Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1Cite this page: Zoshchuk B, Rinehouse N, Yeh YA. Encrusted cystitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/bladderencrustedcystitis.html. Accessed April 3rd, 2025.
Definition / general
- Chronic inflammation of the urinary bladder with mucosal encrustations (J Urol Méd Chir 1914;5:35)
Essential features
- Chronic cystitis caused by Corynebacterium urealyticum or other urease producing bacteria (Front Med (Lausanne) 2021;7:609024)
- Urothelial mucosa with ulcerations, hemorrhage and granulation tissue, calcified necrotic debris with multinucleated giant cells, admixed with acute and chronic inflammatory infiltrate with eosinophils and fibrin deposits (Epstein: Biopsy Interpretation of the Bladder, 3rd Edition, 2016)
Terminology
- Phosphatic encrusted cystitis (Br J Clin Pract 1967;21:463)
- Alkaline encrusted cystitis (Australas Radiol 1981;25:157)
- Corynebacterial encrusted cystitis (Urology 2021;149:e18)
ICD coding
Epidemiology
- Incidence: 0.016 - 0.32% of clinical samples for bacterial cultures (Infect Drug Resist 2015:21;8:129)
- 0.6% occurred in patients who received renal transplant (Front Med (Lausanne) 2021;7:609024)
- Age and gender:
- Any age (mean 55 - 65 years old)
- Male predominance in patients with bacteriuria (Front Med (Lausanne) 2021;7:609024)
- Female predominance in skin colonization of healthy individuals (Infect Drug Resist 2015:21;8:129)
