Table of Contents
Definition / general | Essential features | Methods of specimen collection | CPT coding | Sites | Cytology description | Cytology images | Molecular / cytogenetics description | Biomarker testing | Molecular / cytogenetics images | Sample pathology report | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Petrykowski BL, Policarpio-Nicolas MLC, Reyes MCD. Cytology-general, normal findings & biomarker testing. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/bladdercytologynormal.html. Accessed December 22nd, 2024.
Definition / general
- The Paris system (TPS) is a standardized international reporting system for urinary cytology specimens (Wojcik: The Paris System for Reporting Urinary Cytology, 2nd Edition, 2022)
- Ancillary biomarker testing is utilized to increase both the sensitivity and specificity for diagnosing and surveilling urothelial carcinoma
Essential features
- Methods of specimen collection: voided urine, catheterized urine, bladder or renal pelvis washing, brushing and ileal conduit
- There are cytological features that delineate benign urine specimens from high grade urothelial carcinoma (HGUC)
- Knowledge of cytological features of normal variants such as urothelial cells, glandular cells and renal tubular cells is key to accurate evaluation; there are also common findings that do not necessarily have clinical significance (e.g., crystals)
- Ancillary tests utilizing novel molecular technology as well as biomarkers increases diagnostic accuracy when paired with cytology
- 34 - 42% sensitivity and 96 - 99% specificity for diagnosing and surveilling urothelial carcinoma by cytology
Methods of specimen collection
- Voided urine
- Best retrieved 4 hours after last urination
- 30 mL volume has been suggested for adequacy criteria
- Clean catch or midstream urine is gold standard
- Vaginal cells are a potential contaminant
- Low cellularity
- Urothelial cells and squamous cells
- Intermediate urothelial cells are the majority
- Catheterized urine
- High cellularity
- Cellular degeneration is typical
- Tightly clustered basal urothelial cells
- Bladder washings
