Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Samarska I., Epstein J. Condyloma acuminatum. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/bladdercondyloma.html. Accessed April 2nd, 2025.
Definition / general
- Rare lesion of the urinary bladder, composed of hyperplastic papillary fronds of squamous epithelium with koilocytosis and viral atypia
- Caused by human papillomavirus (HPV) (both low risk HPV and high risk HPV)
Essential features
- Polypoid lesion composed of hyperplastic papillary fronds of squamous epithelium with koilocytosis and viral atypia
- Caused by HPV (both low risk HPV and high risk HPV) but negative RNA in situ hybridization does not exclude condyloma acuminatum
- Often immunocompromised patients and history of anogenital condylomata
- Differential diagnosis includes squamous papilloma, squamous metaplasia, verrucous squamous hyperplasia and papillary urothelial carcinoma
ICD coding
- ICD-10: N32.9 - Bladder disorder, unspecified
Epidemiology
- M > F (Am J Surg Pathol 2019;43:1547)
- Commonly presents after the fourth decade
- Associated with HPV related lesions of genitourinary tract (anogenital condyloma acuminatum, anal in situ neoplasia (AIN), etc) and immunosuppression
- Related to squamous cell carcinoma of bladder (Am J Surg Pathol 2019;43:1547, Am J Surg Pathol 2006;30:883, Am J Surg Pathol 2007;31:1777)
Sites
- Urethra (more common) and urinary bladder (rare)
Pathophysiology
- HPV infection that affects the urinary tract, including the urethra and urinary bladder; is thought to be transmitted through sexual contact with infection of external genitalia (J Infect Chemother 2014;20:741)
- Few studies showed features of HPV infection and cytological atypia of urethral pap smears in high risk HPV positive samples (Diagn Cytopathol 2012;40:597; Diagn Cytopathol 2014;42:491)
