Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Tomar R. Tuberculosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/breastTB.html. Accessed December 21st, 2024.
Definition / general
- Breast is a rare extrapulmonary site of tuberculosis in young women in developing countries
Essential features
- Primary or secondary infection of breast tissue by Mycobacterium tuberculosis (MTB)
- Affects young, multiparous, lactating female patients in endemic regions or with HIV co-infection
- Most common presentation is a breast lump that can mimic a pyogenic abscess or malignancy
- Fine needle aspiration cytology (FNAC) or core needle biopsy (CNB) shows necrotizing granulomatous inflammation; MTB should be confirmed by microbiologic culture, Ziehl Neelsen (ZN) stain or nucleic acid amplification testing (NAAT)
- Successfully responds to antitubercular therapy (ATT)
Terminology
- Tuberculosis (TB) of the breast
- Mammary tuberculosis
- Tubercular mastitis
ICD coding
- ICD-10: A18.89 - tuberculosis of other sites
Epidemiology
- Accounts for 0.1% of breast lesions in Western countries (Indian J Surg 2015;77:1378)
- Constitutes 3 - 4.5% of breast diseases in developing regions like Asia and Africa (Indian J Surg 2015;77:1378)
- Can occur in any age, mostly 20 - 40 years, which parallels with a high incidence of pulmonary TB (Int J Mycobacteriol 2024;13:1)
- Mostly affects young, multiparous, nursing women; less common in prepubescent and postmenopausal patients (Clin Case Rep 2024;12:e8826, Int J Surg Case Rep 2022;96:107242)
- Risk factors: pregnancy, crowded areas, trauma (Int J Surg Case Rep 2022;96:107242)
- Associated with immunosuppressed states, like human immunodeficiency virus (HIV) (Pan Afr Med J 2020;37:282)
- Males are rarely affected (Postgrad Med J 2002;78:422, ANZ J Surg 2006;76:234, Cureus 2019;11:e4709)
Sites
- Breast parenchyma and overlying skin
- Usually unilateral; bilateral localization is rare (Clin Case Rep 2024;12:e8826)
- Axillary lymph node involvement in 50 - 75% of cases
Pathophysiology
- Breast tissue (like spleen or skeletal muscle) provides an infertile environment for the survival and multiplication of TB bacilli
- Lactation makes it more susceptible to infection due to duct ectasia, increased blood supply and potential trauma to nipple
- Breast TB can be primary (breast is the initial route or only site of infection) or secondary (involvement of breast from a tuberculous lesion elsewhere, usually lung) (Ann Thorac Med 2008;3:110)
- Primary mammary TB (rare): direct inoculation of bacilli through lactiferous ducts, nipple lesion, skin abrasion
- Secondary mammary TB (more common): multiple routes of infection, such as lymphatic, hematogenous (miliary) or contiguous spread (World J Surg 1995;19:379, Eur J Cardiothorac Surg 2002;22:324)
- Lymphatic retrograde extension from axillary nodes seems most likely, given the presence of ipsilateral axillary lymphadenitis in > 50% of cases
- Miliary TB with generalized hematogenous dissemination is rare
- Contiguous spread is from intrathoracic foci, pleura or chest wall
Etiology
- Mycobacterium tuberculosis
Clinical features
- Scrofulous swelling of the bosom is its first description by Sir Astley Cooper in 1829
- Lump is the most common symptom (Indian J Surg 2015;77:1378)
- Lumps can be mobile or fixed, mostly in the central or upper outer quadrant (Indian J Surg 2015;77:1378)
- Can be painful or painless (Indian J Surg 2015;77:1378, Int J Mycobacteriol 2024;13:1)
- Solitary or multiple confluent nodules
- Nipple skin retraction can be seen (Indian J Surg 2015;77:1378)
- Purulent nipple discharge is rare (Indian J Surg 2015;77:1378)
- Can be misdiagnosed as a nonspecific abscess, fibroadenoma or carcinoma (Indian J Surg 2015;77:1378)
- Can present with ulcer, fistula or abscess (Indian J Surg 2015;77:1378)
- Peau d'orange or skin thickening over the lesion can be seen
- Ipsilateral axillary lymphadenitis, with enlarged and then matted nodes frequently present
- Constitutional symptoms (fever, malaise, weight loss, night sweats) < 20% of cases
- Clinical classification (Indian J Surg 2015;77:1378, Int J Surg Case Rep 2022;96:107242)
- Original classification by Mckeown et al. (Br J Surg 1952;39:420)
- Nodular caseous tubercular mastitis
- Most common type; affects young female patients
- Well circumscribed, slow growing, painless mass (may mimic fibroadenoma)
- May progress to involve skin (which causes pain), ulcerate or form sinuses
- Histologically: extensive caseation and little fibrosis
- Disseminated or confluent tubercular mastitis
- Second most common type, caused by highly virulent MTB; occurs in older or immunodeficient patients
- Numerous communicating tubercles involving entire breast, caseation common
- Sinus formation and skin thickening with multiple ulcers.
