Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Athanazio D. Papillary urothelial neoplasm of low malignant potential. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/bladderpunlmp.html. Accessed December 23rd, 2024.
Definition / general
- Neoplastic proliferation of the urothelium in a papillary configuration, with no invasion through the basement membrane
- Thickened urothelium or increased cellularity, without marked cytological atypia
Essential features
- Epithelial lining of fibrovascular cores is thicker than normal urothelium
- No nuclear atypia or hyperchromatic nuclei in neoplastic urothelial cells
- Maybe exophytic papillary or endophytic papillary (inverted)
- Exclusion criteria is prior history of urothelial carcinoma
Terminology
- Some authors suggest labeling as urothelial carcinoma WHO 1973 grade 1; however, it is recognized as a separate entity in WHO 2022 classification of urothelial tumors and by Genitourinary Pathology Society (Eur Urol Focus 2022;8:438, Urol Oncol 2020;38:440, Adv Anat Pathol 2021;28:179)
ICD coding
- ICD-O: 8130/1 - papillary transitional cell neoplasm of low malignant potential
- ICD-11: 2F78 & XH5UU5 - neoplasms of uncertain behavior of urinary organs & papillary urothelial neoplasm of low malignant potential
Epidemiology
- Estimated as 3.8% of all Ta urothelial tumors (Urol Oncol 2020;38:440)
- Strong male predominance (M:F = 5:1)
- 3 per 100,000 individuals per year (Zhou: Genitourinary Pathology, 2nd Edition, 2015)
- Peak incidence: 50 - 70 years
- Occurs in all ages (40 - 50% of bladder neoplasms in children) (J Urol 2005;174:1976, BJU Int 2010;106:557)
Sites
- Most diagnosed in the bladder
- Occurs anywhere along urinary mucosae
Pathophysiology
- Molecular pathology shows considerable overlap with low grade noninvasive papillary urothelial carcinoma including TERT promotion and FGFR3 mutations and shortened telomeres (Virchows Arch 2017;471:761, Histopathology 2018;72:795)
Etiology
- At least in adults, etiologic factors are thought to be the same as for urothelial carcinoma: smoking, exposure to other chemicals, heredity, infection, prior radiation and prior chemotherapy with cyclophosphamide (Epstein: Differential Diagnoses in Surgical Pathology - Genitourinary System, 2nd Edition, 2021)
Clinical features
- Gross or microscopic hematuria
- Urine cytology is negative in most cases
Diagnosis
- Cystoscopy: exophytic lesion with varying sizes (no specific cut off) but usually a small and single lesion
Radiology description
- Bladder mass with polypoid configuration and papillary / exophytic surface
