Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Liu BL, Liu Q. Adenocarcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/appendixadenocarcinoma.html. Accessed April 3rd, 2025.
Definition / general
- Malignant gland forming neoplasm of the appendix
Essential features
- Distinction from low grade appendiceal mucinous neoplasm (LAMN) is made by the presence of invasive glands or signet ring cells
- Rare, histologically and molecularly diverse malignancies
- Most commonly found incidentally on a surgical specimen after appendectomy for acute appendicitis or after rupture of the primary tumor with spread of mucin and tumor cells throughout the peritoneal cavity
- Prognosis depends on the tumor subtype, grade and stage
Terminology
- Not recommended by WHO (2019): mucinous cystadenocarcinoma
ICD coding
Epidemiology
- Rare, with an incidence of 0.12 cases per 1,000,000 people per year in the United States (Cancer 2002;94:3307)
- Typically affects patients in their fifth to seventh decade of life (Mod Pathol 2015;28:S67)
- Slight female predominance for mucinous adenocarcinoma (53.9% female) and signet ring cell adenocarcinoma (63.6% female) (Cancer 2016;122:213)
- Slight male predominance for nonmucinous adenocarcinoma (54.6% male) (Cancer 2016;122:213)
Sites
- Anywhere in the appendix
Pathophysiology
- Unknown
Etiology
- Unknown
- Colonic type adenocarcinoma may arise from preexisting adenomas (Clin Colon Rectal Surg 2015;28:247)
- Mucinous adenocarcinoma may arise from appendiceal mucinous neoplasms (Oncologist 2017;22:1107)
Clinical features
- Patients with nonmucinous adenocarcinoma most often present with incidentally identified lesions following appendectomy for appendicitis or other indication (Dis Colon Rectum 2004;47:474)
