Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Peripheral smear description | Peripheral smear images | Positive stains | Negative stains | Flow cytometry description | Flow cytometry images | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Aqil B. with iAMP21. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/bonemarrowneoiAMP21.html. Accessed April 2nd, 2025.
Definition / general
- B lymphoblastic leukemia / lymphoma (B ALL / LBL) with intrachromosomal amplification of RUNX1 gene at structurally abnormal chromosome 21 (iAMP21)
Essential features
- B ALL / LBL with iAMP21 is characterized by amplification, which is defined as ≥ 5 copies of RUNX1 per cell and ≥ 3 copies of RUNX1 on a single abnormal chromosome 21 detected by fluorescence in situ hybridization (FISH) study
- Typically occurs in older children with a median age of 9 years
- Pediatric iAMP21 B ALL has a poor outcome with an increased rate of relapse when treated on standard treatment protocols (Hematol Rep 2019;11:7826)
Terminology
- B ALL / LBL with iAMP21
ICD coding
- ICD-O: 9811/3 - B lymphoblastic leukemia / lymphoma with iAMP21
- ICD-11: 2A70.Y & XH0KD4 - other B lymphoblastic leukemia / lymphoma with recurrent genetic abnormalities & B lymphoblastic leukemia / lymphoma with iAMP21
Epidemiology
- Seen in older children with a median age of 9 years (Cancer Genet 2020:243:52)
- 2% of childhood B ALL / LBL and is rarely seen in adults (J Clin Oncol 2013;31:3397, Nature 2014;508:98)
Sites
- Peripheral blood and bone marrow are involved
Pathophysiology
- iAMP21 is considered to be formed through breakage fusion bridge cycles followed by chromothripsis and other complex structural rearrangements of chromosome 21 (Blood 2015;125:1383)
- Genetic studies demonstrated a common 5.1 Mb region that included RUNX1, which is part of the critical region consistently amplified (chr21:32.8 to 37.9 Mb, GRCh37/hg19) (Blood 2011;117:6848)
- Although RUNX1 is present in the amplified region, there is no conclusive evidence which points towards RUNX1 as a critical event in the pathogenesis of the disease given that it is not overexpressed (J Clin Oncol 2012;30:1663, Blood 2011;117:6848)
Etiology
