Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Alkashash A, Warmke L. Fracture. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/bonefracture.html. Accessed March 31st, 2025.
Definition / general
- Fracture is a partial or complete break in bone
Essential features
- Fracture is a break in bone
- There are many types of fracture, including complete, incomplete, open, closed, comminuted and avulsion, among others
- Fracture healing occurs in multiple stages including hematoma formation, inflammation, soft callus formation, hard callus formation and remodeling
Terminology
- Complete fracture occurs when the bone is broken into separate pieces
- Open (or compound) fracture occurs when the bone breaks through the skin
- Closed (or simple) fracture occurs when the bone is broken but the skin remains intact
- Other descriptions or types of fracture include
- Displaced (ends of bone are not aligned)
- Greenstick (incomplete fracture where a portion of bone is broken, causing the other side to bend)
- Transverse (break in a straight line across the bone), commonly associated with Paget disease and osteopetrosis
- Spiral (break spirals around bone, common in twisting injury)
- Oblique (break is diagonal across bone)
- Compression (bone is crushed)
- Comminuted (bone broken in 3 or more places with many fragments present)
- Segmental (bone broken in 2 places with floating piece of bone)
- Avulsion (fragment of bone breaks where ligament or tendon inserts)
ICD coding
- ICD-10: M84.40XA - pathological fracture, unspecified site, initial encounter for fracture
Epidemiology
- Osgood-Schlatter disease is an enthesopathy, which rarely results in an avulsion fracture at the tibial tubercle, that occurs in young children (age: 10 - 15 years) and represents the most common cause of knee pain in adolescents
- Stress fractures involving the tibial shaft are common in long distance runners and ballet dancers, while those involving the second or third metatarsal bones often occur in military trainees
