Table of Contents
Definition / general | Essential features | Radiology | Odontology | Histology | Microbiology | Sexual assault kit | DNA | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Khan M, Wilson A. Ancillary investigations. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/autopsyancillary.html. Accessed March 30th, 2025.
Definition / general
- Medicolegal autopsy is supplemented by ancillary investigations to help determine or corroborate the cause of death (COD), manner of death (MOD) and to positively identify unknown deceased individuals
- Ancillary investigations include radiology, odontology, histology, microbiology, sexual assault kits, DNA testing and vitreous fluid analysis (Forensic Sci Int 2020;310:110235)
- Ancillary investigations supplement the anatomic findings identified during the autopsy
Essential features
- Common types of ancillary investigations:
- Radiology
- Odontology
- Histology
- Microbiology
- Sexual assault kits
- DNA testing
- Vitreous fluid analysis
Radiology
When to use:
Methods:
Case examples:
Limitations:
Essential features:
Contributed by Allecia Wilson, M.D.
- To identify and document injuries, projectiles, projectile fragments in cases of homicide, incineration, motor vehicle accidents, infant deaths, decomposition or cases of suspicious circumstances (Forensic Sci Med Pathol 2014;10:583)
- Also to positively identify decedents
Methods:
- Conventional radiography, such as whole body Xray scanner (Int J Legal Med 2020;134:655)
- CT scan
- Radiography skeletal survey
- Adjunctive imaging, like fluoroscopy, MRI or CT angiogram, is case dependent
Case examples:
- Images are read by the medical examiner to aid in the gross examination (recovering projectiles or documenting fractures) or a formal consult is performed by a radiologist
- Conventional radiography is used to visualize the bones for fractures and lesions, age estimation and detect foreign bodies (projectiles or projectile fragments)
- Radiography skeletal survey and CT are utilized in child abuse (Forensic Sci Int 2006;164:131)
- MRI is good for visualizing soft tissue and helpful in blunt force trauma, like strangulation
- Tentatively identified decedents with medical hardware on imaging and medical records to document the previous surgery (helps with positive ID)
Limitations:
- Conventional radiology and CT cannot accurately visualize soft tissue and the image quality is user dependent
Essential features:
- Postmortem radiology is used to identify and document projectiles, projectile fragments, motor vehicle accidents, infant deaths and decomposition
- Conventional radiology is performed to visualize bone fractures and detect foreign objects, like projectile or projectile fragments
- Radiograph skeletal survey is done in all cases of child abuse
Contributed by Allecia Wilson, M.D.
Odontology
When to use:
How to perform:
Case examples:
Limitations:
Essential features:
Contributed by Allecia Wilson, M.D.
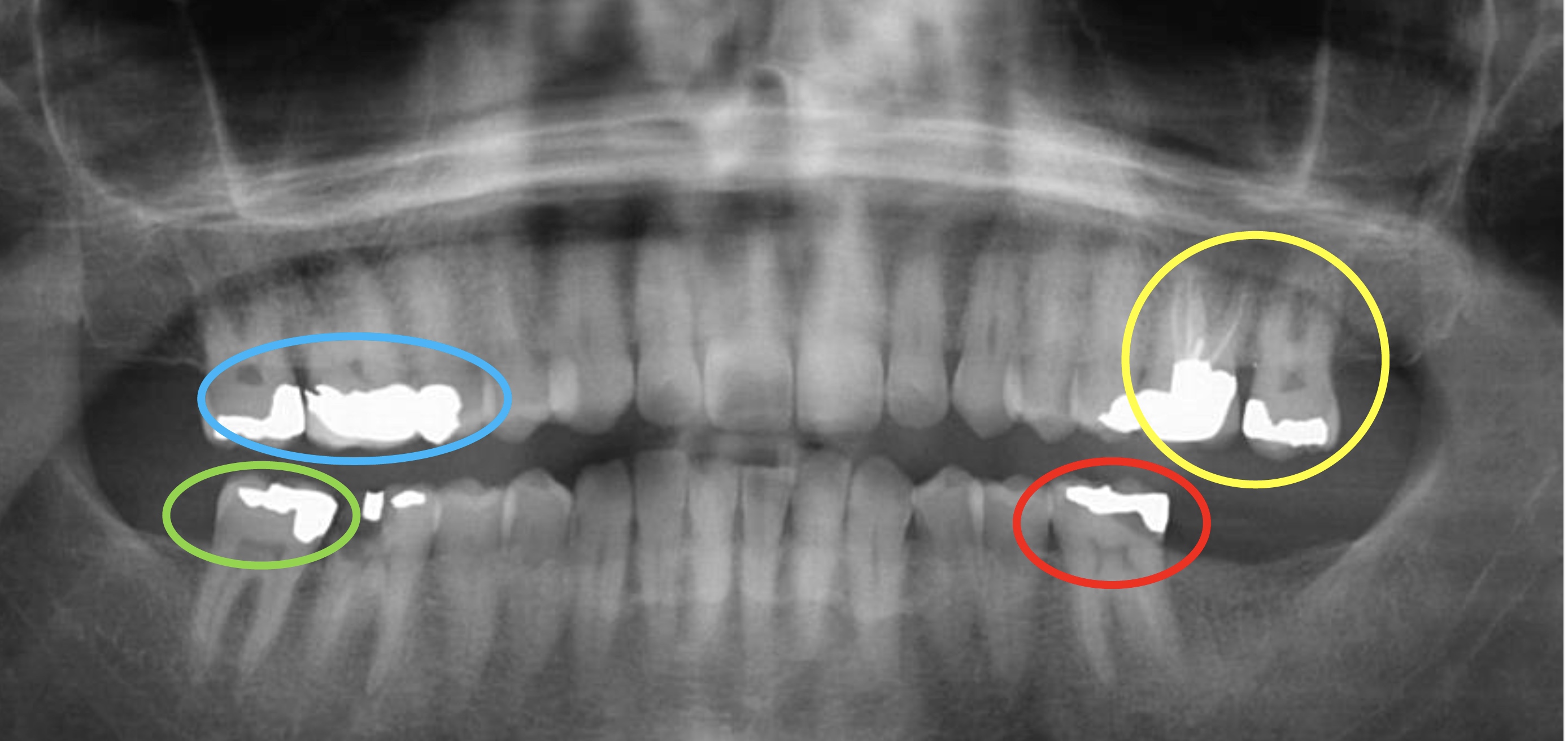
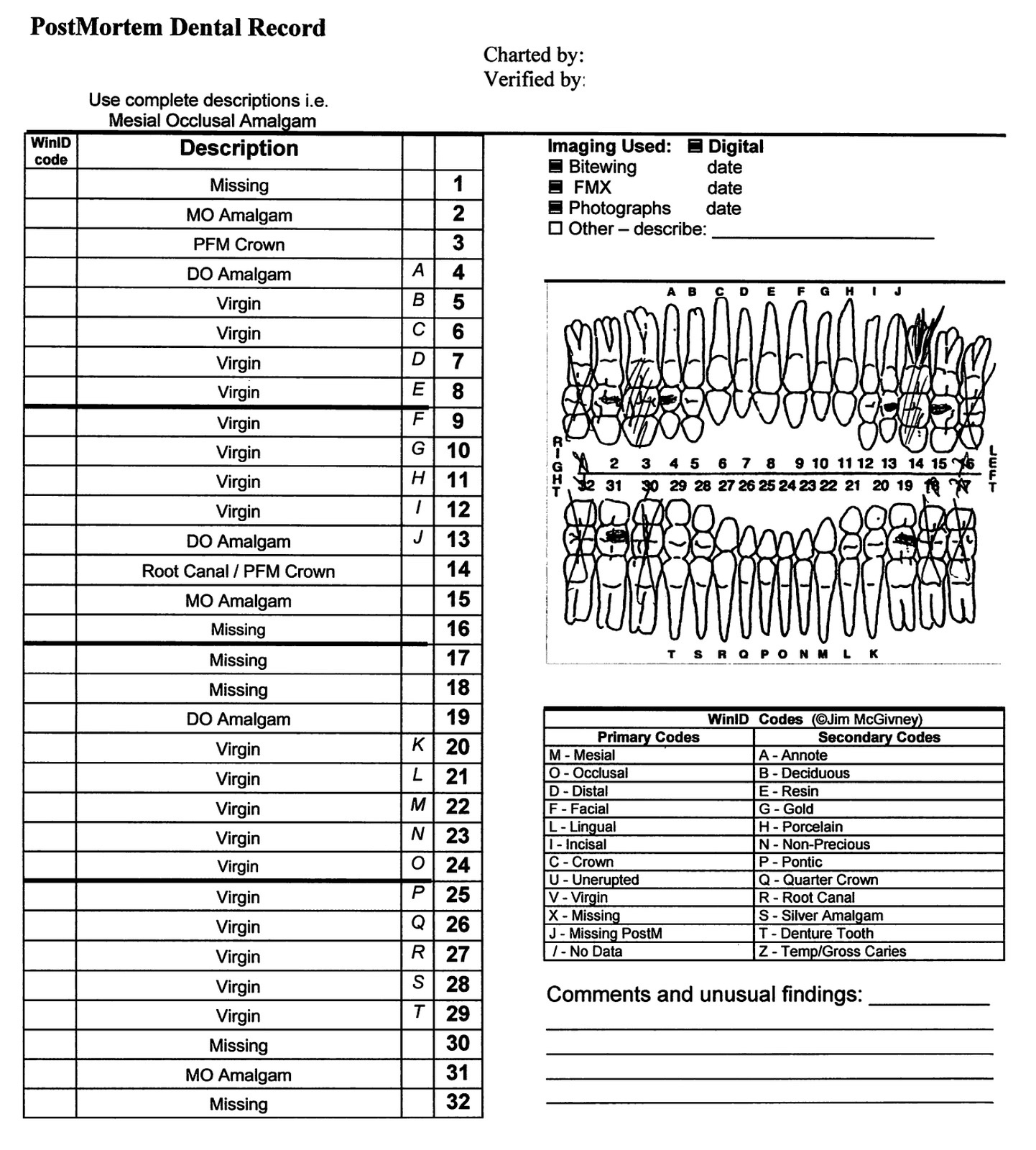
- To positively identify decedents when visual identification is not possible in cases such as incineration, decomposition, severe disfigurement, skeletonization and catastrophic events with multiple unidentified dead bodies, such as airline accidents, terrorist attacks and industrial accidents (StatPearls: Forensic Odontology [Accessed 3 June 2021])
How to perform:
- Forensic dentist photographs the upper and lower teeth and performs a dental exam that includes teeth charting or a dentogram for location and type of teeth fractures, decay, fillings and prostheses
- Comparative analysis is done between the postmortem dental exam and antemortem dental records that include a dentogram and radiology (J Oral Maxillofac Pathol 2019;23:164)
Case examples:
- Antemortem radiology is more specific because fillings are unique to an individual and are stagnant over time, versus dental charting, which may be illegible or frequently change
- Presumptive identification of the decedent can be used to obtain antemortem dental records
- Presumptive identifications include tattoos, government identification and a patient's name on prescription medication or medical records, along with others
Limitations:
- Age dependent; pediatric cases are limited by their growth and development
- Challenging to perform on edentulous decedents or those with poor dentition
Essential features:
- Postmortem dentogram is performed and compared with antemortem dental records to positively identify an unknown decedent
- Antemortem radiology is best because fillings are unique to an individual and are stagnant over time
Contributed by Allecia Wilson, M.D.
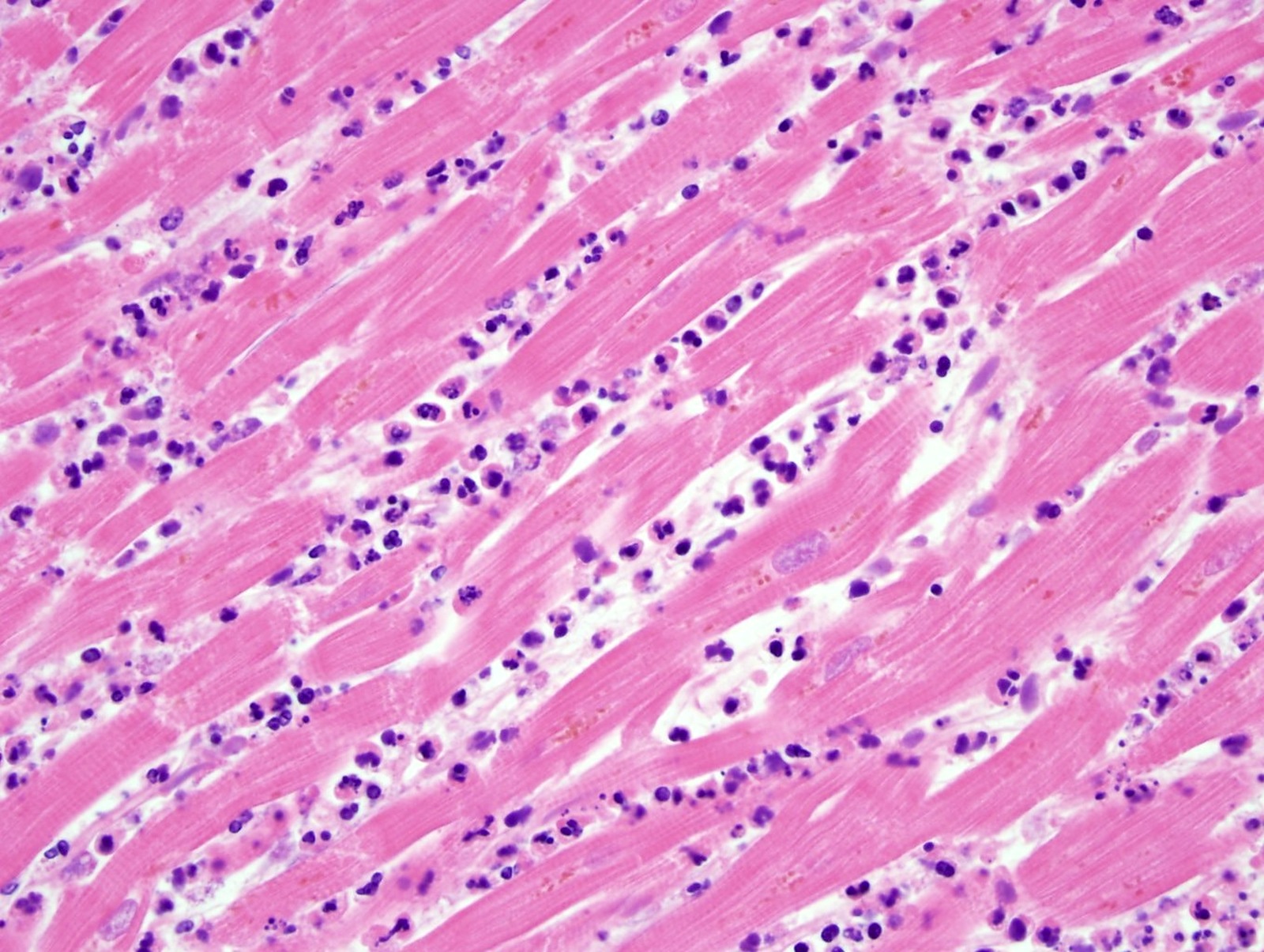
Histology
When to use:
How to perform:
Case examples:
Limitations:
Essential features:
Contributed by Myra Khan, D.O., Michael Caplan, M.D. and Maria Westerhoff, M.D.
