Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Guney AK, Qasem S. Chondrosarcoma (primary, secondary, periosteal). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/bonechondrosarcoma.html. Accessed March 29th, 2025.
Definition / general
- Locally aggressive or malignant group of tumors characterized by formation of cartilaginous matrix
- Primary: arising without a benign precursor
- Secondary:
- Central: arising in preexisting enchondroma
- Peripheral: arising in preexisting cartilaginous cap of an osteochondroma
- Periosteal chondrosarcoma: occurs on the surface of the bone in association with the periosteum
Essential features
- Locally aggressive or malignant group of tumors characterized by formation of cartilaginous matrix and chondrocytes embedded in lacunae
- Histologic grade, extracompartmental spread and local recurrence are important prognostic factors
- Radiology is essential, especially for low grade lesions
- Change in the size or clinical symptoms might be an indicator of malignant transformation in enchondromas and osteochondromas
- IDH1 and IDH2 mutations in approximately 50% of cases
Terminology
- Atypical cartilaginous tumor = tumors resembling grade 1 chondrosarcoma arising in the appendicular skeleton
- Periosteal chondrosarcoma = juxtacortical chondrosarcoma
- Conventional chondrosarcoma = primary, secondary and periosteal chondrosarcomas
- For low grade tumors, the term low grade cartilaginous neoplasm can be used
Epidemiology
- Accounts for ~20% of all malignant bone tumors
- Second most common primary malignant bone tumor after osteosarcoma (Cancer 1995;75:203)
- Middle aged to older adults (secondary and periosteal chondrosarcoma are seen in younger patients)
- M > F
Sites
- Most common sites are the pelvic bones, femur and humerus (Cancer Imaging 2003;4:36)
- Other sites are the trunk, skull and facial bones
- Involvement of the hands and feet is rare
- Periosteal chondrosarcoma involves the metaphysis of long bones, usually distal femur and humerus
- Conventional type chondrosarcoma is also the most common sarcoma arising in the larynx (Am J Surg Pathol 2002;26:836, Head Neck Pathol 2020;14:707)
Etiology
- Unknown etiology for primary chondrosarcoma
- Malignant transformation from benign precursors in secondary chondrosarcomas (J Am Acad Orthop Surg 2010;18:608)
- Increased risk of secondary chondrosarcoma in patients with Ollier disease and Maffucci syndrome (Oncologist 2011;16:1771)
Clinical features
- Pain, local swelling and enlarging mass are the most common presenting symptoms (Semin Diagn Pathol 2014;31:10)
- Neurological symptoms in skull base tumors (StatPearls: Chondrosarcoma [Accessed 9 March 2021])
