Table of Contents
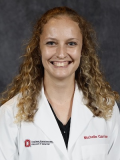
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Garrison M, Zynger DL. Urethral carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/bladderurethralcarcinoma.html. Accessed January 18th, 2025.
Definition / general
- Primary urethral carcinoma is a rare but aggressive genitourinary malignancy that leads to urethral obstruction (Res Rep Urol 2021;13:325)
Essential features
- Primary urethral carcinoma is rare with diverse tumor histology
- Nonspecific clinical findings and lack of screening techniques often lead to late detection and poor prognosis
Terminology
- Urothelial carcinoma
- Squamous cell carcinoma
- Adenocarcinoma of the urethra
ICD coding
- ICD-O: 8140/3 - carcinoma of Littré glands
- ICD-10: C68.0 - malignant neoplasm of urethra
- ICD-11
- 2C93 - malignant neoplasms of urethra or paraurethral gland
- 2C93.0 & XH22Z8 - adenocarcinoma of urethra or paraurethral gland & carcinoma of Skene, Cowper and Littré glands
Epidemiology
- From 2004 to 2016, 436 - 622 new cases of primary urethral carcinoma were diagnosed each year (Cancer Causes Control 2021;32:627)
- Men (68 - 71%) > women (29 - 32%) (Hum Pathol 2018;72:35, World J Urol 2016;34:97, Cancer Causes Control 2021;32:627)
- Median age of diagnosis among men and women is 61 - 71 years old (Hum Pathol 2018;72:35, World J Urol 2016;34:97, Clin Genitourin Cancer 2018;16:e1003, Int J Surg Pathol 2022;30:15, J Surg Oncol 2022;125:907)
- 46% of all patients (male and female) were age 75 or older, 42% were 55 - 74 and 12% were 54 or younger (Cancer Causes Control 2021;32:627)
- Incidence rate highest in Black populations (3.33), followed by White populations (1.72), other race groups (1.57) and Hispanic populations (1.57) (Cancer Causes Control 2021;32:627)
- Race reported as 71% for White population, 16% Black population, 7% Hispanic population and 5% other (Cancer Causes Control 2021;32:627)
- Higher proportion in Black women (12% male, 26% female) (Cancer Causes Control 2021;32:627)