- Osteogenesis imperfecta is a rare condition that predisposes bone to fracture
- Women over the age of 50 with low bone mineral density are at increased risk for fracture (Injury 2006;37:691, Lancet Healthy Longev 2021;2:e580, Osteoporos Int 2005:16:S3)
- Weight bearing exercise and a diet rich in calcium and vitamin D is protective and promotes bone health
- Risk factors in female athletes include body mass index (BMI) < 19, late menarche (≥ 15 years) and participation in lean sports (Med Sci Sports Exerc 2013;45:1843)
Sites
- Common fracture sites in children include the distal radius, supracondylar elbow and clavicle
- Fractures involving the epiphyseal plate or physis represent between 15% and 18% of all pediatric fractures (Clin Orthop Relat Res 2016;474:2531)
- Physeal fractures are classified using the Salter-Harris classification system (types I - V) based on the fracture pattern through the growth plate
- Certain fracture types may raise concern for potential child abuse, including multiple fractures at different healing stages, femur fractures in nonwalking children, bucket handle fractures and fractures affecting the skull, ribs, scapula and ulna (Dtsch Arztebl Int 2018;115:769, BMJ 2008:337:a1518)
- Avulsion fractures most commonly occur around the pelvis, particularly at the origin of the adductor muscles along the inferior pubic ramus and lower thigh where the adductor inserts
Pathophysiology
- Fracture leads to disruption of blood vessels which causes hemorrhage
- Hematoma forms between 2 ends of bone, creating a fibrin mesh that seals the site
- Portions of bone and soft tissue with disrupted blood supply undergo necrosis
- Stage 1: inflammation
- Tissue damage activates wound healing pathways