- Patients with mucinous adenocarcinoma most often present after rupture of the primary tumor with spread of mucin and tumor cells throughout the peritoneal cavity (Clin Colon Rectal Surg 2015;28:247)
- Less common presentations include a palpable mass, obstruction, gastrointestinal bleeding and symptoms related to metastasis
Diagnosis
- Patients are often diagnosed after an appendectomy due to acute appendicitis (Clin Colon Rectal Surg 2015;28:247)
- Sometimes imaging tests, such as Xrays or CT scans, reveal existing tumors
Laboratory
- Nonspecific
- CEA, CA19-9, CA72-4 and CA125 elevation (Anticancer Res 2022;42:4217, Sci Rep 2018;8:2732)
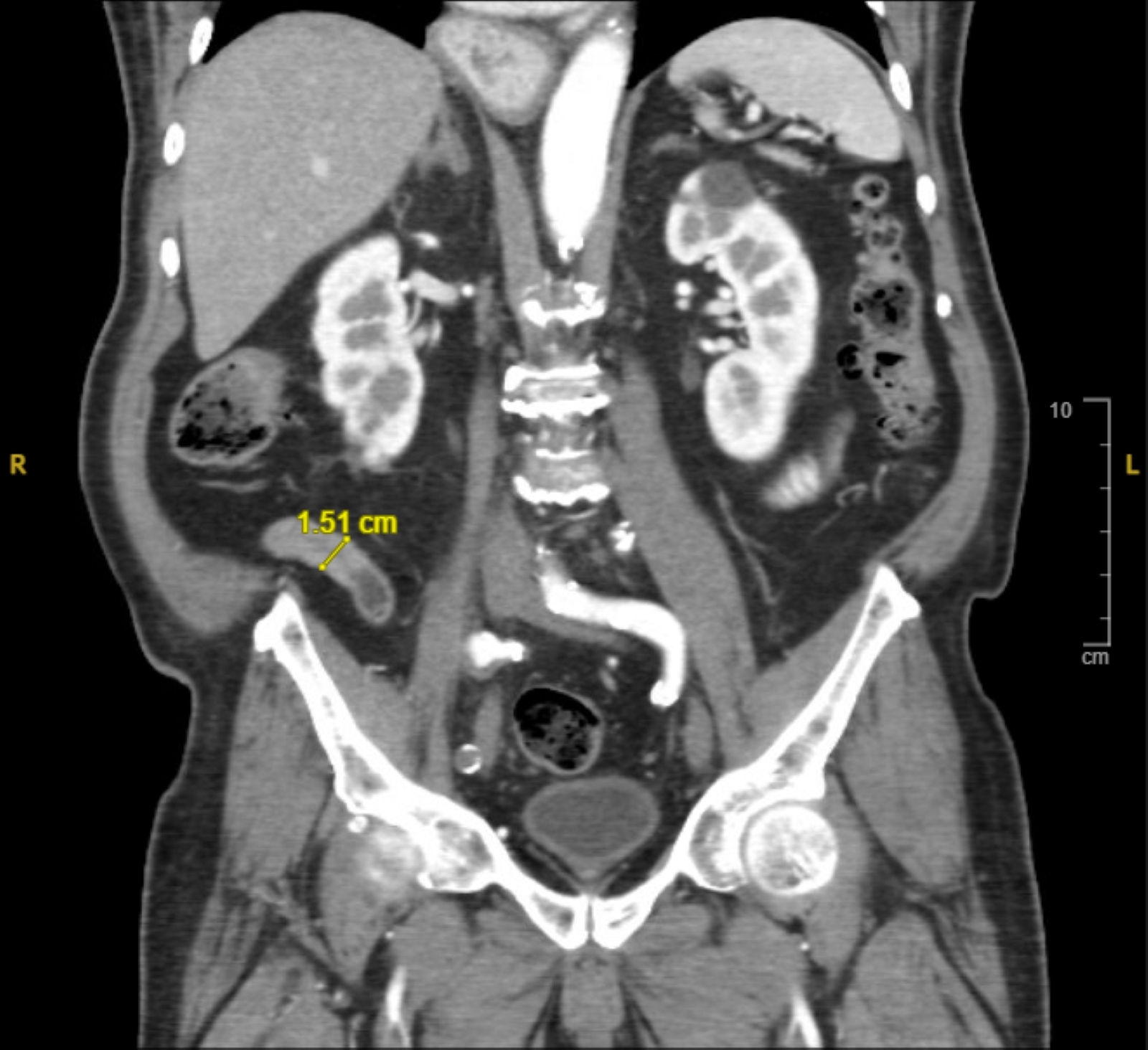
Radiology description
- Nonspecific, features may mimic acute appendicitis (J Med Imaging Radiat Oncol 2022;66:92)