- Change in the size and clinical symptoms might be an indicator of malignant transformation in enchondromas and osteochondromas
Diagnosis
- Diagnosis of chondrosarcoma can be made on imaging studies (Xray, CT scan, MRI) in combination with biopsy specimen (Skeletal Radiol 2013;42:611)
- Radiology is essential, especially in low grade lesions
Radiology description
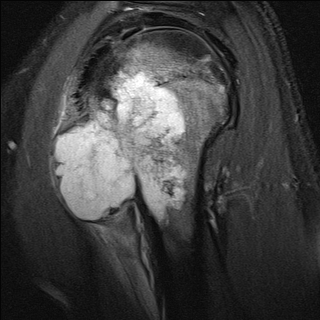
- Xray: popcorn-like calcifications (punctate and ring-like opacities), lytic lesions, endosteal scalloping, thickened cortex, cortical erosion or destruction, soft tissue involvement (Curr Probl Diagn Radiol 2019;48:262)
- Cortical destruction and soft tissue extension of pre-existing enchondromas might be indicators of secondary central chondrosarcoma
- Thick cartilaginous cap > 1.5 - 2 cm in secondary peripheral chondrosarcoma (Radiologe 2016;56:476)
- Multilobular appearance in periosteal chondrosarcoma
- CT scan and MRI: helpful in showing the extent of the tumor
Radiology images
Prognostic factors
- Histologic grade, extracompartmental spread and local recurrence are important prognostic factors (J Bone Joint Surg Br 2002;84:93)
- Atypical cartilaginous tumor / grade I chondrosarcomas are locally aggressive and have a good prognosis (~85% 5 year survival rate)
- Grade II / III chondrosarcomas have a worse prognosis (~50% 5 year survival rate)
