Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Flow cytometry description | Flow cytometry images | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Sukswai N, Khoury J. Blastic plasmacytoid dendritic cell neoplasm. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/bonemarrowneoplasticBPDCN.html. Accessed March 30th, 2025.
Definition / general
- Blastic plasmacytoid dendritic cell neoplasm (BPDCN) is a highly aggressive hematologic malignancy derived from plasmacytoid dendritic cells (pDC) (Curr Hematol Malig Rep 2018;13:477)
Essential features
- Nonneoplastic counterpart: plasmacytoid dendritic cells (Adv Anat Pathol 2009;16:392)
- Over 80% of patients present with skin lesions; other common sites include the bone marrow and lymph nodes
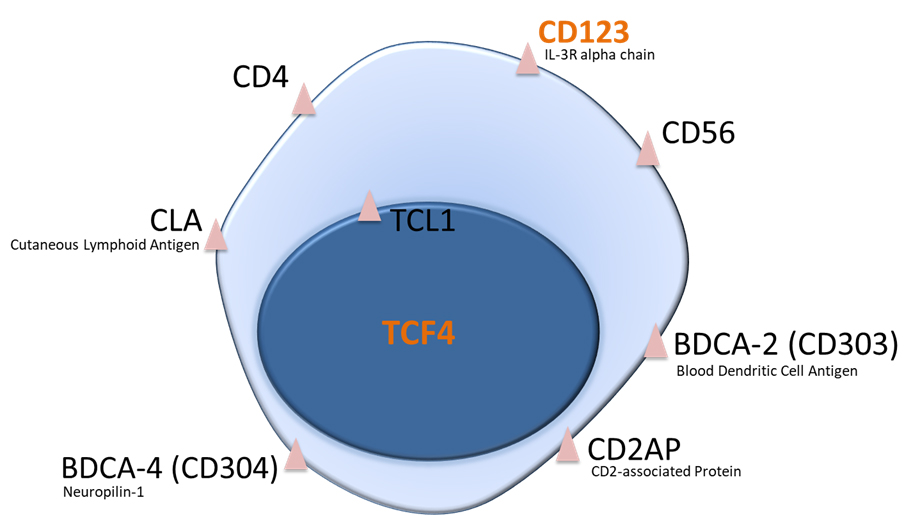
- Expression of CD123 and TCF4 is required for diagnosis; in addition, most cases are positive for CD4, CD56 and TCL1
- Distinction from acute myeloid leukemia (AML) in particular is critical for appropriate therapy selection
Terminology
- Blastic plasmacytoid dendritic cell neoplasm
- Agranular CD4+ / CD56+ hematodermic neoplasm / tumor
- Agranular CD4+ NK cell leukemia
- CD56+ TdT+ blastic NK cell lymphoma
ICD coding
- ICD-O: 9727/3 - blastic plasmacytoid dendritic cell neoplasm
Epidemiology
- Rare, representing < 1% of hematologic malignancies (Leuk Res 2018;73:21)
- Incidence is 0.04 cases per 100,000 in U.S.