- Inverted tumor shows a polypoid shape with a nonpapillary surface
Prognostic factors
- This diagnostic category is justified because the recurrence and progression rates of papillary urothelial neoplasm of low malignant potential (PUNLMP) are expected to be higher than urothelial papilloma and lower than low grade noninvasive urothelial carcinoma
- Recurrence rate: 18 - 20% (Am J Clin Pathol 2010;133:788, Diagn Pathol 2015;10:3)
- Progression rate: 1.9 - 11.1%, mainly to low grade noninvasive papillary urothelial carcinoma (Am J Clin Pathol 2010;133:788, Diagn Pathol 2015;10:3)
- ~1% progress to invasive urothelial carcinoma (Diagn Pathol 2015;10:3)
- Limited data on recurrence of inverted PUNLMP but it seems to be rare (Diagn Pathol 2015;10:3)
- In a population based study from Sweden, 5 year recurrence rates of PUNLMP and noninvasive low grade papillary urothelial carcinoma were 21% and 42%, respectively; progression rates were 0.7% and 4%, respectively (Scand J Urol 2022;56:14)
- Not all series show differences in recurrence and progression between PUNLMP and low grade noninvasive urothelial carcinoma:
- 5 year recurrence rate is 51% for PUNLMP versus 48% for low grade papillary urothelial carcinoma