- Local recurrence is related to tumor size and adequacy of surgical margins
Case reports
- 30 year old woman with periosteal chondrosarcoma and bone metastasis (World J Surg Oncol 2015;13:121)
- 35 year old man with postradiation chondrosarcoma (Int J Biol Markers 2014;29:e440)
- 36 year old man presenting with sciatica (J Orthop Case Rep 2020;10:53)
- 43 year old woman presenting with dyspareunia (Rom J Morphol Embryol 2018;59:927)
- 54 year old man with pain and swelling in the left preauricular area (Med Oral Patol Oral Cir Bucal 2009 Jan;14:E39)
Treatment
- Wide surgical resection is the mainstay of treatment
- Low grade chondrosarcomas are often surgically cured
- Chondrosarcomas are in general resistant to chemotherapy and radiotherapy (Curr Opin Oncol 2016;28:314)
- Chondrogenic tumors require a high dose of radiation (Oncologist 2008;13:320)
- Resection with adjuvant radiotherapy yields the best outcome for high grade chondrosarcomas (Neurosurgery 2017;81:520)
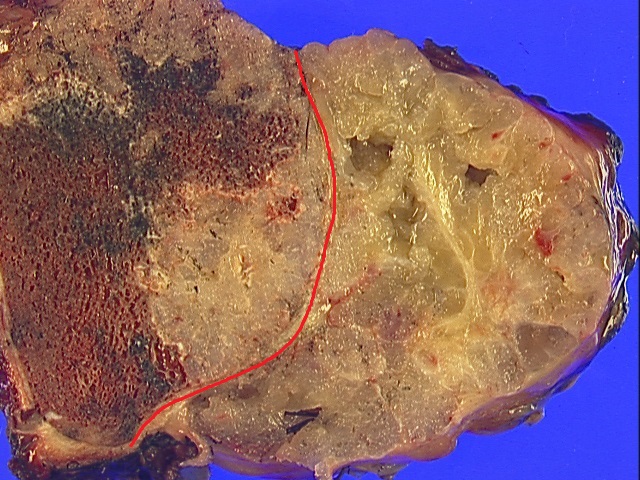
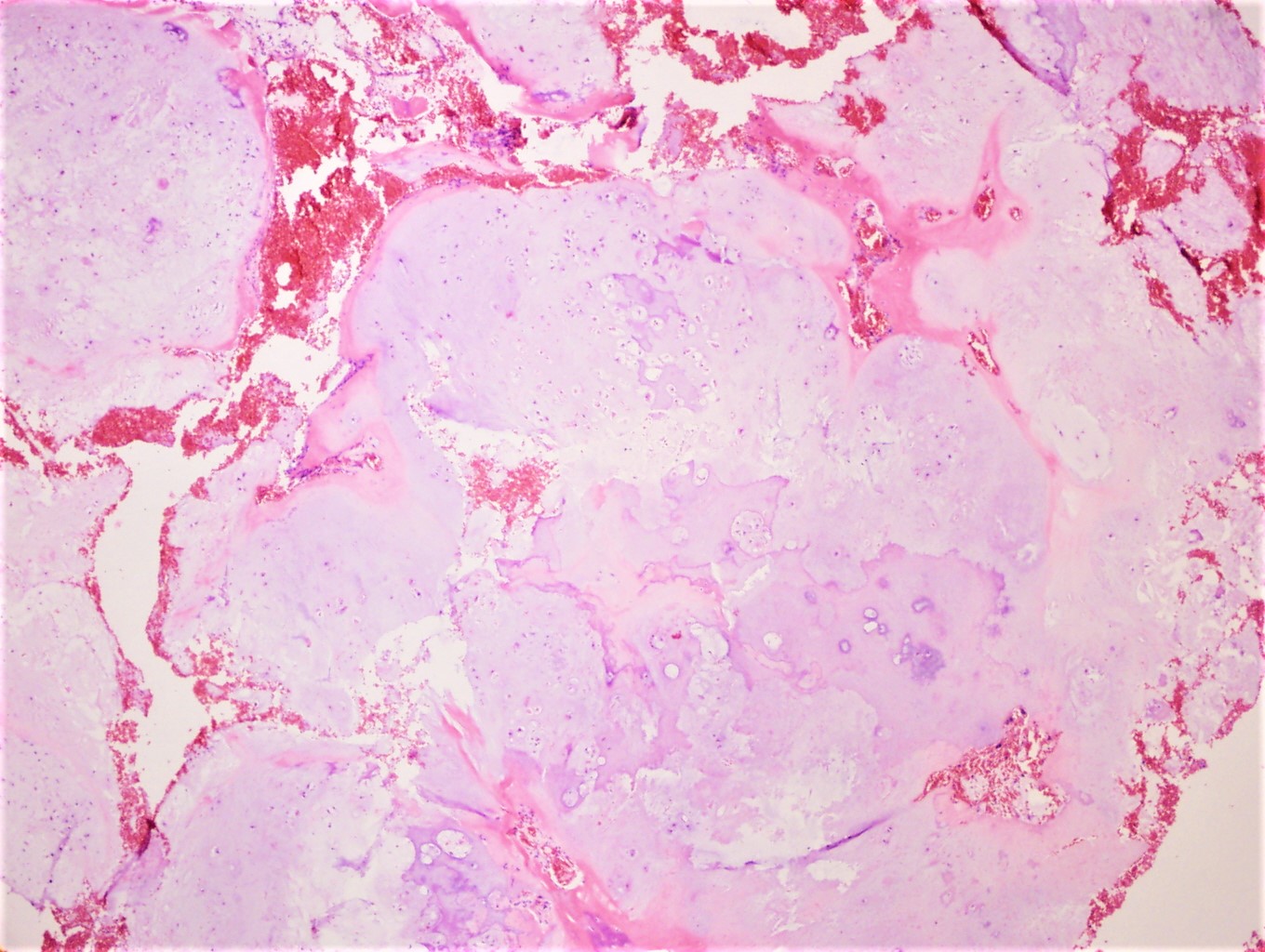
Gross description
- Neoplastic hyaline cartilage has a lobular, gray-tan cut surface
- Cystic changes with myxoid or mucoid material
- Mineralization appears as chalky calcium deposits
- Cortical erosion and soft tissue extension can be seen
- Thick cartilage cap (1.5 - 2 cm) with cystic cavities in secondary peripheral chondrosarcoma