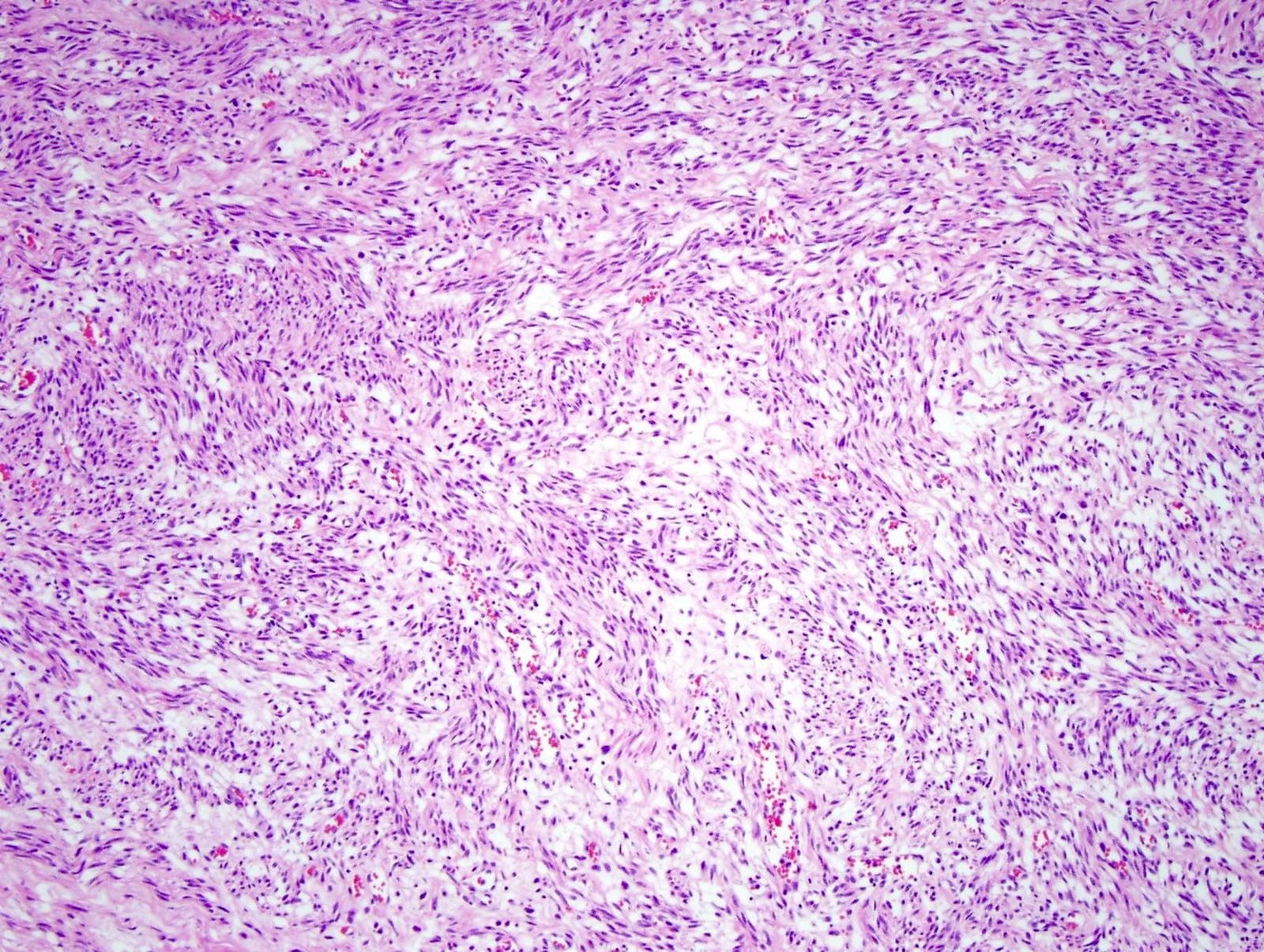
- To support or establish the COD and MOD
- Performed in cases of drug overdose, natural deaths, sudden unexplained death and all pediatric deaths
How to perform:
- Tissue sections are routinely taken from the heart, lungs, kidneys, liver and brain
- Tissue sections are processed and stained with H&E for standard histology
- Special stains can be performed, depending on the H&E
- Special stains include Masson trichrome for fibrosis, Prussian blue for hemosiderin, PAS or GMS for fungi, Gram stain for bacteria, Ziehl-Neelson for mycobacteria and Congo red for amyloid (Acad Forensic Pathol 2018;8:426)
Case examples:
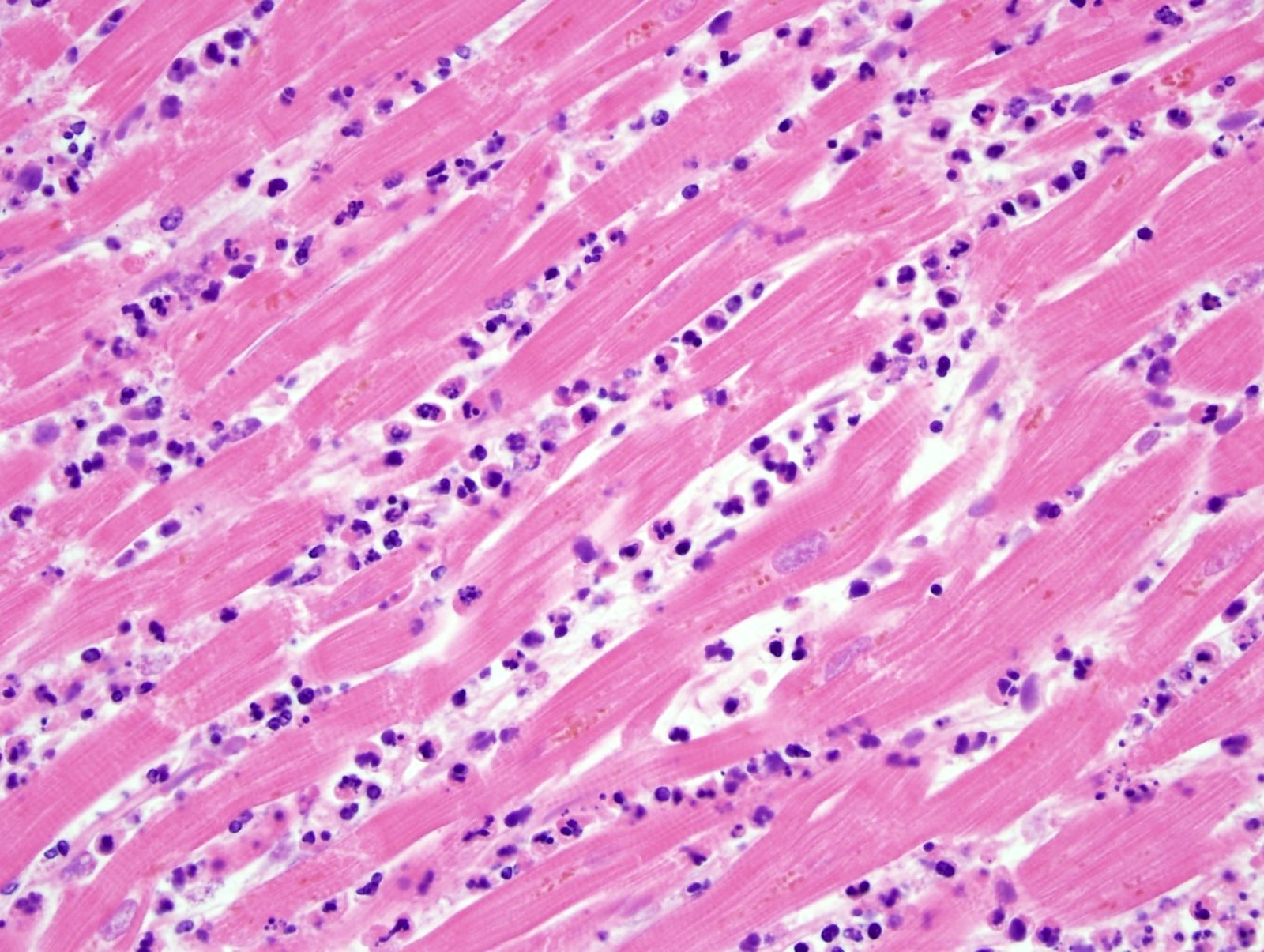
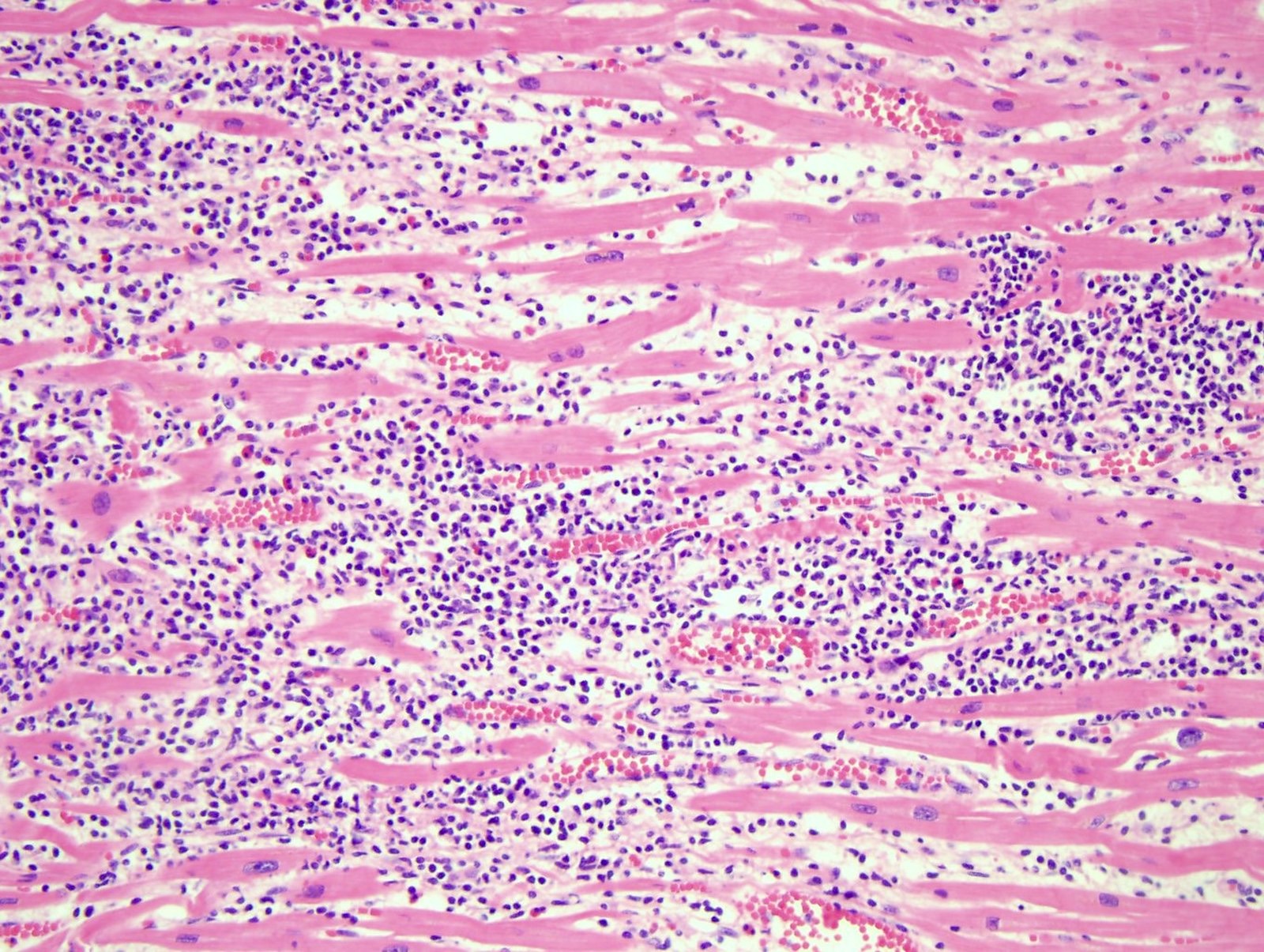
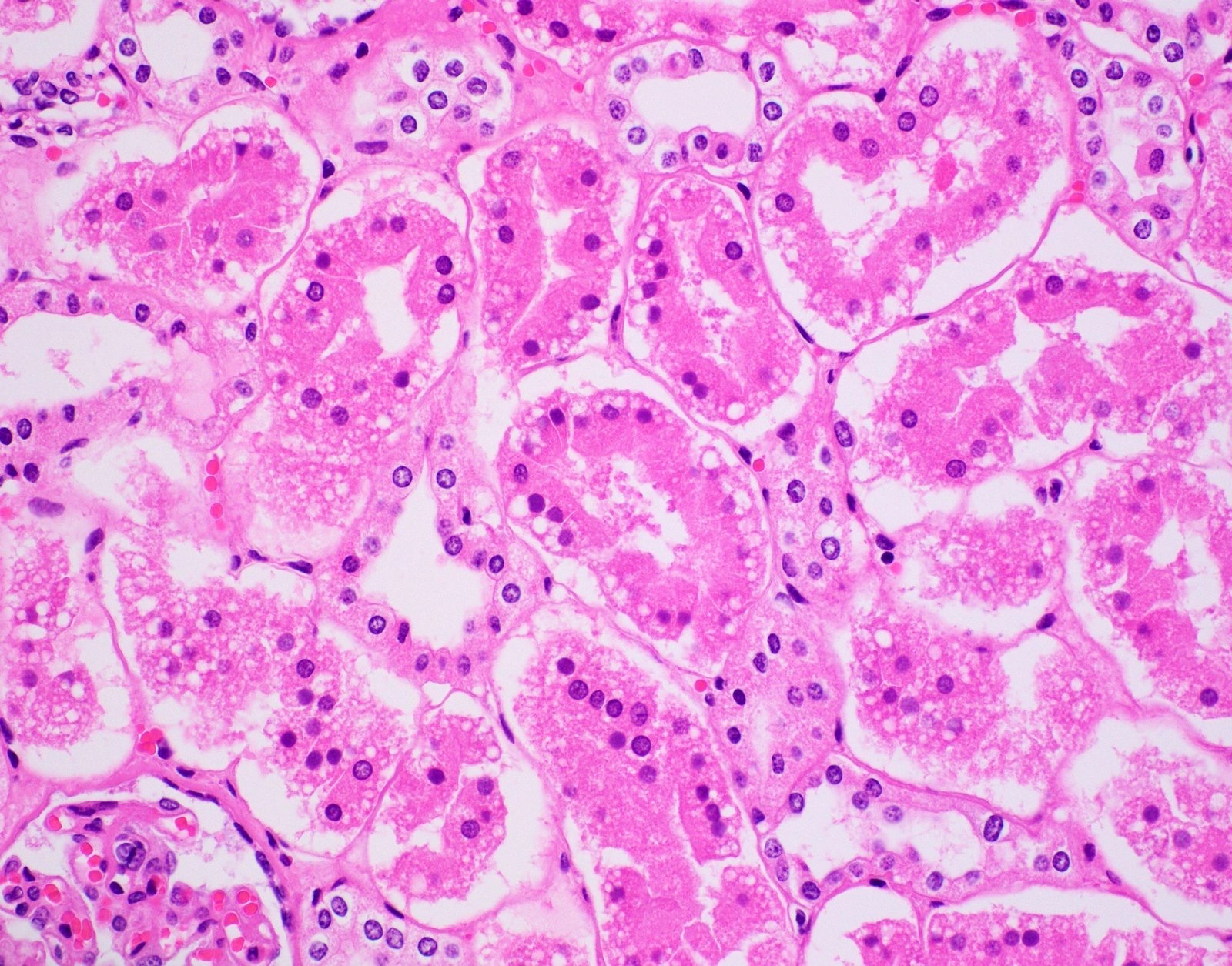
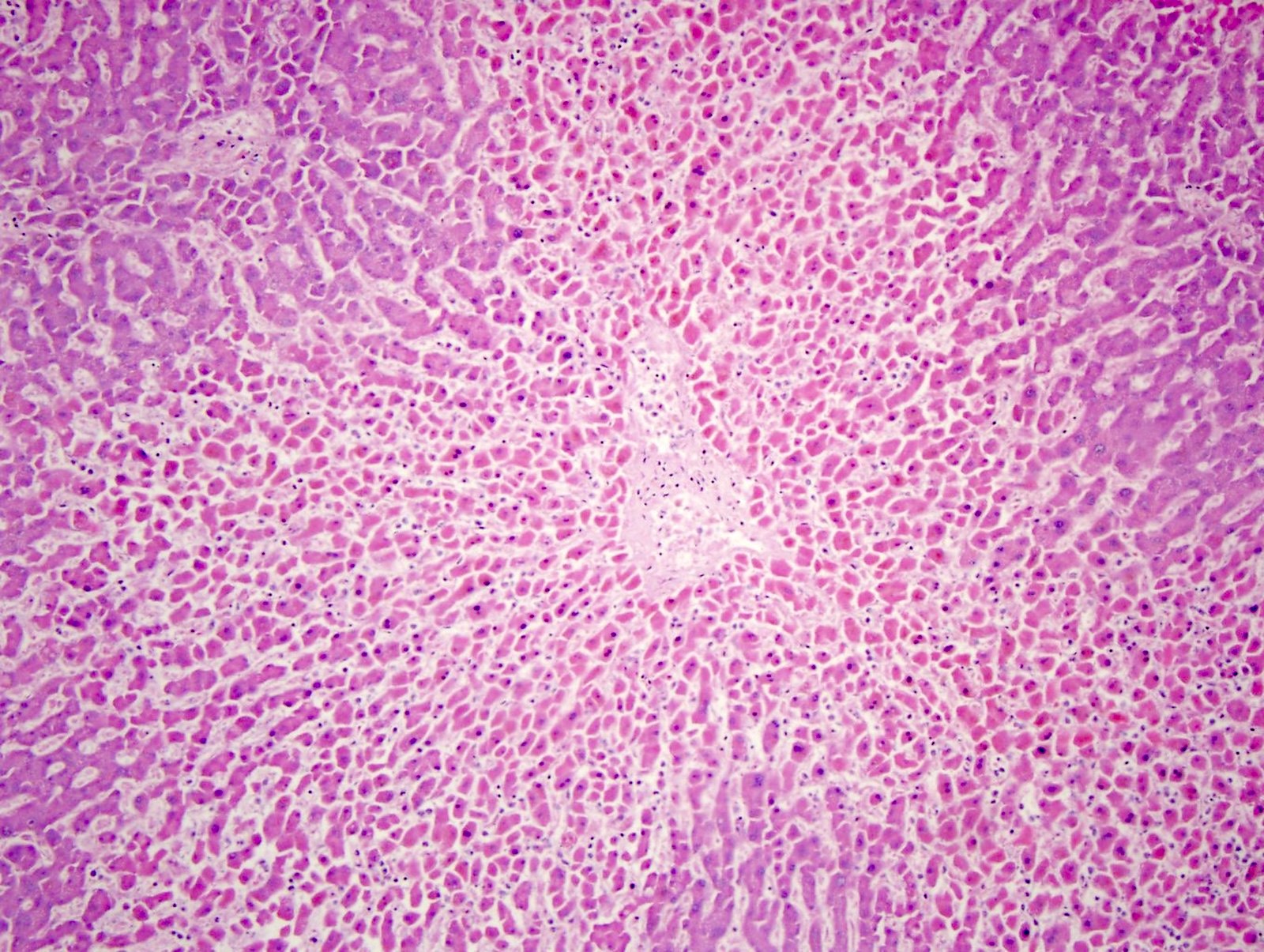
- Cardiac
- Histology helps to date a myocardial infarction:
- Acute myocardial infarction > 4 hours = myocyte necrosis with polymorphonuclear neutrophils (PMNs)
- Subacute myocardial infarction > 3 days = hemosiderin laden macrophages and granulation tissue
- Chronic myocardial infarction > 10 days = collagen deposition
- Acute viral myocarditis shows a lymphocytic infiltration in the myocardium and myocardial necrosis (Forensic Pathology Reviews 2008;5:239)
- Histology helps to date a myocardial infarction:
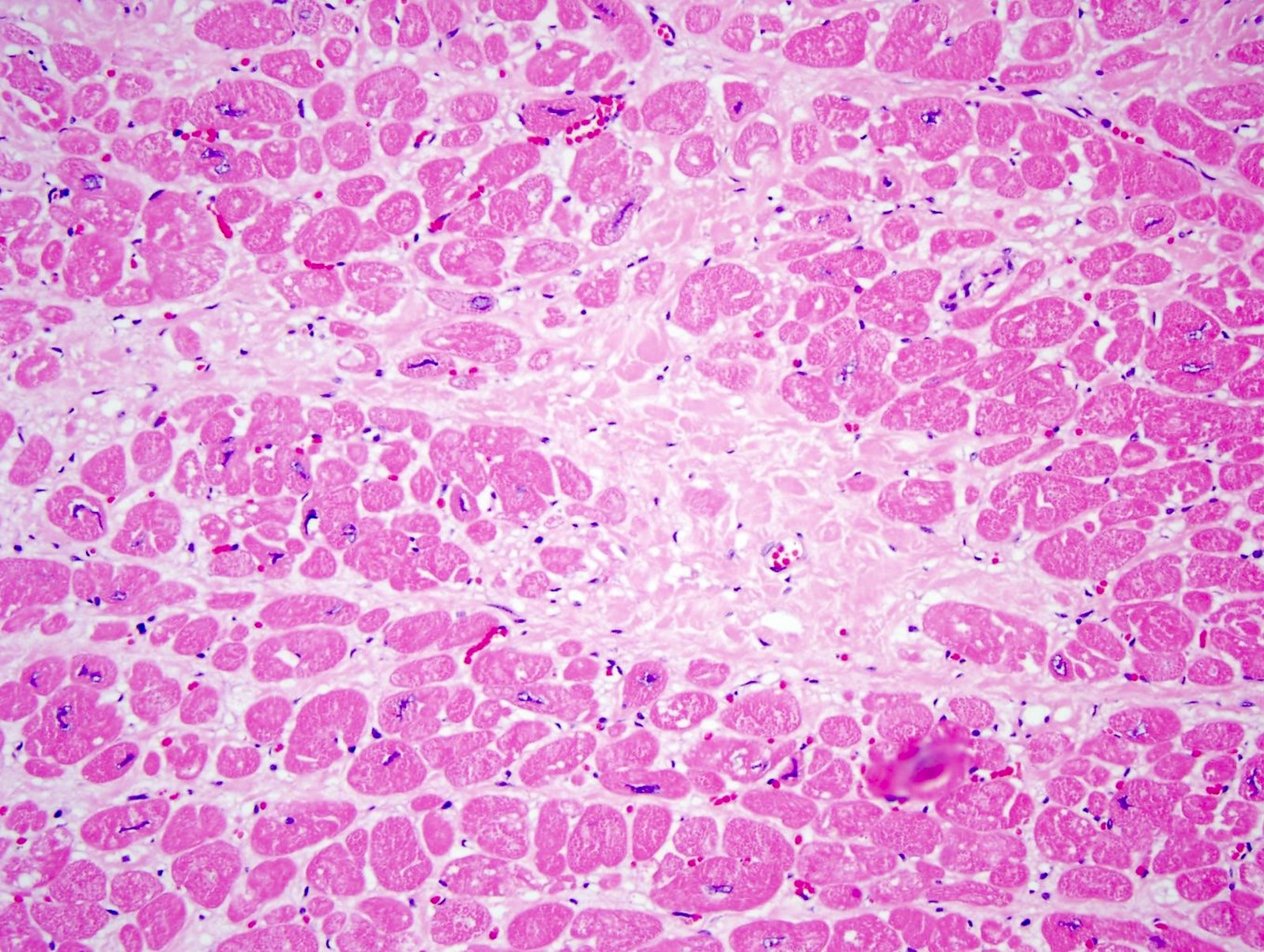
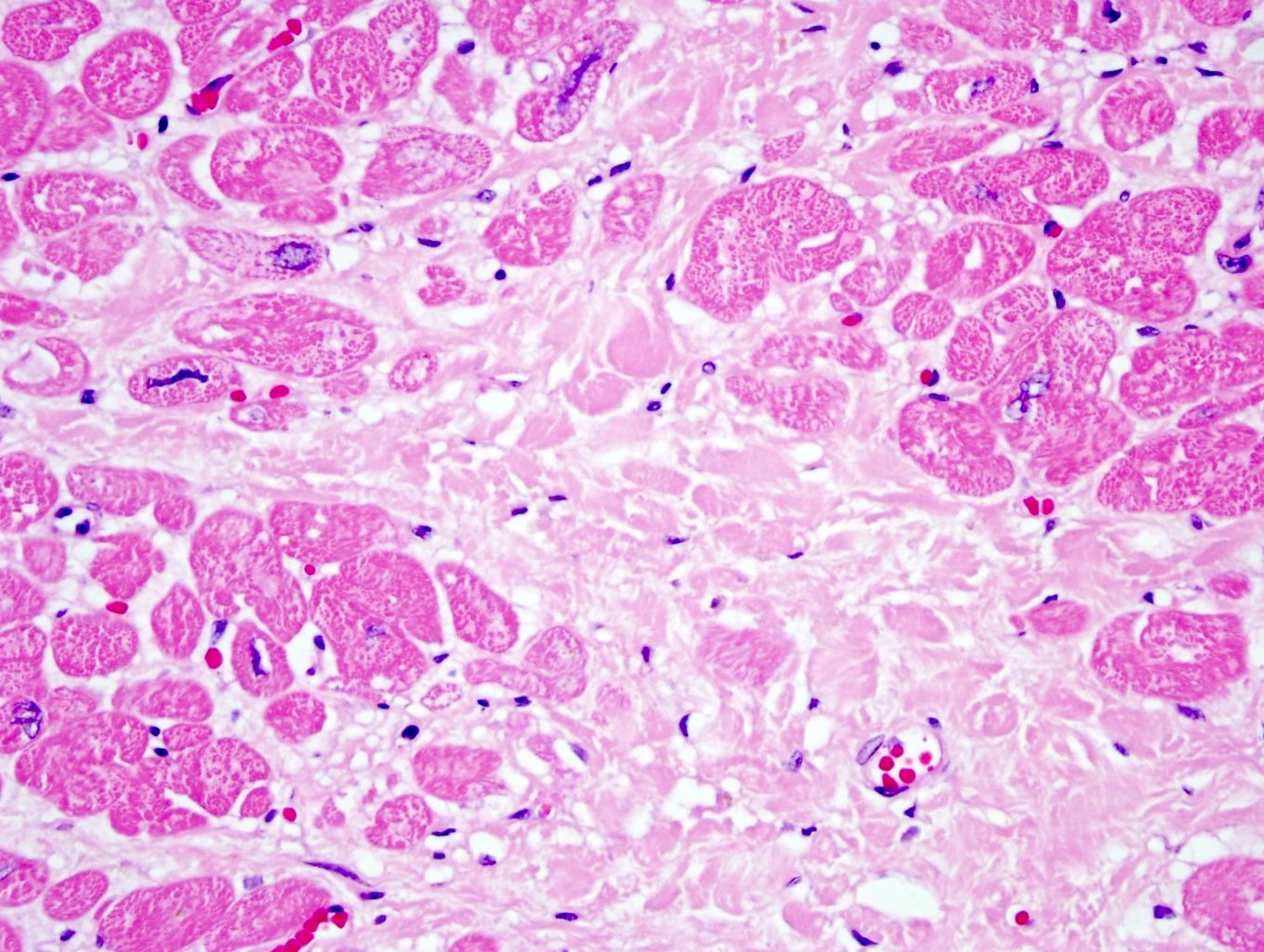
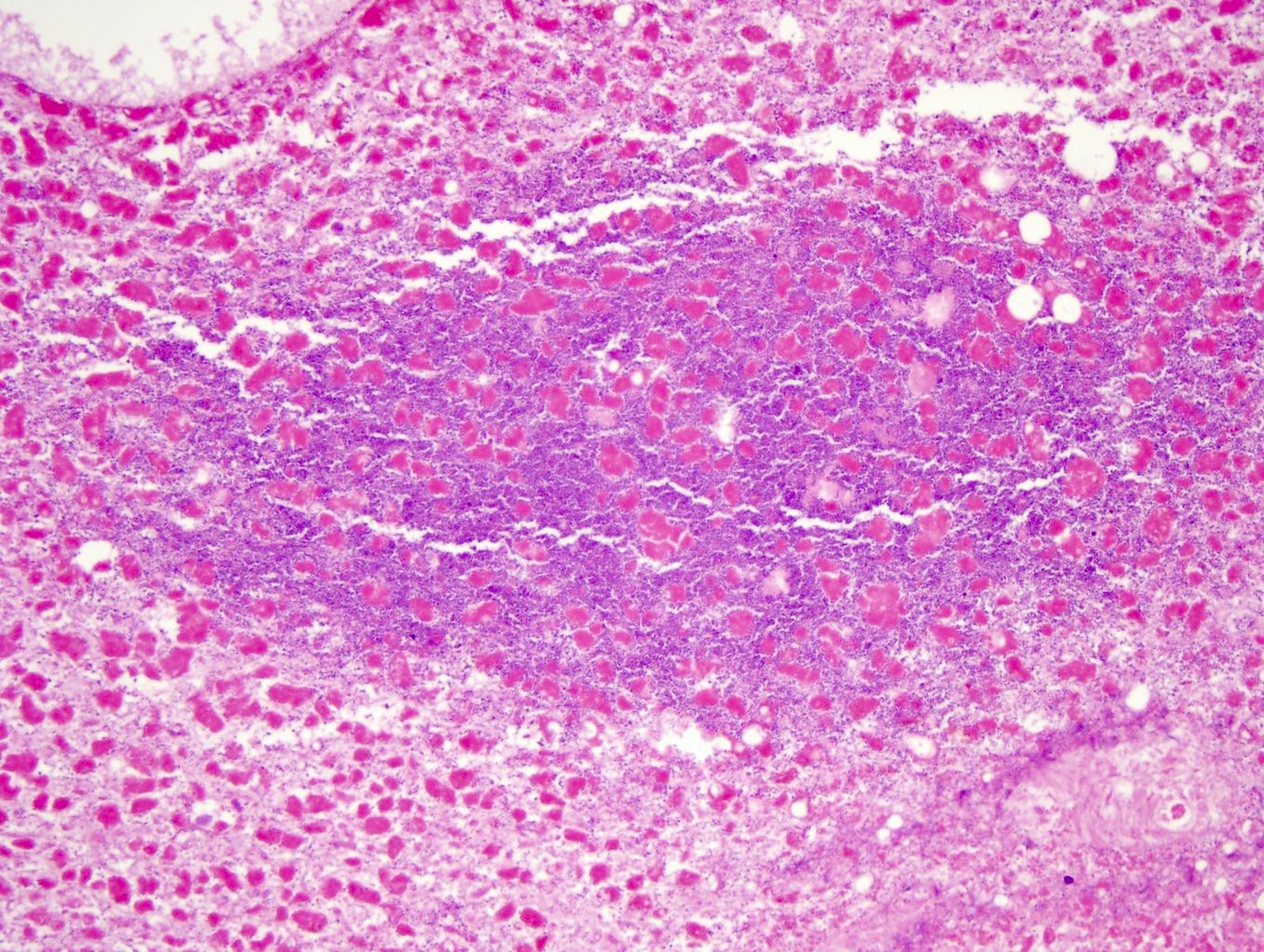
- Lungs
- Pulmonary embolism shows the layering of fibrin, platelets, RBCs and inflammatory cells, that differentiate it from a postmortem blood clot (Forensic Pathology Reviews 2008;5:239)
- Amniotic fluid in the pulmonary blood vessels is diagnostic for an amniotic fluid embolism
- Epithelial cells are highlighted with cytokeratin stains (AE1 / AE3, CAM5.2, CK7 and CK20) (Acad Forensic Pathol 2018;8:426)
- SARS-COVID-19 lung shows diffuse alveolar damages, cytological atypia of pneumocytes, syncytial change and giant cell formation; ISH for viral nuclear capsid antigen is positive in infected cells (Forensic Pathology Reviews 2008;5:239)