- Natural colonizer of human skin and urinary tract
- Transmitted by air or nosocomially (Infect Drug Resist 2015:21;8:129)
- Risk factors (Front Med (Lausanne) 2021;7:609024):
- Urological instrumentation (bladder catheterization)
- Surgical or endoscopic procedure (cystoscopy, cystography)
- Urological disease (urinary tract infections, intravesical mitomycin or bacillus Calmette-Guérin [BCG] instillations, radiation cystitis, drug induced cystitis, urolithiasis, malakoplakia, neurogenic bladder)
- Chronic debilitating disease (diabetes, chronic renal insufficiency, liver cirrhosis, neurological disease, prolonged hospitalization)
- Broad spectrum antibiotic therapy
- Immunocompromised status (kidney transplantation, cancer, cytotoxic drug treatment, immunosuppressive therapy)
Sites
- Encrusted uropathy (Front Med (Lausanne) 2021;7:609024)
- Encrusted cystitis: urinary bladder (IJU Case Rep 2020;3:112)
- Encrusted urethritis: urethra
- Encrusted (uretero) pyelitis: kidney
Pathophysiology
- Urinary colonization and adherence to host tissue:
- Colonization: asymptomatic, positive urine cultures
- Adherence mediated by adhesive pili that covalently anchored to Corynebacterium cell wall (Front Med (Lausanne) 2021;7:609024)
- Formation of struvite and carbonated apatite crystals
- Corynebacterium urealyticum has strong urease activity that hydrolyses urea (pH ≥ 7.1) leading to formation of NH3 and CO2 (see diagram 1)