- Higher risk of B ALL / LBL with iAMP21 occurrence is reported in patients with a constitutional Robertsonian translocation rob(15;21)(q10;q10) and presence of a constitutional ring chromosome 21, r(21)c (Eur J Med Genet 2016;59:162, Nature 2014;508:98)
Clinical features
- Presents with leukopenia and thrombocytopenia (Cancer Genet 2020:243:52)
Diagnosis
- Presence of blasts of B cell lineage differentiation
- FISH studies show ≥ 5 copies of RUNX1 per cell with ≥ 3 copies on a single abnormal chromosome 21
Laboratory
- CBC frequently shows leukopenia or thrombocytopenia
Prognostic factors
- Risk stratification includes older age at the time of diagnosis, initial white blood cell (WBC) count, associated genetic aberrations and minimal residual disease (MRD) (Hematol Rep 2019;11:7826, J Clin Oncol 2013;31:3397)
- Older age (≥ 10 years), WBC count (< 50 K/uL), female sex and detectable MRD at day 29 are considered as poor prognostic factors (J Clin Oncol 2013;31:3397)
- Deletion of SH2B3 is enriched in iAMP21 cases and confers a higher risk of relapse or death (Cancer Genet 2018:226:30, Leukemia 2019;33:1881)
- Pediatric iAMP21 B ALL has a poor outcome with an increased rate of relapse when treated on standard protocols (Hematol Rep 2019;11:7826)
- 4 year event free survival (EFS) and overall survival (OS) have been described as significantly worse for patients with iAMP21 with standard risk B ALL (SR BALL) (J Clin Oncol 2013;31:3397)
Case reports
- 4 year old girl with Down syndrome who developed B ALL with iAMP21 due to a constitutional isodicentric chromosome 21 (Am J Med Genet A 2022;188:2325)
- 9 year old girl with B ALL with iAMP21 development with constitutional ring chromosome 21, r(21)c (Cytogenet Genome Res 2022;162:231)
- 12 year old girl with homozygous deletion of the SH2B3 gene, chromothripsis of chromosome 21 and a non-Robertsonian somatic t(15;21)(q25.3;q22.1) with NTRK3 gene rearrangement in iAMP21 B ALL (Cancer Genet 2022:262:16)
Treatment
- Intensive treatment has overcome the higher risk of relapse on standard treatment in these patients, so they are now treated on HR COG ALL protocols (J Clin Oncol 2013;31:3389, J Clin Oncol 2013;31:3397)
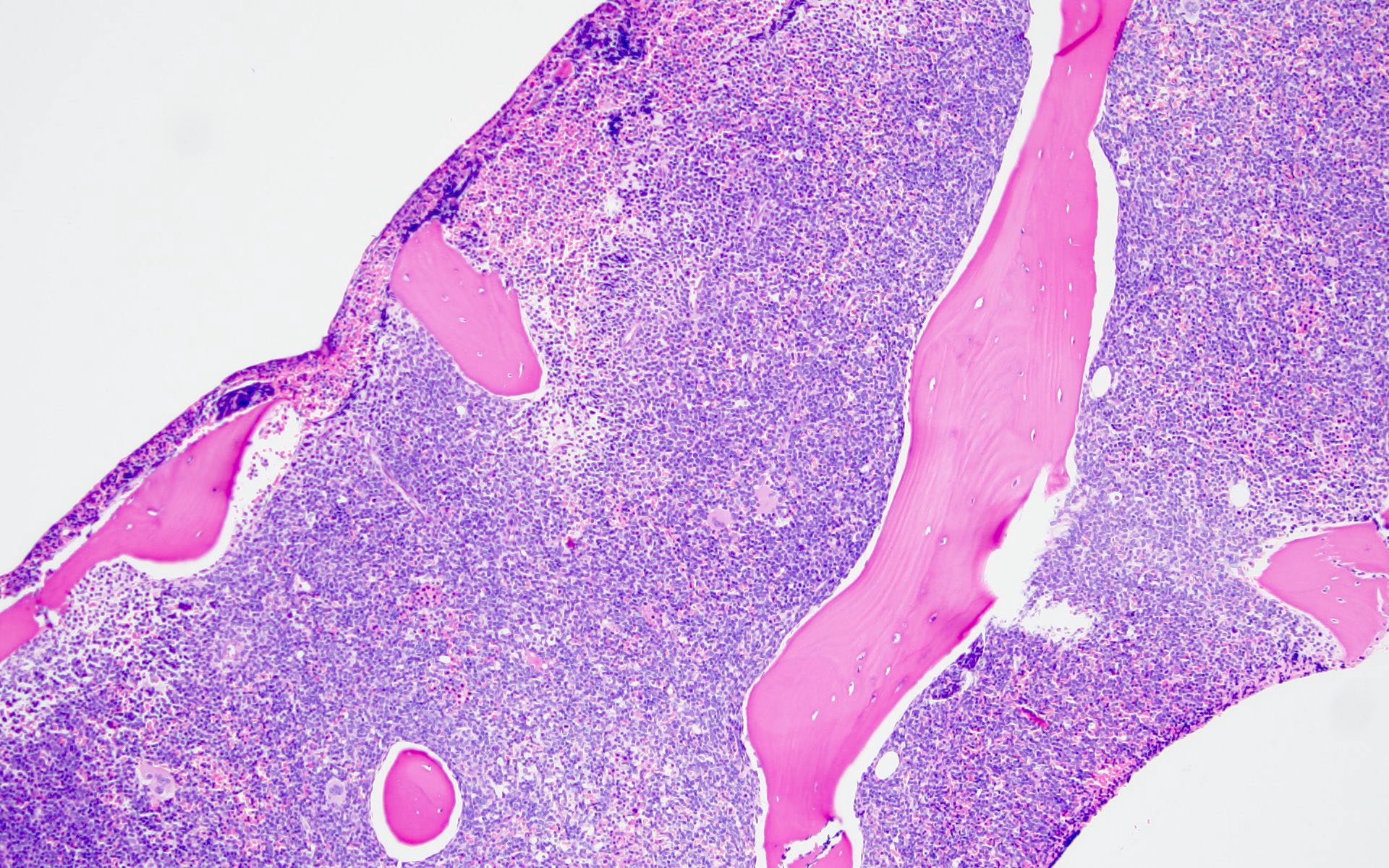
Microscopic (histologic) description