- Intravenous drug user (IVDU) has lung foreign body granuloma with polarizable material (made of talc, starch or other adulterants found injected in drugs like heroin, cocaine, amphetamines, etc.) (Forensic Pathology Reviews 2008;5:239)
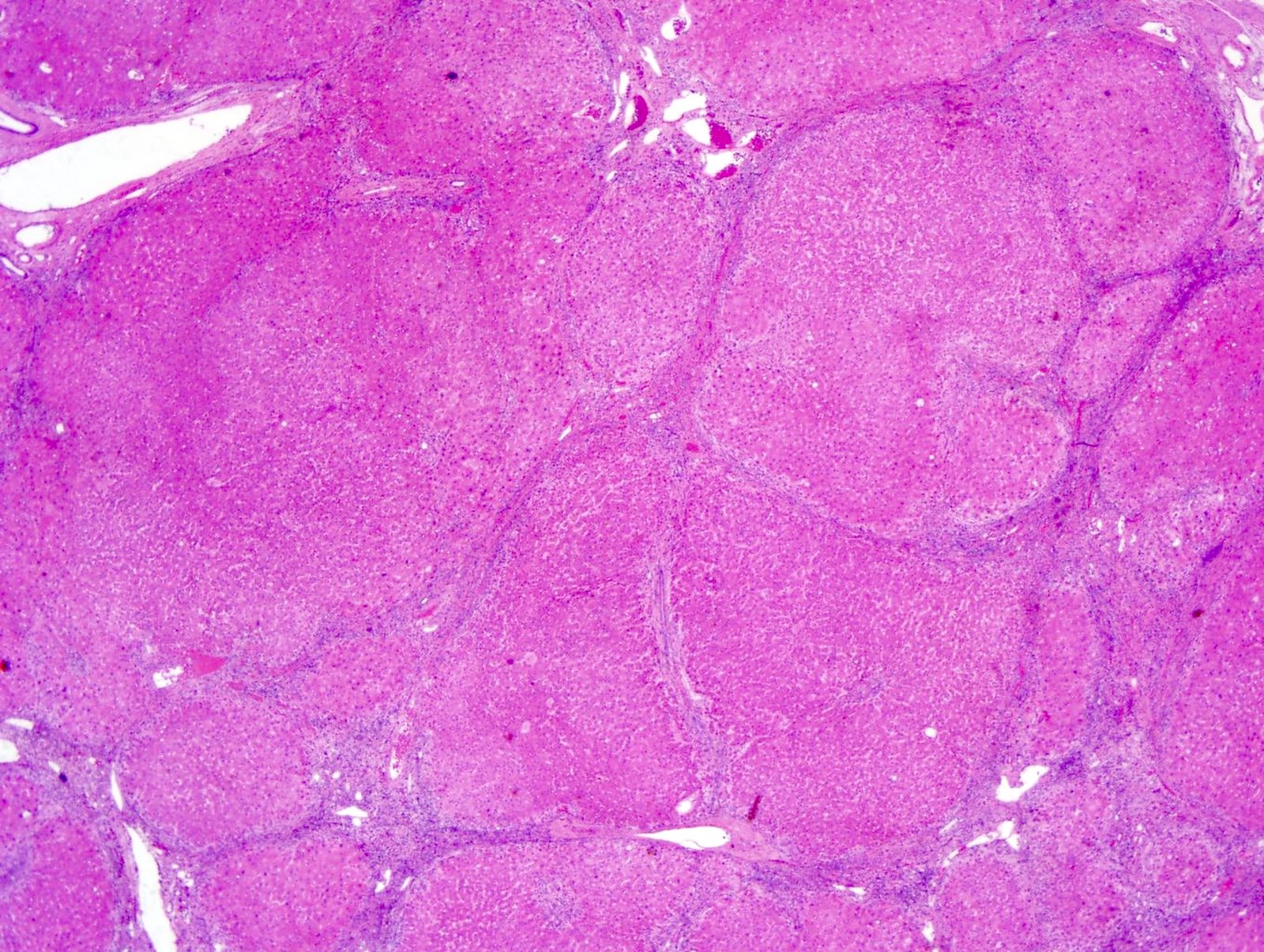
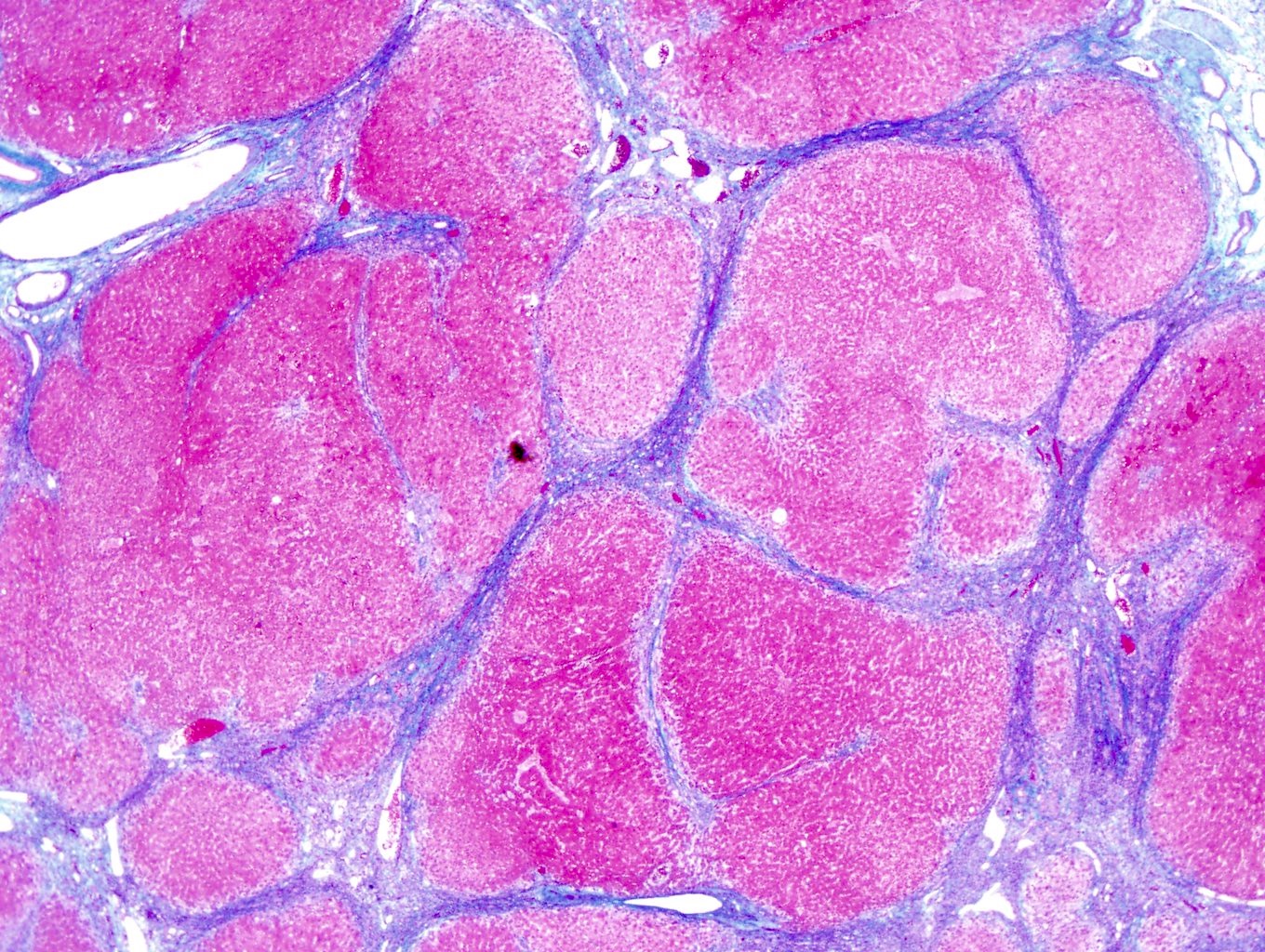
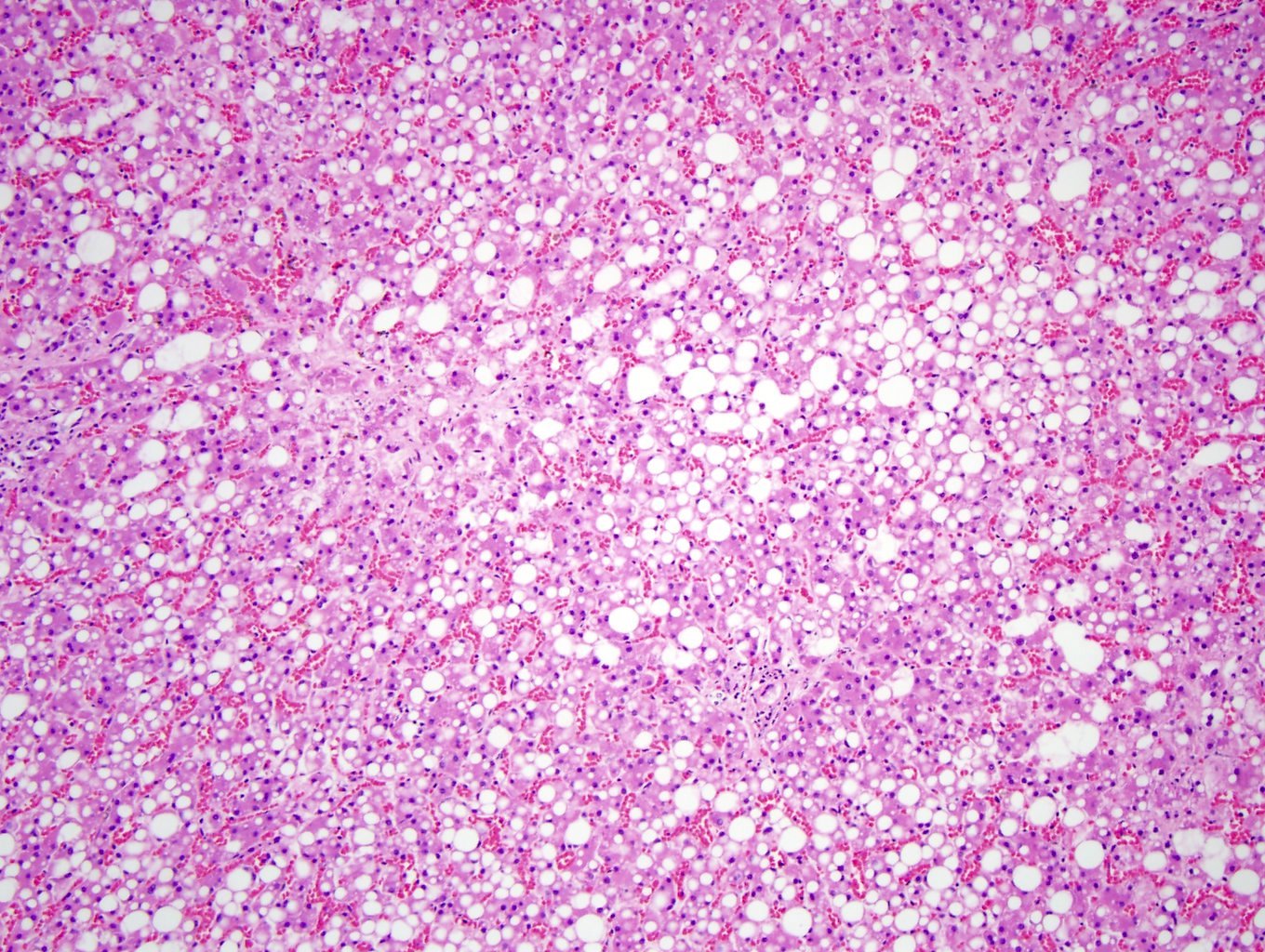
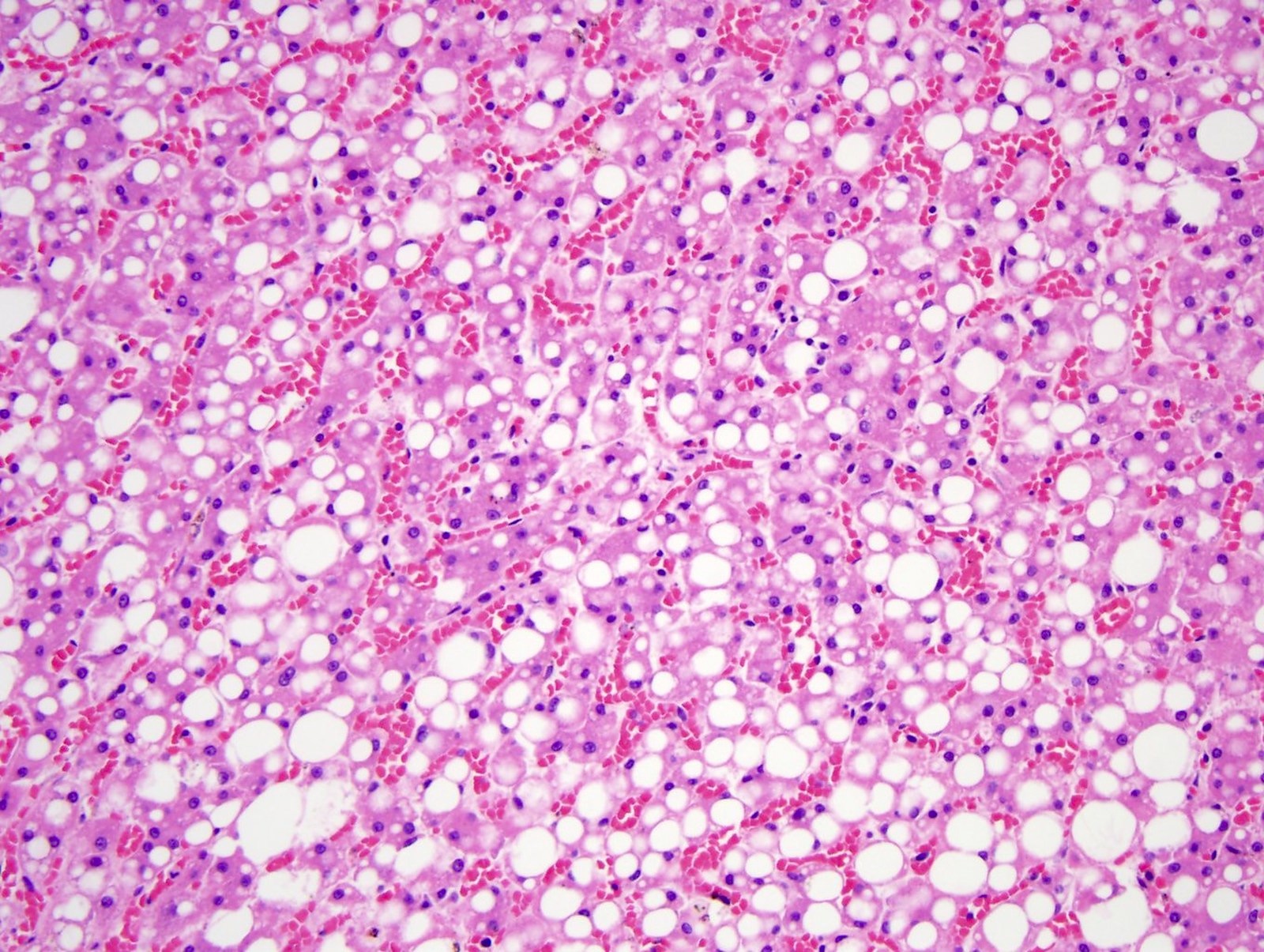
- Liver
- Liver cirrhosis has regenerative nodules of hepatocytes surrounded by fibrous connective tissue that bridges between portal tracts; bridging fibrosis is highlighted by Masson trichrome
- In fatty liver disease, the hepatocytes have a large clear fat vacuole(s) in the cytoplasm pushing the nucleus to an eccentric location, consisting of steatosis
- In acetaminophen toxicity, there is centrilobular hepatic necrosis (zone 3) without acute inflammation (Forensic Pathology Reviews 2008;5:239)
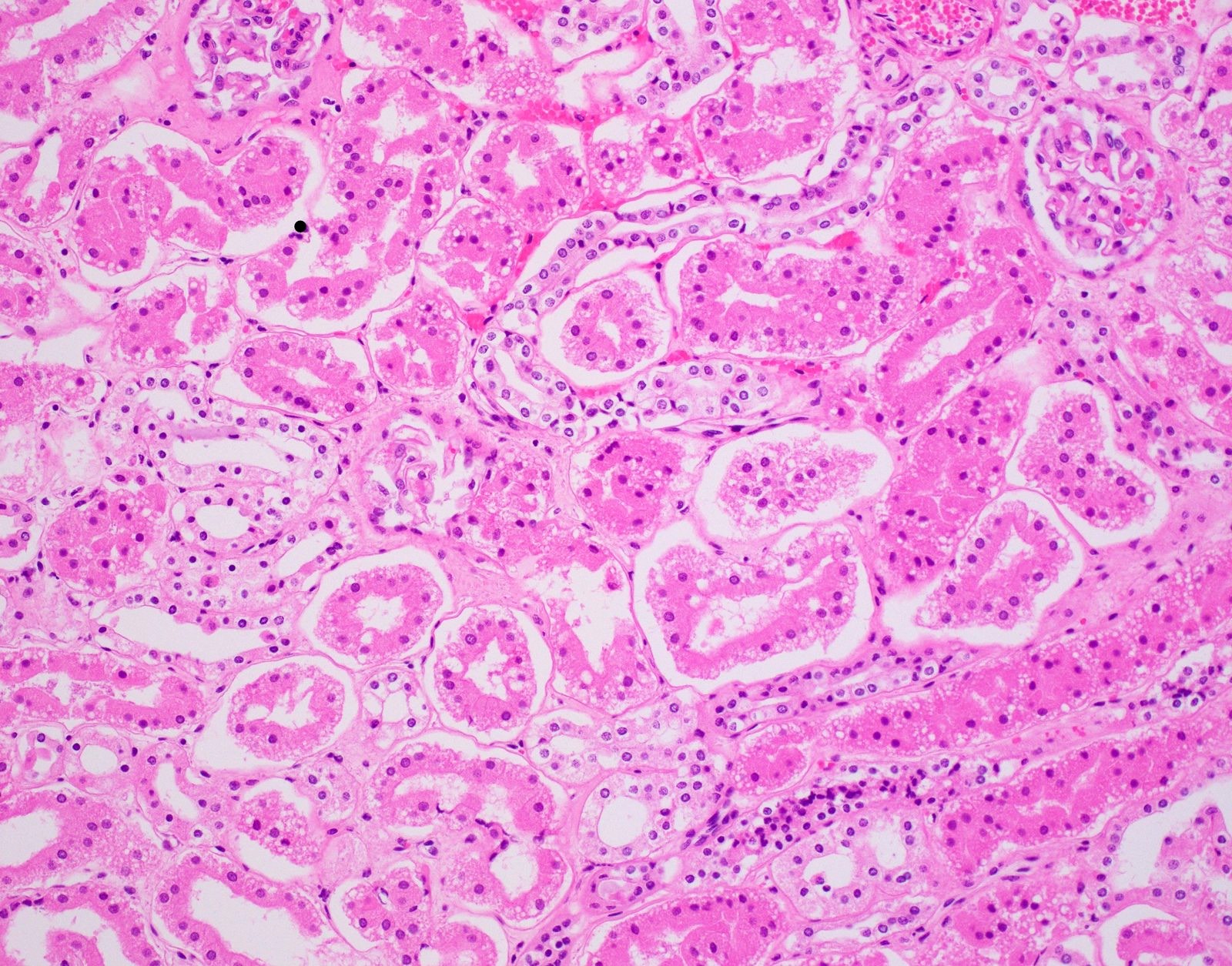
- Renal
- Ethylene glycol toxicity shows polarizable calcium oxalate crystals in degenerated renal tubules (also displays myocardial degeneration, bronchopneumonia and chemical meningoencephalitis) (Forensic Pathology Reviews 2008;5:239)
- Diabetic ketoacidosis (DKA) is supported by renal tubules showing Armanni-Ebstein lesions (PAS positive glycogenated cells) (Acad Forensic Pathol 2018;8:426)
- Brain
- Alzheimer disease shows gliosis and neuronal degeneration
- Bielschowsky silver stain highlights neuritic plaques and fibrillary tangles (Forensic Pathology Reviews 2008;5:239)
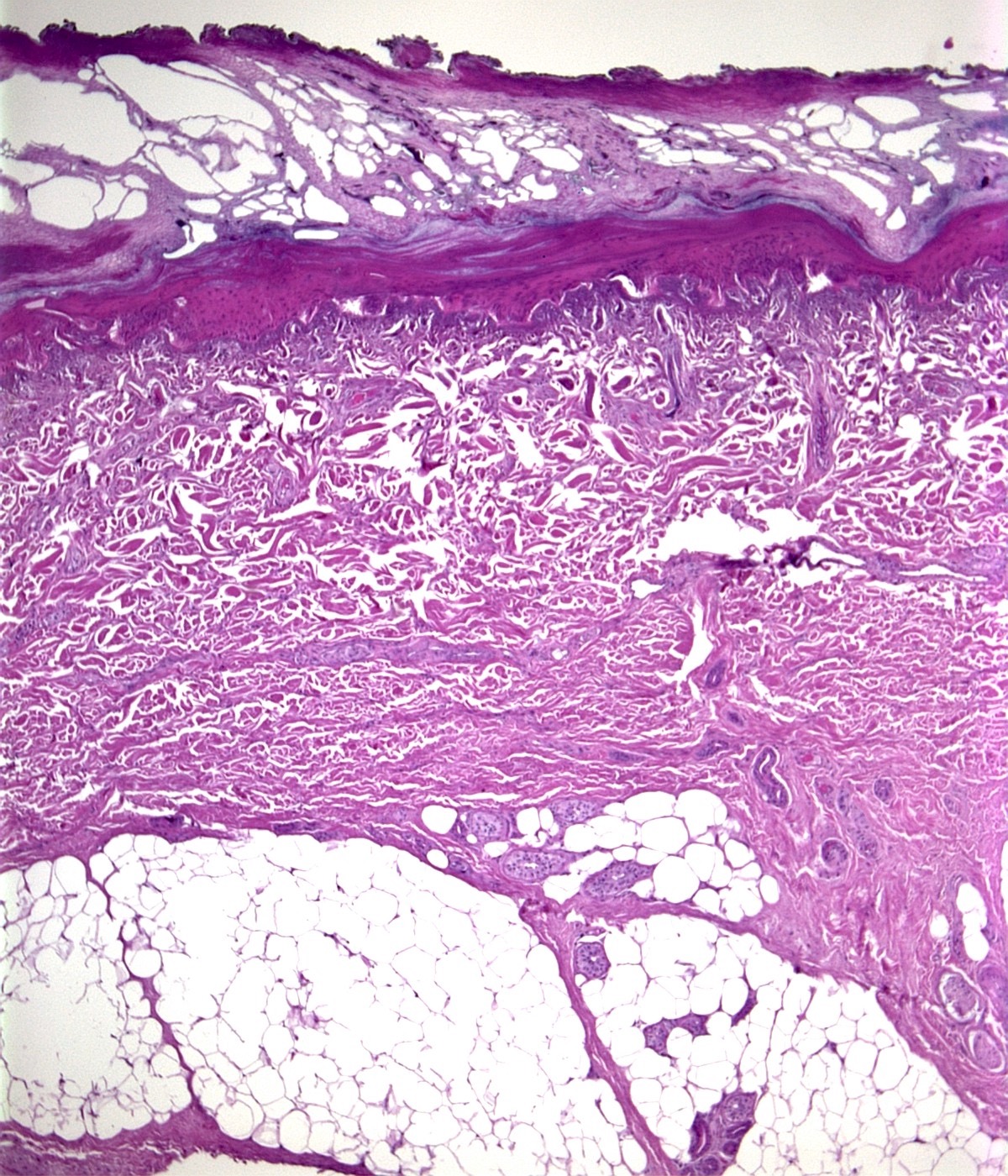
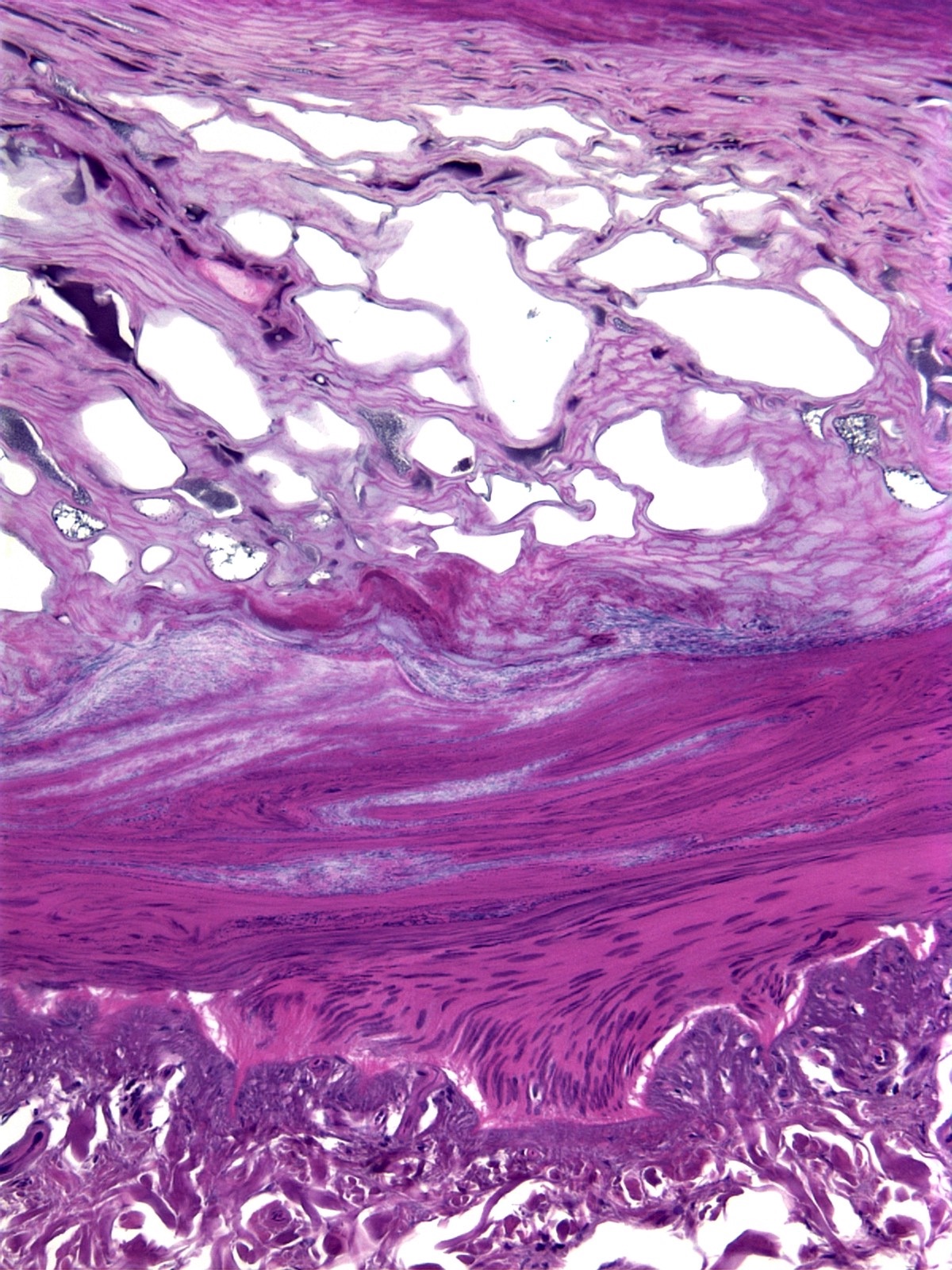
- Skin
- In electrocution, the thermal injury shows epithelial blister and streaming nuclei (Forensic Pathology Reviews 2008;5:239)
- Unknown lesions
- Unknown metastatic lesion (carcinoma, sarcoma, mesothelioma, melanoma or lymphoma) can be identified on histology (Forensic Pathology Reviews 2008;5:239)
Limitations:
- Postmortem enzymatic breakdown of tissue or autolysis can impede histologic diagnosis
- Putrefaction or tissue broken down by postmortem bacteria can impede histologic diagnosis
Essential features:
- Postmortem histology determines or supports COD in:
- Dating a myocardial infarction (> 4 hours = myocyte necrosis with PMNs, > 3 days = hemosiderin laden macrophages and granulation tissue and > 10 days = collagen deposition)
- Acute viral myocarditis (myocardial lymphocytic infiltration)
- Pulmonary embolism (layering of fibrin, platelets, RBCs and acute inflammation)
- Liver cirrhosis (bridging fibrosis highlighted with Masson trichrome)
- Acetaminophen toxicity in the liver has zone 3 necrosis without inflammation
- Diabetic ketoacidosis (Armanni-Ebstein lesions)
- Ethylene glycol toxicity (calcium oxalate crystals in renal tubules)
- Alzheimer disease (Bielschowsky silver stain highlights neuritic plaques and fibrillary tangles)
Contributed by Myra Khan, D.O., Michael Caplan, M.D. and Maria Westerhoff, M.D.
Microbiology
When to use:
How to perform:
Case examples:
Limitations:
Essential features:
Contributed by Michael Caplan, M.D.
- Evidence of infection during autopsy and in all infant deaths
- Routine cultures are taken from the blood, nasal pharynx and lungs; spleen and liver can also be taken
- Tissue samples for microbiology are stored in sterile containers or bottles without additives, refrigerated until transport and sent to the microbiology laboratory 24 - 48 hours after the autopsy (Forensic Sci Med Pathol 2021;17:87)
How to perform:
- Nasal pharyngeal swabs
- Sterile nasopharyngeal swab, 1 for each nostril, is taken before opening the body cavity (Eur J Clin Microbiol Infect Dis 2015;34:1045)
- Swab is inserted until resistance is felt, ensuring the nasopharynx is adequately sampled with respiratory epithelium (N Engl J Med 2020;382:e76)
- Cultures
- When the body cavity is opened and before any dissection, the organ of interest is swabbed with iodine, a deep incision with a sterile blade is made and a sterile swab is taken and placed into a sterile container for cultures