- NH3 combines with H+ to form NH4+
- In alkaline urine, NH4+ reacts to Mg2+ and PO43-, leading to formation of struvite (magnesium ammonium phosphate, NH4MgPO4.6H2O)
- In alkaline urine, CO2 converts to bicarbonate HCO3- which reacts to Ca2+ and PO43-, leading to formation of calcium phosphate crystals (carbapatite, Ca10(PO4)6CO3) (Front Med (Lausanne) 2021;7:609024)
- Infected urine saturates with struvite and calcium phosphate and precipitates, resulting in bladder wall incrustation in a suitable urothelial environment injured by inflammation, malignancy, ischemia or urological instrumentation
- Adherence to medical device:
- Associated with 2 putative surface proteins, surA and surB (Pol J Microbiol 2006;55:189)
- Adherence to foreign body material in the urinary tract
- Initiate nosocomial urinary tract infections of catheterized patients (Pol J Microbiol 2006;55:189)
Etiology
- Corynebacterium urealyticum (formerly coryneform CDC group D2)
- Gram positive, aerobic, urease positive, pleomorphic, lipophilic, acid fast, non-spore forming, asaccharolytic and usually multidrug resistant bacillus (Clin Microbiol Infect 2008;14:632)
- Common skin colonizer and opportunistic pathogen mainly detected in the groin area in hospitalized elderly patients receiving broad spectrum antibiotics
- Pathological even if colony forming units (CFU) < 100,000/mL on urine cultures (Front Med (Lausanne) 2021;7:609024)