- Bone marrow core biopsy is usually hypercellular with extensive marrow replacement by sheets of atypical medium sized blasts, with round to oval nuclear contour, fine chromatin and pinpoint nucleoli
- Lymph nodes show a diffuse or less commonly paracortical blast infiltrate with increased mitotic figures / apoptotic bodies and sometimes interspersed macrophages (starry sky pattern)
Microscopic (histologic) images
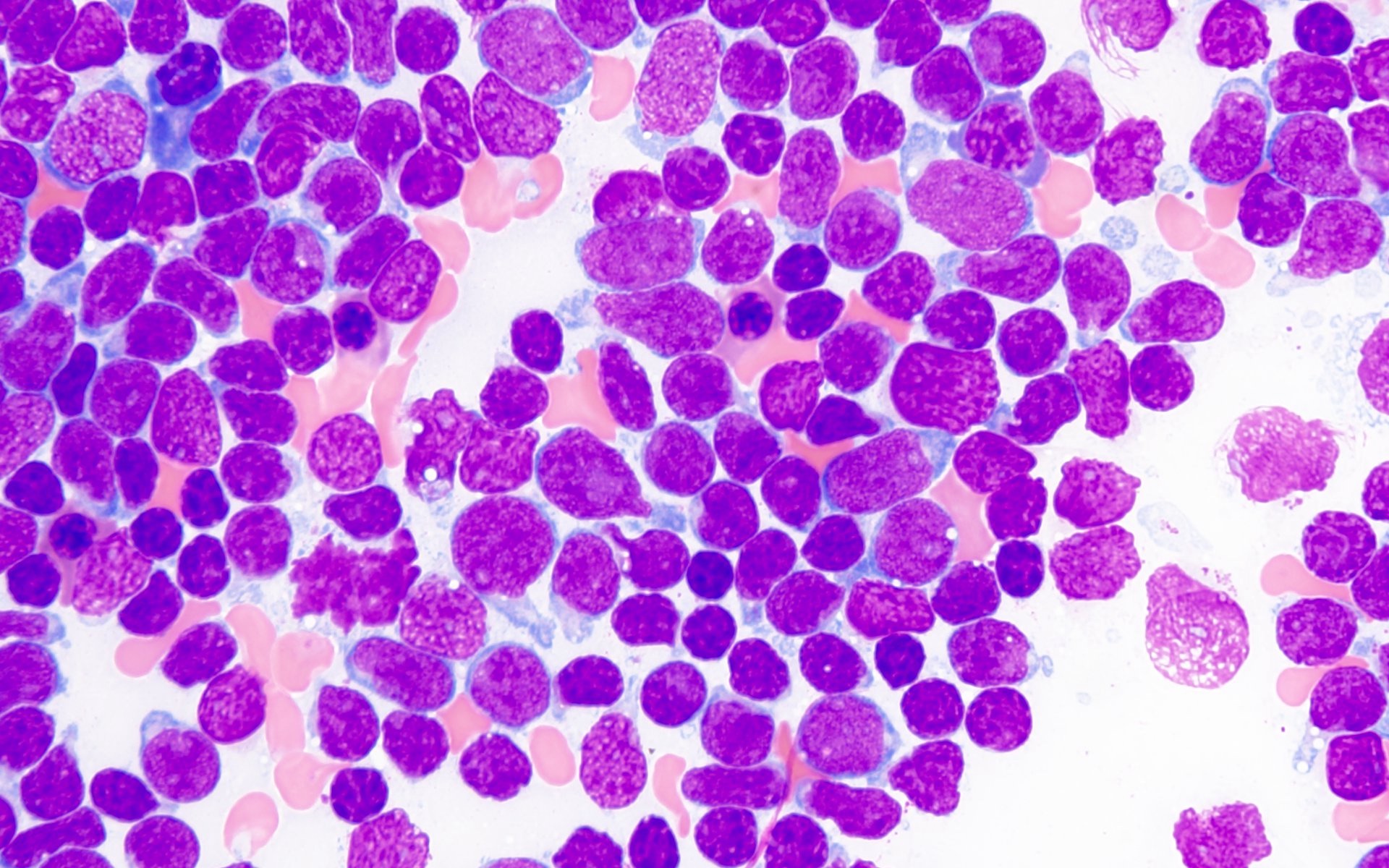
Cytology description
- Aspirate smears and touch preparations show small to medium sized blasts with high N:C ratio, fine nuclear chromatin and prominent nucleoli
- Some of the blasts show cytoplasmic vacuoles and rarely cytoplasmic granules
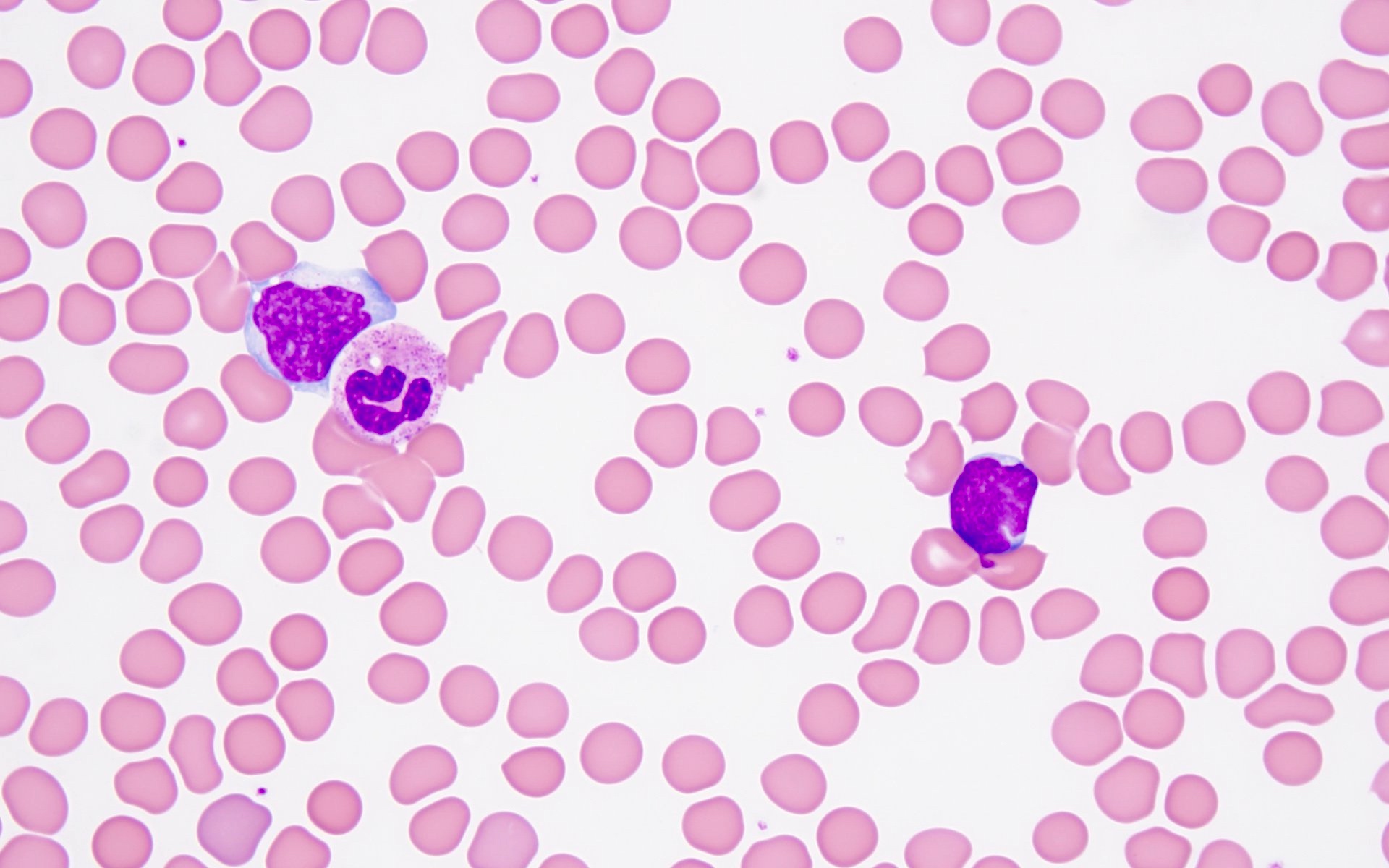
Peripheral smear description
- Circulating blasts are seen, which are small to medium sized cells with high N:C ratio, fine nuclear chromatin and prominent nucleoli
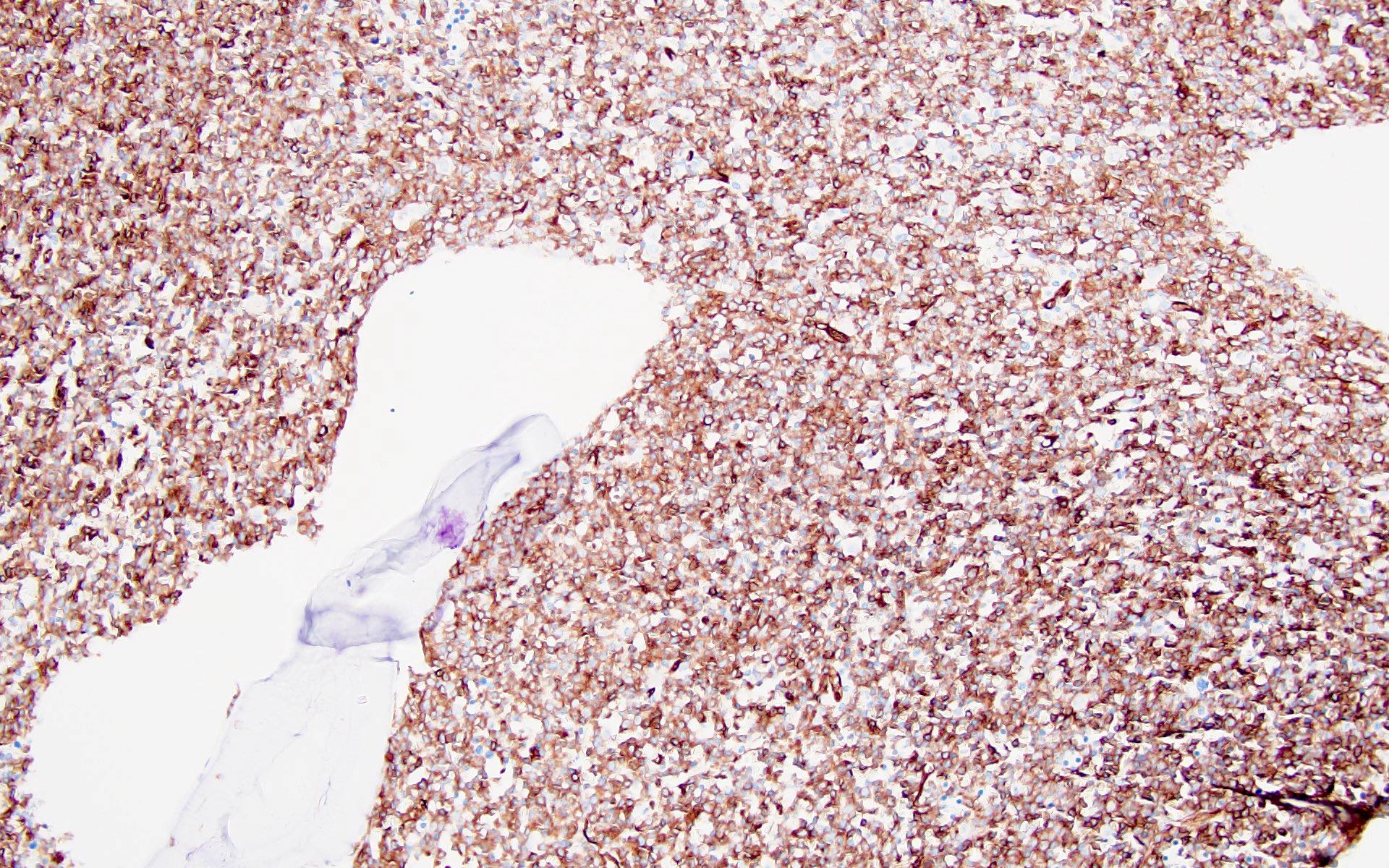
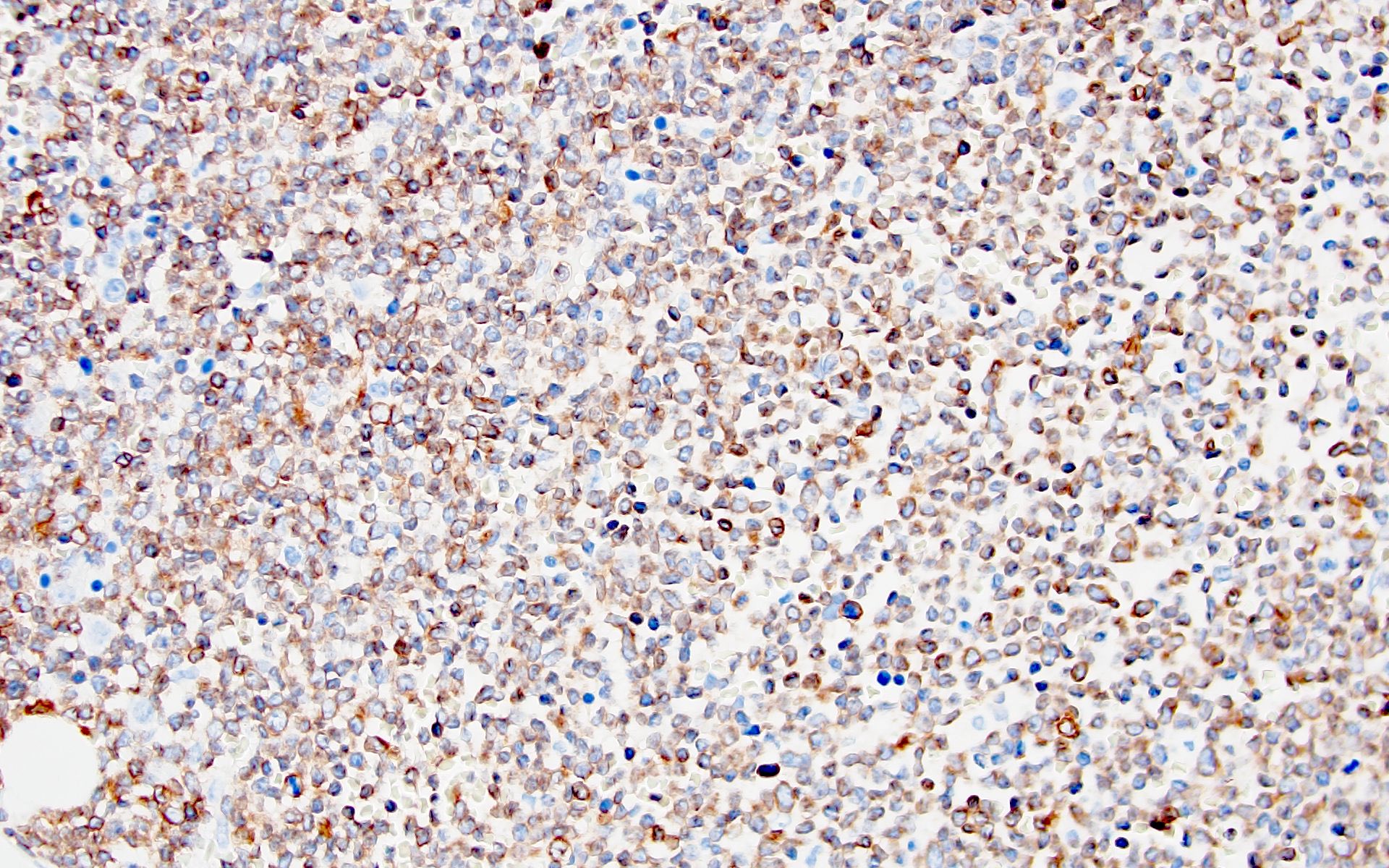
Positive stains
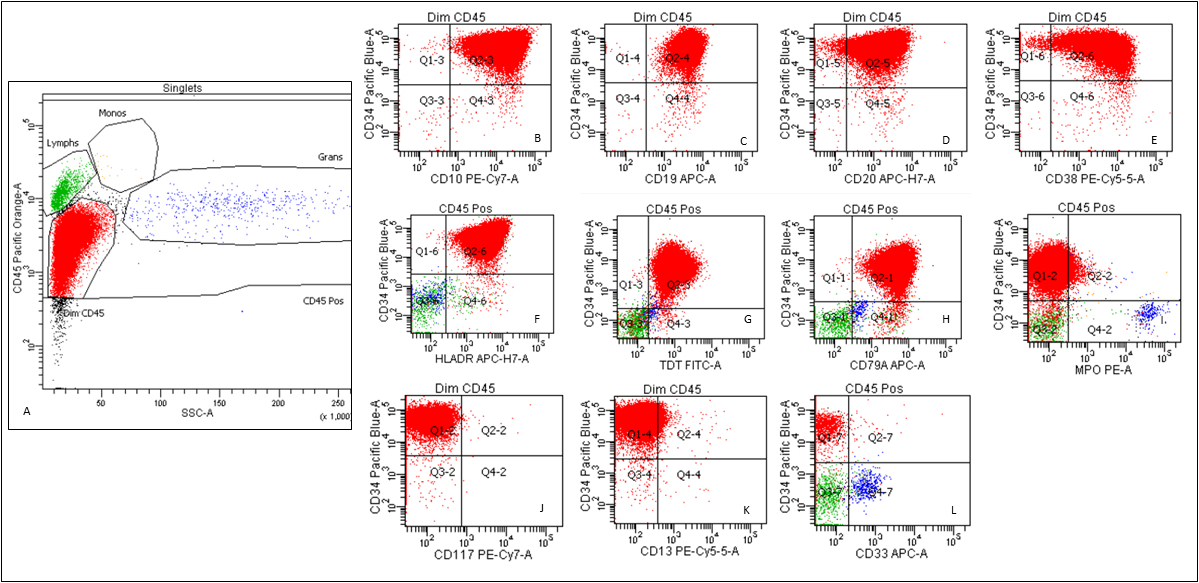
- B cell lineage associated antigens CD19, cCD79a and CD22 (cytoplasmic and surface) by flow cytometry