- Growth factors and cytokines (e.g., TGFβ, PDGF, FGF2, VEGF, M-CSF, IL1, IL6, BMPs, TNFα) are released, leading to clot / thrombus formation, inflammatory cell recruitment, mesenchymal stem cell migration, granulation tissue formation and debris removal (Foot Ankle Clin 2016;21:739, Int Wound J 2015;12:238, Clin Exp Pharmacol Physiol 2012;39:706, Semin Cell Dev Biol 2008;19:459)
- Dead bone resorption begins at 3 days
- Stage 2: soft callus formation
- Periosteal pluripotent cells differentiate into chondroblasts
- Chondroblasts and fibroblasts create a semirigid soft callus, offering mechanical support and serving as a template
- Growth factors (e.g., TFG2, TFGβ3, PDGF, FGF1, IGF, BMP2, BMP4, BMP5, BMP6 and VEGF) play a role (Semin Cell Dev Biol 2008;19:459, Foot Ankle Clin 2016;21:739, Int Wound J 2015;12:238, Clin Exp Pharmacol Physiol 2012;39:706)
- Early callus is reminiscent of disorganized fetal cartilage
- Periosteal inner layer promotes intramembranous bone growth
- Stage 3: hard callus formation
- Elevated osteoblastic activity leads to new vessel formation and woven bone formation in the peripheral soft callus
- New bone replaces the soft callus and forms along lines of stress (Semin Cell Dev Biol 2008;19:459, Foot Ankle Clin 2016;21:739, Int Wound J 2015;12:238, Clin Exp Pharmacol Physiol 2012;39:706)
- Stage 4: remodeling
- Involves orderly bone resorption by osteoclasts and lamellar bone formation by osteoblasts (Semin Cell Dev Biol 2008;19:459, Foot Ankle Clin 2016;21:739, Int Wound J 2015;12:238, Clin Exp Pharmacol Physiol 2012;39:706)
- RANK ligand signaling and cytokines play an important role
Etiology
- Usually caused by trauma (e.g., falls, car accidents, sports injuries)
- Most pediatric fractures result from falls during sports and play (Acta Orthop 2010;81:148)
- Torus (or buckle) fracture is an incomplete fracture of the radius, ulna or both, commonly occurring due to a fall in a young child where the wrist absorbs the impact of the fall
- Repetitive forces (e.g., long distance running, marching, ballet dancing) increase the risk of stress fracture
