Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1Cite this page: Ni P, Liu Q. Diverticulosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/appendixdiverticula.html. Accessed March 31st, 2025.
Definition / general
- Outpouchings of the appendiceal wall; either acquired or congenital
Essential features
- Rare, usually asymptomatic (Int J Surg Pathol 2009;17:231)
- The majority of appendiceal diverticula are acquired (pseudodiverticula), consisting of mucosa, submucosa and serosa but not muscularis propria
- Congenital diverticula (true diverticula) consist of all layers of the appendiceal wall (Int J Surg Pathol 2009;17:231)
- A meta analysis of 11 studies revealed a strong association between appendiceal neoplasms and appendiceal diverticulosis; however, no significant correlation was found between low grade appendiceal mucinous neoplasm (LAMN) and appendiceal diverticulosis in another study (ANZ J Surg 2020;90:1871, Mod Pathol 2020;33:953)
ICD coding
- ICD-10: K38.2 - diverticulum of appendix
Epidemiology
- Uncommon, incidence is ~2% in surgical appendectomy specimens; often underreported due to their small size and asymptomatic nature (Int J Surg Pathol 2009;17:231, ANZ J Surg 2020;90:1871)
- Congenital appendiceal diverticulosis is very rare (incidence of 0.014%) (Int J Surg Pathol 2009;17:231)
- Acquired appendiceal diverticulosis is usually seen in older patients (> 30 years old); M > F (Int J Surg Pathol 2009;17:231, ANZ J Surg 2020;90:1871)
Sites
- Appendix
Pathophysiology
- Acquired appendiceal diverticulosis results from either inflammatory or noninflammatory processes, the former from an appendiceal wall weakened by inflammation and the latter from increased luminal pressure from obstruction (stricture, fecalith, tumors, etc.) and muscular contraction (Int J Surg Pathol 2009;17:231, South Med J 2000;93:76)
- Congenital appendiceal diverticulosis is believed to be associated with chromosomal anomalies, such as trisomy 13 or trisomy 21; other etiology includes developmental anomalies (Int J Surg Case Rep 2020;77:450, Int J Surg Pathol 2009;17:231)
Etiology
- Anatomical features of the appendix, such as a narrow lumen with a closed end, make it susceptible to raised pressure
- Acquired diverticulum results from increased intraluminal pressure of the appendix
- Chromosomal defects may play a role in the formation of congenital diverticulum (ANZ J Surg 2020;90:1871, Int J Surg Pathol 2009;17:231, Int J Surg Case Rep 2020;77:450)