- Cases of bacterial meningitis: sterile swabs of a brain are taken once the cranial cavity is opened
- Cases of sepsis or meningitis: culture spinal fluid
- Cases of endocarditis: culture heart valves
- When the body cavity is opened and before any dissection, the organ of interest is swabbed with iodine, a deep incision with a sterile blade is made and a sterile swab is taken and placed into a sterile container for cultures
- Blood cultures
- Before dissection, heart blood or spinal fluid can be taken by a sterile needle syringe for blood cultures
Case examples:
- Growth of a single microbial isolate is generally considered a true positive (Forensic Sci Med Pathol 2021;17:87)
- Isolation of a pathogenic organism from multiple sites at autopsy likely represents true antemortem bacteremia (Forensic Sci Med Pathol 2021;17:87)
- Growth of multiple endogenous commensal gut bacteria, such as Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa, Enterococcus spp., Clostridia and streptococci, are not pathogenic and considered postmortem bacterial translocation (Forensic Sci Med Pathol 2021;17:87)
- If there is concordance between the microbial growth, patient history, histology and possible imaging, it is reasonable to attribute the microorganism as a causative factor of death; if concordance is lacking, the microbiology findings represent contamination or postmortem bacterial growth (Forensic Sci Med Pathol 2021;17:87)
Limitations:
- Mixed growth represents sample contamination (Forensic Sci Med Pathol 2021;17:87)
- Microbial cultures are subject to postmortem bacterial overgrowth and can be a challenge to interpret
Essential features:
- Growth of a single microbe from multiple sites is consistent with antemortem bacteremia, along with concordance of patient history, histology or imaging
- Mixed microbial growth, especially of endogenous gut bacteria, supports postmortem bacterial overgrowth or contamination
Contributed by Michael Caplan, M.D.