- Obtained by irrigation of the urinary bladder with 50 - 100 mL of normal saline and this procedure is repeated 3 times (Radiol Oncol 2010;44:207)
- Highly cellular and better preserved sample
- Low contamination
- DNA ploidy analysis is gold standard
- Brushings
- Utilization of urethral catheter
- Allows for sampling of ureter or pelvic mass
- Ileal conduit urine
- Cystectomy procedure involves anastomosing the ileum (artificial bladder) to the ureter
- Samples contain an abundance of degenerated intestinal epithelial cells
- Must be continually screened for urothelial tumors
- References: Wojcik: The Paris System for Reporting Urinary Cytology, 2nd Edition, 2022, Cibas: Cytology - Diagnostic Principles and Clinical Correlates, 5th Edition, 2019
CPT coding
- 88112 - cytopathology, enriched / concentrated preparation, nongynecologic (e.g., liquid based slide preparation: ThinPrep, SurePath)
- See Cytology-neoplastic
Sites
- Urinary bladder, upper tracts (renal pelvis, ureters), urethra
- Urinary bladder diversion (ileal conduit, Indiana pouch, neobladder)
- See Cytology-neoplastic
Cytology description
- Urothelial cells
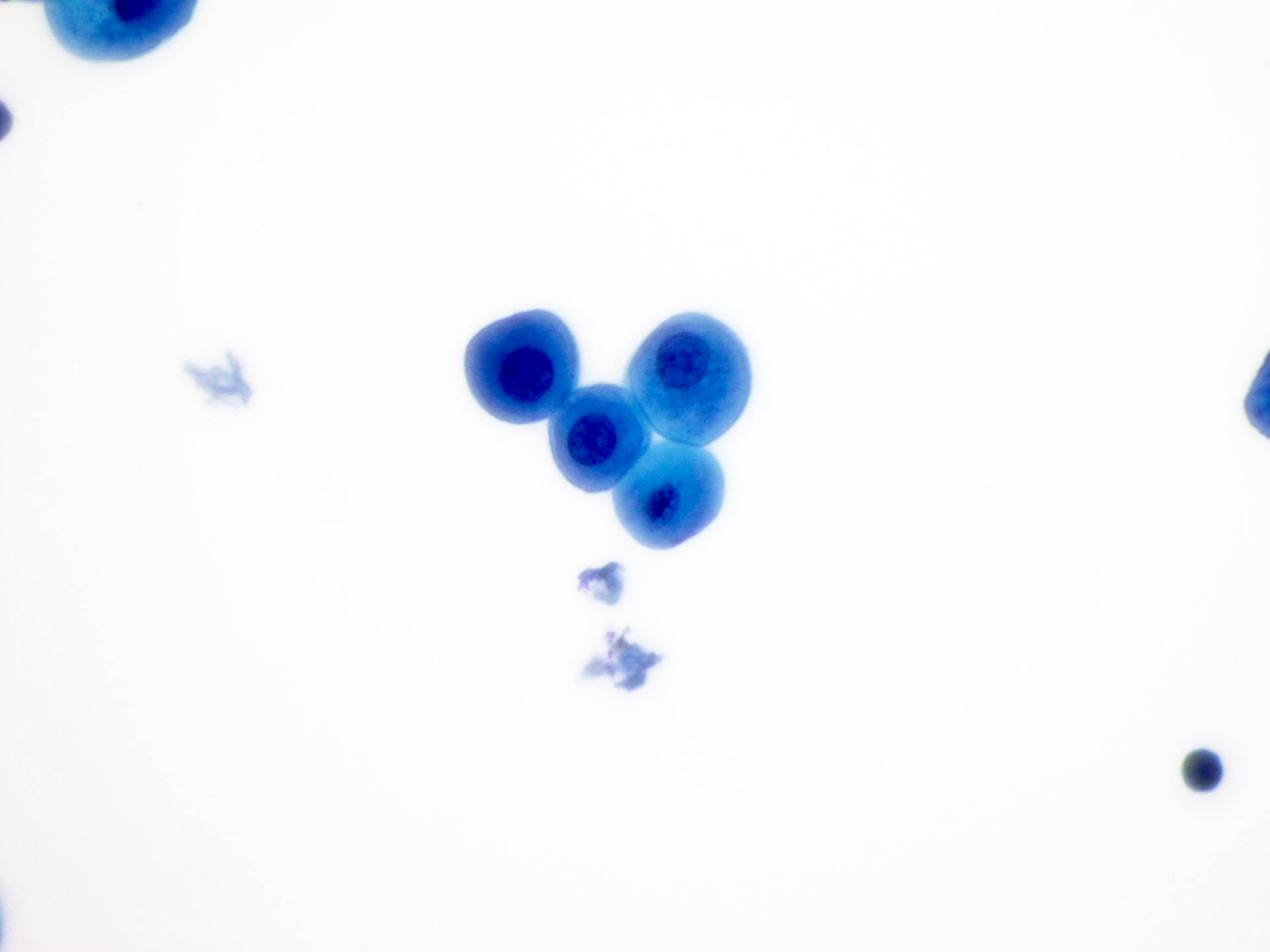
- Umbrella cells
- Canopy shaped large cells with rounded luminal surfaces and scalloped borders
- Low N:C ratio
- May contain a centrally located, single, large nucleus or in many cases, bi or multinucleated
- Smooth nuclear membranes with round to oval nuclei, fine chromatin and occasional prominent nucleolus
- Foamy, vacuolated and abundant cytoplasm, distinct from virally induced koilocytes
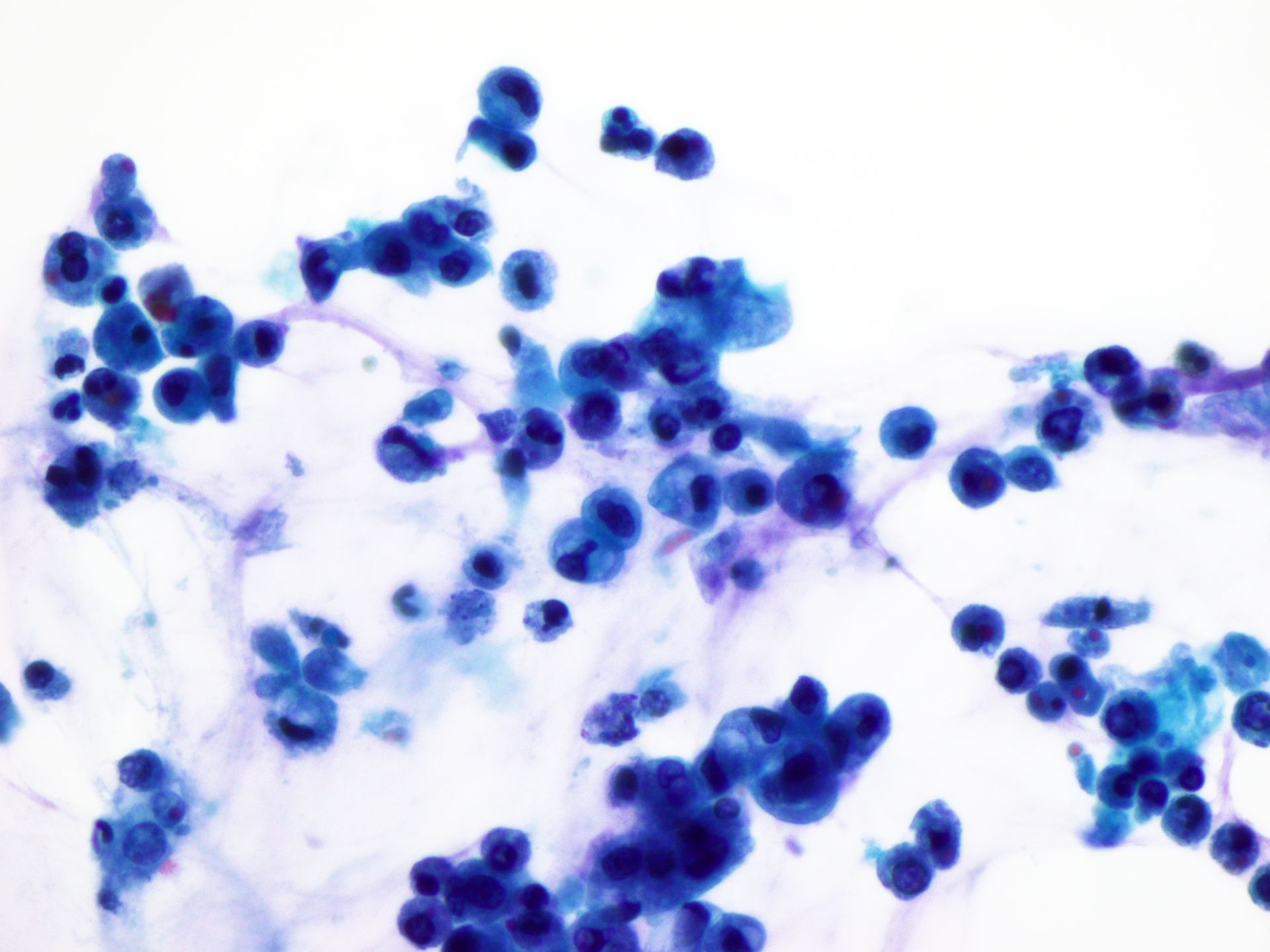
- Intermediate urothelial cells
- Appear like fried eggs or parabasal cells
- Same nuclear size as the superficial cells but less cytoplasm
- Higher N:C ratio than umbrella cells
- Homogeneous cytoplasm, oval nuclei with smooth borders and bland chromatin
- Basal cells
- Monolayer of cells with uniform round and pale nuclei
- High N:C ratios
- May form papillary fragments but lack fibrovascular cores
- Umbrella cells
- Squamous epithelial cells
- In women, they may originate from the vagina, perineum, urethra and bladder trigone
- In both men and women, they may originate from the urethra
- Glandular cells