- Overall, urothelial carcinoma is the most common histological subtype (53%), followed by squamous cell carcinoma (24%), adenocarcinoma (15%) and other (9%) (Cancer Causes Control 2021;32:627)
- Men: urothelial (39 - 64%), squamous cell carcinoma (24 - 54%), adenocarcinoma (9%) and other (4%) (Actas Urol Esp (Engl Ed) 2022;46:70, Cancer Causes Control 2021;32:627)
- Women: urothelial (29 - 45%), squamous cell carcinoma (19 - 25%), adenocarcinoma (27 - 40%) and other (7 - 19%) (Cancer Causes Control 2021;32:627, World J Urol 2013;31:147, J Surg Oncol 2022;125:907)
- One study proposed classification of a new hybrid tumor with both urothelial and squamous features, a basaloid appearance and expression and frequent identification of p16 or HPV18 as the overwhelming histology (82%) in the urethra for both men and women (Hum Pathol 2018;72:35)
Sites
- Men (among all histologic subtypes) (World J Urol 2016;34:97)
- Proximal (prostatic + membranous) urethra only: 54%
- Distal (penile) urethra only: 36%
- Proximal + distal urethra: 10%
- Women (among all histologic subtypes) (Clin Genitourin Cancer 2018;16:e1003, World J Urol 2016;34:97)
- Proximal urethra only: 29 - 44%
- Distal urethra only: 21 - 69%
- Proximal + distal urethra: 2 - 33%
Etiology
- Chronic inflammation and irritation of the urinary tract are risk factors for the development of primary urethral carcinoma
- Men: history of sexually transmitted infections (HPV16), urethral stricture, intermittent catheterization and history of radiation therapy (Hum Pathol 2022;129:71)
- Women: recurrent urinary tract infections and urethral diverticula (Clin Genitourin Cancer 2018;16:e1003)
- 77% of patients with urothelial carcinoma of the urethra had a prior history of urothelial carcinoma of the bladder (Int J Surg Pathol 2022;30:15)
Clinical features
- Common presenting features include mass lesion (75 - 79%), urethral narrowing (20%) obstructive urinary tract symptoms (82%) and hematuria (67%) (Hum Pathol 2018;72:35, Clin Genitourin Cancer 2018;16:e1003)
