Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Akinsanya AO, Warmke L. Bizarre parosteal osteochondromatous proliferation. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/bonebizarreparosteal.html. Accessed December 26th, 2024.
Definition / general
- Benign, surface based lesion of bone frequently involving the small bones of the hands and feet, first described by Nora in 1983 (Am J Surg Pathol 1983;7:245)
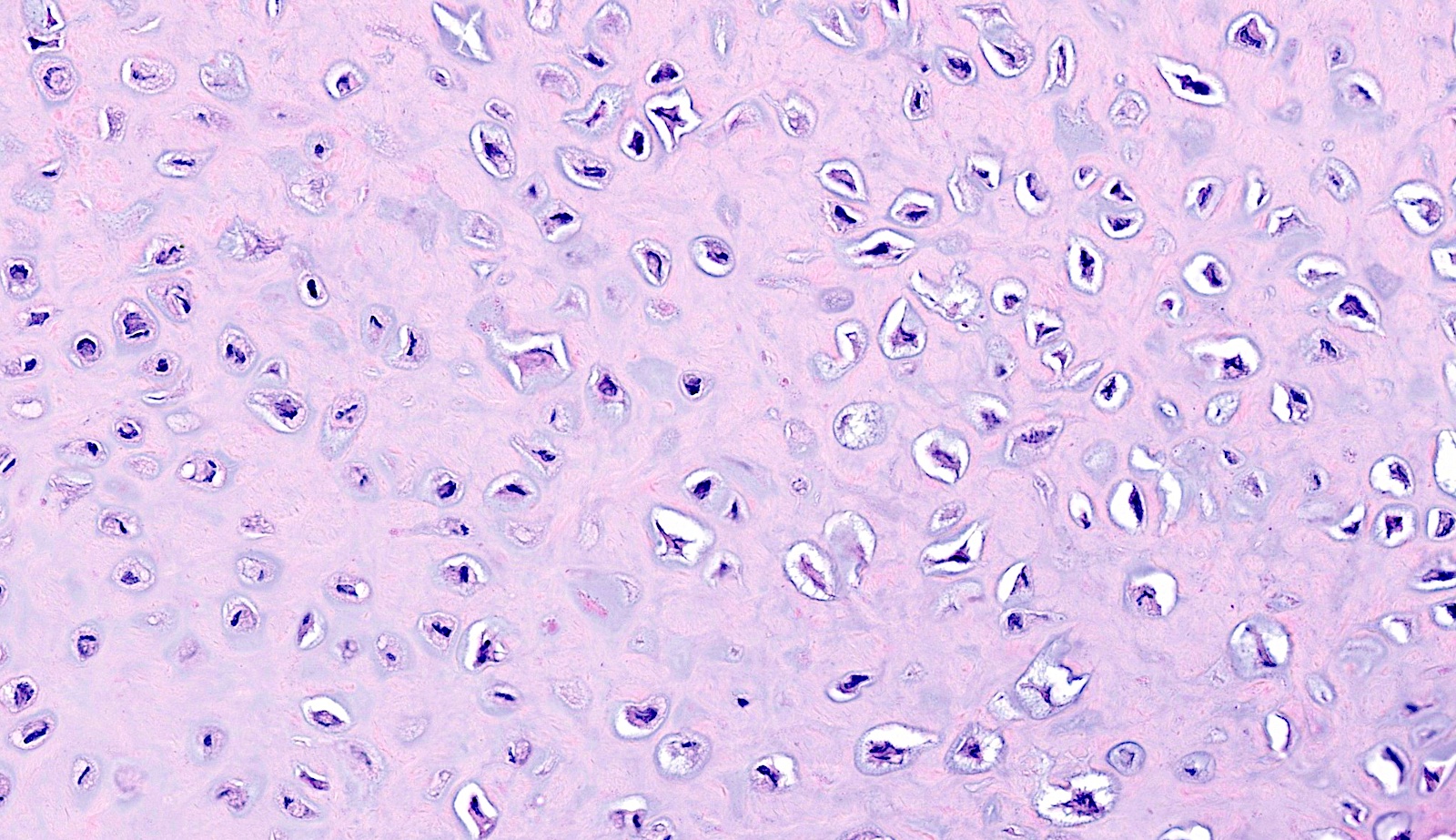
- Consists of an admixture of bland spindle cells, disorganized cartilage and benign bone with a characteristic basophilic matrix described as blue bone
Essential features
- Exophytic bony growth with intact cortex
- Disorganized cellular lesion comprising spindle cells, atypical chondrocytes and bone
- Presence of blue bone is characteristic
Terminology
- Not recommended by the WHO: Nora lesion
- Abbreviation: BPOP
ICD coding
Epidemiology
- Usually affects young adult patients (Mod Pathol 2023;36:100011)