- Mucinous adenocarcinoma: thick walled appendix with hyperenhancement; intraperitoneal fluid
- Nonmucinous adenocarcinoma: nodular mural thickening or soft tissue attenuation
Prognostic factors
- Prognosis depends on the tumor subtype, grade and stage and tumor location (Ann Surg 1994;219:51, Dis Colon Rectum 2004;47:474)
- 5 year survival rate
- Stage I - III
- Mucinous adenocarcinoma: 51.1 - 82%
- Nonmucinous adenocarcinoma: 39.8 - 68.9%
- Stage IV
- Mucinous adenocarcinoma: 11.3 - 56.7%
- Nonmucinous adenocarcinoma: 6 - 29.7%
- Signet ring cell carcinoma: 7% (World J Clin Cases 2015;3:538)
- Worse prognosis with high propensity for metastasis (Ann Surg Oncol 2006;13:624)
- Stage I - III
- Tumor location: tumors involving the base of appendix carry better prognosis than those of distal appendix, as obstruction in the lumen and associated acute appendicitis lead to early recognition
- 5 year survival rate
Case reports
- 27 year old man with right lower abdominal pain and retroperitoneal mass (Int J Surg Case Rep 2023;105:108001)
- 58 year old man with bilateral abdominal pain (Clin Case Rep 2022;10:e05349)
- 69 year old man with acute appendicitis (Cureus 2022;14:e28903)
- 84 year old woman with history of appendiceal adenocarcinoma presented with a left breast lump (BMJ Case Rep 2021;14:e240808)
- 90 year old woman with gross hematuria found to have a mass involving the appendix and the urinary bladder (Urol Case Rep 2022;45:102256)
Treatment
- Adenocarcinoma confined to the appendix
- Right hemicolectomy (Dis Colon Rectum 2019;62:1425)
- Regional lymph node metastasis rate: 20 - 67%
- Formal colectomy allows for more complete staging with therapeutic benefit
- Adenocarcinoma with peritoneal metastasis
- Consider cytoreductive surgery and intraperitoneal chemotherapy (Dis Colon Rectum 2019;62:1425)
Clinical images
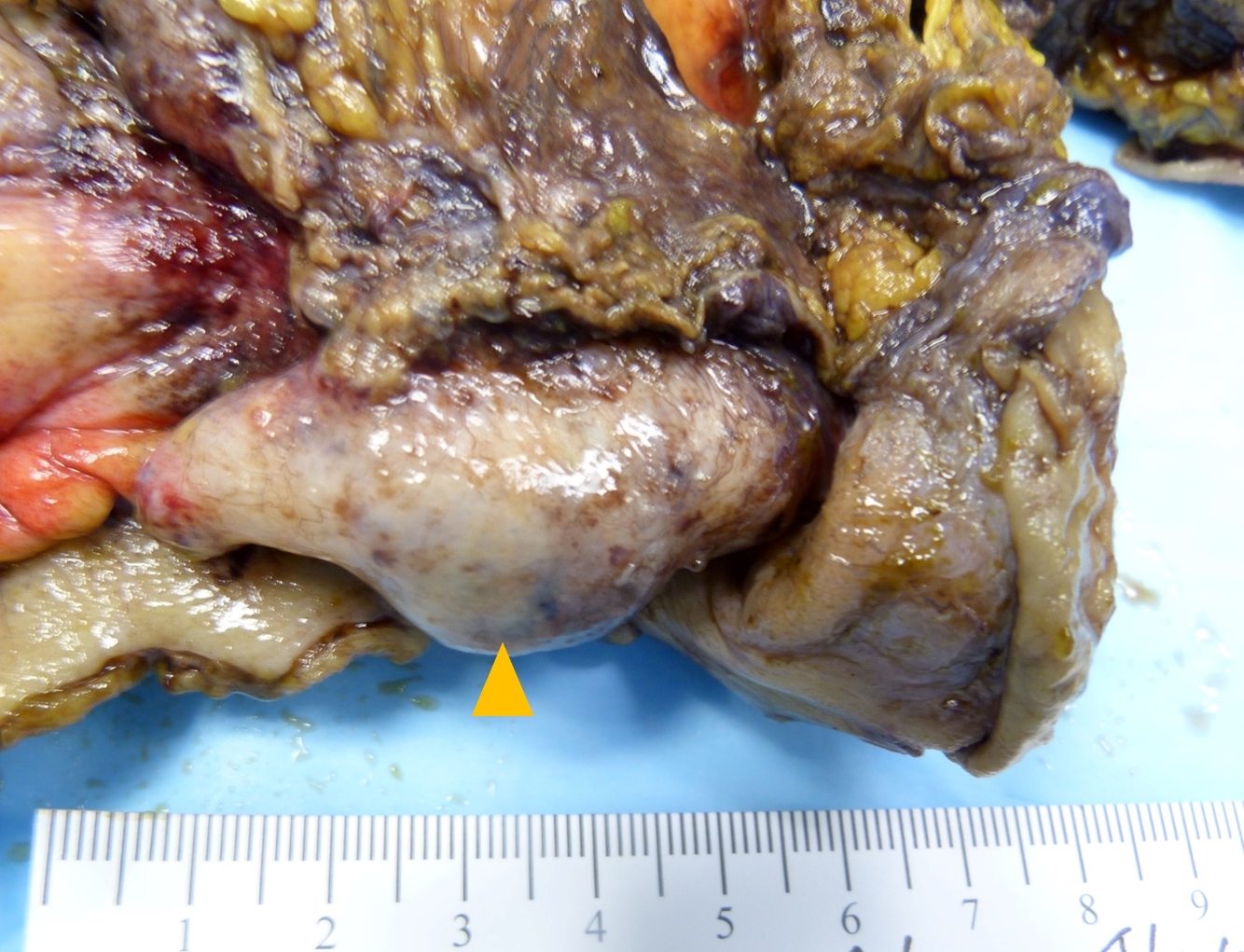
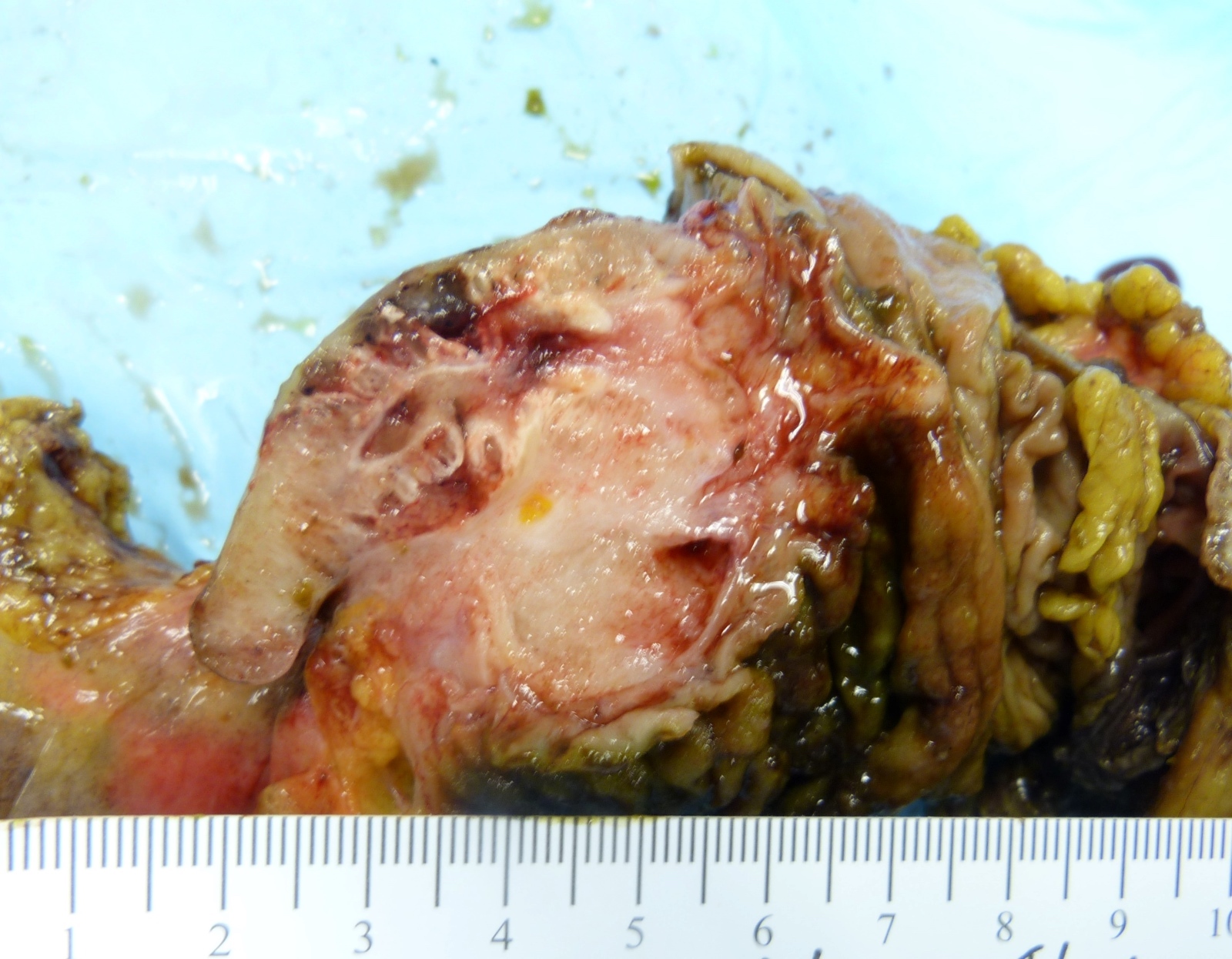
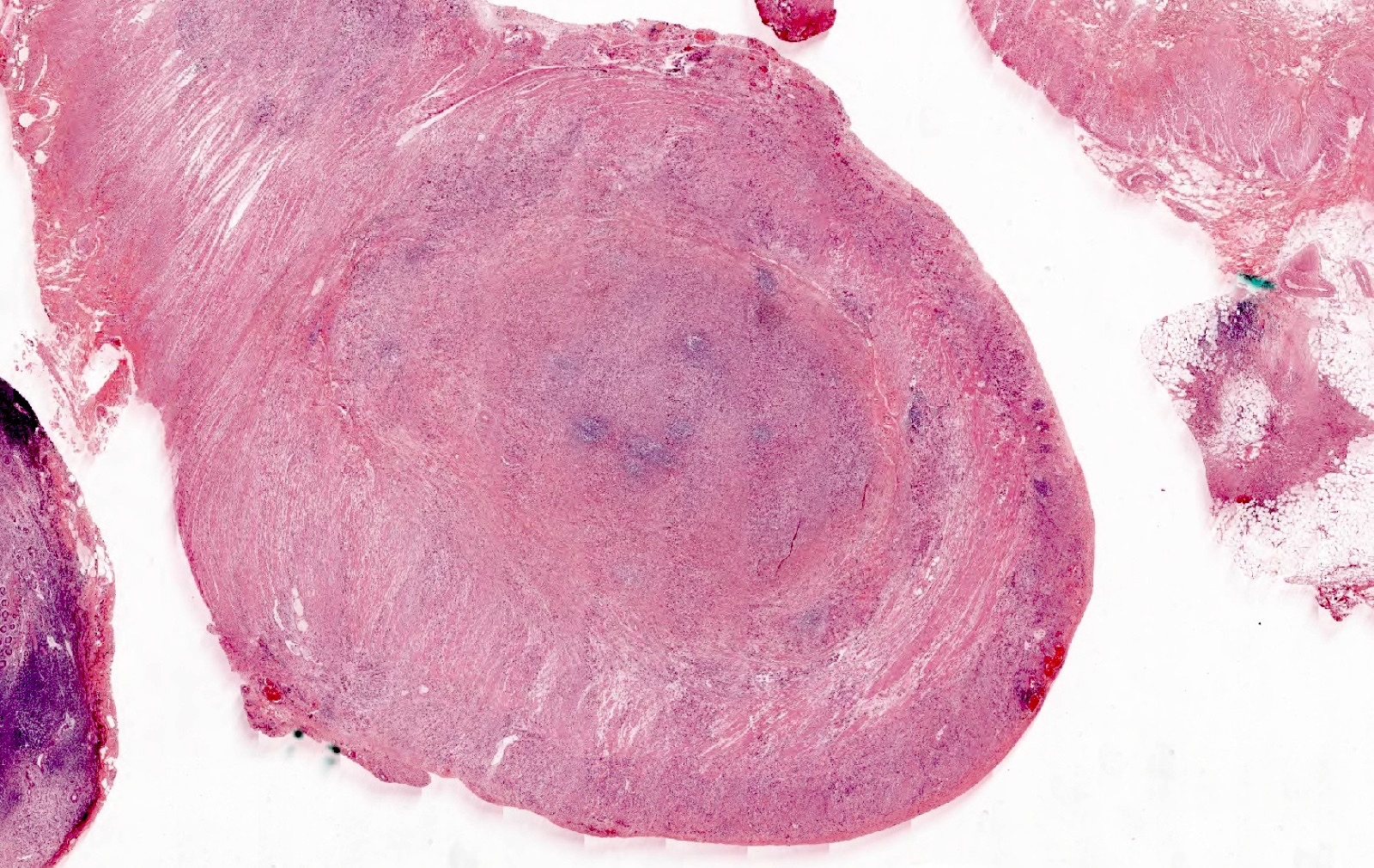
Gross description
- Appendiceal wall nodular or circumferential thickening
- May have cystic dilation of appendix due to luminal obstruction
- Copious gelatinous mucin in mucinous adenocarcinoma (Radiographics 2017;37:1059)
Gross images
Frozen section description
- See Microscopic (histologic) description below
- Diagnosis of primary adenocarcinoma of appendix on frozen section leads to right hemicolectomy even when the margin is negative (Arch Pathol Lab Med 2005;129:1558)
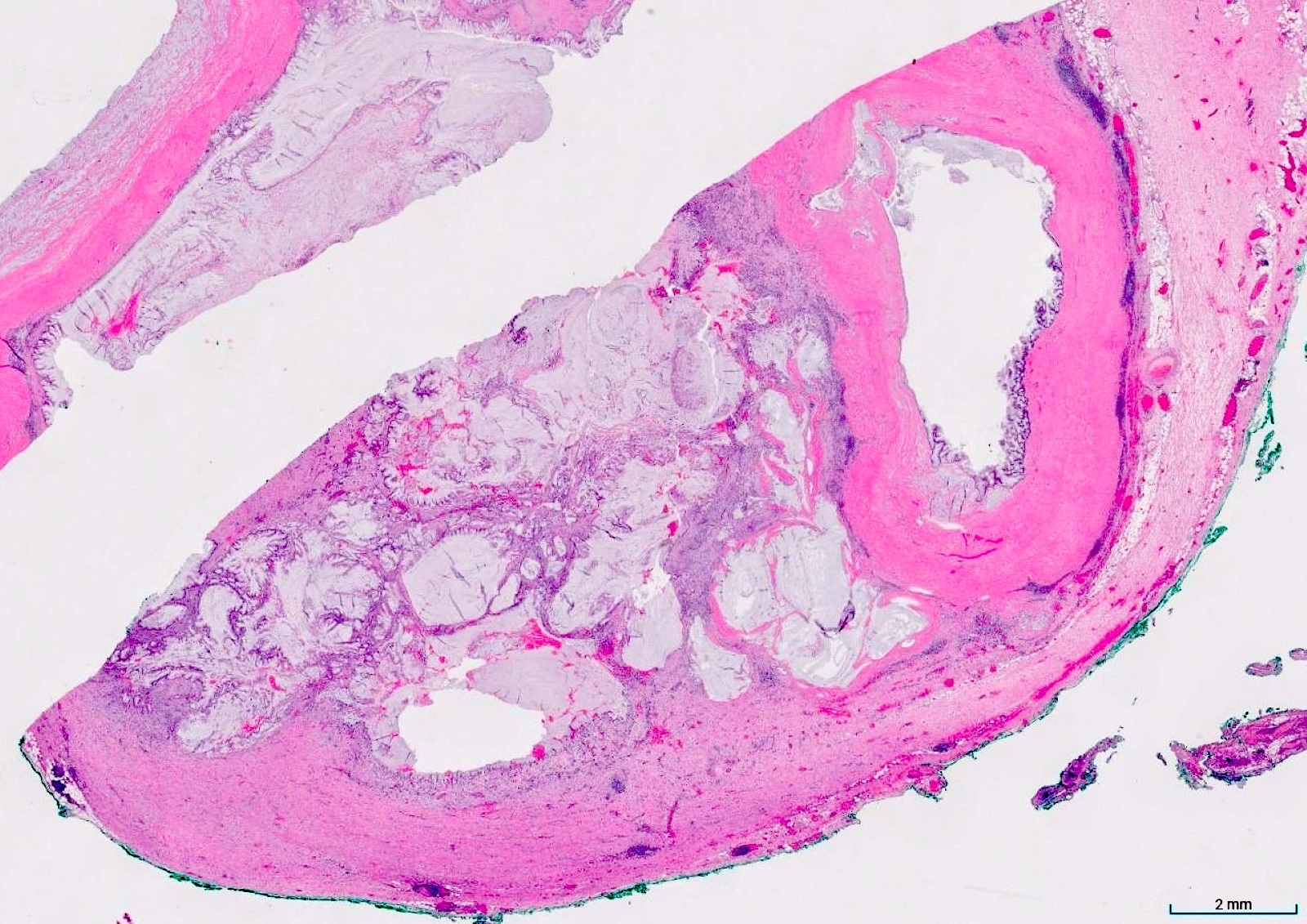
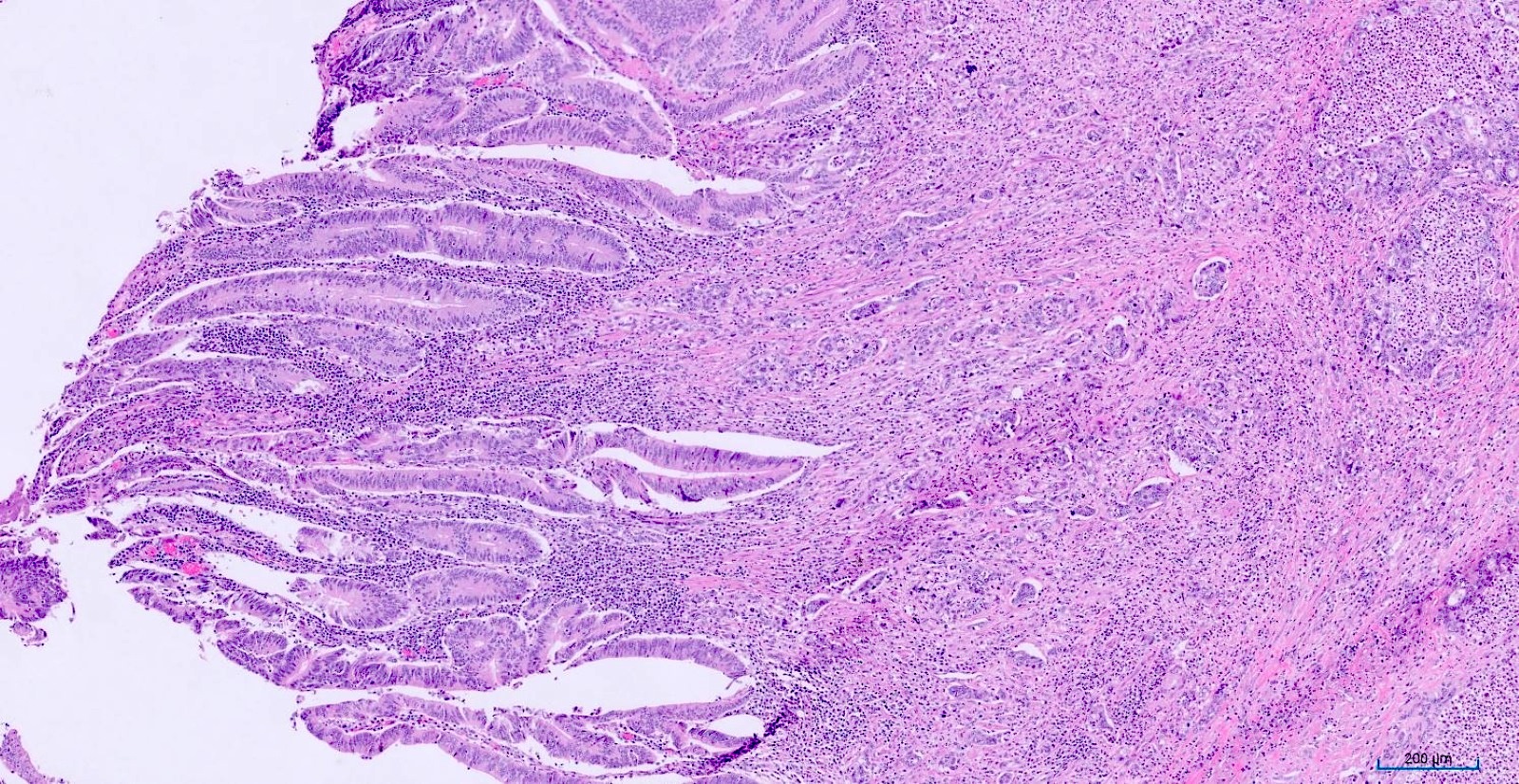
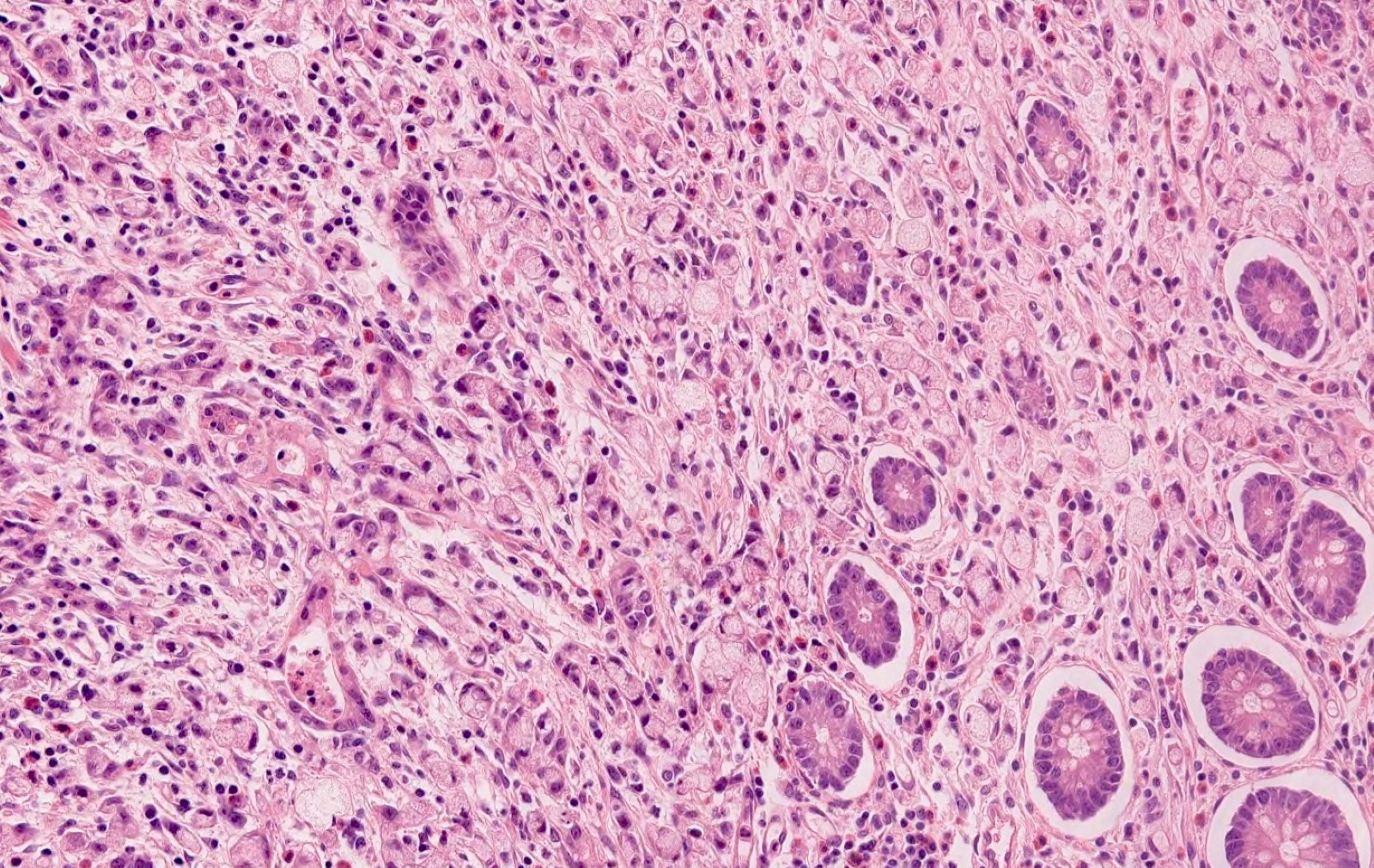
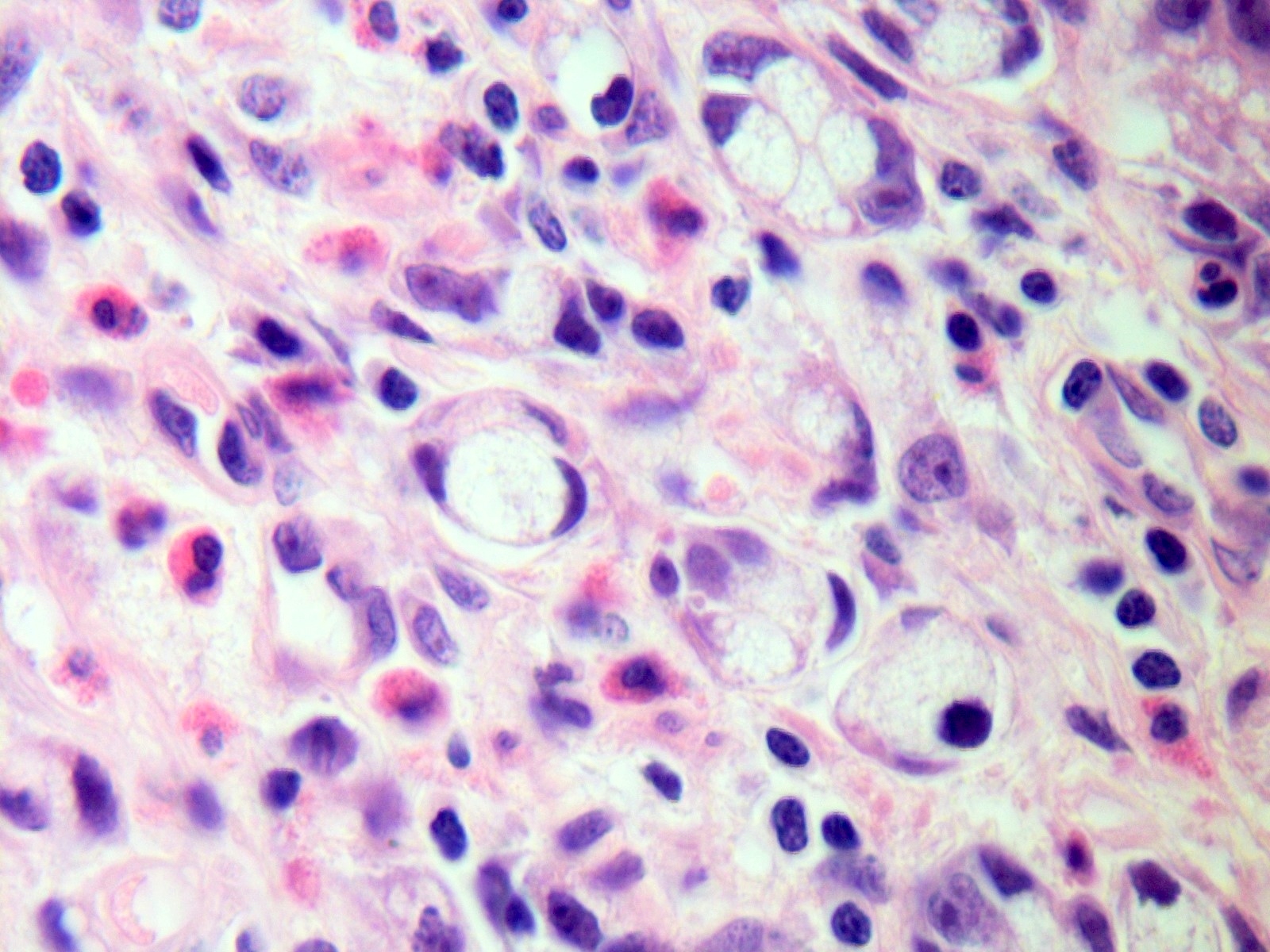
Microscopic (histologic) description
- Nonmucinous adenocarcinoma (J Pathol Transl Med 2021;55:247)
- Resembles colorectal adenocarcinoma
- Neoplastic glands with columnar cells containing hyperchromatic nuclei; often cribriform and with necrotic debris
- 2 tiered grading system based on gland formation (WHO 5th edition)
- Low grade (well to moderately differentiated): ≥ 50% gland formation
- High grade (poorly differentiated): < 50% gland formation
- Resembles colorectal adenocarcinoma
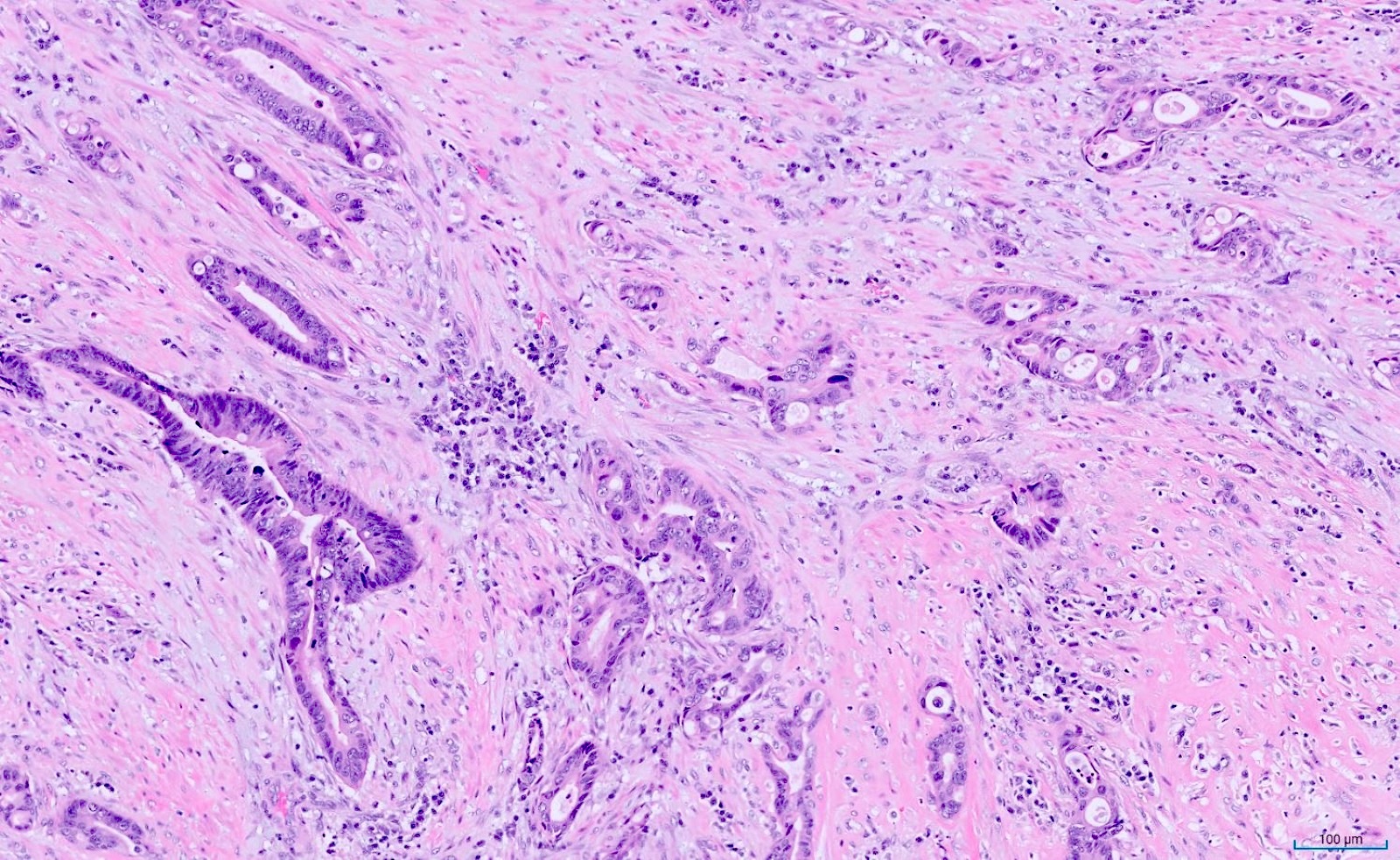
- Mucinous adenocarcinoma (Mod Pathol 2017;30:1177)
- Similar to those of the colon and rectum; requires > 50% extracellular mucin
- Irregular and jagged glands infiltrating the appendiceal wall or floating in the mucin; arranged as single cells, strips, clusters or complex glandular structures
- Often with high grade cytology