- Highly susceptible to norfloxacin and vancomycin (J Clin Microbiol 1985;21:788)
- Other bacteria: Ureaplasma urealyticum, Proteus vulgaris, Streptococcus haemolyticus, Streptococcus viridans, Staphylococcus species, Pseudomonas aeruginosa, Escherichia coli, Corynebacterium gluconolyticum, Arcanobacterium pyogene (Front Med (Lausanne) 2021;7:609024)
Diagrams / tables
Clinical features
- Fever (25 - 50%), urinary frequency, urgency, stranguria, nycturia, suprapubic / pelvic pain, vesical tenesmus, costovertebral angle tenderness, dysuria (Br J Urol 1993;72:571)
- Less often nausea, anorexia and weight loss
- Commonly macroscopic hematuria detected in 75 - 100%
- Urination of mucus, purulent debris, calcified necrotic debris, gravel or renal stones
Diagnosis
- Clinical manifestations: urinary frequency, urgency, dysuria
- Past clinical history and predisposing conditions
- Urinalysis: alkaline urine (pH > 7.0), leukocytes
- Urine microbiological cultures: positive for urease producing bacteria, commonly Corynebacterium urealyticum (J Med Microbiol 1998;47:79)
- Radiological findings: thickening bladder wall with calcifications (Xray, ultrasound, CT scan)
- Other conditions in the differential diagnosis of urinary tract encrustations or calcifications need to be excluded by means of cystoscopy and histopathological examination (Front Med (Lausanne) 2021;7:609024)