- Wide age range with a peak in the third to fourth decades of life
- No sex predilection
Sites
- Typically affects the small bones in the hands and feet
- Hands are the most common, followed by feet and long bones (Insights Imaging 2023;14:109)
- Rarely reported on craniofacial bones
Pathophysiology
- Recurrent cytogenetic abnormalities include t(1;17)(q32;q21), inv(7) and inv(6) (Hum Pathol 2004;35:1063, Cancer Genet 2013;206:402)
- Alterations are different from translocations associated with subungual exostosis (Int J Cancer 2011;128:487)
Etiology
- Viewed by some as part of a spectrum encompassing florid reactive periostitis and turret exostosis (Skeletal Radiol 2006;35:497)
- Favored by others to represent a neoplasm due to recurrent cytogenetic abnormalities
- Possible traumatic etiology has been suggested (Skeletal Radiol 1992;21:301)
Clinical features
- Typically presents as a slow growing, firm and painless mass
- Often present for a few months to several years
- Usually presents as a relatively small lesion, 1 - 3 cm
- Some cases may grow rapidly, clinically raising concern for malignancy
- May cause local symptoms due to mass effect
- History of trauma reported in minority of patients (Mod Pathol 2023;36:100011)
Diagnosis
- Exophytic bony lesion with intact cortex
- Presence of 3 components: spindle cells, bone and atypical cartilage
Radiology description
- Ultrasound
- Calcified soft tissue mass
- No extension into underlying cortex (Insights Imaging 2023;14:109)
- Radiograph
- Periosteal soft tissue swelling (early stage) (Insights Imaging 2023;14:109)
- Progressive mineralization over several months
- Ossified surface based mass (late stage)
- Computed tomography (CT) scan
- Ossified surface based mass in contiguity but not continuity with underlying cortex
- No cortical breakthrough
- Usually no bone marrow extension
- Exceptional cases have reported medullary continuity (Skeletal Radiol 2007;36:829, Skeletal Radiol 2011;40:1487)