- No association between appendiceal diverticulosis and colonic diverticulosis (Am Surg 2006;72:221)
Clinical features
- Asymptomatic and usually an incidental finding (Int J Surg Pathol 2009;17:231)
- Once diverticulitis develops, patients can present with low grade fever, vague and intermittent pain in the right lower quadrant abdomen but typically without nausea or vomiting (Int J Surg Pathol 2009;17:231, World J Gastroenterol 2015;21:3921)
- Patients with appendiceal diverticulitis have a higher perforation rate than acute appendicitis (World J Gastroenterol 2015;21:3921)
- Appendiceal diverticulosis and diverticulitis can be divided into 4 morphologic types (Surg Gynecol Obstet 1989;168:13, Int J Surg Pathol 2009;17:231)
- Type 1: appendix with acute appendiceal diverticulitis
- Type 2: acute appendicitis with acute appendiceal diverticulitis
- Type 3: acute appendicitis with noninflamed diverticulum
- Type 4: appendix with diverticulum
Diagnosis
- Appendiceal diverticula are diagnosed microscopically on appendectomy specimens
- Appendiceal diverticula can be identified radiologically; however, detection is usually difficult due to their small size and superimposed inflammation
Laboratory
- Nonspecific laboratory findings including leukocytosis and increased C reactive protein level if appendiceal diverticulitis developed
Radiology description
- Computed tomography (CT) can detect diverticula as round cystic outpouchings of the appendiceal wall and may outperform colonoscopy and barium enema for detecting diverticula (World J Gastroenterol 2021;27:4441)
- Compared with typical acute appendicitis, appendiceal diverticulitis tends to exhibit a larger diameter, periappendiceal fat stranding and extraluminal fluid on CT (Jpn J Radiol 2017;35:225)
Radiology images
Prognostic factors
- Risk factors associated with acquired appendiceal diverticula include age > 30 years old, cystic fibrosis and Hirschsprung disease (Int J Surg Pathol 2009;17:231)
- Association between diverticulosis and neoplasms (e.g., low grade mucinous neoplasia, sessile serrated lesion, carcinoid tumor and carcinoma) (ANZ J Surg 2020;90:1871)
Case reports
- 18 year old woman with inflamed congenital diverticulum (J Surg Case Rep 2023;2023:rjad116)
- 19 year old woman with congenital appendiceal diverticulum (Cureus 2021;13:e14488)
- 72 year old man with a 20 mm cecal lesion during a colonoscopy, which turned out to be an appendiceal diverticulum at the appendiceal base (BMC Gastroenterol 2022;22:262)
- 73 year old woman with appendiceal diverticulum associated with chronic appendicitis (Int J Surg Case Rep 2014;5:961)
Treatment
- Appendectomy is the treatment of choice for symptomatic appendiceal diverticulitis
- Prophylactic appendectomy may be beneficial for appendiceal diverticulosis due to its higher perforation rate, higher mortality rate and association with neoplasm (Am Surg 2006;72:221, ANZ J Surg 2020;90:1871)
Gross description
- Acquired appendiceal diverticula are often small (2 - 5 mm) and multiple, most commonly occurring at the distal one - third of the appendix and also along the mesenteric border (Int J Surg Pathol 2009;17:231)
- Congenital appendiceal diverticulosis is usually present as a single diverticulum at the antimesenteric side (Int J Surg Pathol 2009;17:231)
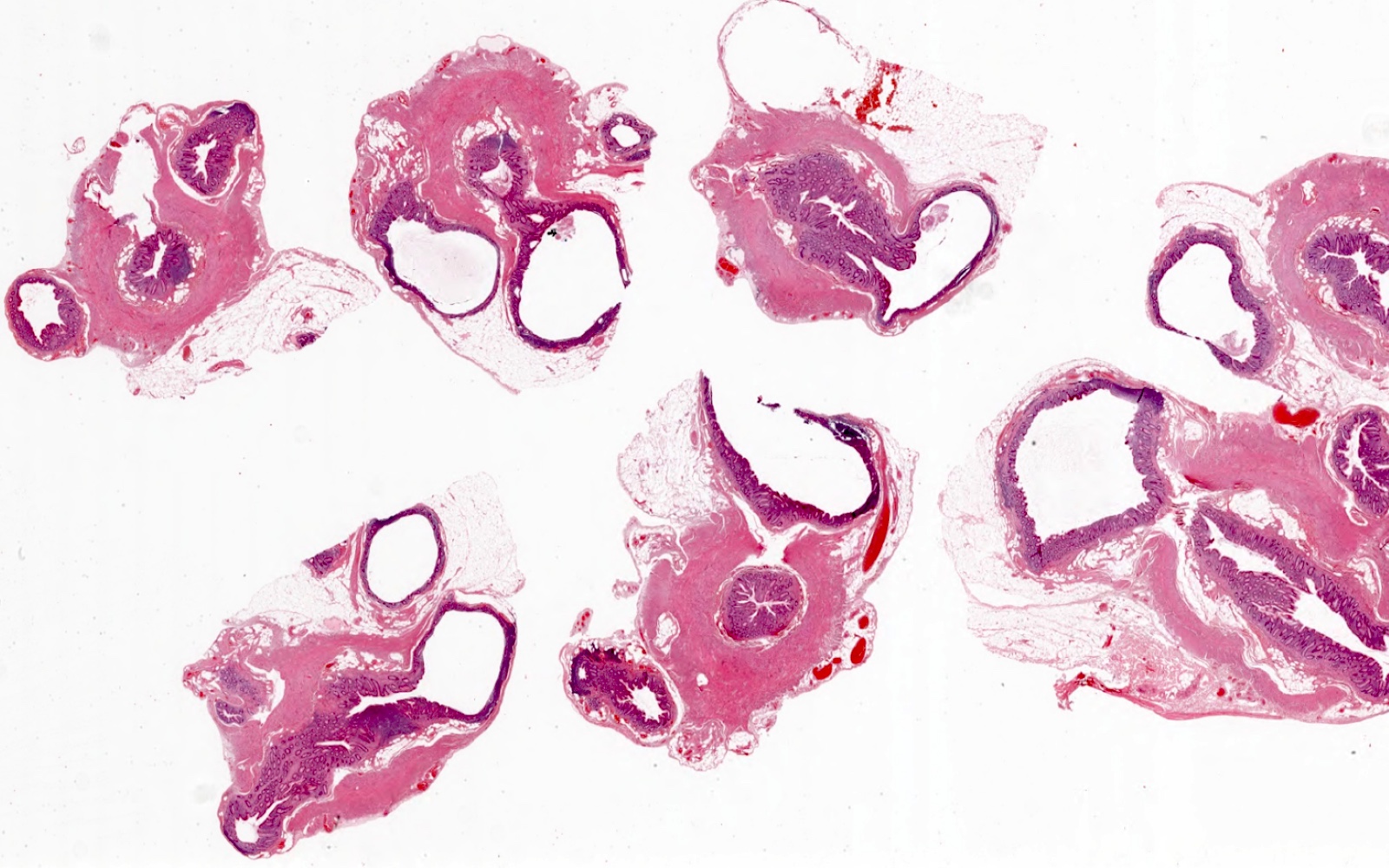
Gross images
Microscopic (histologic) description
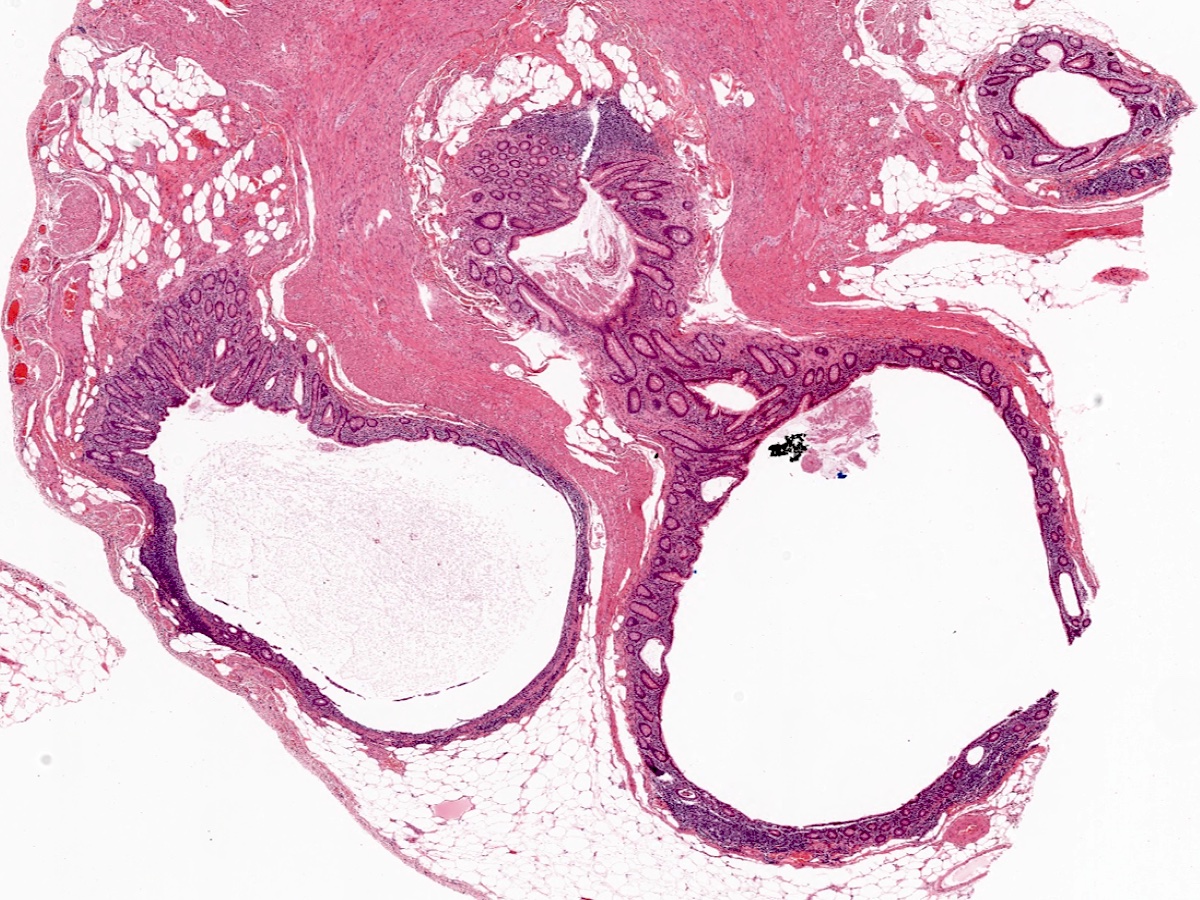
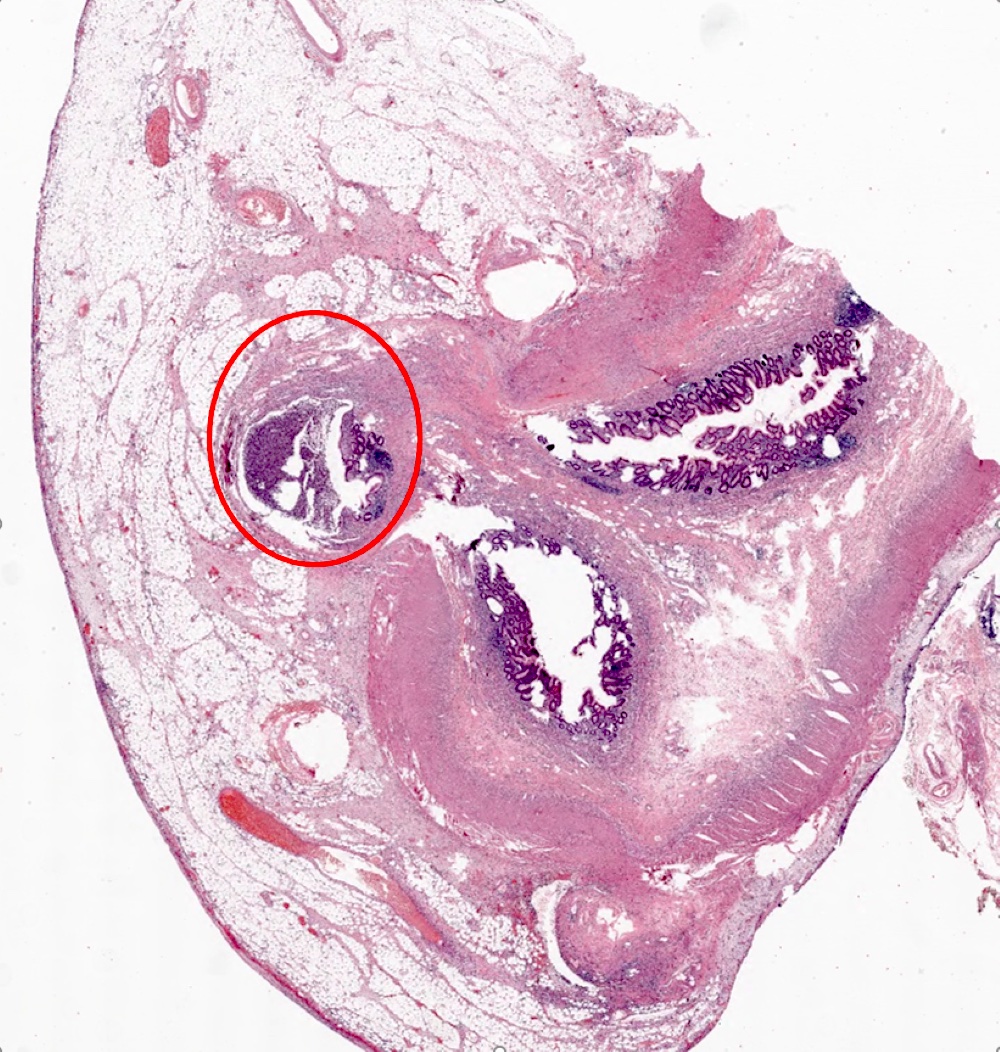
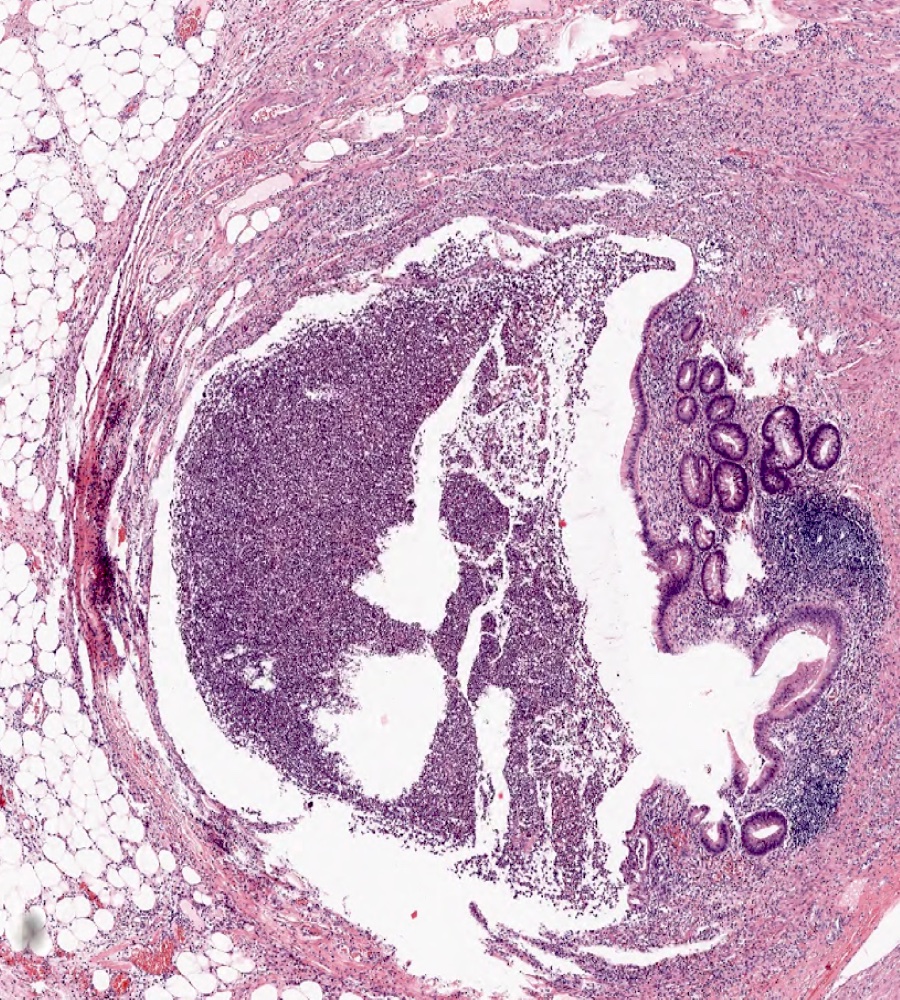
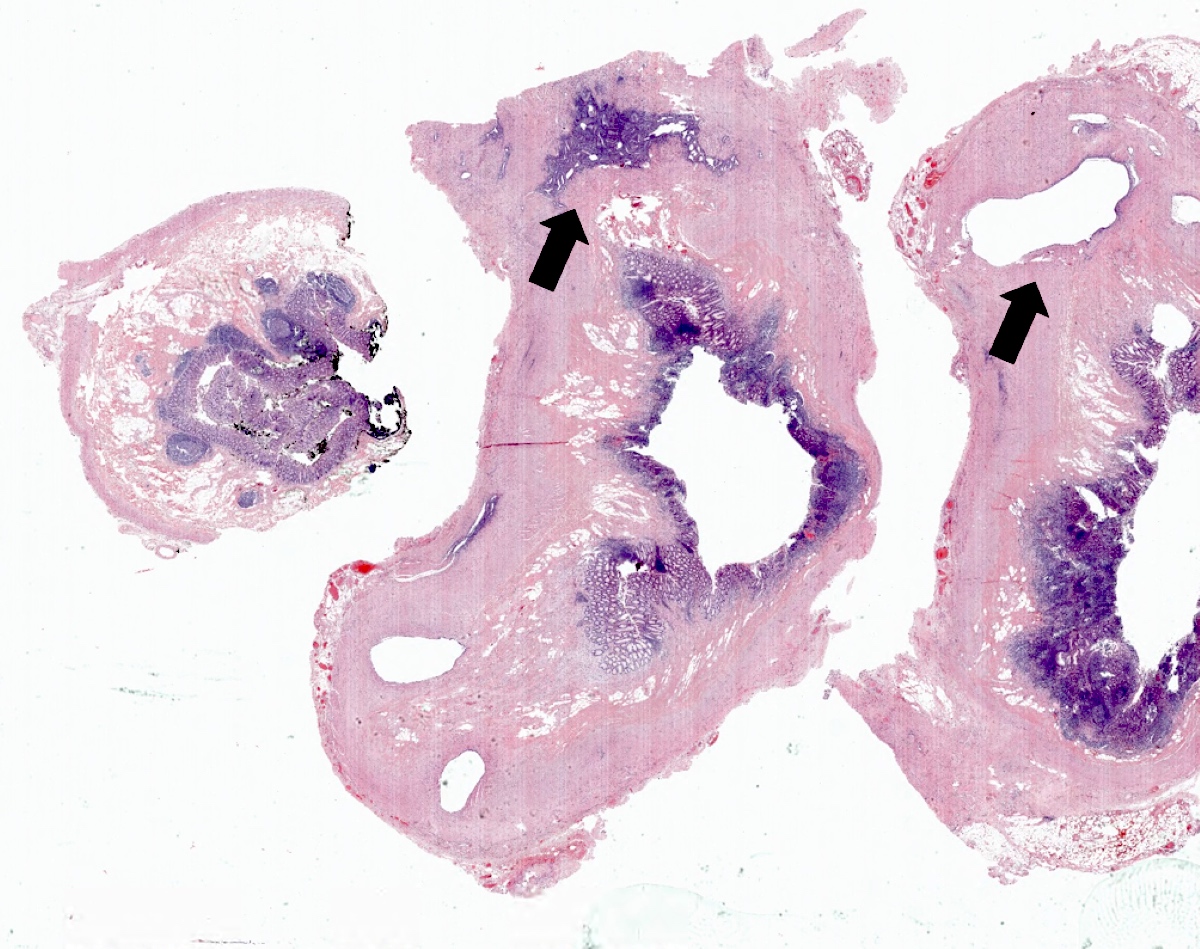
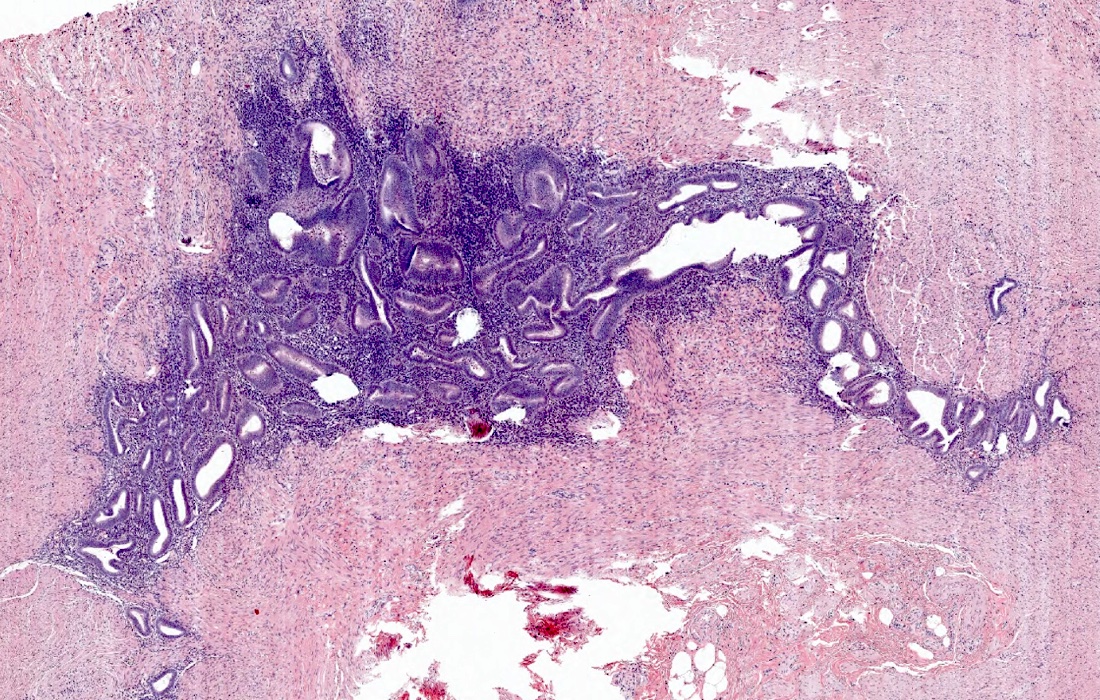