- Pathologic fractures occur when bone is broken through an area weakened by preexisting disease by a degree of stress that would have left normal bone intact (e.g., osseous metastasis, multiple myeloma, osteoporosis)
- Avulsion fractures occur from repeated trauma at sites of ligamentous and tendinous insertions
Diagrams / tables
Clinical features
- Sudden and intense pain (Emerg Radiol 2016;23:365)
- Visible bone deformity
- Inability to move or put weight on limb
- Swelling, bruising and bleeding
Diagnosis
- Complete medical history (including description of injury)
- Bone deformity may be evident on physical examination
- Fracture confirmed on imaging studies (e.g., Xray, computerized tomography [CT], magnetic resonance imaging [MRI])
- Careful correlation of all available clinical, radiologic and pathologic features of each case is essential (Am J Clin Pathol 1969;52:14)
Laboratory
- In setting of delayed union, often check erythrocyte sedimentation rate (ESR), C reactive protein (CRP), vitamin D, calcium, thyroid and parathyroid hormone levels and HbA1c
- In setting of pathologic fracture, often check CBC, BMP, serum protein electrophoresis (SPEP), PSA and other tumor markers (in addition to imaging with CT of chest / abdomen / pelvis)
Radiology description
- Radiographs are first line modality (Emerg Radiol 2016;23:365)
- Plain radiographs can show periosteal thickening, lucency and a discrete fracture line
- CT can be useful in detecting occult fractures
- MRI highlights periosteal edema, bone marrow and intracortical signal abnormality associated with fracture (Emerg Radiol 2016;23:365)
- Radionuclide bone scans can detect stress injuries as soon as 2 - 8 days after symptoms (Radiology 1979;132:431)
- Excessive callus formation with periosteal new bone formation may be mistaken for a bone forming tumor
Radiology images
Prognostic factors
- Fracture takes several weeks to months to heal, depending on the severity and extent of the injury