- Magnetic resonance imaging (MRI)
- Low to intermediate signal on T1 weighted sequences
- Intermediate to high signal on T2 weighted sequences
- Hyperintensity at the periphery representing cartilage
- Contrast enhancement can be seen
Radiology images
Prognostic factors
- Benign clinical course
- Recurrence is relatively frequent, reported up to 55%, sometimes multiple times (Am J Surg Pathol 1993;17:691)
- Recurrences are nondestructive and managed by re-excision
- No capacity to metastasize
Case reports
- 11 year old girl with a 2.5 cm wrist mass with medullary cavity continuity (BMC Musculoskelet Disord 2024;25:588)
- 35 year old man with a 3 cm left hand mass (Cureus 2023;15:e50439)
- 40 year old man with a 3 cm mass of second metatarsal head (J Orthop Case Rep 2024;14:99)
- 46 year old man with a 5 cm slow growing foot mass (J Orthop Surg (Hong Kong) 2019;27:2309499019828511)
Treatment
- Conservative management in asymptomatic cases
- Treatment consists of simple surgical excision
- Re-excision for local recurrences
- Wide resection may be required in recurrent cases (J Hand Surg Am 2004;29:520)
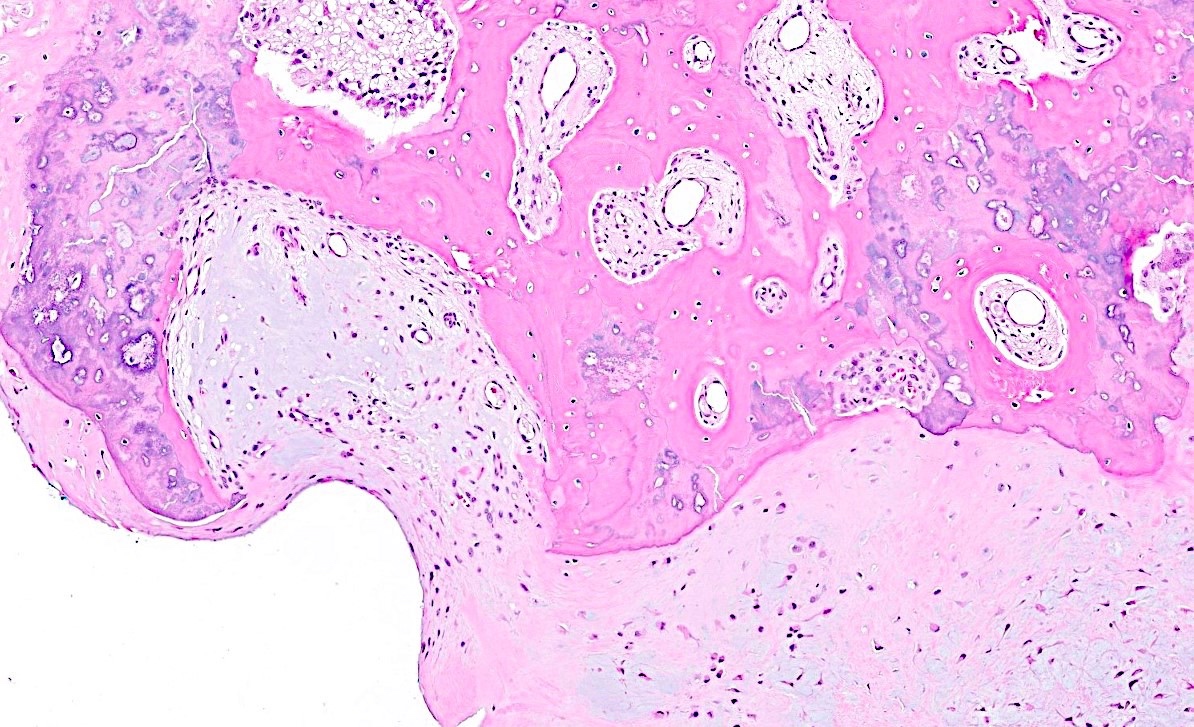
Gross description
- Exophytic bony lesion
- Bony matrix with overlying cartilage (Am J Surg Pathol 1983;7:245)
- Most tumors measure 1 - 3 cm
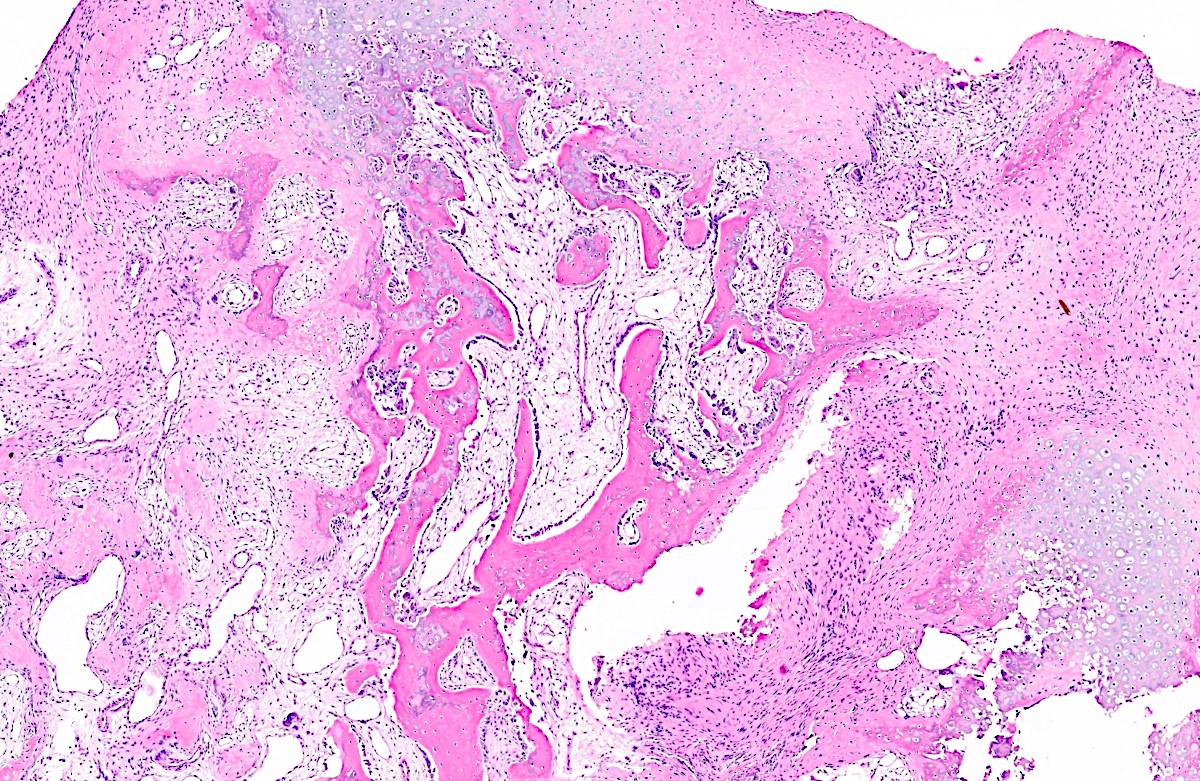
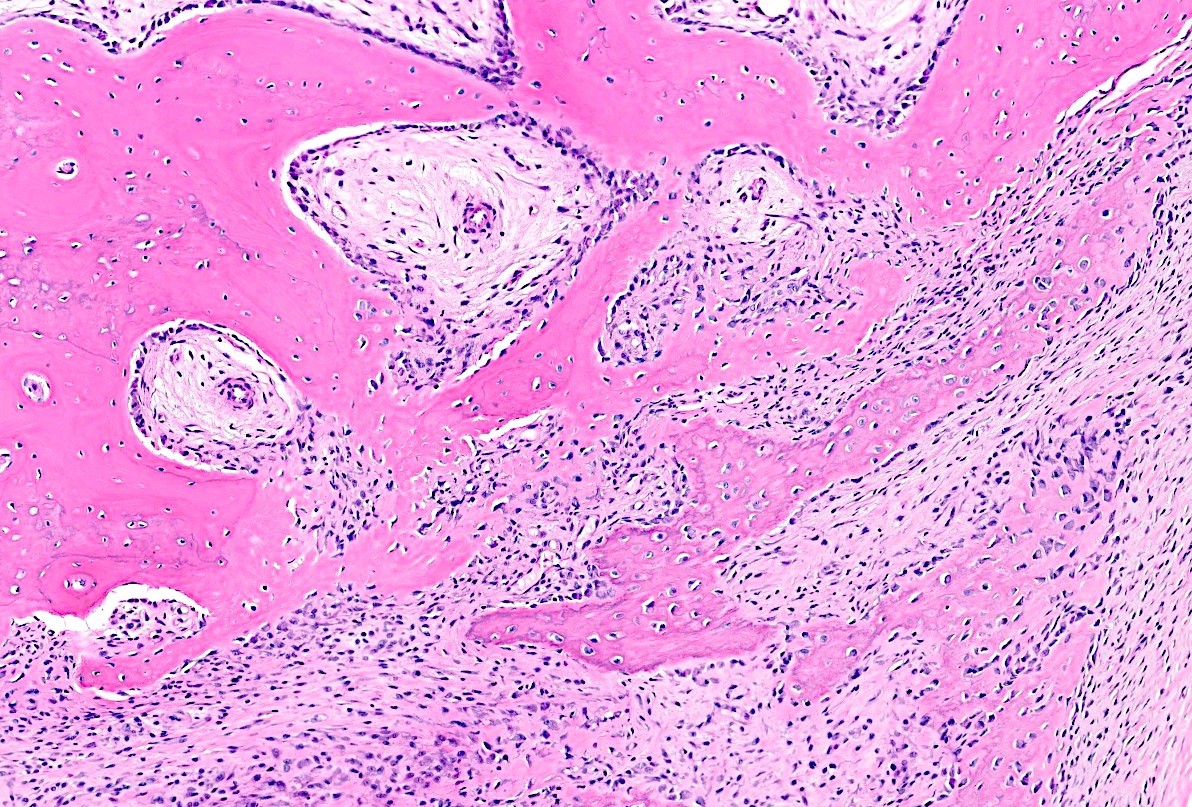
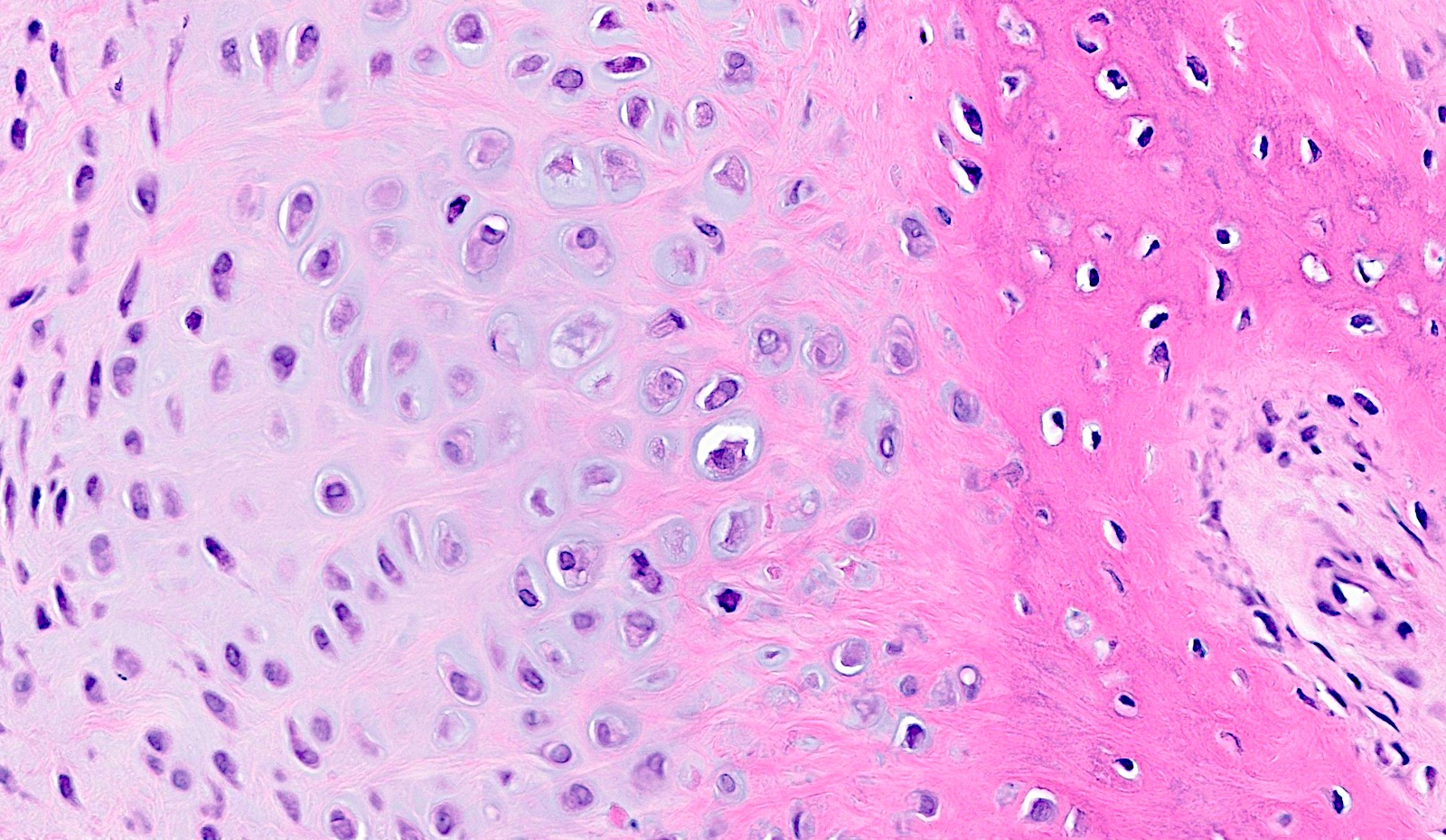
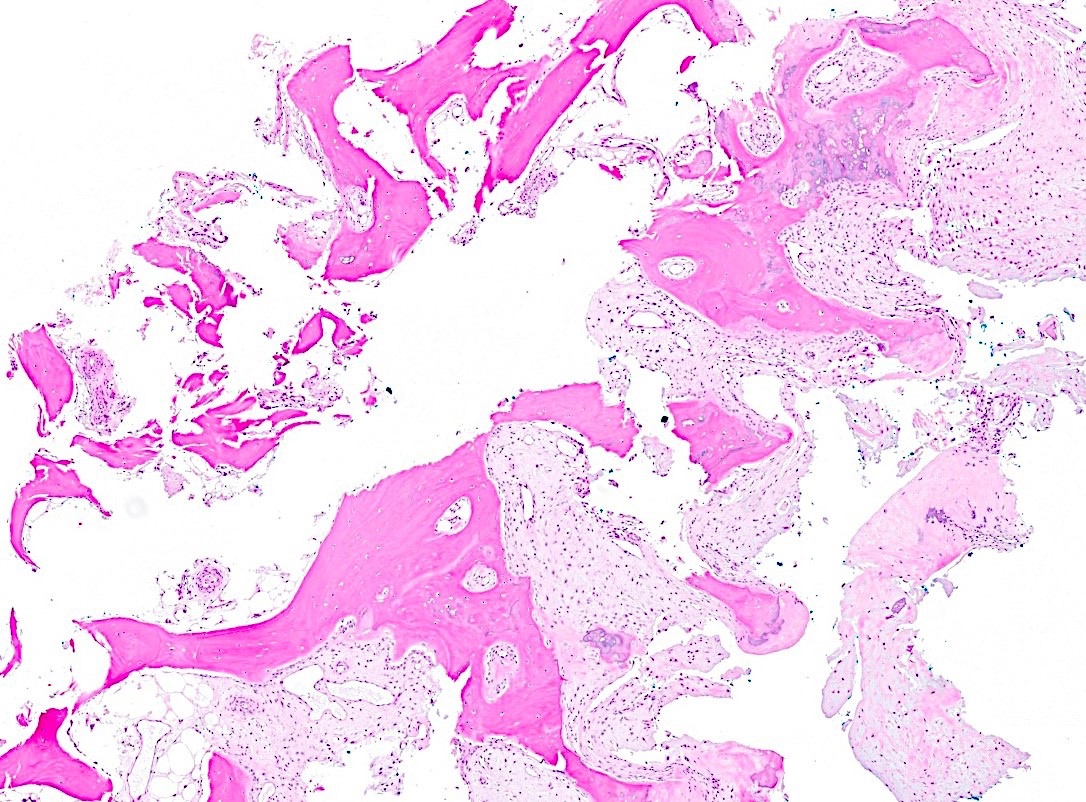
Microscopic (histologic) description
- Composed of a variable mixture of disorganized cartilage, bone and fibrous tissue
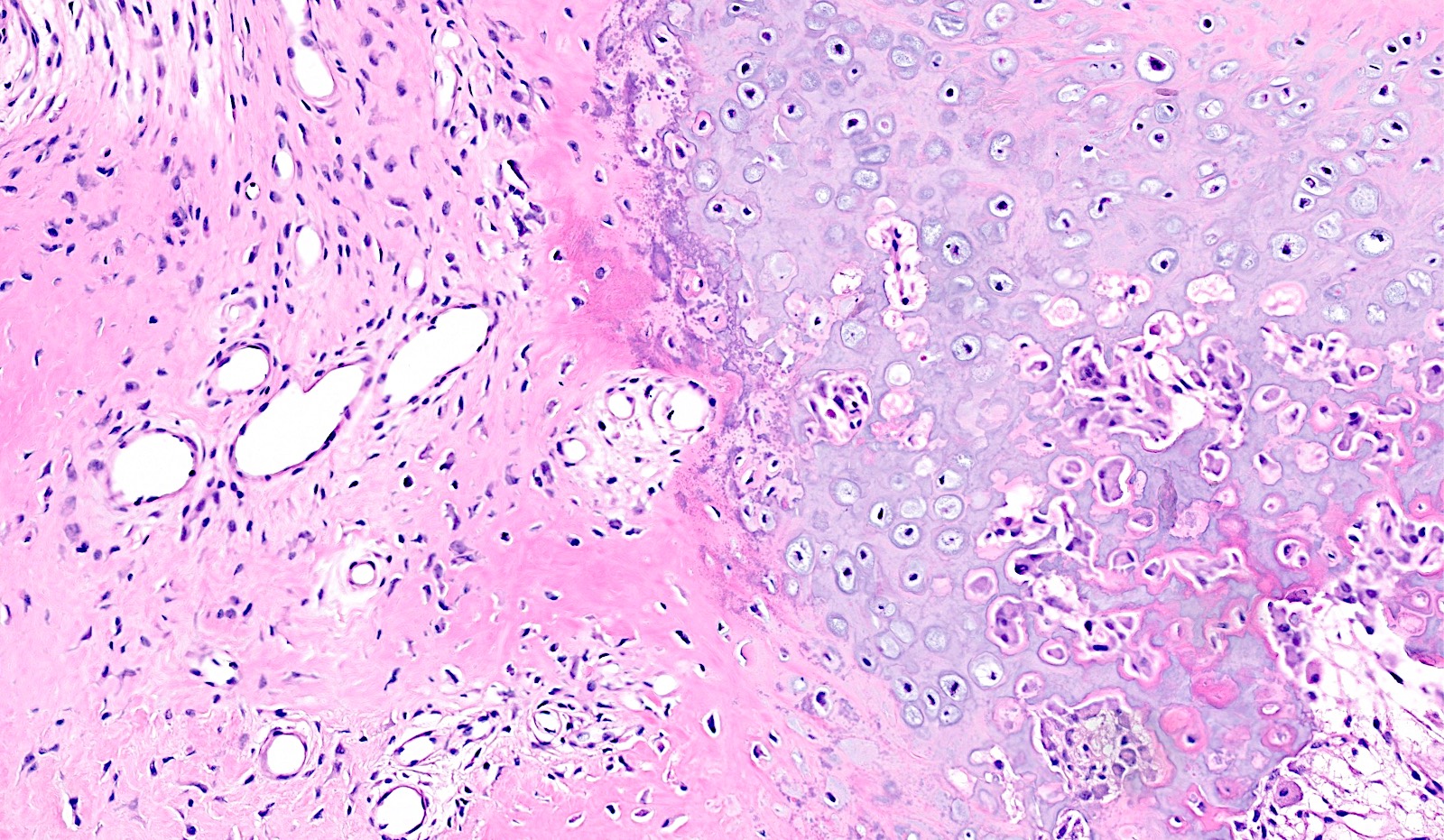
- Cartilage
- Disorganized cartilage often observed as outermost layer of BPOP
- Large, atypical chondrocytes
- Nuclei can be enlarged and binucleated
- Can be hypercellular
- Transitions to trabeculae of bone via endochondral ossification with an irregular interface
