Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Pezhouh MK, Heyraty MP. Granulomatous appendicitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/appendixidiopathicgran.html. Accessed December 22nd, 2024.
Definition / general
- Granulomatous inflammation of appendix
Essential features
- Granulomatous inflammation of appendix
- Clinically resembles acute appendicitis
- Does not recur after appendectomy
Terminology
- Granulomatous appendicitis
ICD coding
- ICD-10
- K36 - other appendicitis
- K37 - unspecified appendicitis
- K35.8 - other and unspecified acute appendicitis
- K35.80 - unspecified acute appendicitis
- K35.89 - other acute appendicitis
- K35.890 - other acute appendicitis without perforation or gangrene
- K35.891 - other acute appendicitis without perforation, with gangrene
Epidemiology
- Identified in 0.1 - 2% of appendectomies; depends on geographical distribution of underlying disease (Clin Case Rep 2021;9:e05074)
Sites
- Appendix
Pathophysiology
- Granulomatous inflammation of the appendix, due to variety of etiologies, leads to an acute or subacute increase in intraluminal and intramural pressure and acute or subacute inflammatory processes
Etiology
- Idiopathic granulomatous appendicitis is rare and is a diagnosis of exclusion
- Secondary granulomatous appendicitis can be due to infectious etiologies such as Yersinia, tuberculosis, fungal and parasitic infection and noninfectious etiologies such as interval appendicitis, Crohn's disease, sarcoidosis or other granulomatous disease (Int J Surg Pathol 2010;18:14)
Clinical features
- Main symptom is acute or subacute abdominal pain
- Other symptoms include fever, anorexia, vomiting, diarrhea and malaise
- On physical examination, tenderness and rebound tenderness can be seen
- Similar to acute appendicitis (Surgeon 2003;1:286)
Diagnosis
- Definite diagnosis is based on histological examination and special stains; serologic test, tissue microbial culture and PCR are sometimes necessary for diagnosis of underlying disease
Radiology description
- Nonspecific, enlarged appendix, thickened appendicular wall, presence of right lower quadrant fat stranding surrounding the appendix and enlarged mesenteric lymph nodes (Abdom Imaging 2003;28:280, J Clin Imaging Sci 2012;2:73)
Case reports
- 17 year old boy with nausea and right lower quadrant abdominal pain (Clin Case Rep 2021;9:e05074)
- 20 year old diabetic man with a 3 day history of right lower quadrant abdominal pain associated with fever, vomiting and anorexia (Cureus 2022;14:e23247)