- Children’s thicker and more metabolically active periosteum accelerates healing and remodeling, requiring earlier treatment (StatPearls: Greenstick Fracture [Accessed 9 November 2023])
- Physeal fractures may cause growth disturbances, limb length differences, angular deformities and occasionally delayed union or nonunion
- Poor nutritional status can impede fracture healing
- Caffeine, alcohol and tobacco negatively impact healing process (Am J Prev Med 2000;18:96)
- Chronic nonunion of fracture site can lead to pseudoarthrosis
- Increased callus formation occurs in unstable areas
- Fractures may not heal due to improper immobilization, devascularization of bone fragments, persistent infection or interposition of soft tissue between ends of bone
Case reports
- 14 year old boy with hyperplastic fracture callus of femur mimicking osteosarcoma (Front Endocrinol (Lausanne) 2021:12:622674)
- 17 year old boy with avulsion fracture of anterior inferior iliac spine mimicking bone tumor (Oman Med J 2014;29:220)
- 63 year old woman with humeral shaft hypertrophic nonunion mimicking malignant lesion (BMJ Case Rep 2013:2013:bcr2013202671)
- 65 year old woman with osteoporosis and insufficiency subchondral fracture (Am J Surg Pathol 2000;24:464)
- 69 year old woman with multiple osteoporotic fractures mimicking metastatic bone disease (Am J Med Sci 2020;360:309)
Treatment
- Splint or cast to immobilize the injured area
- Medication for pain control
- Traction to align the broken bone
- Debridement and lavage of open fracture (Chin J Traumatol 2018;21:187)
- Surgery with internal (metal rods or pins inside the bone) or external (metal rods or pins outside the body) fixation (Radiographics 2003;23:1569)
- Physical therapy to regain strength and mobility
Clinical images
Gross description
- Visibly deformed or misshapen bone or joint
- Exposed bone visible through skin in open fracture (Chin J Traumatol 2018;21:187)
- Associated tumor may be present in pathologic fracture
- Bone enlargement at the fracture site is evident during callus formation
