - 3 of the following features (J Clin Pathol 2020;73:445):
- Lobulocentric mixed inflammatory infiltrate composed of lymphocytes, neutrophils and scattered multinucleated giant cells
- Round to oval cystic spaces (lipid vacuoles) rimmed by neutrophils (microabscesses)
- Nonnecrotizing granulomas
- Combined with either:
- Presence of coryneform gram positive bacilli (rod shaped bacteria arranged in V shaped forms or palisades like Chinese characters) within lipid vacuoles or
- Positive Corynebacteria culture or molecular testing
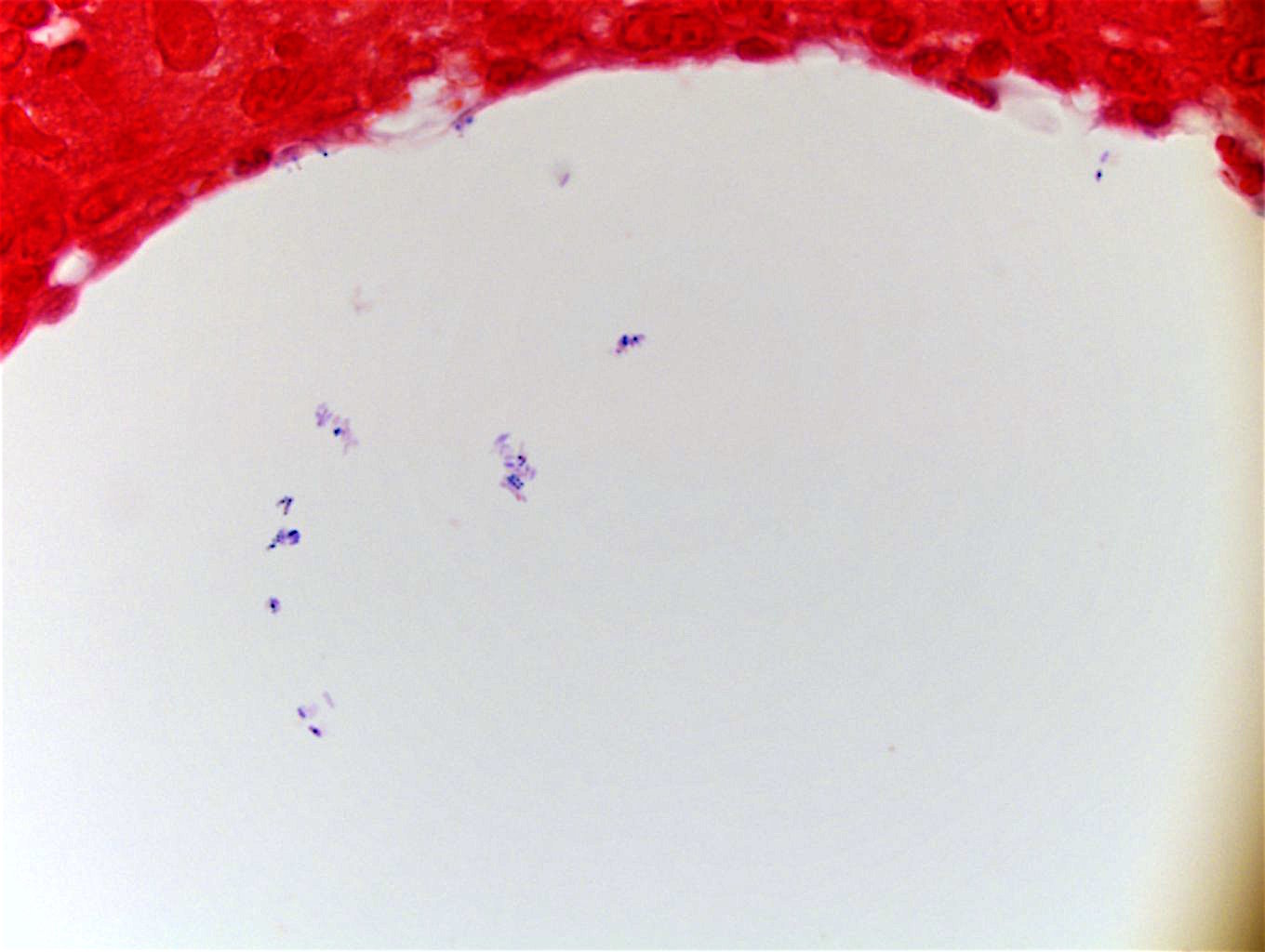
Microscopic (histologic) images
Cytology description
- Cytologic diagnosis may be difficult
- Limited by significant cytomorphologic overlap with granulomatous mastitis and other inflammatory breast lesions
- Features suggestive of cystic neutrophilic granulomatous mastitis on ThinPrep include cystic spaces, inflammatory cells such as neutrophils with aggregates of epithelioid histiocytes, multinucleated giant cells, lymphocytes and plasma cells and lack of necrosis (Diagn Cytopathol 2018;46:966)
