Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Piazza Y, Kaseb H. Undifferentiated pleomorphic sarcoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/boneMFH.html. Accessed April 1st, 2025.
Definition / general
- Undifferentiated pleomorphic sarcoma (UPS) is a pleomorphic malignant neoplasm of bone lacking a distinct line of differentiation
Essential features
- Distinct clinicopathologic entity in the WHO Soft Tissue and Bone Tumours classification (5th edition)
- Mesenchymal tumor of bone
- Pleomorphic spindle shaped and epithelioid cells in a storiform or fascicular growth pattern
- No osteoid or cartilage matrix production
- No identifiable line of differentiation; diagnosis of exclusion
- Diagnosis requires correlation with clinical, radiological and pathologic findings
Terminology
- Malignant fibrous histiocytoma of bone, pleomorphic fibrosarcoma of bone
- This terminology is currently not recommended
ICD coding
Epidemiology
- Extremely rare (2 - 6% of all primary malignant bone tumors) (J Orthop Sci 2011;16:476)
- No distinct predilection for gender (Cancer 1997;79:482)
- Usually older adults (> 40 years)
Sites
- Usually unicentric (Cancer 1997;79:482)
- Long tubular bones, particularly around the knee (Cancer 1997;79:482)
- Femur is most commonly involved, followed by tibia and humerus
- Among the bones of the trunk, pelvic bones are most commonly affected
Pathophysiology
- Shows many diverse genetic alterations and chromosomal structural aberrations
- Chromosomal gains are more common than losses (Semin Diagn Pathol 2021;38:163)
- Chromosomal losses of 8p, 9p, 10, 13q and 18q and gains of 4q, 5p, 6p, 7p, 8q, 12p, 14q, 17q, 19p, 20q, 22q and X have been reported
- Loss of heterozygosity in multiple genes has been reported, including