- Cystoscopic examination: ulcerations, erythema, increased vascularity, yellow or white plaques firmly attached to the bladder mucosa (World J Clin Cases 2020;8:4234)
- See diagram 2
Laboratory
- Urinalysis:
- Urinary ammonia-like odor
- Alkaline urine (pH > 7.0)
- Microscopic hematuria
- Pyuria
- Struvite crystalluria
- Gritty calcified debris or stones
- Mucopurulent debris (Front Med (Lausanne) 2021;7:609024)
- Microbiological culture:
- Conventional urine cultures often negative for Corynebacterium urealyticum
- No specific transport media
- Prolonged incubation in 5% CO2, 35 - 37 °C, for 48 - 72 hours
- Nonselective media including blood agar or cysteine lactose electrolyte deficient agar
- Selective media including lipid enriched peptone based CBU agar or Loeffler serum medium (3 parts of sheep or horse serum plus 1 part of glucose broth) (J Med Microbiol 1998;47:79, Infect Drug Resist 2015:21;8:129)
Radiology description
- Abdominal Xray shows calcifications lining the entire bladder wall, occasionally thin and radiolucent encrustations (AJR Am J Roentgenol 2002;178:389)
- Sonogram shows thickening of the bladder wall with linear or irregular echogenic material lining the bladder wall (AJR Am J Roentgenol 2002;178:389)
- Unenhanced CT shows thick or thin, irregular or regular, superficial calcifications of the bladder wall (Int J Surg Case Rep 2020;77:392)
Case reports
- 27 year old man with urinary frequency, urgency and dysuria for 2 months (World J Clin Cases 2020;8:4234)