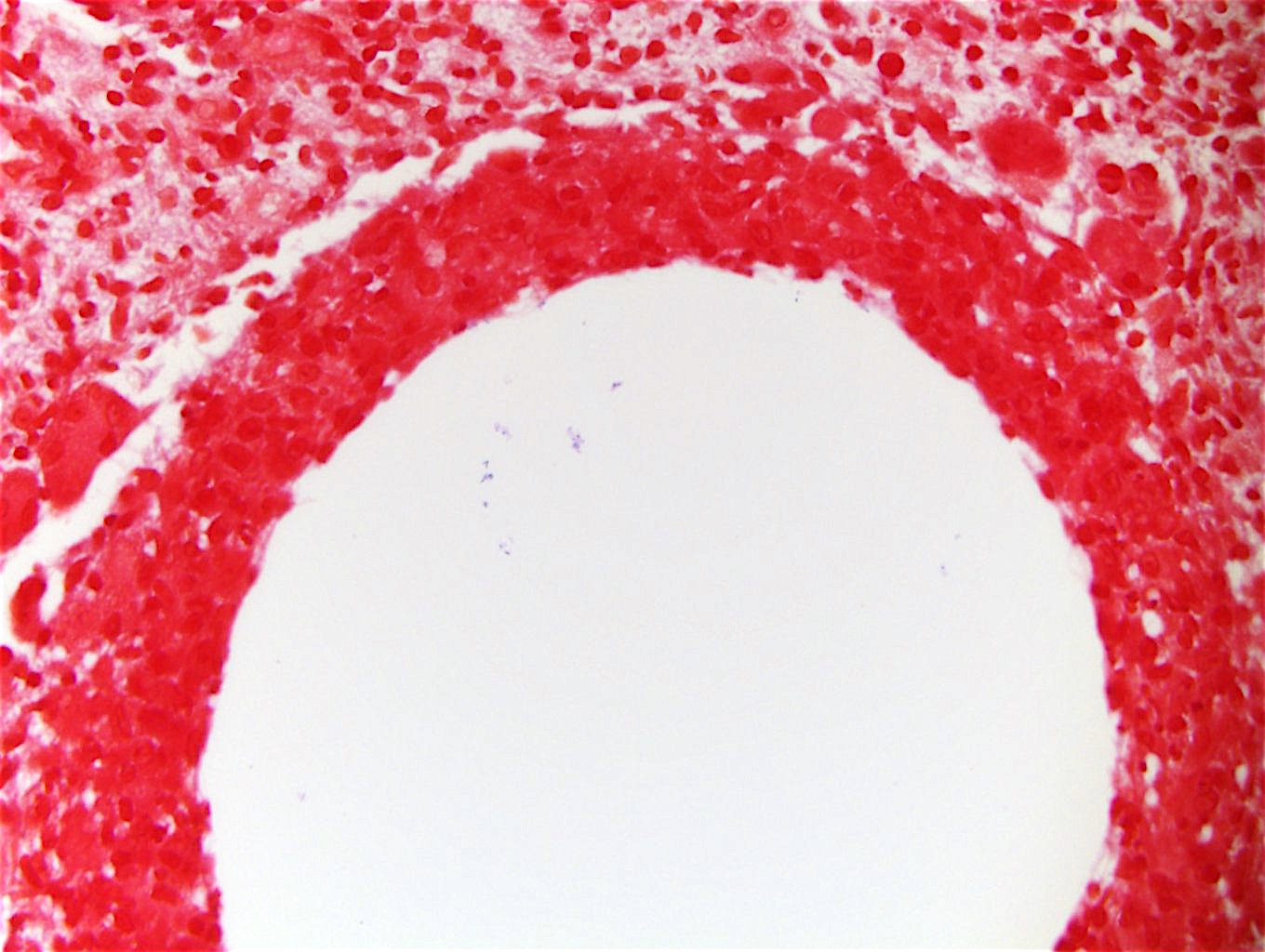
Positive stains
- CD68: positive in histiocytes
- Gram positive coryneform bacteria within lipid vacuoles:
- Rod shaped bacteria arranged in V shaped forms or palisades like Chinese characters
- Bacteria may not be identified in all lipid vacuoles
- Thick section Gram stain performed at 6 µm (vs 4 µm) improves both detection rate and ease of identification of gram positive bacilli (Am J Clin Pathol 2020;153:593)
Negative stains
- Pancytokeratin: negative in histiocytes
Molecular / cytogenetics description
- Matrix assisted laser desorption / ionization time of flight mass spectrometry (MALDI-TOF MS)
- 16S rRNA and rpoB gene sequencing (J Thorac Dis 2017;9:3239, J Clin Microbiol 2005;43:1934, Int J Surg Pathol 2020;28:371)
Sample pathology report
- Right breast, core biopsy:
- Cystic neutrophilic granulomatous mastitis (see comment)
- Comment: A tissue gram stain highlights gram positive bacilli, supporting the diagnosis. Controls are appropriate.