- CDKN2A, RB1, TP53 and ING1 (Genes Chromosomes Cancer 2011;50:291)
- Mutations in TP53 (~30%) or chromatin remodeling genes (~40%) including ATRX, DOT1L and H3F3A are most frequent (J Pathol 2019;247:166)
Etiology
- Largely unclear and unknown
- First described in 1972 by Frieda Feldman and David Norman (Radiology 1972;104:497)
- Most cases are de novo (primary) (Semin Diagn Pathol 2021;38:163, Cancer 1997;79:482)
- Secondary (nearly 30% of cases)
- Some cases arise from preexisting bone disease
- Bone infarct, Paget disease
- Prior irradiation in the field of the affected bone
- Rare cases were associated with metallic prosthesis or hardware
- Some cases associated with hereditary diaphyseal medullary stenosis (Hardcastle syndrome)
- Some cases arise from preexisting bone disease
Clinical features
- Depends on location
- Knee pain or swelling or mass
- May present with pathologic fracture (Semin Diagn Pathol 2021;38:163, Skeletal Radiol 2021;50:1491)
- Metastases
- Pulmonary metastases are common (Cancer 1997;79:482)
- Occurs in 35 - 50% of undifferentiated pleomorphic sarcoma of bone cases
- TNM staging of bone tumors
Diagnosis
- Diagnosis requires correlation with clinical, radiological and pathologic findings
- Pathologic findings
- Pleomorphic spindle shaped and epithelioid cells in a storiform or fascicular growth pattern
- No osteoid or cartilage matrix production
- No identifiable line of differentiation; diagnosis of exclusion
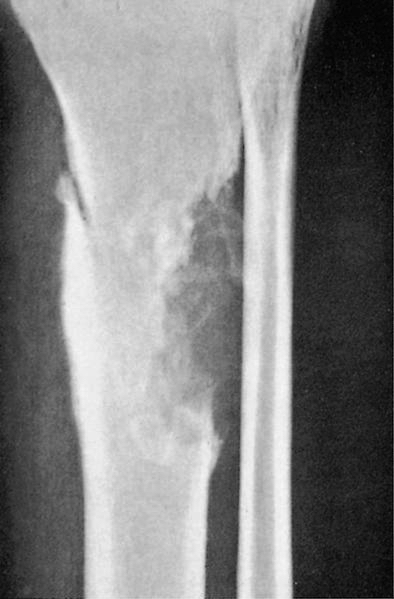
Radiology description
- Radiological features are nonspecific but the majority of cases demonstrate an aggressive osteolytic neoplasm with ill defined margins, cortical destruction, an associated soft tissue mass and pathologic fracture (Skeletal Radiol 2021;50:1491)