- M:F = 3:1
- Most patients are in fifth or sixth decades of life but the disease can affect any age group, including pediatric
Sites
- Skin, bone marrow, lymph nodes and spleen are most common but any anatomic site can be involved
- CSF involvement at presentation in up to 10% of patients, more at relapse (Oncotarget 2016;7:10174)
Pathophysiology
- Postulated cell of origin is pDC, which plays an important role in bridging the innate and adaptive immune systems (Curr Hematol Malig Rep 2018;13:477)
- Monoallelic and biallelic 12p / ETV6 deletions seem to represent an early pathogenic event (Leuk Res 2018;73:86)
- BPDCN specific transcriptional network regulated by the E-box transcription factor TCF4 (also known as E2-2) that plays a master regulatory role in BPDCN cells and appears to be in turn regulated by the bromodomain and extraterminal domain (BET) protein BRD4 (Cancer Cell 2016;30:764)
- Epigenetic dysregulation is very common and results from mutations in genes involved in DNA methylation, histone methylation and chromatin remodeling (Haematologica 2019;104:729)
- Frequent NR3C1 haploinsufficiency linked to aberrant overexpression of a novel long noncoding RNA (lncRNA) gene, lincRNA-3q, whose product is involved in G1/S cell cycle transition through E2F (Blood 2016;127:3040)
- BPDCN cells are highly dependent on BCL2 for survival (Cancer Discov 2017;7:156)
- Neoplastic cells in BPDCN have features of nonactivation state and seem to arise in a background of immunodeficiency (Blood Cancer J 2019;9:99)
Etiology
- No known etiology
- Frequent association with other myeloid malignancies, including chronic myelomonocytic leukemia and myelodysplastic syndrome
- No bacterial or viral pathogen (Blood Adv 2020;4:1006)
Clinical features
- Skin lesions, with heterogeneous manifestations of bruise-like, violaceous maculopapular lesions, nodules, plaques or exanthema
- ~10% of patients have an overt leukemic presentation (Am J Hematol 2013;88:1055)
- B symptoms
- Lymphadenopathy
- Splenomegaly
Diagnosis
- Malignant infiltrate of blastoid cells; need to distinguish from mature pDC proliferations (MPDCP)