Etiology
- Caused by HPV (both low risk HPV and high risk HPV)
Clinical features
- Complaints of micturition pain, urinary frequency, urgency and nocturia up to three times per night (Urol Case Rep 2017;12:76)
- Often immunocompromised patients (history of organ transplantation, HIV/AIDS, viral hepatitis, autoimmune disease, etc.) and history of anogenital condylomata (Am J Surg Pathol 2019;43:1547, Am J Surg Pathol 2006;30:883)
Diagnosis
- Cystoscopy
- Diagnosis is by biopsy or surgical resection
Prognostic factors
- Often recurs
- At risk for in situ and invasive squamous cell carcinoma
Case reports
- 30 year old woman with history of HPV positive anal and genital warts (Urol Case Rep 2017;12:76)
- 30 year old woman diagnosed 12 months after renal transplantation (Transpl Infect Dis 2017;19)
- 33 year old man with renal transplant diagnosed 5 years after transplantation (Transplant Proc 2018;50:2553)
- 34 year old man with renal transplant (Clin Genitourin Cancer 2017;15:e739)
- 62 year old man with rheumatoid arthritis and symptoms of urinary obstruction (Am J Case Rep 2018;19:1522)
Treatment
- Transurethral resection
- Some studies suggest that BCG, which is often used for recurrent or multiple noninvasive papillary urothelial carcinomas, is also an effective therapy for recurrent penile or uterine cervical condylomata and thus can be used for treatment of condyloma acuminatum of the urinary bladder
Gross description
- Depends on the size of the lesion and often not remarkable
- Smooth, pink-tan, papillary
Microscopic (histologic) description
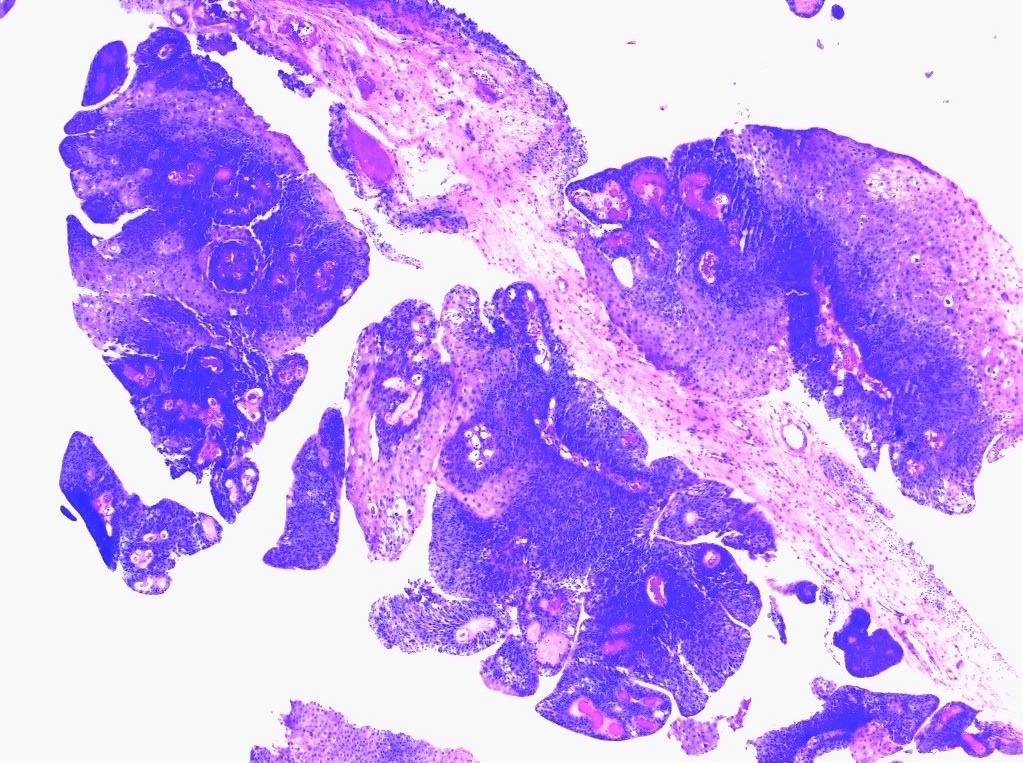
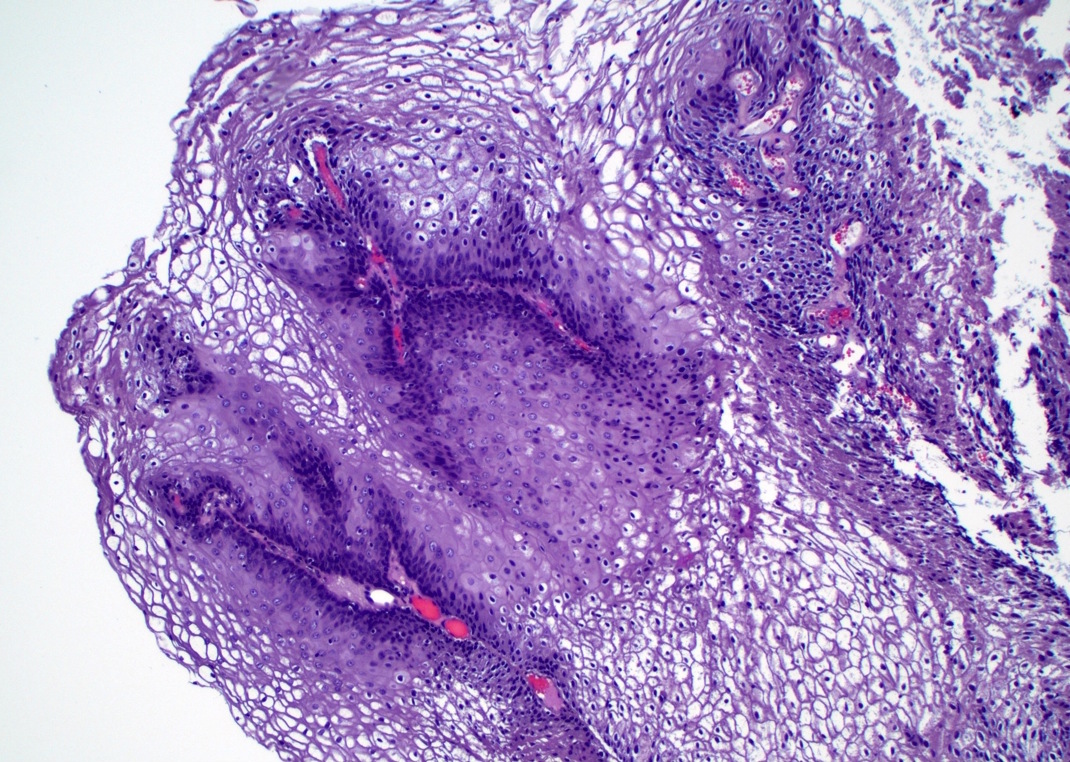
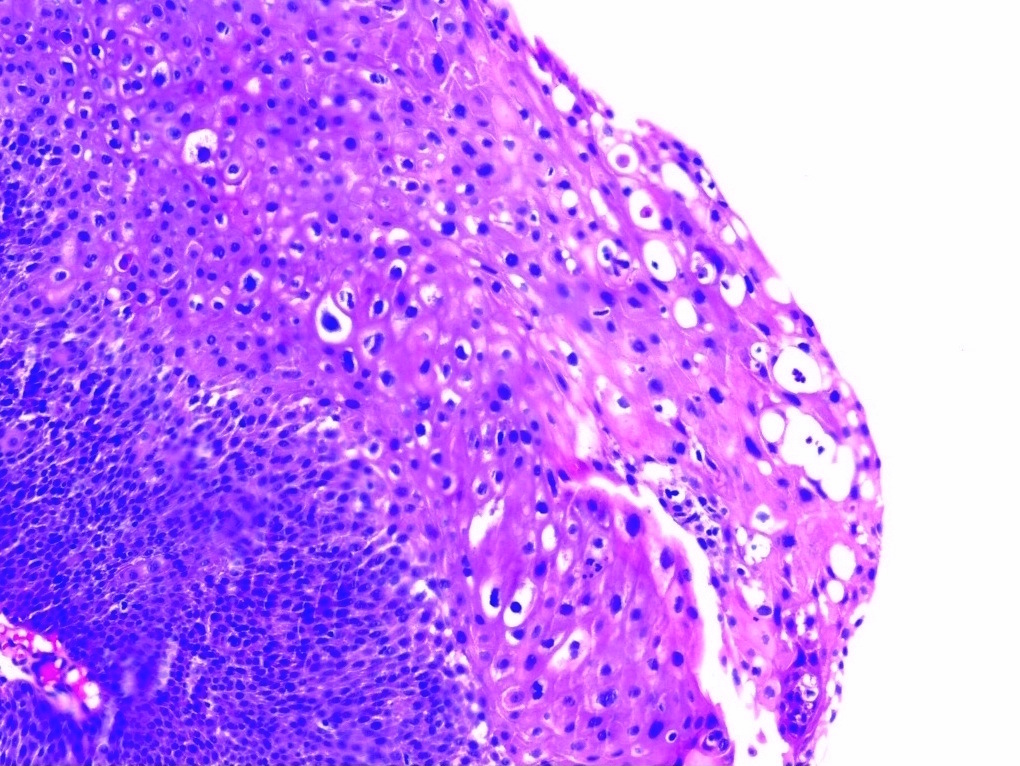
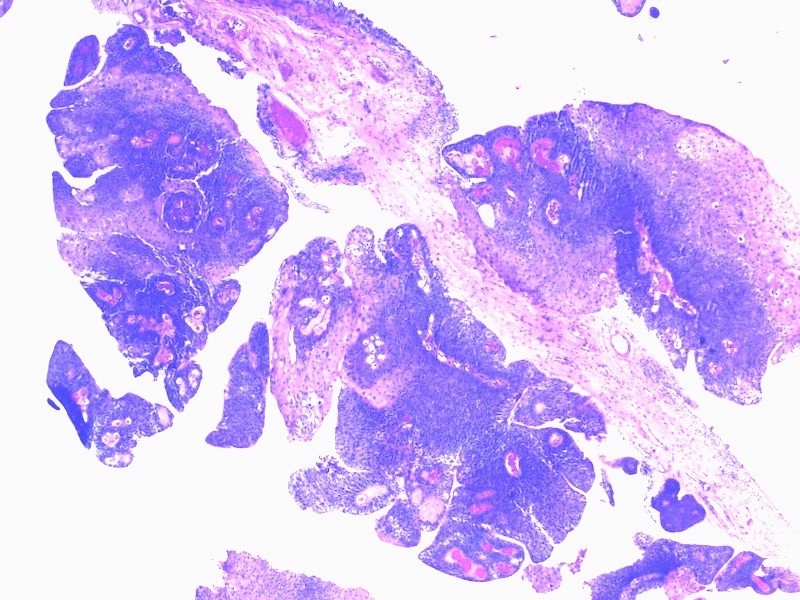
