Table of Contents
Definition / general | Essential features | Physiology | Diagrams / tables | Clinical features | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Electron microscopy description | Videos | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Sardana R, Parwani A. Histology. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/bladderhistology.html. Accessed March 28th, 2025.
Definition / general
- Hollow muscular elastic organ that sits on the pelvic floor and stores urine
Essential features
- Layers of bladder wall (from inside out)
- Urothelium: specialized stratified lining epithelium, impermeable barrier
- Lamina propria: connective tissue containing vessels, lymphatics, nerve endings and a few elastic fibers
- Muscularis propria: also called detrusor muscle; consists of 3 layers (inner longitudinal, middle circular and outer longitudinal)
- Serosa / adventitia: serosa is loose connective tissue covering bladder dome; the remaining area is covered by adventitia
- Important to histomorphologically differentiate the layers in order to properly stage the tumors, determine therapy and estimate survival
Physiology
- Located in the extraperitoneal space of the pelvis, behind the pubic bones (StatPearls: Histology, Bladder [Accessed 14 April 2022])
- Extends into the abdomen when distended
- 2 main parts
- Upper part is above the ureteric orifices and is composed of the apex and body
- Lower part is beneath the ureteric orifices and is composed of the fundus, trigone and neck
- Urothelium is 5 - 7 cell layers thick in a contracted bladder and 2 - 3 cells thick in a distended bladder (Am J Physiol Renal Physiol 2009;297:F1477)
Clinical features
- Urothelium is exclusive to the conducting passages of the urinary system (renal pelvis, ureter, bladder, upper urethra and prostatic ducts) (Am J Physiol Renal Physiol 2009;297:F1477)
- > 90% of bladder carcinomas arise from the urothelium, mostly from the posterior wall of the bladder (Nat Cell Biol 2014;16:982)
- In practice, sampling tangentially to the basement membrane can generate an artificially thick mucosa, hence urothelial thickness is of low utility in the assessment of urothelial neoplasms
- Squamous epithelium is common in the trigone area of females; abundant intracytoplasmic glycogen and lack of keratinization makes it histologically similar to vagina or cervix (Am J Anat 1962;111:319)
- von Brunn nests, cystitis cystica and cystitis glandularis represent a continuum of proliferative or reactive changes