- Progression to muscle invasive disease is 3.9% for PUNLMP versus 2.6% for low grade papillary urothelial carcinoma (Urol Oncol 2020;38:440)
Case reports
- 9 year boy with relapsed PUNLMP (BMC Urol 2019;19:36)
- 19 year old man with gross hematuria (J Diagn Med Sonogr 2014;30:249)
- 19 year old male chronic smoker with PUNLMP with foci of osseous metaplasia in fibrovascular cores (Indian J Pathol Microbiol 2022 May 26 [Epub ahead of print])
Treatment
- Surgical: transurethral resection with no need of further topical treatments
Clinical images
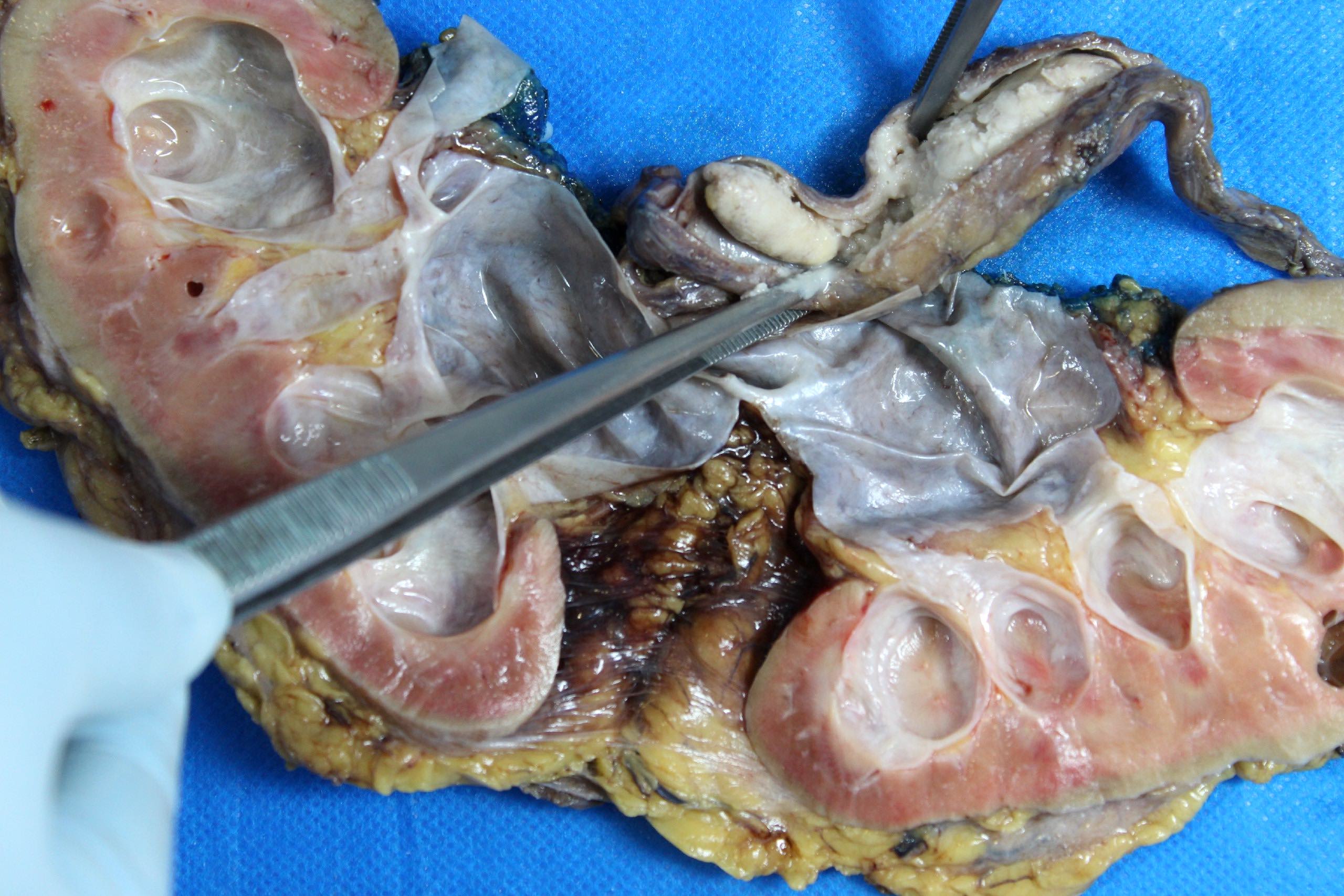
Gross description
- Variable size but most tumors are single and regular polypoid masses measuring < 2 cm
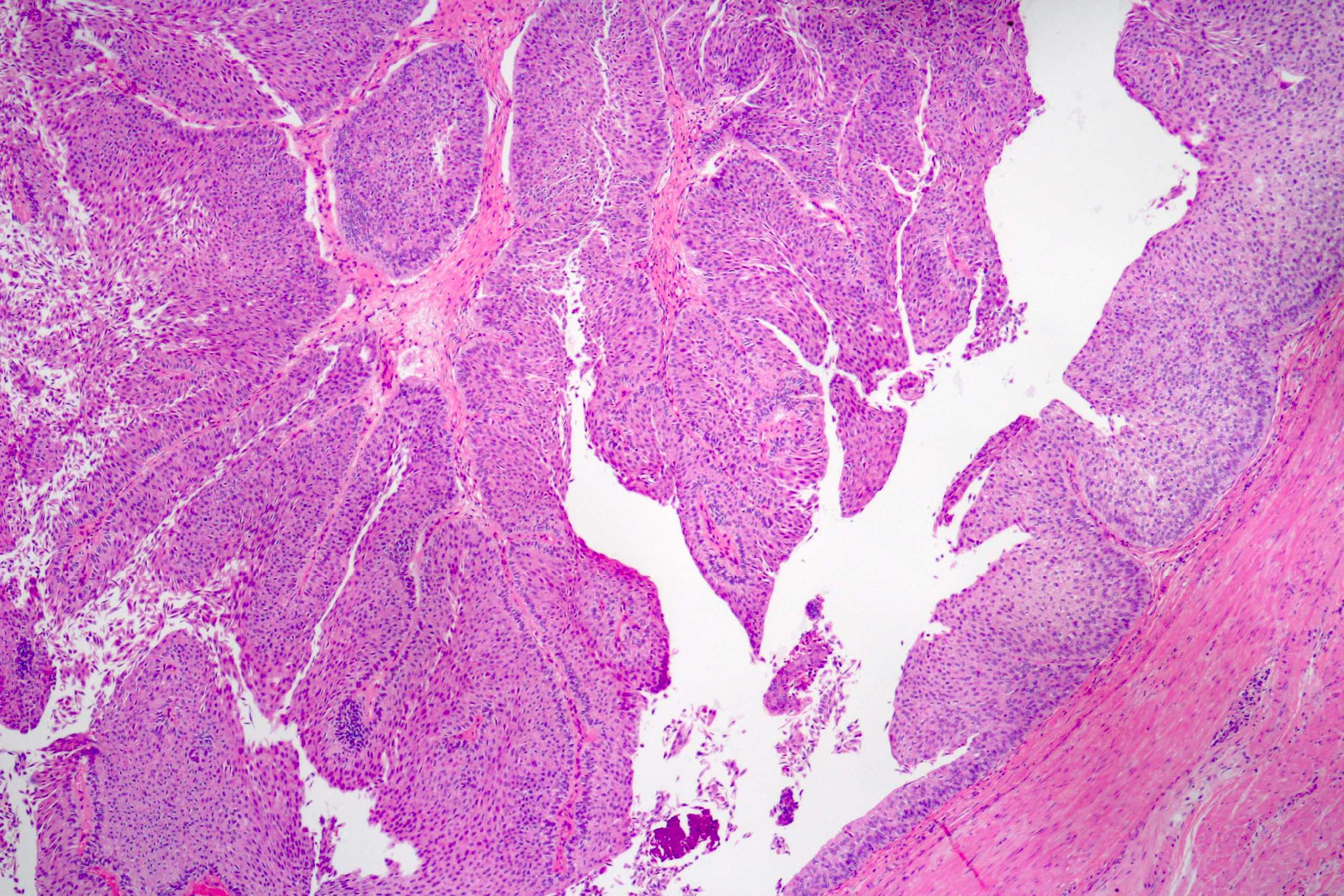
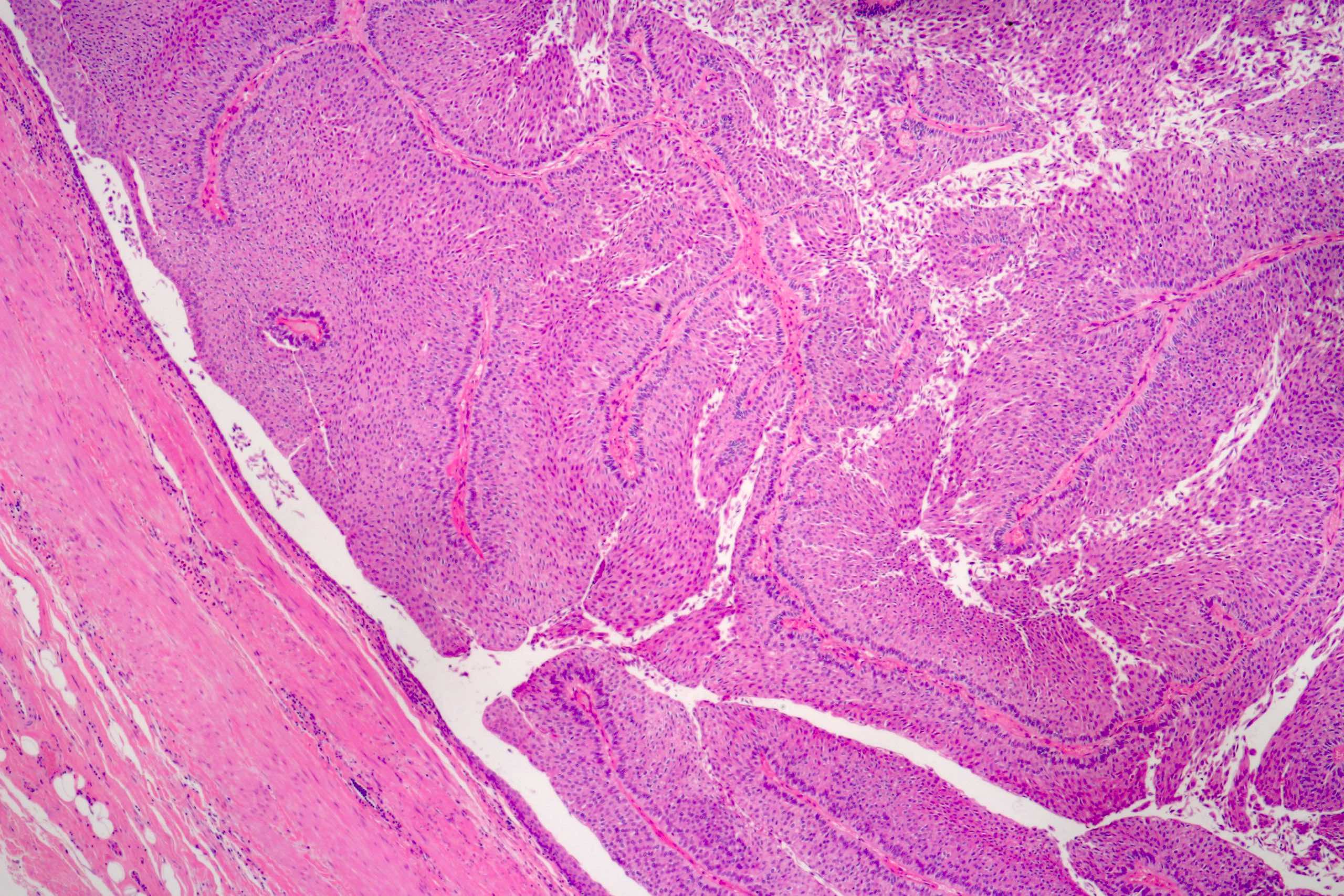
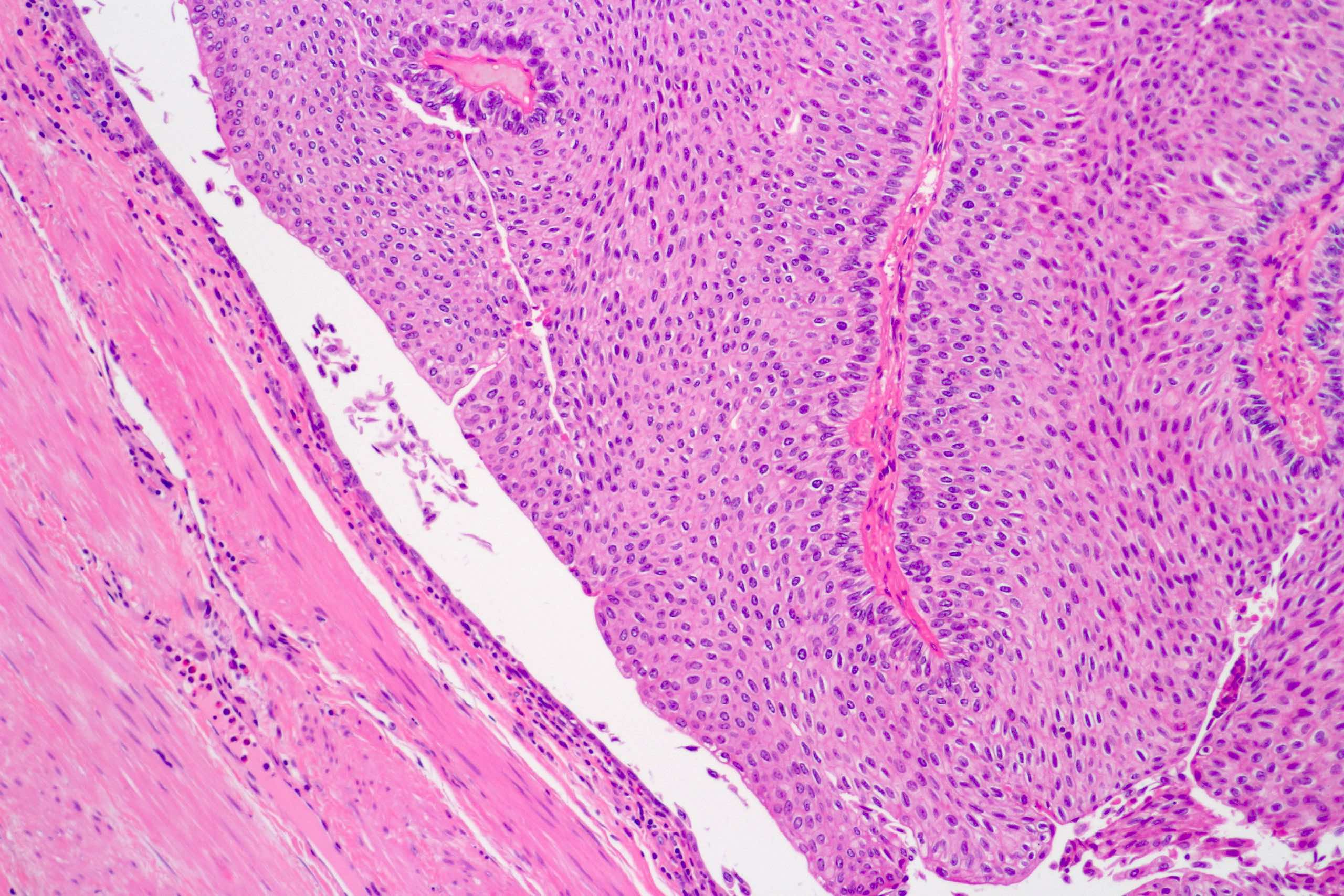
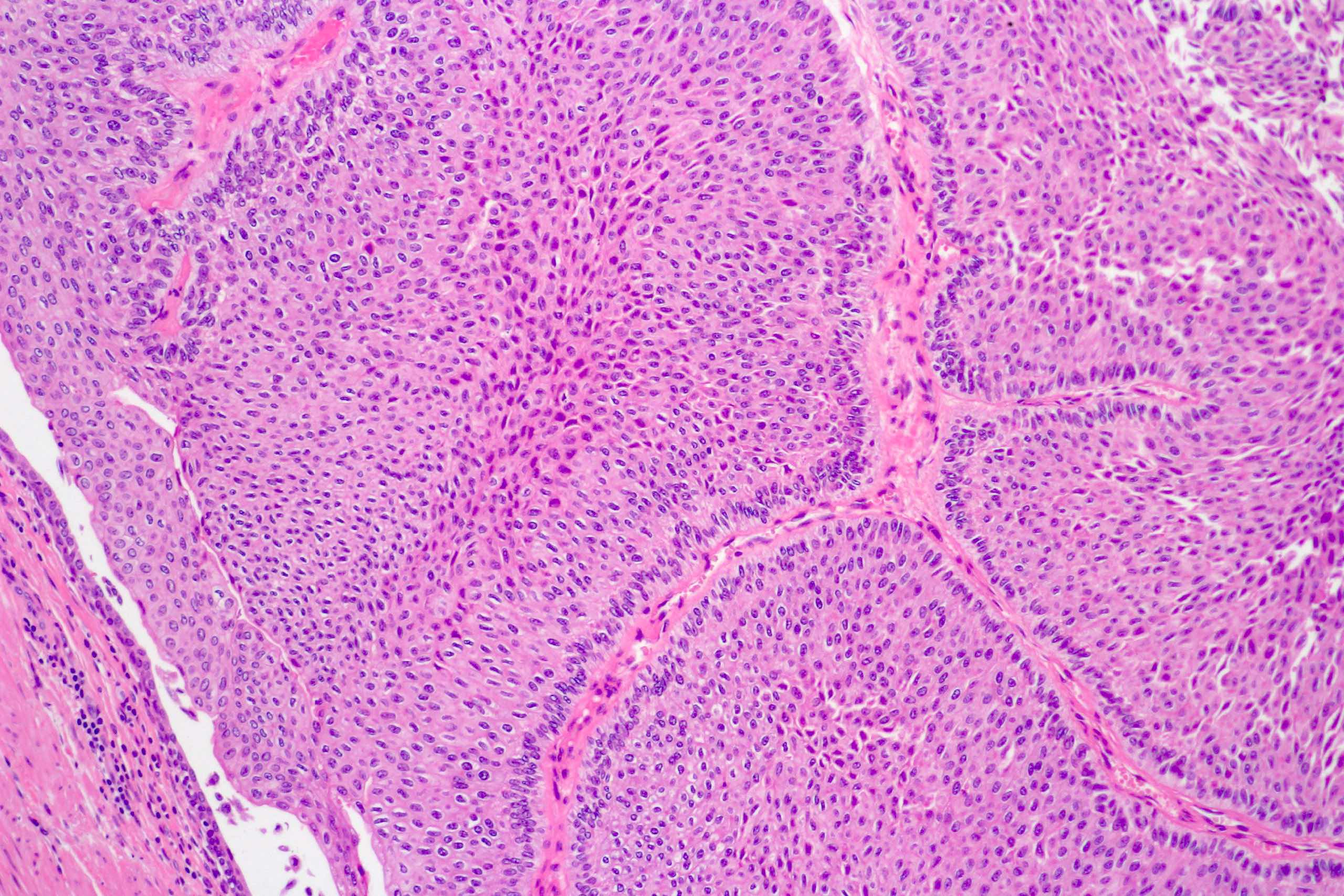
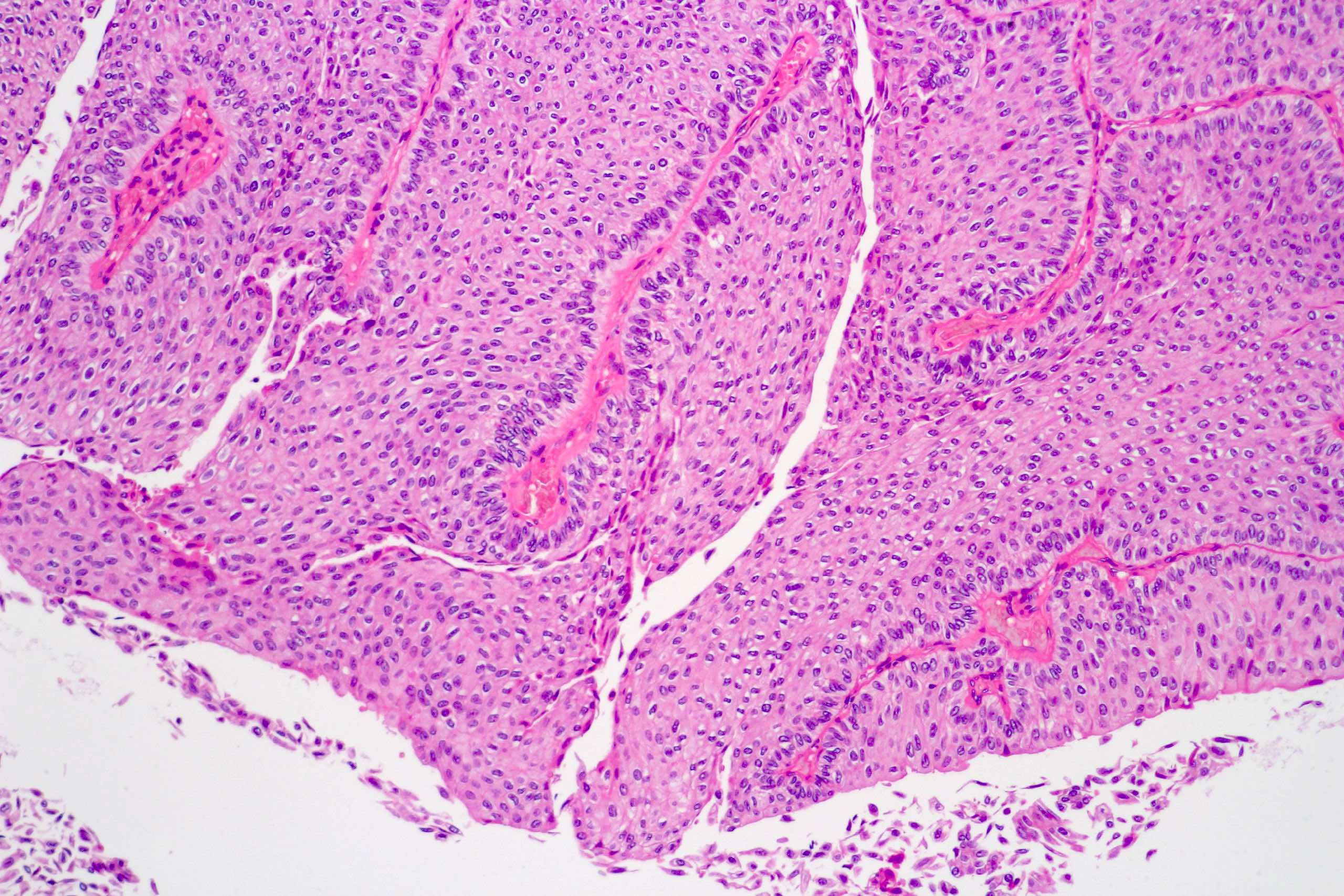
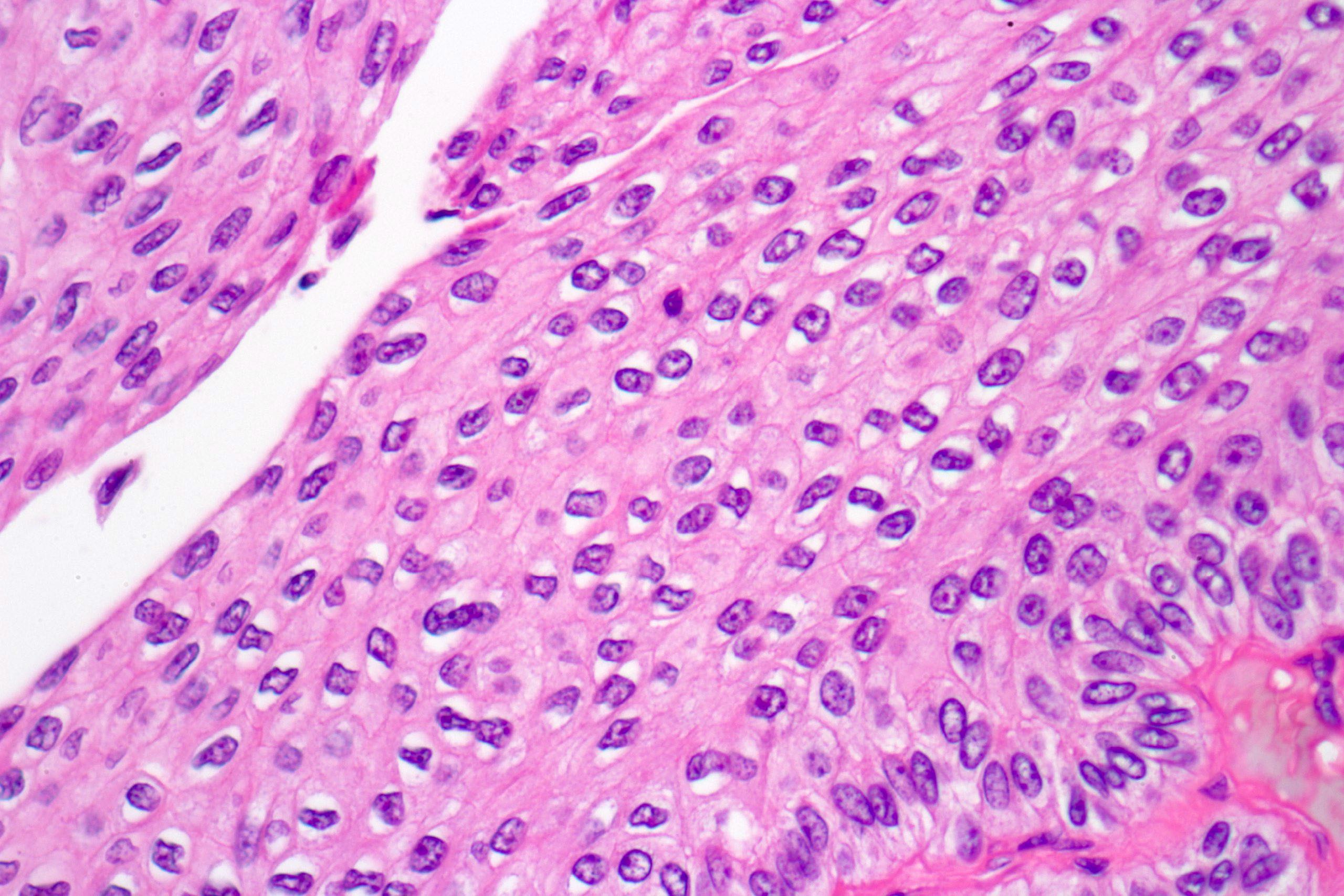
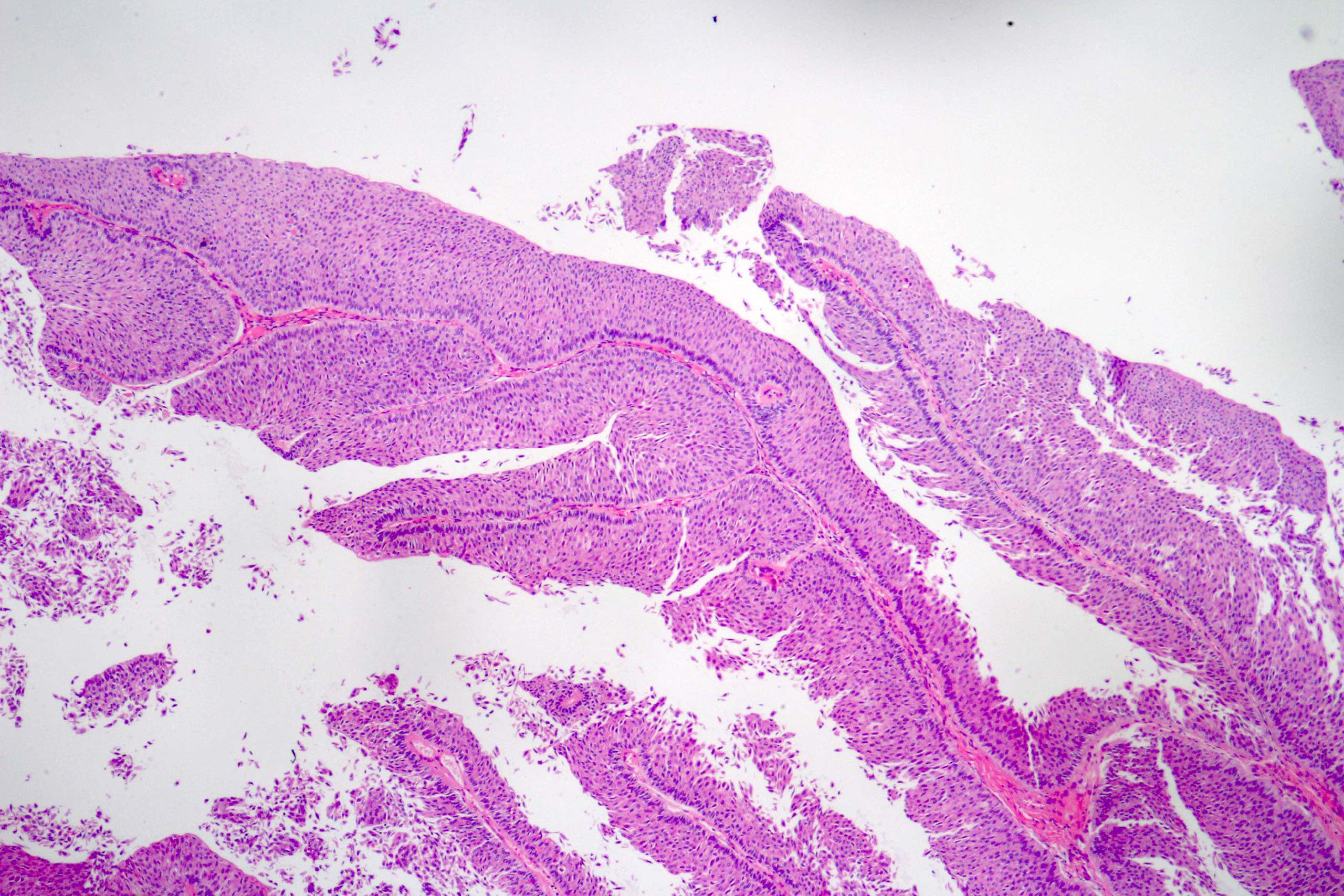
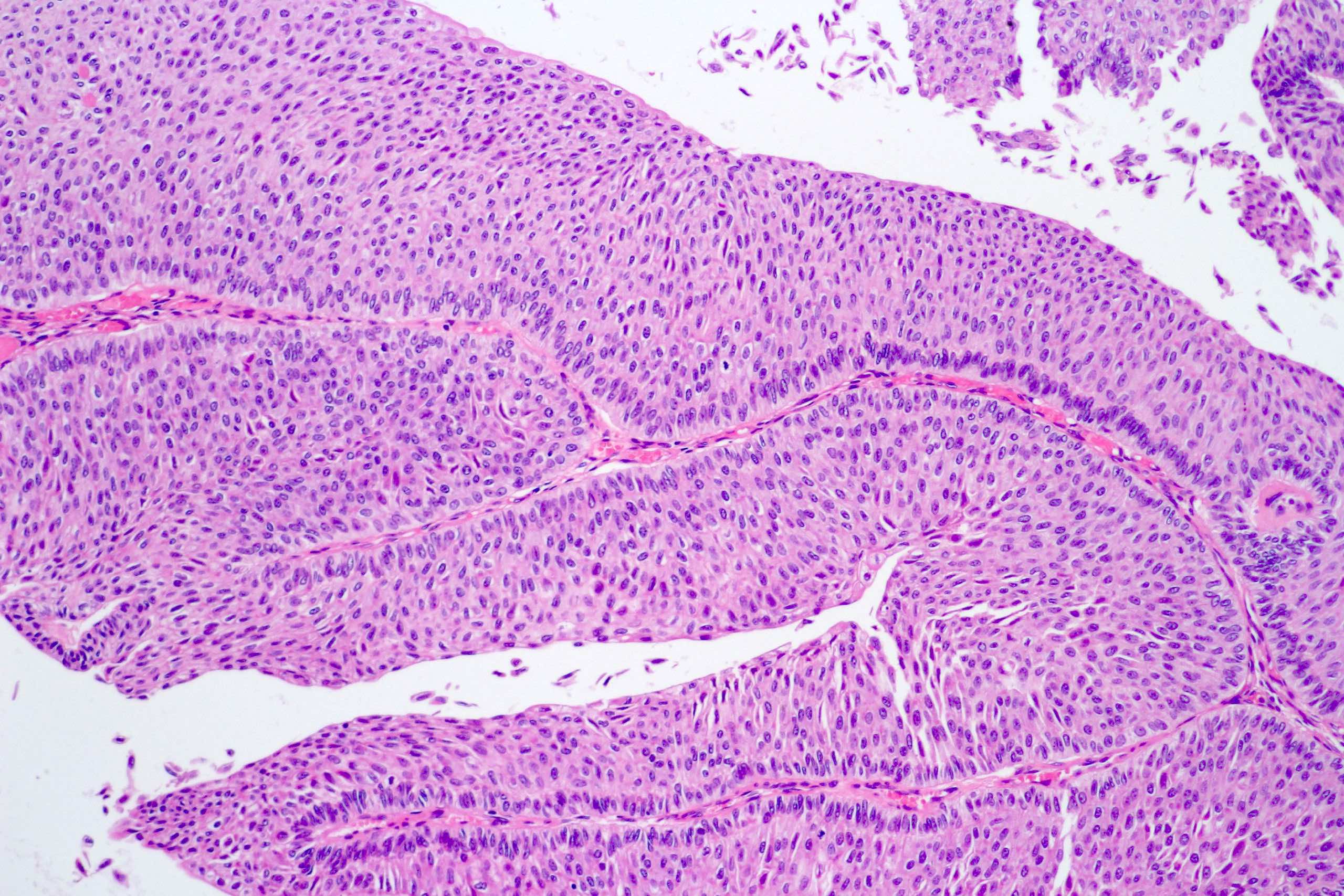
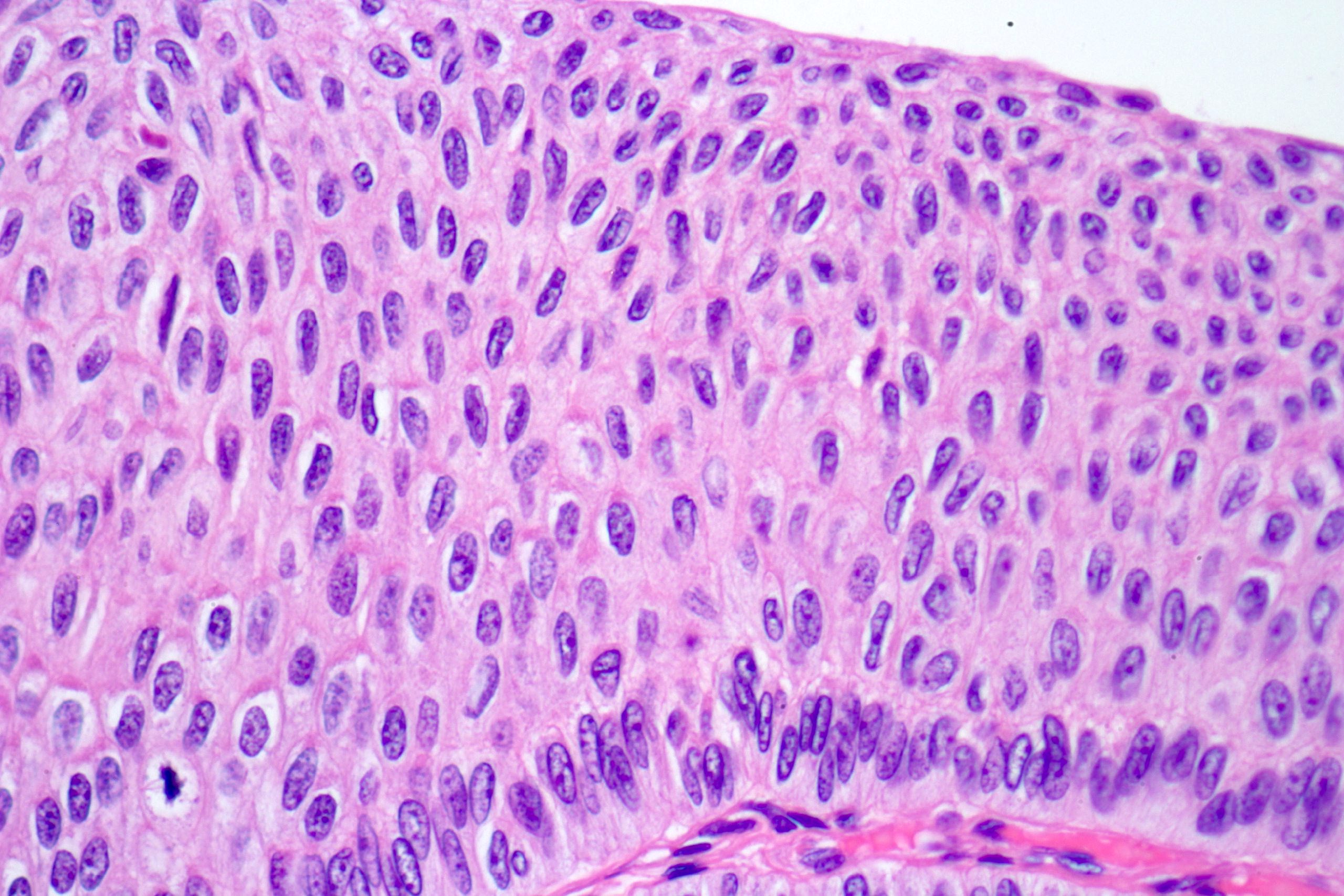
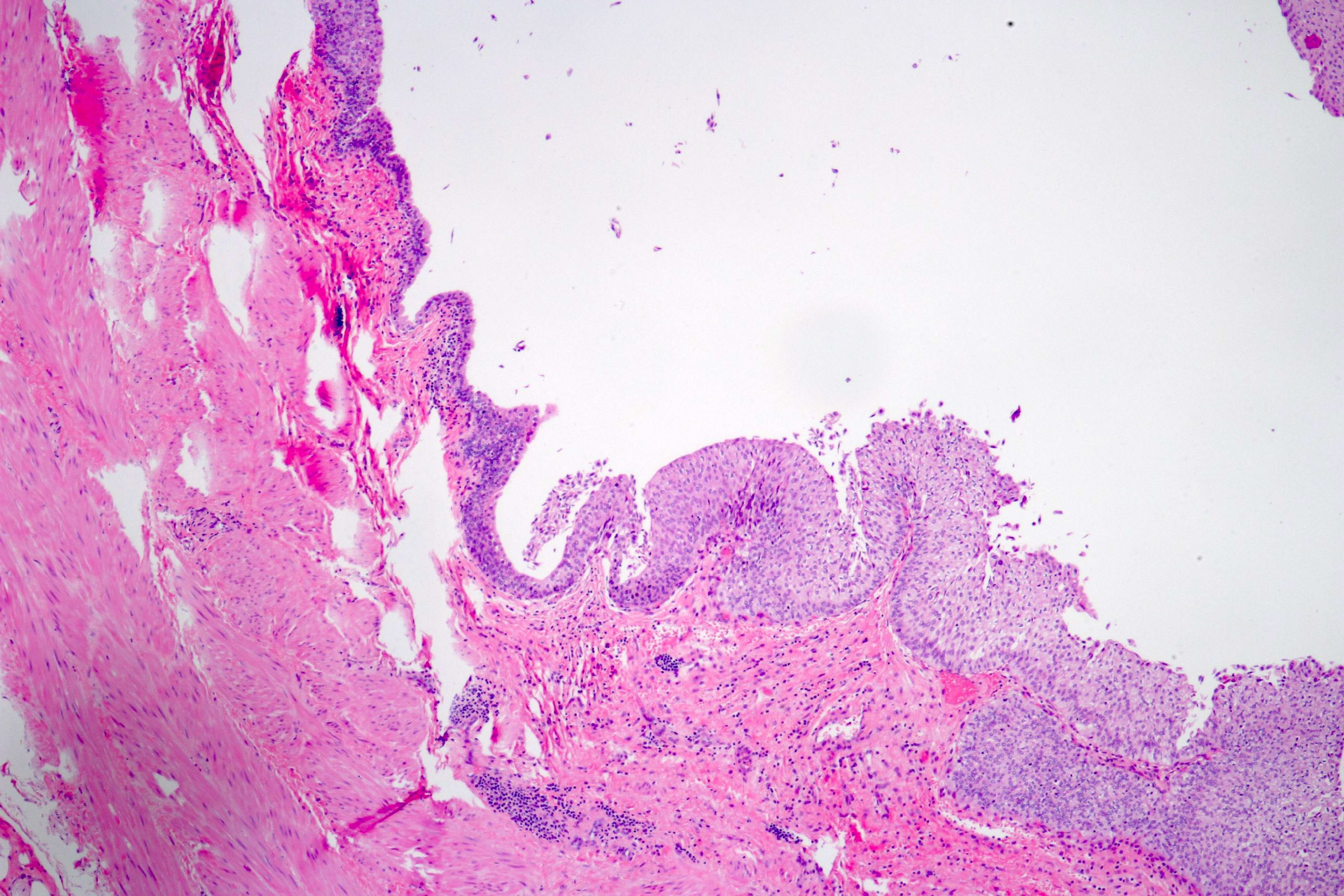
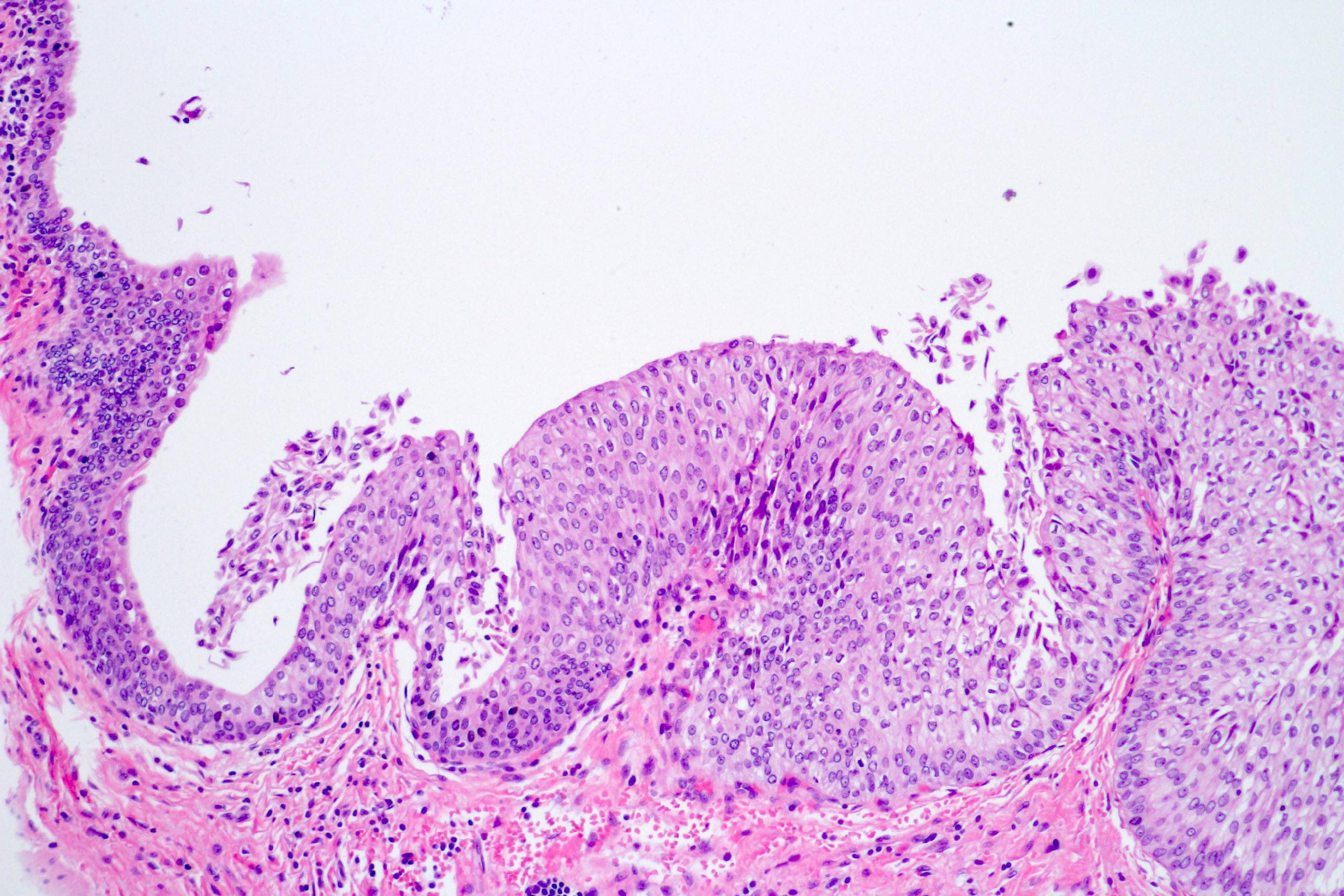
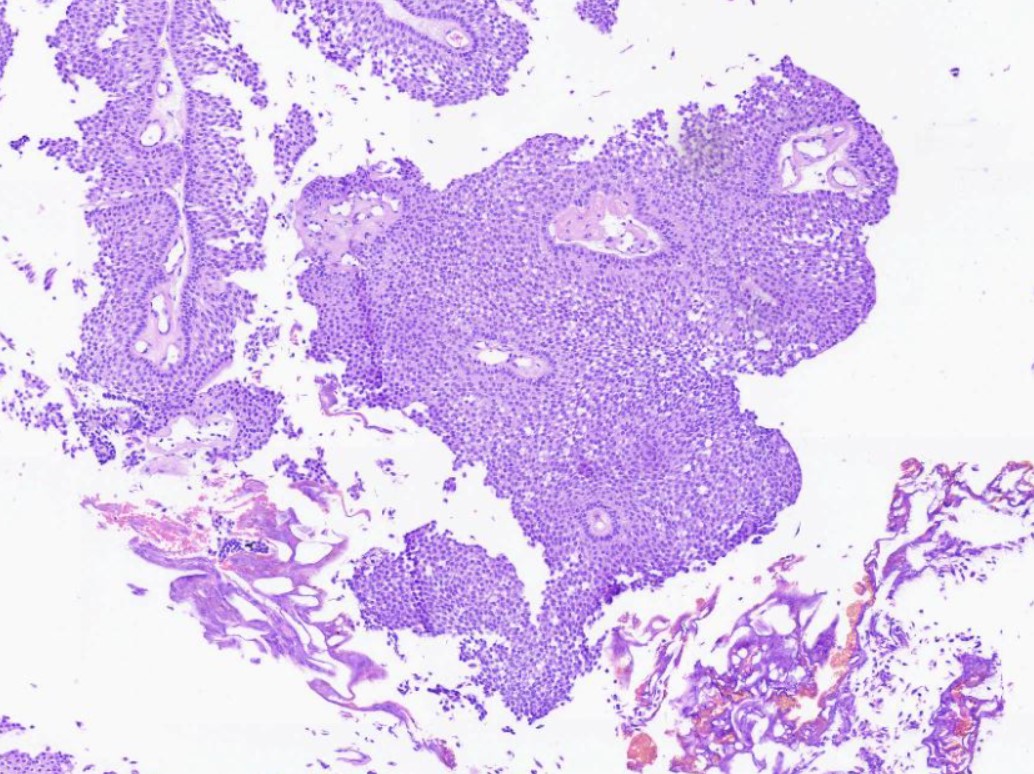
Microscopic (histologic) description
