Table of Contents
Definition / general | Complications | Microscopic (histologic) description | Microscopic (histologic) imagesCite this page: Pernick N. Bone marrow transplantation. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/bonemarrowbmt.html. Accessed April 2nd, 2025.
Definition / general
- Indications:
- Aplastic anemia, osteopetrosis or other primary / congenital bone marrow disease
- Post high dose chemotherapy for malignancy
- Posttransplant if blood counts do not recover as expected
- Autologous transplantation:
- Graft is patient's own marrow, often after monoclonal antibodies to tumor or cell sorting regimen
- Allogeneic transplantation:
- Graft is from another individual after recipient myeloablative preparatory regimen of high dose chemotherapy, total body radiation or monoclonal antibodies
- Nonmyeloablative allogeneic stem cell transplantation:
- In elderly or those with relatively indolent disease
- Myeloablative steps are reduced or eliminated as curative potential is largely due to graft versus tumor effect
- Similar outcome as traditional approach in patients > age 50 years (Blood 2005;105:1810)
- Examination of bone marrow morphology recommended posttransplant in additional to traditional molecular studies (Arch Pathol Lab Med 2006;130:1479)
- Peripheral blood transplant:
- Uses CD34+ stem cells
- Preparation:
- Chemotherapy, total body irradiation to:
- Immunosuppress patient to prevent rejection
- Eradicate tumor cells (antitumor antibodies also used for this purpose)
- Chemotherapy, total body irradiation to:
Complications
- Infection, graft rejection, graft versus host disease, recurrence of malignancy
- Infection:
- Due to immunosuppression
- Less common due to antibiotics, growth factors
- Graft rejection:
- Rare with matched siblings
- Common with unrelated donors
- Characterized by decreasing marrow cellularity and progressive cytopenia
- Decrease in a myeloid cell line may predict impending rejection or be due to drugs or viruses
- Erythroid hypoplasia may be due to parvovirus B19 infection in immunocompromised patients
- Dyserythropoiesis and dysgranulopoiesis may reflect toxic effect of immunosuppressive drugs or antibiotics
- Maturation arrest of granulocytes may occur due to various drugs
- Granulocyte growth factors cause hyperplasia of immature forms and leukemoid peripheral blood reaction with Döhle bodies, abnormally segmented neutrophils and atypical granulation
- Graft versus host disease:
- Associated with increased lymphocytes, plasma cells and eosinophils
Microscopic (histologic) description
- Successful engraftment:
- 0 - 1 week:
- Usually not biopsied
- Marked hypocellularity, hemorrhage, proteinaceous debris, scattered fat cells and macrophages
- 1 - 2 weeks:
- Adipose tissue present
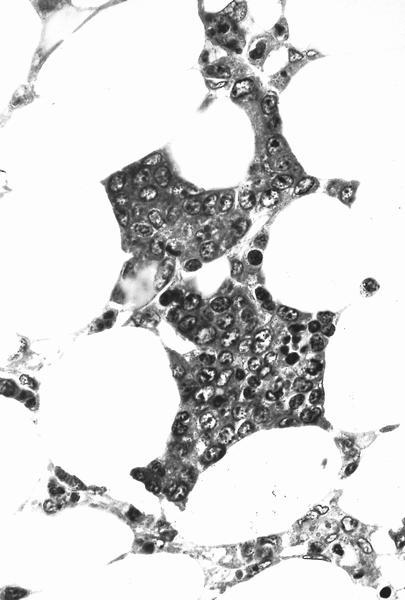
- 2 - 3 weeks:
- Scattered islands of hematopoietic cells
- Often erythroid precursors initially, then promyelocytes and myelocytes
- 5 - 10 weeks:
- Increasing erythroid precursors, granulocytes and megakaryocytes
- Megakaryocyte reconstitution may lag behind other cell lines
- 0 - 1 week: