Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Yu YHS, Downes MR. Noninvasive papillary urothelial carcinoma low grade. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/bladderlgpap.html. Accessed December 25th, 2024.
Definition / general
- Neoplastic proliferation of the urothelium in a papillary configuration, with no invasion through the basement membrane
- Low grade architectural and cytologic abnormality, absence of high grade features, such as irregular nuclei with frequent, prominent nucleoli and mitoses, pleomorphism
Essential features
- Noninvasive papillary urothelial neoplasm with low grade cytoarchitectural abnormality
- Loss of polarity, rare mitoses, subtle variation in nuclear size but no significant pleomorphism
- Immunohistochemistry not helpful for diagnosis
- Hematuria common presentation
- Disease related death and progression is rare but recurrence common
Terminology
- Grade 1 and subset of grade 2 carcinomas from 1973 WHO classification
ICD coding
- ICD-O: 8130/2 - papillary transitional cell carcinoma, noninvasive
Epidemiology
- Incidence: 5 per 100,000 people per year (J Urol 1999;162:702)
- M:F = 3:1
- Median age: 70 years
- Lynch syndrome, especially MSH2 carriers, clinically earlier stage and low grade (Int J Urol 2018;25:151)
Sites
- Most commonly found in posterior and lateral walls of bladder
- 85% of urothelial neoplasms of renal pelvis are papillary but only 34% of them are low grade (Mod Pathol 2005;18:11)
- Anywhere with urothelium
Pathophysiology
- Normal urothelium, through loss of chromosome 9, becomes hyperplasia
- Followed by further genetic alterations, such as mutations in FGFR3, which activates mitogen activated protein (MAP) kinase pathway, leading to development of low grade noninvasive papillary urothelial carcinoma (Int J Clin Oncol 2008;13:287)