- On magnetic resonance imaging (MRI), the tumor is heterogeneous on T1 and T2 weighted images (Semin Diagn Pathol 2021;38:163)
- Tumors are usually centered in the metadiaphyseal region of long bones and occasionally extend into the epiphysis
Radiology images
Prognostic factors
- Depends on staging
- Overall, 5 year and 10 year survival rates of 38.3% and 30.5%, respectively (J Surg Oncol 2020;121:1097)
- Localized disease tends to have a favorable prognosis
- Secondary undifferentiated pleomorphic sarcoma and metastatic disease are associated with a poorer prognosis
Case reports
- 40 year old man with avascular necrosis of the femur secondary to sickle cell disease further developed into undifferentiated pleomorphic sarcoma (Int J Surg Case Rep 2020:77:243)
- 76 year old man treated with unresectable undifferentiated pleomorphic sarcoma treated with carbon ion radiotherapy (J Rural Med 2022;17:176)
- 77 year old woman with undifferentiated pleomorphic sarcoma presented with cardiac tamponade (J Investig Med High Impact Case Rep 2022:10:23247096221141190)
Treatment
- Radical surgery with adjuvant chemotherapy
- Radiotherapy for unresectable tumors
Gross description
- Tumor is usually centered in the medullary cavity (Semin Diagn Pathol 2021;38:163)
- Tumor grows with a permeative pattern, encasing preexisting bony trabecula (Semin Diagn Pathol 2021;38:163)
- Variable color (white-gray, tan-yellow and tan-brown)
- Typically shows cortical bone destruction and soft tissue mass
- Areas of necrosis and hemorrhage
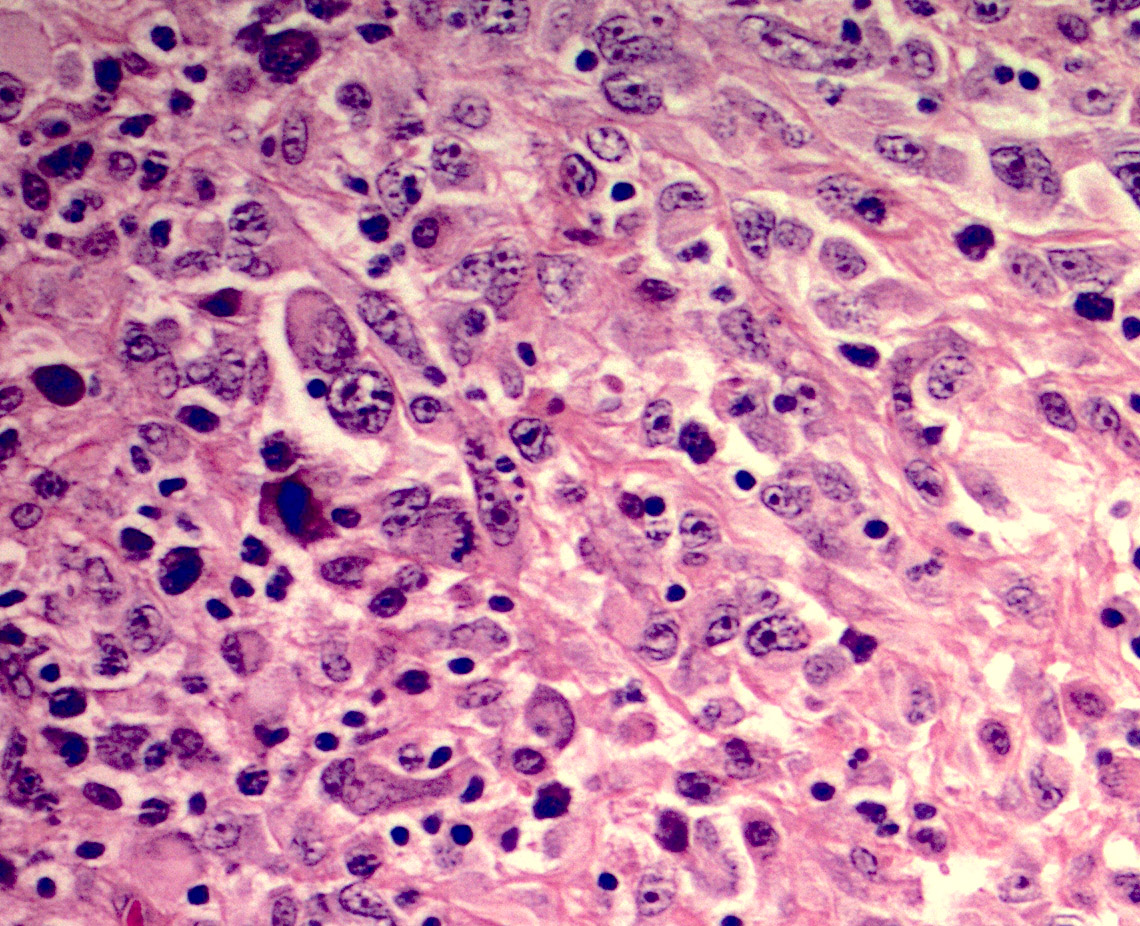
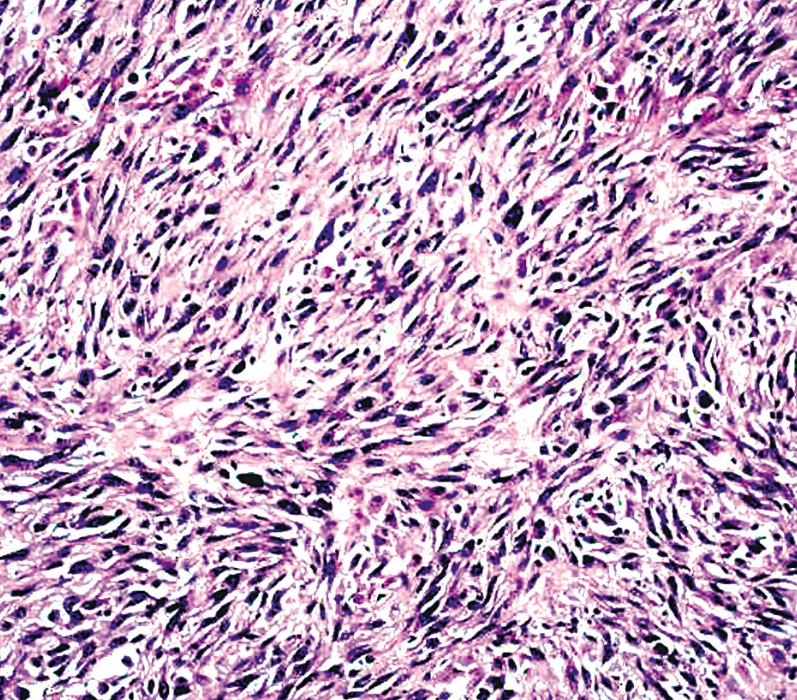
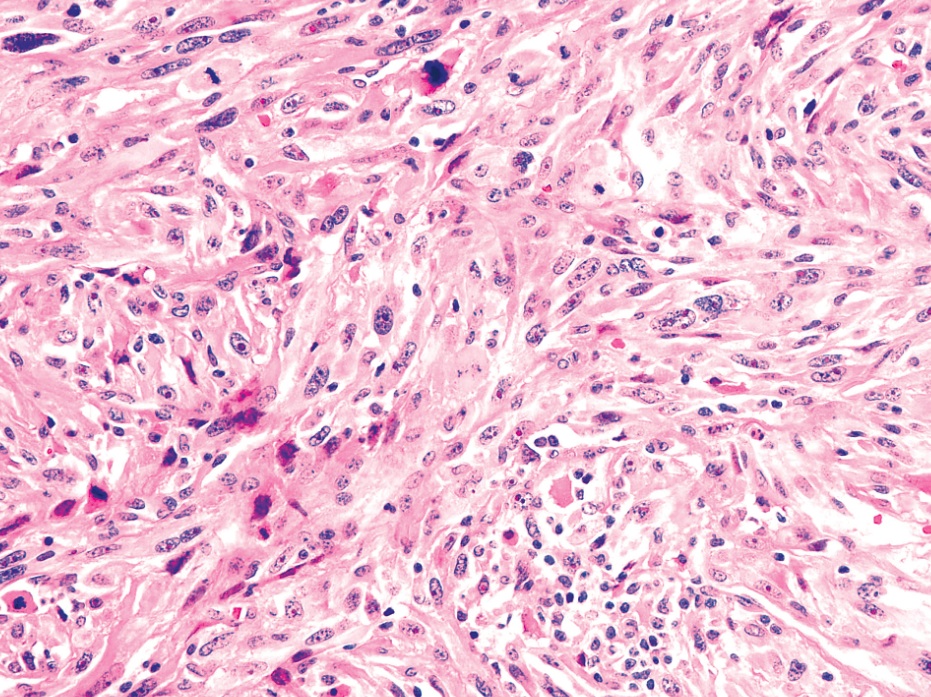
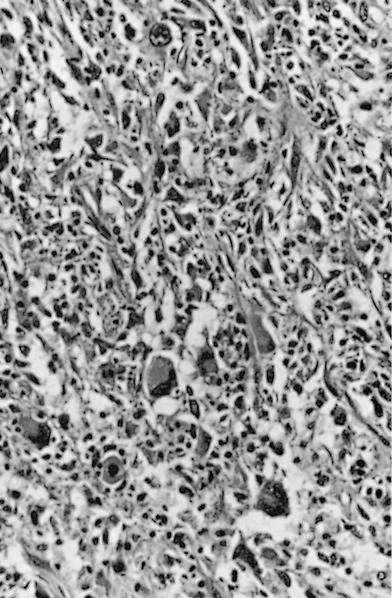