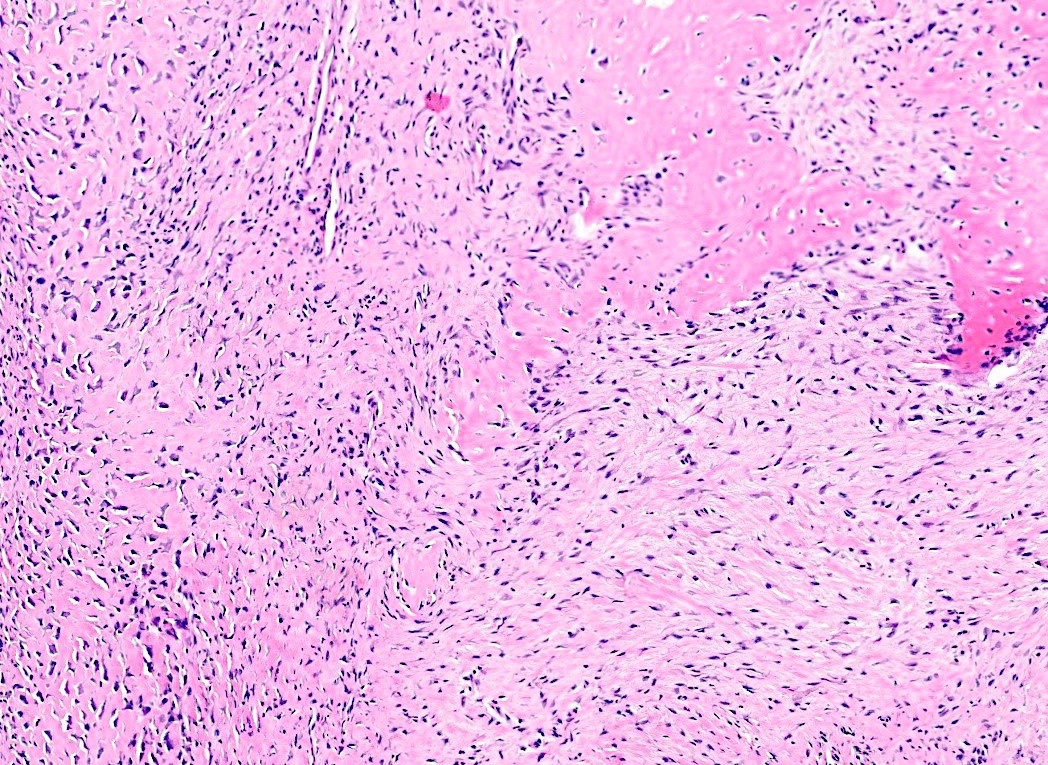
- Bone
- Benign appearing trabeculae
- Contiguous with underlying cortex
- Between cartilage and bone is characteristic basophilic stroma, so called blue bone (Am J Surg Pathol 1993;17:691, J Orthop 2018;15:138)
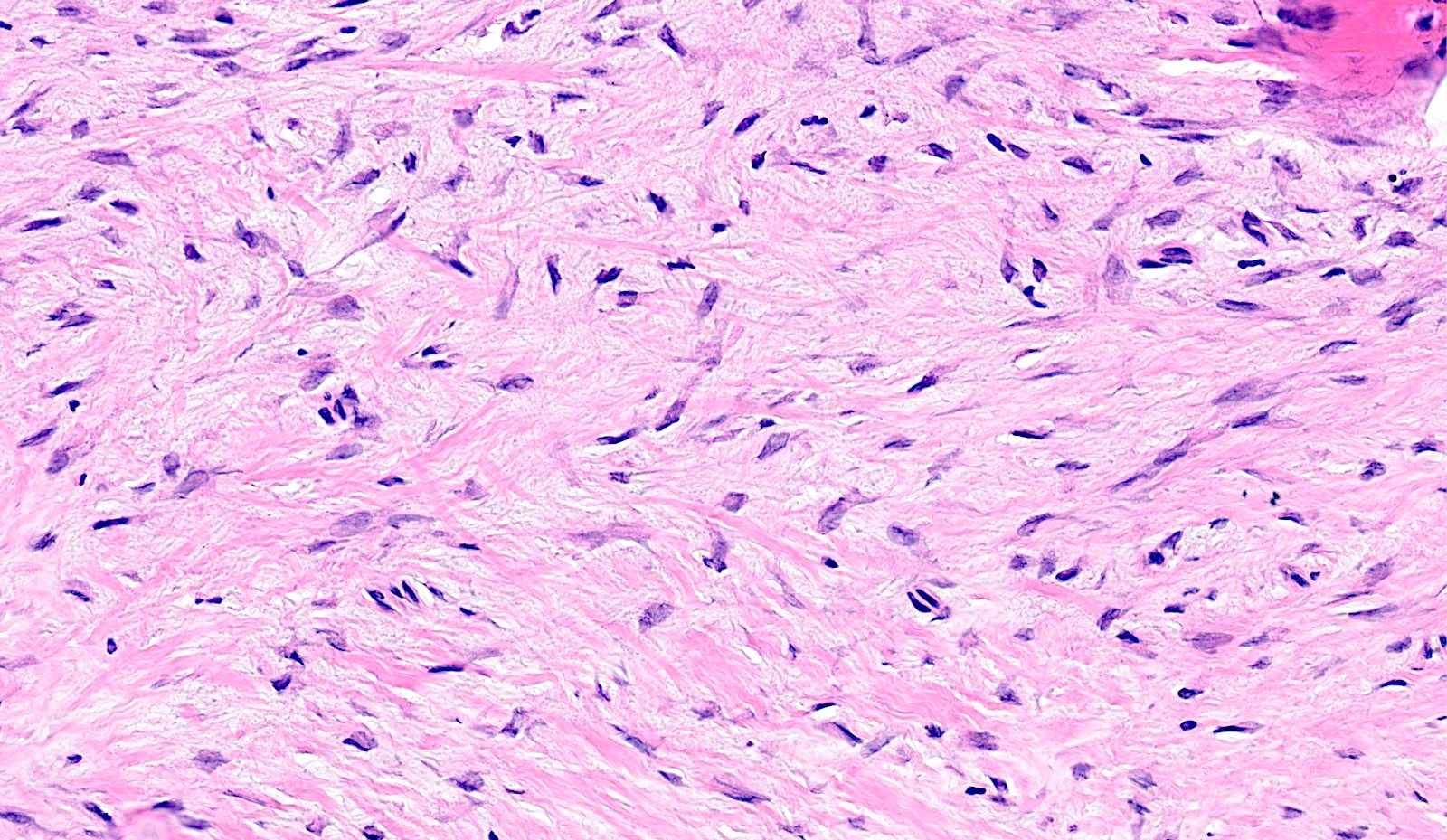
- Fibrous tissue
- Spindle to stellate shaped cells present between bony trabeculae
- Hypercellular to loosely arranged
- Minimal cytologic atypia
- No atypical mitotic figures
Microscopic (histologic) images
Cytology description
- Cellular spindle cell proliferation
- Focal calcifications
- No significant atypia (Skeletal Radiol 2001;30:282)
Positive stains
- Usually noncontributory
- CD68 can highlight scattered osteoclasts
- Safranin O is variably positive in cartilaginous areas (Hum Pathol 2002;33:1205)
Negative stains
Molecular / cytogenetics description
- Recurrent chromosomal abnormalities, including t(1;17)(q32-42;q21-23) and inv(7)(q21.1-22q31.3-32) have been reported
- Abnormalities correspond to COL1A2::LINC-PINT and COL1A1::MIR29B2CHG fusions (Mod Pathol 2023;36:100011)
- Molecular findings implicate disruption of type 1 collagen in tumorigenesis
Molecular / cytogenetics images
Videos
Nora lesion
Sample pathology report
- Bone, left ring finger, mass, excision:
- Bizarre parosteal osteochondromatous proliferation (see comment)
- Comment: Histologic sections show a well circumscribed lesion composed of an admixture of benign bone, cartilage and spindle cells. The spindle cells have focally hypercellular areas but no significant cytologic atypia. The cartilage component has atypical features with binucleated forms. There are distinct areas of basophilic stroma (blue bone) at the interface of the cartilaginous and bony elements. No atypical mitotic figures and no areas of necrosis are identified. The clinical, radiologic and histomorphologic features are consistent with the above diagnosis.