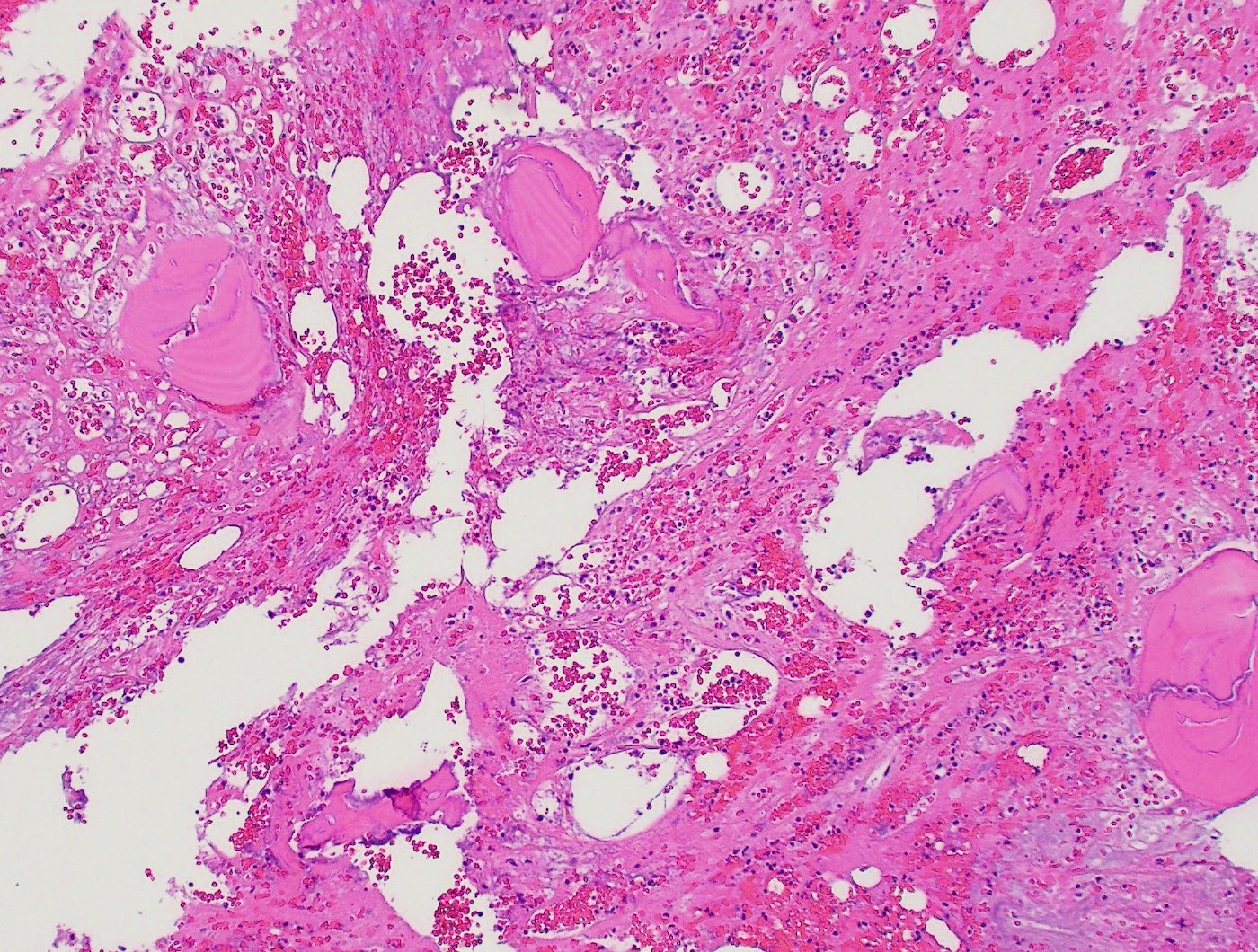
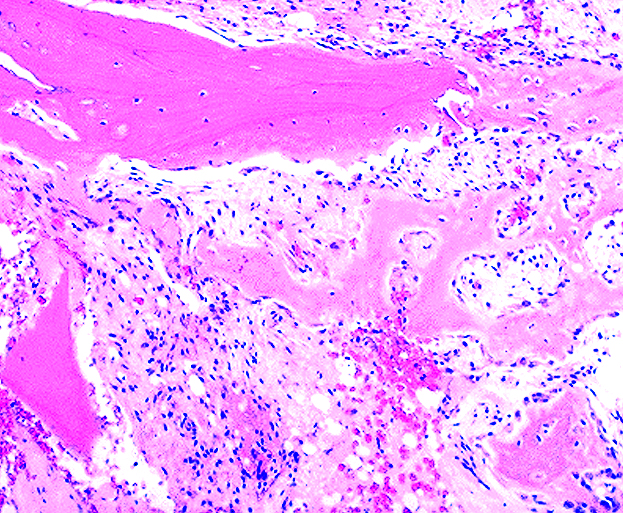
Frozen section description
- Fragments of reactive bone (may be difficult to cut)
- Background of hemorrhage, fibrin and inflammatory cells
- Lack of atypia
- Fracture may impact the reliability of frozen section assessment of periprosthetic joint infection (Hip Int 2022;32:87)
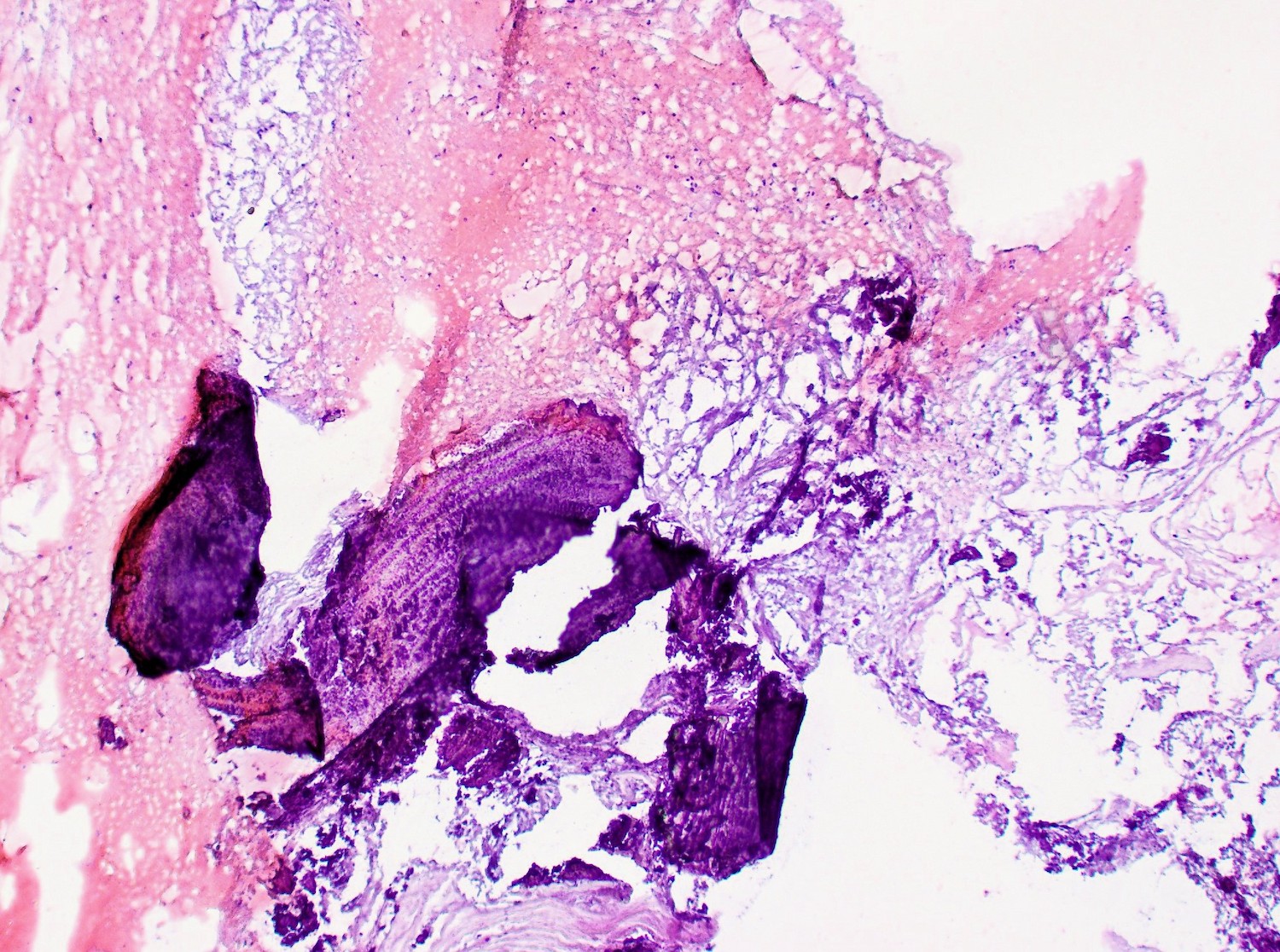
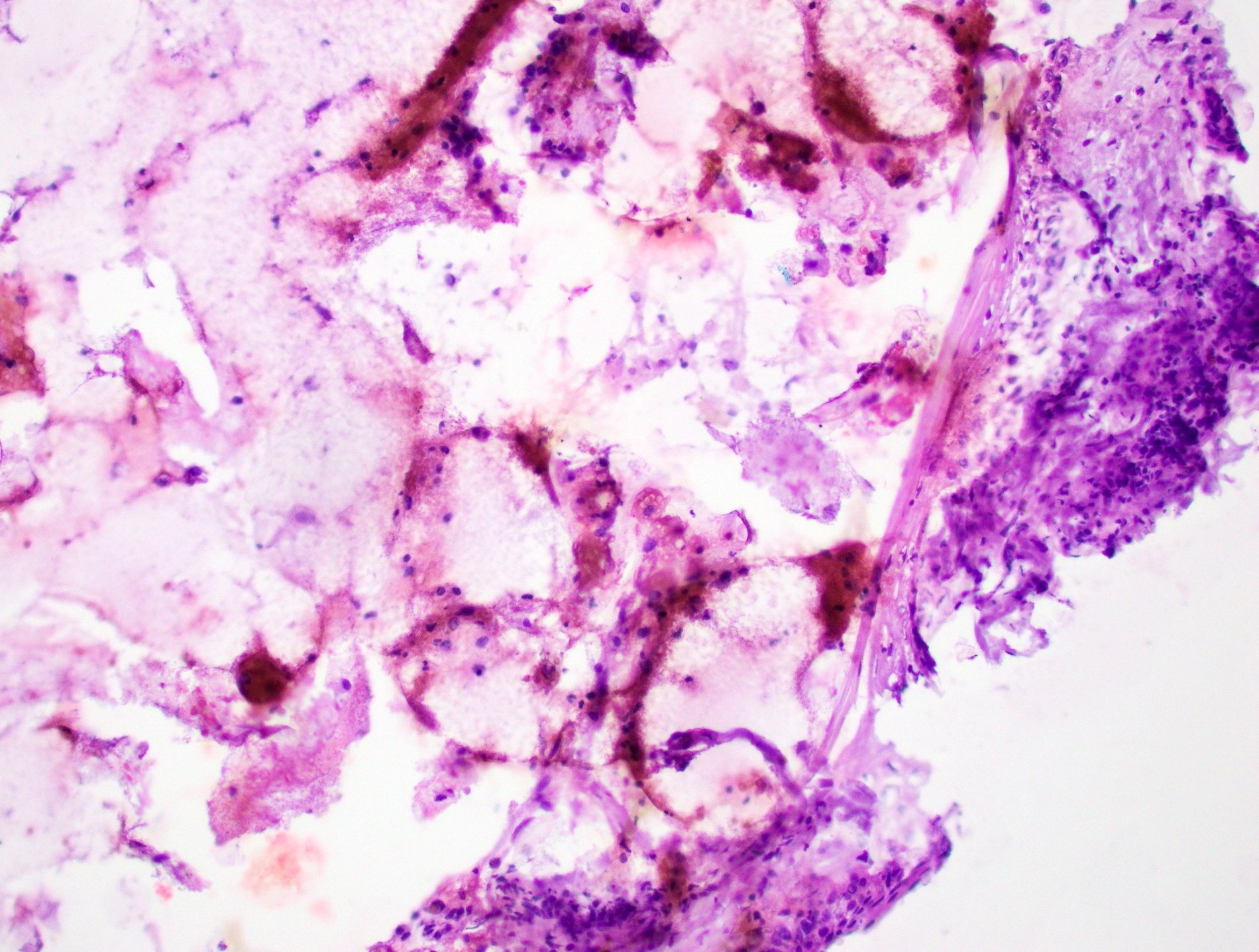
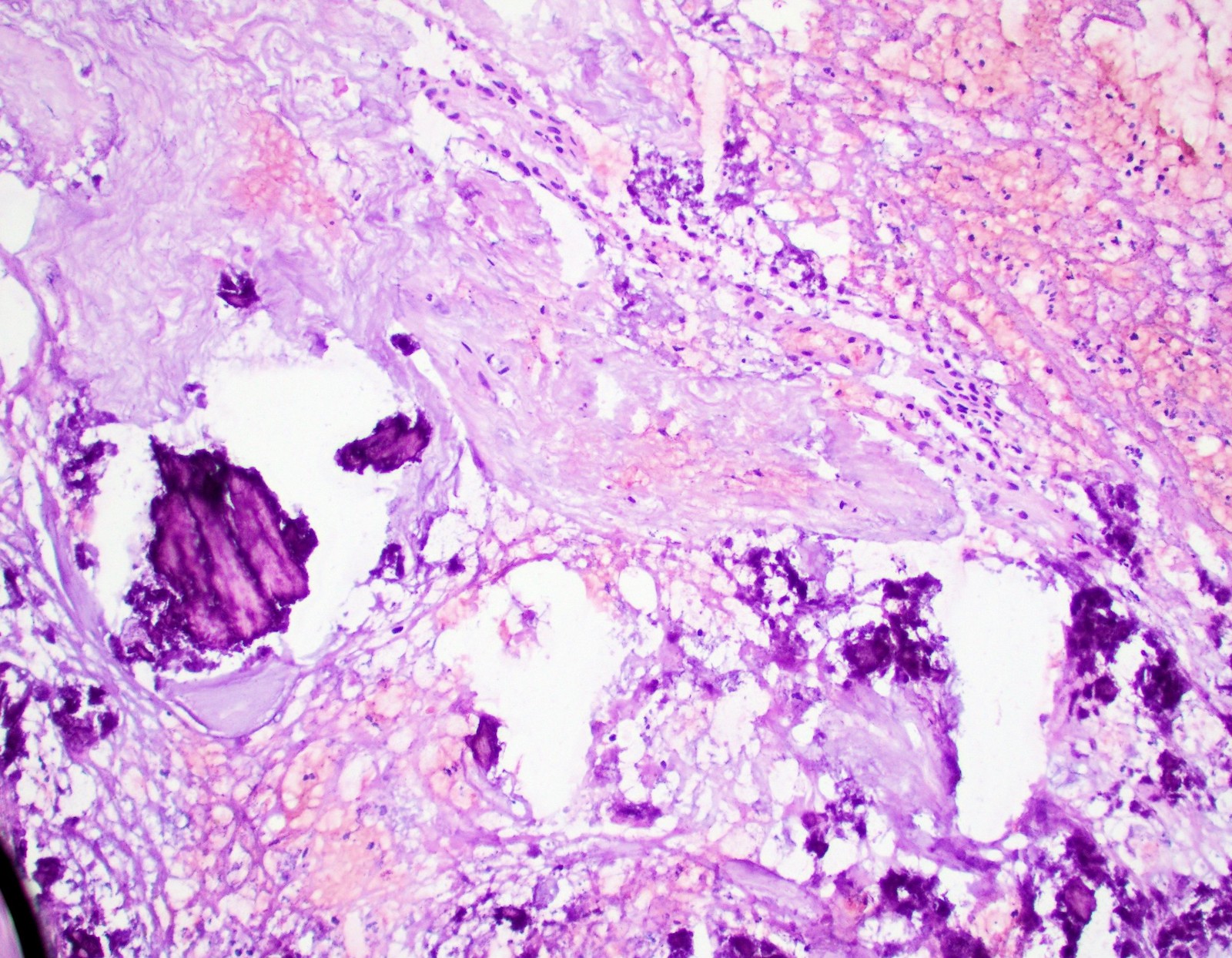
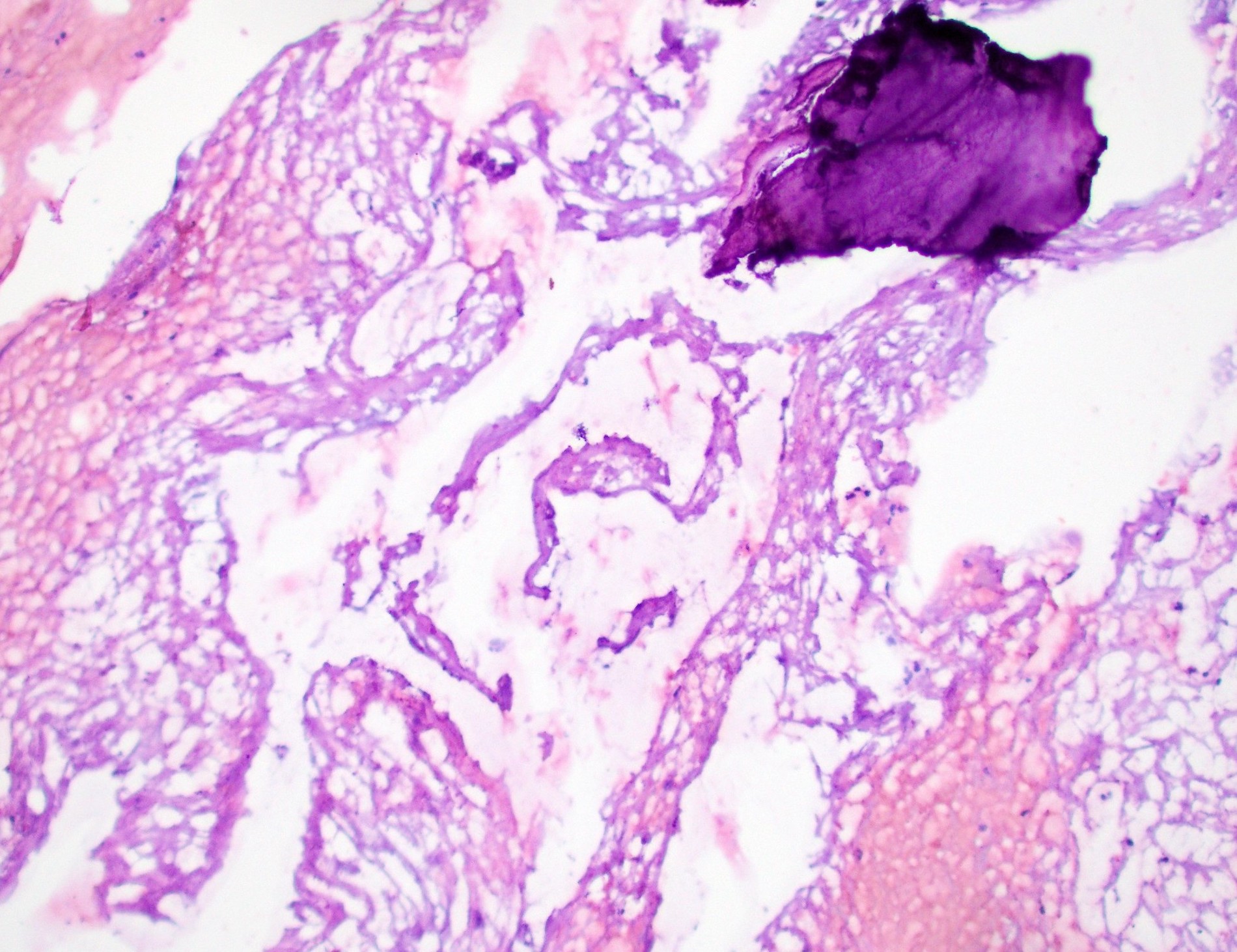
Frozen section images
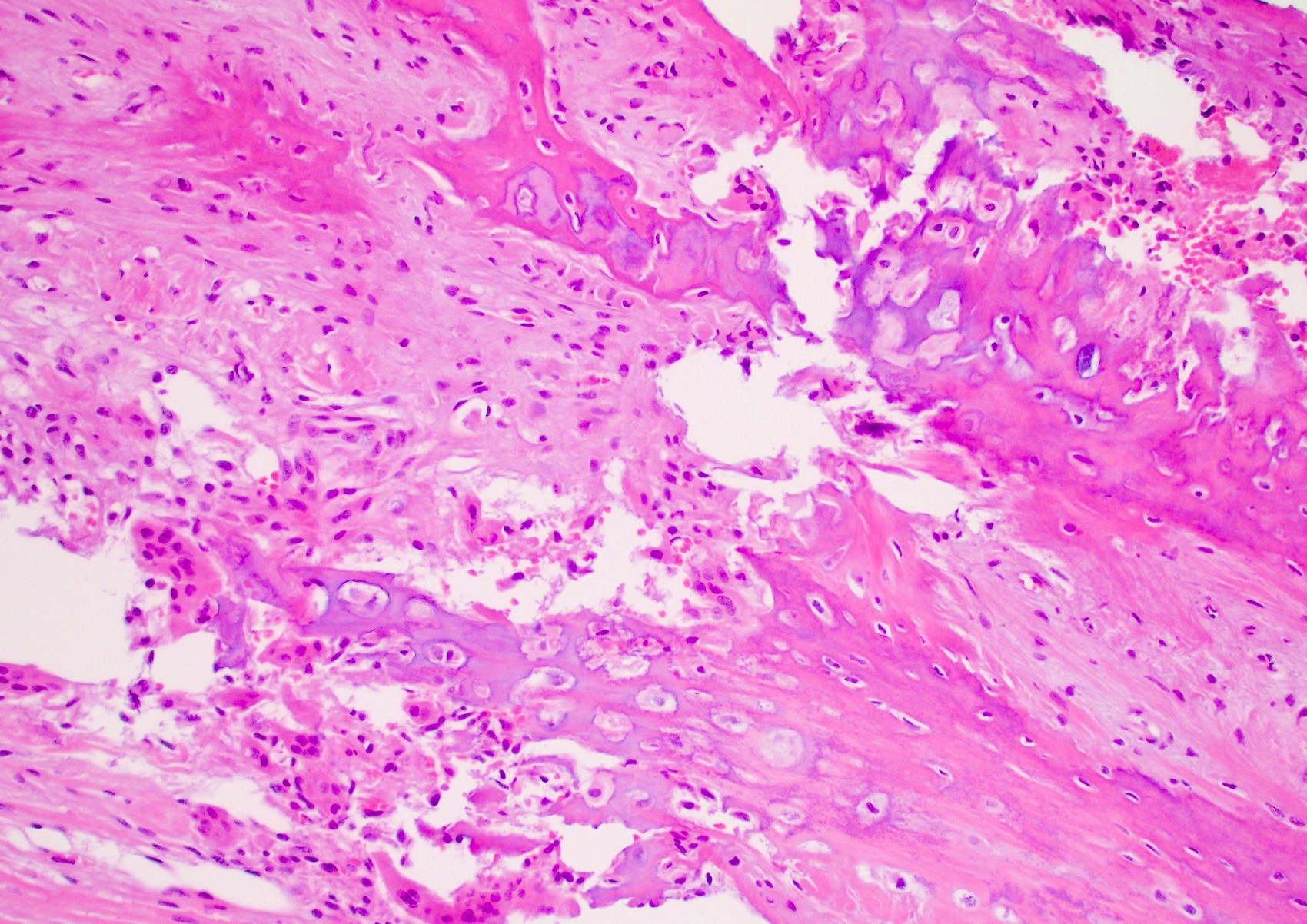
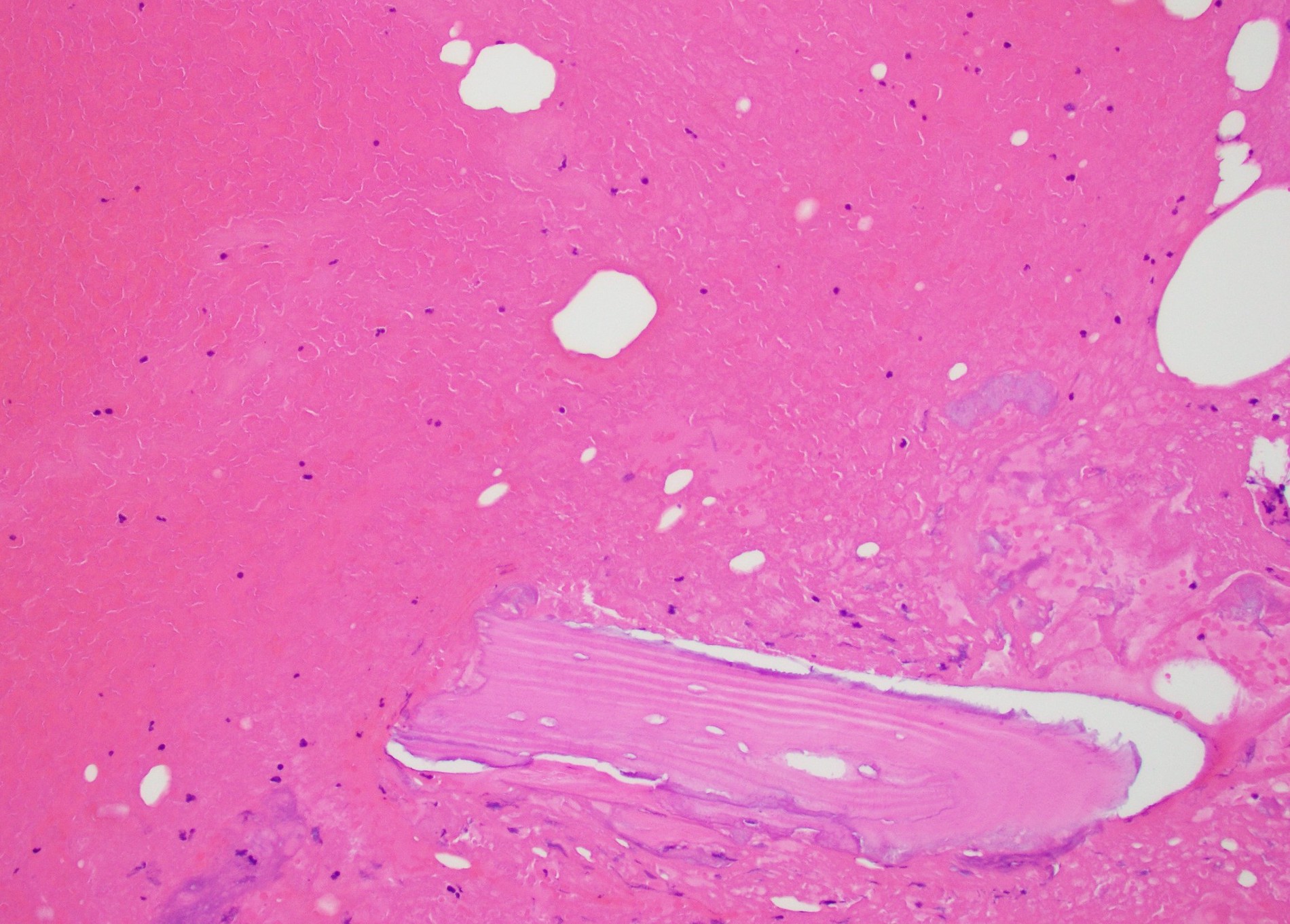
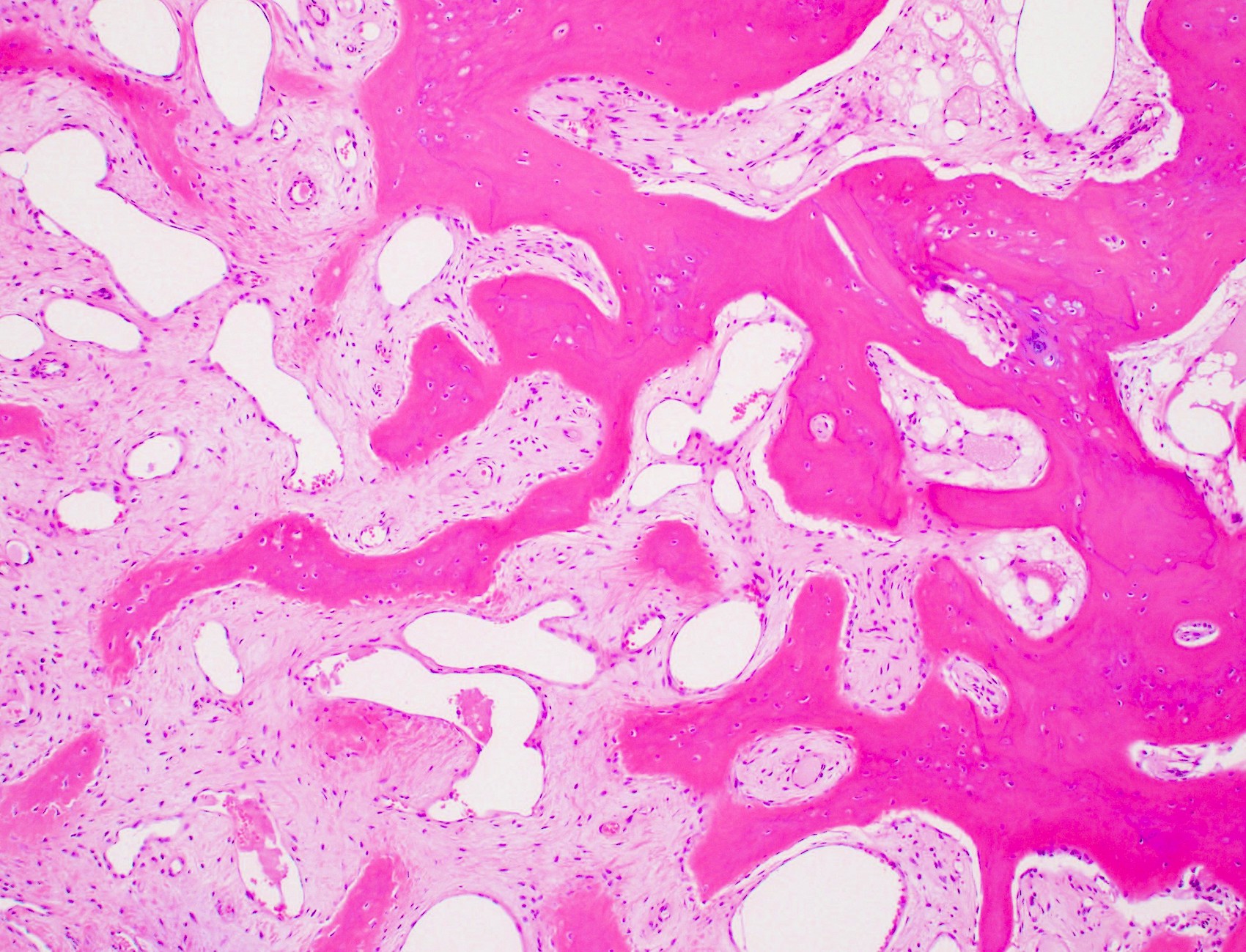
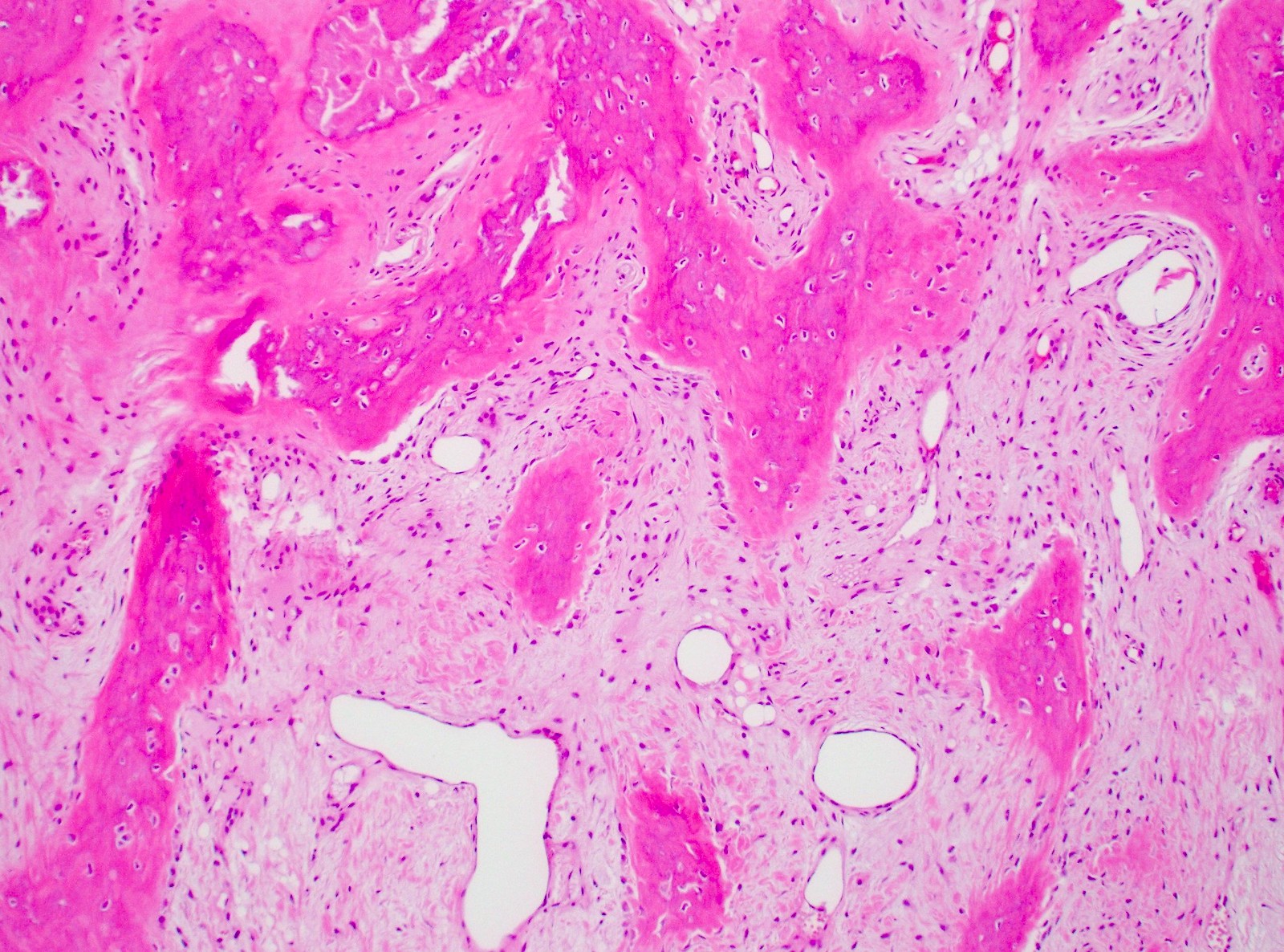
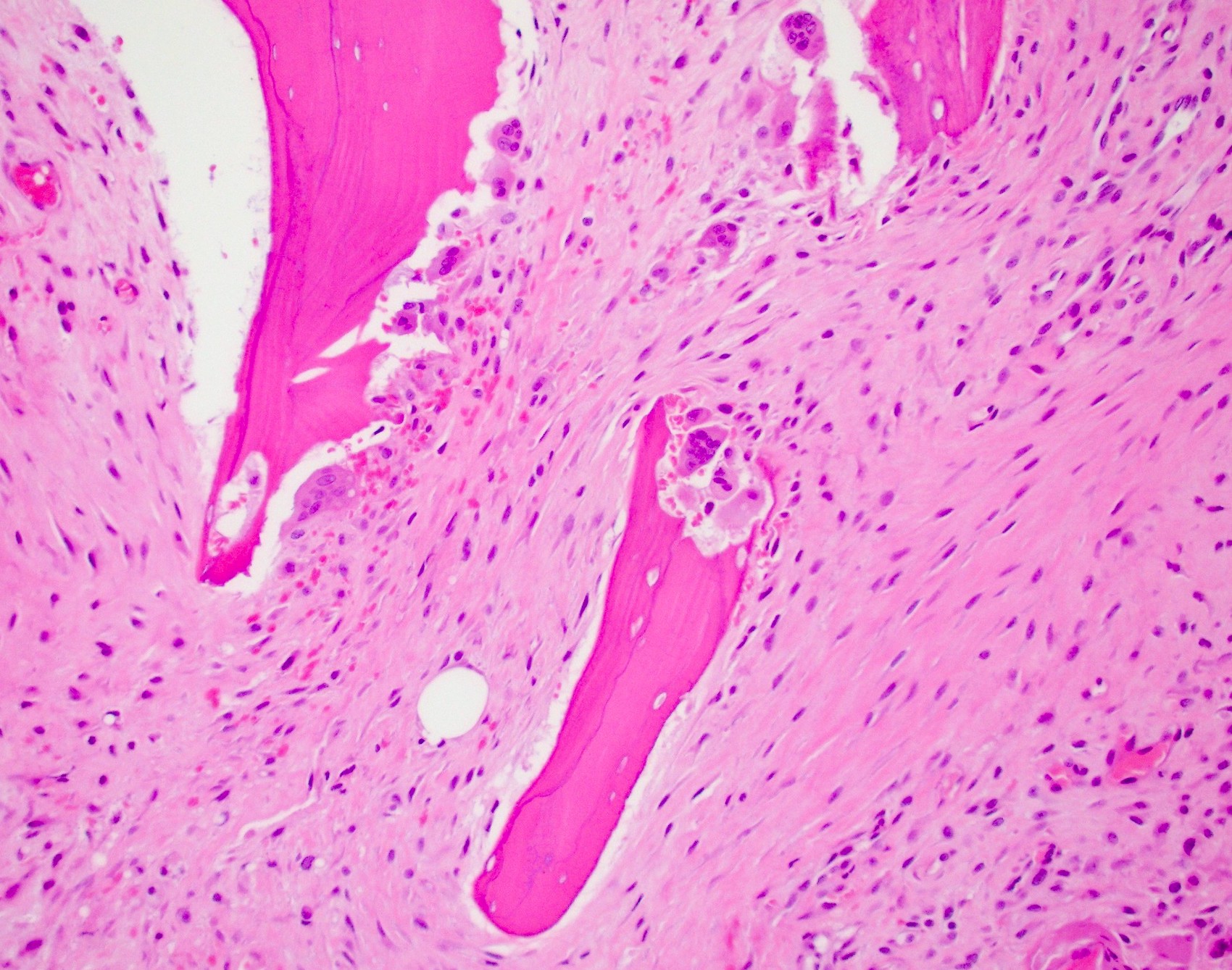
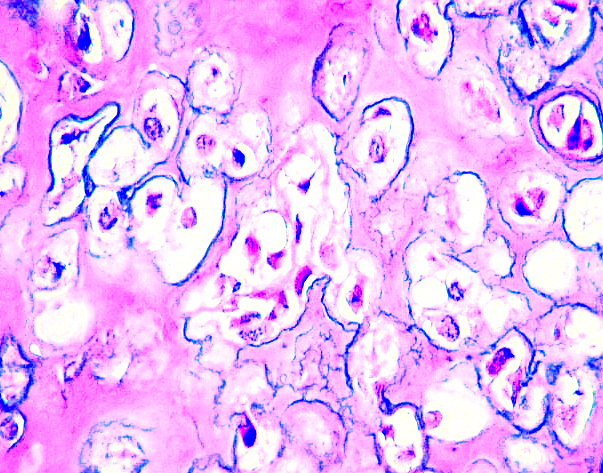
Microscopic (histologic) description
- First few days (< 3 days): organizing hemorrhage, edema, hematoma with neovascularization, acute inflammatory cells, necrotic bone (empty lacunae) adjacent to fracture site (Semin Diagn Pathol 2011;28:102)
- 3 - 7 days: granulation tissue, reactive fibroblasts, tissue culture appearance (Semin Diagn Pathol 2011;28:102)
- Fine wisps of bone present by 7 days and definite osteocartilaginous differentiation by 10 days (Semin Diagn Pathol 2011;28:102)
- 1 - 2 weeks: proliferating fibrovascular tissue, increased cellularity, islands of immature bone and cartilage, disordered organization
- 2 - 3 weeks onwards: anastomosing trabeculae of woven bone rimmed by prominent osteoblastic cells
- Mixture of hyaline cartilage, woven and lamellar bone trabeculae in plexiform pattern with zoning
Microscopic (histologic) images
Cytology description
- Numerous uniform, benign looking osteoblasts and osteoclastic giant cells (Acta Cytol 2001;45:445)
- Spindle cell clusters composed of fibroblasts
- Small fragments of bony spicules
- Lack of true cellular atypia
- Hemorrhagic background
Videos
Common types of bone fracture