- Confirmation of pDC immunophenotype by flow cytometry or immunohistochemistry
- Cytogenetic and molecular studies usually not required for diagnosis
Laboratory
- Cytopenias are common but some patients have normal CBC findings
Prognostic factors
- No known pathologic or molecular prognostic factors
Case reports
- 62 year old woman with BPDCN exhibiting unusual lymphoid features and macrovacuoles (Ann Hematol 2019;98:2221)
- 63 year old man with disseminated blastic plasmacytoid dendritic cell neoplasm (Blood 2015;126:558)
Treatment
- Tagraxofusp, a CD123 targeted immunotoxin, is the first FDA approved treatment for BPDCN (N Engl J Med 2019;380:1628)
- ALL type induction chemotherapy regimens are associated with better outcomes compared with AML type regimens
- Allogeneic stem cell transplant is recommended for patients who achieve first complete remission and are fit (Hematol Oncol Clin North Am 2020;34:621)
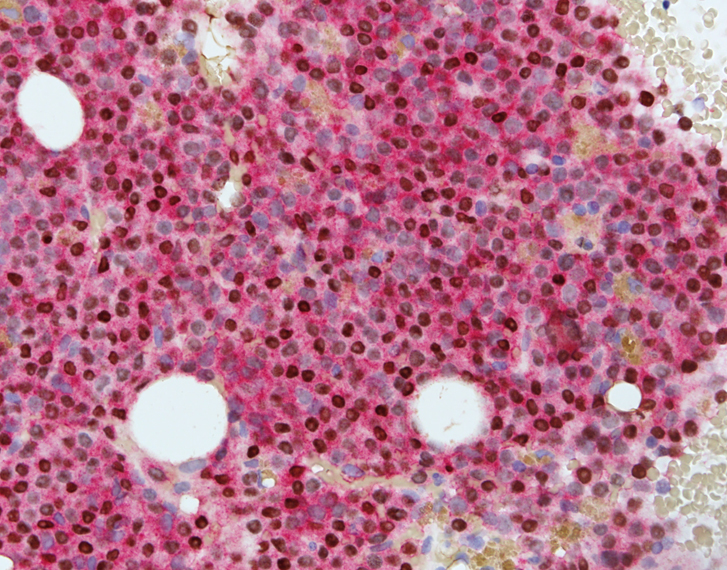
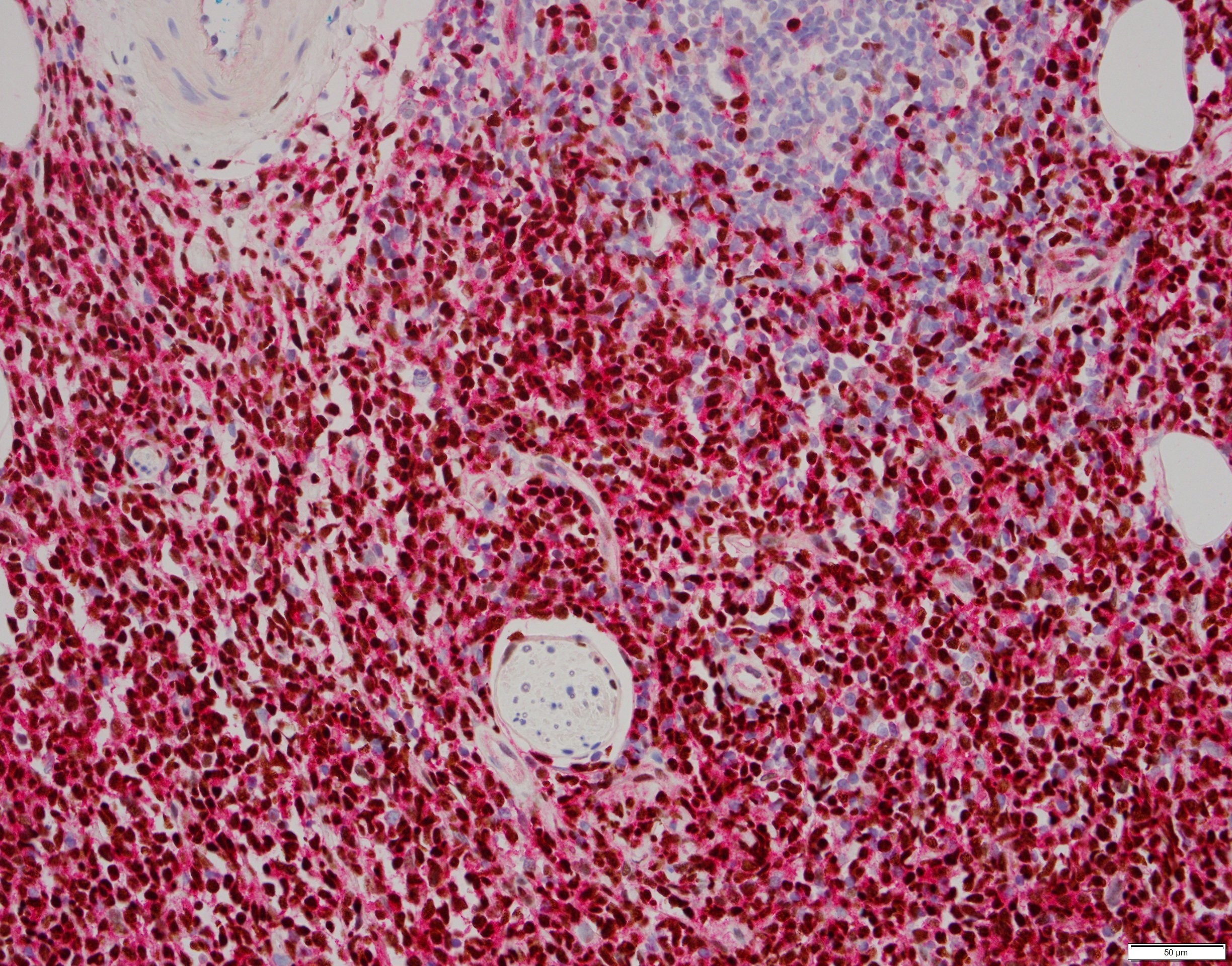