- Exophytic lesion
- Nonkeratinizing, hyperplastic papillary fronds of squamous epithelium
- Lack free floating papillary fronds
- Cells with koilocytosis and viral atypia (Am J Surg Pathol 2006;30:883)
Microscopic (histologic) images
Molecular / cytogenetics description
- RNA in situ hybridization testing for low risk and high risk HPV is needed
- Can be positive for either low risk or high risk HPV or both (Am J Surg Pathol 2019;43:1547)
- Negative RNA in situ hybridization for HPV does not exclude condyloma acuminatum if the histology is characteristic (Am J Surg Pathol 2019;43:1547)
Sample pathology report
- Urinary bladder, papillary lesion, transurethral resection:
- Condyloma acuminatum (see comment)
- Comment: The lesion is positive for low risk HPV. Condyloma acuminatum of bladder can be associated with in situ or invasive squamous cell carcinoma. Therefore, close followup is warranted. Additional sampling is recommended to exclude concomitant squamous cell carcinoma if clinically indicated.
Differential diagnosis
- Squamous papilloma:
- More common in women
- Shows free floating papillary fronds
- Well established fibrovascular cores
- Lined by a benign squamous nonkeratinizing epithelium
- Lacks koilocytosis or viral atypia
- Unrelated to HPV infection
- Squamous metaplasia:
- Can be divided into nonkeratinizing and keratinizing types
- Nonpolypoid flat lesion consisting of a thickened squamous epithelium with an overlying thick keratin layer
- Squamous dysplasia may be seen
- Glycogenated squamous metaplasia have cleared out cytoplasm but lacks papillary growth and viral atypia
- Verrucous squamous hyperplasia:
- Spiking squamous hyperplasia with marked hyperkeratosis, parakeratosis and elongation of the rete pegs
- No viral atypia