How do broken bones heal?
Sample pathology report
- Bone and soft tissue, right tibia, biopsy:
- Fracture callus (see comment)
- Comment: This biopsy contains fragments of reactive bone admixed with benign hyaline cartilage and fibrovascular stroma with scattered inflammatory cells. Prominent osteoblastic rimming is present along the trabeculae of immature woven bone. No marked cytologic atypia and no evidence of malignancy is identified.
Differential diagnosis
- Osteosarcoma:
- Overt pleomorphism present
- Frequent and atypical mitotic figures
- Lace-like tumor osteoid production without osteoblastic rimming
- Infiltrative borders that entrap preexisting bone
- Lacks history of trauma or vigorous exercise
- Lacks zonal distribution of fracture callus
- Osteoid osteoma / osteoblastoma:
- Composed of irregular woven bone
- Cartilaginous matrix and fibrous component with granulation tissue missing
- May mimic stress fracture on imaging; however, lucent nidus of osteoid osteoma is typically round instead of linear
- Fibrosarcoma:
- High grade sarcoma with fibroblastic differentiation
- Fascicles of pleomorphic, spindle shaped cells with fascicular growth pattern
- Atypical mitotic figures common
- Fibrous dysplasia:
- Woven bone trabeculae randomly arranged and curvilinear
- Inconspicuous osteoblastic rimming
- Spindle cells are arranged in storiform pattern
- No / rare osteoclasts
- Chondrosarcoma:
- Infiltrating growth pattern encasing preexisting bone
- Frequent myxoid change present (grade 2)
- Neoplastic chondrocytes have varying degrees of cytologic atypia
- Aseptic bone necrosis:
- Usually occurs in younger patients
- Wedge shaped infarction
- Total necrosis of bone trabeculae and bone marrow
Additional references
Board review style question #1
Fracture healing and repair occurs through multiple stages that mimic the natural development of the skeletal system. What is the appropriate chronological order of the different stages of fracture repair?