- 40 year old woman with pelvic pain and urinary tract infection for the past 4 years (Int Braz J Urol 2018;44:1252)
- 62 year old man with urosepsis (Int J Surg Case Rep 2020;77:392)
- 73 year old man with hematuria and dysuria (IJU Case Rep 2020;3:112)
Treatment
- Endoscopic mucosal resection of encrusted calcifications
- Urinary acidification: acetohydroxamic acid
- Systemic glycopeptides antibiotic (especially teicoplanin and vancomycin) therapy for a few weeks to a few months (Front Med (Lausanne) 2021;7:609024)
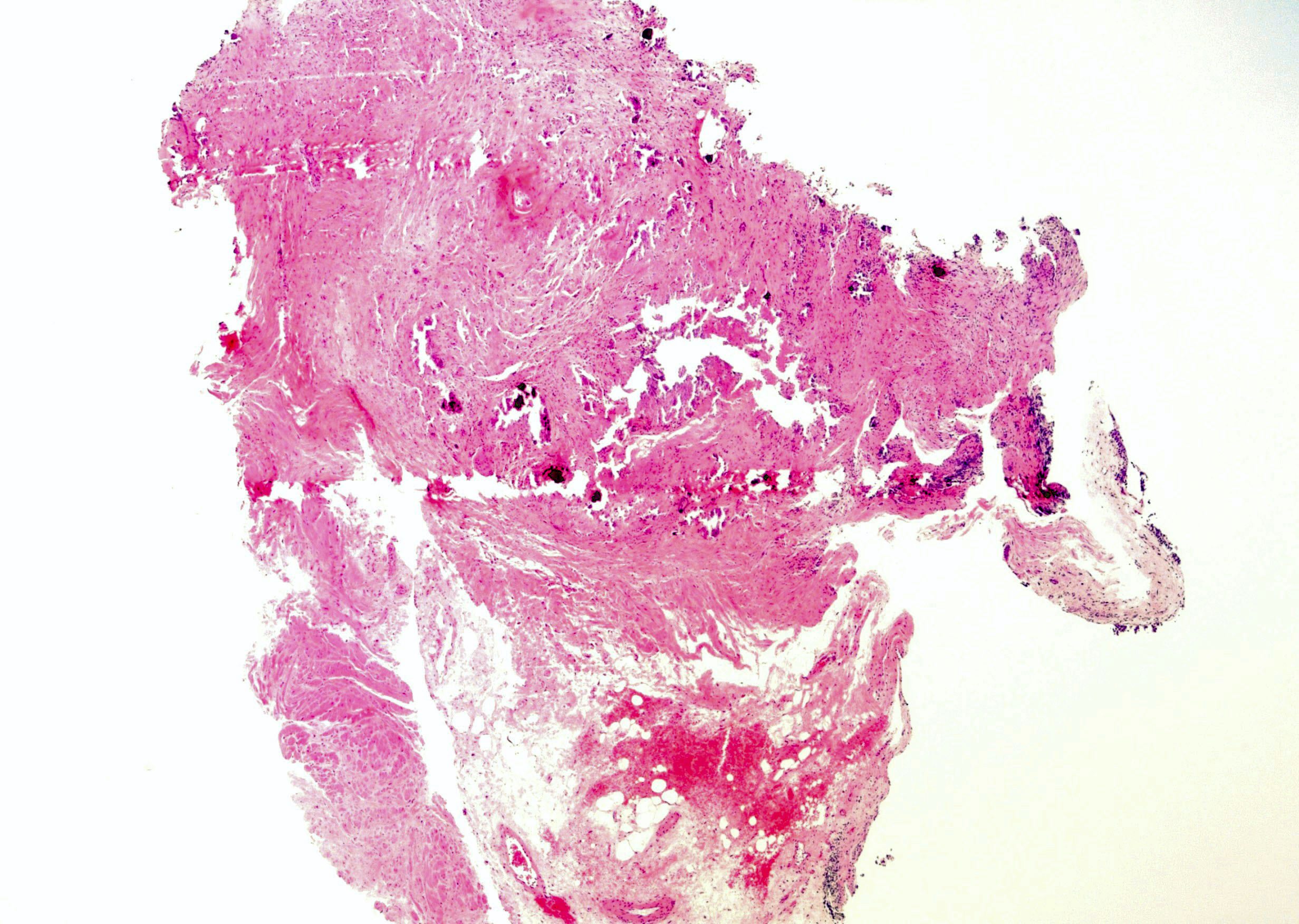
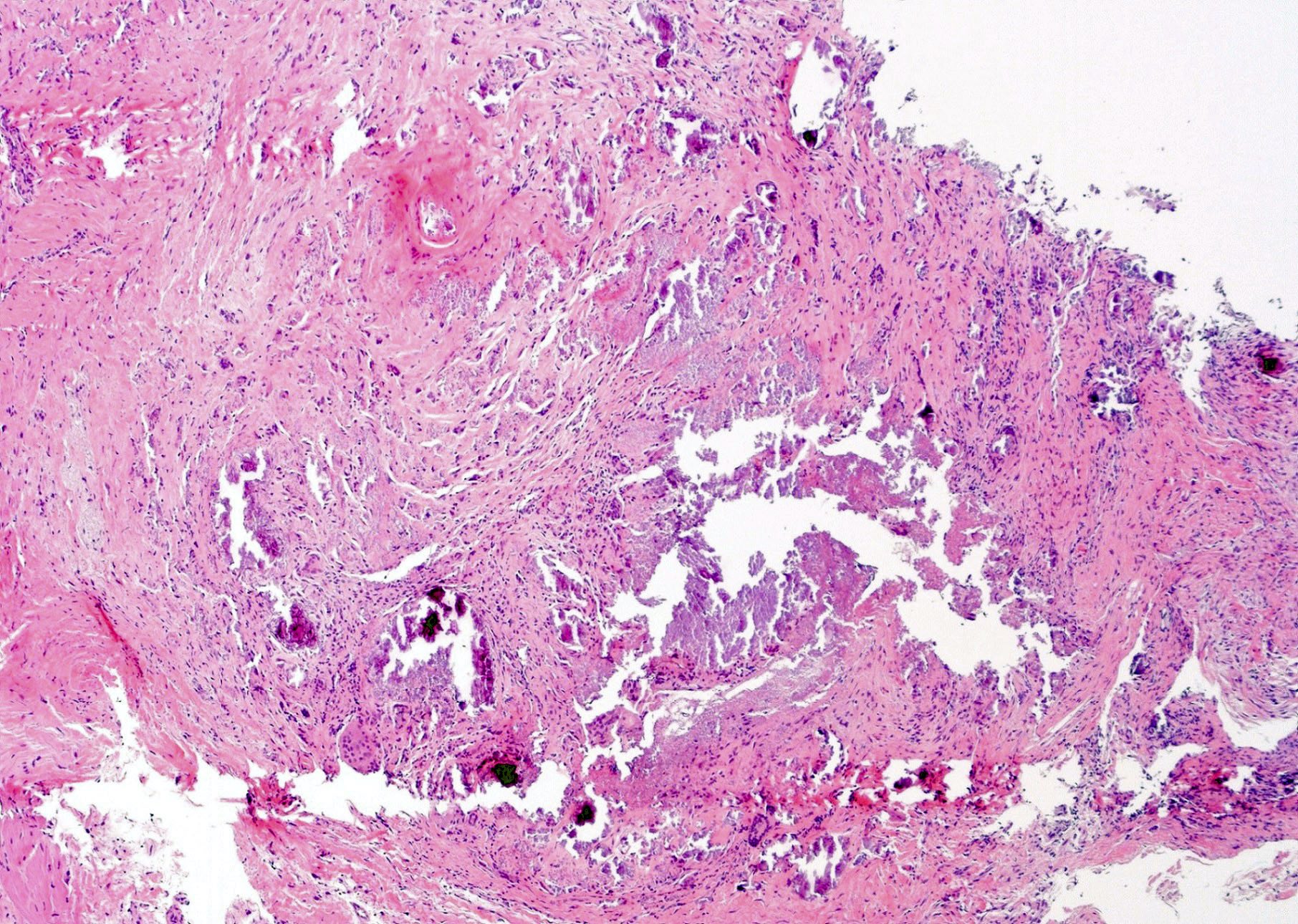
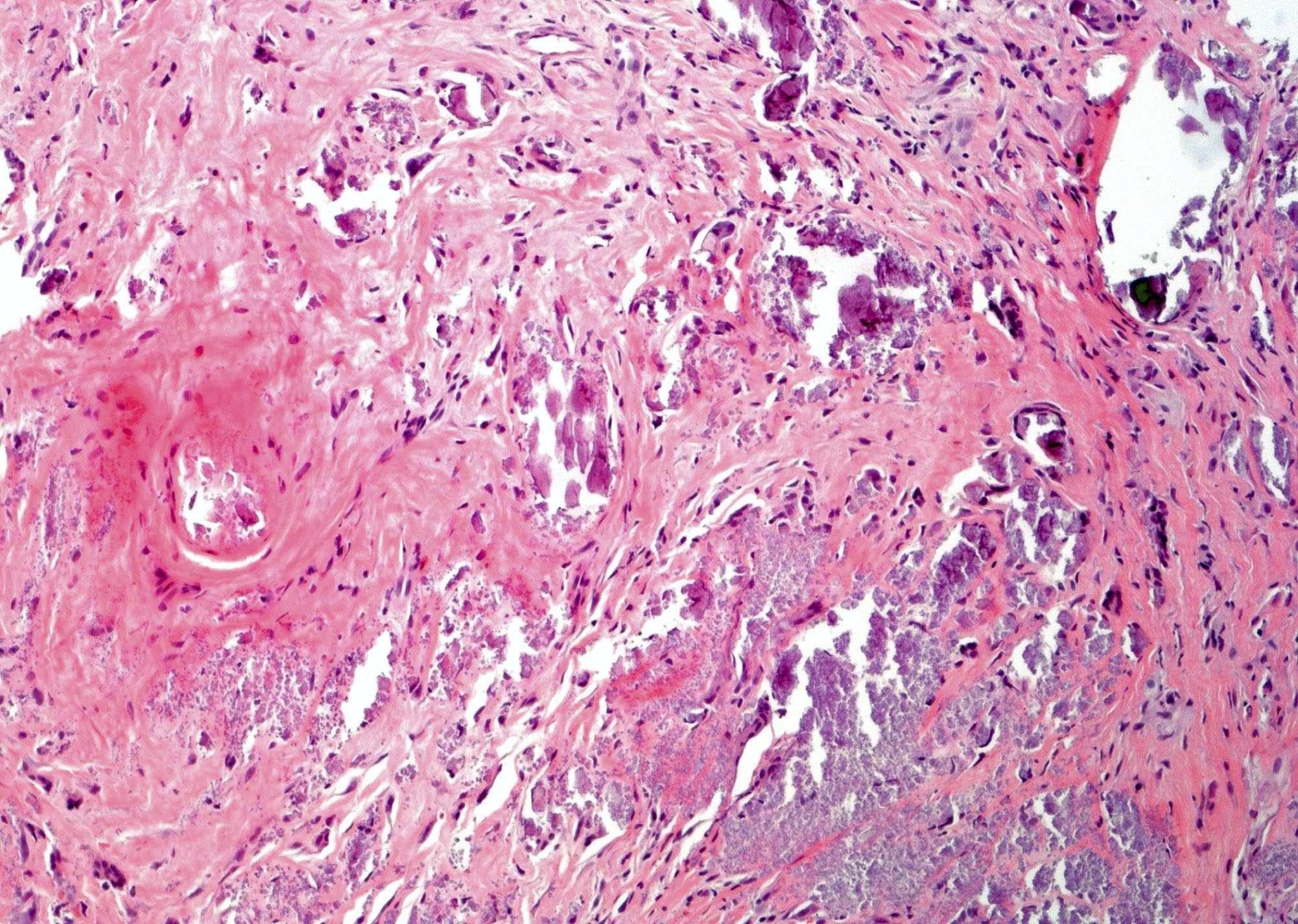
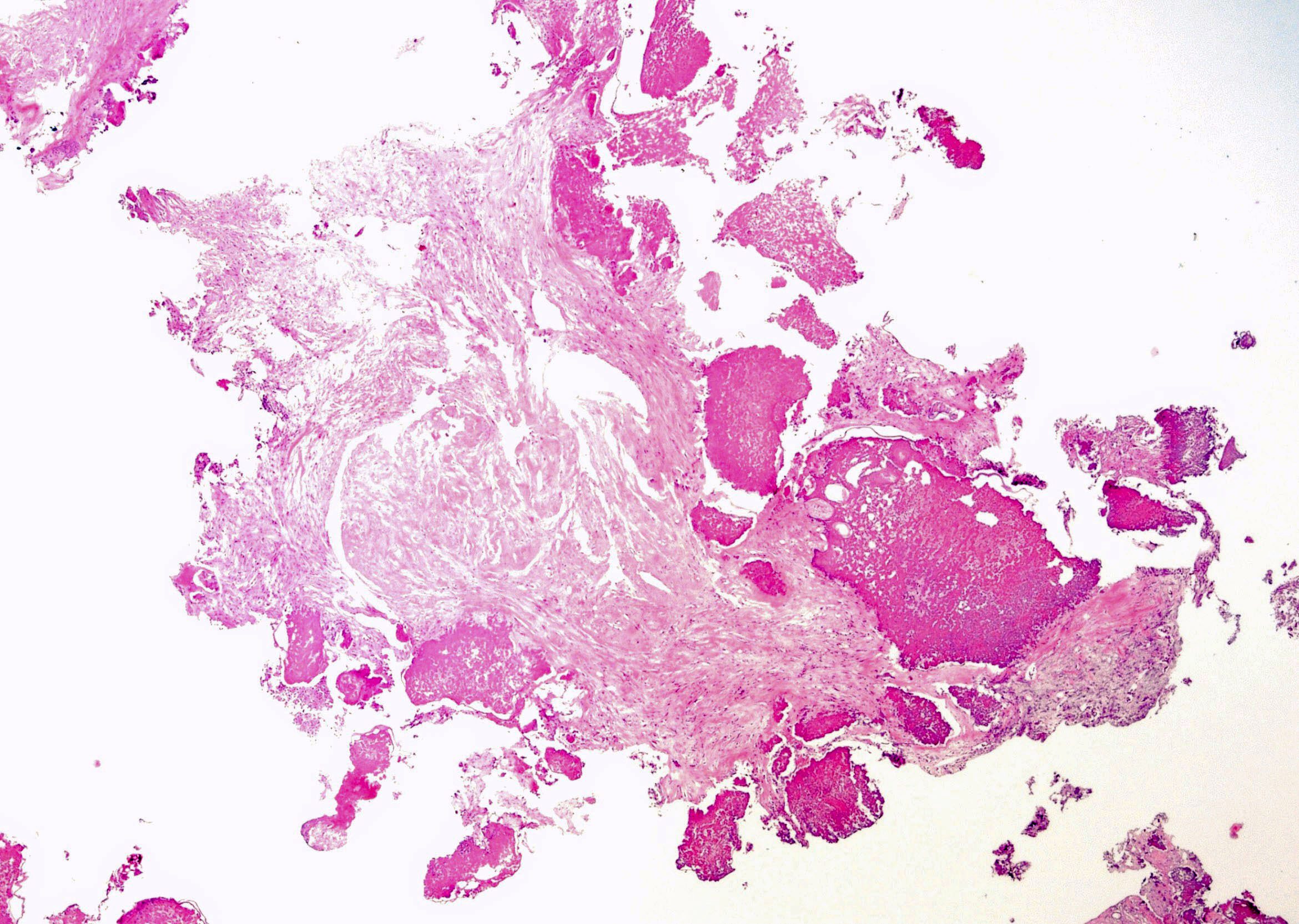
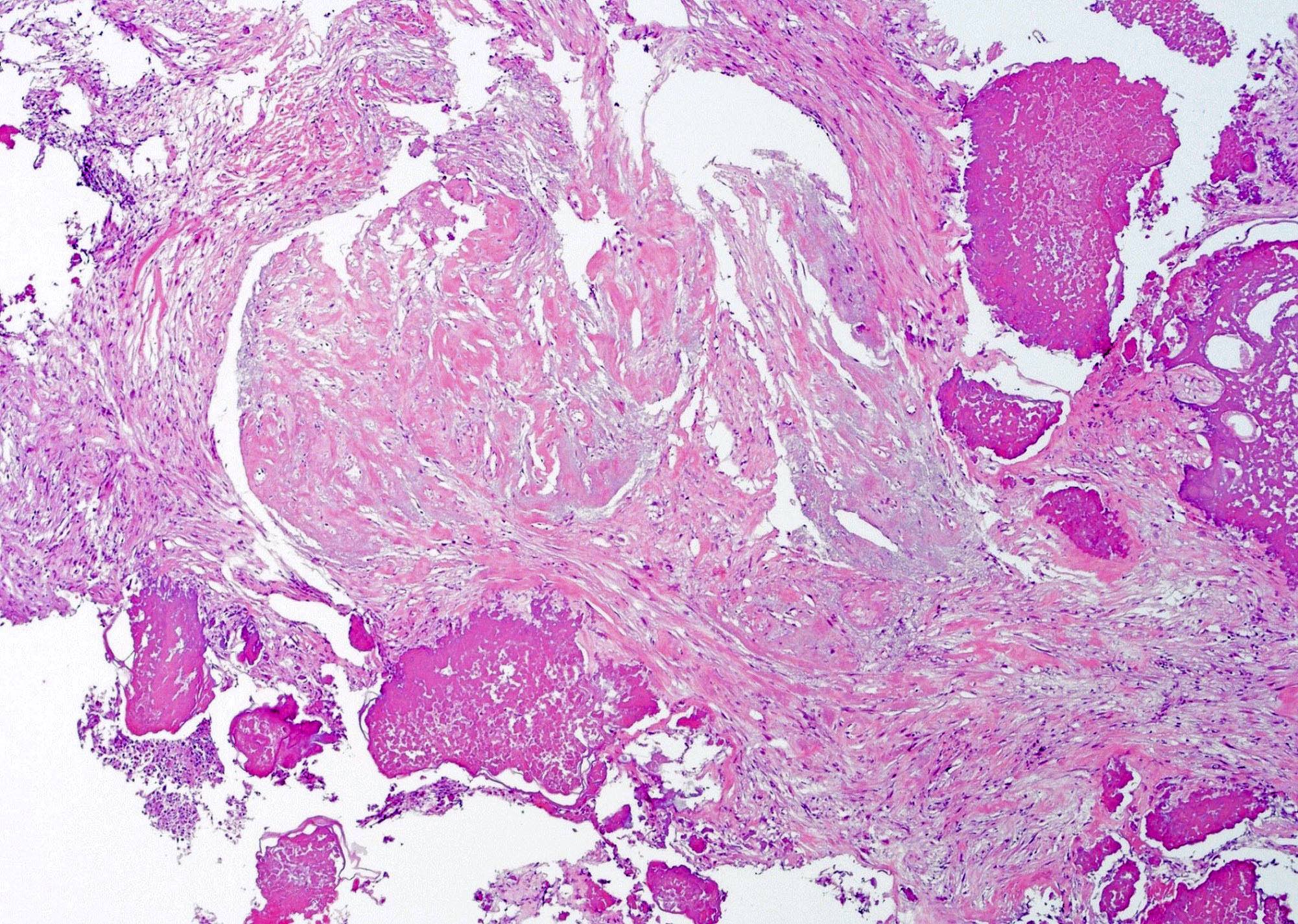
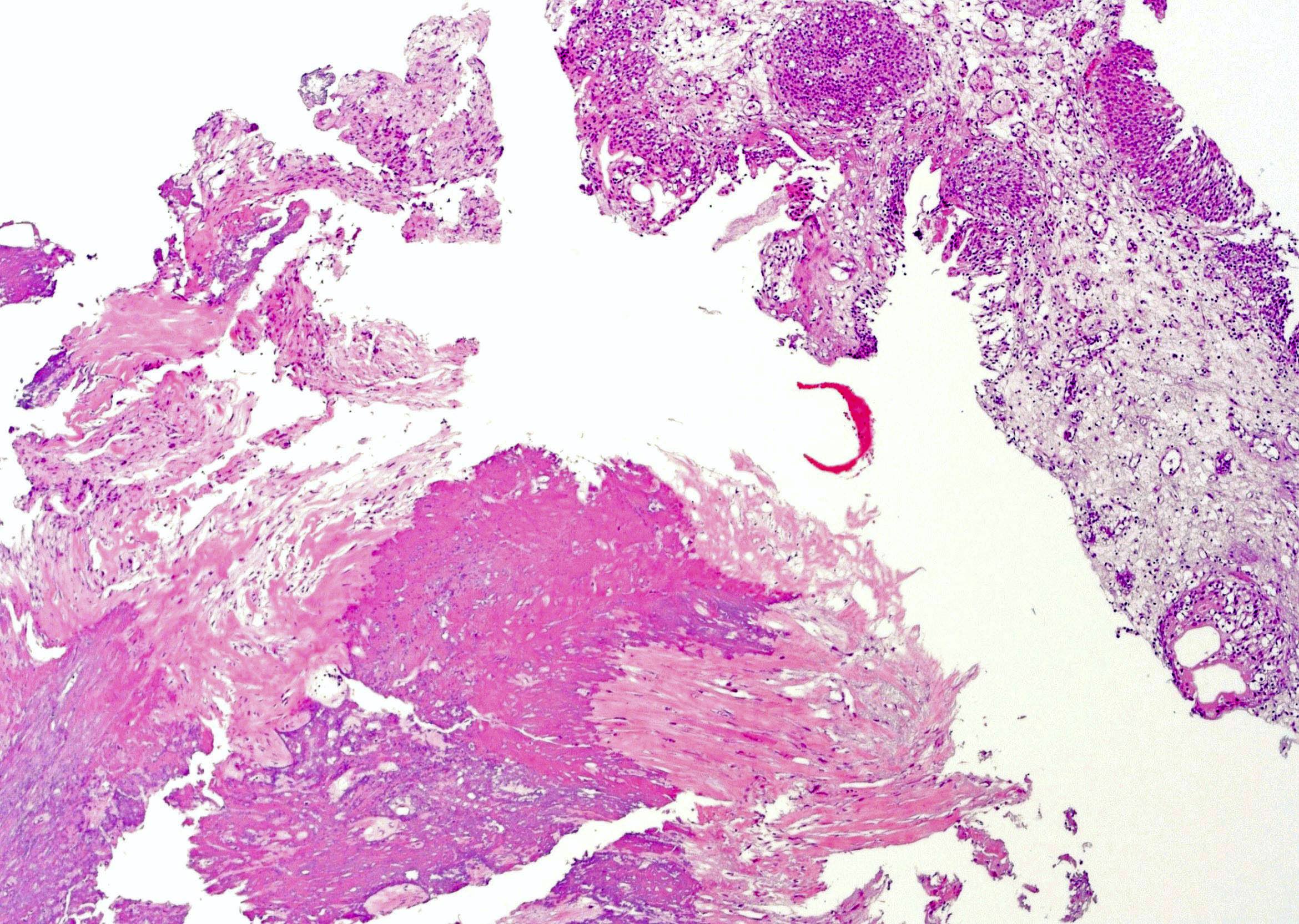
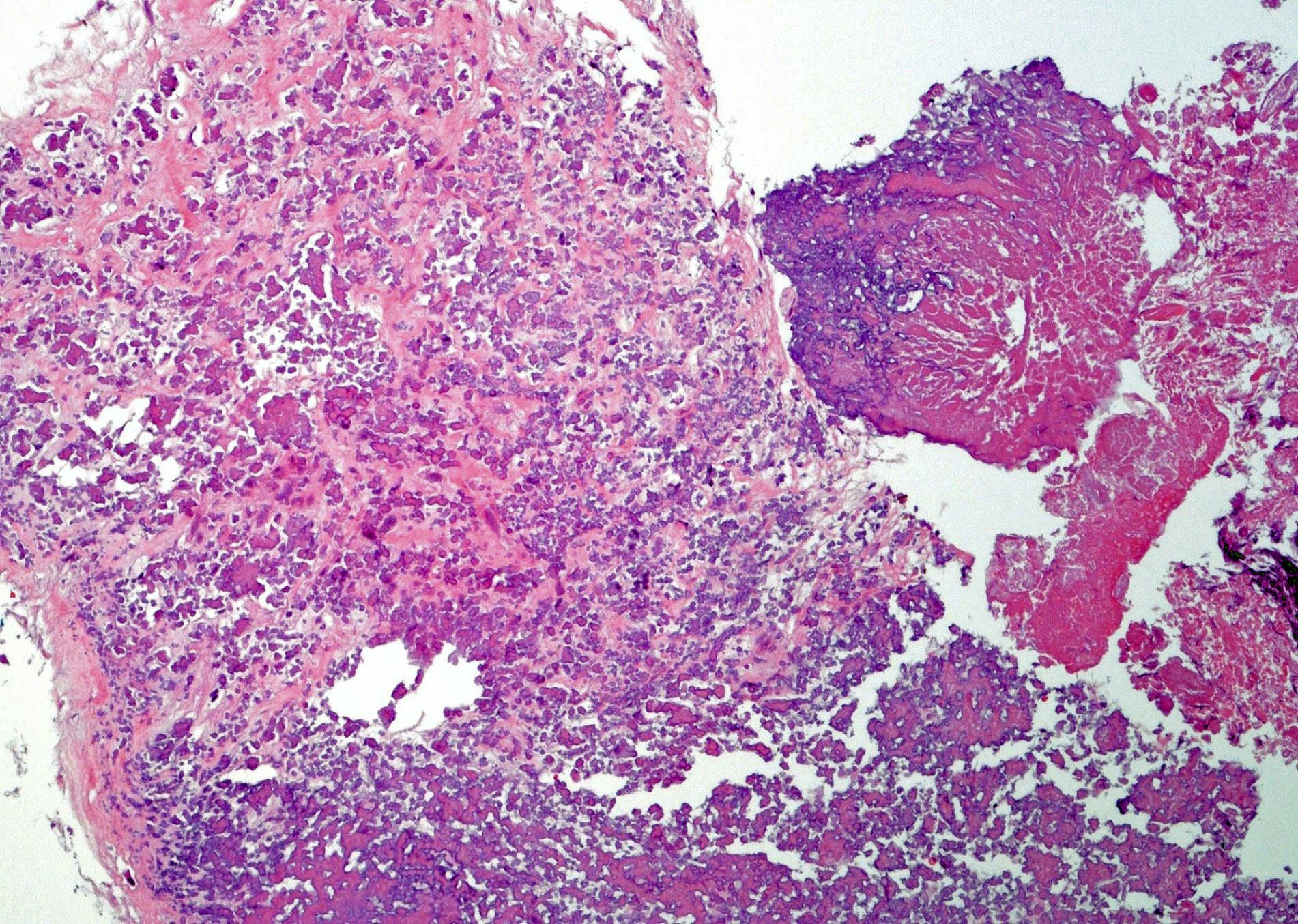
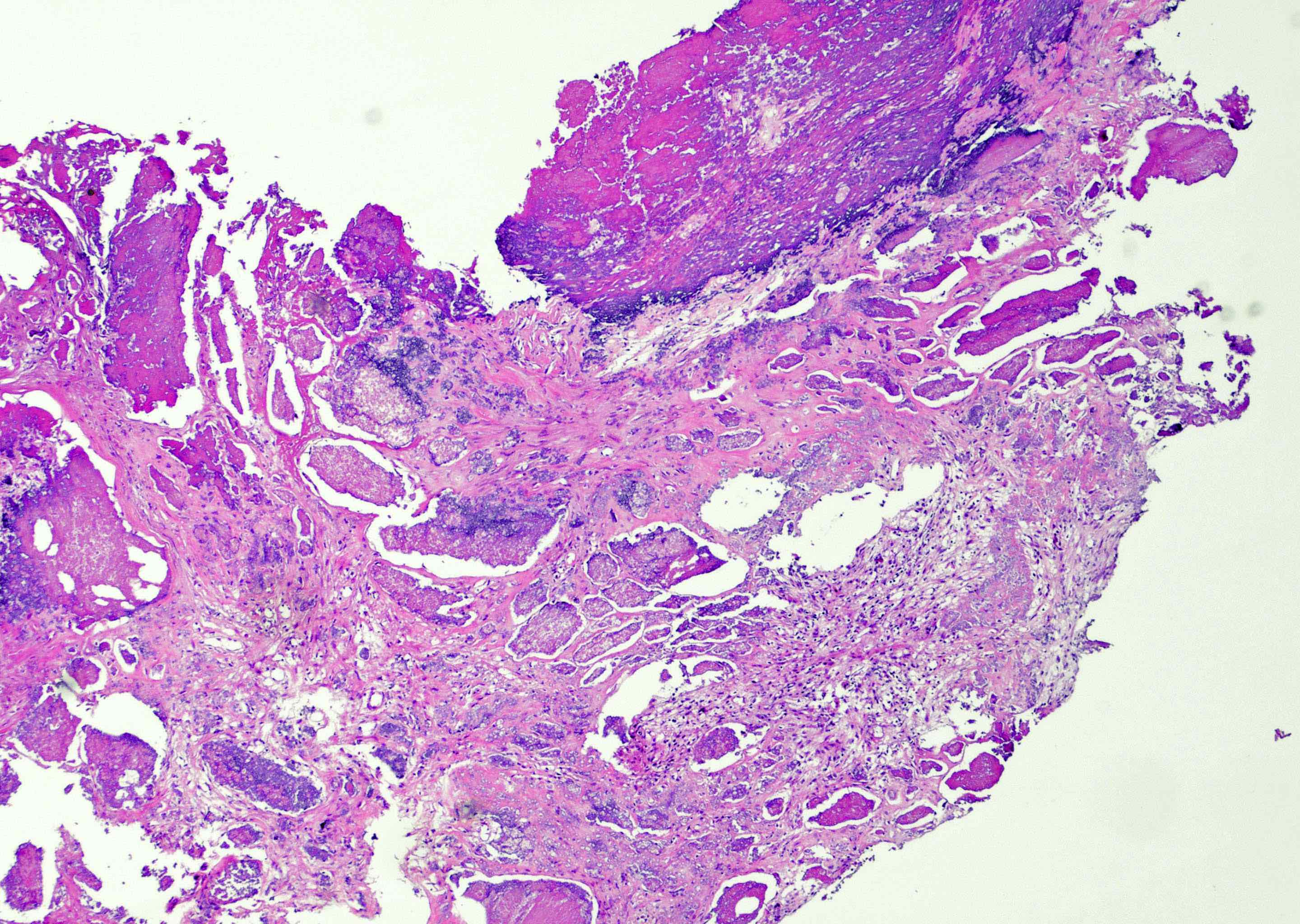
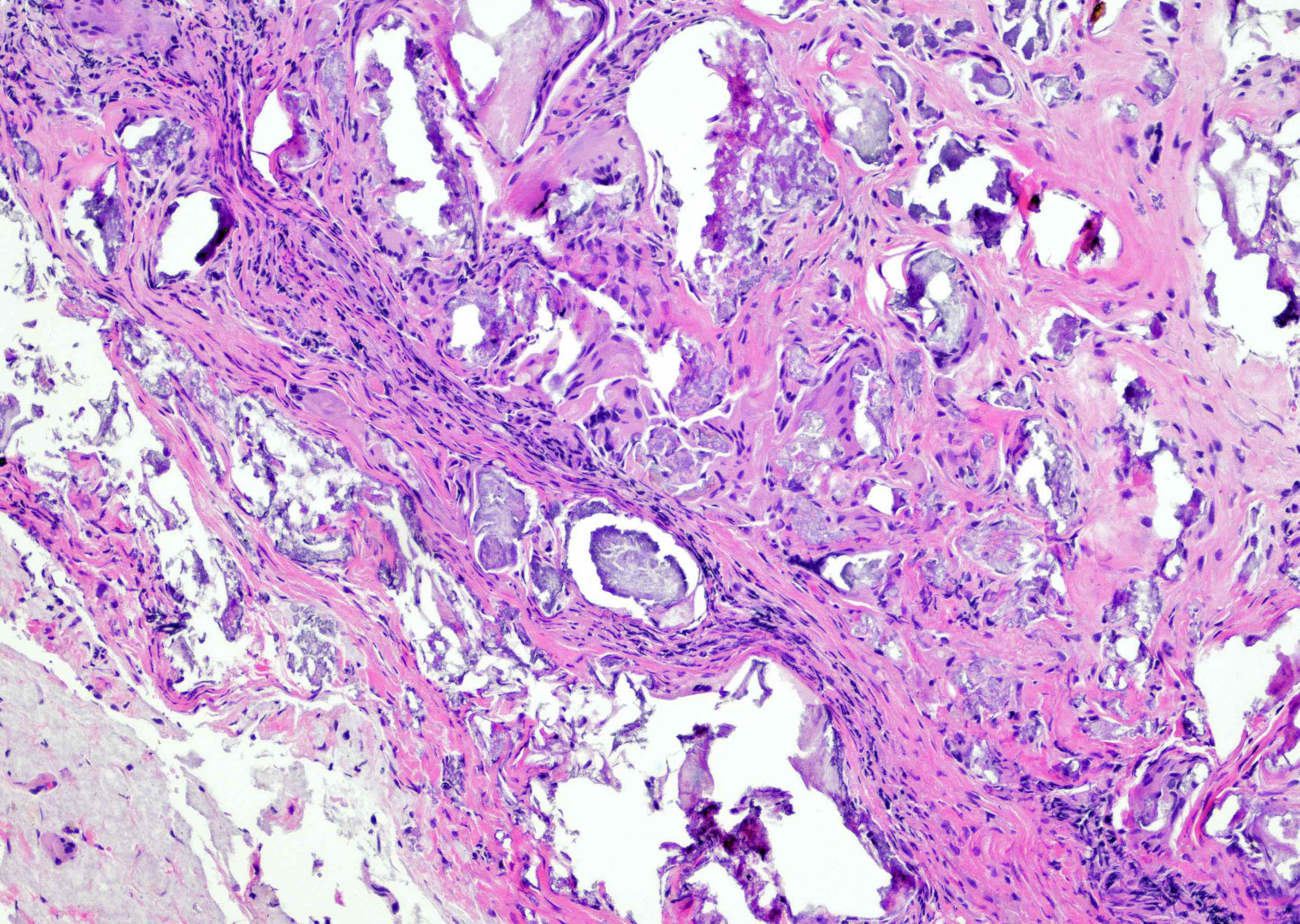
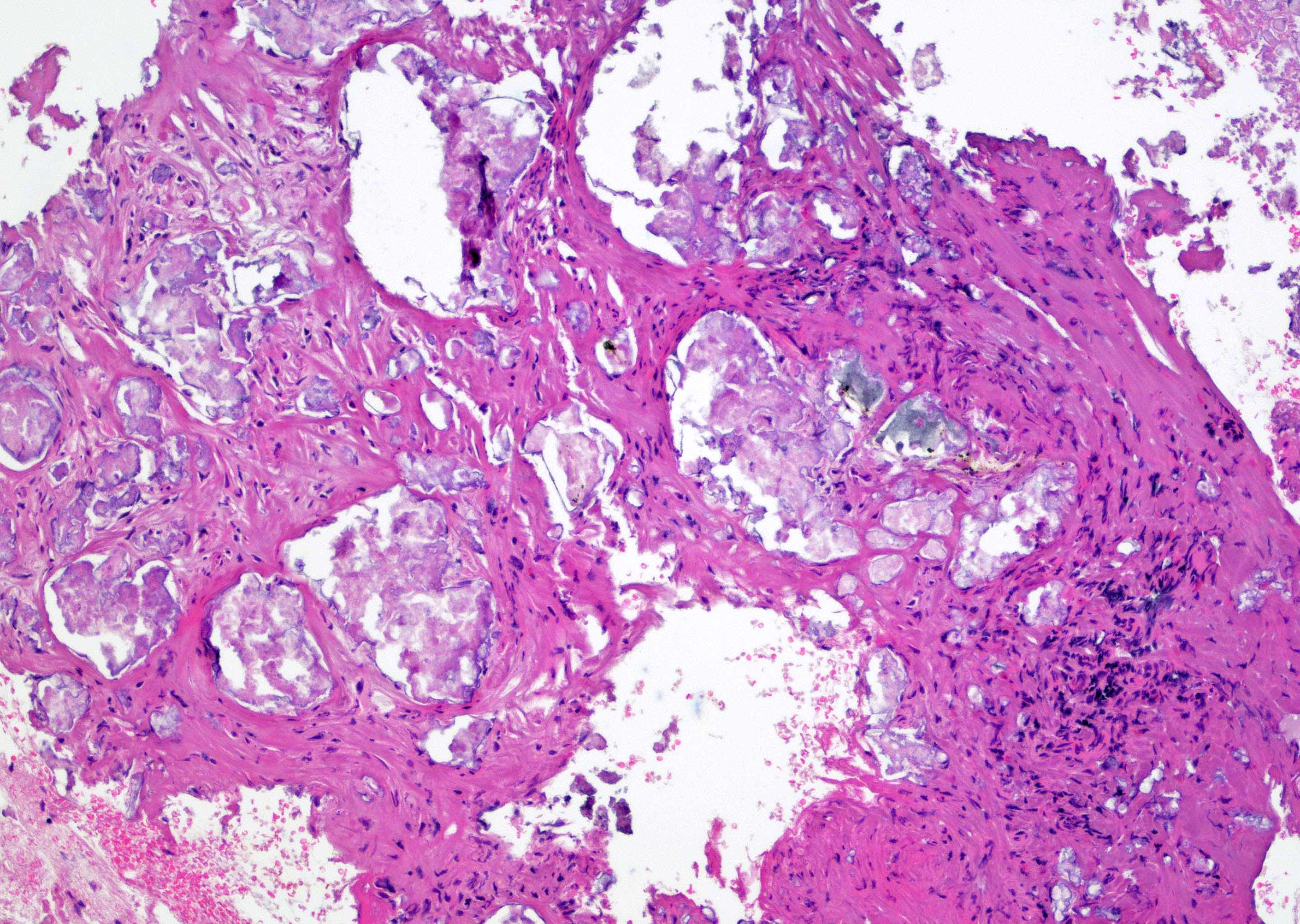
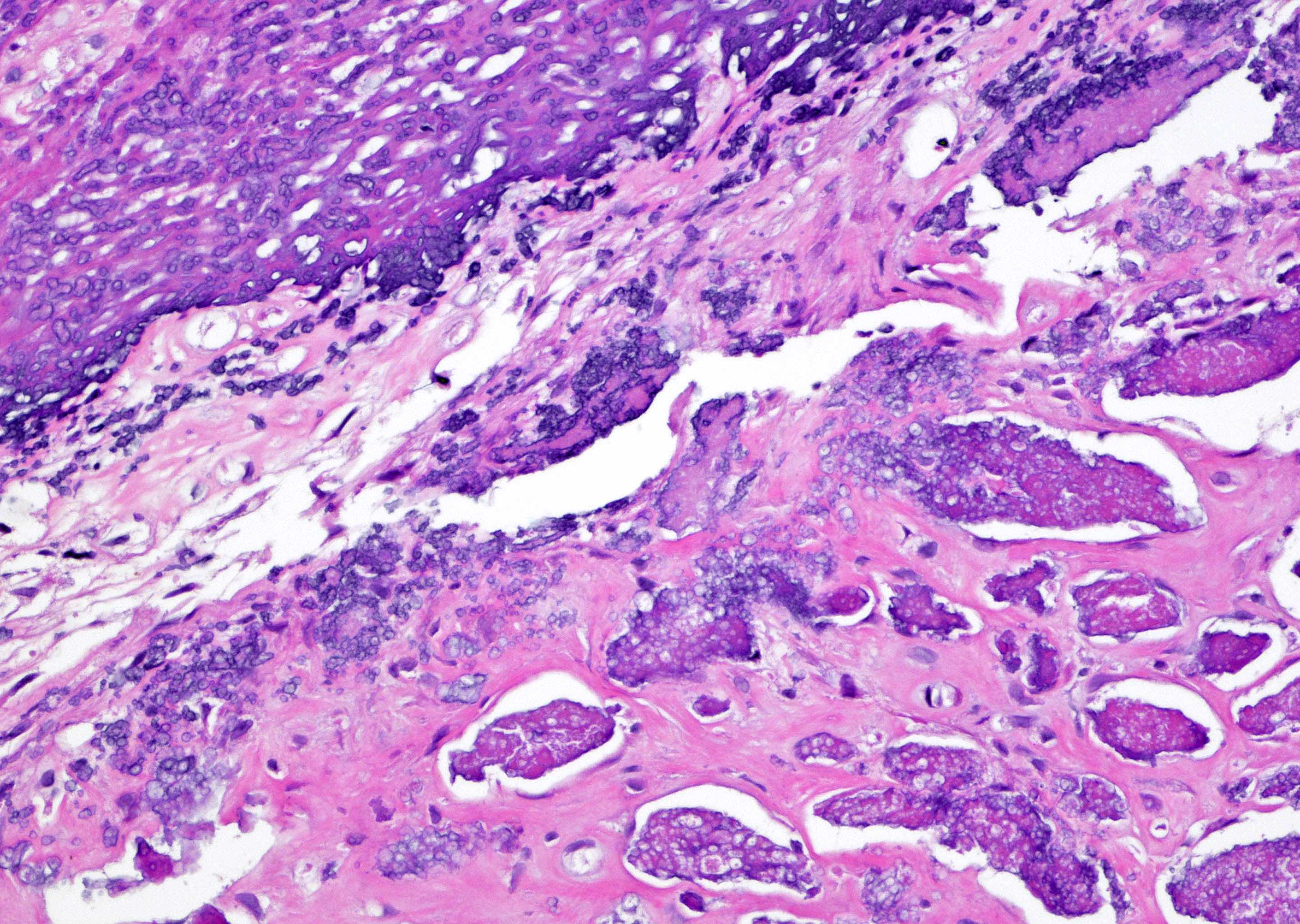
Microscopic (histologic) description
- May form 3 distinct layers
- First superficial layer:
- Ulceration and necrotic urothelial tissue
- Calcified necrotic debris (demonstrated by von Kossa staining)
- Degenerative changes with squamous metaplasia in nonaffected urothelium
- Second layer:
- Lamina propria with edematous and granulation tissue
- Inflammatory infiltrate with lymphocytes, plasma cells, neutrophils, sometimes granulomas