- Periosteal chondrosarcoma appears as a large, lobular mass attached to the surface of bone (Am J Surg Pathol 1985;9:666)
Frozen section description
- Nodules of hyaline cartilage with variable atypia (Sarcoma 2014;2014:902104)
- For low grade tumors, the term low grade cartilaginous neoplasm can be used
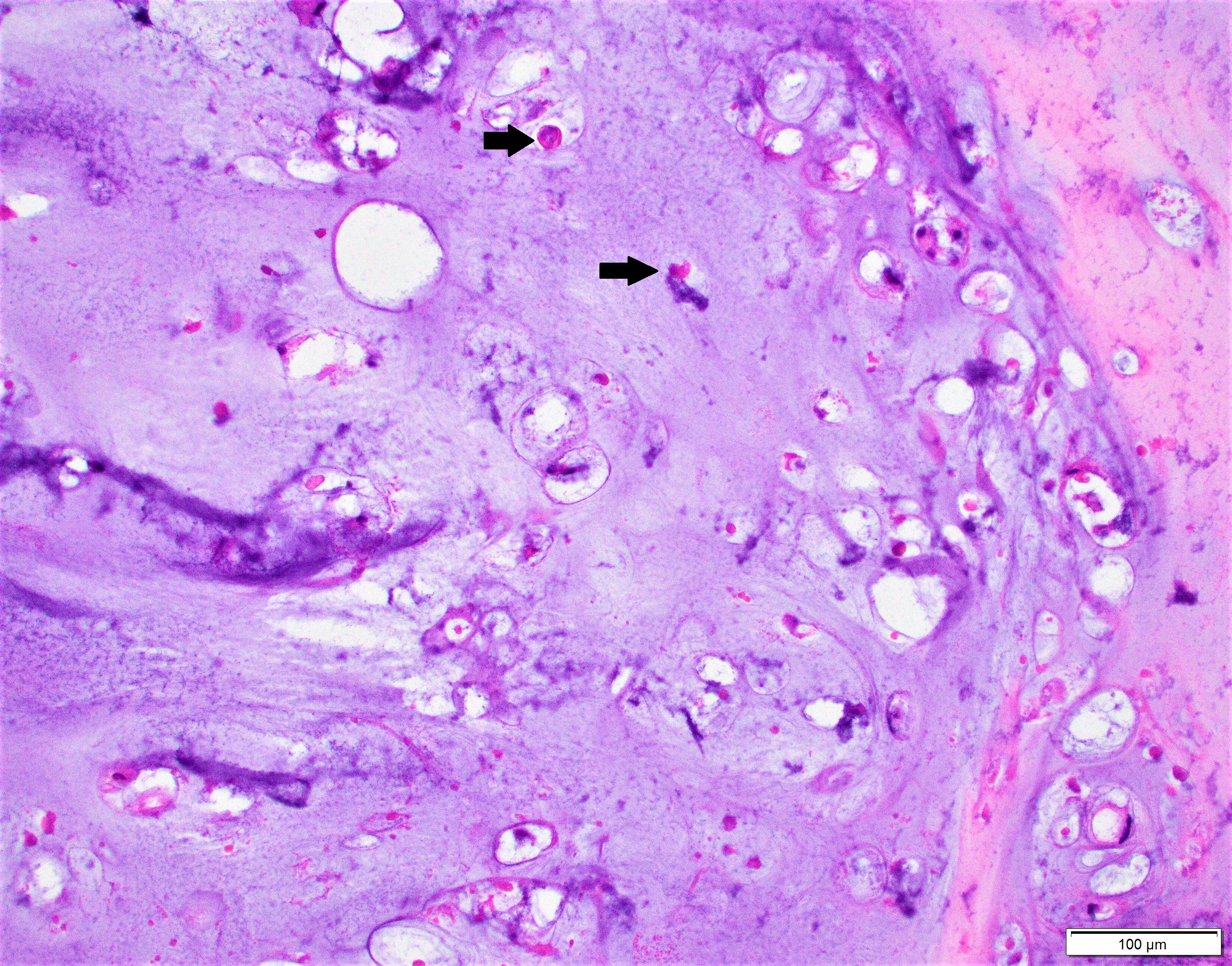
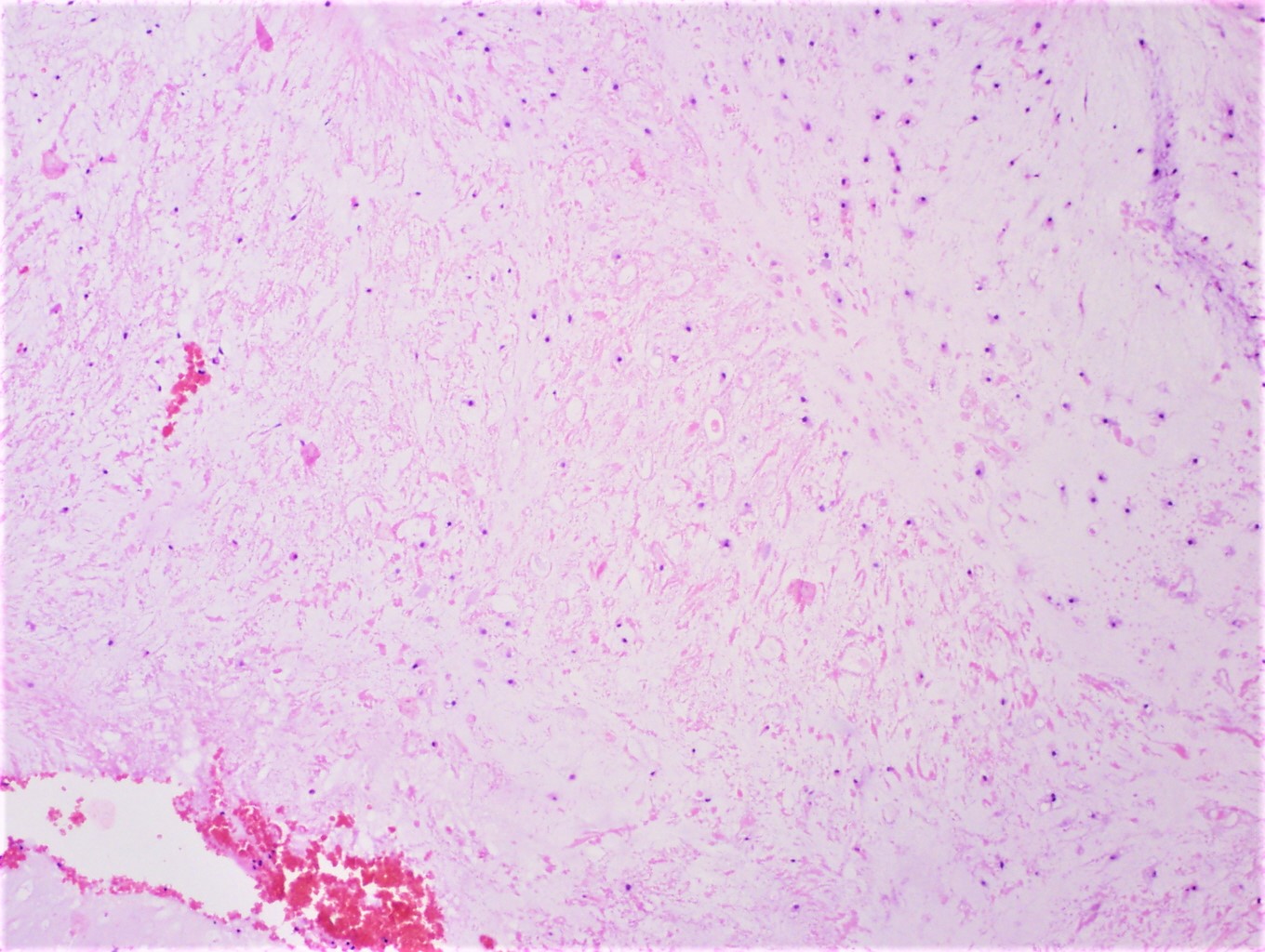
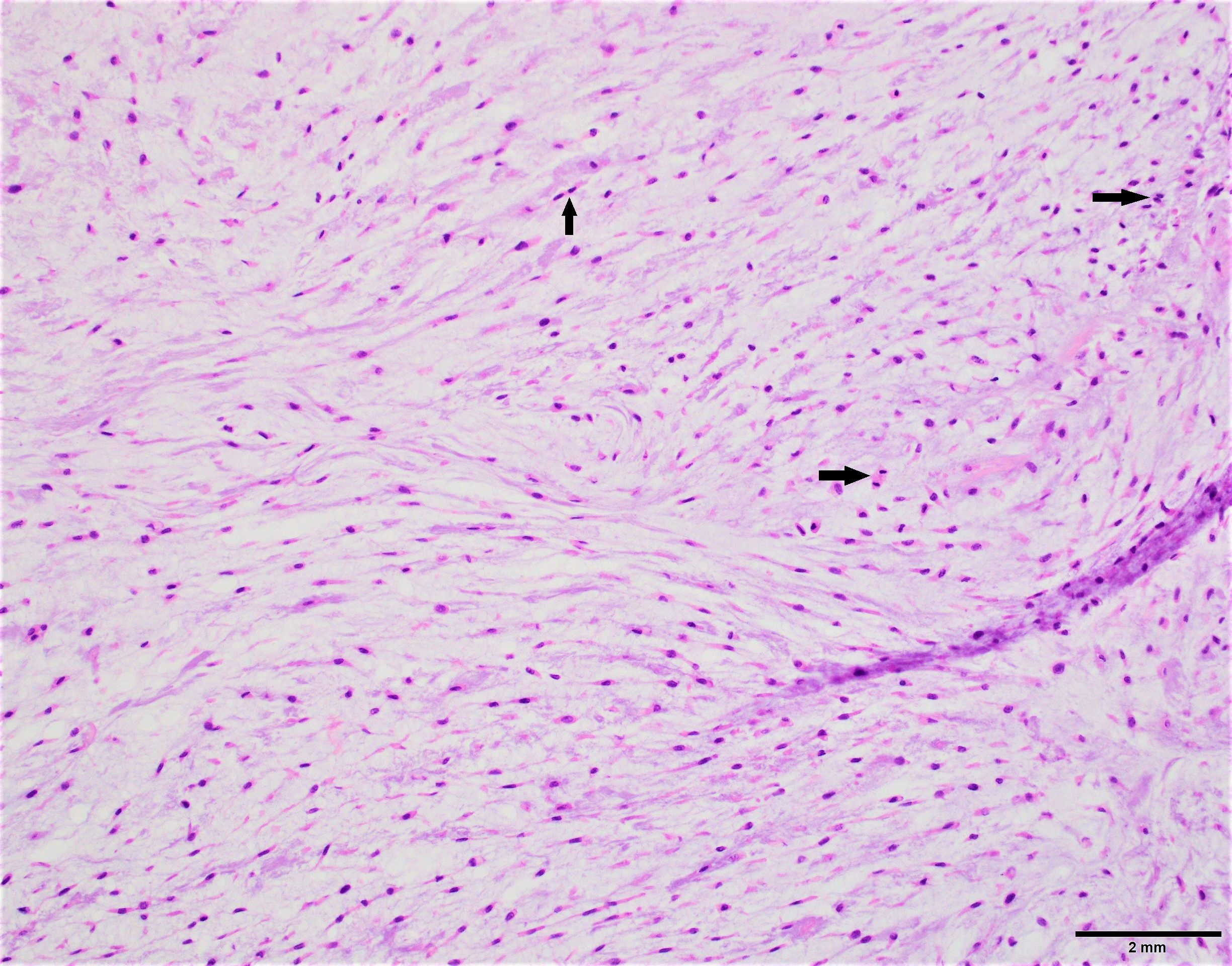
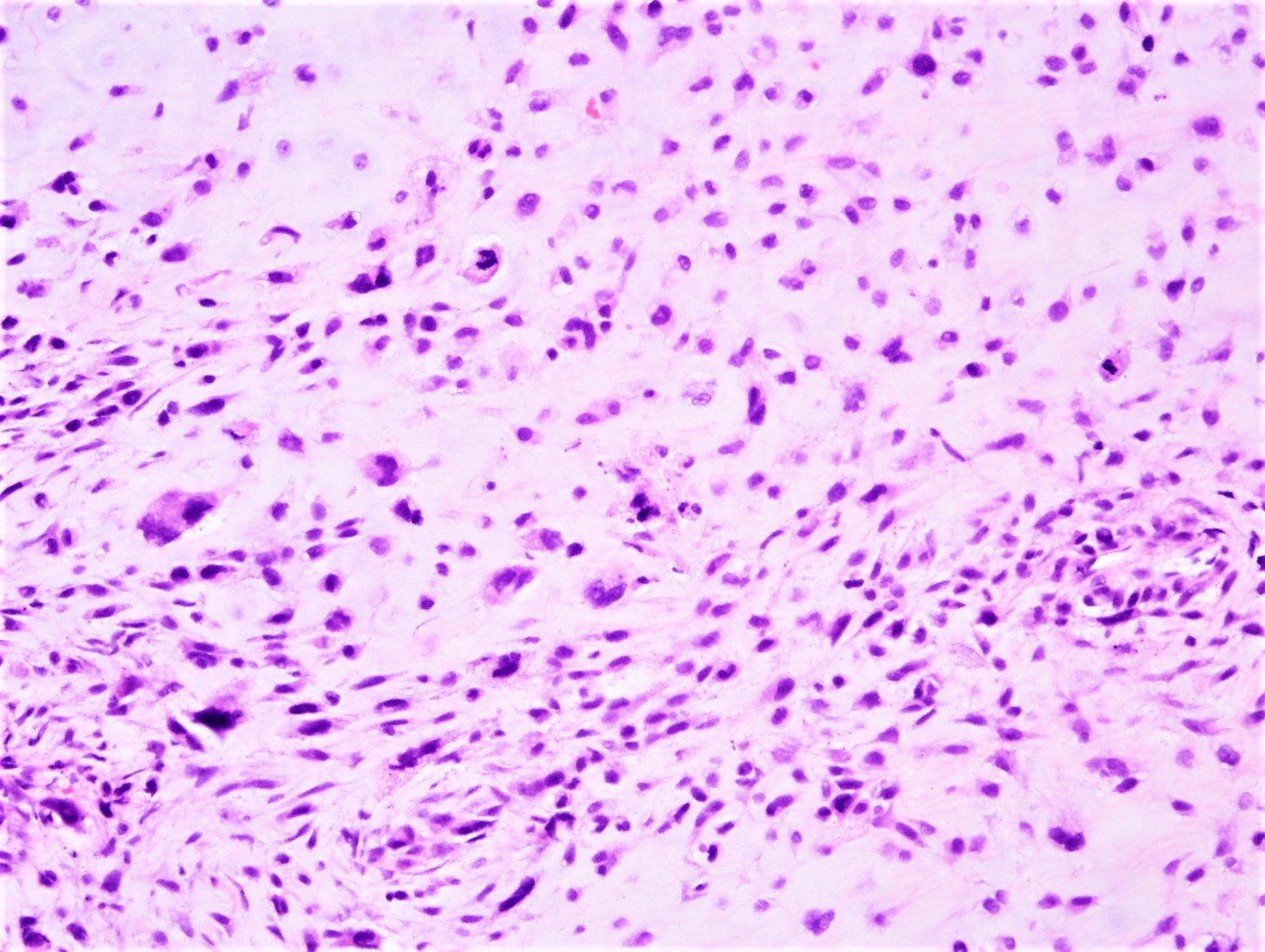
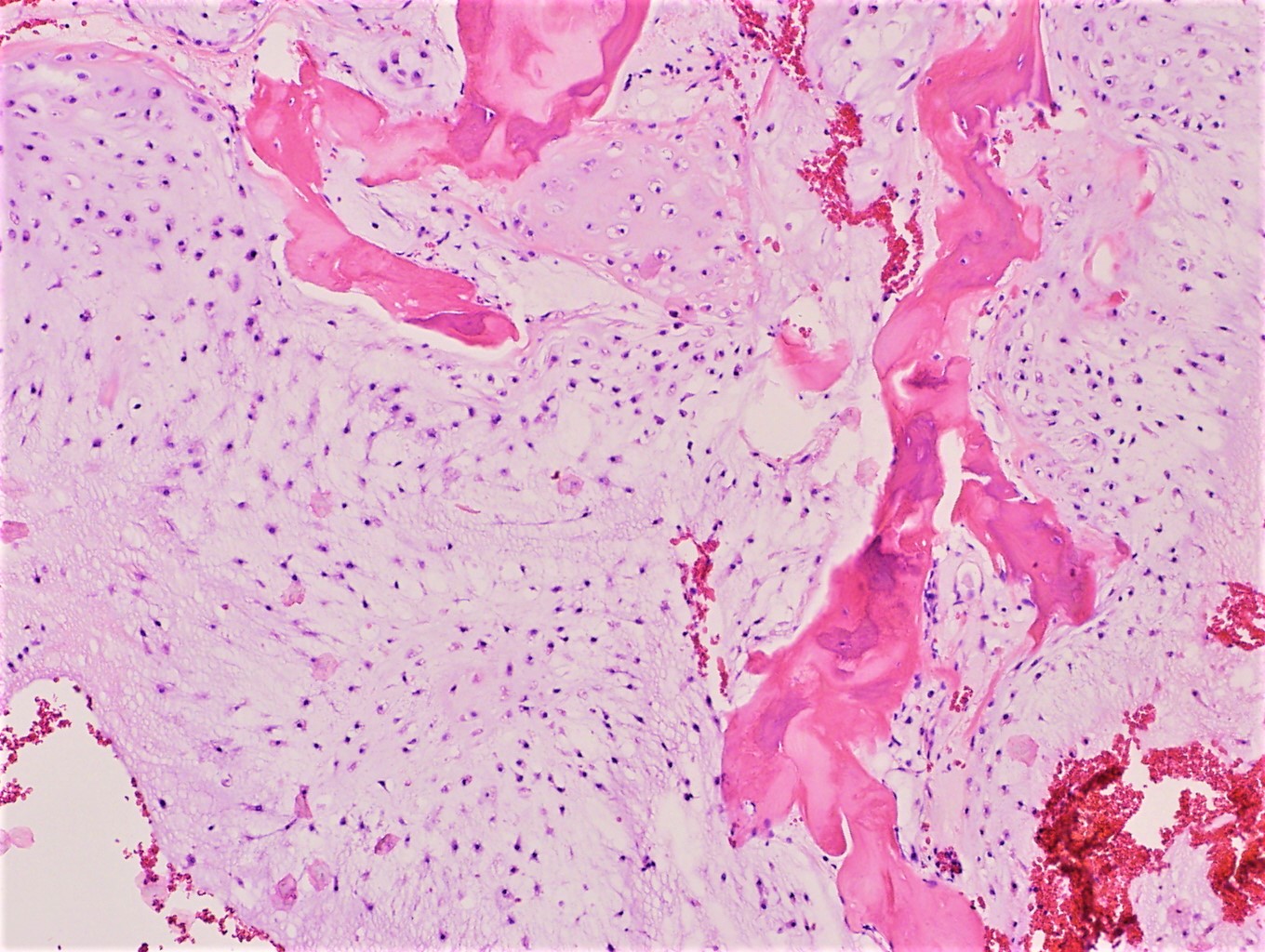
Microscopic (histologic) description
- Abundant cartilaginous matrix with chondrocytes embedded in lacunae
- Lobular or diffuse growth (depending on grade)
- Permeation of intertrabecular spaces
- Varying degrees of increased cellularity, nuclear atypia and mitotic activity
- Grade I: minimally increased cellularity, nodular growth and occasional binucleate nuclei
- Grade II: moderate cellularity and diffuse growth
- Grade III: high cellularity, marked atypical cells, pleomorphic appearance and easily identifiable mitotic figures
- Myxoid changes, chondroid matrix liquefaction and necrosis can be seen
- Formation of nodules and cystic cavities can be seen in secondary peripheral chondrosarcoma (generally low grade tumors)
- Periosteal chondrosarcoma:
- Grade I or II tumors seen on the external surface of the bone