- von Brunn nests (proliferative cystitis)
- Reactive proliferative change is present in 85 - 95% of bladders; frequency increases with age; more common at the trigone
- Nests of cytologically benign urothelium in lamina propria; with regular spacing and same extent to horizontal level at base of proliferation
- Bladder wall urachal remnants: cystically dilated epithelial lined structures are sometimes found in biopsies from the dome or anterior wall of the bladder
Gross description
- Hollow muscular viscus resembling an inverted pyramid when empty and a sphere when distended (Microbiol Spectr 2015;3:10)
- Flat internal (mucosal) surface when distended; throws into abundant folds when empty
- Lies posterior to the pubic bone, anterior to the uterus in females and anterior to the rectum in males
- Partially retroperitoneal, with its peritoneal covered dome projecting into the abdomen when fully distended
- Triangular shaped area at the base of the bladder called the trigone
Microscopic (histologic) description
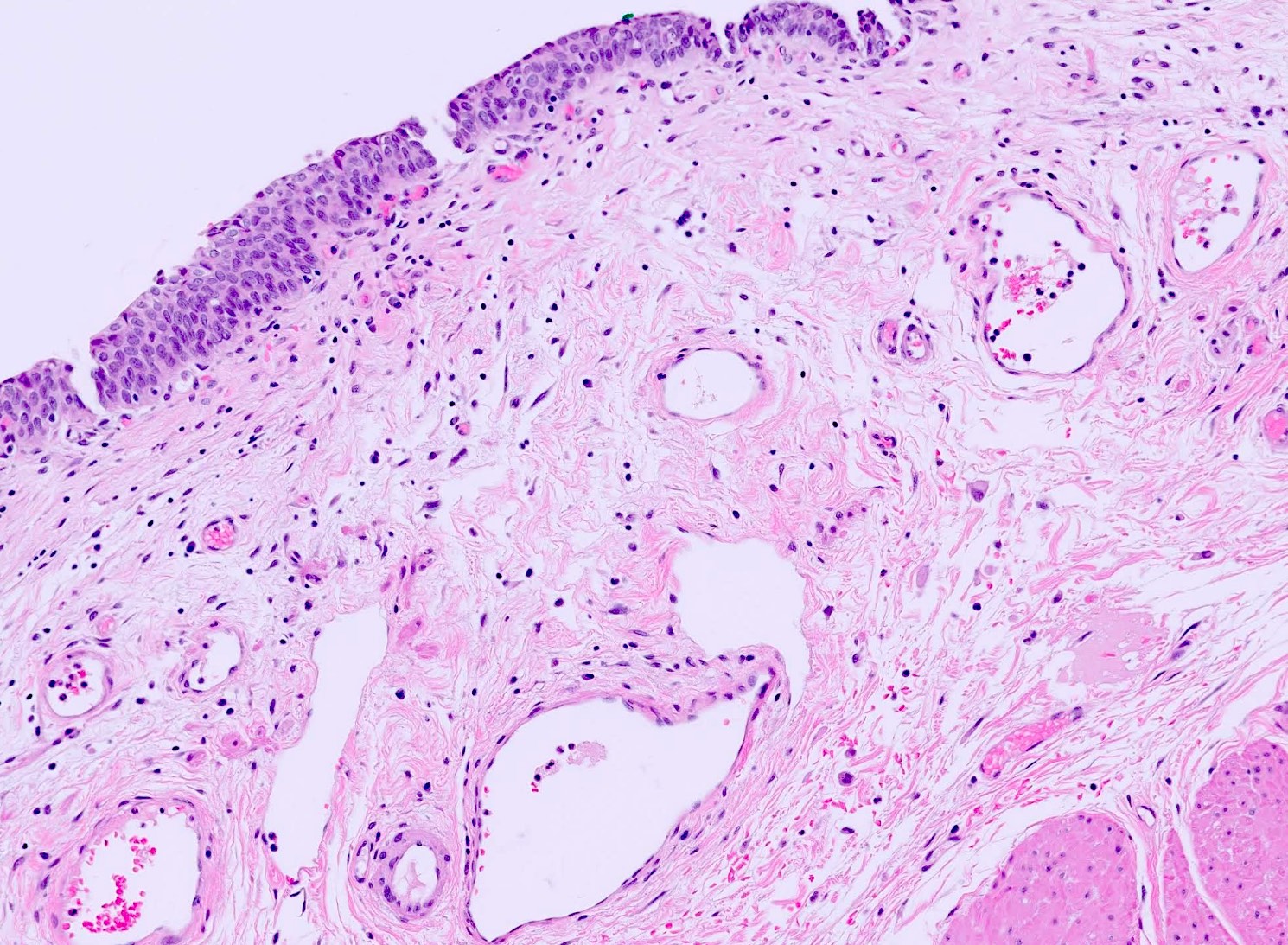
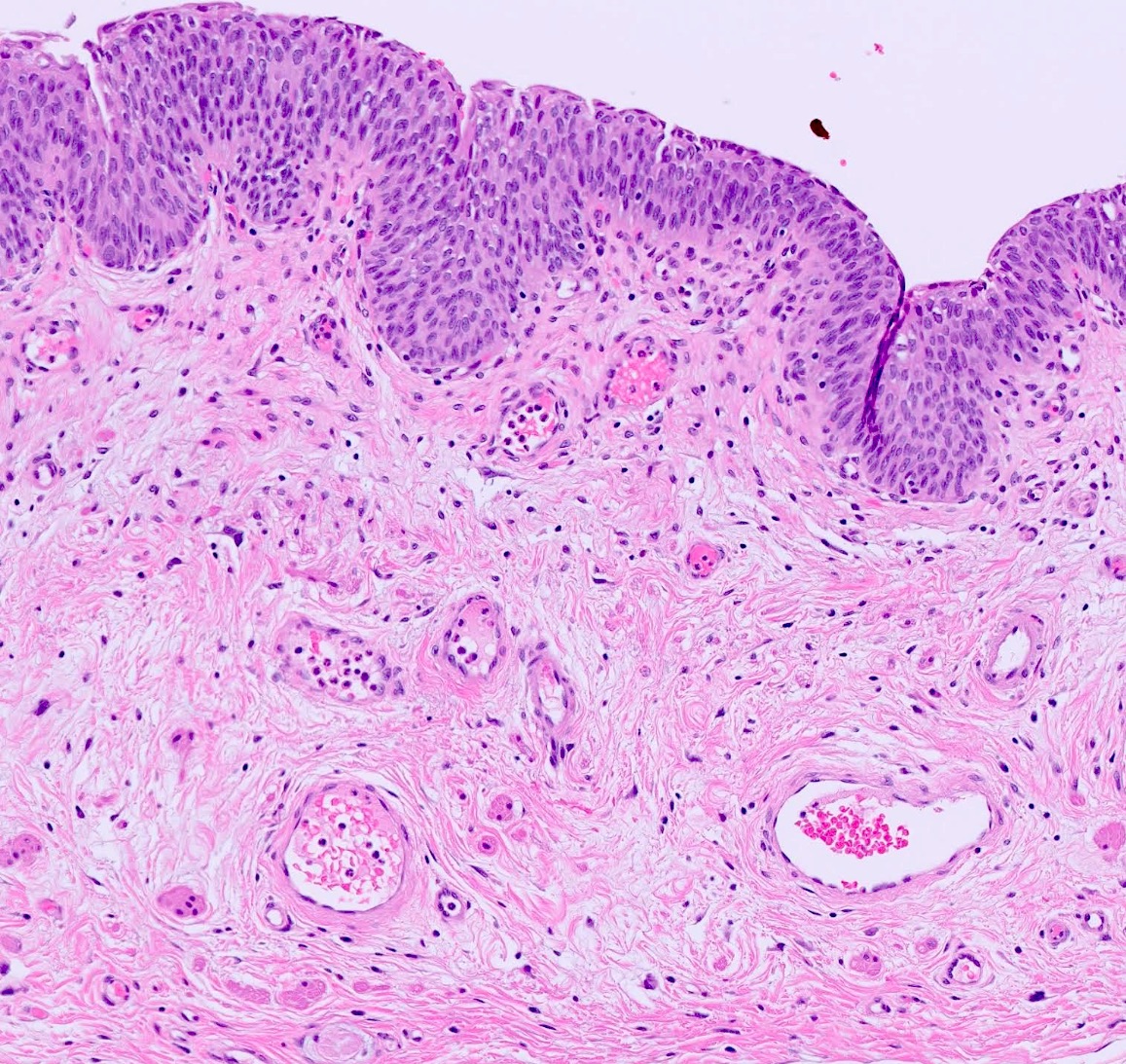
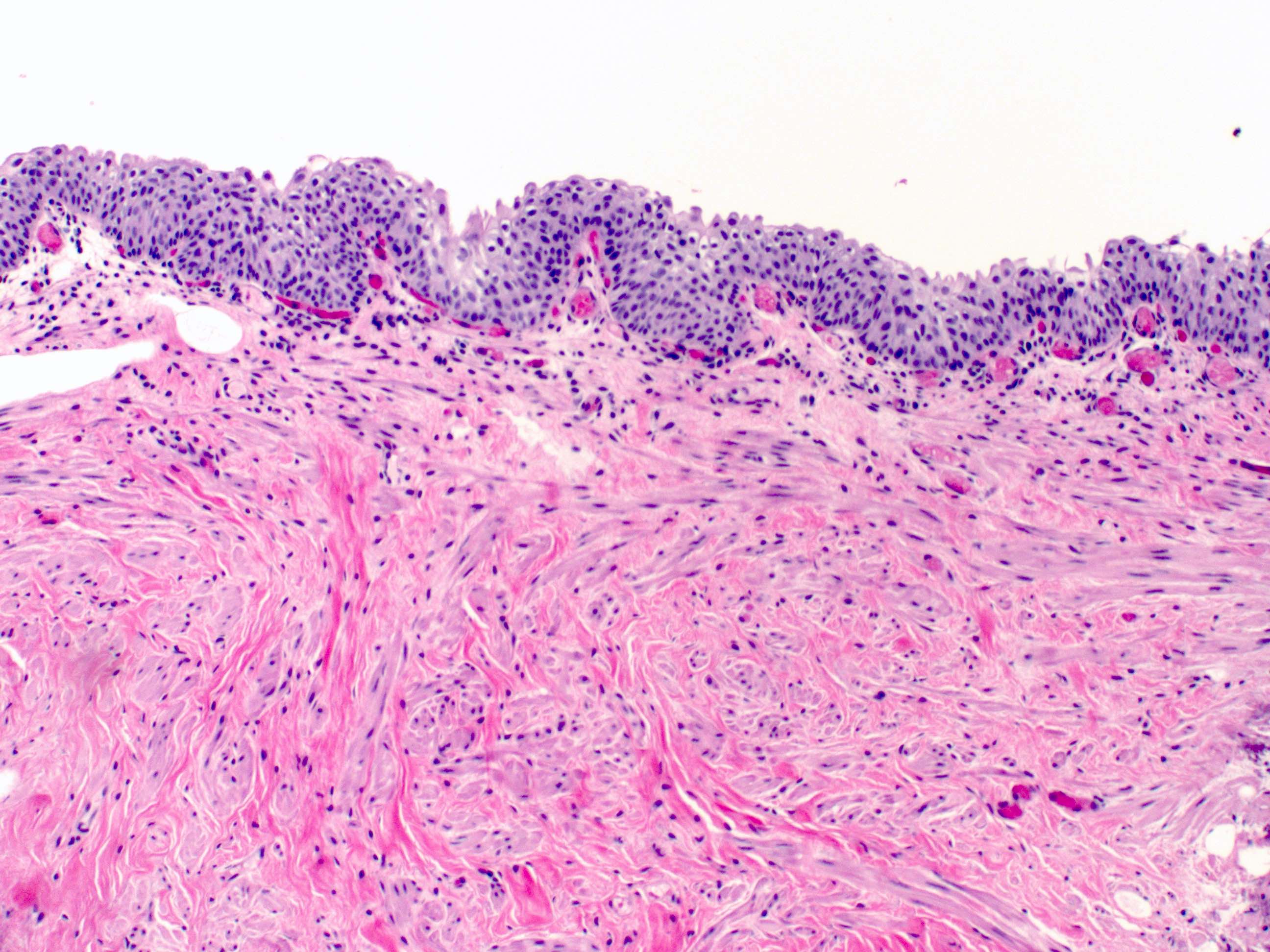
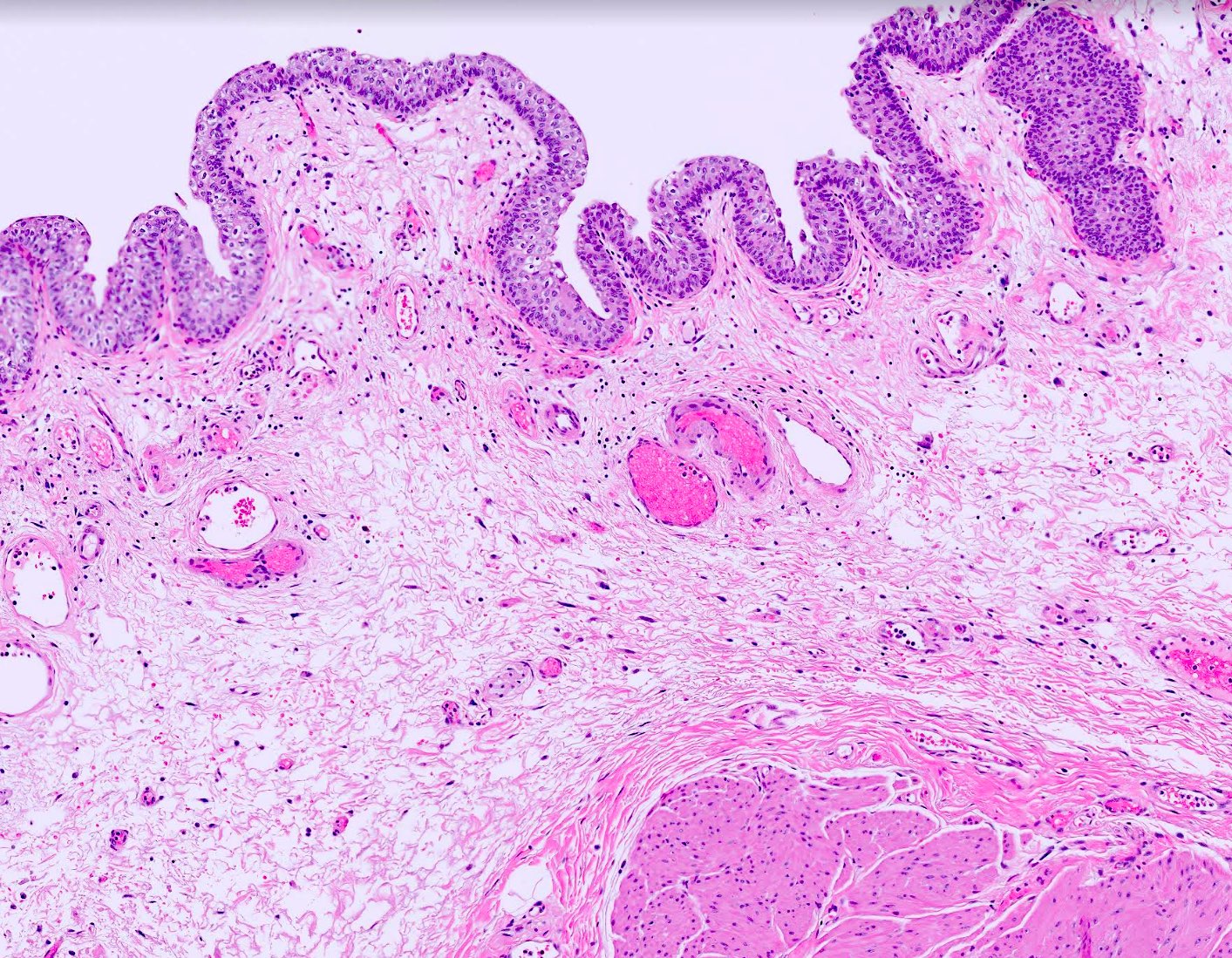
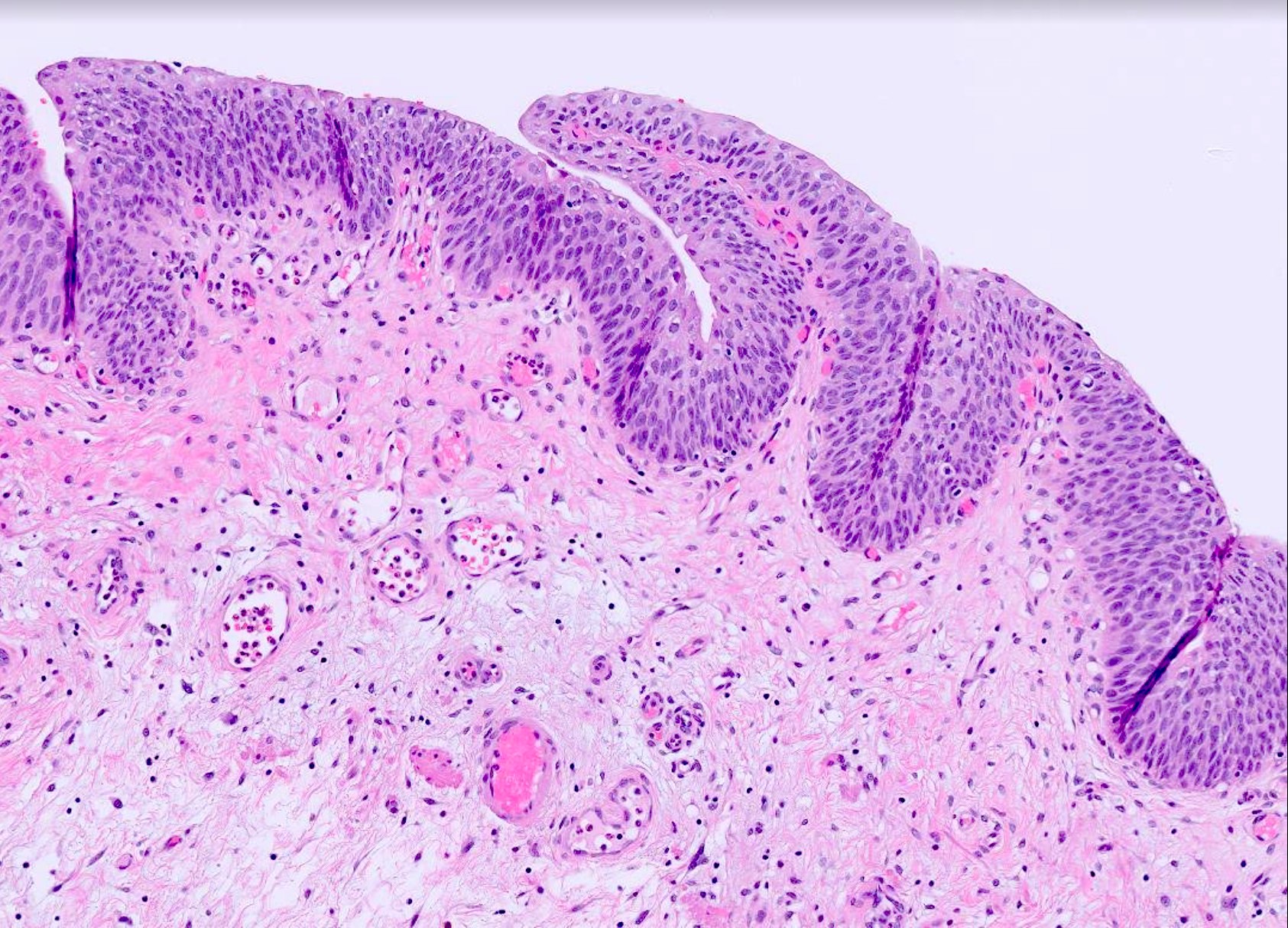