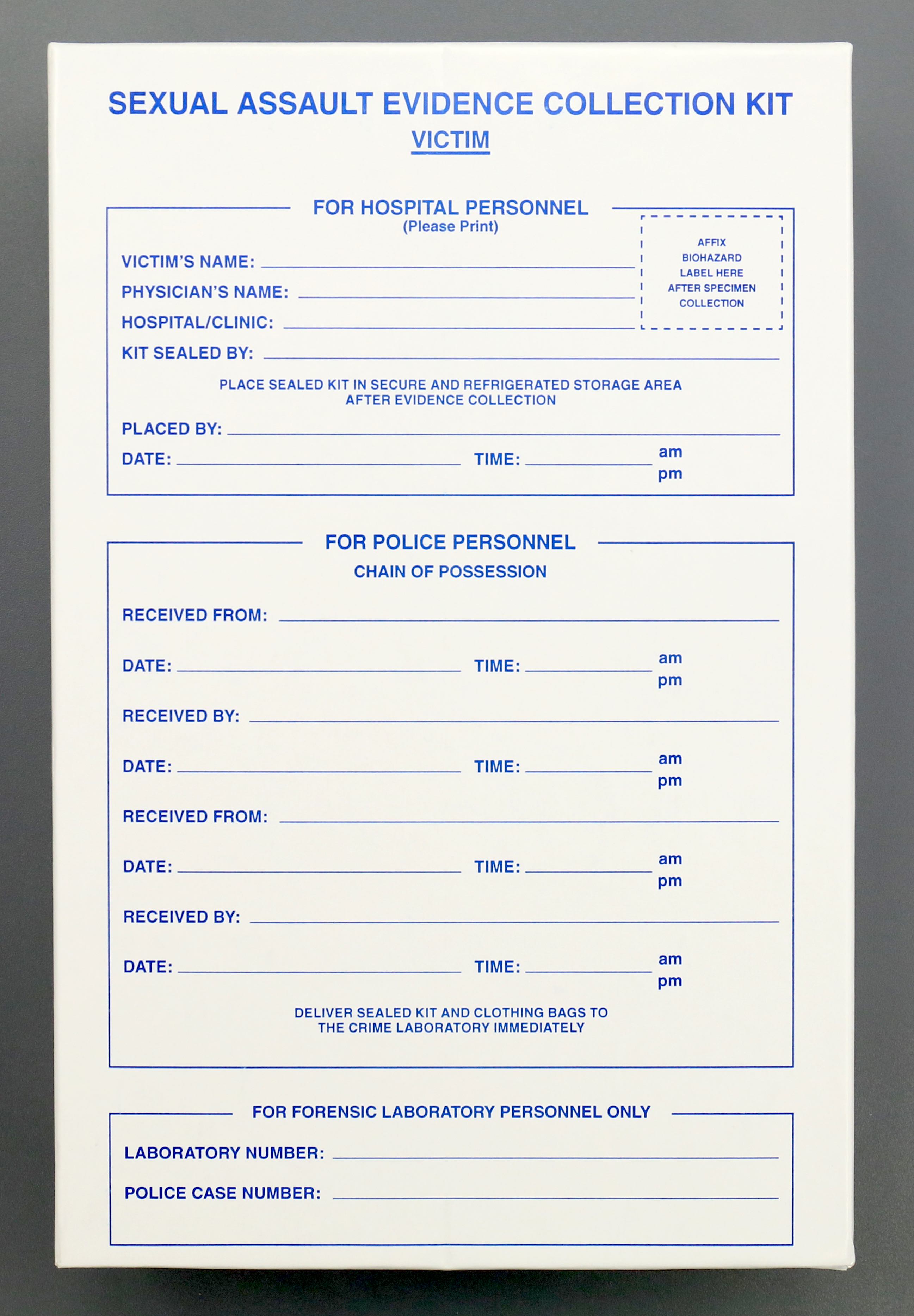
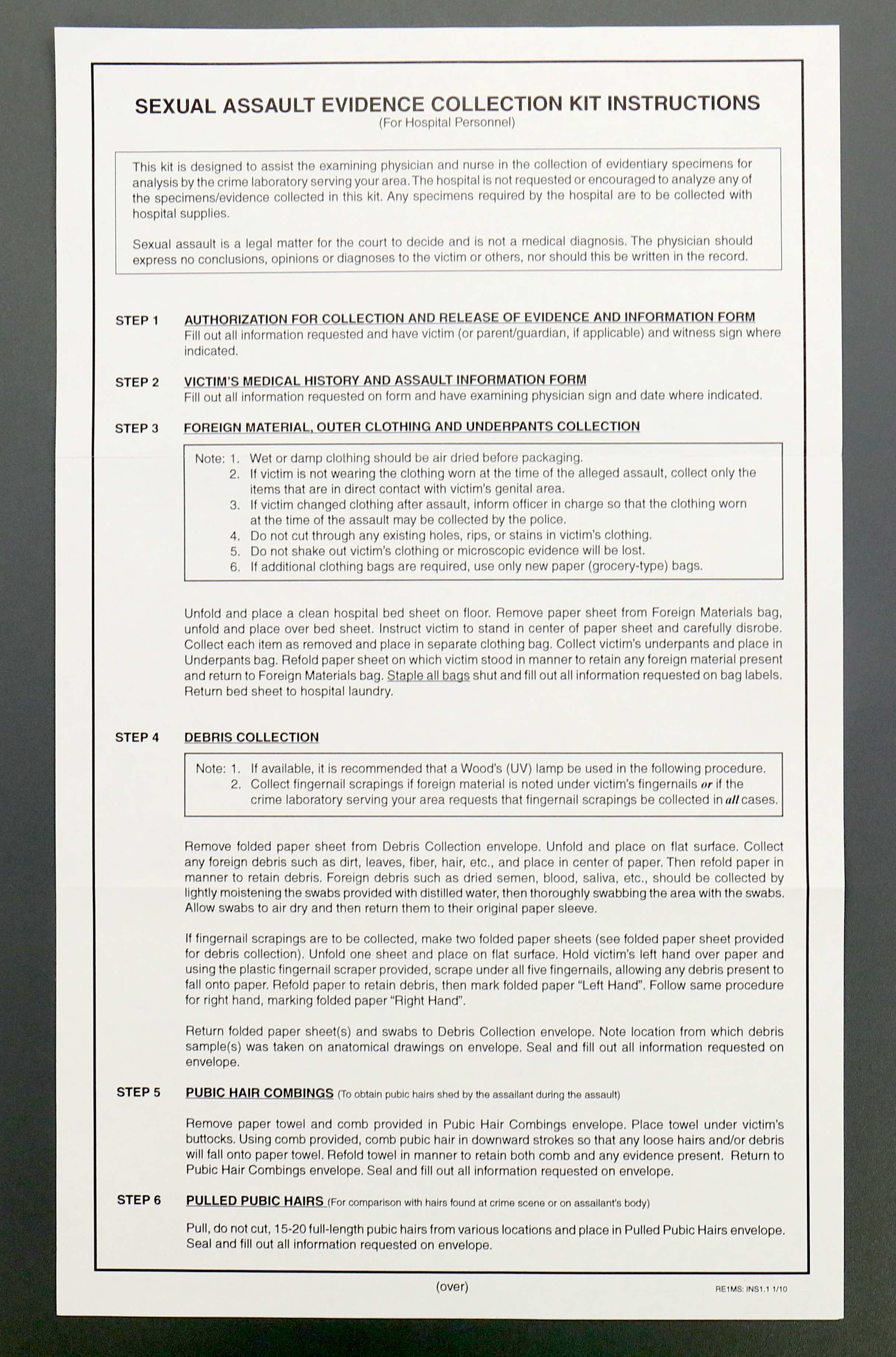
Sexual assault kit
When to use:
How to perform:
Results:
Limitations:
Essential features:
Contributed by Myra Khan, D.O.
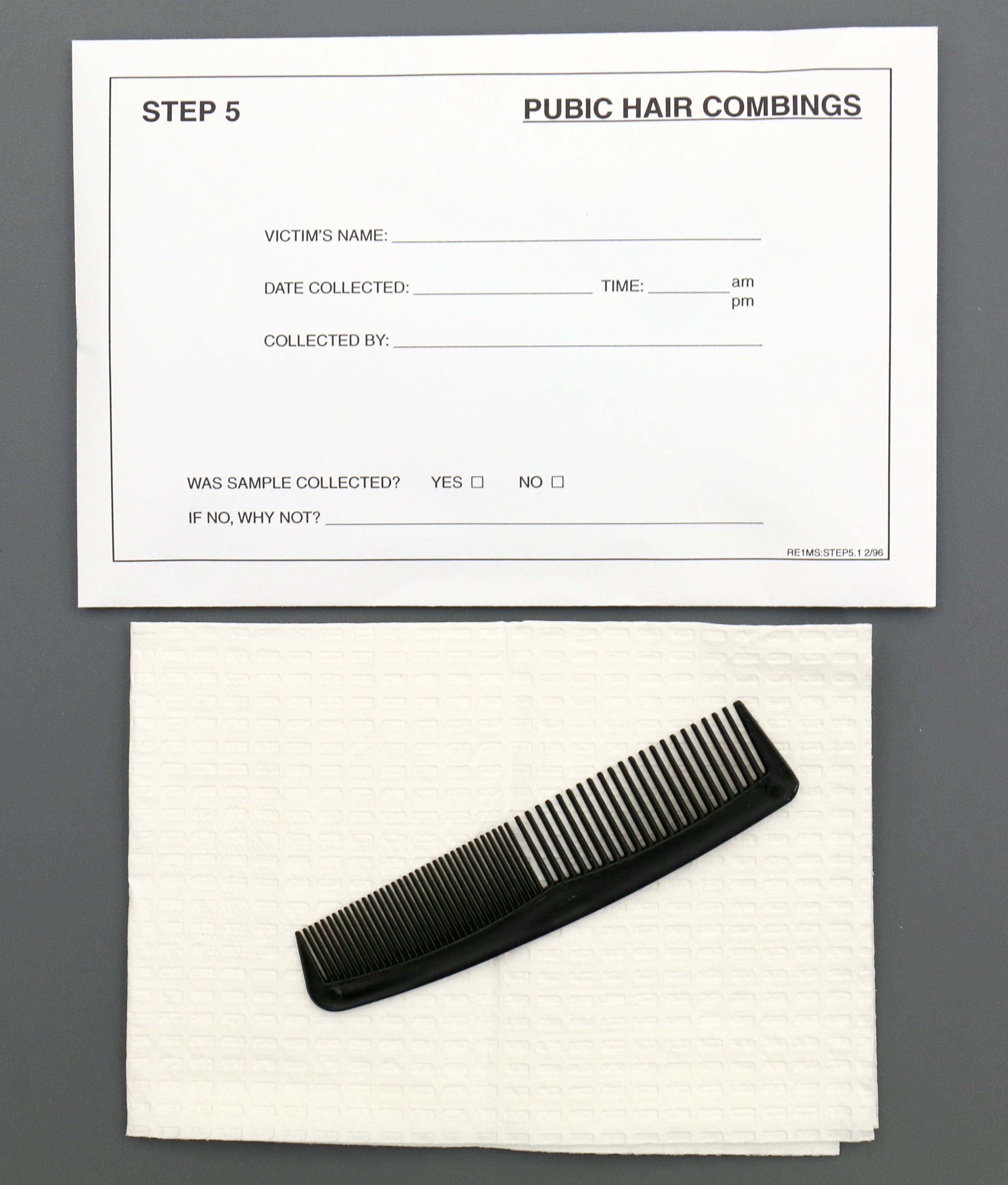
- All cases of sexual assault or suspected sexual assault, physical assault, strangulation, prostitution, if a decedent is found in a compromising position and physical trauma is identified in the genitalia at autopsy
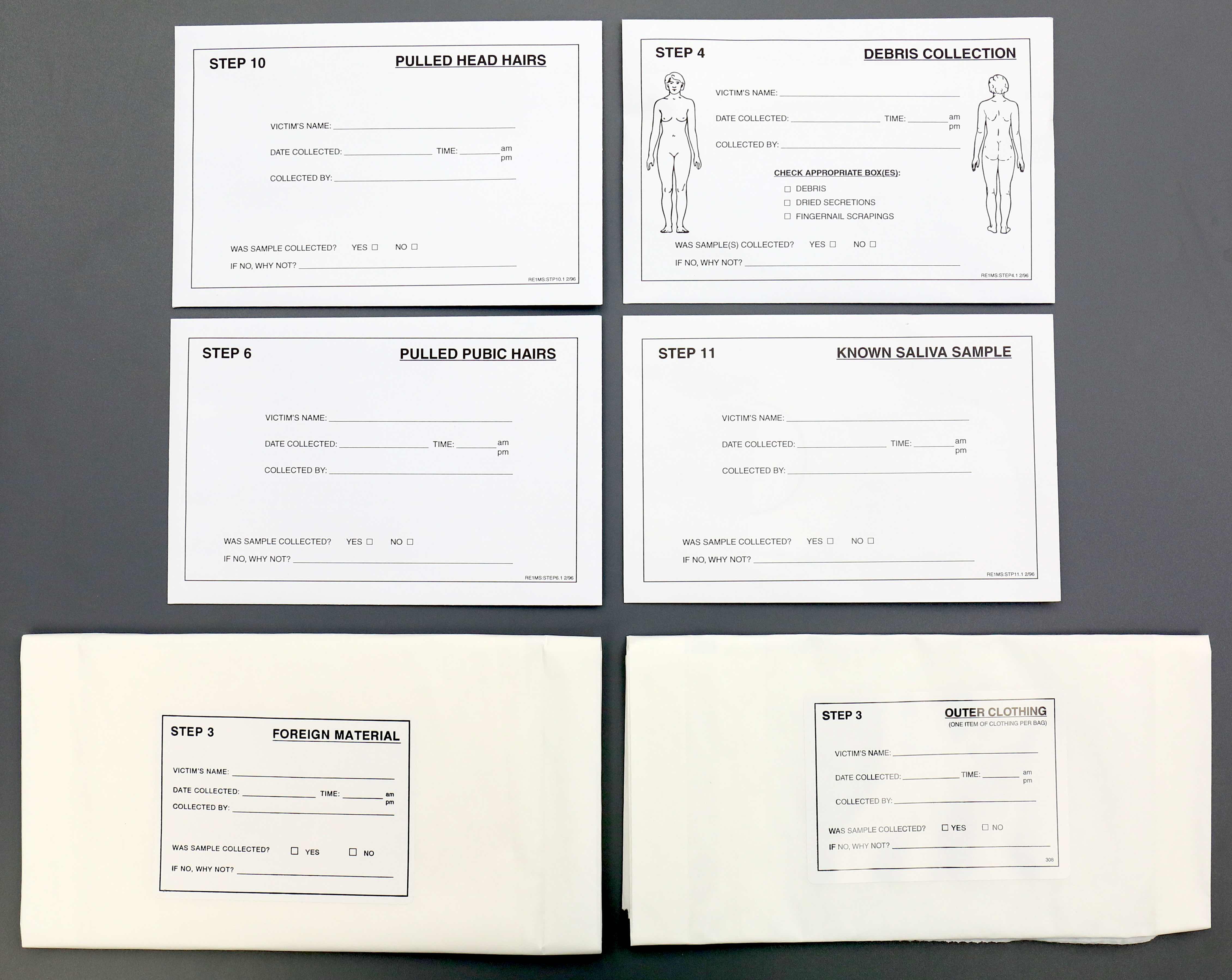
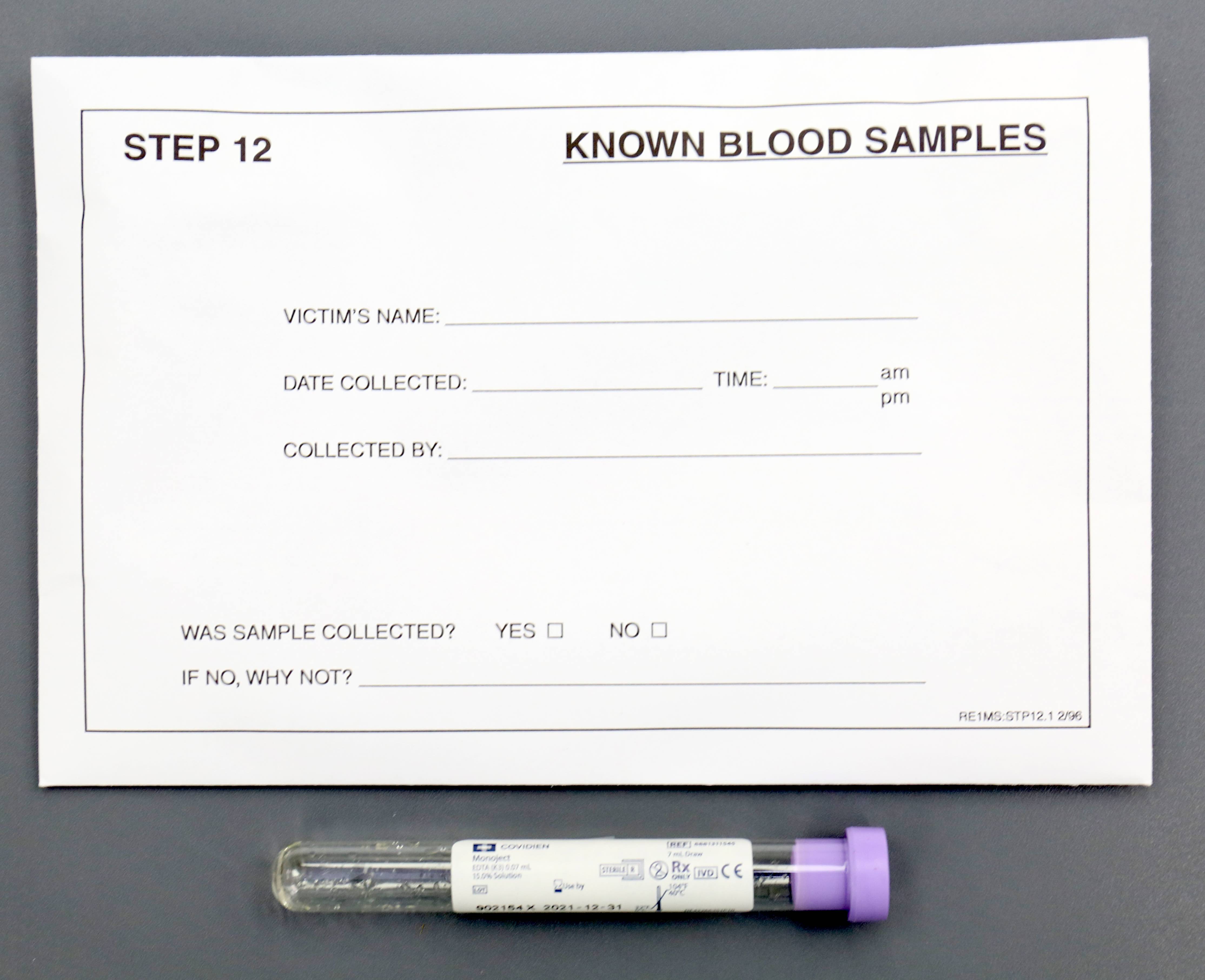
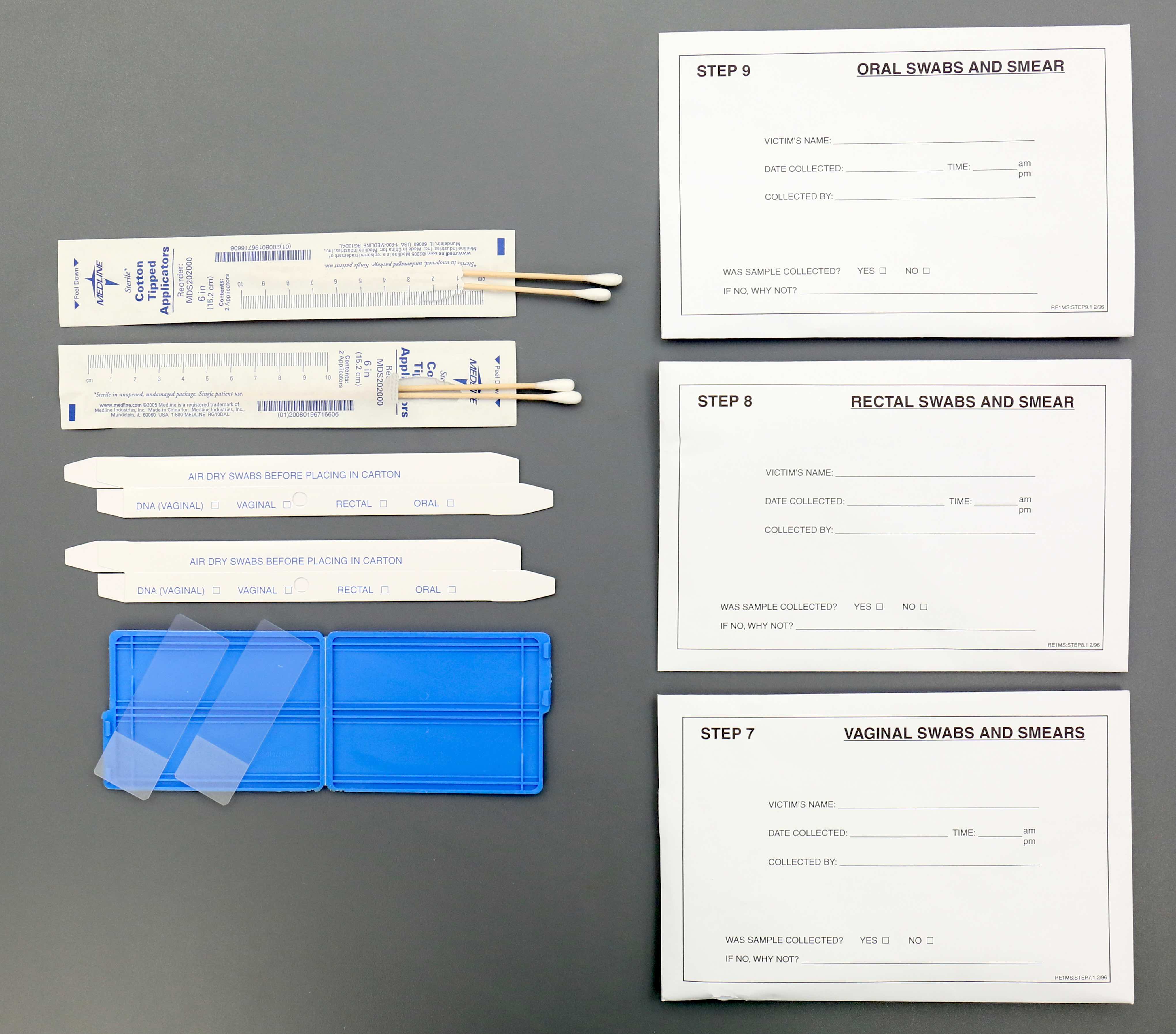
How to perform:
- Use a sexual assault kit that contains sterile saline, cotton tip swabs, a speculum, an anoscope, glass slides, envelopes, combs, self sealing bags and a white bedsheet
- Cotton tip swabs to collect DNA are first wet with sterile saline and 2 sets are swabbed to any area of the body (bite marks, breasts and around the neck); start from the top of the body and move down, air dry the swabs and place in the correctly labeled envelope
- Cervix, anal and rectal swabs are taken before vaginal swabs because fluid from the vagina drips down
- Speculum is inserted into the vagina to visualize the cervix and is swabbed
- Vaginal and cervical swabs are smeared on glass slides to visualize sperm; sperm can be recovered from the body days after death
- Anoscope is used to visualize the anus for trauma and swabbed
- Pubic and scalp hair is combed and pulled in different areas and each is placed in separate envelopes (labeled "pulled hair" and "combed hair"); combing allows the collection of foreign hairs and fibers
- Self sealing bags are used to collect and preserve evidence, like any clothing
- White bedsheet goes under the body to catch any missed evidence
Results:
- Swabs and other evidence collected are used for DNA analysis
- Even if no sperm are identified, chemical tests, like acid phosphatase, can be positive in absence of sperm (J Forensic Leg Med 2013;20:578)
Limitations:
- Decedent's body that is washed before the autopsy inhibits collection
- Improper order of evidence collection at autopsy
Essential features:
- Do not wash the body before evidence collection
- Take swabs of the cervix, anus and rectum because fluid from the vagina drips down the perineum and can contaminate results
- Vaginal and cervical slides can be made to look for sperm
- Comb and pull pubic and scalp hair in various locations and put it into separate envelopes to collect foreign hairs and fibers
Contributed by Myra Khan, D.O.