- Noninvasive papillary urothelial neoplasm with exophytic or endophytic (inverted) configuration; a cut off of > 80% is proposed by the Genitourinary Pathology Society to designate a urothelial neoplasm of inverted type (Adv Anat Pathol 2021;28:179)
- Epithelial lining of fibrovascular cores is thicker than normal urothelium: urothelial cells show monotonous appearance and slight cytoplasmic and nuclear enlargement
- No variation in nuclear size, shape or chromatin pattern
- Preserved polarity of urothelial cells
- Mitoses are rare and basally located
- No hyperchromatic nuclei in urothelial cells in intermediate layers of neoplastic epithelium
Microscopic (histologic) images
Contributed by Daniel Athanazio, M.D., Ph.D. and Luciana Schultz, M.D., Ph.D. (source: Instituto de Anatomia Patológica)
Cytology description
- Usually not detected in urinary cytology, unless entire papillary formations are seen (then a diagnosis of low grade urothelial neoplasm, including both PUNLMP and low grade noninvasive papillary urothelial carcinoma, may be suggested as a comment within the diagnosis of “negative for high grade urothelial carcinoma”)
- The Paris System states that, in most cases, urinary cytology is unable to detected low grade urothelial neoplasms, including PUNLMP (J Am Soc Cytopathol 2016;5:177, J Am Soc Cytopathol 2022;11:62)
Positive stains