- Less often eosinophils, mast cells, fibroblasts and histiocytes
- Small vascular thrombosis (may present)
- Crystal deposition
- Microabcesses with bacterial microcolonies (may present)
- Third layer:
- Fibrosis of the muscularis may present (Front Med (Lausanne) 2021;7:609024, Epstein: Biopsy Interpretation of the Bladder, 3rd Edition, 2016)
Microscopic (histologic) images
Contributed by Bohdan Zoshchuk, M.D. and Y. Albert Yeh, M.D., Ph.D.
Positive stains
- Calcified fragments staining with von Kossa special stain (Histochem Cell Biol 2021;156:523)
Negative stains
- Noncalcified tissues negative for von Kossa special stain (Histochem Cell Biol 2021;156:523)
Electron microscopy description
- Calcifying nanoparticles with electron dense shell and central electron lucent core (Int J Nanomedicine 2008;3:385)
Molecular / cytogenetics description
- Detection and identification of Corenybacterium urealyticum
- Polymerase chain reaction (PCR) amplification and 16S rRNA gene sequencing (Infect Drug Resist 2015:21;8:129)
- RNA polymerase beta subunit encoding (rpoB) gene sequencing (Infect Drug Resist 2015:21;8:129)
- Restriction fragment length polymorphism: digestion of bacterial chromosomal DNA or plasmids (J Clin Microbiol 2005;43:1934)
Sample pathology report
- Urinary bladder, biopsy:
- Bladder tissue with acute and chronic inflammation and abundant calcification (see comment)