- Ipsilateral axillary lymph nodes are usually enlarged and matted
- Sclerosing tubercular mastitis (rare)
- Extensive fibrosis, nipple retraction, no suppuration
- Common in the involuting breast in older age; it mimics scirrhous carcinoma
- Tuberculous mastitis obliterans (rare)
- Duct infection induces proliferation of lining epithelium and marked periductal fibrosis, leading to ductal occlusion and cystic dilations (cystic mastitis)
- Acute miliary tubercular mastitis (rare)
- Part of a generalized disseminated form of TB with hematogenous spread
- Nodular caseous tubercular mastitis
Diagnosis
- FNAC is the investigation of choice (Indian J Surg 2015;77:1378)
- Gold standard for diagnosis: detection of M. tuberculosis by Ziehl-Neelsen staining for acid fast bacteria or organism isolation from the lesion on culture (Int J Mycobacteriol 2024;13:1)
- TB mastitis is paucicellular / paucibacillary (Indian J Surg 2015;77:1378)
- See Molecular / cytogenetics description
Laboratory
Radiology description
- Ultrasound (US) / mammography / magnetic resonance imaging (MRI): not sensitive or specific but can give diagnostic clues (Int J Mycobacteriol 2024;13:1)
- US: heterogenous hypoechoic lesion, peripheral hypervascularization and edematous infiltration of the breast fat tissue or skin bulge (Int J Surg Case Rep 2022;96:107242, Insights Imaging 2021;12:19)
- Mammography: diffuse heterogenous limited opacity with microcalcifications and skin retraction at times (Int J Surg Case Rep 2022;96:107242, Insights Imaging 2021;12:19)
- Chest Xray: normal (Int J Surg Case Rep 2022;96:107242)
Prognostic factors
- Prognosis is good with antitubercular treatment (Pan Afr Med J 2020;37:282)
Case reports
- 24 year old woman with bilateral breast tuberculosis (Clin Case Rep 2024;12:e8826)
- 28 and 35 year old women presented with neoplastic-like tuberculosis of the breast (Int J Surg Case Rep 2022;96:107242)
- 31 year old Indian woman presented with tubercular mastitis mimicking a malignancy (Prague Med Rep 2020;121:267)
- 34 year old woman presented with rare extrapulmonary presentation of tuberculosis (Clin Case Rep 2023;11:e7728)
- 45 year old postmenopausal woman presented with coexistence of carcinoma and tuberculosis in 1 breast (J Transl Int Med 2015;3:32)
- 52 year old woman with breast tuberculosis presented with a painful lump (IDCases 2021;26:e01341)
Treatment
- Often delayed due to difficulty in confirming the diagnosis
- Antitubercular treatment (95% success rate with 6 month treatment) (Indian J Surg 2015;77:1378)
- Surgical drainage of abscess may be needed
