Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Shaker N, Qasem S. Periosteal chondroma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/bonechondroma.html. Accessed December 25th, 2024.
Definition / general
- Rare benign cartilaginous neoplasm that arises on the surface of cortical bone beneath periosteum
Essential features
- Children and young adults
- Well defined dome shaped lesion on the surface of the bone
- Composed of benign hyaline cartilage
- No connection with medullary cavity (radiologically)
Terminology
- Juxtacortical chondroma, subperiosteal chondroma
ICD coding
- ICD-O: 9221/0 - periosteal chondroma
- ICD-11: 2E82 & XH3BC3 - benign chondrogenic tumors & periosteal chondroma
Epidemiology
- < 2% of all chondromas
- Affects children and young adults, predominantly < 30 years of age (Oncol Lett 2015;9:1637)
- M:F = 1.5:1
Sites
- Small bones of the hands and long bones of the skeleton, particularly proximal metaphyseal or diaphyseal regions of humerus and femur (Oncol Lett 2015;9:1637)
Pathophysiology
- A subset of periosteal chondromas harbor mutations in one of the IDH genes (J Pathol 2011;224:334)
- Other cytogenetic abnormalities have been reported
Etiology
- Unknown
Clinical features
- Usually small; < 3 cm in diameter (Case Rep Orthop 2014;2014:763480)
- Typically painless, may cause swelling / palpable mass
Diagnosis
- Depends greatly on radiologic features
Radiology description
- Sharply defined juxtacortical mass
- Contains popcorn or ring-like calcifications, characteristic of cartilaginous tumors