- Comment: The urothelial mucosa shows ulcerations and extensive calcified necrotic debris admixed with many multinucleated giant cells. Granulation tissue with acute and chronic inflammatory infiltrate, eosinophils and fibrin deposits are present. Clinical correlation with urinalysis and microbiological culture is highly recommended. These findings are consistent with encrusted cystitis in the right clinical context.
Differential diagnosis
- Bladder stones or foreign bodies (Urol Int 2007;79:32)
- Schistosomiasis:
- Submucosal calcifications, calcified ova present (Indian J Pathol Microbiol 2017;60:614)
- Tuberculosis:
- Acidic urine, submucosal calcifications, caseating granulomas with or without acid fast bacilli
- Amyloidosis:
- Submucosal calcifications, amorphous aggregates staining with Congo red stain (Urology 2021;156:e12)
- Calcified bladder tumor:
- Usually following intravesical BCG or cytotoxic drug therapy; calcifications with necrotic tumor fragments present (Urology 1993;42:89)
Additional references
Board review style question #1
A bladder biopsy is shown above from a male patient with a history of bladder instrumentation. The entity depicted above is characterized by deposition of inorganic salts within injured urothelial mucosa due to the action of the urea splitting bacteria. What is the diagnosis?
- Emphysematous cystitis
- Encrusted cystitis
- Eosinophilic cystitis
- Interstitial cystitis
- Malakoplakia
Board review style answer #1