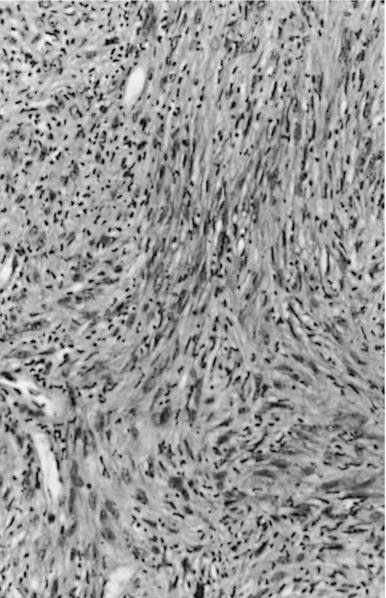
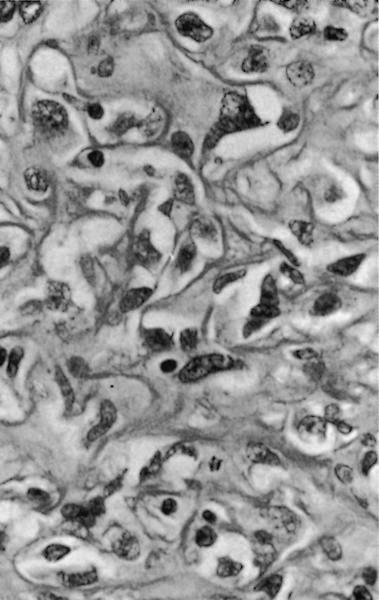
Microscopic (histologic) description
- Usually hypercellular and composed of spindle shaped, epithelioid or polygonal cells with marked pleomorphism arranged in a haphazard, storiform and fascicular growth pattern
- Storiform pattern is the most common pattern (Cancer 1997;79:482)
- Background could be hyalinized with some inflammatory cells
- No osteoid or cartilaginous matrix
- Usually atypical mitotic figures and necrosis is present
- Considered a grade 3 sarcoma and is distinguished from grade 2 adult type fibrosarcoma by the significantly greater degree of atypia and architectural arrangement (Semin Diagn Pathol 2021;38:163)
Microscopic (histologic) images
Positive stains
Negative stains
- Negative for all distinct lineage markers
- Variable (Semin Diagn Pathol 2021;38:163)
Sample pathology report
- Bone, right distal femur, radical resection (status postneoadjuvant chemotherapy):
- Residual undifferentiated pleomorphic sarcoma of bone (see synoptic report)
- Synoptic report
- Tumor size: 11.3 x 8.0 x 8.0 cm
- Tumor location: right distal femur
- Percent treatment response: ~80% (~20% residual viable tumor)
- Discontinuous tumor foci: not identified
- Lymphovascular invasion: not identified
- Surgical margins: negative for tumor
- Lymph nodes: 1 benign lymph node (0/1)
- Additional findings: biopsy site
- Stage (AJCC, 8th edition): ypT2 ypN0
Differential diagnosis
- High grade sarcomas:
- Osteosarcoma:
- Typically shows osteoid matrix and positive SATB2
- Leiomyosarcoma:
- Some areas could show fascicles of spindled cells
- SMA positivity with an additional myogenic marker
- Rhabdomyosarcoma:
- Synovial sarcoma:
- Morphology consistent with monophasisc or biphasic could be helpful for differentiation
- Harbors t(X;18)(p11;q11) SYT::SSX fusion
- Osteosarcoma:
- Metastatic sarcomatoid carcinoma:
- Typically has a different clinical presentation
- Usually partially / diffusely CK positive
- Metastatic carcinoma:
- Metastatic melanoma:
- Dedifferentiated chondrosarcoma:
- Usually shows IDH1 or IDH2 mutations (Hum Pathol 2017:65:239)
- Usually shows a well differentiated cartilaginous component
- Shows some distinct clinical, radiologic and pathologic features
- Fibrous dysplasia:
- Caused by mutations in GNAS gene
Additional references
Board review style question #1
Board review style answer #1
E. Vimentin. The only stain that is usually positive in undifferentiated pleomorphic sarcoma of bone is vimentin. Answers A - D are incorrect because CD31, desmin, myogenin and SATB2 are usually negative or show focal positivity in this tumor.
Comment Here
Reference: Undifferentiated pleomorphic sarcoma
Comment Here
Reference: Undifferentiated pleomorphic sarcoma
Board review style question #2
Which of the following risk factors has been associated with undifferentiated pleomorphic sarcoma of bone?
- Diaphyseal medullary stenosis
- Ethnic origin
- Increased alcohol consumption
- Nonmetallic prosthesis or hardware
- Smoking
Board review style answer #2
A. Diaphyseal medullary stenosis. Diaphyseal medullary stenosis has been shown to be associated with undifferentiated pleomorphic sarcoma of bone. Answers B - E are incorrect because all of these other risk factors have not been shown to be associated with undifferentiated pleomorphic sarcoma of bone.
Comment Here
Reference: Undifferentiated pleomorphic sarcoma
Comment Here
Reference: Undifferentiated pleomorphic sarcoma