- Glandular cells from the urinary tract have small nuclei and vacuolated cytoplasm, often appearing as multilayered tissue fragments or single cells
- Potential origins of glandular cells in urologic samples include the bladder dome (urachal remnant) or trigone and changes from these areas are developmental, not metaplastic
- Benign glandular cells in voided urine from women typically originate from the uterine corpus or cervix
- Endometrial cells form 3 dimensional clusters with scant cytoplasm, irregular nuclei, vesicular chromatin and small nucleoli
- Endometriosis involving the urinary tract can present with very small hyperchromatic cells, either in voided urine or ureter brushings
- Renal tubular cells (RTCs)
- Histiocyte size and degenerated
- High N:C ratio if originating from distal convoluted tubules or low N:C ratios with granular cytoplasm if originating from proximal convoluted tubules
- Can be small and have scant cytoplasm or large with vacuolated cytoplasm
- May form casts
- Degenerative changes
- Smaller than preserved urothelial cells
- Hyperchromatic nuclei with mildly irregular nuclear borders
- N:C ratio remains < 0.5
- Melamed-Wolinska bodies are present, which are large eosinophilic intracytoplasmic inclusions
- Severe degeneration can cause fragmented, abundant, vacuolated or granular cytoplasm
- Interface between the nucleus and cytoplasm becomes indistinct
- Severely degenerated cells should not be considered when rendering a specimen diagnosis
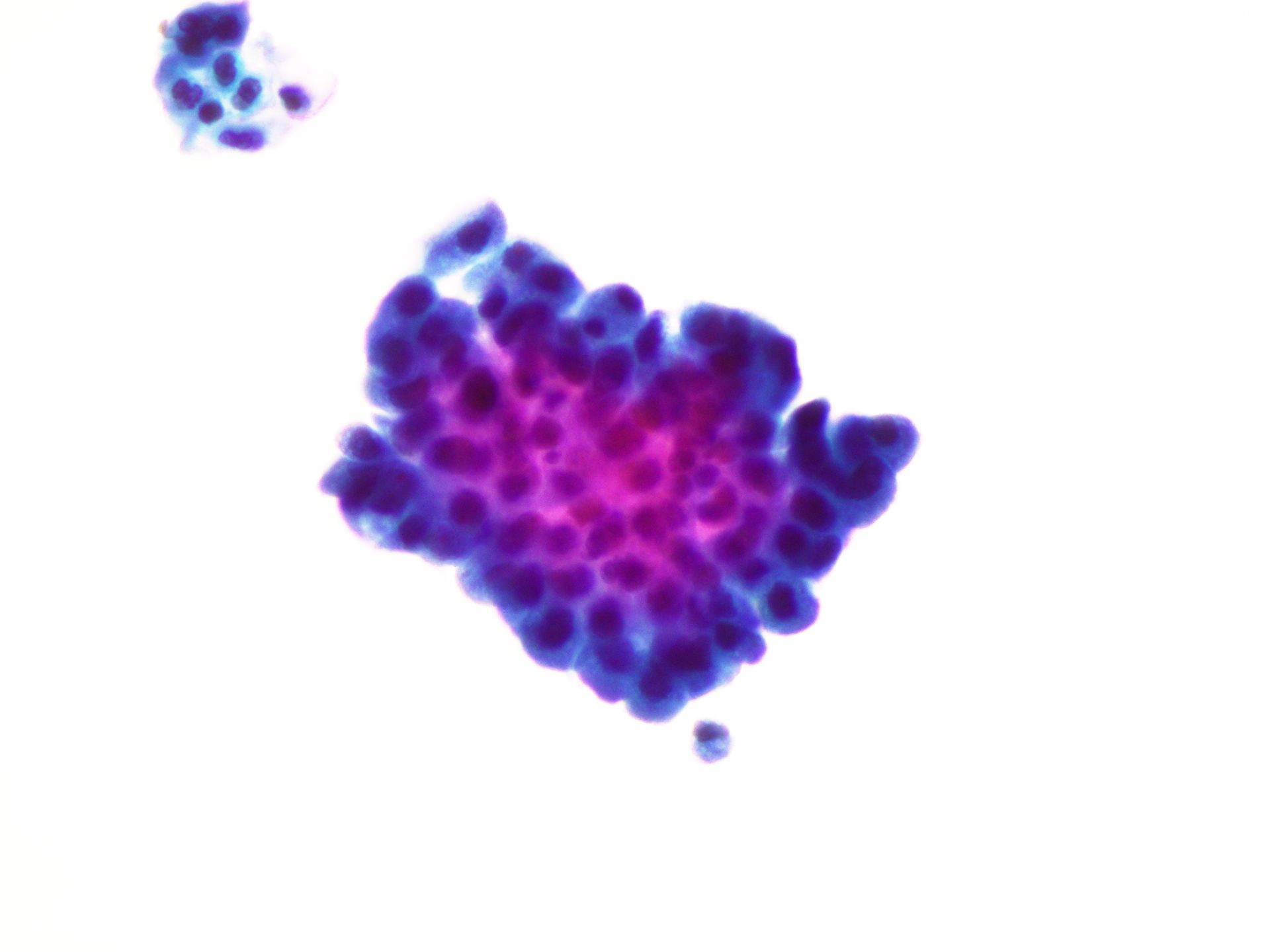
- Benign urothelial tissue fragments
- Benign urothelial cells in papillary clusters with community borders
- Normal N:C ratio
- These fragments can be difficult to assess
- Conglomerate of overlapping cells may make it appear atypical, with hyperchromasia, high N:C ratio and distorted irregular shape
- Cytological evaluation is more accurate at the edge of the fragment
- Urinary crystals
- Common finding
- Not usually interpreted on cytology report
- Triple phosphate: shaped like prisms / coffin lids
- Uric acid: vary in shape and size
- Calcium oxalate: oval, dumbbell shaped
- Ammonium biurate: spiculated spheres
- Cysteine: hexagonal
- Casts
- Granular cast: coarse or finely granular debris
- Hyaline cast: glassy, homogeneous texture
- Granular and hyaline casts can be found in normal urine
- Red blood cell casts are indicative of glomerular disease
- White blood cell casts are indicative of tubulointerstitial disease or transplant rejection
- References: Wojcik: The Paris System for Reporting Urinary Cytology, 2nd Edition, 2022, Cibas: Cytology - Diagnostic Principles and Clinical Correlates, 5th Edition, 2019
Cytology images
Molecular / cytogenetics description
Biomarker testing
- UroVysion™
- Fluorescence in situ hybridization assay (FISH)
- Gains of 3, 7 and 17 as well as loss of 9p21 abnormalities are determined using fluorescently labeled pericentromeric DNA probes
- Sensitivity of 84.2% and specificity of 91.8% for urothelial carcinoma detection
- Has been shown to be positive in nonurothelial carcinomas, such as primary and secondary bladder adenocarcinoma, squamous cell carcinoma, urachal carcinoma or metastatic carcinoma
- U-FISH has the advantage of high sensitivity and specificity in cytologically uncertain and negative urine samples not affected by hematuria, urinary tract infection or Bacillus Calmette Guerin (BCG) induced inflammatory response
- Sensitivity of FISH to detect low grade tumors is low
- Utilized for the follow up monitoring of bladder cancer
- FISH has a higher sensitivity and specificity as compared to other noninvasive detection techniques
- Bladder tumor antigen (BTA) (Urol Oncol 2023;41:484.e17)
- Complement factor H related protein secreted by malignant cells
- Food and Drug Administration (FDA) approved the point of care (POC) test BTA stat™ and enzyme linked immunosorbent assay (ELISA) test BTA TRAK™ for surveillance of patients with urothelial carcinoma with concurrent use of cystoscopy
- Urine collection should be without fixative / preservative
- Higher sensitivity than cytology
- Use of BTA as biomarker may improve surveillance, allowing more effective tracking for the presence or recurrence of high grade UC
- Elevated false positive rate in patients with common urinary tract diseases (urinary tract infection [UTI], urolithiasis)
- Sensitivity and specificity of these tests affected by patient selection in studies