- Acquired appendiceal diverticulosis (pseudodiverticulum), consisting of mucosa and submucosa, are outpouchings through the weakened muscularis propria
- When inflamed, mixed inflammatory cells including neutrophils are present in association with diverticulum
- Ruptured diverticulum may mimic appendiceal mucinous neoplasm with extravasated mucin pool (Am J Surg Pathol 2009;33:1515)
- Association with mucosal Schwann cell proliferation (Int J Surg Pathol 2013;21:603)
- Congenital appendiceal diverticulosis (true diverticulum) comprises all layers of the appendiceal wall including the muscularis propria; less likely to perforate (Int J Surg Case Rep 2020;77:450)
Microscopic (histologic) images
Videos
Acute appendicitis accompanied by appendiceal diverticulitis
Sample pathology report
- Appendix, appendectomy:
- Appendiceal diverticulosis with associated active chronic diverticulitis
- Appendix, appendectomy:
- Ruptured appendiceal diverticulum with associated mucin extravasation in the periappendix, inflammation and fibrosis (see comment)
- Comment: The appendix has been entirely sectioned and reviewed. Negative for dysplasia or neoplasm.
Differential diagnosis
- Appendiceal endometriosis:
- Appendiceal mucinous neoplasm:
- Extrusion of mucin seen in ruptured diverticula can mimic low grade appendiceal mucinous neoplasm (LAMN)
- However, LAMN is lined by neoplastic epithelial cells with diminished or decreased lamina propria, which should not be identified in diverticula (Am J Surg Pathol 2009;33:1515)
Board review style question #1
Which of the following is correct regarding the entity shown in the image above?
- All cases exhibit a higher perforation rate
- It can be acquired or congenital
- It is a frequently encountered lesion and is commonly observed in routine surgical specimens
- It is an insignificant pathological finding; therefore, it does not require reporting
Board review style answer #1
B. It can be acquired or congenital. Answer C is incorrect because the entity is appendiceal diverticulosis, which is a rare finding. Answer D is incorrect because there is a strong association between appendiceal diverticulosis and neoplasms; therefore, reporting of diverticulosis is required. Answer A is incorrect because appendix with acquired diverticulosis (acquired but not all diverticulosis) has a greater likelihood of perforation and mortality when inflamed.
Comment Here
Reference: Diverticulosis
Comment Here
Reference: Diverticulosis