- Markers of urothelial differentiation (not helpful in the differential diagnosis)
Negative stains
- Not helpful
Molecular / cytogenetics description
- Not relevant for the diagnosis
- Similar findings to low grade noninvasive papillary urothelial carcinoma
- TERT promoter mutation in 33 - 63% (Virchows Arch 2017;471:761, Histopathology 2018;72:795)
- One study reported higher rate of PUNLMP recurrence in patients with TERT promoter mutation, similar to low grade noninvasive papillary urothelial carcinoma (Histopathology 2018;72:795)
- FGFR3 mutations in 30 - 60% (Virchows Arch 2017;471:761, Histopathology 2018;72:795)
Videos
Differential diagnosis of noninvasive endophytic urothelial neoplasms
PUNLMP at cytology
Sample pathology report
- Bladder, lesion, transurethral resection:
- Papillary urothelial neoplasm of low malignant potential (see comment)
- Muscularis propria is present
- Comment: The sample shows urothelial neoplasia with thickened epithelial lining and no atypia. There are no invasive foci. The findings are consistent with the diagnosis of urothelial neoplasm of low malignant potential (PUNLMP), an indolent tumor expected to have lower rates of recurrence and progression when compared to noninvasive low grade papillary urothelial carcinoma. For a sample of an incompletely resected multifocal