Differential diagnosis
- Florid reactive periostitis:
- Occurs most commonly in phalanges of hands and feet
- Cellular spindle cell component
- New bone formation with osteoblastic rimming
- Scant cartilaginous elements
- Myositis ossificans:
- Often associated with trauma
- Ossification progresses from periphery to center with zonal phenomenon
- Usually separated from adjacent bone but may be juxtacortical
- Fibro-osseous pseudotumor of digits:
- May harbor USP6 gene rearrangements (Ann Diagn Pathol 2018;35:53)
- Has fasciitis-like spindle cell component (Ann Diagn Pathol 2008;12:21)
- Disorganized osseous component
- Subungual exostosis:
- Composed of fibrocartilaginous tissue at the periphery
- Cartilage may look atypical
- Bone forms by endochondral ossification with irregular bone - cartilage interface
- Exclusively arises in the distal phalanx of the fingers and toes
- Commonly presents in adolescents and young adults
- Lacks both blue bone and marrow continuity
- Frequently painful
- Associated with rearrangements of COL12A1 and COL4A5 genes (Int J Cancer 2006;118:1972)
- Periosteal chondroma:
- Commonly arises from metaphysis and diaphysis of tubular bones
- May exhibit saucerization and sclerotic margination of underling cortex
- Small, lobulated tumor, usually < 5 cm in size
- Well demarcated from cortex
- Chondrocytes lack significant cytologic atypia
- Focal myxoid change may occur
- Osteochondroma:
- Most commonly occurs in long bones
- Well organized, uniform cartilaginous cap without atypia
- May be sessile or pedunculated
- Exhibits corticomedullary continuity with underlying native bone
- Fatty intertrabecular spaces are present
- No fibrous or spindle cell component
- Parosteal osteosarcoma:
- Larger lesion
- Most commonly arises in the posterior distal femur
- Atypical spindle cell component between osseous trabeculae
- May have invasion of underlying marrow cavity
- Cartilage cap often appreciated
- MDM2 amplification in a subset
- Periosteal osteosarcoma:
- Prominent periosteal reaction with sunburst or hair on end appearance
- Atypical cartilage and bone
- Most commonly occurs on diaphysis of femur and tibia
Additional references
Board review style question #1
Board review style answer #1
D. Small bones of the hand. BPOP occurs most frequently in the small bones of the hands and feet. Answers A and C are incorrect because long bones are the next most common location of BPOP. The posterior aspect of the distal femur is classic for parosteal osteosarcoma. Answer B is incorrect because it rarely occurs in the craniofacial bones.
Comment Here
Reference: Bizarre parosteal osteochondromatous proliferation
Comment Here
Reference: Bizarre parosteal osteochondromatous proliferation
Board review style question #2
A 35 year old man presents with a painless, slow growing 2.5 cm mass on the phalanx of his right middle finger. On imaging, the lesion appears to be a surface lesion, abutting the cortex of the bone without continuity with the underlying marrow cavity. Histologic sections of the excision show a circumscribed lesion composed of an admixture of benign bone, disorganized cartilage and bland spindle cells with focal areas of distinct blue bone. What is the most likely diagnosis?
- Bizarre parosteal osteochondromatous proliferation (BPOP)
- Osteochondroma
- Parosteal osteosarcoma
- Periosteal osteosarcoma
Board review style answer #2
A. Bizarre parosteal osteochondromatous proliferation (BPOP). The histologic image shows a benign appearing lesion composed of variable areas of disorganized cartilage, benign bone and bland fibrous tissue with focal areas of characteristic blue bone. These findings, together with the clinical presentation and location, are consistent with BPOP. Answer D is incorrect because periosteal osteosarcoma tends to arise in long bones and has overtly atypical and malignant bony and cartilaginous elements. Answer B is incorrect because osteochondroma has a uniform and organized cartilage cap, resembling a growth plate, as well as medullary continuity. Blue bone is not associated with osteochondroma. Answer C is incorrect because parosteal osteosarcoma is a malignant bone forming tumor that classically arises on the posterior aspect of the distal femur. It consists of trabeculae of woven bone with atypical spindle cells and rarely occurs in small bones.
Comment Here
Reference: Bizarre parosteal osteochondromatous proliferation
Comment Here
Reference: Bizarre parosteal osteochondromatous proliferation