- Cortical invasion, soft tissue extension and size (> 5 cm) can be helpful in distinguishing from periosteal chondroma (AJR Am J Roentgenol 2001;177:1183)
Microscopic (histologic) images
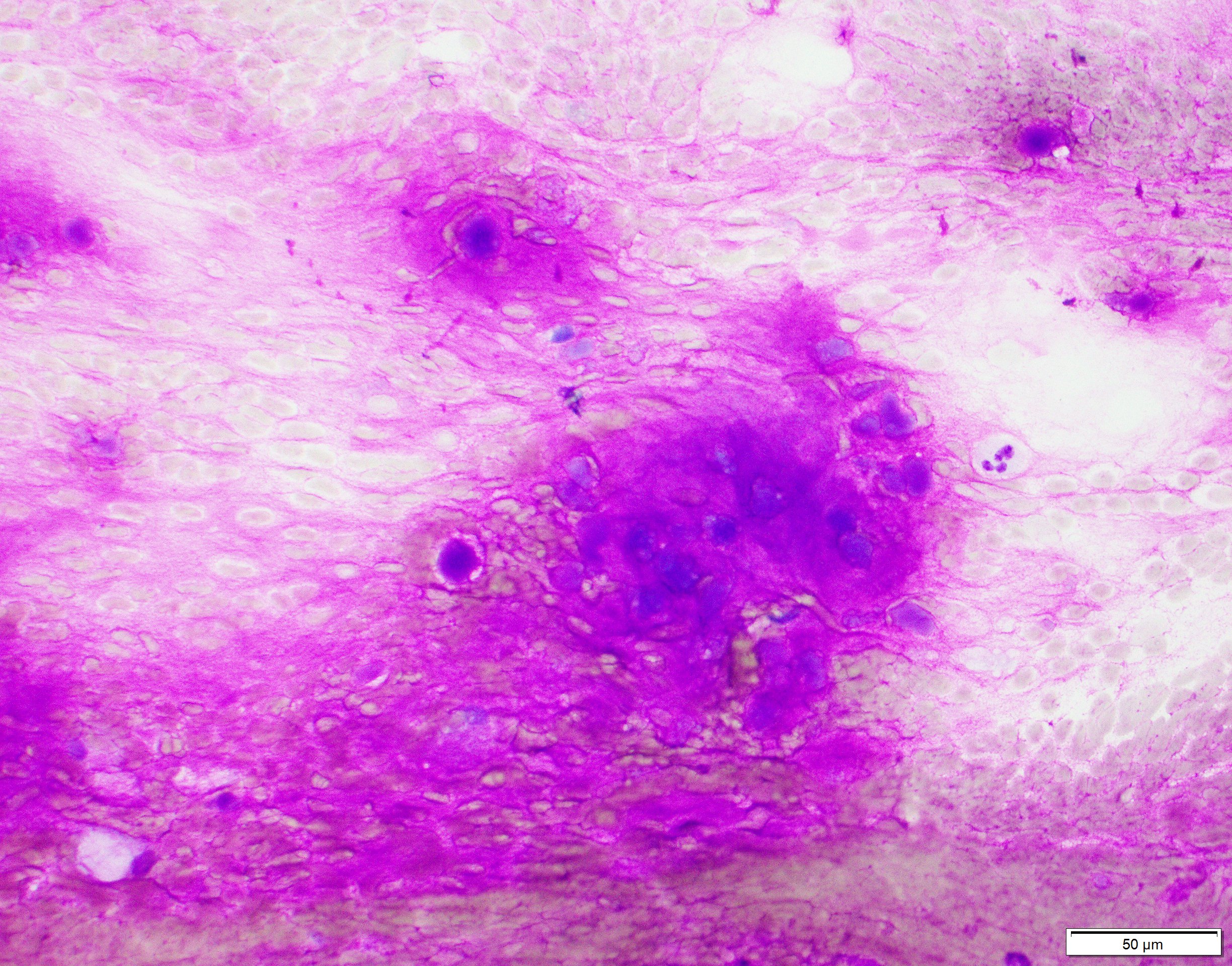
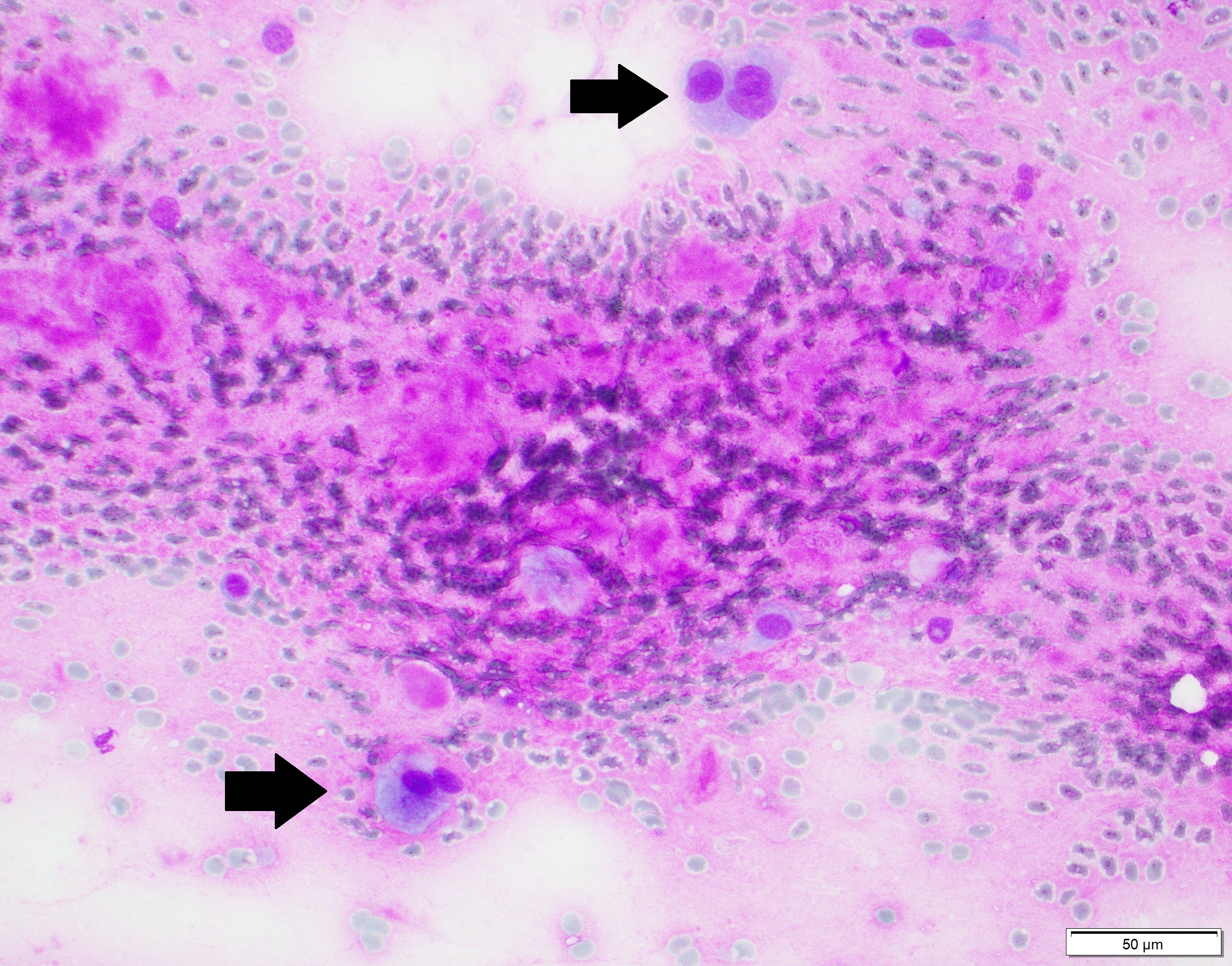
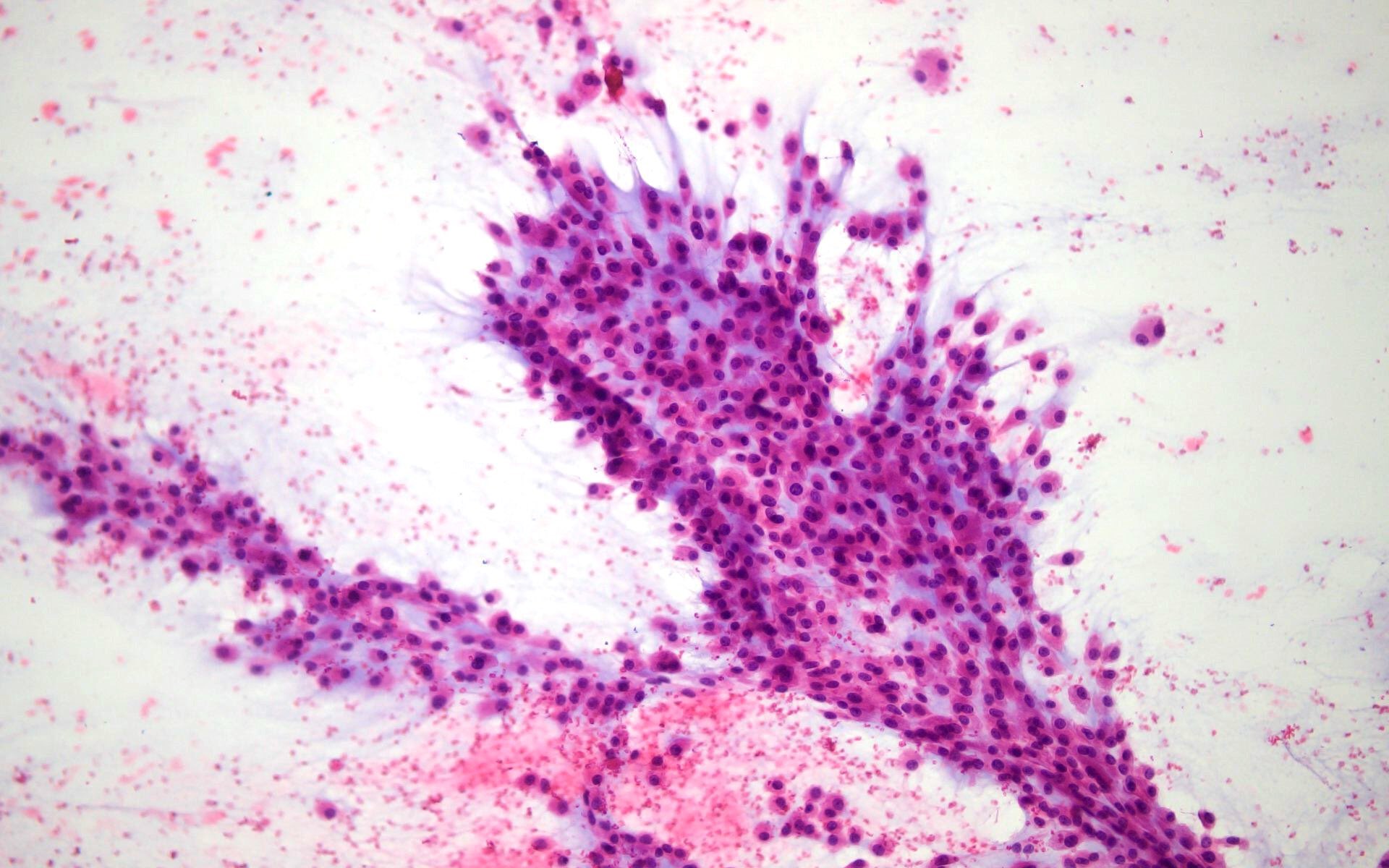
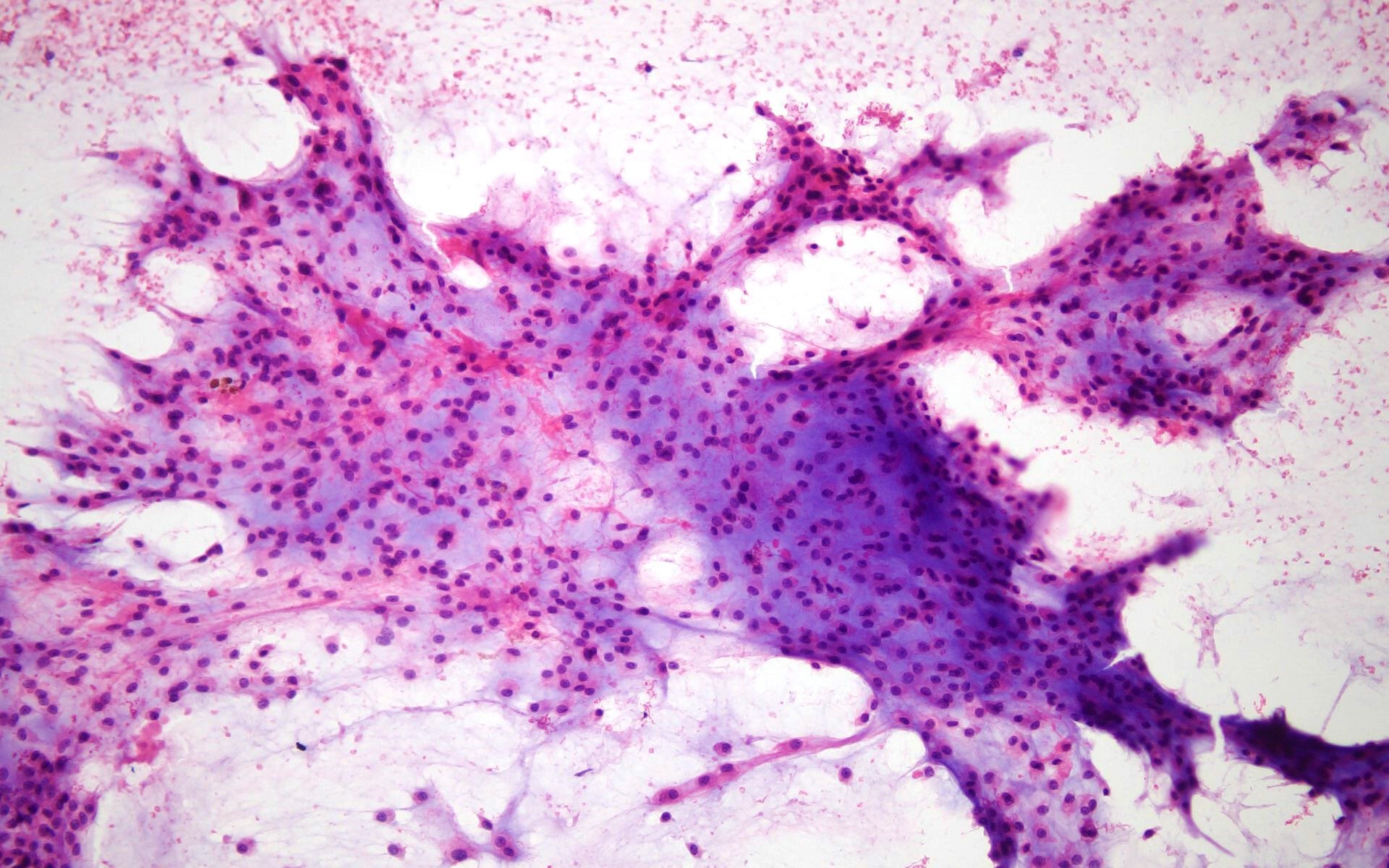
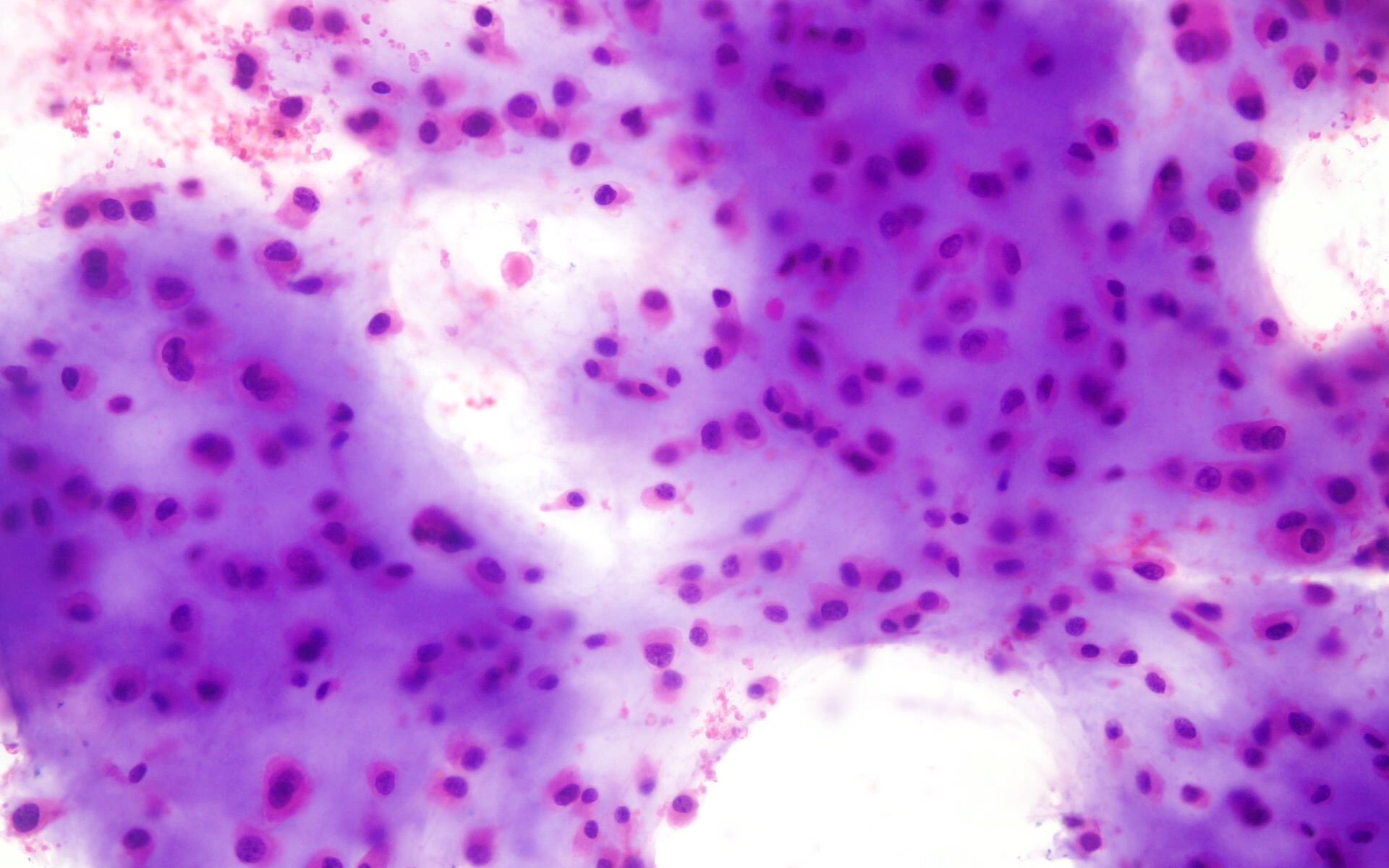
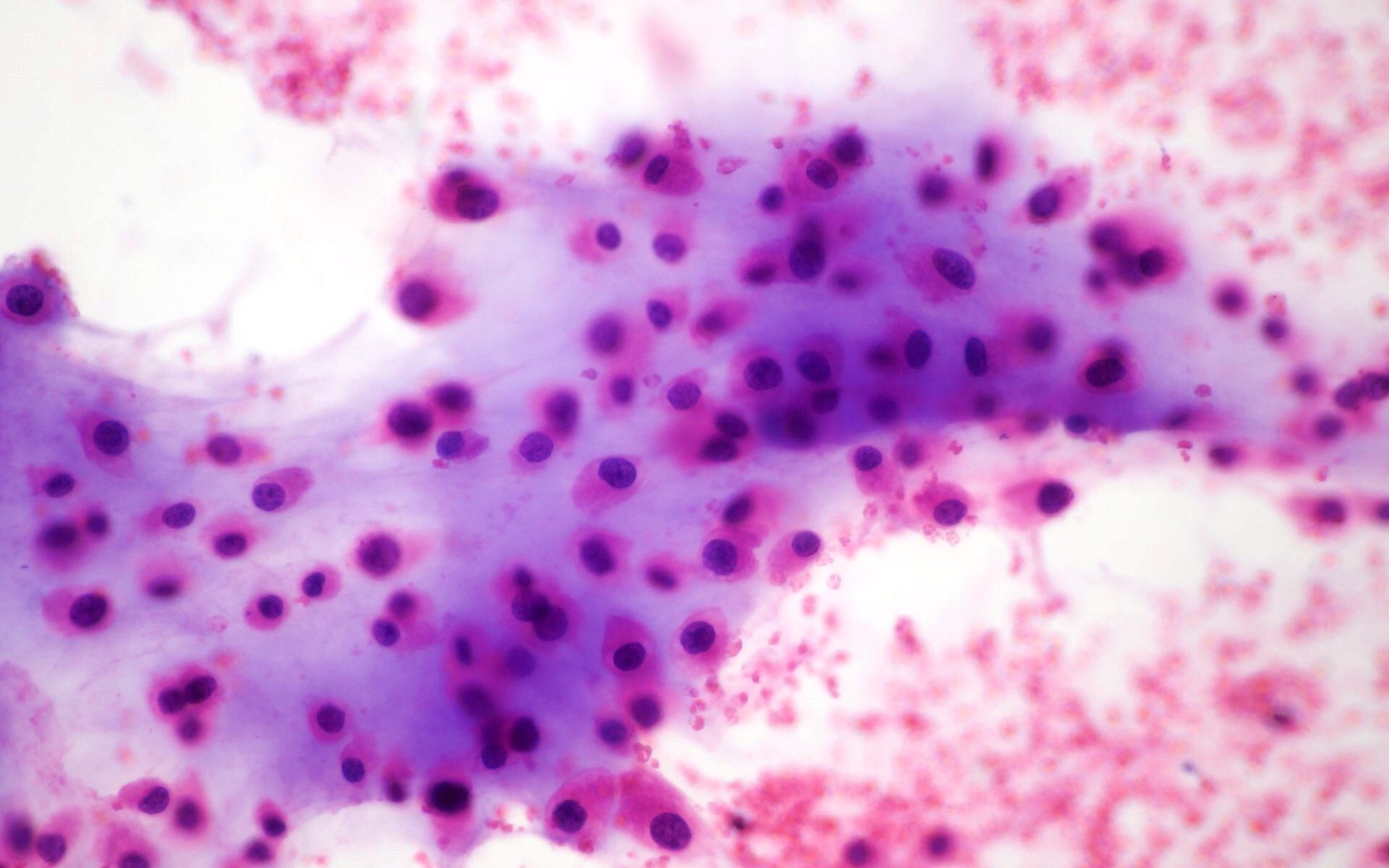
Cytology description
- Abundance of extracellular matrix material, which is best appreciated on air dried, Giemsa based stained material
- Recognizable lacunae, often containing binucleated or multinucleated chondrocytes
- Atypical cartilaginous tumor / grade I chondrosarcoma is cytomorphologically indistinguishable from an enchondroma
- Grade II / III chondrosarcomas are more cellular, more atypical with more myxoid matrix
- Cytology is more reliable in metastatic than primary tumors (Diagn Cytopathol 2006;34:413)
Cytology images
Positive stains
- Stains are not necessary in the majority of cases
- S100: uniformly strongly positive but in grade III it can be focally negative in less differentiated areas
- D2-40 (Appl Immunohistochem Mol Morphol 2009;17:131)
Negative stains
Molecular / cytogenetics description
- IDH1 and IDH2 mutations in approximately 50% of cases
- Aneuploidy is seen with increasing histologic grade