or larger tumor, complete excision of all visible lesions for pathologic analysis is recommended. The diagnosis of PUNLMP requires exclusion of prior history of urothelial carcinoma. In cases involving a prior history of carcinoma, the present tumor should be considered a recurrence of the original neoplasia.
Differential diagnosis
- Noninvasive papillary urothelial carcinoma, low grade:
- At least scattered atypical / hyperchromatic nuclei in a neoplastic urothelium with preserved polarity
- More than rare mitoses should favor urothelial carcinoma
- Urothelial papilloma:
- No atypia in the urothelial lining of delicate fibrovascular cores, limited to 6 - 7 layers of urothelial cells
- No fused papillae
- Polypoid / papillary cystitis:
- Edematous or fibrotic stroma with broad base cores of papillary outlines
- Reactive epithelial changes may be present
- Urothelial hyperplasia, urothelial proliferation of unknown malignant potential or atypical urothelial proliferation (flat or tented):
- No true, delicate fibrovascular core
Additional references
Board review style question #1
A transurethral resection of bladder was performed on a 60 year old man. Histological examination showed a noninvasive papillary lesion with fibrovascular cores lined by thickened urothelium with cells with monotonous appearance and no nuclear atypia. Which of the following additional information would exclude the diagnosis of urothelial neoplasm of low malignant potential?
- Multicentric disease
- Prior history of prostate adenocarcinoma
- Prior history of urothelial carcinoma
- Size larger than 3 cm
Board review style answer #1
C. Prior history of urothelial carcinoma
Comment Here
Reference: Papillary urothelial neoplasm of low malignant potential
Comment Here
Reference: Papillary urothelial neoplasm of low malignant potential
Board review style question #2
The differential diagnosis between urothelial neoplasm of low malignant potential and noninvasive low grade papillary urothelial carcinoma usually shows poor reproducibility in different studies. Which of the following is the most important criterion favoring the diagnosis of urothelial carcinoma?
- EGFR3 mutation
- Scattered hyperchromatic nuclei among intermediate neoplastic urothelial cells
- TERT promoter mutation
- TP53 mutation
Board review style answer #2
B. Scattered hyperchromatic nuclei among intermediate neoplastic urothelial cells
Comment Here
Reference: Papillary urothelial neoplasm of low malignant potential
Comment Here
Reference: Papillary urothelial neoplasm of low malignant potential