- Other genetic alterations: PIK3CA, loss of 11p or CCND1
Etiology
- Smoking (Int J Epidemiol 2016;45:857)
- Occupational exposure to chlorinated hydrocarbons, polycyclic aromatic hydrocarbons and aromatic amines (Eur Urol 2014;66:59)
- Arsenic exposure (Cancer Epidemiol Biomarkers Prev 2014;23:1529)
Clinical features
- Most common presentation: painless hematuria (gross or microscopic)
- Gross hematuria associated with more advanced pathologic stage (BJU Int 2016;117:783)
- Disease associated death and progression is rare (< 5%)
- Recurrence common (48 - 71%)
Diagnosis
- Cystoscopy: exophytic lesion, solitary or multiple, with varying size
- CT urography or ultrasound
- Urine cytology
Radiology description
- CT urography shows hydronephrosis and filling defects (Abdom Radiol (NY) 2018;43:663)
- Ultrasound can detect hydronephrosis and any intraluminal bladder masses
Prognostic factors
- WHO / ISUP histologic grade
- Concomitant urothelial carcinoma in situ: higher recurrence rate
- Multifocal disease: higher disease associated mortality and progression
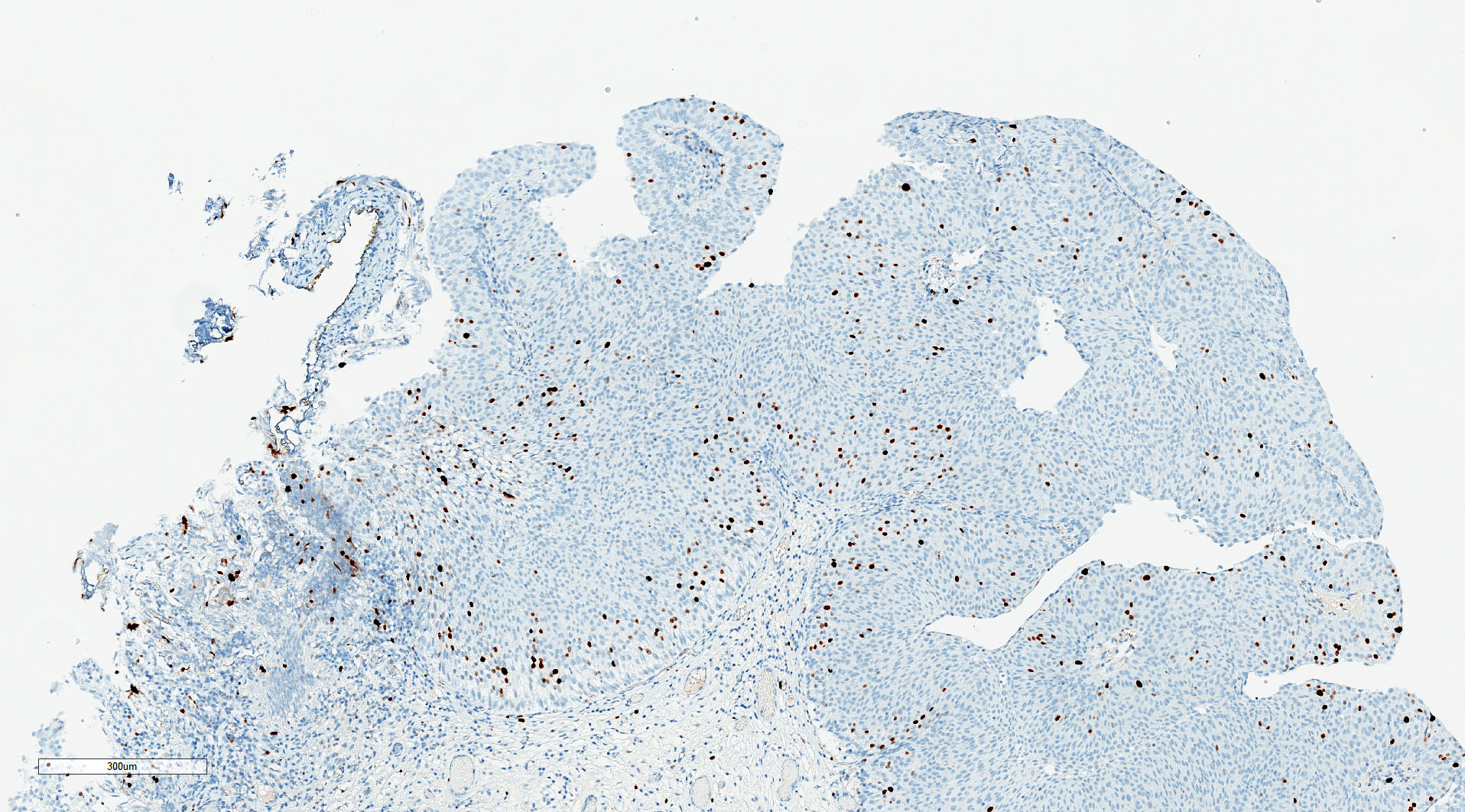
- High Ki67: poor prognosis (Int J Mol Sci 2018;19:2548)
- Mutations in FGFR3 and PIK3CA lower recurrence rate (Cancer Res 2006;66:7401)
- PTEN deletions: increased recurrence rate (Virchows Arch 2018;472:969)
Case reports
- 31 year old man with low grade papillary noninvasive urothelial carcinoma mimicking xanothogranulomatous pyelonephritis (Int J Immunopathol Pharmacol 2020;34:2058738420925720)
- 49 year old woman with urachal low grade noninvasive papillary urothelial carcinoma (BMJ Case Rep 2013;2013:bcr2013200635)