- TP53 mutations and affected active signaling pathways (RB1, CDKN2A, CDK) are identified particularly in high grade chondrosarcomas (J Cell Mol Med 2009;13:2843)
Videos
Chondrosarcoma versus enchondroma
Sample pathology report
- Tibia, biopsy:
- Low grade cartilaginous neoplasm (see comment)
- Comment: The differential diagnosis includes enchondroma and low grade chondrosarcoma. Clinical and radiologic correlation is recommended.
- Femur, resection:
- Chondrosarcoma, grade II (see comment)
- Surgical margins are negative
- See synoptic report below
- Comment: The diagnosis is made in conjunction with radiologic findings.
Differential diagnosis
- Chondroblastic osteosarcoma:
- If there is significant osteoid formation, then it is osteosarcoma
- Clinical and radiological correlation is helpful (typically younger patients)
- Enchondroma:
- No aggressive features radiologically
- Cytologically almost indistinguishable from low grade chondrosarcoma
- Less cellular, uniform hyaline, abundant matrix calcification
- Small, uniform, round nuclei with homogenous chromatin
- Fracture callus:
- Sometimes can contain abundant proliferating cartilage looking like cartilaginous neoplasia
- Chondroid matrix is less mineralized and dark blue in color
- Clinical and radiological correlation is helpful
- Chondromyxoid fibroma:
- Clinically and radiologically not aggressive