- PAX5, by immunohistochemistry
- Variable CD10 and CD20
- TdT and CD34
- CD38, CD45 (dim) and HLA-DR
- Nonspecific esterase may show multifocal punctate or Golgi staining (inhibited by sodium fluoride)
- Periodic acid-Schiff (PAS) shows coarse chunky cytoplasmic staining
Negative stains
- Myeloperoxidase
- CD3 (surface and cytoplasmic)
Flow cytometry description
- See Positive stains
Molecular / cytogenetics description
- FISH ETV6::RUNX1 fusion probe set is most commonly used to identify iAMP21
- Conventional chromosome analysis further identifies the abnormalities of chromosome 21 along with additional chromosomal aberrations (Blood 2015;125:1383)
- Chromosomal microarray (CMA) or next generation sequencing (NGS) based copy number analysis are being utilized for the identification of iAMP21 (Blood 2015;125:1383)
- Secondary genomic abnormalities that have been reported include gain of chromosomes X, 10 and 14, loss of chromosomes 7/7q and 11q (including KMT2A) and deletions involving IKZF1, CDKN2A/B, PAX5, SH2B3, ETV6 and RB1 as well as rearrangements of P2RY8::CRLF2, ETV6:RUNX1 and BCR::ABL1 (Blood 2011;117:2129, Blood 2011;117:6848, Cancer Genet 2018:226:30, Mol Cytogenet 2016:9:84, Leukemia 2019;33:1881, Leukemia 2014;28:1015)
- Given the unique nature and poor prognosis of the B ALL with iAMP21, cases with genomic lesions that may suggest different subcategory of B ALL / LBL classification should still be included as B ALL / LBL with iAMP21 (Semin Hematol 2019;56:90)
- RAS signaling pathway mutations, including NRAS (45%), KRAS (18%), FLT3 (20%), PTPN11 (11%), BRAF (2%) and NF1 (2%), have been frequently described in cases with iAMP21 (Leukemia 2016;30:1824)
Molecular / cytogenetics images
Sample pathology report
- Peripheral blood, bone marrow aspirate and left posterior iliac crest bone marrow core biopsy:
- B lymphoblastic leukemia with iAMP21 involving ~90% of a hypercellular (90% cellular) bone marrow (see comment)
- Comment: The cytogenetic analysis showed complex karyotype including an ider(21) resulting in an amplification of the RUNX1 gene, which was confirmed by the concurrent FISH analysis. FISH study was positive for amplification of RUNX1 (84%).