- 75 year old woman with multicentric synchronous low grade noninvasive papillary carcinoma involving vagina, bladder and renal pelvis (Virchows Arch 2017;471:347)
Treatment
- Surgical: transurethral resection
- Adjuvant: usually not indicated for low grade
- Mitomycin C
Gross description
- Exophytic papillary lesions, single or multiple; can vary greatly in size
Frozen section description
- Papillary lesion with fibrovascular core, low grade nuclear features
- Infrequent mitoses, basal / suprabasal location
- Reference: Taxy: Biopsy Interpretation - The Frozen Section, 2nd Edition, 2013
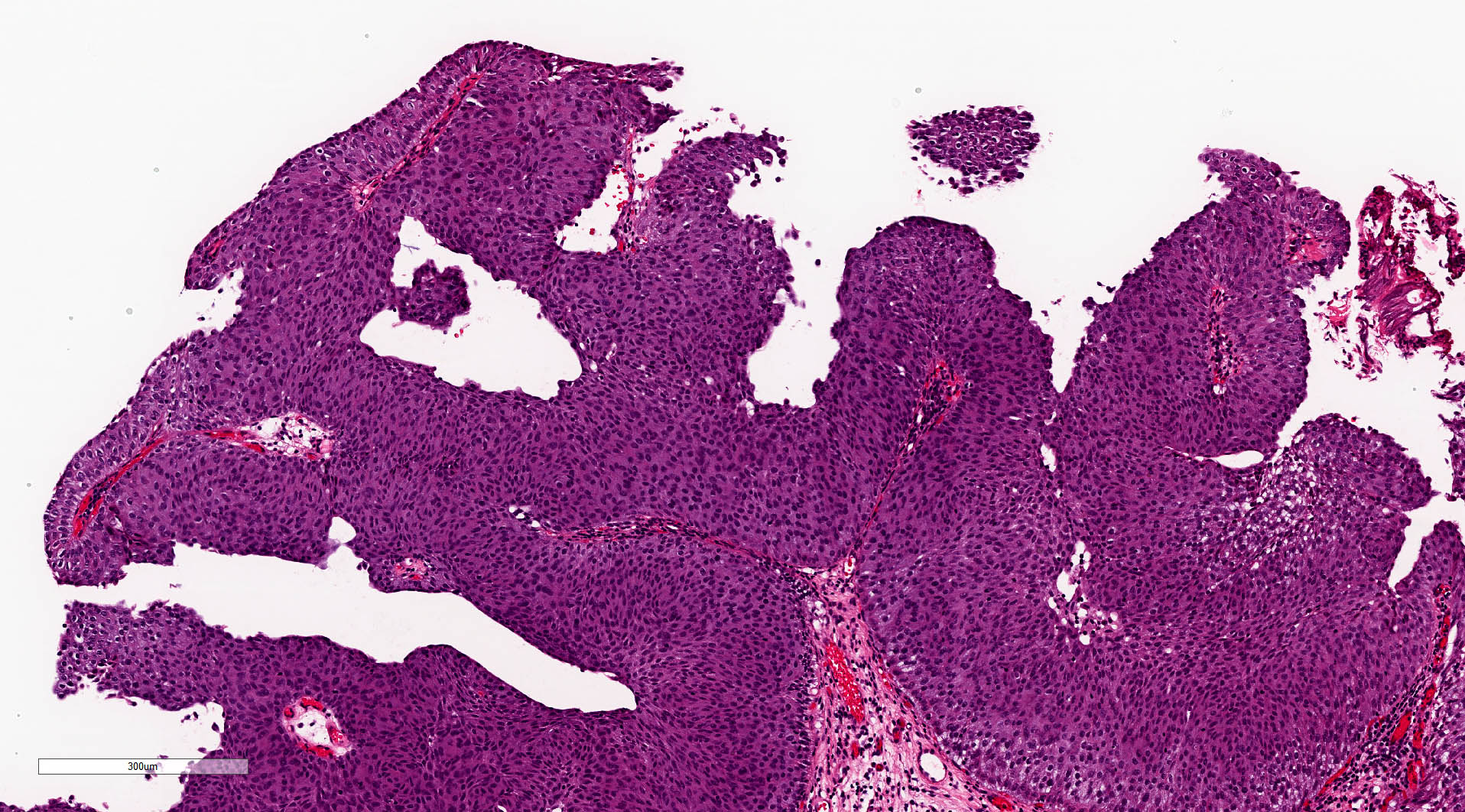
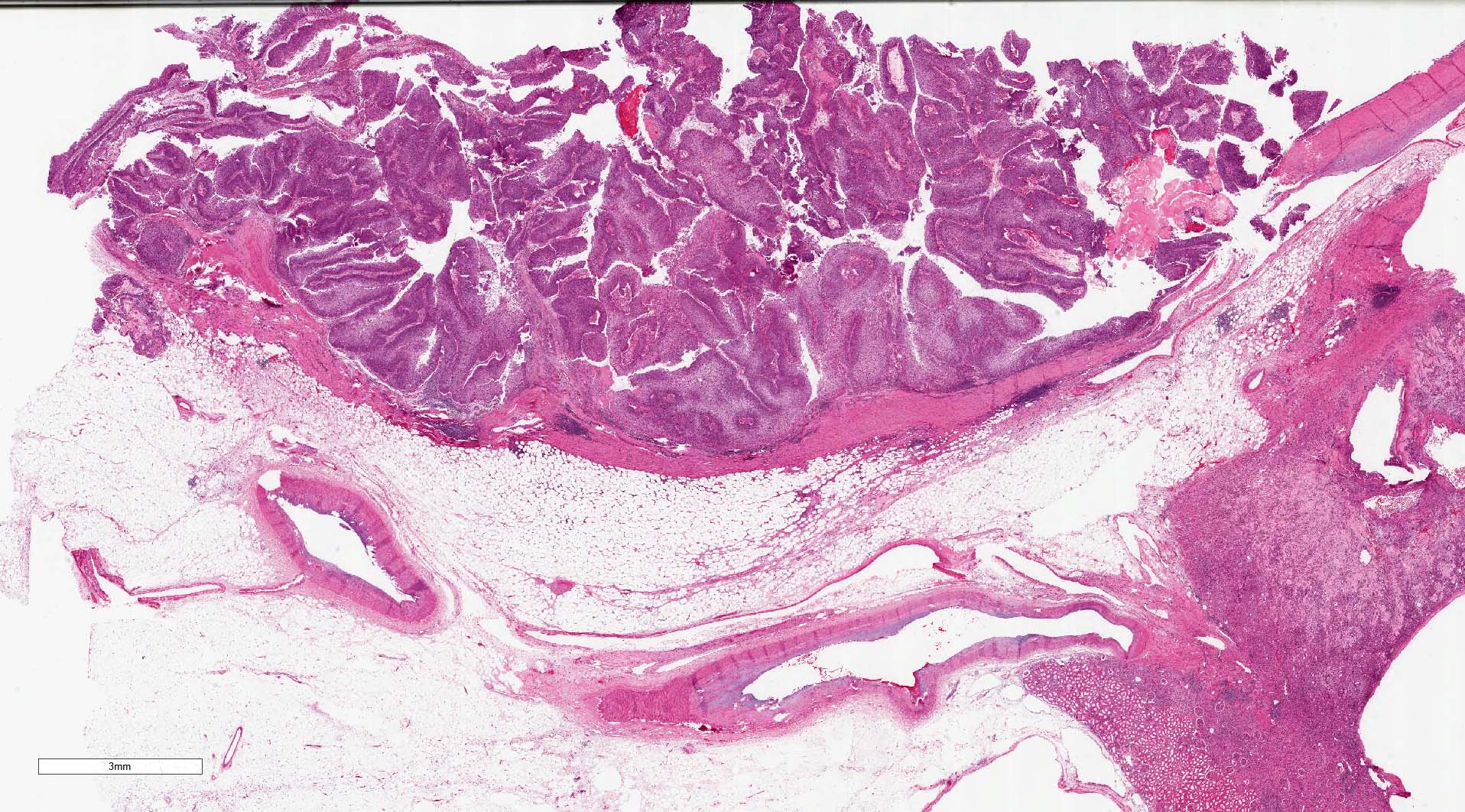
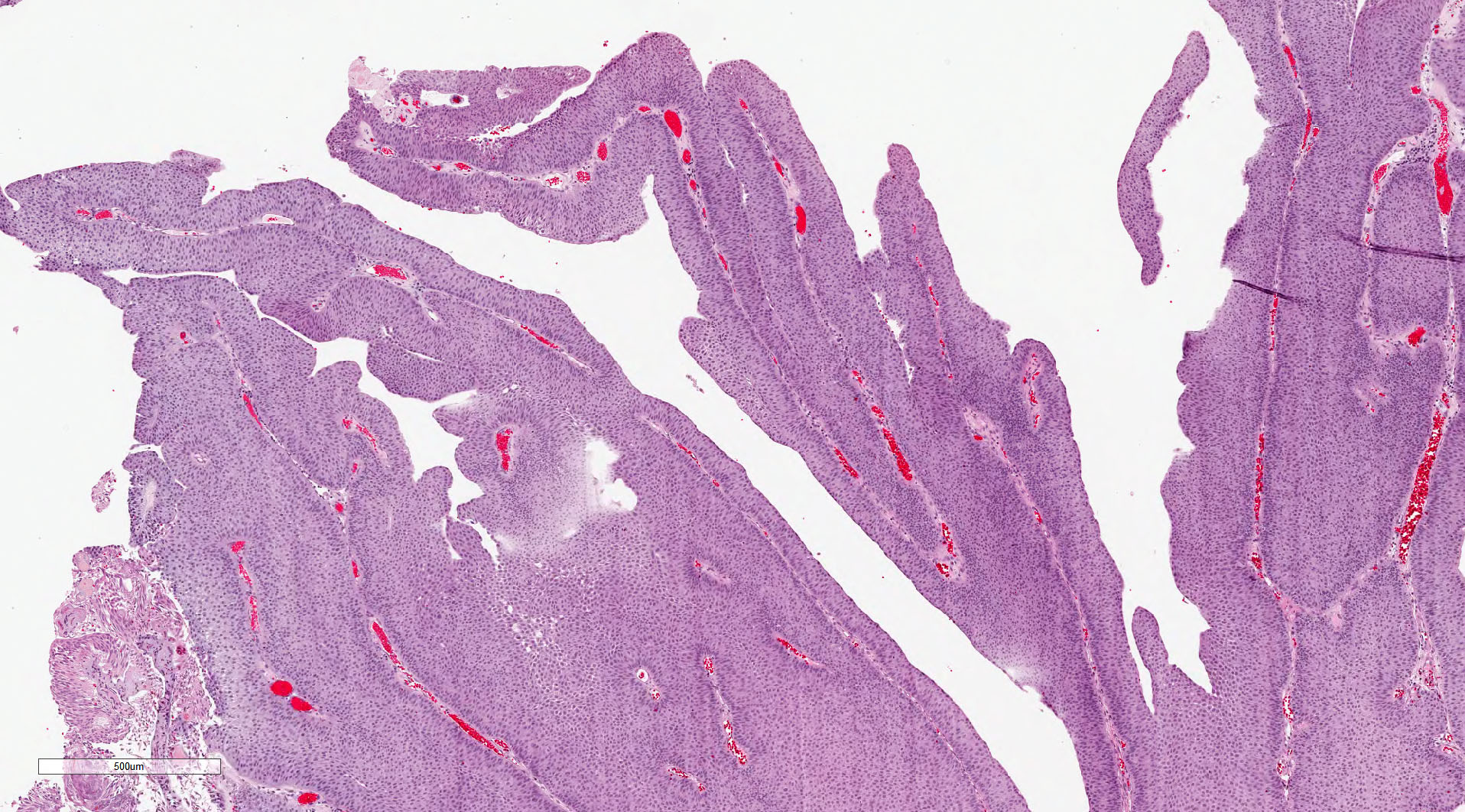
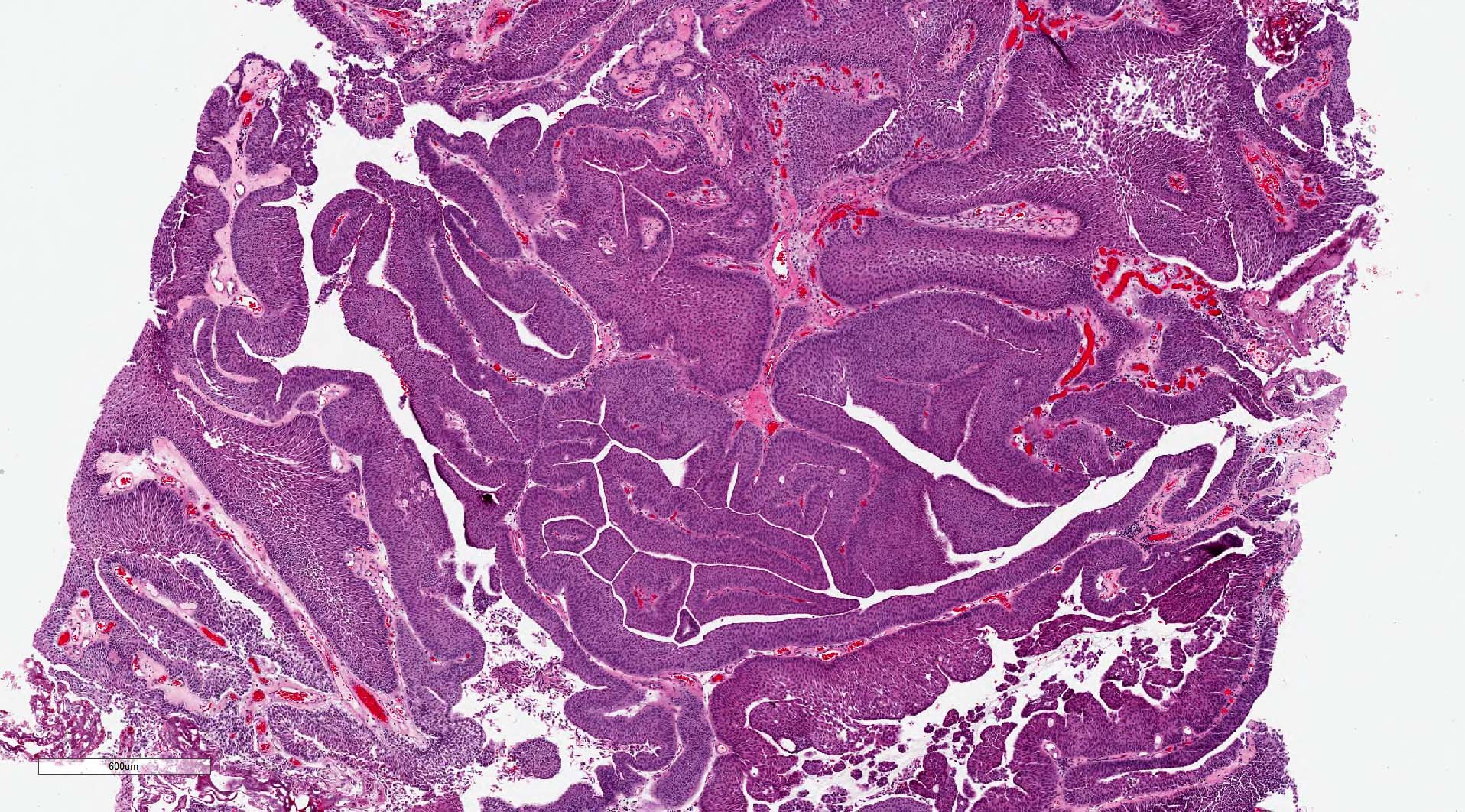
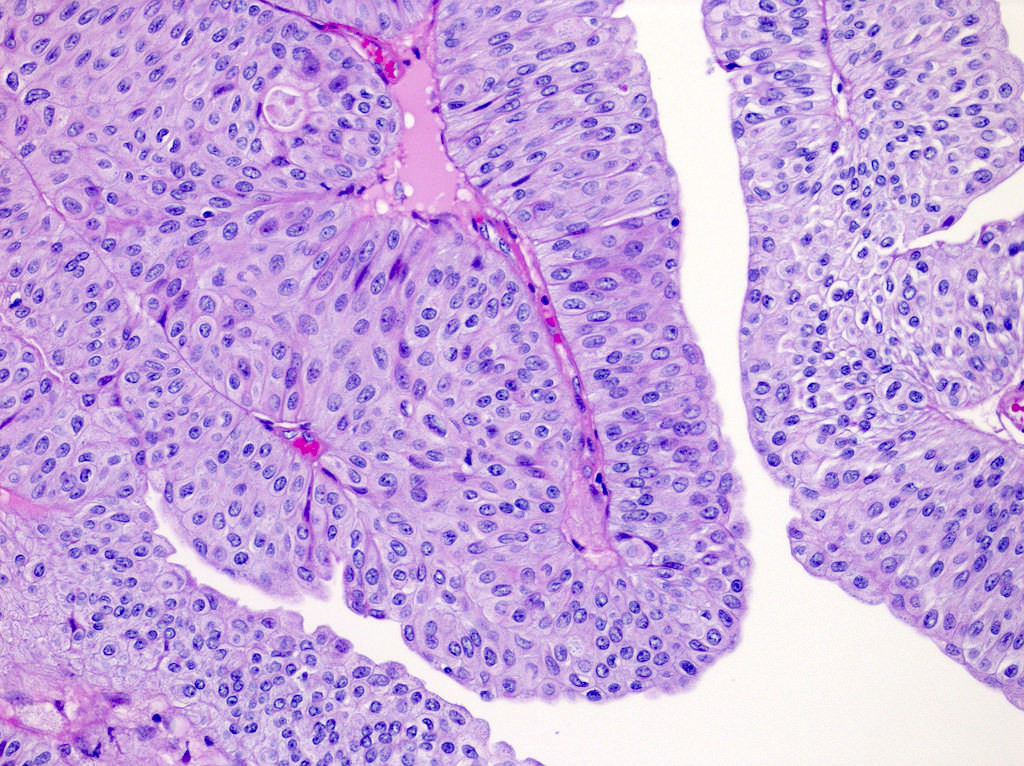
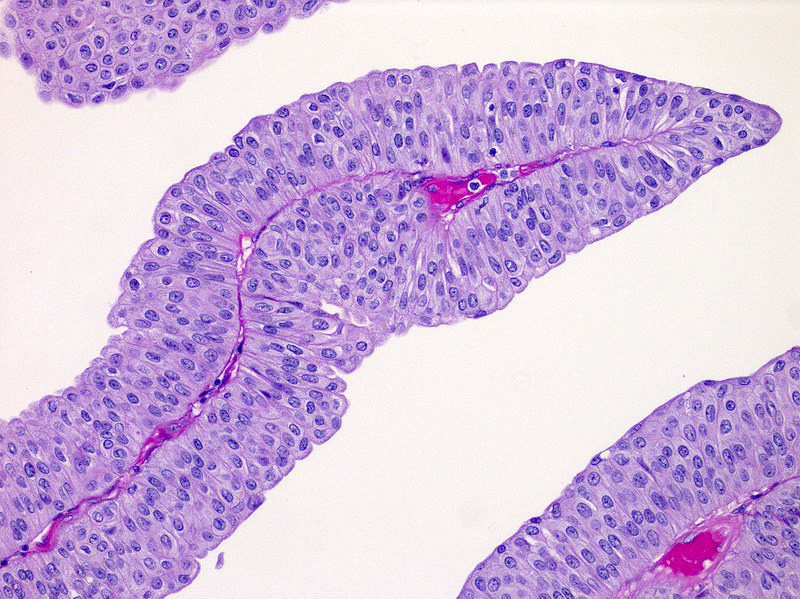
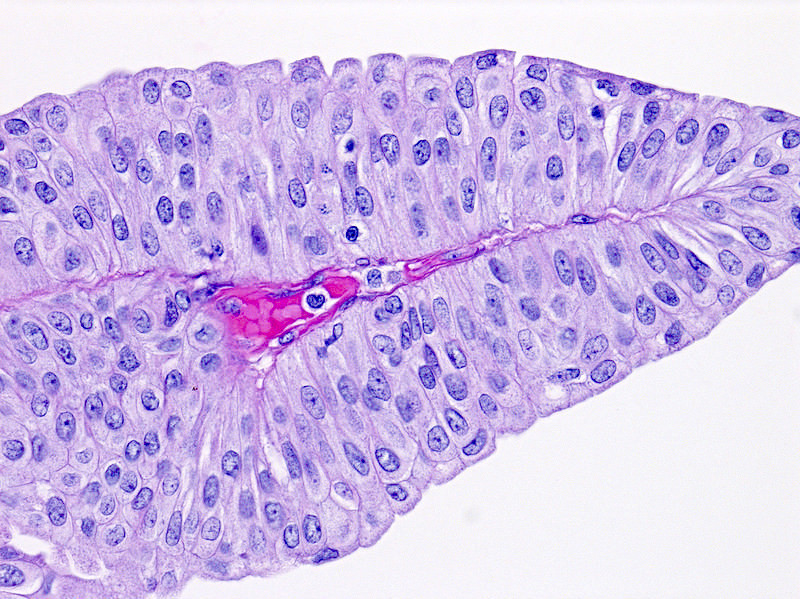