- 4 layers (from inside out): urothelium, lamina propria, muscularis propria, serosa / adventitia
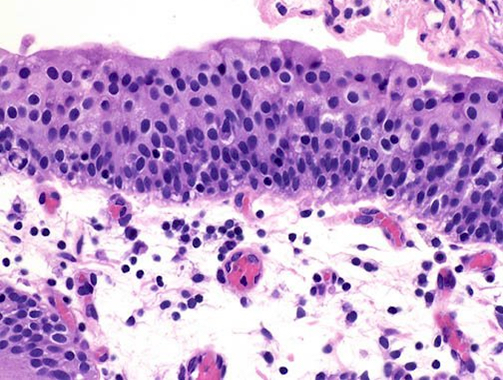
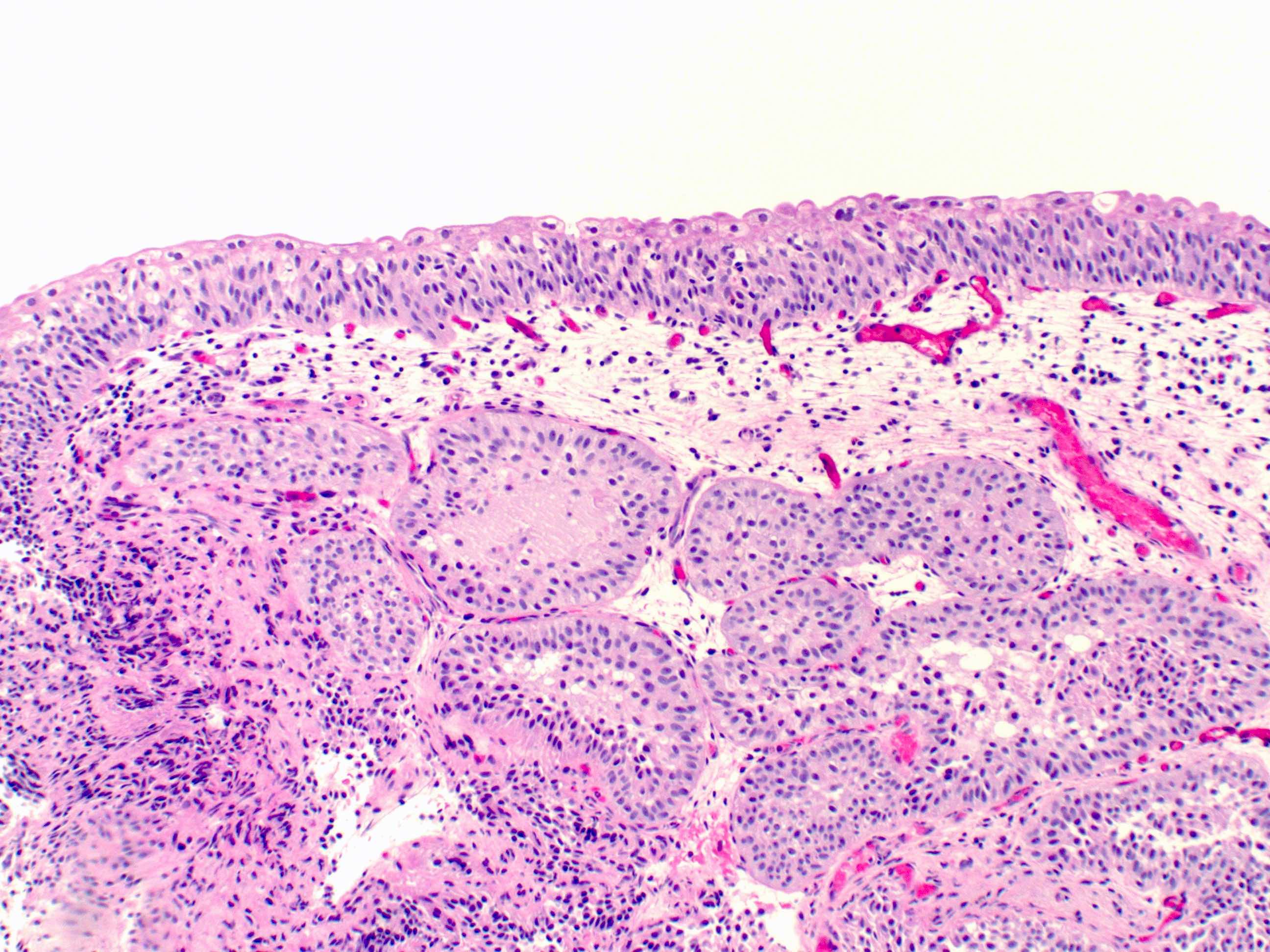
- Urothelium: 3 layers of cells
- Umbrella / apical cells (superficial layer)
- Formerly called transitional epithelium, intermediate between nonkeratinizing squamous and pseudostratified columnar epithelium
- Dome / pyramid shaped, large and ovoid, frequently binucleated cells with abundant eosinophilic cytoplasm
- Scalloped surface outline often overlapping 2 or more of the underlying cells
- Superficial cytoplasm is fuzzy, indistinct and more intensely stained than the rest of the cytoplasm
- Luminal surface of the cells appears thickened and more densely stained
- Form an impermeable barrier; tight junctions between the cells decrease paracellular flux while uroplakins form a superficial plaque
- Intermediate cells
- Multicell layering, depending on the stage of distension
- Cuboidal to low columnar with well defined borders and amphophilic cytoplasm that is rich in glycogen
- Uninucleated cells: ovoid nuclei with fine granular chromatin, no mitotic figures arranged regularly along the long axis at right angles to surface
- Basal cells
- Single layer in contact with basal lamina