Microscopic (histologic) description
- Diffuse infiltrate seen on bone marrow biopsy (trephine) and clot preparation with replacement of hematopoietic elements
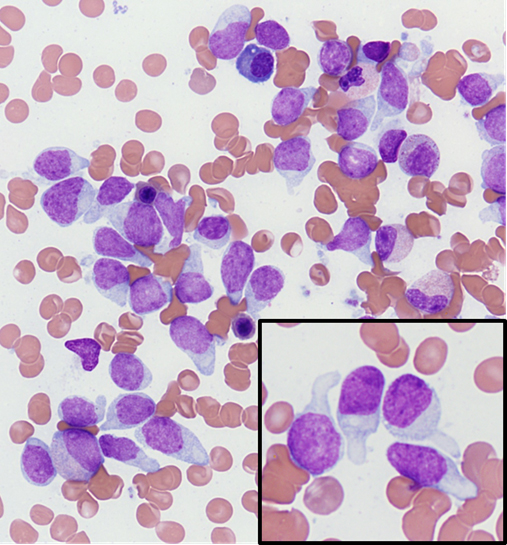
- On Wright-Giemsa preparations, the neoplastic cells are elongated with a tapered lightly basophilic agranular cytoplasm that ends with a tail shaped structure; the nucleus has blastoid features with open chromatin and a prominent nucleolus
- In some cases, neoplastic cells have cytoplasmic microvacuoles with a peculiar arrangement along the cytosolic aspect of the cell membrane resembling a pearl necklace
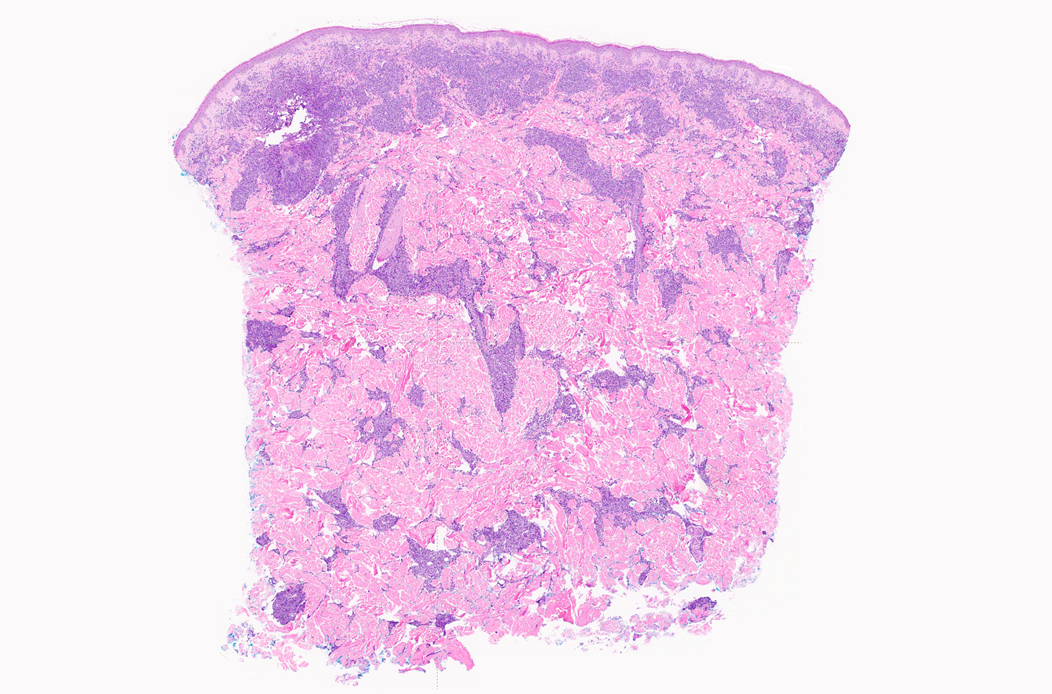
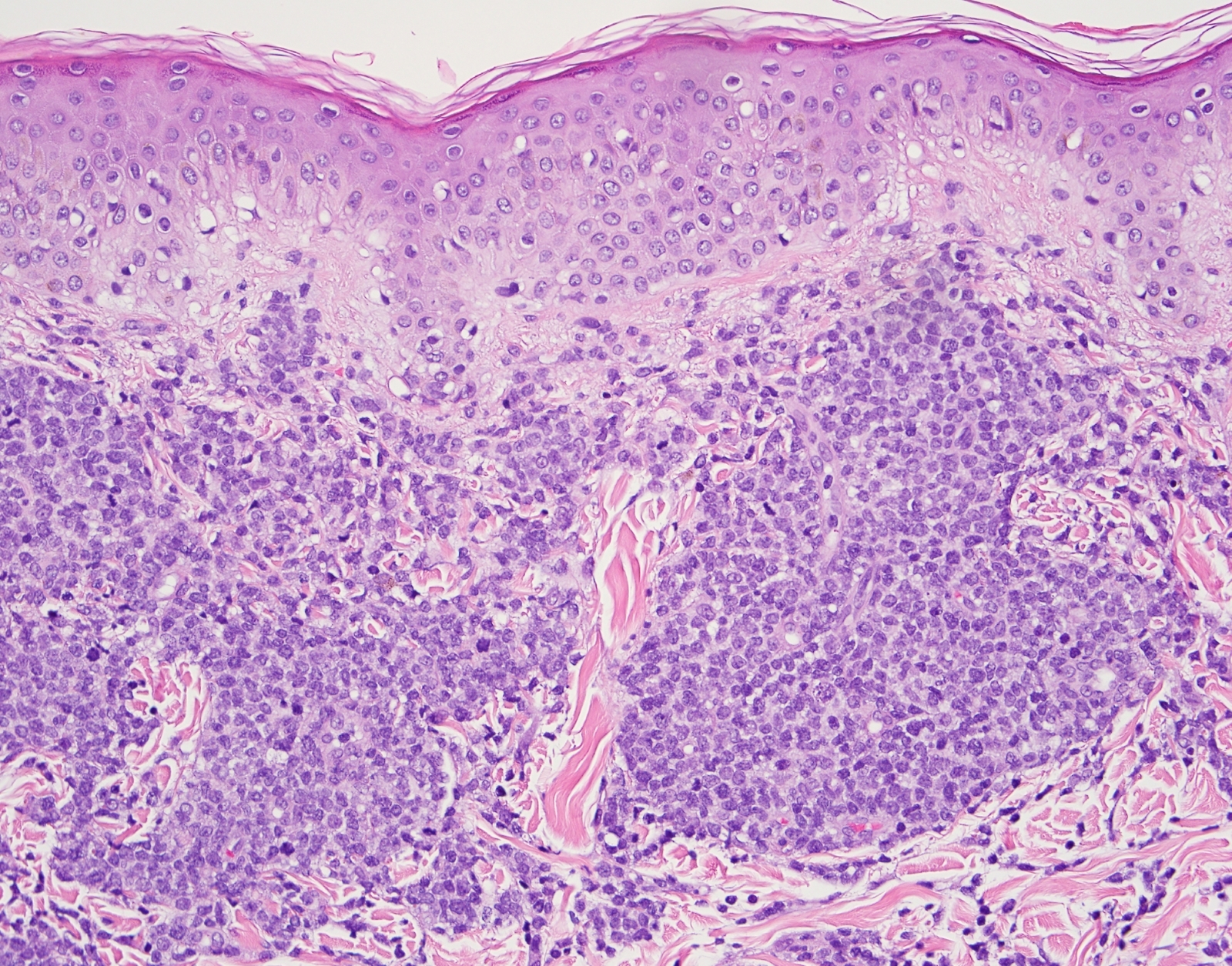
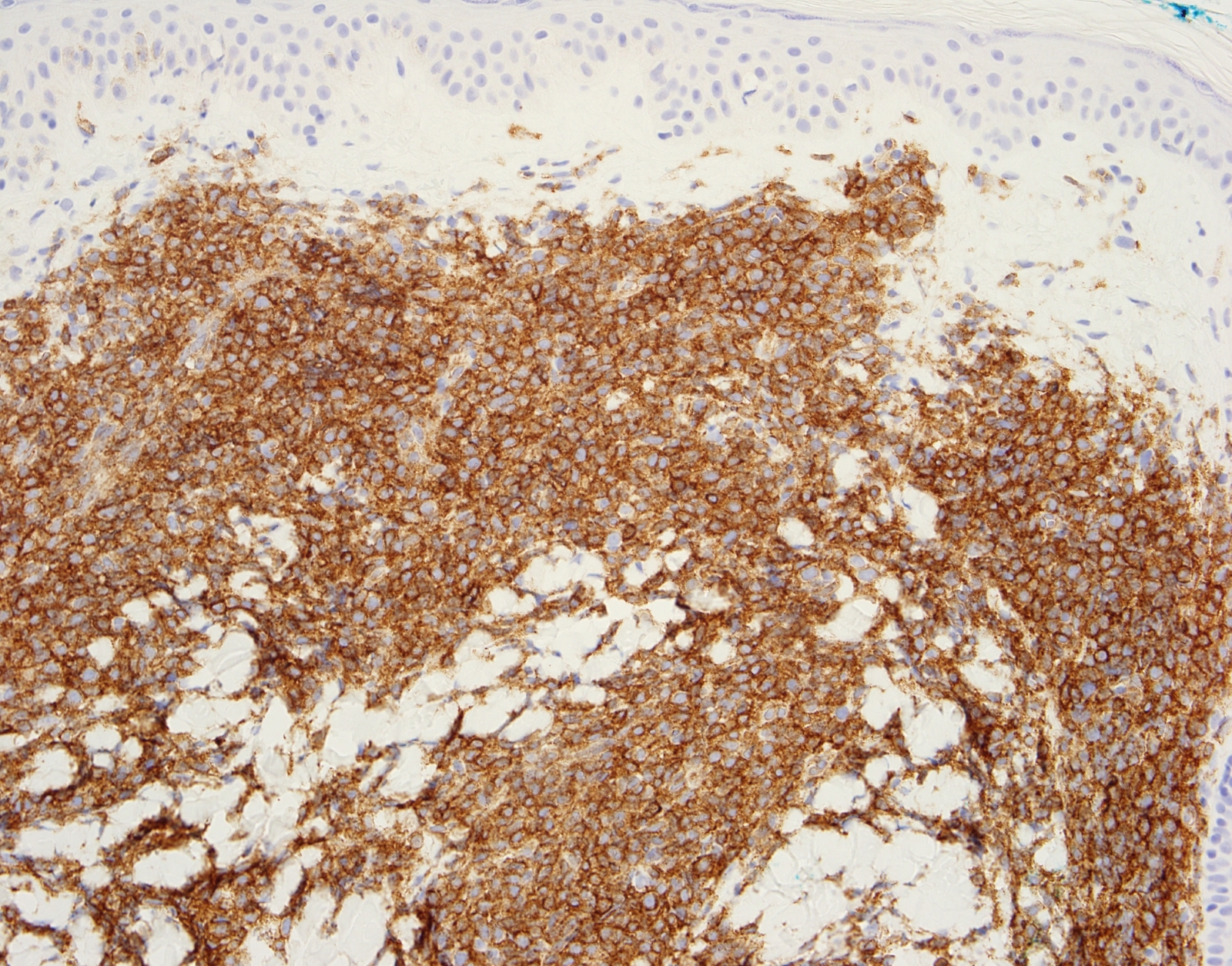
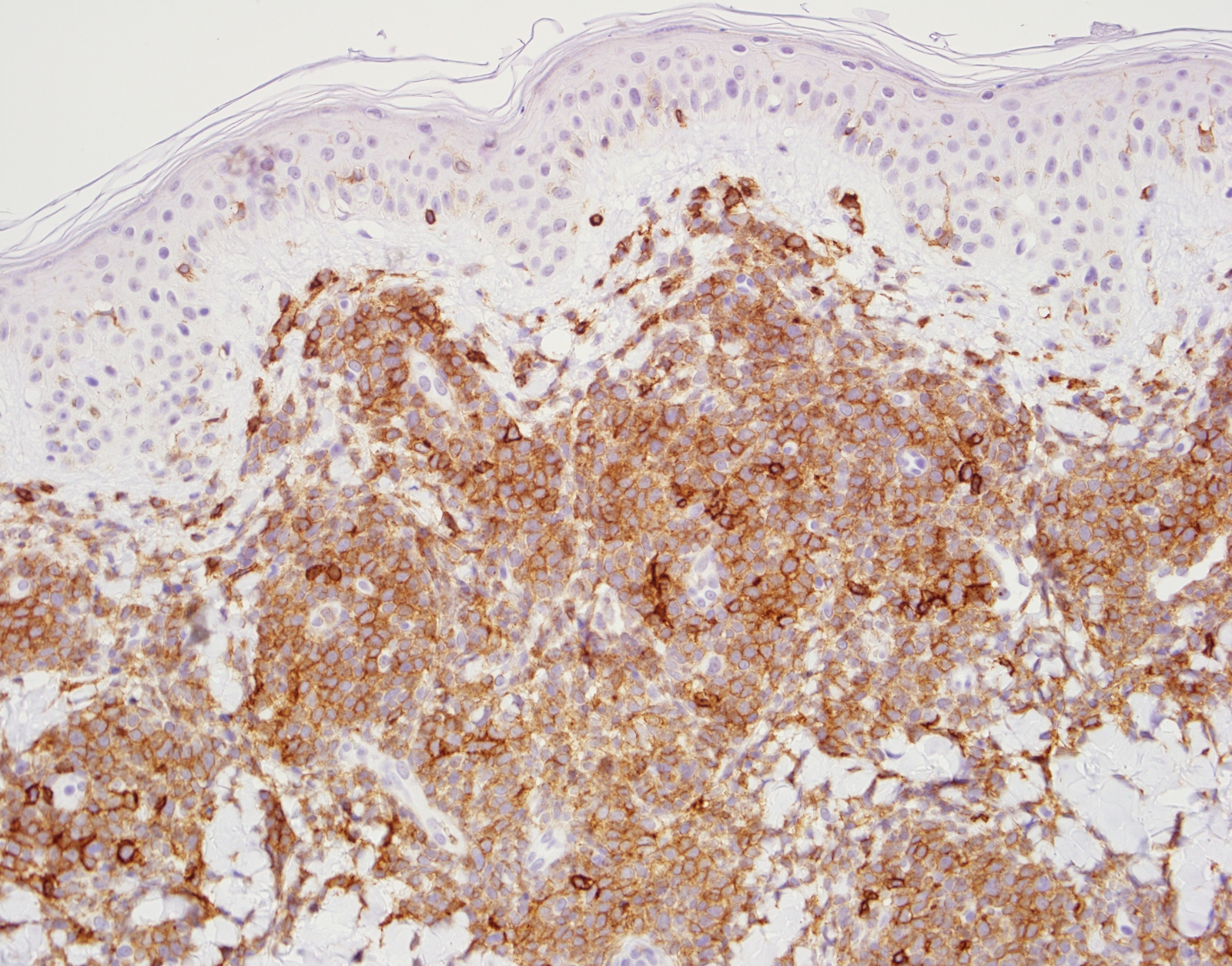
- Skin involvement is characterized by infiltrates of immature neoplastic cells with blastoid morphology involving the superficial and deep dermis, often with extension into the subcutis; the epidermis is typically spared; mitotic figures are usually identified readily