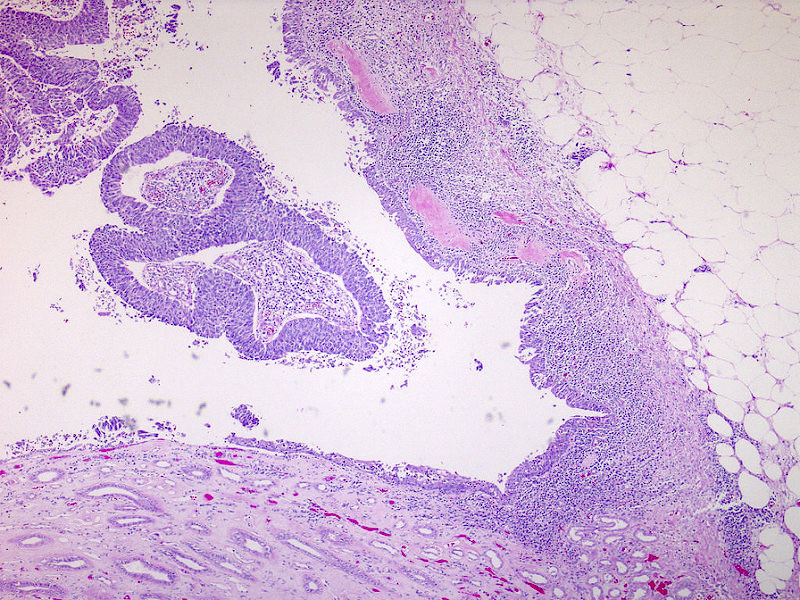
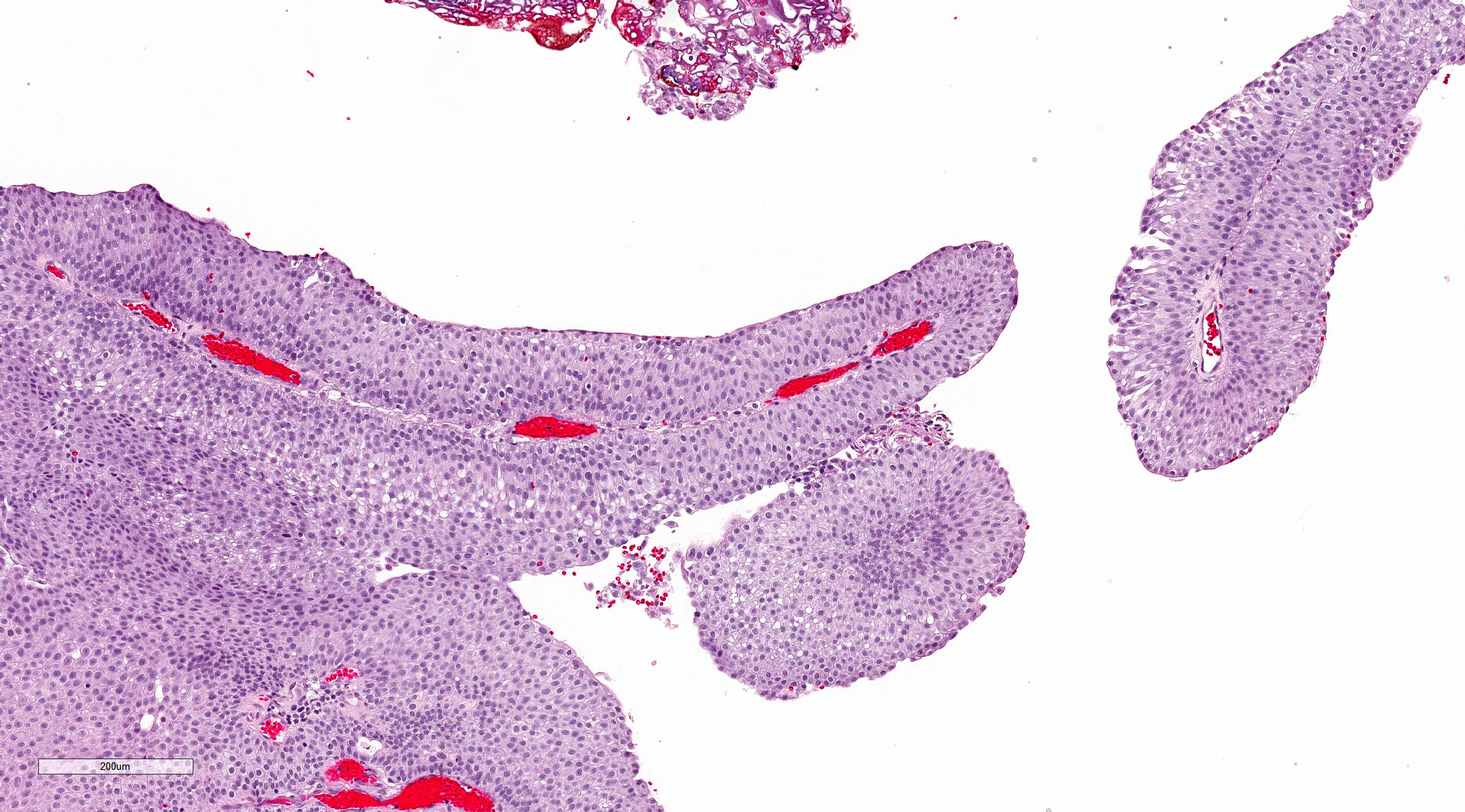
Microscopic (histologic) description
- Neoplastic urothelium lining fibrovascular cores
- Long, slender papillae with minimal fusing or branching
- Orderly architecture at low magnification, some loss of polarity and mild pleomorphism at medium magnification
- Cells generally uniform in size, may have slight variation but no significant nuclear pleomorphism or nucleomegaly, occasional slight irregularities in nuclear contour
- Mitoses may be present but not atypical and usually confined to lower half of urothelium
- Inverted growth pattern (exophytic and endophytic components) may be present
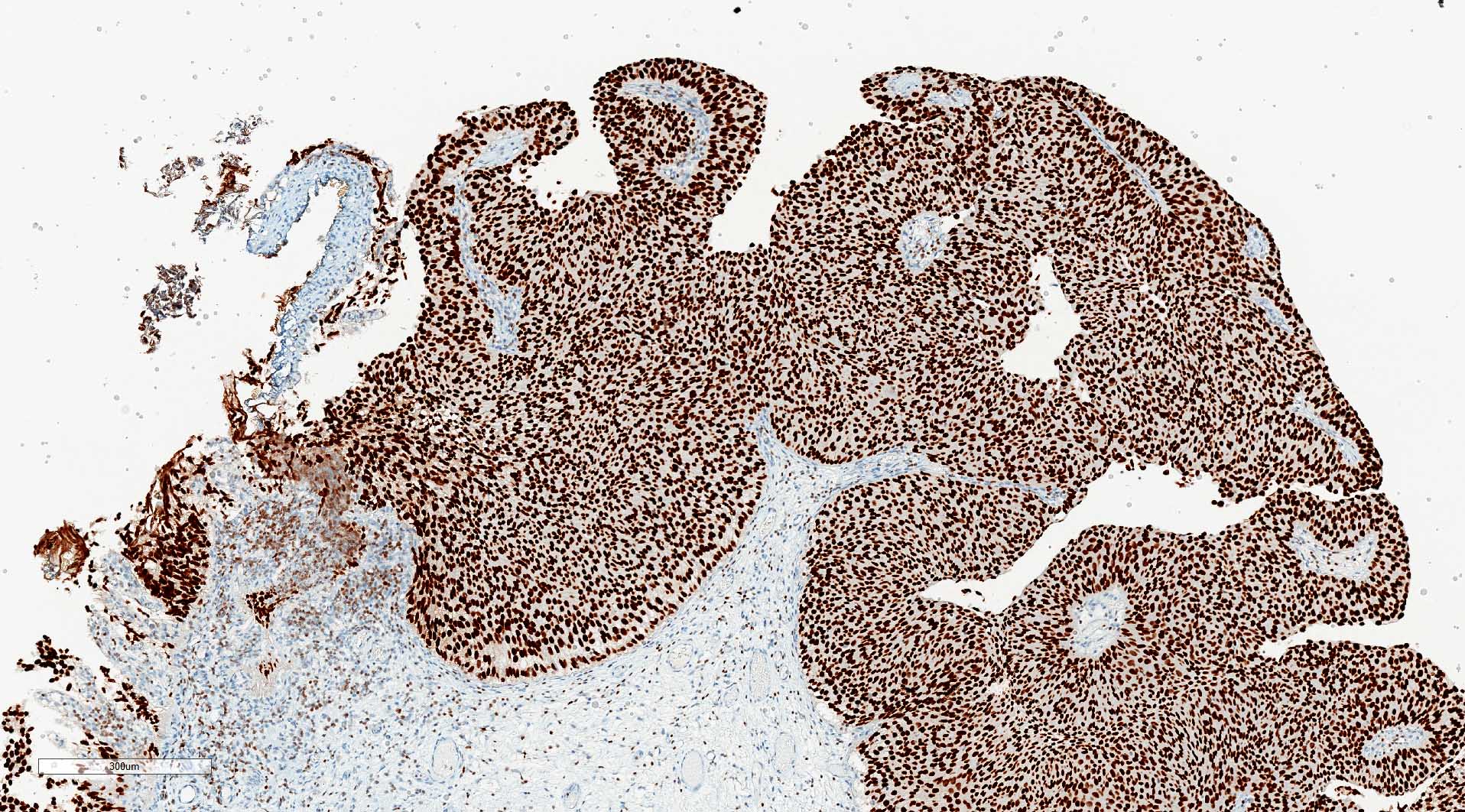
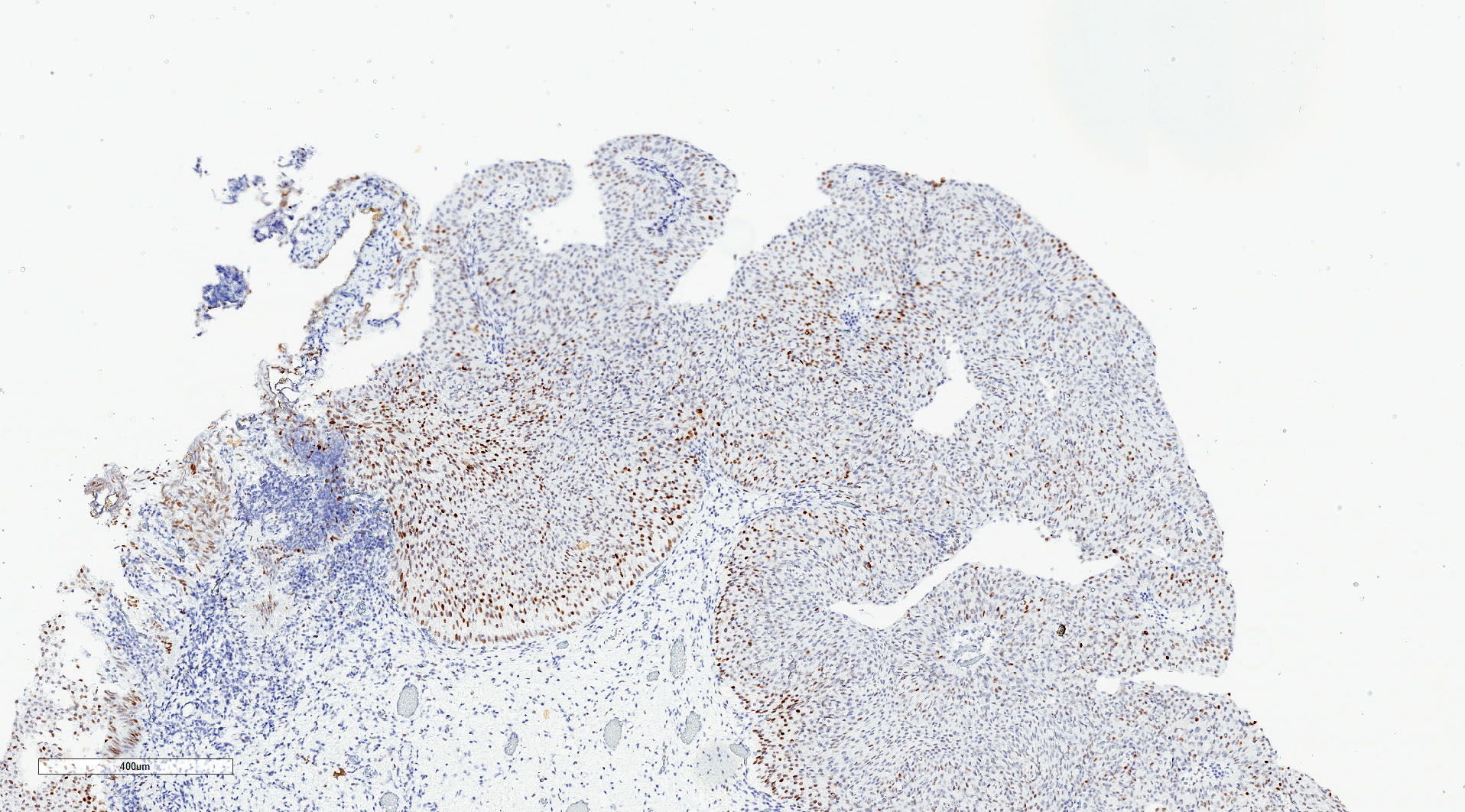
Microscopic (histologic) images
Contributed by Michelle R. Downes, M.D., Nicole K. Andeen, M.D. and Maria Tretiakova, M.D.