- Stat™ sensitivity: 64% (range 58 - 69%) specificity: 77% (range 73 - 81%)
- TRAK™ sensitivity: 65% (range 54 - 75%) specificity: 74% (range 64 - 82%)
- Nuclear matrix protein 22 (NMP22) (Urol Clin North Am 2000;27:47, Urol Oncol 2023;41:484.e17)
- Detects nuclear matrix protein that comes from apoptotic cells
- Nuclear matrix proteins play a part in DNA replication, RNA transcription and gene expression regulation
- NMP22 is elevated in malignant tumor cells
- Utilized for diagnosis and surveillance of urothelial carcinoma
- Common bladder conditions (UTI, urolithiasis, trauma) may cause elevated NMP22
- Has a sensitivity of 32 - 92% and a specificity of 51 - 94%
- False positive risk if voided urine samples obtained within 5 days after instrumentation
- FDA approved: quantitative ELISA NMP22 test kit and qualitative NMP22 BladderChek point of care test
- Cost effective: cheaper than a cytology urine reading
- Bladder cancer immunofluorescence assay (BCIA)
- 3 fluorescent monoclonal antibodies (M344, LDQ10 and 19A211)
- Detect carcinoembryonic antigen and sulfated mucin glycoproteins on voided urine
- Combined with cytology for surveillance
- More sensitive in detecting low grade tumors
- UBC® rapid test
- Measures cytokeratin 8 and 18 fragments based on immunochromatographic methods
- Uses a photometric reader
- High rate of false positive results
- Sensitivity: 53.3 - 70.8%, specificity: 61.4 - 93.8%
- Other ancillary tests
- FDA approved
- Wide variety of tests utilizing ELISA, polymerase chain reaction (PCR), next generation sequencing (NGS), microRNA, genetic profiling
- ADXBLADDER, CxBladder Monitor, Bladder EpiCheck, uCAPP-Seq, AssureMDx, UroSeek
- NGS has a high sensitivity for both low and high grade UC
- References: Wojcik: The Paris System for Reporting Urinary Cytology, 2nd Edition, 2022, Hoda: Diagnostic Liquid-Based Cytology, 1st Edition, 2017
Sample pathology report
- Urine cytology (voided), satisfactory for evaluation:
- Negative for high grade urothelial carcinoma (see comment)
- Comment: Urothelial cells, squamous cells, mixed inflammatory cells and microscopic hematuria. Urothelial cells have normal N:C ratios and lack features of high grade urothelial carcinoma, such as hyperchromasia, nuclear irregularities or coarse / clumped chromatin.