- Breast abscess not responding to antibiotics should be evaluated for TB (Clin Case Rep 2024;12:e8826)
Gross description
- Nodular, indurated gray or tan tissue with yellow to white foci of caseous necrosis
- Confluent nodular lesions with central cavitation grossly resemble necrotic carcinoma or suppurative abscess
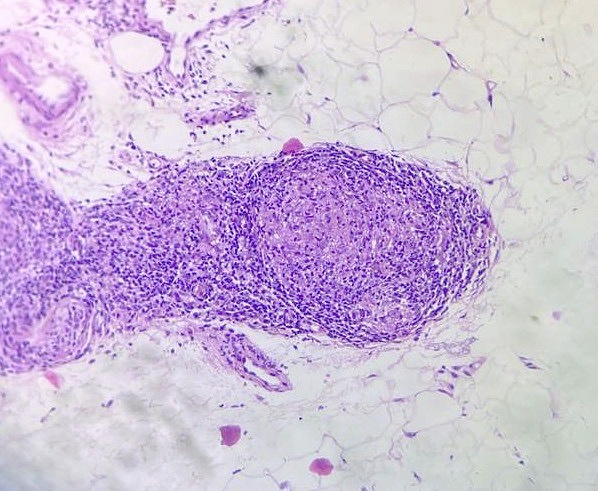
Microscopic (histologic) description
- Epithelioid cell granulomas
- Langhans giant cells
- Caseous necrosis
- Lymphohistiocytic aggregates
- Fibrosis can be seen
- TB mastitis affects ducts more than lobules (Turk Patoloji Derg 2022;38:40, Indian J Surg 2015;77:1378)
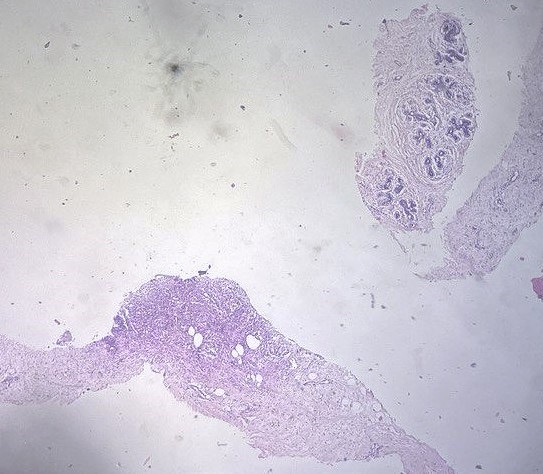
Microscopic (histologic) images
Contributed by Reena Tomar, M.B.B.S., M.D.
Cytology description
- Smears from left breast are moderately cellular showing epithelioid cell granulomas, Langhans giant cells with caseous necrosis
- Lymphoid cells with histiocytes are also seen
- Clusters of ductal cells are seen in background
- Reference: Turk Patoloji Derg 2019;35:128
Cytology images
Positive stains
- Stain for AFB is positive for rod shaped beaded pink Mycobacterium tuberculosis bacilli
- Ziehl-Neelsen stain
Molecular / cytogenetics description
- GeneXpert MTB RIF: cartridge based automated test that identifies Mycobacterium DNA and response to rifampicin (RIF) by nucleic acid amplification techniques (NAAT) (Turk J Med Sci 2023;53:744, IDCases 2021;26:e01341)
- Molecular tests shown below are for tuberculosis in general and still in experimental phases for breast TB
| Advantages | Disadvantages | |
| Polymerase chain reaction (PCR) | Rapid, high sensitivity and specificity; low sample requirement | Costly; may not confirm active infection |
| GeneXpert MTB / RIF | Rapid, detects rifampicin resistance, automated | Expensive; false negatives in low burden samples |
| Line probe assay (LPA) | Rapid multidrug resistance testing | Complex, costly; requires higher bacterial load |
| Loop mediated isothermal amplification (LAMP) | Fast, cost effective, minimal equipment needed | Limited validation for breast TB; not widely available |
| Interferon gamma release assay (IGRA) | Noninvasive; useful for detecting latent TB | Cannot confirm active TB; lower sensitivity in immunocompromised patients |
Sample pathology report
- Left breast, Trucut biopsy:
- Tubercular mastitis (see comment)
- Microscopy: Section shows benign breast ductules with fibrocollagenous stroma with adjacent mature adipose tissue with the presence of multiple well defined epithelioid cell granulomas, caseous necrosis and Langhans giant cells. Lymphohistiocytic infiltrate is also seen. Ziehl-Neelsen stain for AFB is positive.