- Mononucleated, cuboidal cells with mitotic capability
- Cylindrical, can be flat when bladder wall is stretched; some have longitudinal nuclear grooves
- Gradual turnover but significant regenerative ability
- Umbrella / apical cells (superficial layer)
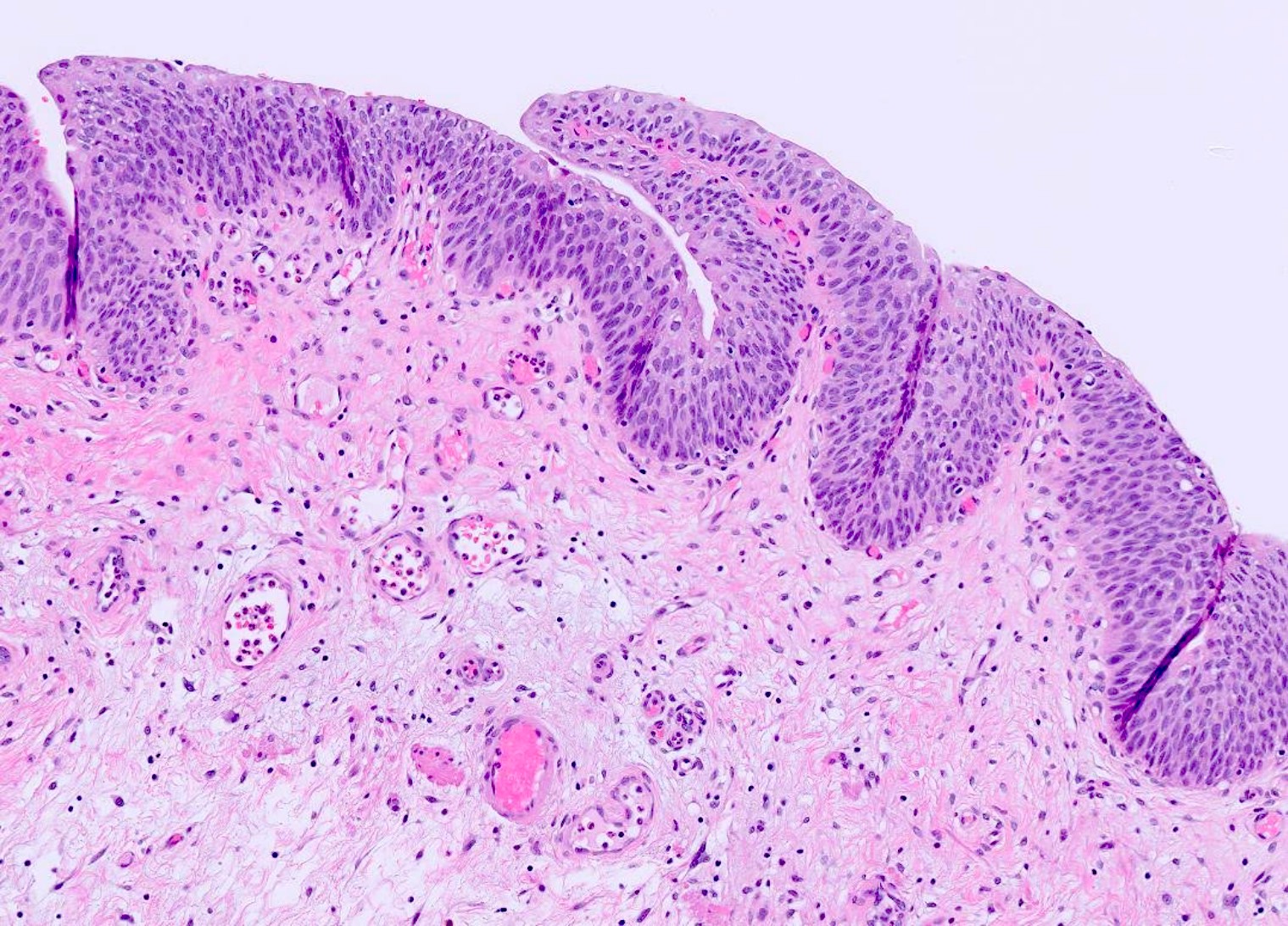
- Lamina propria
- Dense connective tissue containing a rich vascular network, lymphatic channels, sensory nerve endings, elastic fibers and interspersed adipose tissue
- Forms thick mucosal folds when the viscus is contracted
- Thickness varies with the degree of distention and is generally thinner in the areas of the trigone and bladder neck
- Discontinuous isolated bundles of muscularis mucosa (wisps of smooth muscle) may be present; 5% of bladders may have a well developed, continuous muscularis mucosa (Am J Surg Pathol 1987;11:668)
- Hyperplastic muscularis mucosa (more common in women) may resemble muscularis propria (Am J Surg Pathol 2007;31:1420, Ann Diagn Pathol 2007;11:395)
- Important to distinguish muscularis mucosa from muscularis propria for accurate staging; smoothelin antibody is negative, while vimentin is positive in the former (Int J Biol Markers 2017;32:e305)