- Microscopic description (optional): Sections show a perilobular mixed inflammatory infiltrate composed of central lipid vacuoles rimmed by neutrophils and an outer cuff of epithelioid histiocytes. Some of the lipid vacuoles contain sparse, rod shaped, gram positive bacilli. The surrounding inflammatory infiltrate contains multinucleated giant cells, lymphocytes and neutrophils. The morphology combined with the presence of gram positive bacilli on Gram stain is consistent with cystic neutrophilic granulomatous mastitis.
Differential diagnosis
- Granulomatous mastitis due to other causes:
- Infection (bacterial, fungal, parasitic):
- Tuberculosis mastitis:
- Necrotizing or nonnecrotizing granulomas composed of epithelioid histiocytes, Langerhans type multinucleated giant cells, eosinophils, lymphocytes and plasma cells commonly affecting ducts rather than lobules
- Ziehl-Neelsen staining, culture or polymerase chain reaction can be used for establishing the diagnosis
- Tuberculosis mastitis:
- Foreign body reaction:
- Presence of foreign material
- Fat necrosis:
- Clinical history, vacuoles lacking gram positive bacilli
- Autoimmune diseases:
- Granulomatosis with polyangiitis:
- Positive pANCA and cANCA, prominent vasculitis
- Rheumatoid arthritis:
- Joint symptoms, elevated rheumatoid factor, fibrinoid necrosis surrounded by lymphocytes and plasma cells
- Granulomatosis with polyangiitis:
- Sarcoidosis:
- Non-necrotizing epithelioid granulomas, asteroid bodies, Schaumann bodies
- Granulomatous lobular mastitis:
- Diagnosis of exclusion, negative microbiologic examination, without known etiology
- Infection (bacterial, fungal, parasitic):
- Subareolar breast abscesses / squamous metaplasia of lactiferous ducts (SMOLD):
- Strongly associated with smoking
- Predominantly anaerobic organisms
Additional references
Board review style question #1
A 35 year old woman presents with a right breast mass. Core biopsy shows empty appearing cystic spaces rimmed by neutrophils and an outer cuff of epithelioid histiocytes. Some vacuoles contain sparse, rod shaped bacilli. Which organism is most commonly associated with this type of granulomatous mastitis?
- Corynebacterium diphtheriae
- Corynebacterium kroppenstedtii
- Mycobacterium tuberculosis
- Staphylococcus aureus
- Staphylococcus epidermidis
Board review style answer #1
B. Corynebacterium kroppenstedtii. Cystic neutrophilic granulomatous mastitis is most commonly associated with Corynebacterium kroppenstedtii.
Comment Here
Reference: Cystic neutrophilic granulomatous mastitis
Comment Here
Reference: Cystic neutrophilic granulomatous mastitis
Board review style question #2
Cystic neutrophilic granulomatous mastitis most commonly affects which of the following patient population?
- Female smokers
- Parous women
- Postmenopausal women
- Women living in endemic areas of tuberculosis
- Women with a history of Corynebacterium diphtheriae infection
Board review style answer #2
B. Parous women. Cystic neutrophilic granulomatous mastitis most commonly affects women who are currently pregnant or have been pregnant.
Comment Here
Reference: Cystic neutrophilic granulomatous mastitis
Comment Here
Reference: Cystic neutrophilic granulomatous mastitis
Board review style question #3
Which of the following statements is true regarding cystic neutrophilic granulomatous mastitis?
- Diagnosis may require matrix assisted laser desorption / ionization time of flight mass spectrometry
- Gram positive bacilli are identified in nearly all cases
- Resolution typically takes days
- Usually presents as a painless palpable mass in postmenopausal women
Board review style answer #3
A. Diagnosis may require matrix assisted laser desorption / ionization time of flight mass spectrometry. Diagnosis of cystic neutrophilic granulomatous mastitis may require culture, 16S rRNA gene sequencing or matrix assisted laser desorption / ionization time of flight mass spectrometry.
Comment Here
Reference: Cystic neutrophilic granulomatous mastitis
Comment Here
Reference: Cystic neutrophilic granulomatous mastitis