- Among men with bulbar and penile urethral carcinoma, 46% presented with urethral abscess (Actas Urol Esp (Engl Ed) 2022;46:70)
- Inguinal lymph nodes are the most common regional metastatic site (Hum Pathol 2018;72:35)
- Liver and lung are the most frequent distant metastatic sites (Hum Pathol 2018;72:35)
Diagnosis
- Physical examination for suspicious masses or indurations through palpation of external genitalia (Eur Urol 2013;64:823)
- Bilateral inguinal lymph node palpation to assess for the presence of enlarged lymph nodes (Eur Urol 2013;64:823)
- Role of urinary cytology limited due to varying sensitivity (Eur Urol 2013;64:823)
- Urethrocytoscopy with biopsy is diagnostic (Eur Urol 2013;64:823)
Radiology description
- Magnetic resonance imaging (MRI) visualized all tumors in one study with appearance as intermediate signal intensity on T2 imaging (Hum Pathol 2018;72:35)
Radiology images
Prognostic factors
- Staging is based on TNM, refer to links for the current system for women and men
- Recurrence rate of 53% for urethral carcinoma (World J Urol 2016;34:97)
- Pathologically advanced (pT3 or greater), pathologically or clinically node positive disease and proximal tumor location associated with recurrence (World J Urol 2016;34:97)
- Most common sites of recurrence were lymph nodes (12%) and urethra (18%) (World J Urol 2016;34:97)
- Clinical nodal assessment 93% accurate in predicting pathological lymph node involvement (World J Urol 2016;34:97)
- Median survival of 21 months (mean of 39 months) and 10 year survival of 25% for surgical patients (Hum Pathol 2018;72:35)
- Among patients without metastatic disease that underwent radical urethrectomy, 5 year cancer specific mortality free survival was 62% (87% for those with 36 month disease free interval) (J Surg Oncol 2024;129:1348)
- 5 year survival for T3 - 4 N0 - 2 patients was 54% (84% for those with 36 month disease free interval)
- Urothelial carcinoma
- 1 year overall survival rate of 73%; 3 year overall survival rate of 33% (Int J Surg Pathol 2022;30:15)