Board review style question #1
Which of the following describes the U-FISH (UroVysion™) test for bladder cancer?
- Utilizes 3 fluorescent monoclonal antibodies (M344, LDQ10 and 19A211) to detect carcinoembryonic antigen and sulfated mucin glycoproteins on voided urine
- Detects complement factor H related protein secreted by malignant cells
- Identifies nuclear matrix protein that comes from apoptotic cells
- Uses fluorescently labeled pericentromeric DNA probes to detect gains of 3, 7 and 17 as well as loss of 9p21 abnormalities
Board review style answer #1
D. Uses fluorescently labeled pericentromeric DNA probes to detect gains of 3, 7 and 17 as well as loss of 9p21 abnormalities. Answer B is incorrect because bladder tumor antigen (BTA) utilizes complement factor H related protein secreted by malignant cells. Answer C is incorrect because nuclear matrix protein 22 detects nuclear matrix protein that comes from apoptotic cells. Answer A is incorrect because bladder cancer immunofluorescence assay (BCIA) utilizes 3 fluorescent monoclonal antibodies (M344, LDQ10 and 19A211) to detect carcinoembryonic antigen and sulfated mucin glycoproteins on voided urine.
Comment Here
Reference: Cytology-general, normal findings & biomarker testing
Comment Here
Reference: Cytology-general, normal findings & biomarker testing
Board review style question #2
Board review style answer #2
C. Melamed-Wolinska bodies. Melamed-Wolinska bodies are present, which are large eosinophilic intracytoplasmic inclusions. These are seen in degenerative changes. Answer A is incorrect because the morphology is of spiculated spheres. Answer D is incorrect because renal tubular cells (RTCs) have a morphology consisting of high N:C ratio if originating from distal convoluted tubules or low N:C ratios with granular cytoplasm if originating from the proximal convoluted tubules. Answer B is incorrect because these cells consist of coarse or finely granular debris.
Comment Here
Reference: Cytology-general, normal findings & biomarker testing
Comment Here
Reference: Cytology-general, normal findings & biomarker testing