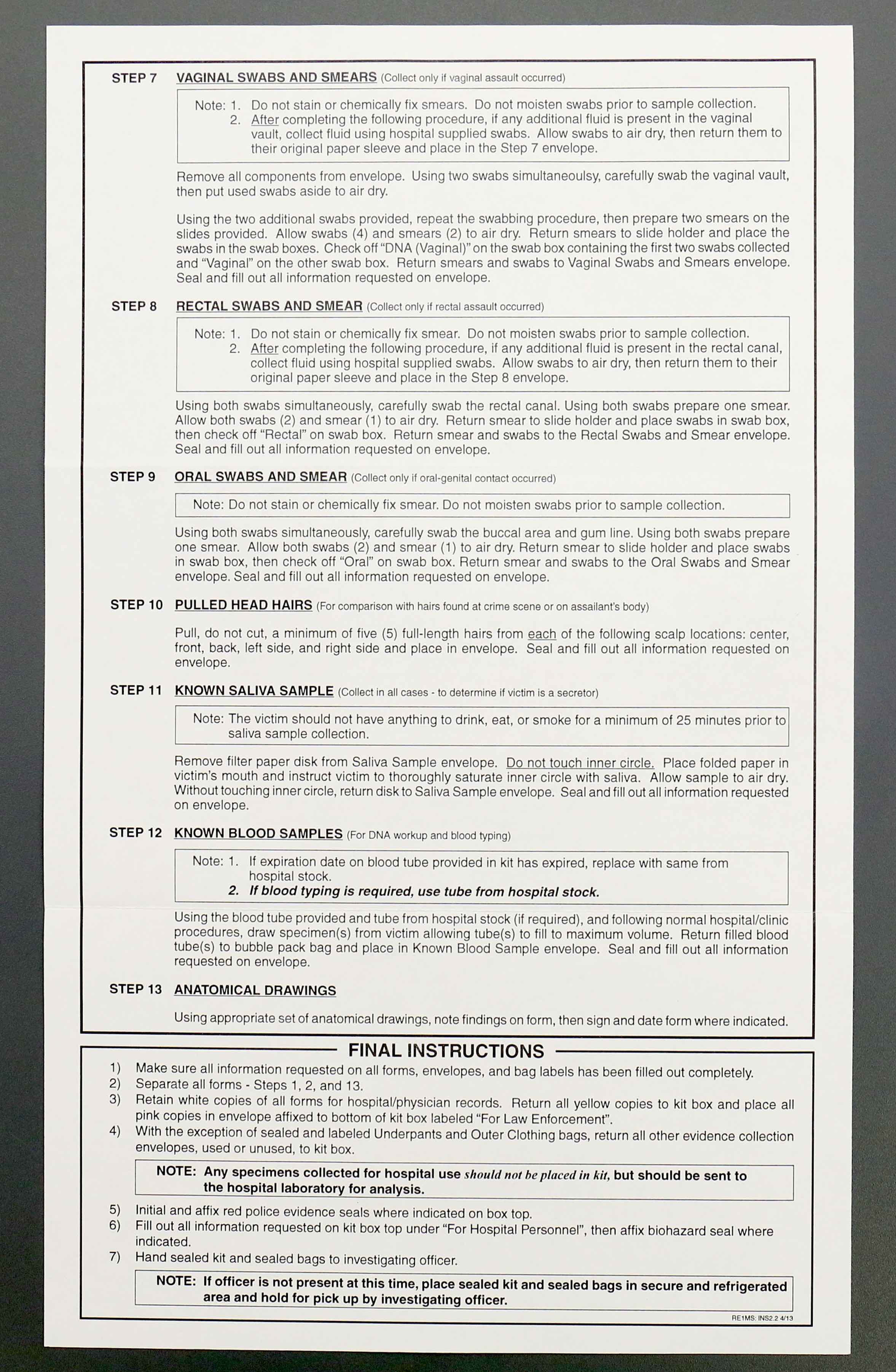
DNA
When to use:
Specimens:
Methods:
How to interpret:
Limitations:
Essential features:
Contributed by Myra Khan, D.O.
- To identify decedents, suspected cases of sexual assault, physical assault in which DNA could have been transferred between individuals and paternity testing
Specimens:
- Any tissue with nucleated cells, commonly semen and blood but also the follicle in pulled hair, saliva in bite marks, fingernail clippings and skeletal muscle
- In advanced decomposition, teeth, ribs and femurs are sufficient
- Blood preserved on DNA spot cards
Methods:
- PCR:
- Amplifies short DNA sequences of specific alleles (Exp Mol Med 2001;33:101)
- Advantages: simple, short turnaround time and analyzes very small amounts of DNA (0.1 to 1.0 ng)
- Disadvantages: susceptible to contamination and PCR loci have few alleles it will recognize
- Short tandem repeats (STR):
- PCR used to identify DNA with high discriminatory power
- STR loci are repeating sequences of 2 - 6 base pairs that occur every 1 in 10,000 nucleotides and are unique to each individual
- In the U.S., 13 STR loci are used and the average random match probability is rarer than 1 in a trillion among unrelated people (Am J Hum Genet 1994;55:175)
- Advantages: rapid and need small amount of DNA (like wiping from a full metal jacket penetrating a body)
- Mitochondrial DNA (mtDNA):
- Found in the cytoplasm and inherited maternally
- Siblings and maternal relatives have identical mtDNA
- Only used when biological material to be analyzed is scant or degraded (Cells 2019;8:100)
How to interpret:
- Insufficient amount of DNA means the specimen is inadequate in size, degraded or contaminated
- DNA profiles match, which can mean:
- Samples are from the same person
- Error in collection or at the lab occurred and the samples actually came from different people
- 2 individuals have the same DNA profile, such as identical twins
- Not enough tests were performed to differentiate between the 2 samples
- Different DNA profiles mean the DNA does not match the test subject
Limitations:
- In completely skeletonized decedent remains, it is challenging to collect adequate amounts of DNA
Essential features:
- DNA is collected at autopsy in the form of semen and blood
- Techniques for DNA identification are PCR, STR and mtDNA
- Even if DNA profiles match, caution should be maintained, as there may have been an error in collection or not enough tests performed to differentiate between the 2 samples
Contributed by Myra Khan, D.O.