Microscopic (histologic) images
Positive stains
Negative stains
- Lineage specific markers, including CD3, CD19, CD20, PAX5, lysozyme, myeloperoxidase
- CD34
- MNDA (Am J Surg Pathol 2016;40:502)
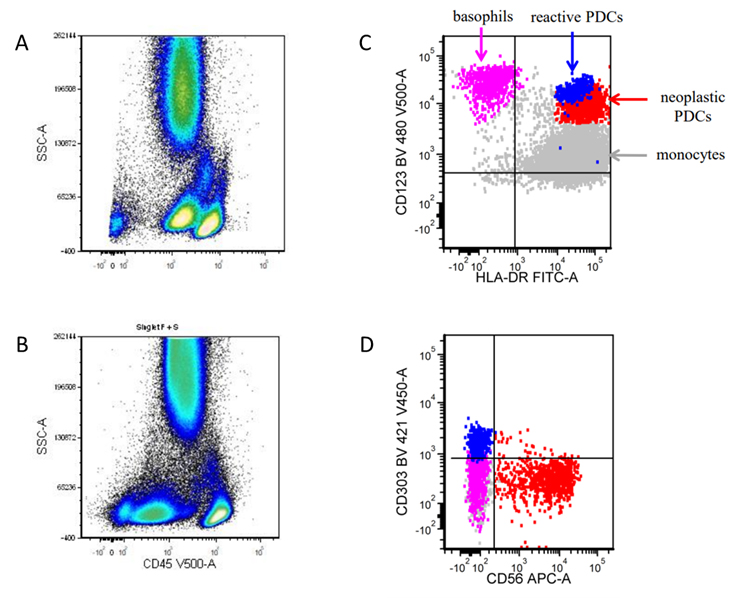
Flow cytometry description
- 3 primary diagnostic aims (Haematologica 2020 Apr 2 [Epub ahead of print]):
- Distinguish between BPDCN and other types of acute leukemia, mainly AML
- Detect mature pDC proliferations in the context of other myeloid neoplasms, primarily chronic myelomonocytic leukemia
- Detection of measurable / minimal residual disease (MRD)
- Neoplastic cells fall into the blast gate on CD45 / SSC
- Detection of MRD requires careful distinction between BPDCN cells and nonneoplastic pDCs
Molecular / cytogenetics description
- Complex karyotype is common
- Many adult patients have MDS associated chromosomal abnormalities and gene mutational profile
- Gene rearrangements detected commonly: ETV6, MYC
- Structural chromosomal losses, commonly involving 13q14 (RB1), 9p21.3 (CDKN2A/CDKN2B), 12p13.2-p13.1 (CDKN1B, ETV6), 7p12.2 (IKZF1)