- 24 year man presented with acute abdominal pain localized in the right iliac fossa with rebound tenderness for 24 hours (BMJ Case Rep 2020;13:e238955)
- 26 year old woman presented with persistent right lower abdominal pain and mass on computed tomography (CT) scan suggesting an inflammatory tumor around appendix (Surg Today 2007;37:690)
- 28 year old man with Crohn's disease presenting as granulomatous appendicitis (Case Rep Gastroenterol 2019;13:398)
Treatment
- Dependent on the etiology of granulomatous appendicitis
Gross description
- Appendix can be normal appearing or show erythema, perforation, abscess formation or thick wall appearance
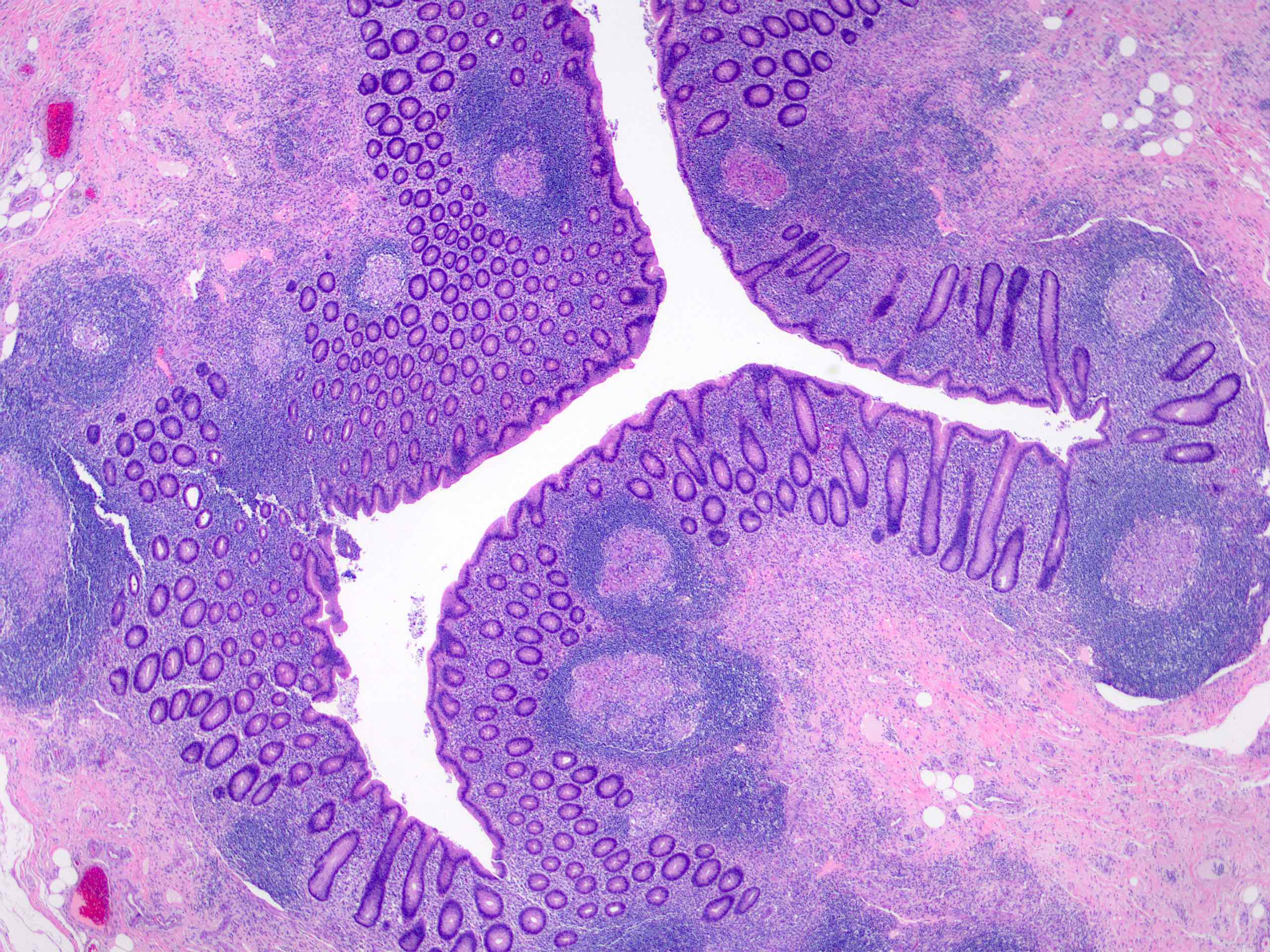
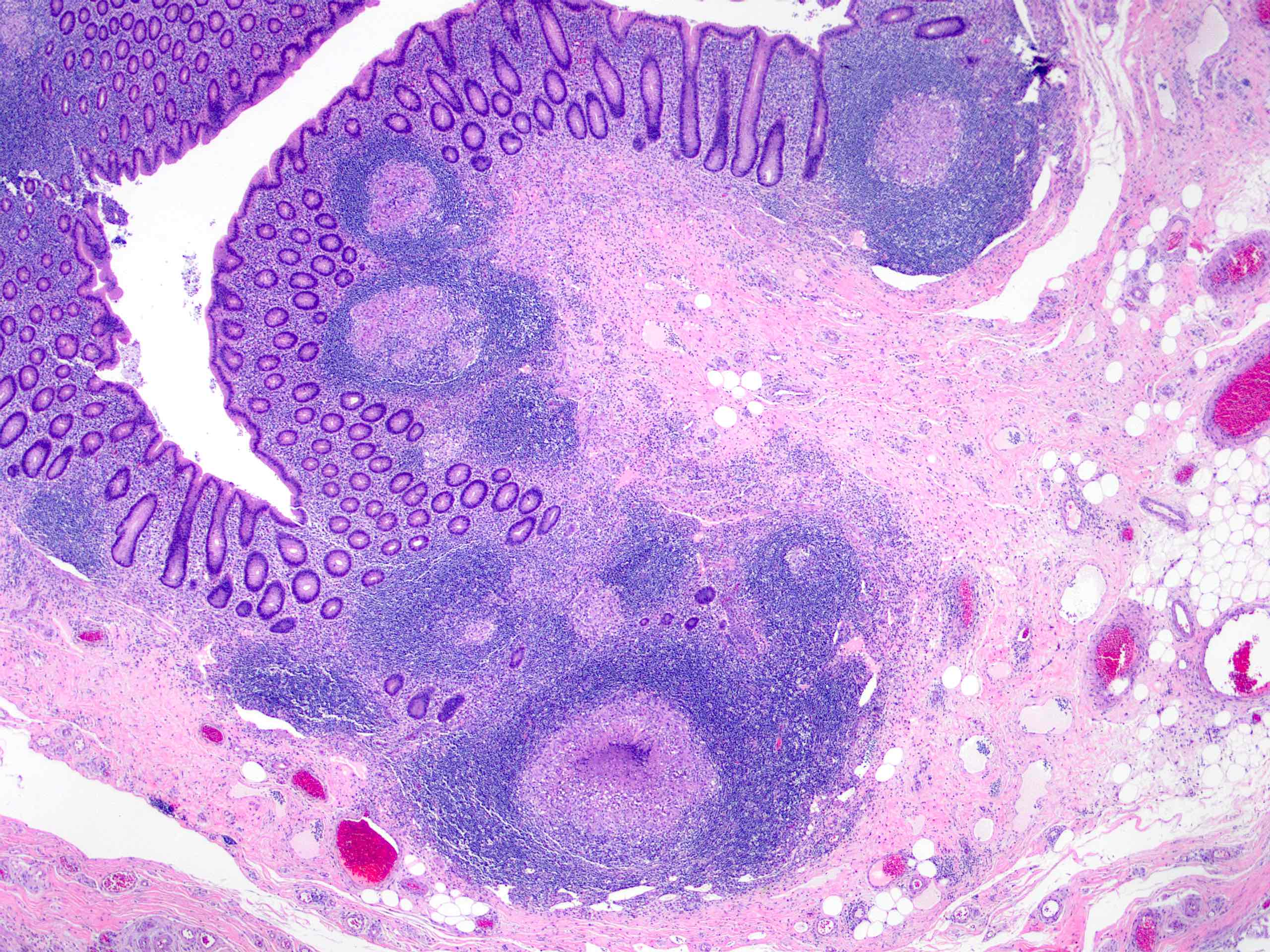
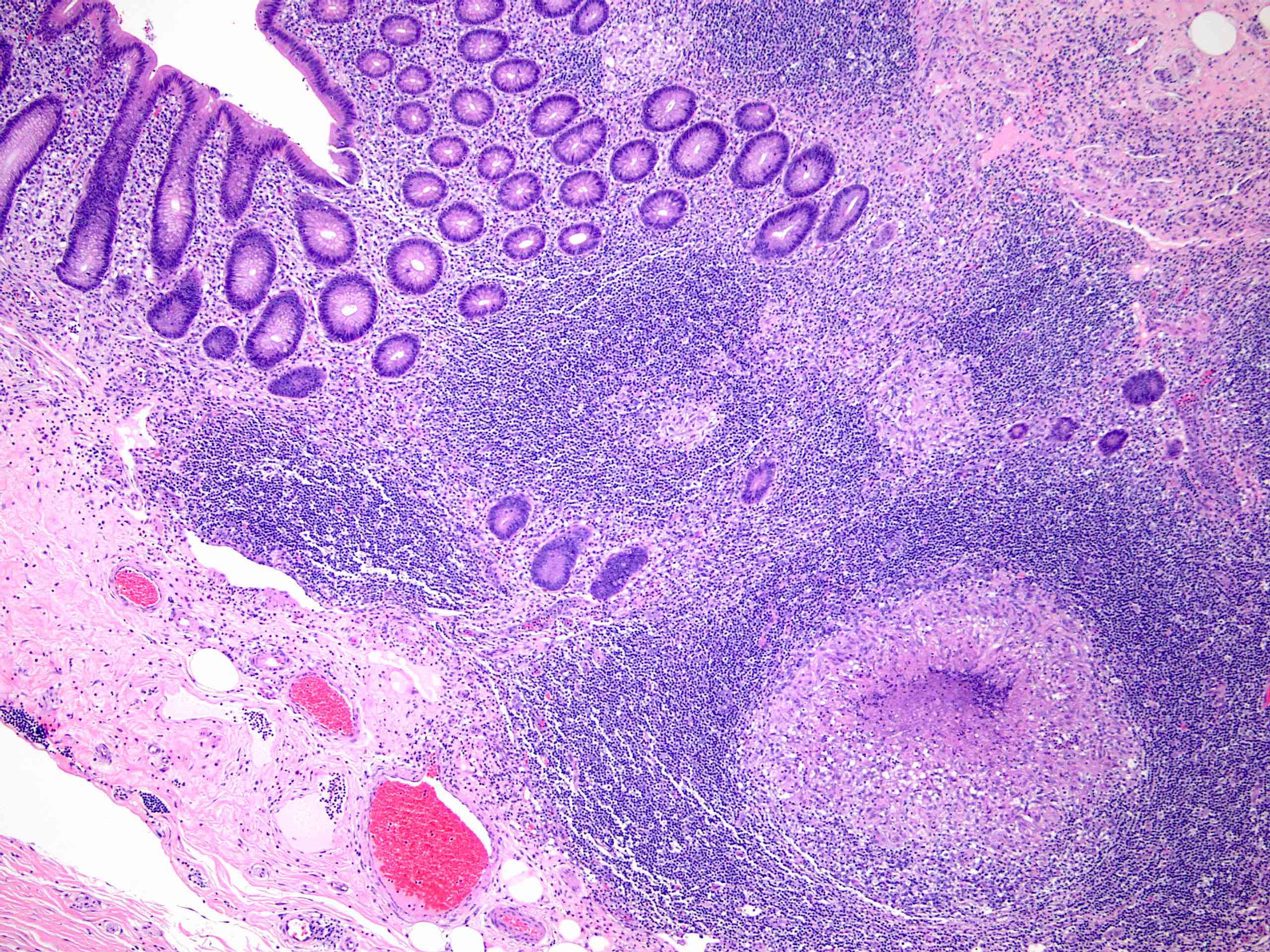
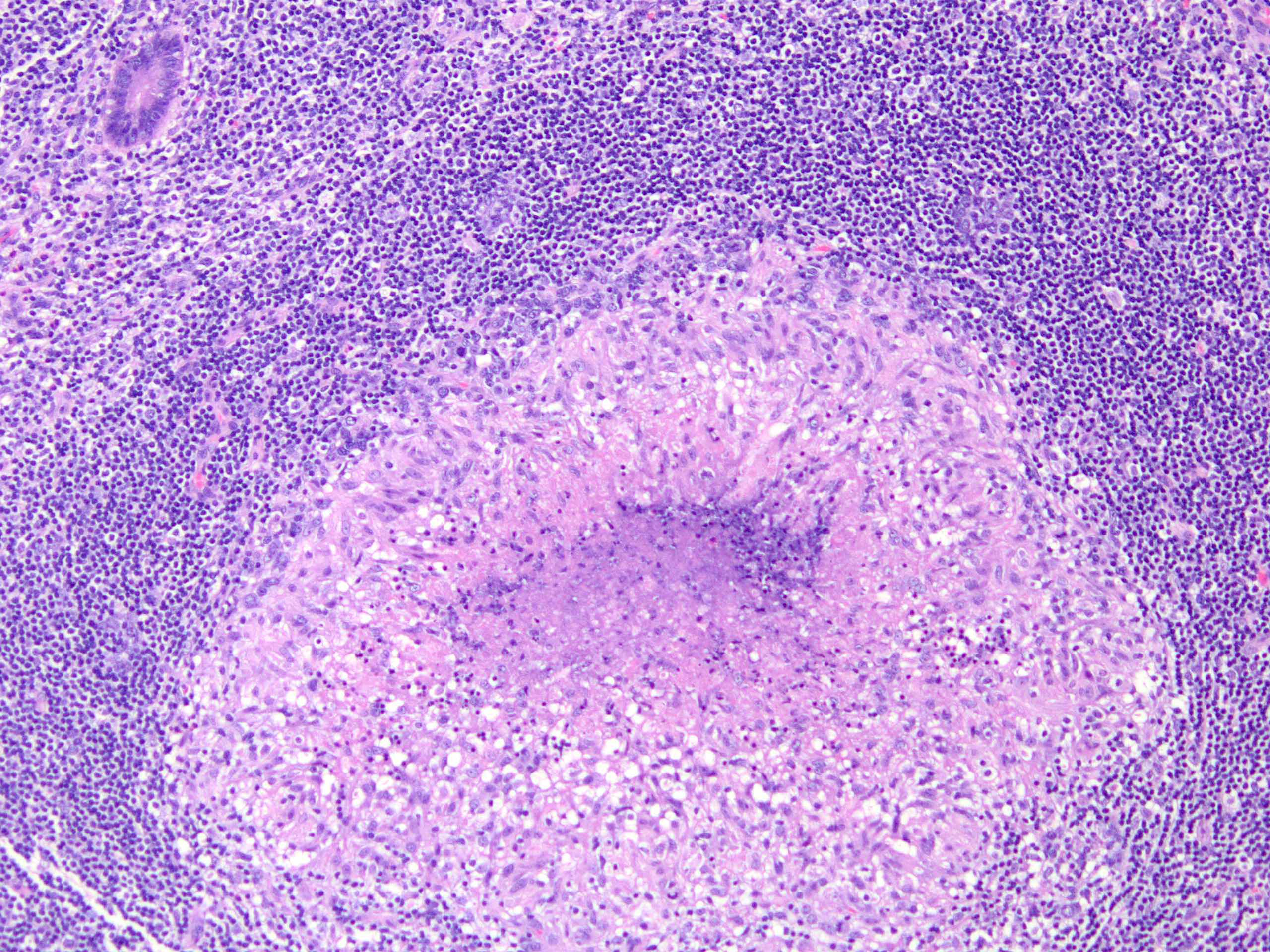
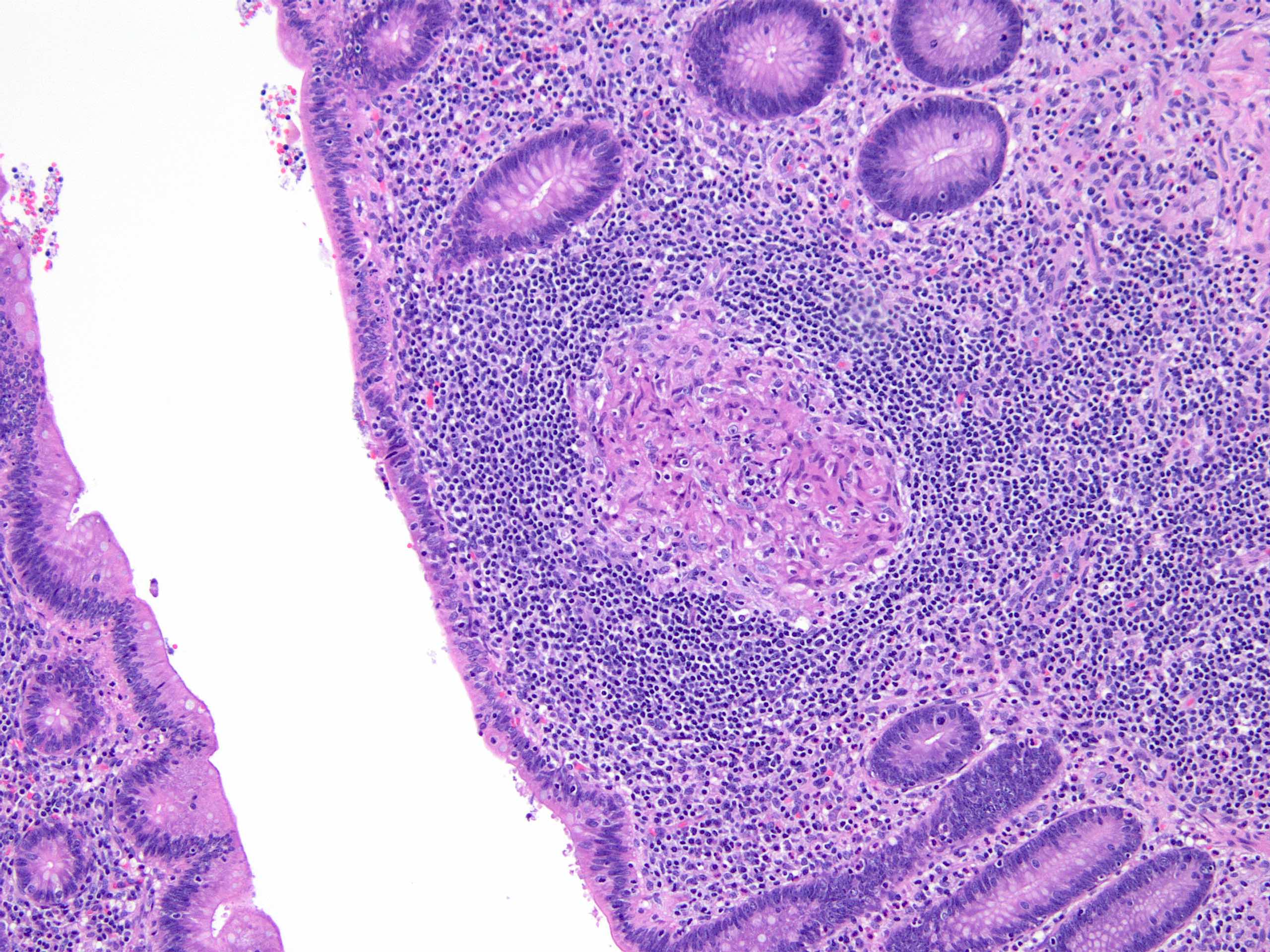
Microscopic (histologic) description
- Presence of necrotizing or nonnecrotizing granulomas with or without focal acute inflammation, mucosal erosion, ulceration, fissures or lymphoid aggregates (Hum Pathol 1993;24:595)
- Presence of numerous granulomas is a histopathologic feature distinguishing idiopathic granulomatous appendicitis from Crohn's disease (Hum Pathol 1993;24:595)