- Previous history of urothelial carcinoma of the bladder confers no effect on overall survival (Int J Surg Pathol 2022;30:15)
- Men
- Bulbar or penile urethral carcinoma (all histologic subtypes) yielded a mean 5 year overall survival of 50%, cancer specific survival 66% and relapse free survival of 58%; 62% with recurrence after surgery after a median of 6.3 months (Actas Urol Esp (Engl Ed) 2022;46:70)
- Proximal squamous cell carcinoma confers poor survival outcomes with a mean survival of 14 months and 90% develop distant metastatic disease (Eur Urol Focus 2021;7:163)
- Women
- Median overall survival (all histologic subtypes): 70 months (J Surg Oncol 2022;125:907)
- 5 year survival: 67% for stage 0 - II, 53% for stage III and 17% for stage IV (World J Urol 2013;31:147)
- Node positive and tumor size of ≥ 3 cm confer worse overall survival (J Surg Oncol 2022;125:907)
- 5 year survival: adenocarcinoma (31%), urothelial carcinoma (61%) and squamous cell carcinoma (64%) (World J Urol 2013;31:147)
- Advanced disease present: adenocarcinoma (65%), urothelial carcinoma (32%) and squamous cell carcinoma (53%) (World J Urol 2013;31:147)
Case reports
- 54 year old man with low grade papillary tumor of the anterior urethra (Ann Med Surg (Lond) 2022;76:103561)
- 67 year old woman with primary clear cell adenocarcinoma of the urethra (BMC Womens Health 2022;22:251)
- 68 year old man with urethral bulbar carcinoma with mixed urothelial and squamous differentiation (Mol Clin Oncol 2022;17:142)
- 76 year old woman with urothelial carcinoma with squamous metaplasia (Int J Surg Case Rep 2023;109:108505)
Treatment
- Among all patients with primary urethral carcinoma, rates of treatment with adjuvant radiotherapy and chemotherapy have increased over time (World J Urol 2013;31:147)
- Adjuvant radiotherapy: 28% of patients from 1989 to 1998; 43% from 1999 to 2008
- Adjuvant chemotherapy: 4% from 1989 to 1998; 12% from 1999 to 2008
- Men