- Mutations detected commonly: TET2, ASXL1, IDH1, IDH2, DNMT3A, EZH2, SF3B1, SRSF2, ZRSR2, FLT3, KIT, KRAS, NRAS
Sample pathology report
- Bone marrow, aspiration, clot and core biopsy:
- Diagnosis: blastic plasmacytoid dendritic cell neoplasm (see comment)
- Comment:
- Immunohistochemistry: positive for TCF4 / CD123 coexpression
- Flow cytometry: large population of neoplastic cells, positive for CD123, CD4, CD56, CD303 (decreased), HLA-DR and TdT; negative for CD3 (surface and cytoplasmic), CD19 and myeloperoxidase
- Karyotype: 48, XY, t(6;8)(p12;q24.2), add(7)(p11.2), del(13)(q12q22), +16, add(20)(q11.2), +21[10]/46, XY[10]
- Mutation profile: ASXL1, TET2, NRAS
Differential diagnosis
- Acute myeloid leukemia / myeloid sarcoma:
- Mature plasmacytoid dendritic cell proliferation:
- B lymphoblastic lymphoma:
- T lymphoblastic lymphoma:
- Neuroendocrine tumor (including Merkel cell carcinoma):
- Chromogranin+, synaptophysin+, cytokeratin 20+, TCF4 / CD123- dual color
Board review style question #1
Which of the following immunophenotypic markers is typically negative in blastic plasmacytoid dendritic cell neoplasm?
- CD56
- CD123
- CD3
- CD4
- CD45
Board review style answer #1
C. CD3. All others are typically positive in BPDCN but can also be positive in other neoplasms including acute myeloid leukemia.
Comment Here
Reference: Blastic plasmacytoid dendritic cell neoplasm
Comment Here
Reference: Blastic plasmacytoid dendritic cell neoplasm
Board review style question #2
Which of the following dual stains are specific and sensitive for differentiating blastic plasmacytoid dendritic cell neoplasm from acute leukemia, both of which may show overlapping features?
- CD56 and CD4
- CD123 and TCF4
- CD123 and CD19
- TCF4 and MPO
- TCL1 and CD3
Board review style answer #2
B. CD123 and TCF4. Highly sensitive and specific tool for differentiating blastic plasmacytoid dendritic cell neoplasm from acute leukemia.
Comment Here
Reference: Blastic plasmacytoid dendritic cell neoplasm
Comment Here
Reference: Blastic plasmacytoid dendritic cell neoplasm