- Plain radiographs may show a discernible soft tissue mass with underlying cortical saucerization or scalloping, subjacent cortical sclerosis and overhanging margins
- CT may be helpful in identifying the presence of scattered calcification and the lack of intramedullary extension (Case Rep Orthop 2014;2014:763480)
- On MRI, periosteal chondroma typically appears as a well circumscribed juxtacortical mass with intermediate signal intensity on T1 weighted images and high signal intensity on T2 weighted images (Case Rep Orthop 2014;2014:763480)
Radiology images
Prognostic factors
- Benign tumor with a reported recurrence rate of 3.6% (Oncol Lett 2015;9:1637)
Case reports
- 12 year old girl with a swelling in the chest wall (Indian J Thorac Cardiovasc Surg 2019;35:101)
- 39 year old man with a pelvic mass (Int J Burns Trauma 2020;10:174)
- 54 year old woman presented with difficulty ambulating and worsening cognition (Cureus 2018;10:e2099)
- 55 year old woman with neck pain (Cureus 2019;11:e4523)
- 56 year old man with a painless swelling above the left clavicle (Int J Surg 2009;7:140)
Treatment
- Surgical management in the form of intralesional, marginal or en bloc resection, is the mainstay of therapy
- Marginal excision and curettage are preferable options if the diagnosis is certain prior to surgery (Oncol Lett 2015;9:1637)
Gross description
- Well defined, waxy blue-gray
- Size: < 5 cm
- Focal calcification and lobulation (Am J Surg Pathol 1982;6:631)
- Bone buttressing at the lateral edge but no medullary invasion
Gross images
Frozen section description