- Locally advanced disease or metastasis: neoadjuvant therapy often recommended before surgical resection (Eur Urol Focus 2021;7:163)
- Distal (penile and bulbar carcinoma): partial penectomy (8 - 75%), total penectomy (17 - 54%) and transurethral resection (8 - 38%) (Int J Urol 2006;13:716, Actas Urol Esp (Engl Ed) 2022;46:70)
- Proximal: total penectomy (41%) and radical cystectomy / total penectomy with ileal conduit (59%) (Int J Urol 2006;13:716)
- Proximal squamous cell carcinoma: panurethrectomy (80%) and radical prostatectomy (20%) (Eur Urol Focus 2021;7:163)
- Women
- Among all histologic subtypes: 43% surgery alone, 16% radiotherapy alone and 22% surgery and radiotherapy (World J Urol 2013;31:147)
- T1 or Tis: 30% were treated with cystourethrectomy, 40% underwent local excision and 30% received chemotherapy and radiation (Clin Genitourin Cancer 2018;16:e1003)
- Locally advanced, nonmetastatic disease: 52% received multimodal therapy (radical cystourethrectomy, lymph node dissection and chemotherapy or radiation) and 48% received nonmultimodal therapy (radical cystourethrectomy alone, local excision with or without additional therapy or chemotherapy with or without radiation therapy), with no difference in survival (Clin Genitourin Cancer 2018;16:e1003)
Clinical images
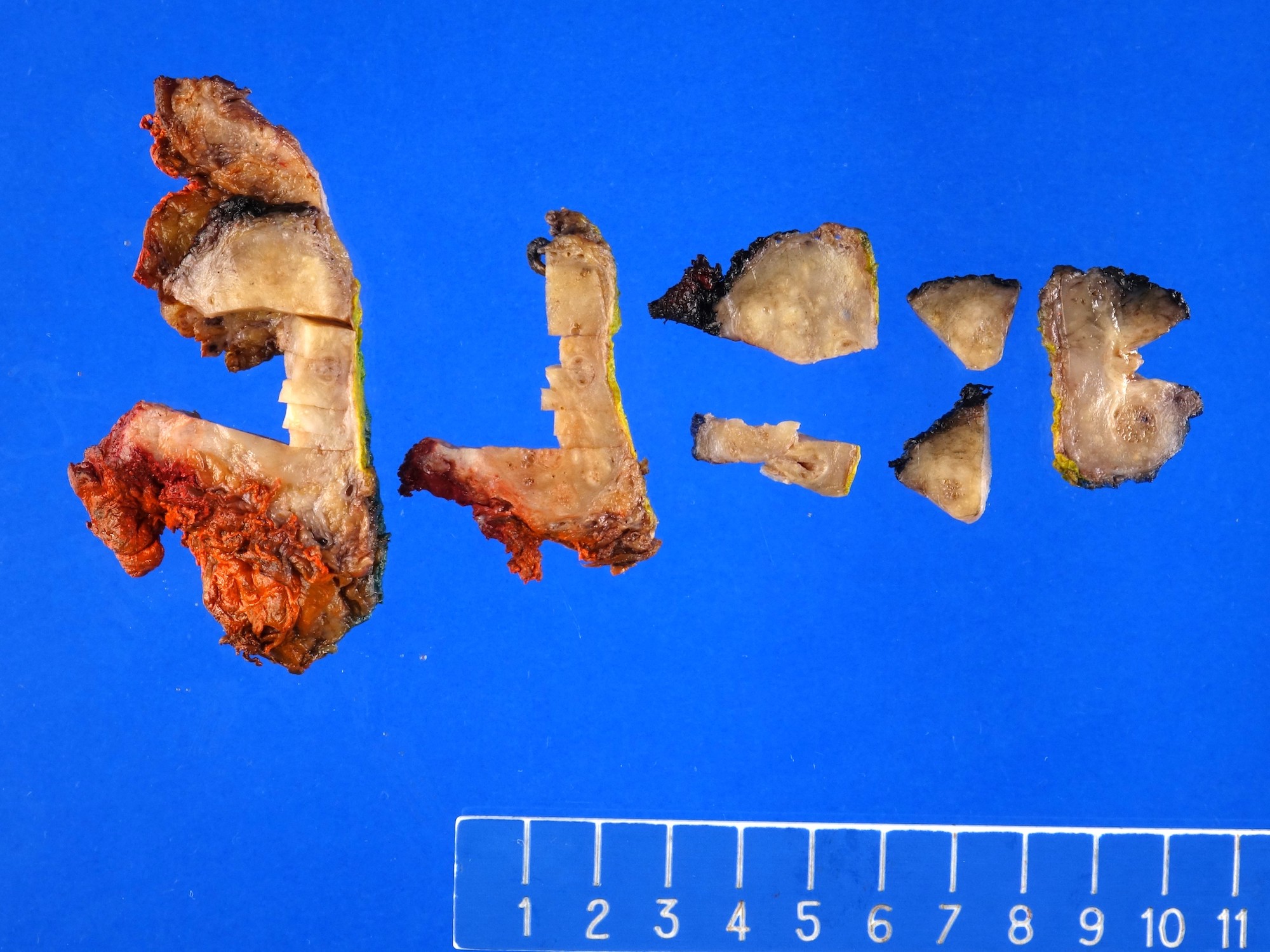
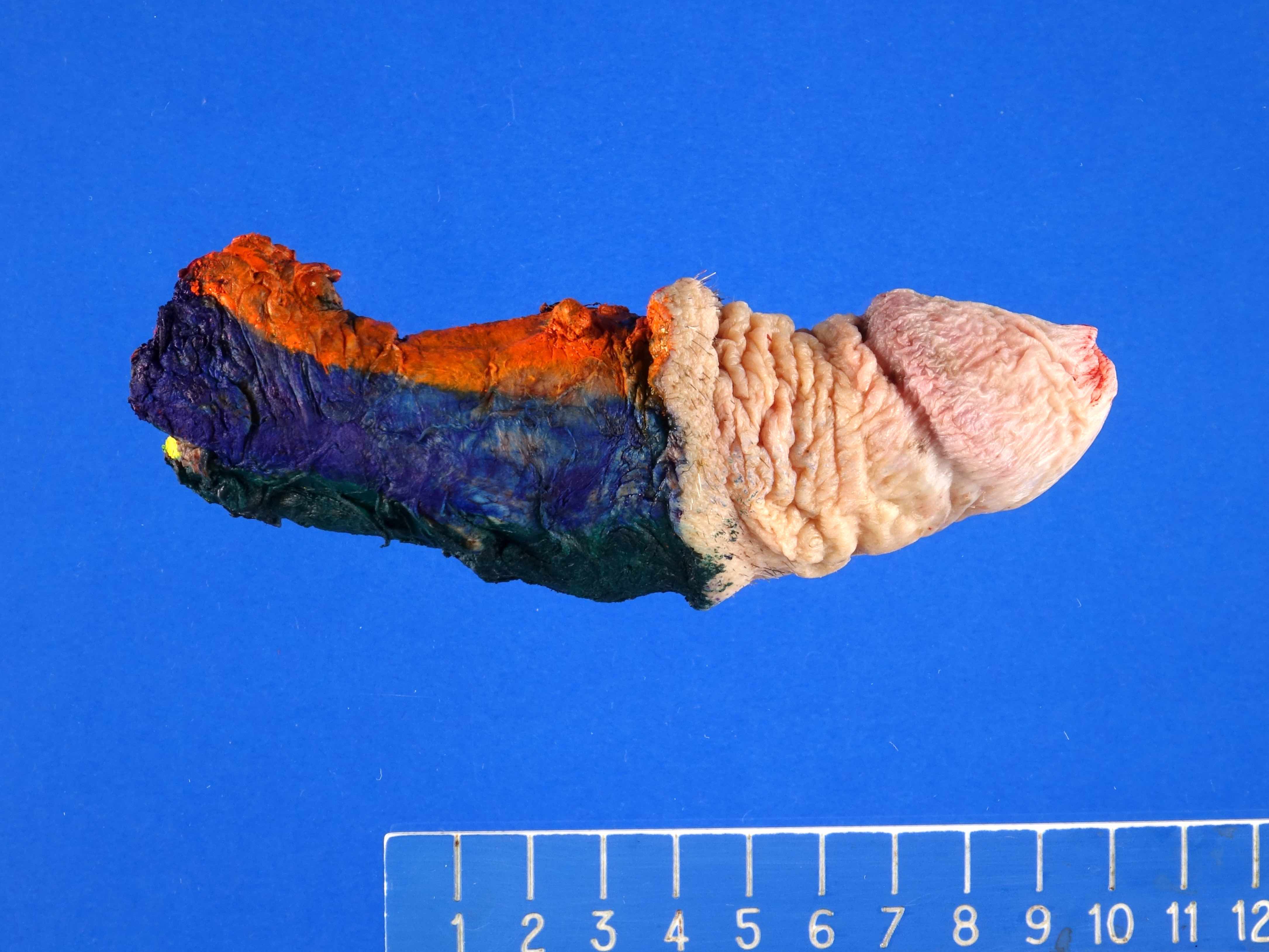
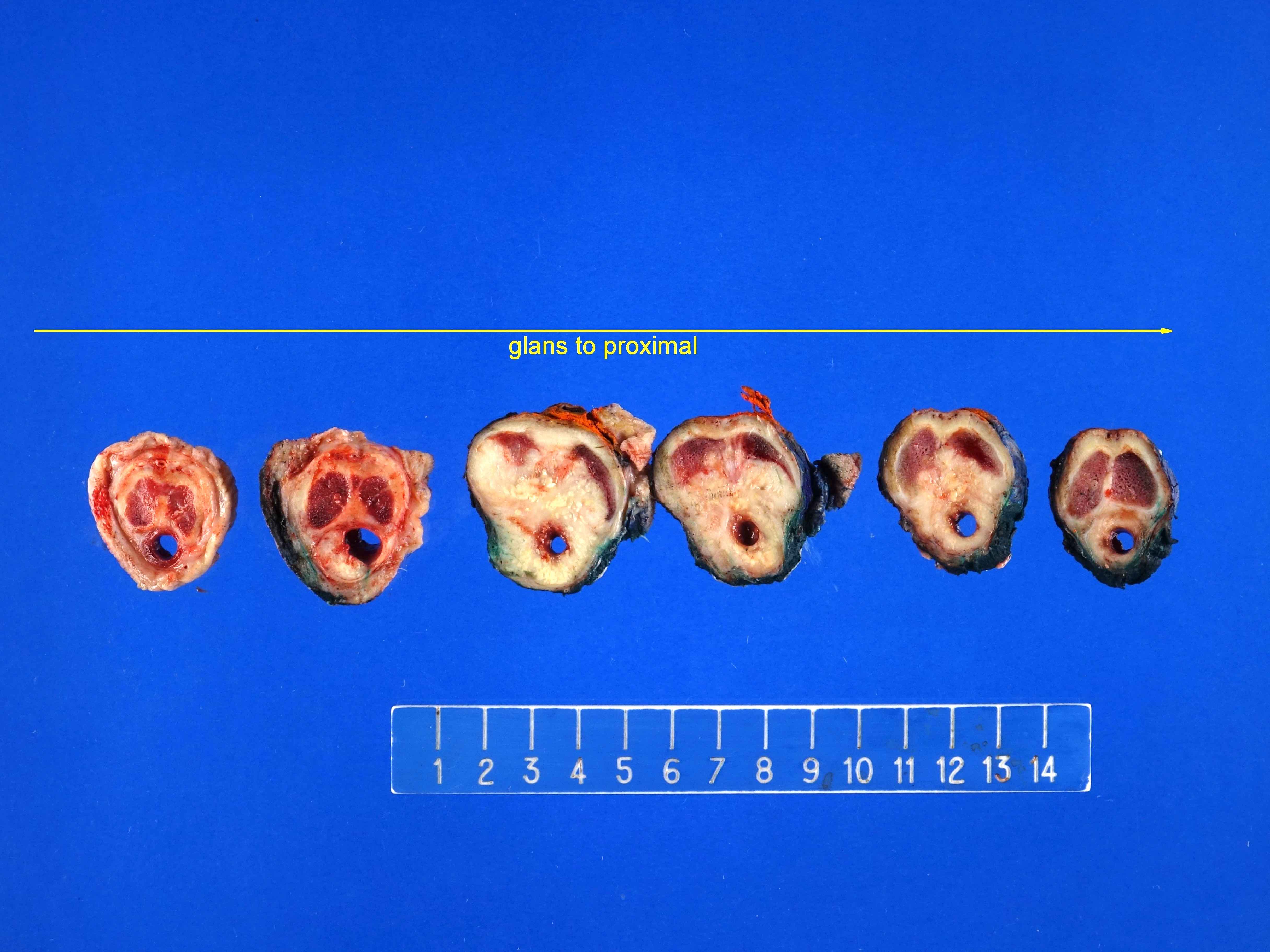
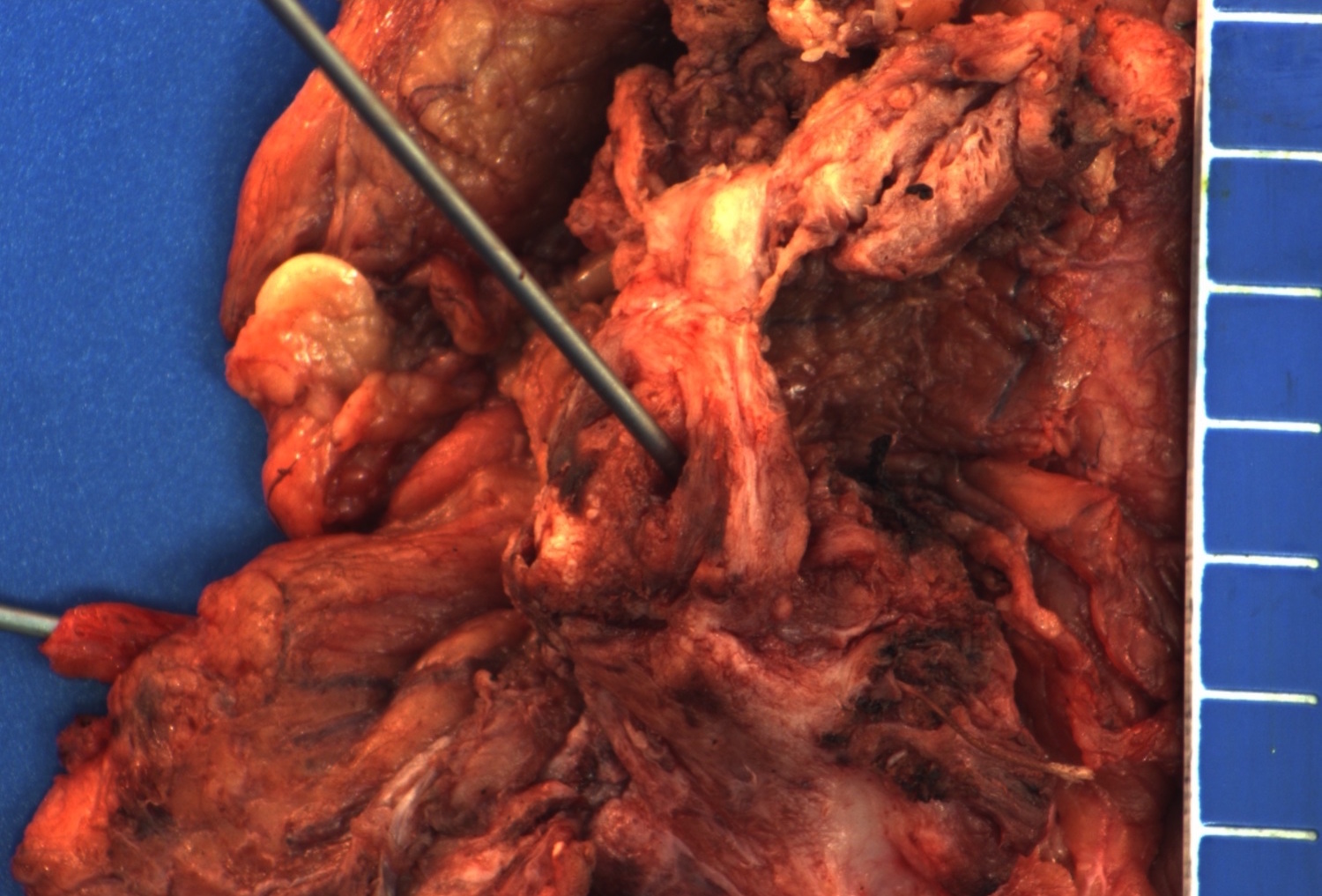
Gross description
- Poorly circumscribed mass with white to yellow-tan appearance (Hum Pathol 2018;72:35)
- Mean size: 3.7 cm (range: 0.5 - 6 cm) (Hum Pathol 2018;72:35)
- Range of appearances
- Fungated mass with protrusion to urethral lumen
- Flat lesions with invasion of surrounding tissue (Hum Pathol 2018;72:35)
Gross images
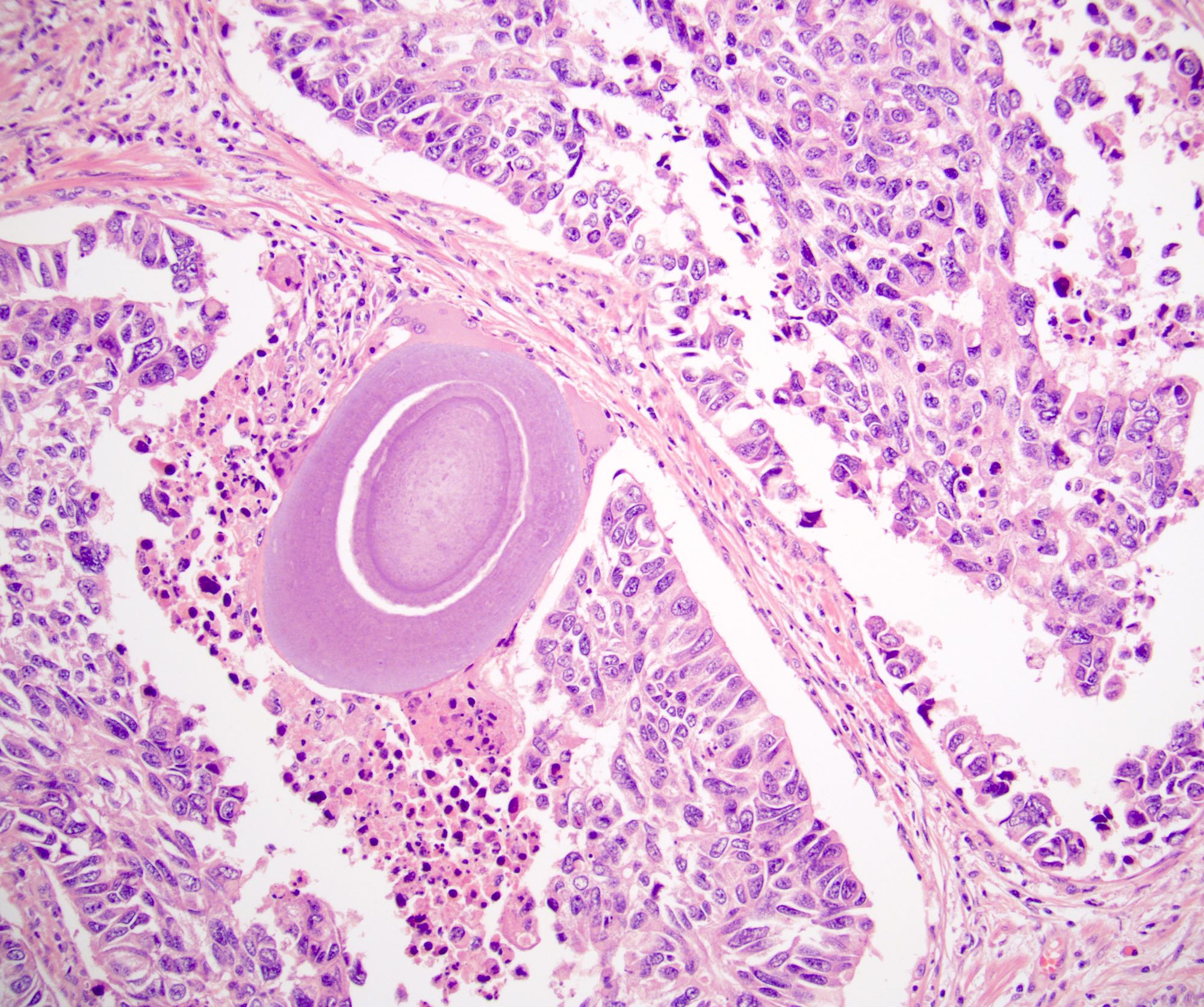
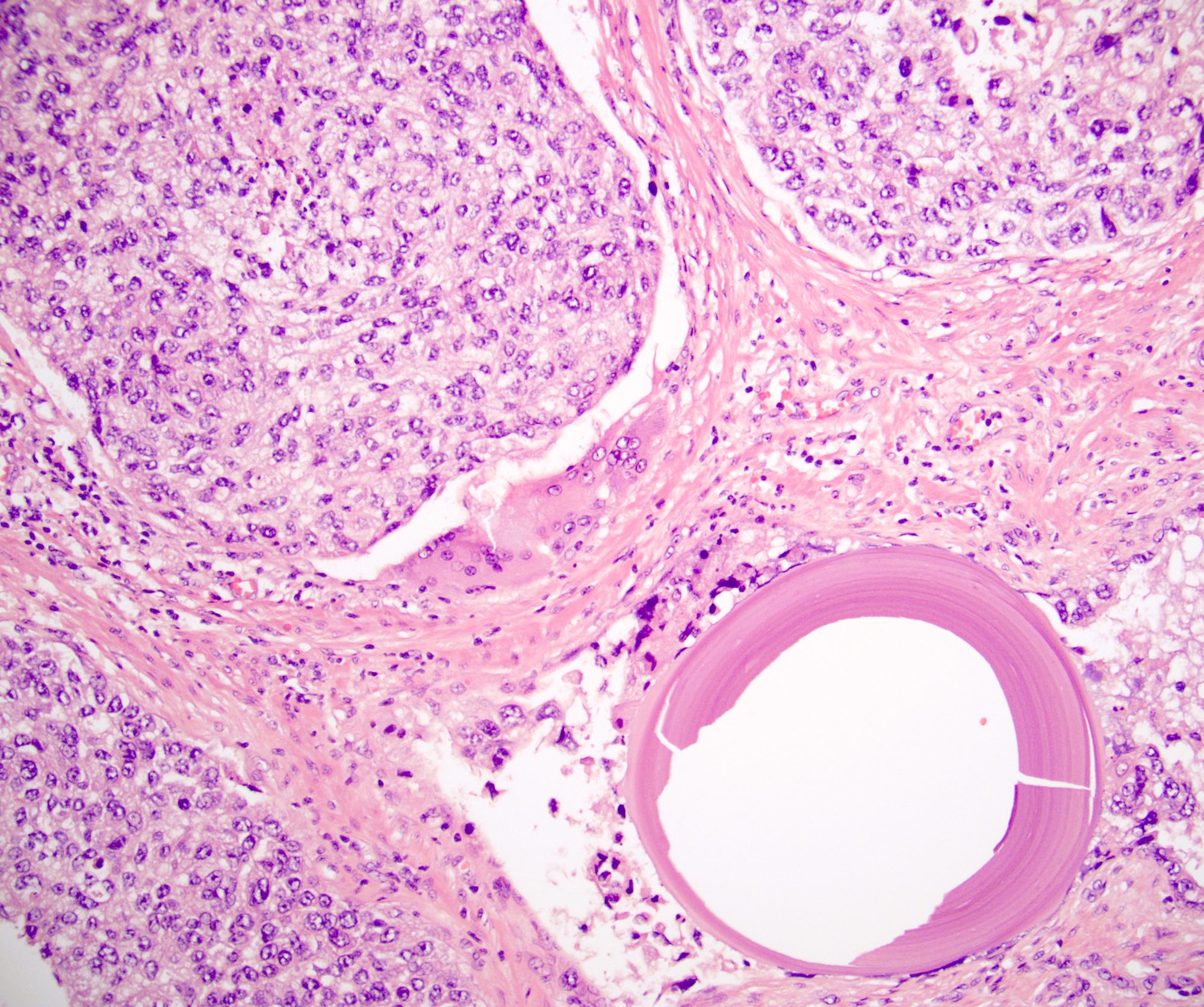
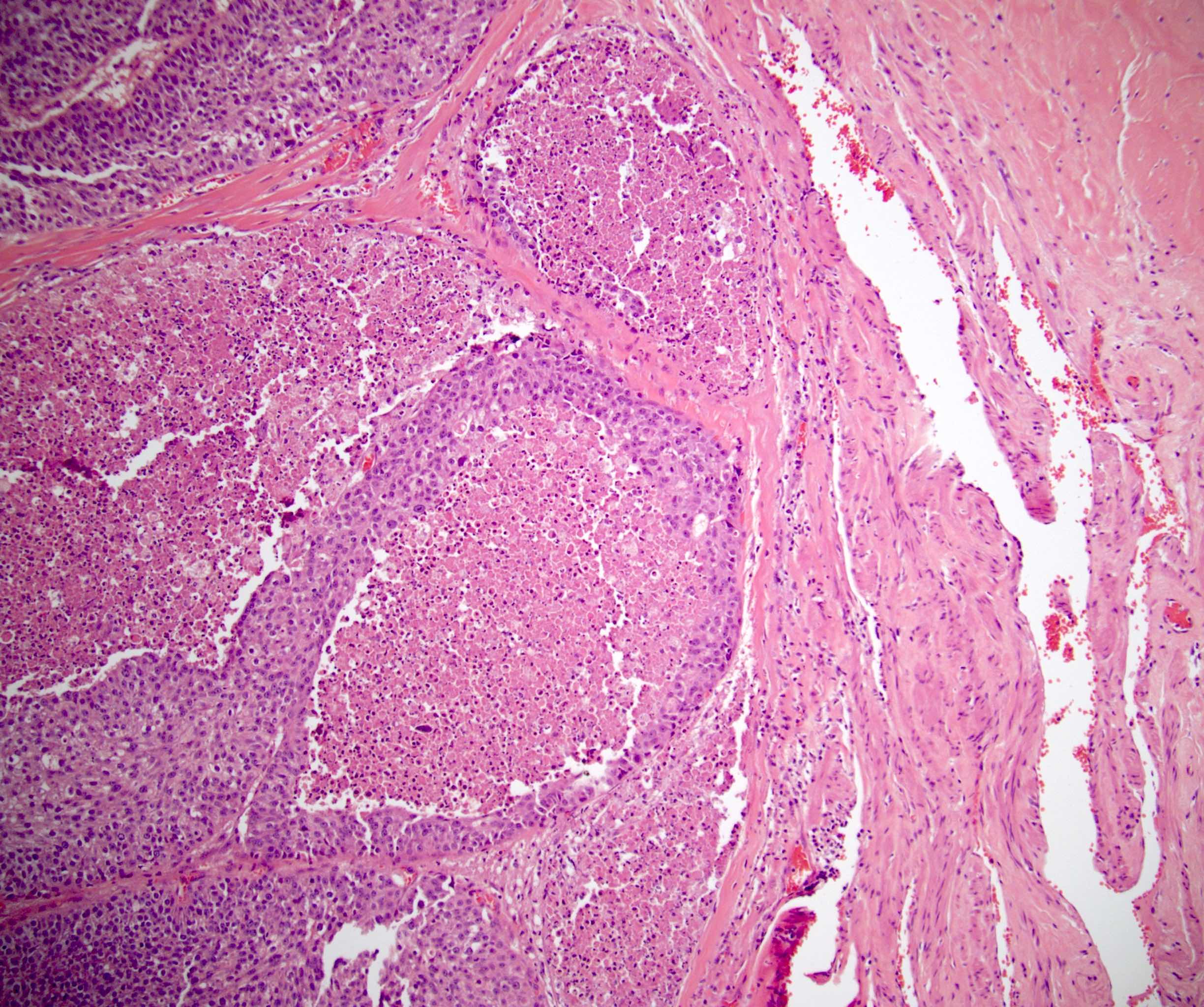
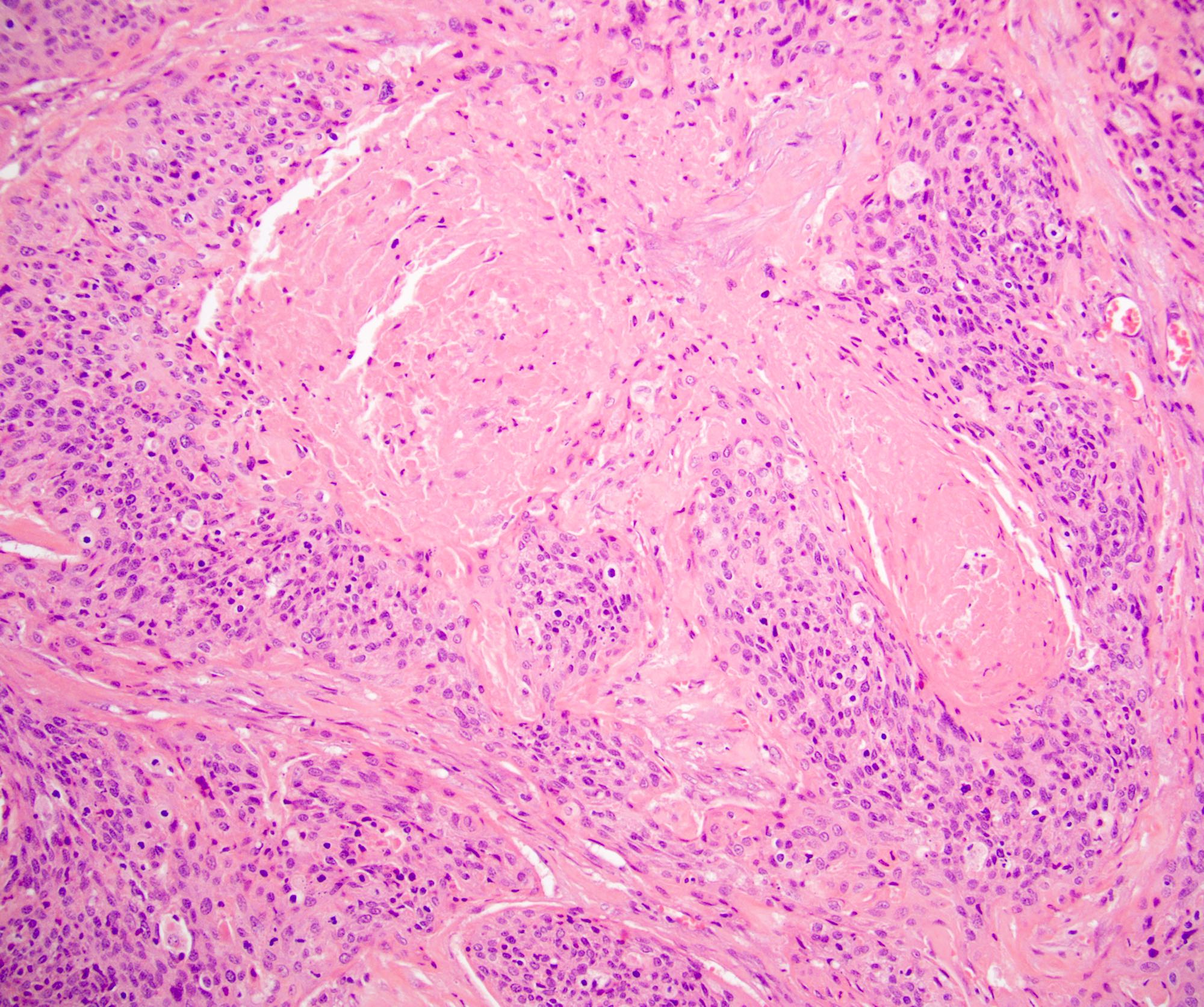
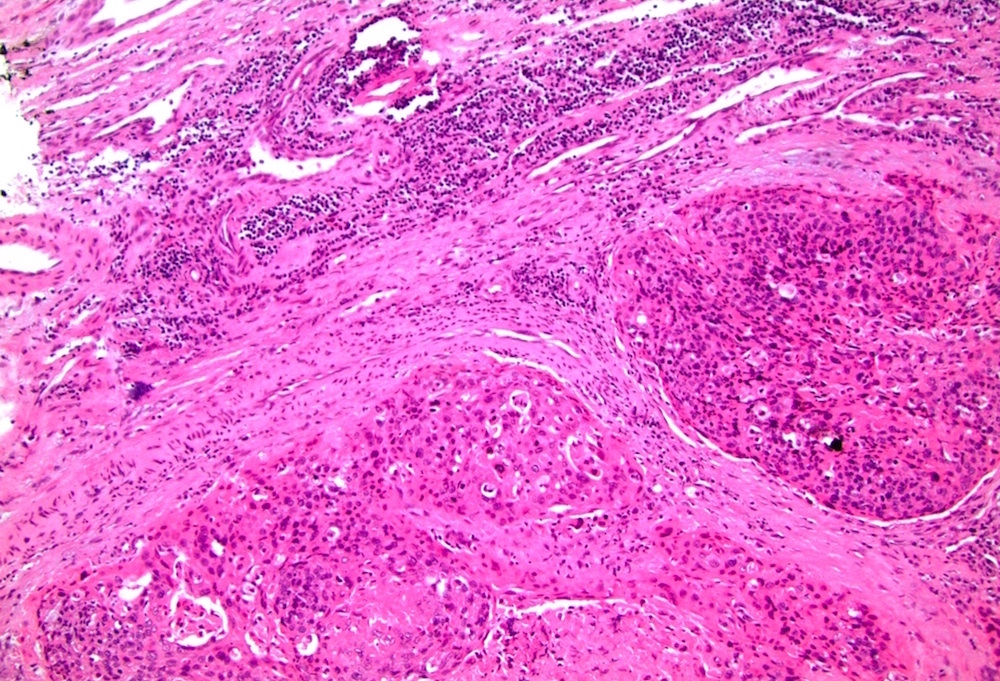
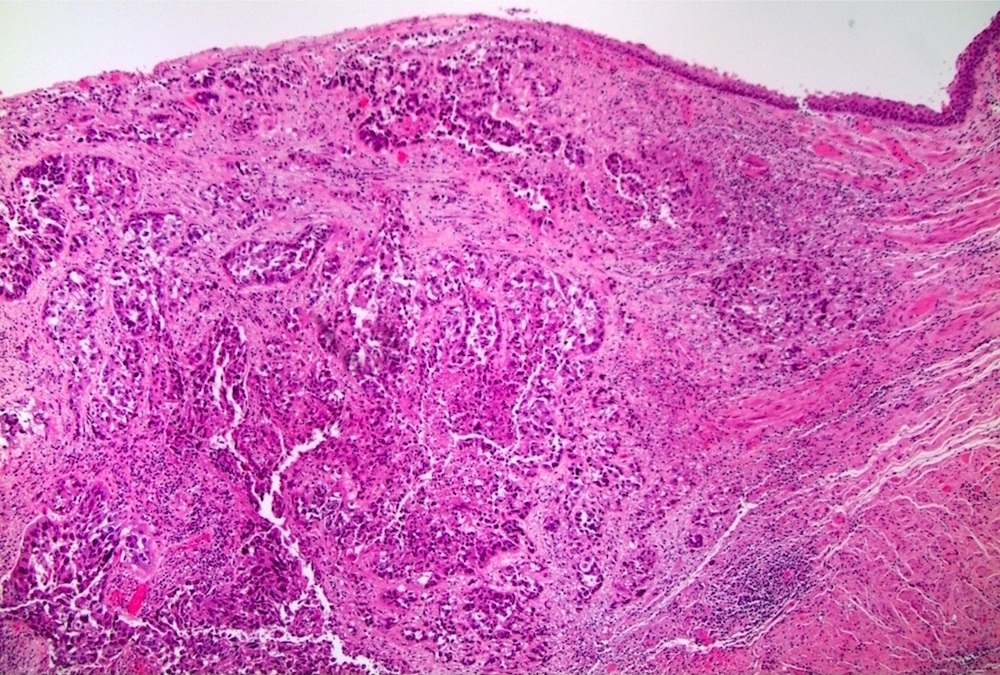
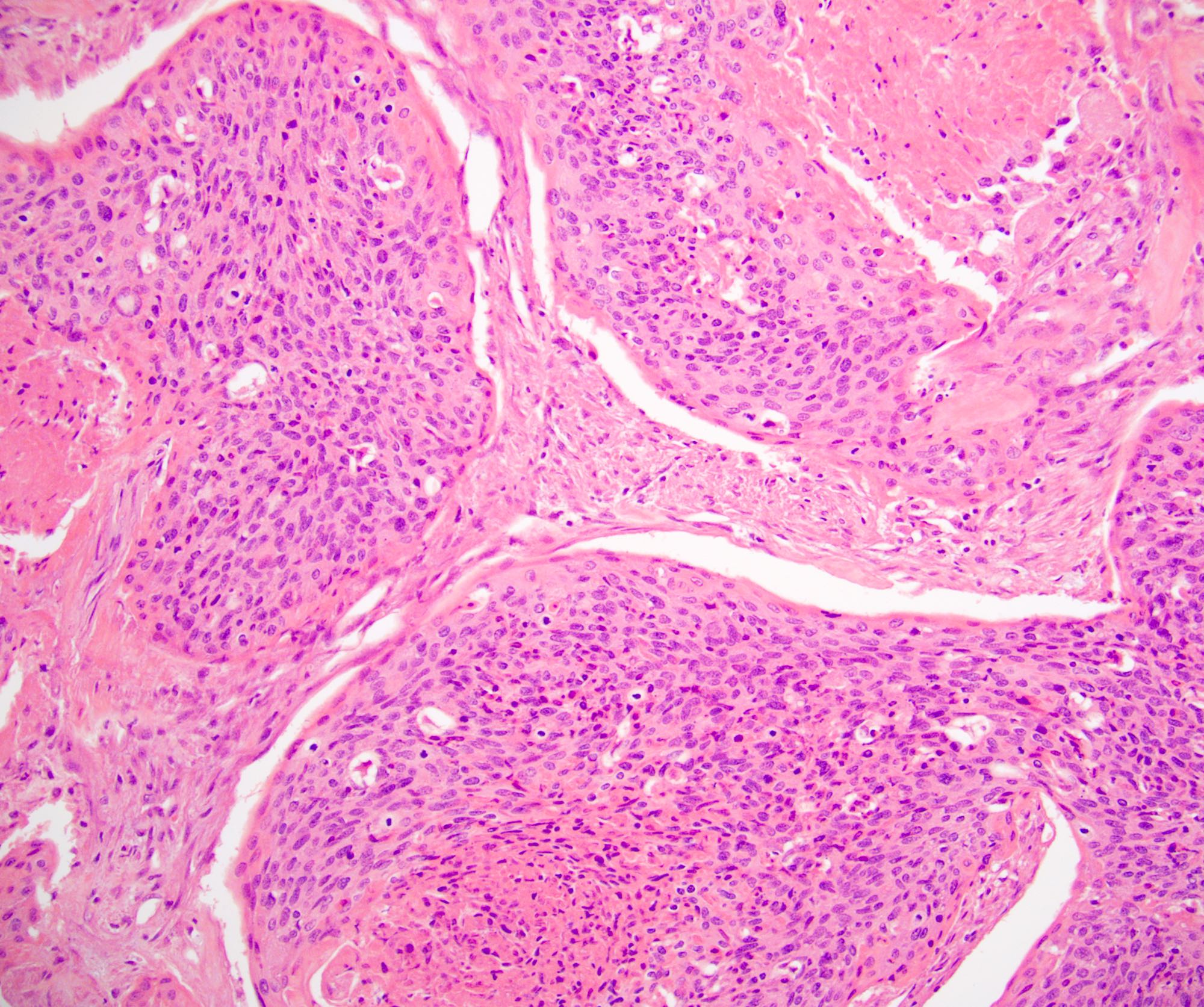
Microscopic (histologic) description