- Peripheral blood smear: The blood smear shows normocytic anemia with anisopoikilocytosis including ovalocytes, teardrop forms and rare schistocytes. Rare blasts are present, which are small to intermediate sized cells with round to cleaved nuclei, open chromatin, occasional small nucleoli and scant cytoplasm. There is absolute neutropenia. Platelets are decreased with unremarkable morphology.
- Bone marrow aspirate: The bone marrow aspirate smear shows sheets of blasts with similar morphologic features as described above. Few scattered megakaryocytes and rare erythroid precursors are seen.
- Bone marrow core biopsy (decalcified): The unilateral bone marrow core biopsy is hypercellular for age (~90% cellular). There is extensive replacement by sheets of atypical medium sized mononuclear cells, with round to irregular nuclear contour, fine chromatin and pinpoint nucleoli. Background hematopoiesis is markedly decreased. Few scattered megakaryocytes are present.
Differential diagnosis
- B lymphoblastic leukemia / lymphoma with BCR::ABL1 fusion:
- B ALL / LBL defined by BCR::ABL1 fusion due to rearrangement between the BCR gene on chromosome 22q.11.2 and the ABL1 oncogene on chromosome 9q34.1
- Blasts frequently express myeloid markers, such as CD13, CD33 and CD25 (Int J Clin Exp Pathol 2014;7:6225)
- Poor prognosis (Blood 2008;111:1827)
- B lymphoblastic leukemia / lymphoma with KMT2A rearrangement:
Board review style question #1
Board review style answer #1
D. t(15;21). Robertsonian translocation between chromosomes 15 and 21, rob(15;21)(q10;q10)c, have a > 2,700 fold increased risk of developing iAMP21 ALL.
Answers A and B are incorrect because they are different subcategories of B ALL, which are classified based on t(9;11) / KMT2A rearrangement and t(9;22) / BCR:ABL1 fusion.
Answer C is incorrect because it is seen in acute promyelocytic leukemia, which is associated with t(15;17) / PML::RARA fusion.
Comment Here
Reference: with iAMP21
Comment Here
Reference: with iAMP21
Board review style question #2
Which FISH probe set is utilized for diagnosing AML with iAMP21?
- 5' CRLF2 and 3' CRLF2 (Xp22.3 and Yp11.3), break apart
- 5' PDGFRB and 3' PDGFRB, break apart (5q33)
- ABL1 (9q34) and BCR (22q11.2), fusion
- ETV6 (12p13.2) and RUNX1 (21q22.3)
Board review style answer #2
D. ETV6 (12p13.2) and RUNX1 (21q22.3) shows amplification of RUNX1.
Answer A is incorrect because CRLF2 break apart probe is used to identify BCR::ABL1-like B ALL.
Answer C is incorrect because it is used to identify B ALL, BCR::ABL1 positive cases.
Answer B is incorrect because PDGFRB rearrangement positivity helps to identify myeloid / lymphoid neoplasm with PDGFRB rearrangement.
Comment Here
Reference: with iAMP21
Comment Here
Reference: with iAMP21