- Comment: Advise follow up after antitubercular treatment.
Differential diagnosis
- Breast carcinoma:
- Clinically can mimic malignancy due to a painful solid lump
- Pyogenic / nonspecific abscess:
- Clinically presents as an ulcer, abscess with fever, which is also seen in tubercular mastitis
- Absence of TB bacilli on Ziehl-Neelsen stain can lead to misdiagnosis of pyogenic abscess
- Pyogenic abscess will respond to antibiotics, which is ineffective in tubercular mastitis
- Pathological findings of granulomatous inflammation encompass a wide range of differential diagnoses, such as
- Sarcoidosis:
- Noncaseating granulomas with other features like asteroid bodies
- Necrosis is rarely seen
- Lobular granulomatous mastitis:
- Noncaseating granulomas
- Absence of TB bacilli on Ziehl-Neelsen stain
- Treatment includes steroids, which may flare up tuberculosis
- Granulomatous reaction to tumor, leprosy, cat scratch disease, syphilis, histoplasmosis, Cryptococcus, Crohn's disease
- Sarcoidosis:
Board review style question #1
A 30 year old woman presented with a 2 x 2 cm firm, indurated mass in her right breast. She has associated nipple retraction and no axillary lymphadenopathy with a history of tuberculosis treated 5 years ago. A biopsy shows granulomatous inflammation and PCR is positive for Mycobacterium tuberculosis. Which of the following diagnoses is most likely?
- Granulomatous mastitis
- Invasive ductal carcinoma
- Primary tuberculous mastitis
- Secondary tuberculous mastitis
Board review style answer #1
D. Secondary tuberculous mastitis arises from an existing tuberculosis focus elsewhere in the body, commonly in the lungs. The patient's history of tuberculosis, granulomatous inflammation and positive PCR suggest a secondary spread rather than primary inoculation. Answer C is incorrect because the patient has a history of tuberculosis. Answer A is incorrect because a history of tuberculosis was indicated and PCR is positive for Mycobacterium tuberculosis. Answer B is incorrect because there are no malignant cells seen in the biopsy.
Comment Here
Reference: Tuberculosis
Comment Here
Reference: Tuberculosis
Board review style question #2
A 22 year old nulliparous woman presents with a mobile breast lump with a focal abscess on the skin and a fever for 10 days. The patient comes from a crowded community. She is not responding to a week of antibiotics. Chest Xray was normal and erythrocyte sedimentation rate (ESR) was raised. A Trucut biopsy demonstrates features shown in the image above. What is the probable diagnosis?
- Breast carcinoma
- Cystic neutrophilic granulomatous mastitis (CNGM)
- Pyogenic abscess
- Tubercular mastitis
Board review style answer #2
D. Tubercular mastitis. The patient is not responding to antibiotics and comes from a crowded environment with constitutional symptoms of tuberculosis. Answer C is incorrect because the patient is not responding to antibiotics. Answer A is incorrect because the lump is mobile and the patient is clinically presenting with symptoms of tuberculosis. Answer B is incorrect because CNGM mainly occurs in multiparous women and responds to antibiotics.
Comment Here
Reference: Tuberculosis
Comment Here
Reference: Tuberculosis