Microscopic (histologic) images
Sample pathology report
- Appendix, appendectomy:
- Appendix with numerous granulomas, focally necrotizing (see comment)
- Comment: Sections show an appendix with granulomatous inflammation (focally necrotizing). There is no evidence of chronicity. Multiple levels were evaluated. Acid fast bacteria (AFB) stain is negative for mycobacteria, Grocott Gomori methenamine silver (GMS) stain is negative for fungal organisms. Possible etiologies include but are not limited to infectious etiologies, including Yersinia pseudotuberculosis, Mycobacterium tuberculosis, fungal or parasitic infection or sarcoidosis. Crohn's disease is less favored (due to lack of other features of inflammatory bowel disease [IBD]) but should be excluded clinically. Idiopathic granulomatous appendicitis may occur but is rare. Clinical correlation is recommended.
Differential diagnosis
- Crohn's disease involving the appendix:
- Crohn's disease infrequently affects the appendix (Am J Surg Pathol 2021;45:1703)
- Distinction relies mainly on clinical history along with presence of active inflammation and crypt architectural distortion
- Appendiceal diverticulosis:
- Congenital (true) or acquired (false) (incidence of 0.014% and 1.9%, respectively) (Hum Pathol 2008;39:1823)
- Occurs in relatively older age group (Surg Today 2012;42:363)
- Distinction relies on presence of diverticula
- Interval appendicitis:
- Patients with complicated appendicitis (i.e., rupture) treated with antibiotics followed with delayed appendectomy
- Distinction relies on the clinical history
Board review style question #1
A 20 year old man presented to the emergency department with right lower quadrant abdominal pain and tenderness, vomiting, fever and anorexia. Appendectomy with clinical diagnosis of acute appendicitis was done and histologic examination is shown in the image above. What is the diagnosis?
- Acute appendicitis
- Appendix diverticula
- Granulomatous appendicitis
- Mucocele
Board review style answer #1
C. Granulomatous appendicitis. This section shows the formation of multiple granulomas. Answer A is incorrect because no significant acute inflammation supportive of acute appendicitis is present. Answer B is incorrect because no diverticula are identified. Answer D is incorrect because mucocele is a clinical diagnosis referring to a dilated appendix.
Comment Here
Reference: Granulomatous appendicitis
Comment Here
Reference: Granulomatous appendicitis
Board review style question #2
A 17 year old boy presented with mild right lower quadrant abdominal pain, malaise and mild fever for 2 weeks. He was diagnosed with ruptured acute appendicitis and was treated with antibiotics. He presented 2 months after for an appendectomy. Histologic evaluation of the appendix revealed chronic inflammation and multiple granulomas. What is the most likely underlying cause of granulomatous appendicitis in this patient?
- Crohn's disease
- Interval appendectomy
- Sarcoidosis
- Tuberculosis
Board review style answer #2
B. Interval appendectomy. Interval appendectomy is an important cause of granulomatous inflammation in the appendix. Clinical history is the main clue in this scenario. Answer A is incorrect because Crohn's disease rarely involves the appendix. Answer D is incorrect because tuberculosis often presents with systemic symptoms and necrotizing granulomatous inflammation. Answer C is incorrect because sarcoidosis often shows well formed nonnecrotizing granulomas. Presence of a clinical history is helpful.
Comment Here
Reference: Granulomatous appendicitis
Comment Here
Reference: Granulomatous appendicitis