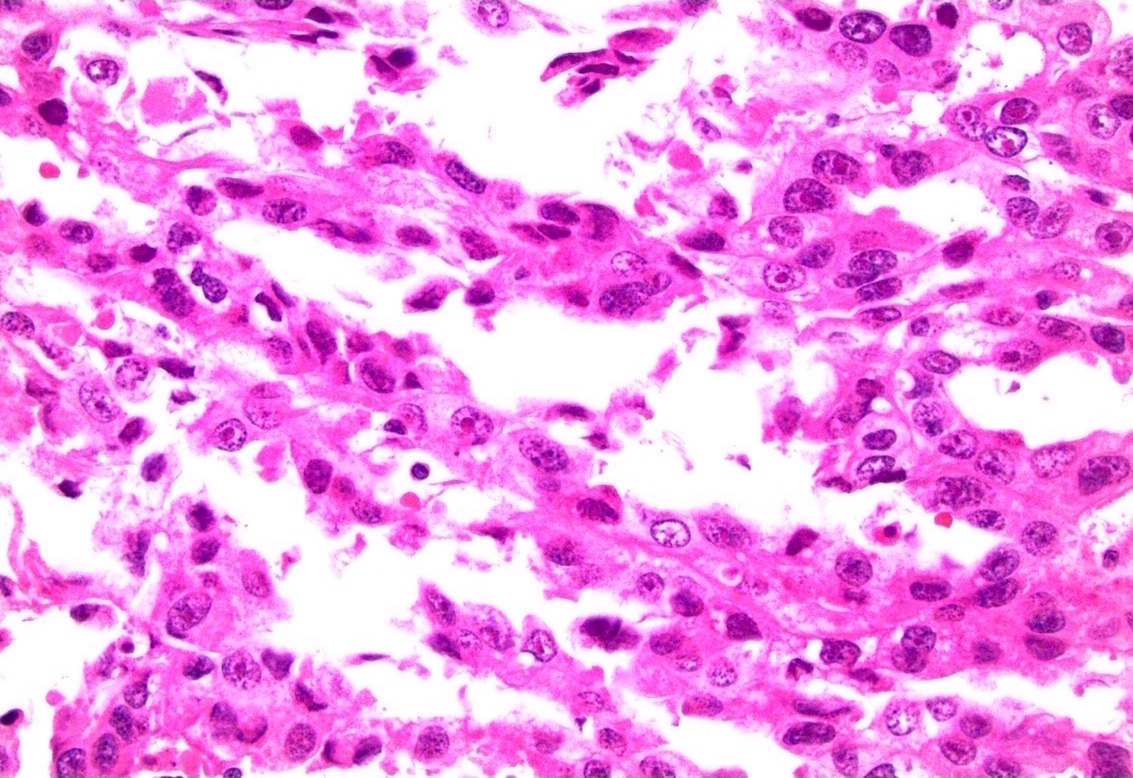
- Urothelial carcinoma
- Cytologically malignant urothelial cells with visible cell membranes, marked nucleomegaly, irregular nuclei, prominent nucleoli, dark chromatin and identifiable mitoses
- Squamous cell carcinoma
- Sheets of large, pleomorphic tumor cells with focal or abundant keratinization (depending on the degree of differentiation), ample cytoplasm, intercellular bridges, prominent nuclear atypia and high mitotic activity
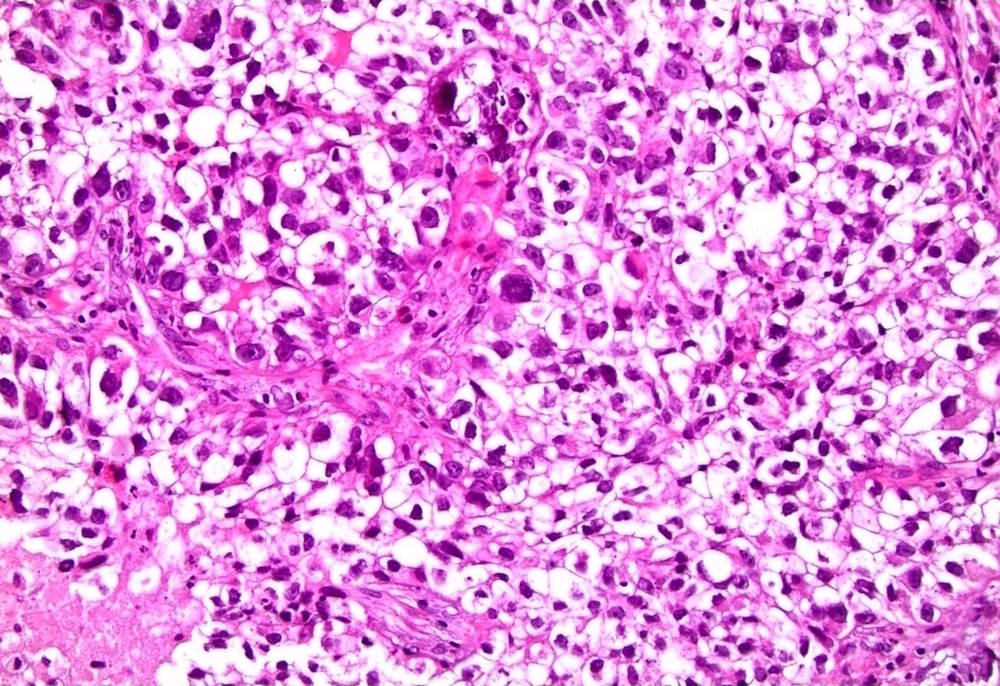
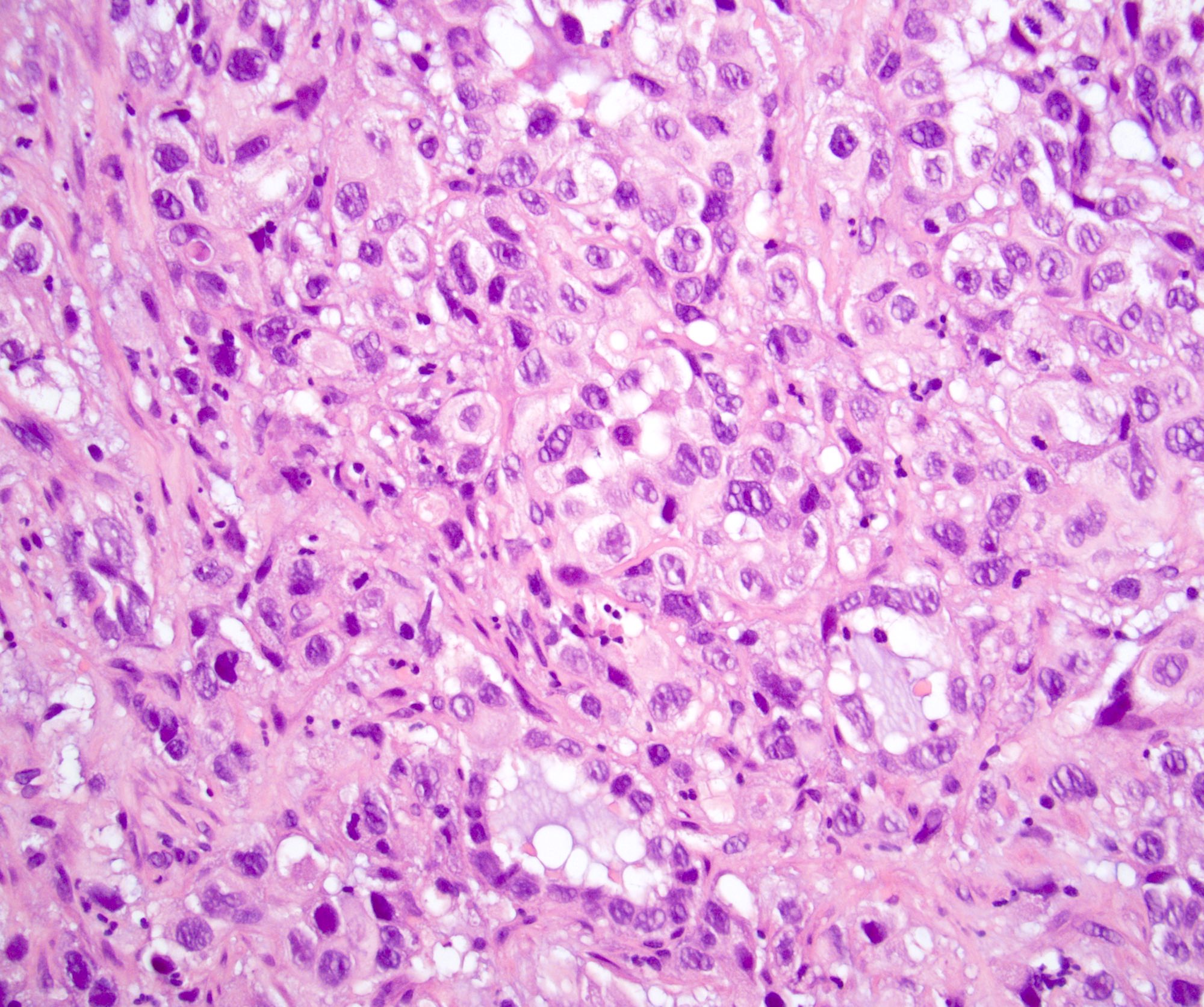
- Adenocarcinoma
- Composed of simple or pseudostratified columnar epithelium, apical cytoplasm and basally located hyperchromatic nuclei
- Occasional vacuolated cytoplasm with mucin or can be a true mucinous tumor with mucin pools
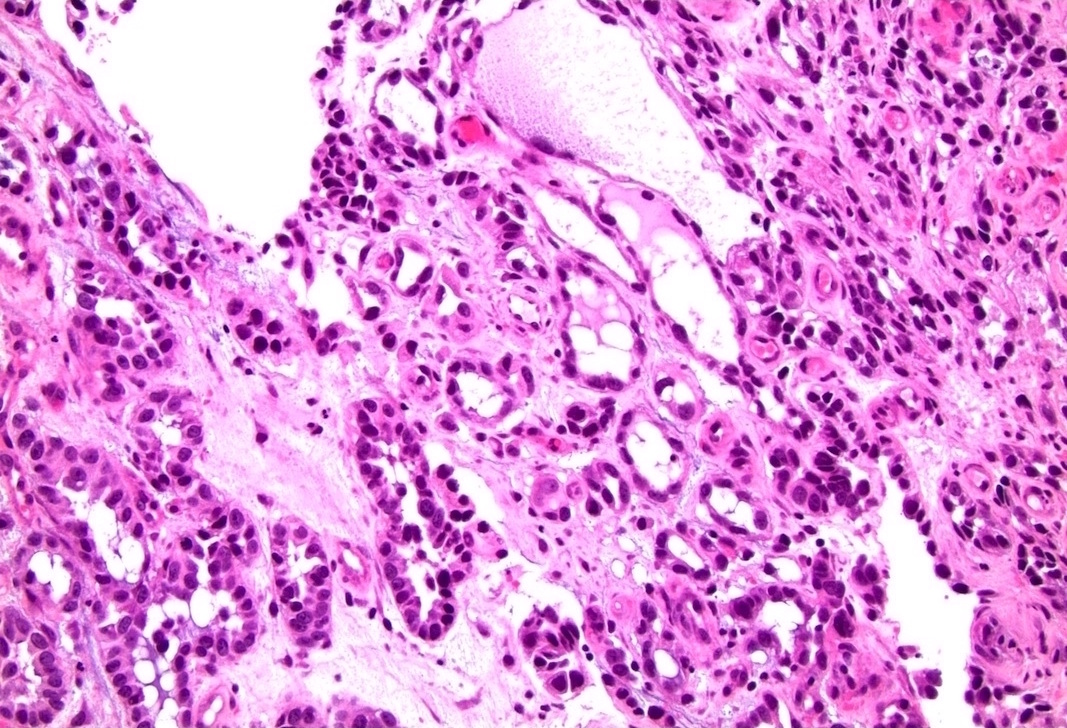
- Clear cell adenocarcinoma
- May have glandular, tubulocystic, solid / diffuse, papillary or micropapillary growth patterns
- Cuboidal, variably sized cells with abundant clear or eosinophilic cytoplasm and cytoplasmic vacuoles
- Nuclei that are hyperchromatic, pleomorphic and have prominent nucleoli
- Hobnail changes and extracellular mucoid material may be present
- Mitoses and necrosis are often seen
- One study proposed a hybrid tumor with urothelial and squamous features, similar to basaloid squamous cell carcinoma, as the histology for most urethral tumors (Hum Pathol 2018;72:35)
Microscopic (histologic) images
Cytology description
- Positive cytology seen in 59% with primary urethral carcinoma (Urology 2004;63:33)
- Sensitivity greatest for urothelial cell carcinoma (80%) and lowest for squamous cell carcinoma (50%) (Urology 2004;63:33)
Positive stains
- Urothelial carcinoma (Hum Pathol 2013;44:2760)
- Squamous cell carcinoma
- Adenocarcinoma
- CK20 (variable), CDX2 (variable), cytoplasmic beta catenin
- Clear cell adenocarcinoma (Virchows Arch 2013;462:193, Arch Pathol Lab Med 2008;132:1417, Diagn Pathol 2022;17:87)
Negative stains
- Urothelial carcinoma (Hum Pathol 2013;44:2760)