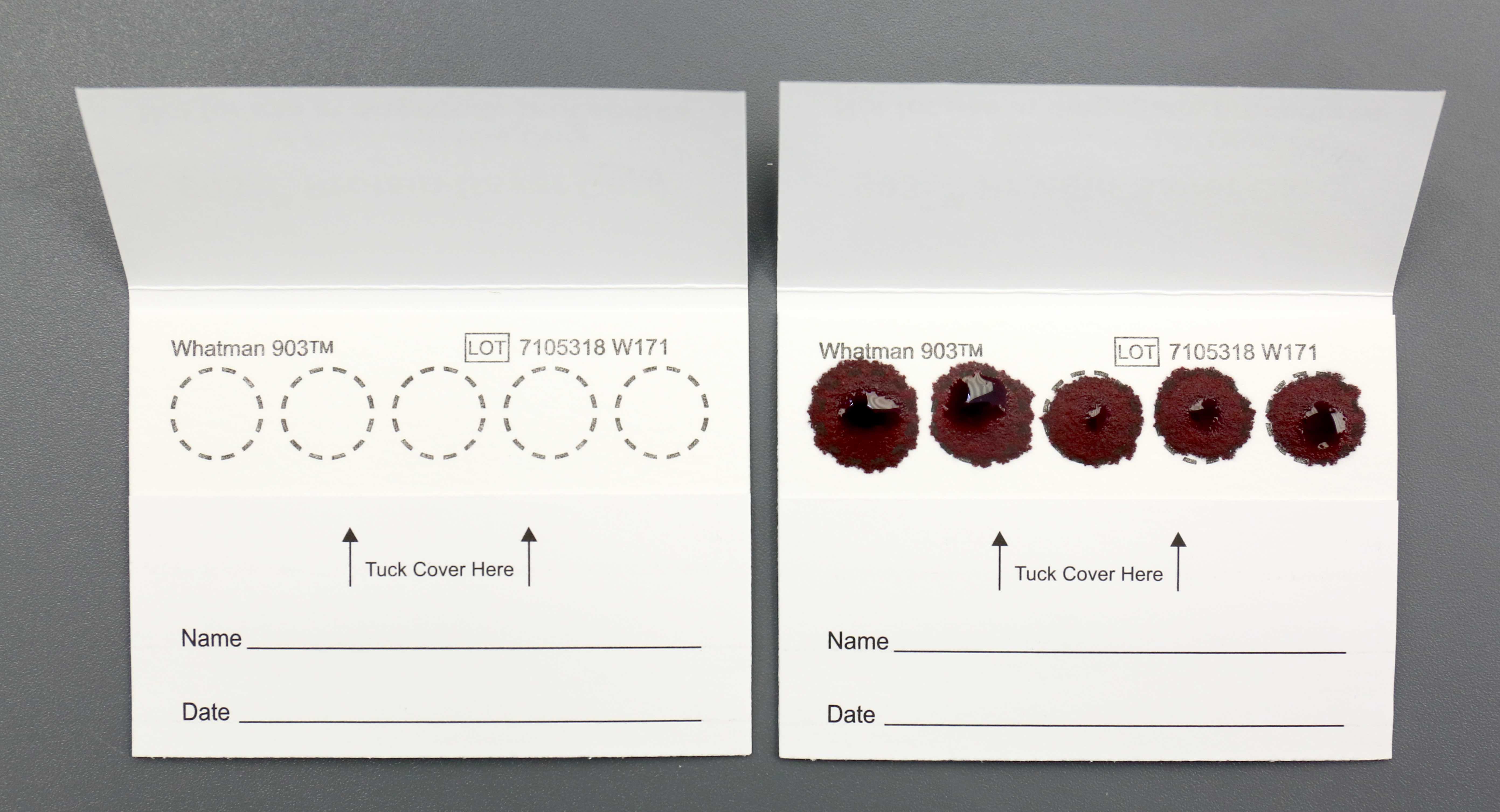
Board review style question #1
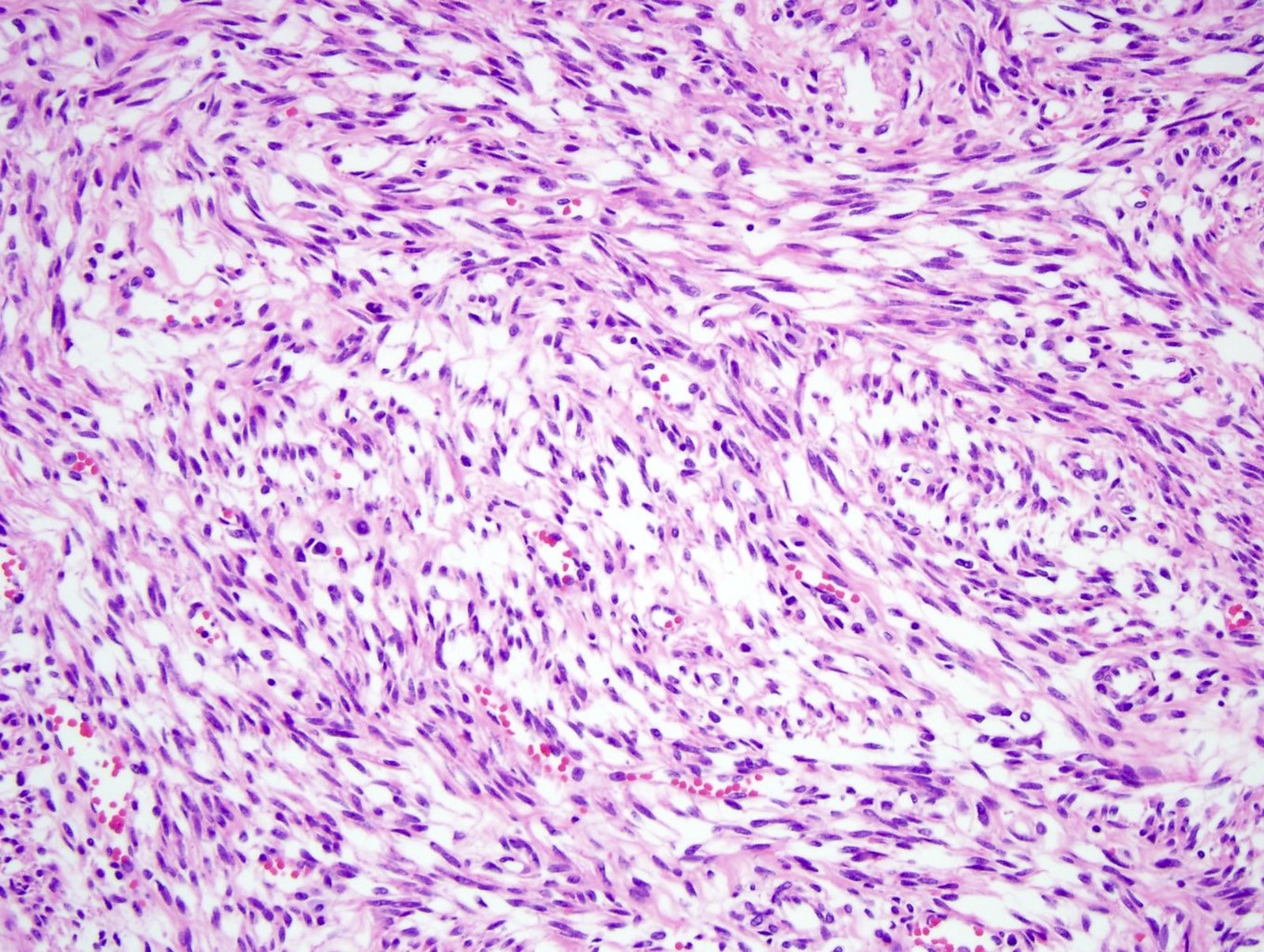
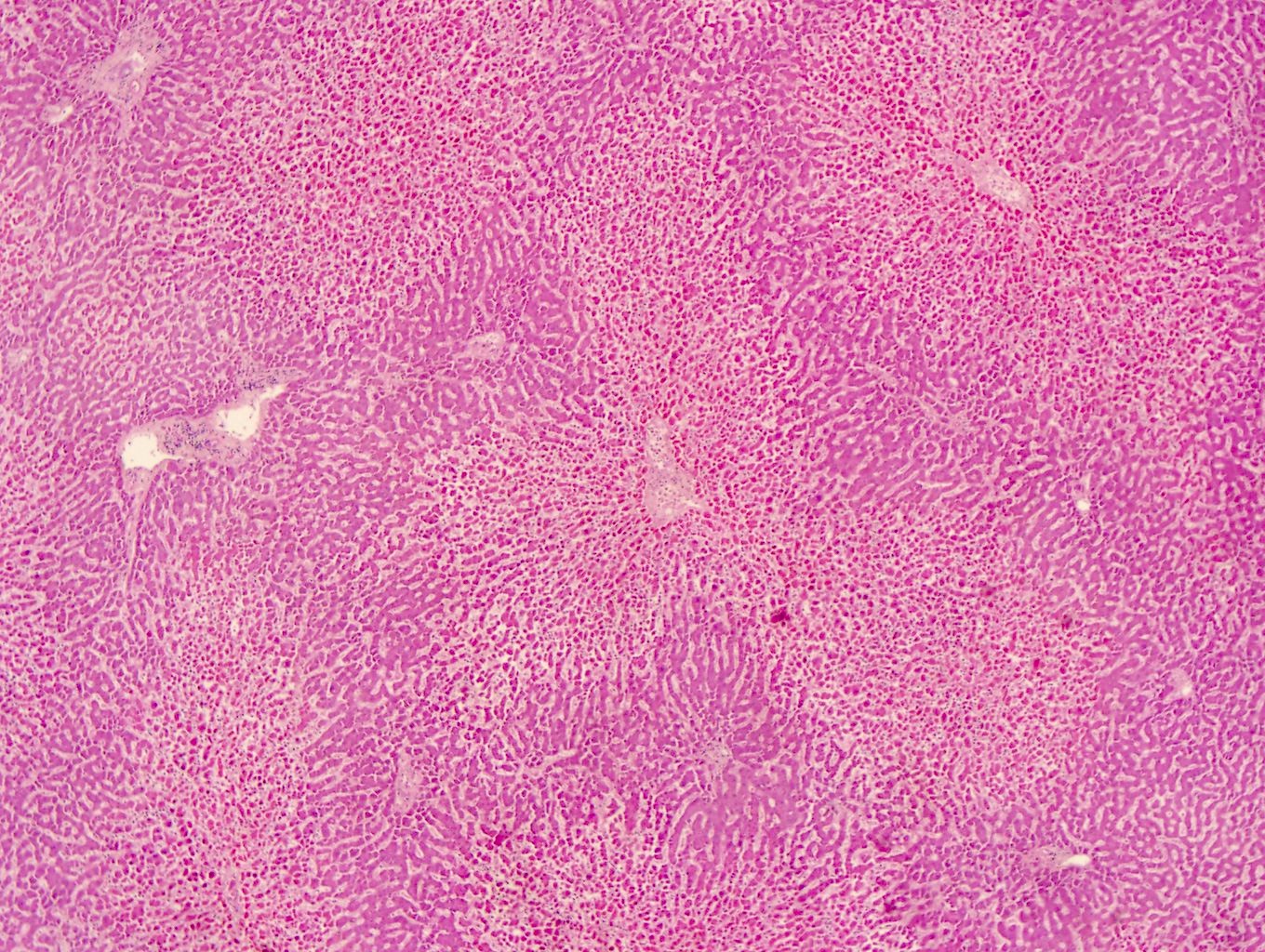
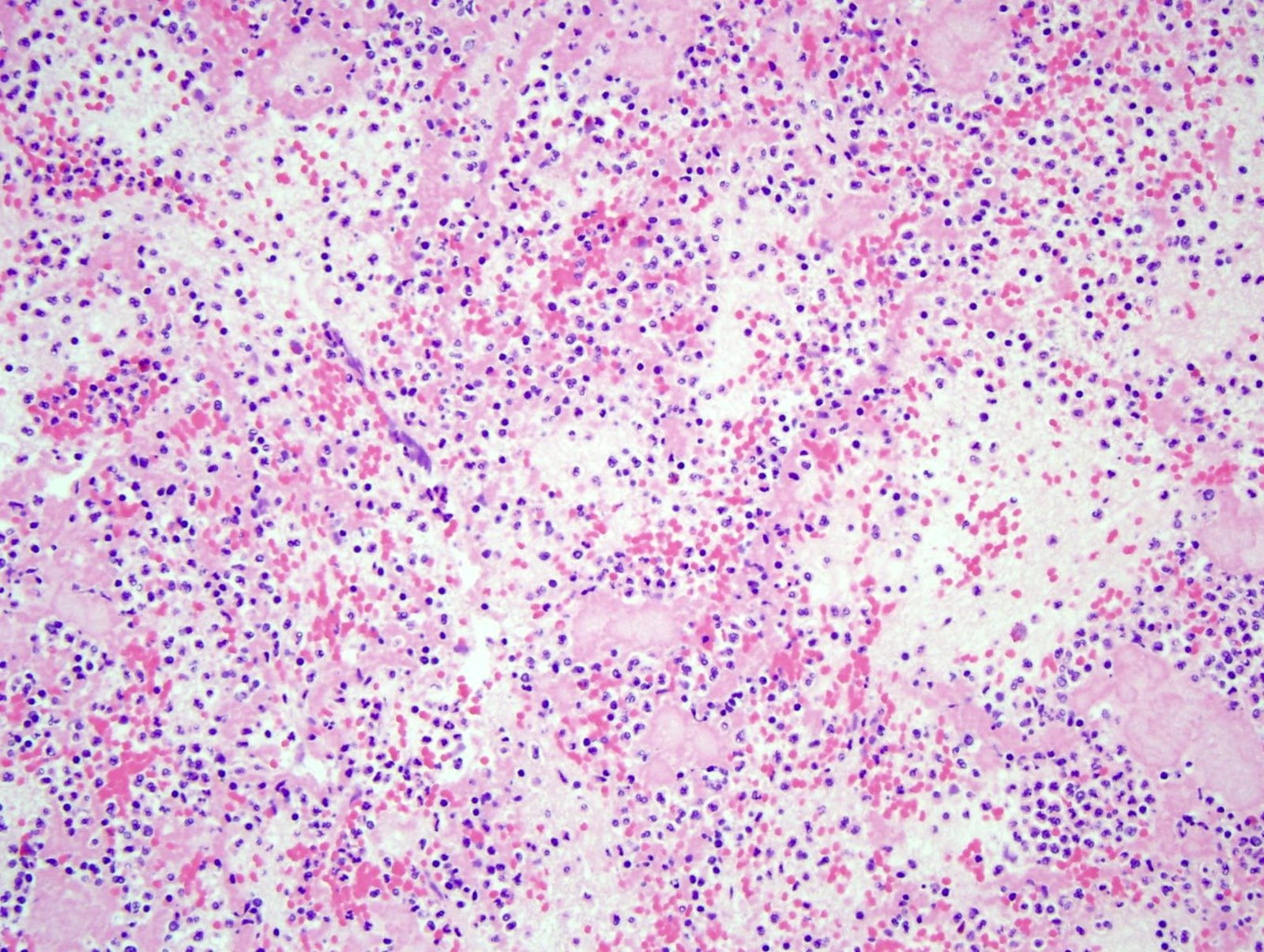
A 55 year old woman presents to the emergency room with chest pain and is diagnosed with a myocardial infarction. Despite medical intervention, she dies and an autopsy is performed. Based on the histological image of the myocardium, what is the age of the myocardial infarct?
- Acute myocardial infarct
- Between a subacute and chronic / remote myocardial infarction
- Chronic / remote myocardial infarct
- Subacute myocardial infarct
Board review style answer #1
Board review style question #2
A 65 year old alcoholic man is found dead on the sidewalk. At autopsy, a purulent abscess is identified in his right middle lung lobe and sterile cultures of the lung are taken. The cultures grow Klebsiella pneumoniae and the histological exam of the lungs is significant for acute pneumonia. Toxicology did not detect drugs of abuse. No other significant natural disease is identified. What is the cause of death?
- Acute alcohol intoxication
- Acute on chronic alcoholism
- Acute pneumonia
- Chronic alcoholism
Board review style answer #2