- Interstitial cells of Cajal act as nerve signal transducer between the smooth muscle cells and nerve endings
- Adipose tissue may be present within deep lamina propria (in small localized aggregates), while it is always found within muscularis propria; carefully differentiate between the two, especially in transurethral resection of bladder tumor (TURBT) specimens as it can overstage the tumor (Am J Surg Pathol 2000;24:1286)
- Muscularis propria
- 3 layers: inner and outer longitudinal layers and a central circular layer
- Layers are distinct near bladder neck, elsewhere there is no definite orientation
- Bladder's body has a higher smooth muscle content compared with the trigone
- Rarely nests or cords of paraganglia associated with nerves and vessels; clear or granular cytoplasm with round or vesicular nuclei
- Carefully distinguish from invasive carcinoma
- Cytokeratin negative and chromogranin positive
- Significantly thickened in urinary flow obstruction
- Serosa / adventitia
- Thin connective tissue layer covering the bladder dome and continuous with the peritoneal layer of the abdominal wall
- Contains blood vessels of various sizes
- Adventitia, an outermost layer of loose connective tissue in areas where there is no serosa
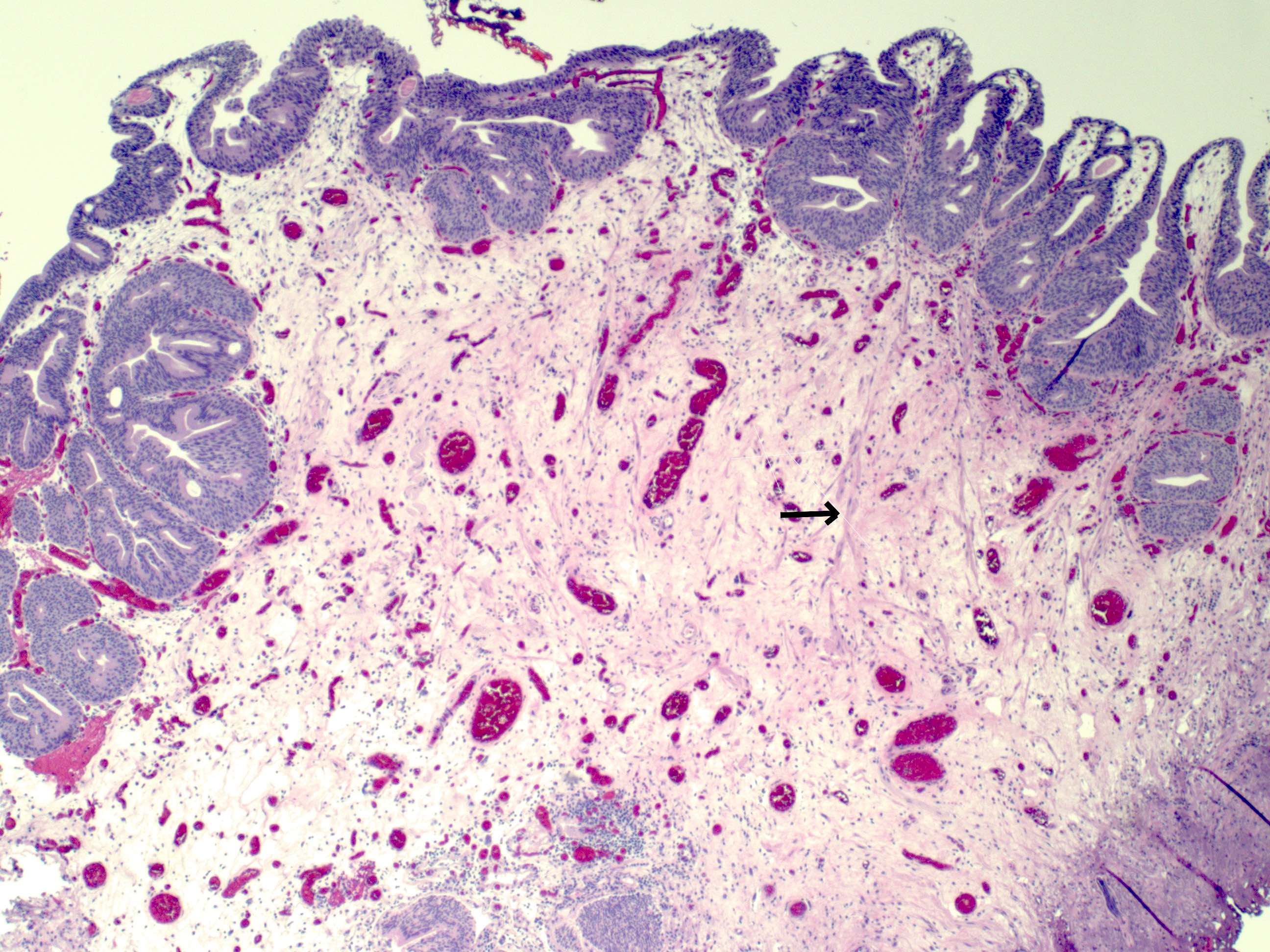