- Stellate cells
- More myxoid and less chondroid background
- SMA positive
Additional references
Board review style question #1
A 54 year old man had an 8 cm mass in the femur, which was resected. Which of the following is the best assessment?
- Radiotherapy is the mainstay of treatment
- Skull is the most common site
- The most likely genetic abnormalities are IDH1 and IDH2 mutations
- The tumor is sensitive to chemotherapy
- There is a female predominance
Board review style answer #1
C. The most likely genetic abnormalities are IDH1 and IDH2 mutations
Comment Here
Reference: Chondrosarcoma (primary, secondary, periosteal)
Comment Here
Reference: Chondrosarcoma (primary, secondary, periosteal)
Board review style question #2
A 45 year old man had a biopsy from a 7 cm mass in the proximal humerus demonstrating a low grade cartilaginous lesion. Which of the following is true?
- Correlation with radiologic findings is essential
- Fingers and toes are common sites for this neoplasm
- Molecular testing is important for diagnosis
- The tumor cells strongly stain with cytokeratin
- This tumor is common in pediatric population
Board review style answer #2
A. Correlation with radiologic findings is essential
Comment Here
Reference: Chondrosarcoma (primary, secondary, periosteal)
Comment Here
Reference: Chondrosarcoma (primary, secondary, periosteal)