- These lesions are typically sent for frozen section; frozen section would show mature hyaline cartilage
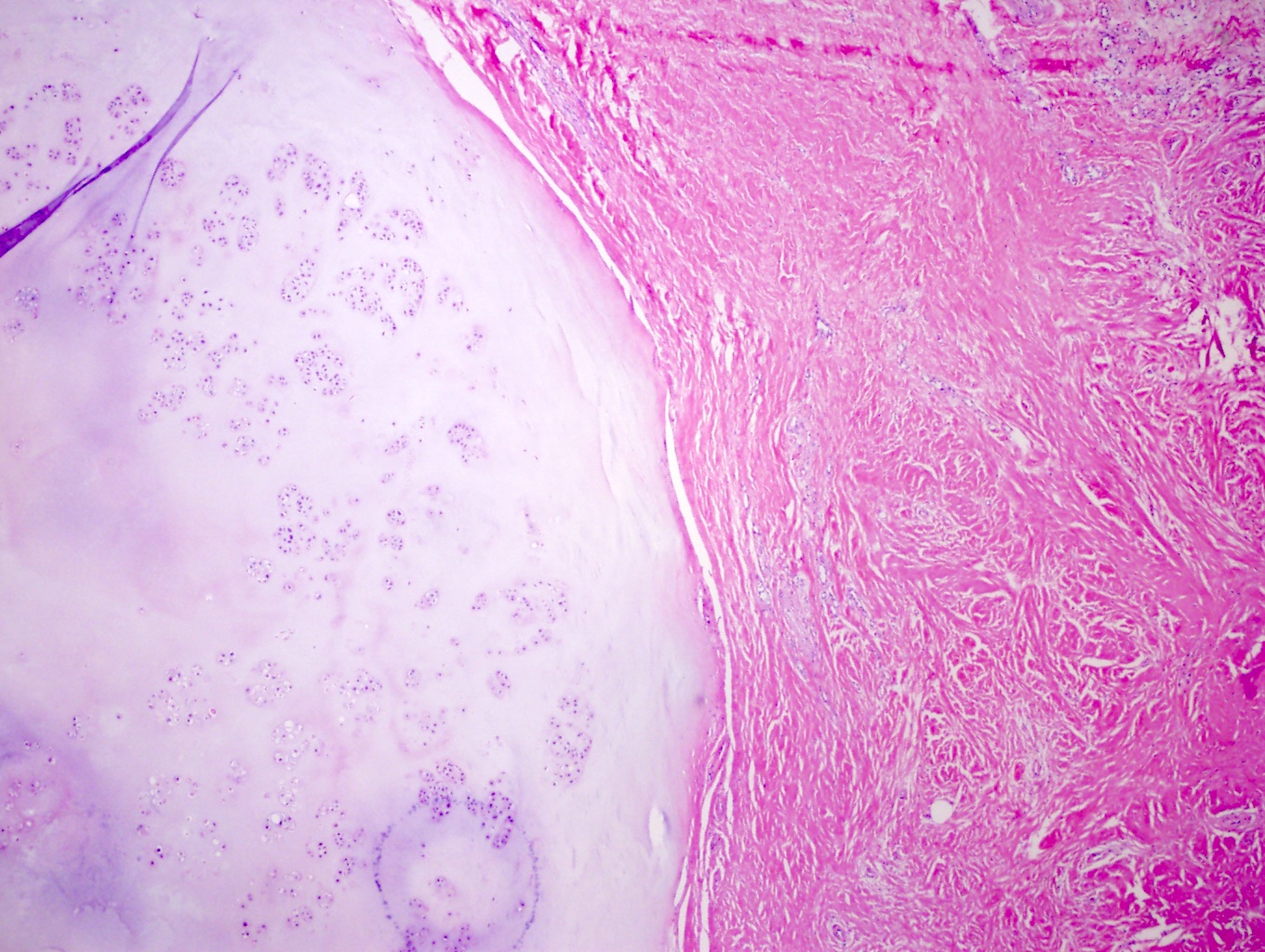
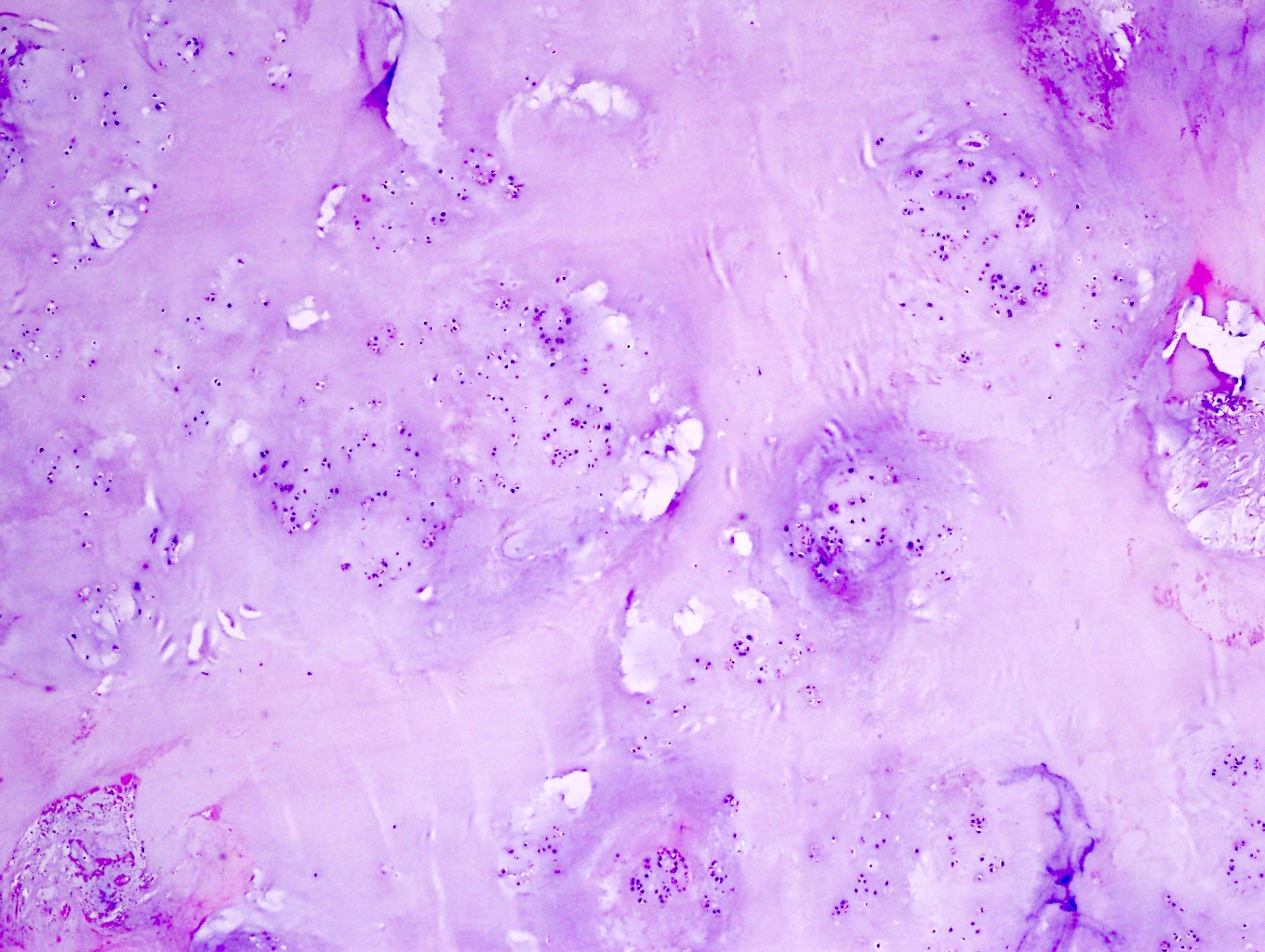
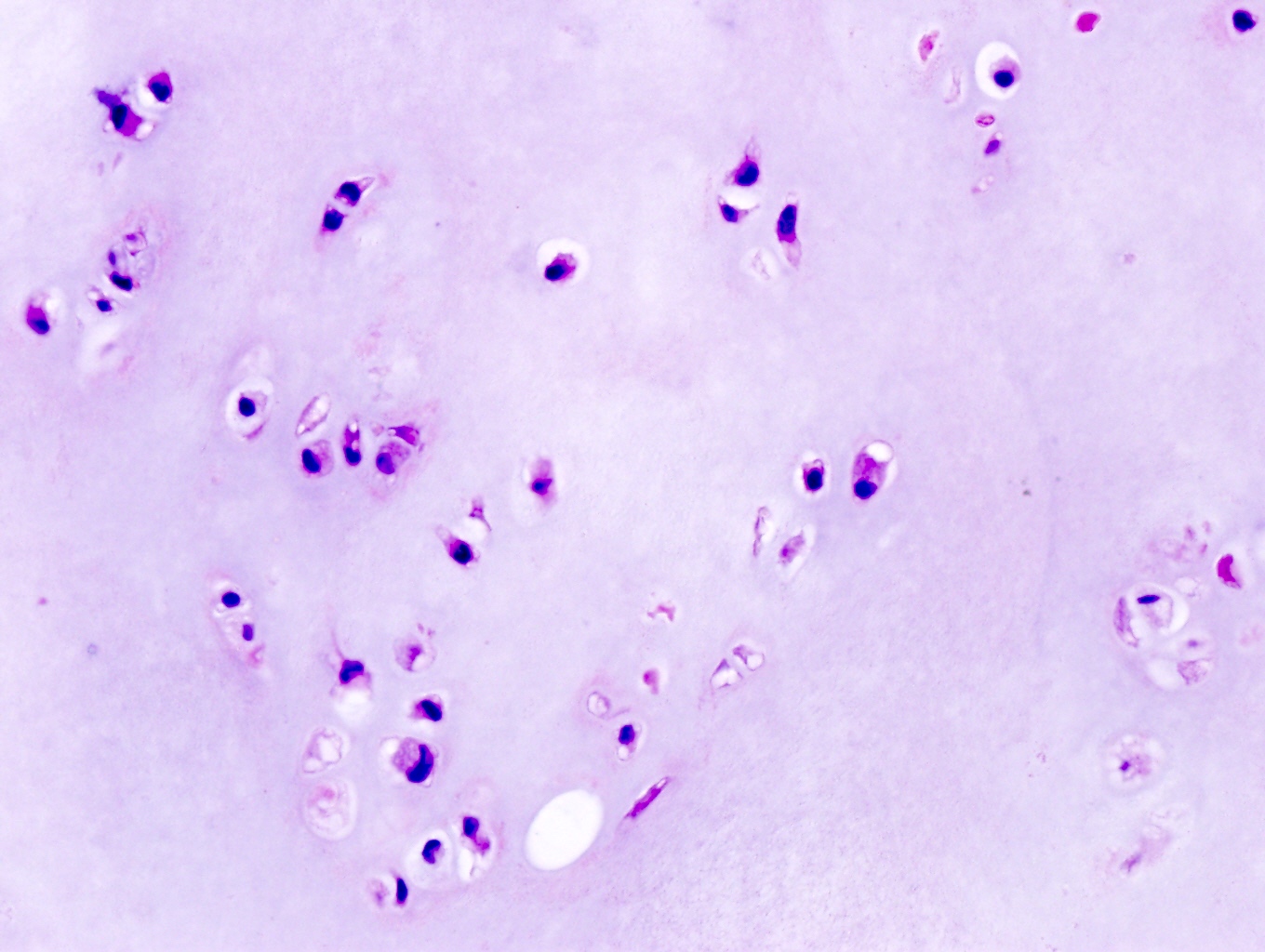
Microscopic (histologic) description
- Well demarcated from the underlying sclerotic bone, which may be focally eroded but never permeated
- Lobular architecture
- Covered by a continuous layer of attenuated periosteum
- Cellularity is variable but generally low
- Chondrocytes do not show cytologic atypia
- Occasionally, some tumors are more cellular and exhibit a greater degree of nuclear pleomorphism, including spindling and binucleation
- Invasion of surrounding soft tissue or medullary canal is not seen
Microscopic (histologic) images
Molecular / cytogenetics description
- IDH1 and IDH2 mutations have been identified in periosteal chondromas (Am J Surg Pathol 1982;6:631)
- No consistent cytogenetic abnormality has been reported
Sample pathology report
- Humerus, excision:
- Periosteal chondroma (see comment)
- Comment: The diagnosis is made in concert with radiologic findings.
Differential diagnosis
- Periosteal chondrosarcoma:
- Favored: if tumor size > 5 cm
- Definitive diagnosis: presence of invasion into haversian system in addition to radiologic findings of a destructive bone lesion
- Periosteal osteosarcoma:
- Radiology: lucent, fusiform mass on the surface of bone, with variable mineralization; the cortex is thickened with periosteal reaction
- Histology: poorly delineated lobules of atypical cartilage with intervening bands of primitive sarcomatous cells and neoplastic bone formation