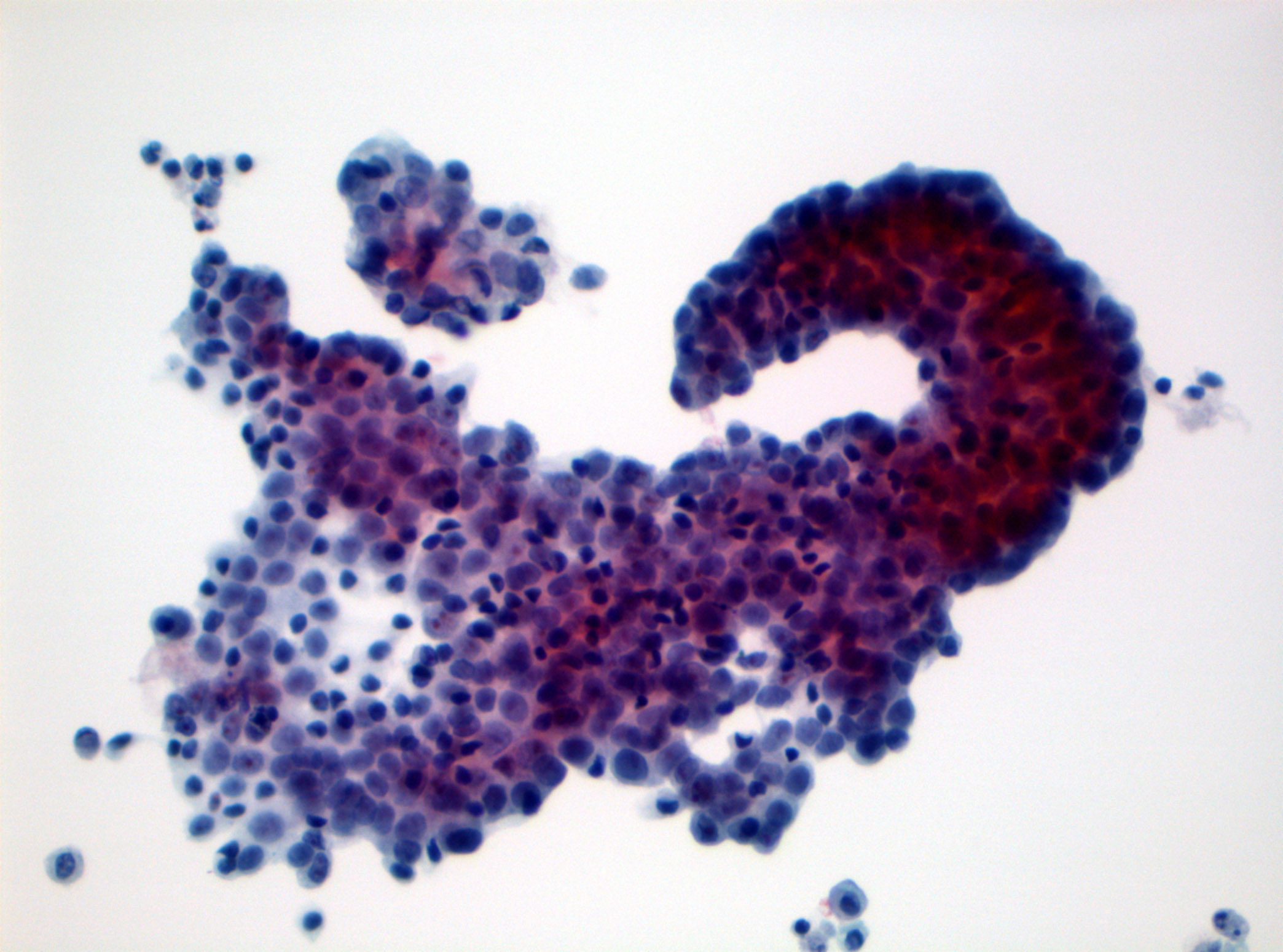
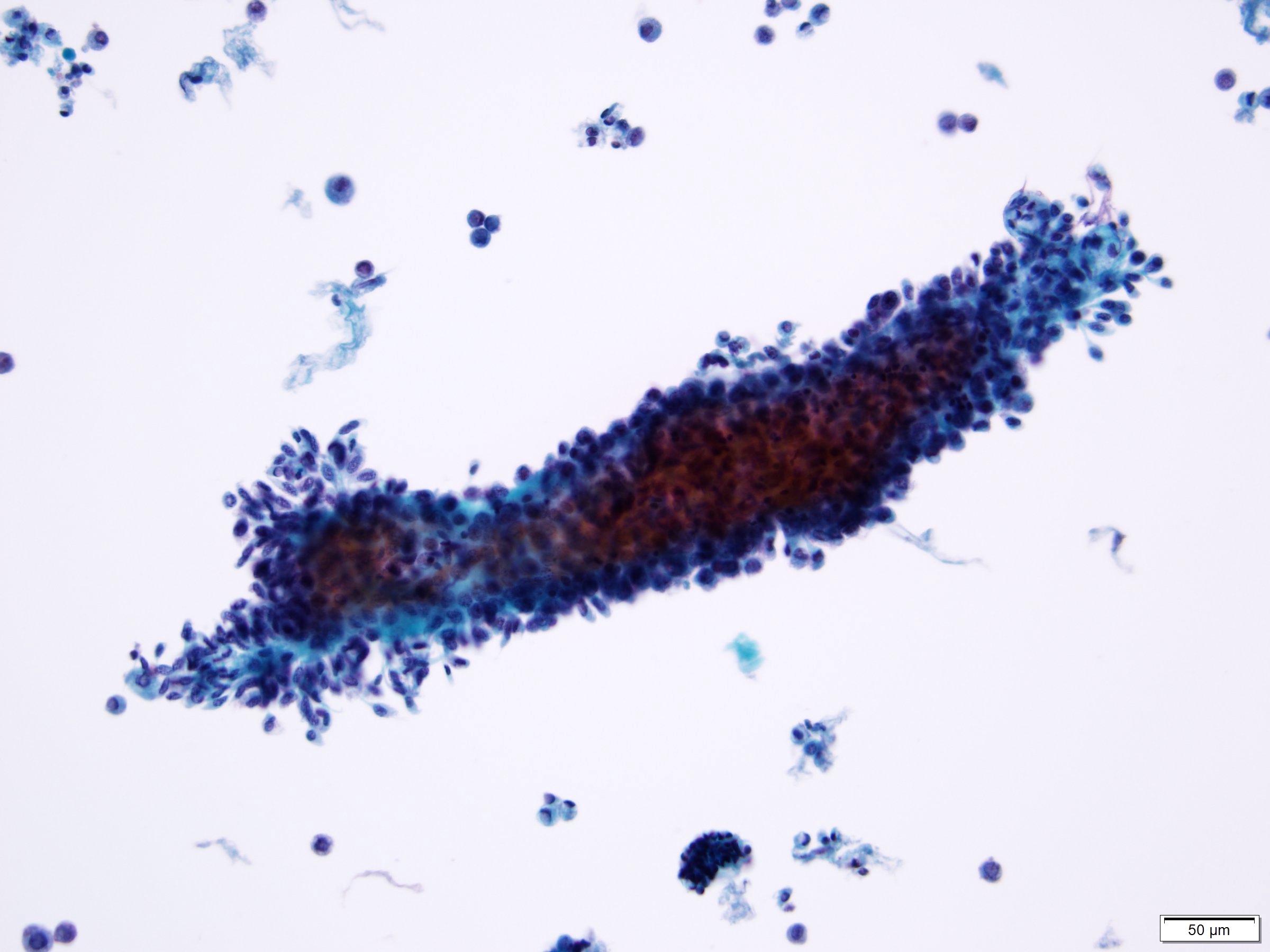
Cytology description
- Lower sensitivity in low grade tumors compared with high grade (Urol Oncol 2015;33:66.e25)
- 2016 Paris Working Group reporting system recommended
- 3 dimensional cellular clusters or papillae with fibrovascular cores
- Increase in monotonous single cells with increased nuclear/cytoplasmic ratio and irregular nuclear contours
- For additional information, refer to the topic cytology-neoplastic
Cytology images
Positive stains
- GATA3: 97.5% in papillary lesions (SpringerLink: GATA-3 Expression in all Grades and Different Variants of Primary and Metastatic Urothelial Carcinoma [Accessed 5 April 2021])
- p63: 100% in noninvasive papillary carcinoma (Am J Surg Pathol 2014;38:e20)
- High molecular weight cytokeratin (Cancer 2003;97:1876)
- CK5/6: basal layer (Adv Urol 2020;2020:4920236)
- CK7 (Bratisl Lek Listy 2013;114:431)
Negative stains
- STAG2 in upper tract urothelial cancer (Ann Surg Oncol 2017;24:4059)
- Mismatch repair (MMR) protein (MLH1, MSH2, PMS2, MSH6) is lost in mismatch repair deficient tumors (Lynch syndrome)
Electron microscopy description
- Subset with urothelial eddies show microvillous projections and increased intercellular space (Int J Clin Exp Pathol 2013;6:1458)
- Low grade papillary urothelial carcinoma has zonula occludens (tight junctions) and well developed macula adherens (desmosomes), with fewer surface vesicles than normal epithelium
Molecular / cytogenetics description
- Activating mutations in FGFR3
- Somatic mutations in TERT promoter in 50% of low grade papillary noninvasive urothelial carcinomas; more commonly associated with FGFR3 mutated tumors (Histopathology 2018;72:795)
- Inactivating mutations in cohesion complex gene STAG2 in 32 - 36% noninvasive urothelial carcinomas; associated with low histologic grade and low tumor stage (Ann Surg Oncol 2017;24:4059)
- PIK3CA (25% cases) TSC1, HRAS, APC
- Epigenetic silencing of tumor suppressor genes through promoter hypermethylation: RUNX3, CDKN2A, MLH1, MGMT, VHL, DAPK, TBX2, TBX3, GATA2, ZIC4, GSTP1, CDH1 (Eur Urol 2012;61:1245, Nat Rev Urol 2013;10:327)