- E-cadherin, CD44s, PAX8, PSA, PSAP
- Squamous cell carcinoma
- Adenocarcinoma
- Clear cell adenocarcinoma
Molecular / cytogenetics description
- PIK3CA found to be the most frequently targeted genomic alterations of advanced urethral carcinoma (Urol Oncol 2021;39:731.e1)
- Adenocarcinoma: PTEN was the top potentially targetable genomic alteration (Urol Oncol 2021;39:731.e1, Int J Surg Pathol 2021;29:447)
- Clear cell adenocarcinoma: focal copy number loss at SMAD4 and ARID2 loci, truncating mutation in ATM, ALK mutation (Am J Pathol 2014;184:584)
Sample pathology report
- Prostate, radical prostatectomy:
- Invasive urothelial carcinoma, high grade (see synoptic report)
- Surgical margins, negative for carcinoma
- Comment: The tumor expresses GATA3, CK7, CK20 and p63 and has focal, patchy expression of CK5/6.
- Penile urethra, biopsy:
- Carcinoma consistent with invasive urothelial carcinoma, high grade (see comment)
- Carcinoma invades corpus spongiosum
- Comment: The tumor expresses GATA3, CK7, CK20 and p63 and has focal, patchy expression of CK5/6.
- Female urethra, biopsy:
- Clear cell adenocarcinoma of the urothelial tract
- Comment: The tumor expresses PAX8, CK7 and AMACR and is negative for p16, CK20 and p63.
Differential diagnosis
- Mimickers of primary urethral urothelial carcinoma
- Urothelial carcinoma arising from the bladder:
- Clinical history, imaging and gross description are critical for differentiation
- Inverted urothelial papilloma:
- Typically develops at trigone of bladder but can develop anywhere that urothelium is present (Ann Diagn Pathol 2019;38:11)
- Absent mitotic activity without cellular atypia (Ann Diagn Pathol 2019;38:11)
- Urothelial carcinoma arising from the bladder:
- Mimickers of primary urethral squamous cell carcinoma
- Mimickers of primary urethral adenocarcinoma
- Prostatic adenocarcinoma:
- Colonic adenocarcinoma:
- Colonic adenocarcinoma expresses nuclear beta catenin but not CK7, p63 and GATA3
- Mimickers of clear cell adenocarcinoma