- Parosteal osteosarcoma:
- Radiology: mineralized, lobular mass at the bone surface; the underlying cortex may be normal, thickened or destroyed
- Histology: well formed bone trabeculae with intervening fascicles of spindle cells with minimal atypia and low mitotic activity
- MDM2 amplification
- Bizarre parosteal osteochondromatous proliferation:
- Radiology: well circumscribed calcified mass on the cortical surface
- Histology: disorganized cellular lesion composed of spindle cells, atypical chondrocytes and bone; the presence of blue bone is characteristic
- Periosteal chondromyxoid fibroma:
- Radiology: often multilobated with prominent calcifications
- Histology: myxoid stroma with stellate cells
- Soft tissue chondroma:
- Radiology: well demarcated, separated from the bone and has calcifications
- Histology: nodules of well delineated cartilage, matrix is hyaline or myxoid and may calcify; chondrocytes show limited atypia and little mitotic activity
Additional references
Board review style question #1
Board review style answer #1
Board review style question #2
Which of the following is true for periosteal chondroma?
- Bone buttressing is characteristic on gross examination
- En bloc resection is the preferred therapy
- Molecular testing is helpful for differentiating this lesion from chondrosarcoma
- Tumor size > 5 cm is not unusual
Board review style answer #2
A. Bone buttressing is characteristic on gross examination
Comment Here
Reference: Periosteal chondroma
Comment Here
Reference: Periosteal chondroma









%20type%20gross.jpg)