- Hard callus, soft callus, inflammation, remodeling, hematoma
- Hematoma, inflammation, soft callus, hard callus, remodeling
- Remodeling, hematoma, inflammation, hard callus, soft callus
- Soft callus, hematoma, remodeling, inflammation, hard callus
Board review style answer #1
B. Hematoma, inflammation, soft callus, hard callus, remodeling. Fracture healing starts when a hematoma forms between the 2 ends of bone, creating a fibrin mesh that seals the site. Next, tissue damage leads to inflammation and the activation of wound healing pathways. Chondroblasts and fibroblasts create a soft callus and new bone eventually replaces the soft callus with a hard callus. Lastly, remodeling leads to bone resorption and lamellar bone formation. Answers A, C and D are incorrect because the different stages of fracture repair are not listed in the appropriate chronological order as listed in answer B.
Comment Here
Reference: Fracture
Comment Here
Reference: Fracture
Board review style question #2
Osgood-Schlatter disease may rarely result in which of the following types of fracture?
- Avulsion fracture
- Bucket handle fracture
- Greenstick fracture
- Open (compound) fracture
Board review style answer #2
A. Avulsion fracture. Osgood-Schlatter disease is an enthesopathy, which rarely results in an avulsion fracture of the tibial tubercle. It usually affects young, active adolescents experiencing growth spurts and frequently presents as anterior knee pain. Answer D is incorrect because an open (compound) fracture is associated with trauma and results in the fractured bone poking through the skin. Answer C is incorrect because a greenstick fracture is an incomplete fracture that frequently occurs in young children after a fall. Answer B is incorrect because a bucket handle fracture is a metaphyseal corner fracture that is associated with child abuse and nonaccidental injury.
Comment Here
Reference: Fracture
Comment Here
Reference: Fracture