- This lesion might be related to invasive squamous cell carcinoma
- Papillary urothelial carcinoma:
- Can have clear cytoplasm
- Lacks viral atypia
- Typically has more exophytic free floating papillary fronds
- High-grade noninvasive urothelial carcinoma with FGFR3 mutation:
- Has a urothelial lining with polygonal cells, distinct cell borders, clear cell to eosinophilic cytoplasm and prominent koilocytic nuclei
Additional references
Board review style question #1
- A 30 year old woman presents with micturition pain and urinary obstruction symptoms. Transurethral bladder resection revealed a polypoid mass, composed of hyperplastic papillary fronds of squamous epithelium with koilocytosis and viral atypia. What would be the most appropriate ancillary test?
- Immunohistochemistry for p40 and p63
- Immunohistochemistry for CK20 and p53
- RNA ISH for low risk and high risk HPV
- Immunohistochemistry for p16
Board review style answer #1
C. RNA ISH for low risk and high risk HPV. The lesion may be a urinary bladder condyloma acuminatum.
Comment Here
Reference: Condyloma acuminatum
Comment Here
Reference: Condyloma acuminatum
Board review style question #2
- Transurethral resection of a bladder mass in a 45 year old man with a history of renal transplantation revealed a condyloma acuminatum of the prostatic urethra. Which lesion can be related to the condyloma acuminatum?
- No clinically significant relation known
- Squamous cell carcinoma (either invasive or in situ)
- Invasive urothelial carcinoma
- Squamous metaplasia
Board review style answer #2
B. Squamous cell carcinoma (either invasive or in situ). Patients are at risk for concomitant or subsequent squamous cell carcinoma (either invasive or in situ).
Comment Here
Reference: Condyloma acuminatum
Comment Here
Reference: Condyloma acuminatum