- MicroRNA alterations (J Pak Med Assoc 2018;68:759)
- Loss of chromosome 9 (9q and 9p in low grade)
Videos
Urothelial carcinoma, papillary and invasive
Sample pathology report
- Bladder, lesion, transurethral resection:
- Noninvasive papillary urothelial carcinoma, low grade
- Muscularis propria is present
Differential diagnosis
- Papillary urothelial neoplasm of low malignant potential (PUNLMP):
- Similar appearance at low and intermediate power
- No architectural or cytologic abnormalities (lacks variation in nuclear size / shape and polarity is maintained)
- Noninvasive papillary urothelial carcinoma, high grade:
- High grade features present, although may be focal
- Nucleomegaly, nuclear pleomorphism, irregular nuclear contours and clumped chromatin
- Mitoses readily identifiable
- Polypoid cystitis:
- Edematous or fibrotic papillary cores
- Broad base papillary excrescences
- Reactive epithelial changes may be present
- Urothelial papilloma:
- Papillary lesions with normal nondysplastic urothelium
- No cytologic atypia
- Inverted papilloma:
- Endophytic growth pattern of urothelium into lamina propria
- Degenerative atypia may be present
Additional references
Board review style question #1
A transurethral resection of bladder was performed on a 62 year old man. Histological examination showed a noninvasive papillary lesion. Which of the following is true about the lesion depicted above?
- Immunohistochemistry is helpful for diagnosis
- Mitoses are rare and usually confined to lower half of urothelium
- Nuclear pleomorphism is marked
- Progression to invasive disease is common
Board review style answer #1
B. Mitoses are rare and usually confined to lower half of urothelium. Diagnosis: low grade noninvasive papillary urothelial carcinoma.
Comment Here
Reference: Noninvasive papillary urothelial carcinoma low grade
Comment Here
Reference: Noninvasive papillary urothelial carcinoma low grade
Board review style question #2
Board review style answer #2
D. Low grade noninvasive papillary urothelial carcinoma
Comment Here
Reference: Noninvasive papillary urothelial carcinoma low grade
Comment Here
Reference: Noninvasive papillary urothelial carcinoma low grade