- Nephrogenic metaplasia:
- Minimal atypia or mitotic activity
- Overlapping immunoprofile
- Nephrogenic metaplasia:
Board review style question #1
A female urethra is resected with the primary tumor shown in the above image. The tumor strongly and diffusely expresses CK5/6 and p63 but is negative for PAX8 and only has weak expression of GATA3. What is the best diagnosis?
- Adenocarcinoma, intestinal type
- Clear cell adenocarcinoma
- Squamous cell carcinoma
- Urothelial carcinoma
Board review style answer #1
C. Squamous cell carcinoma. The most common 2 tumors primary to the female urethra are urothelial carcinoma and squamous cell carcinoma. Squamous cell carcinoma characteristically expresses CK5/6 and p63 and does not express PAX8. GATA3 can be positive but is often weaker in intensity compared to urothelial carcinoma. Answer A is incorrect because adenocarcinoma, intestinal type would show gland formation and be negative for CK5/6 and p63. Answer B is incorrect because clear cell adenocarcinoma would show tubules, hobnailed cells and clear cells and would express PAX8 but not CK5/6 and p63. Answer D is incorrect because urothelial carcinoma usually has a strong expression of GATA3 and does not have a diffuse and strong expression of CK5/6. Both urothelial carcinoma and squamous cell carcinoma express p63.
Comment Here
Reference: Urethral carcinoma
Comment Here
Reference: Urethral carcinoma
Board review style question #2
Board review style answer #2
B. Clear cell adenocarcinoma. Clear cell adenocarcinoma can have many growth patterns including glandular, tubulocystic, solid / diffuse, papillary or micropapillary. The cells can be cuboidal or hobnailed and have clear or eosinophilic cytoplasm. The tumor typically expresses PAX8. Answers A, C and D are incorrect because adenocarcinoma, intestinal type, squamous cell carcinoma and urothelial carcinoma do not have the described morphology and they do not express PAX8.
Comment Here
Reference: Urethral carcinoma
Comment Here
Reference: Urethral carcinoma