Microscopic (histologic) images
Cytology description
- In voided urines, transitional cells are shed singly; whereas in washings / brushings, the cells are aggregated in sheets and clusters
- Superficial and intermediate urothelial cells are seen in voided urine
- Superficial, intermediate and basal urothelial cells are seen in catheterized urine and bladder washings
- Superficial / umbrella cells:
- Low N:C ratio with pale finely granular chromatin, smooth nuclear contour and clear cytoplasm
- Intermediate and basal cells:
- High N:C ratio, smaller nuclei with even spacing and darker chromatin than superficial cells
- Melamed-Wolinska bodies: round to oval, hyaline, red or green-blue cytoplasmic inclusions seen within degenerated, benign or malignant urothelial cells (Diagn Cytopathol 2011;39:117)
Positive stains
- Full thickness: GATA3, CK7, CK8/18, CK19, CD138, S100P, thrombomodulin
- Basal / parabasal: p63, 34betaE12, CK5/6, CD44s
- Umbrella cells only: CK20, uroplakin II, uroplakin III (Adv Urol 2020;2020:4920236, Am J Clin Pathol 2014;142:864)
Electron microscopy description
- Superficial urothelial cells form an impermeable barrier via numerous junctional complexes
- Trilaminar (asymmetric) unit membrane composed of 2 dense layers of unequal thickness and a central lucent layer with interspersed normal areas which act like hinges
- Surface plasma membrane consists of inflexible apical plaques containing uroplakins (Kidney Int 2016;89:612)
Videos
Shotgun histology bladder
Additional references
Board review style question #1
Which of the following characteristics is true regarding the histology displayed in the picture?
- Muscular layer is consistently organized into 3 distinct layers
- Superficial layer consists of only umbrella cells, which have a high regenerative capacity
- Umbrella cells are CK20+ and CD44s-
- Well defined continuous muscularis mucosa can be always seen
Board review style answer #1
C. Umbrella cells are CK20+ and CD44s-. Superficial cells or the umbrella cells of urothelium are CK20+ and CD44s-, while basal cells are CK20- and CD44s+.
Comment Here
Reference: Bladder - Histology
Comment Here
Reference: Bladder - Histology
Board review style question #2
Board review style answer #2
C. Muscularis mucosa. The wispy, incomplete fascicles of muscle represent muscularis mucosae. They are morphologically and histochemically distinct from muscularis propria.
Comment Here
Reference: Bladder - Histology
Comment Here
Reference: Bladder - Histology