- 3 tiered grading system (AJCC 8th Cancer Staging Manual) (Mod Pathol 2014;27:1521, J Pathol Transl Med 2021;55:247, Adv Anat Pathol 2018;25:38)
- G1 (well differentiated): only applies to low grade mucinous neoplasm
- G2 (moderately differentiated): conventional mucinous adenocarcinoma without signet ring cell component
- G3 (poorly differentiated): high grade mucinous adenocarcinoma with signet ring cells component (< 50%)
- May rupture with transcoelomic spread to the peritoneum or ovaries
- Similar to those of the colon and rectum; requires > 50% extracellular mucin
- Signet ring adenocarcinoma (J Pathol Transl Med 2021;55:247)
- Similar to signet ring cell adenocarcinoma elsewhere in the GI tract; requires > 50% signet ring cells
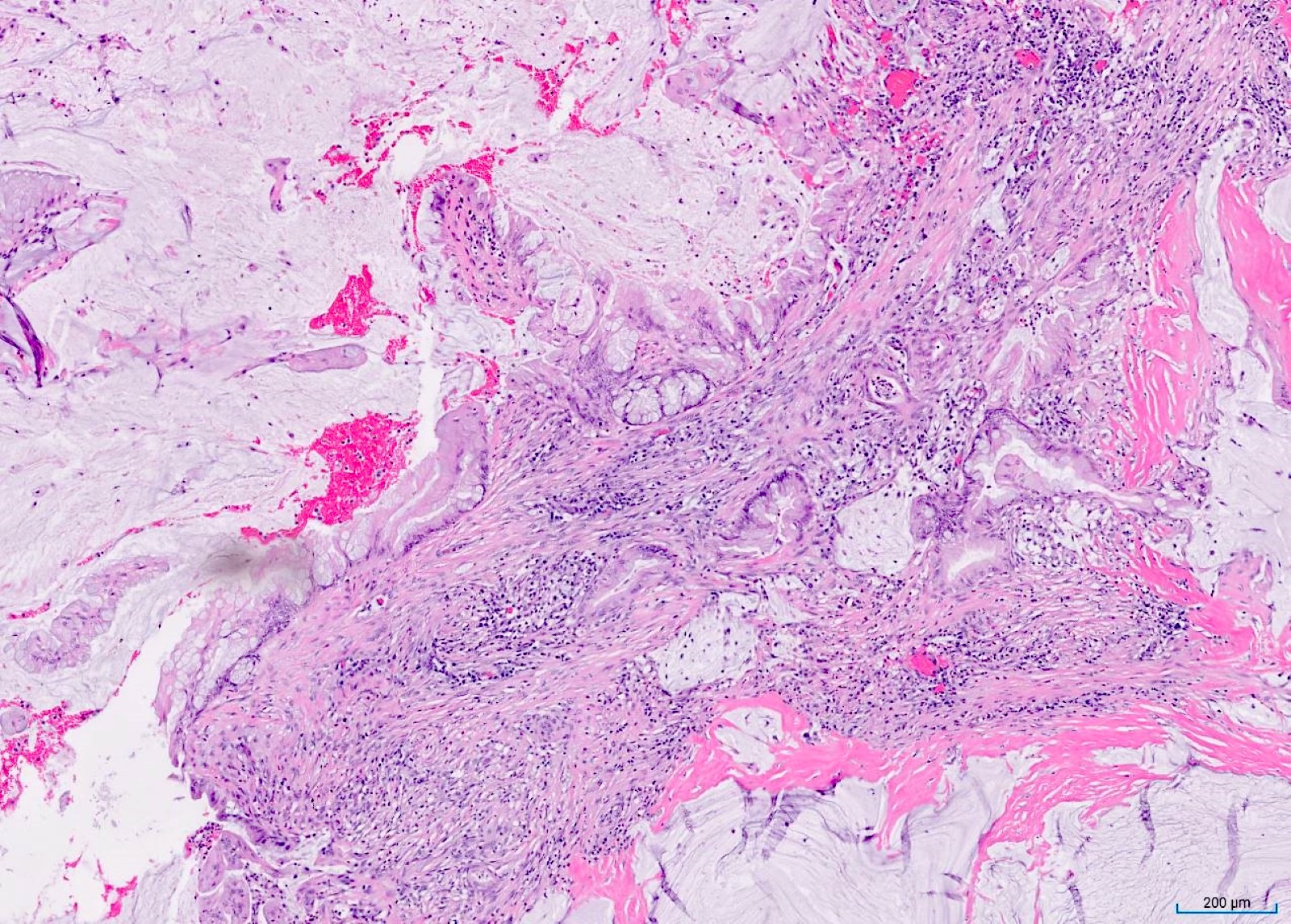
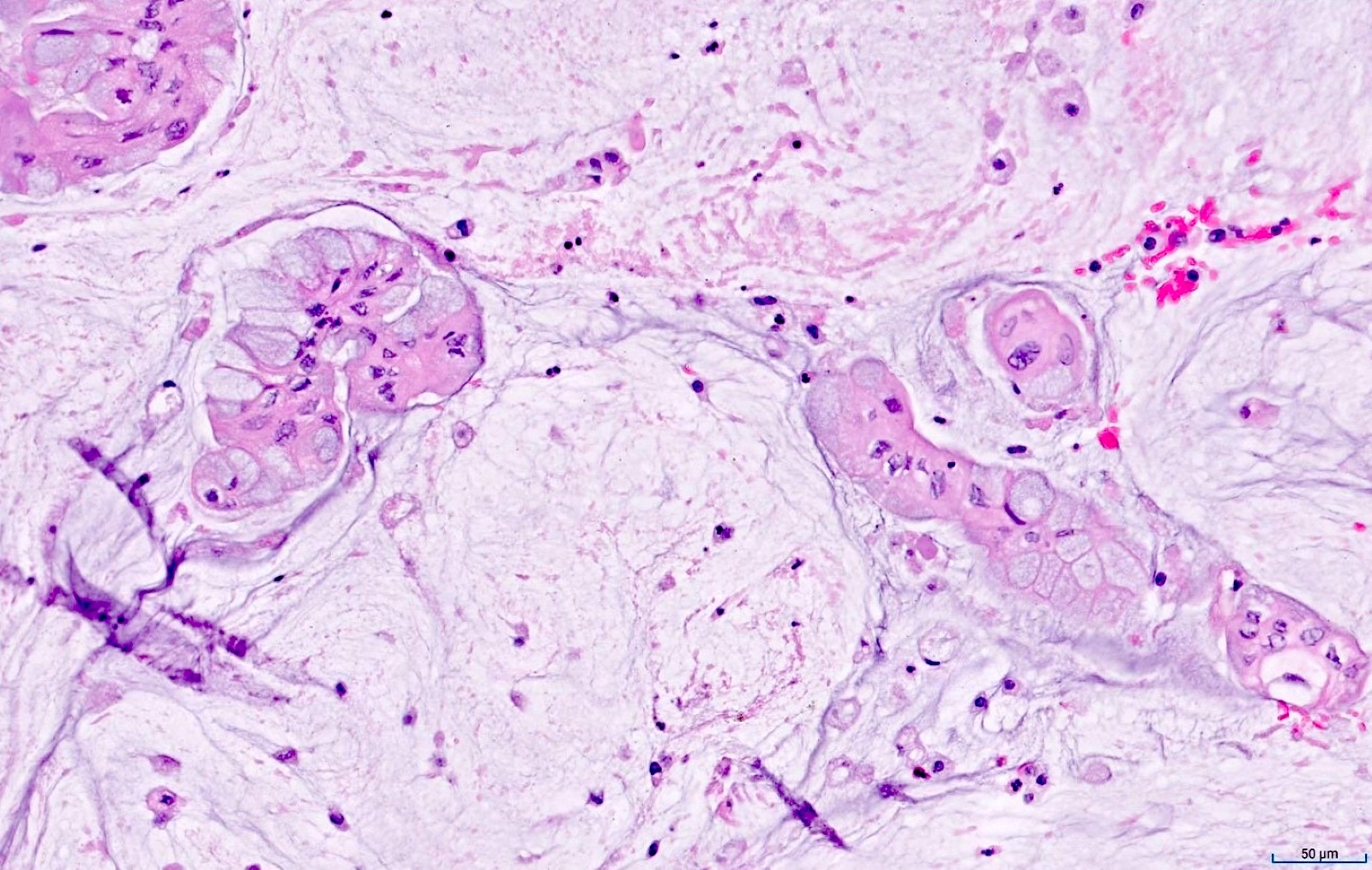
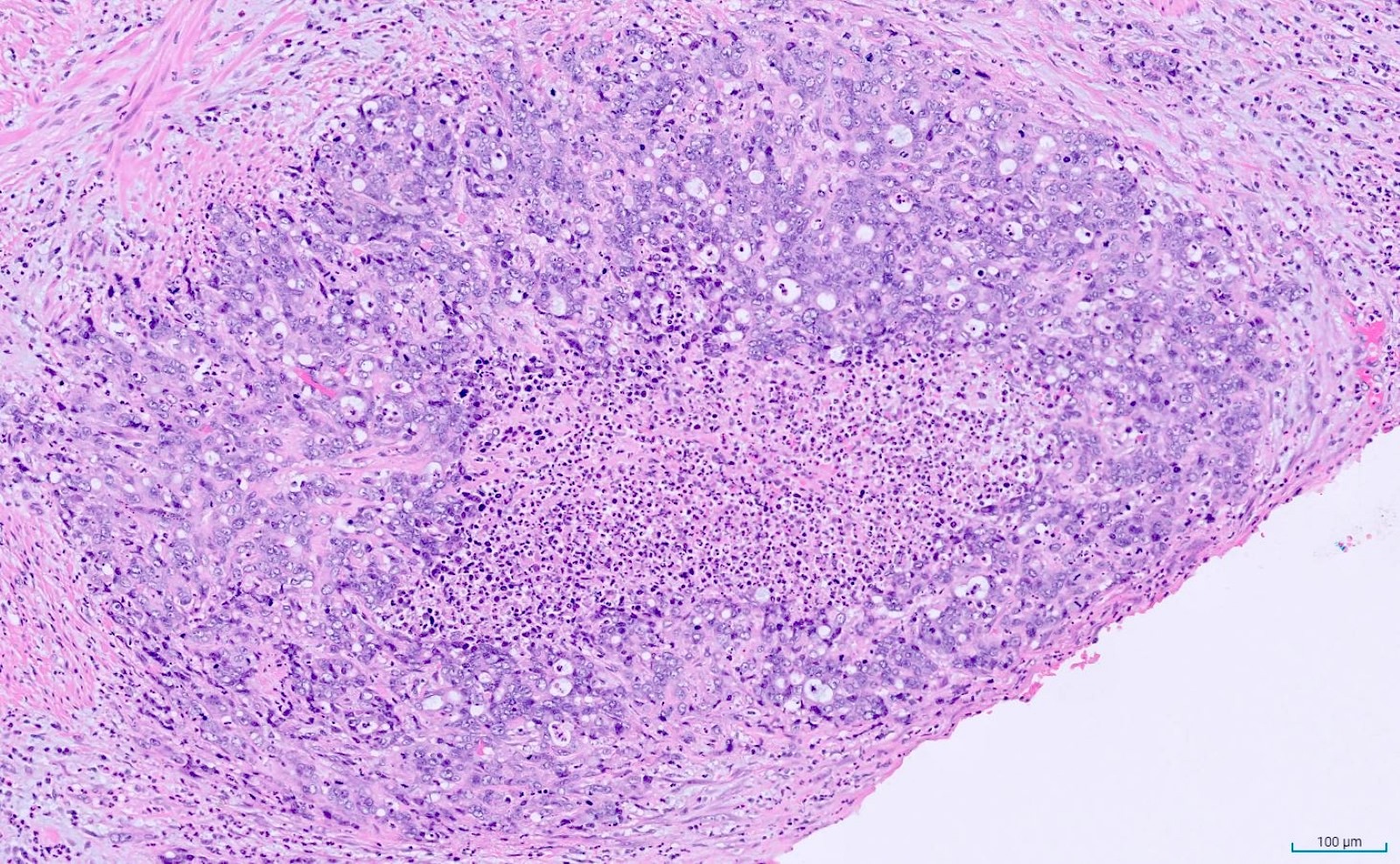
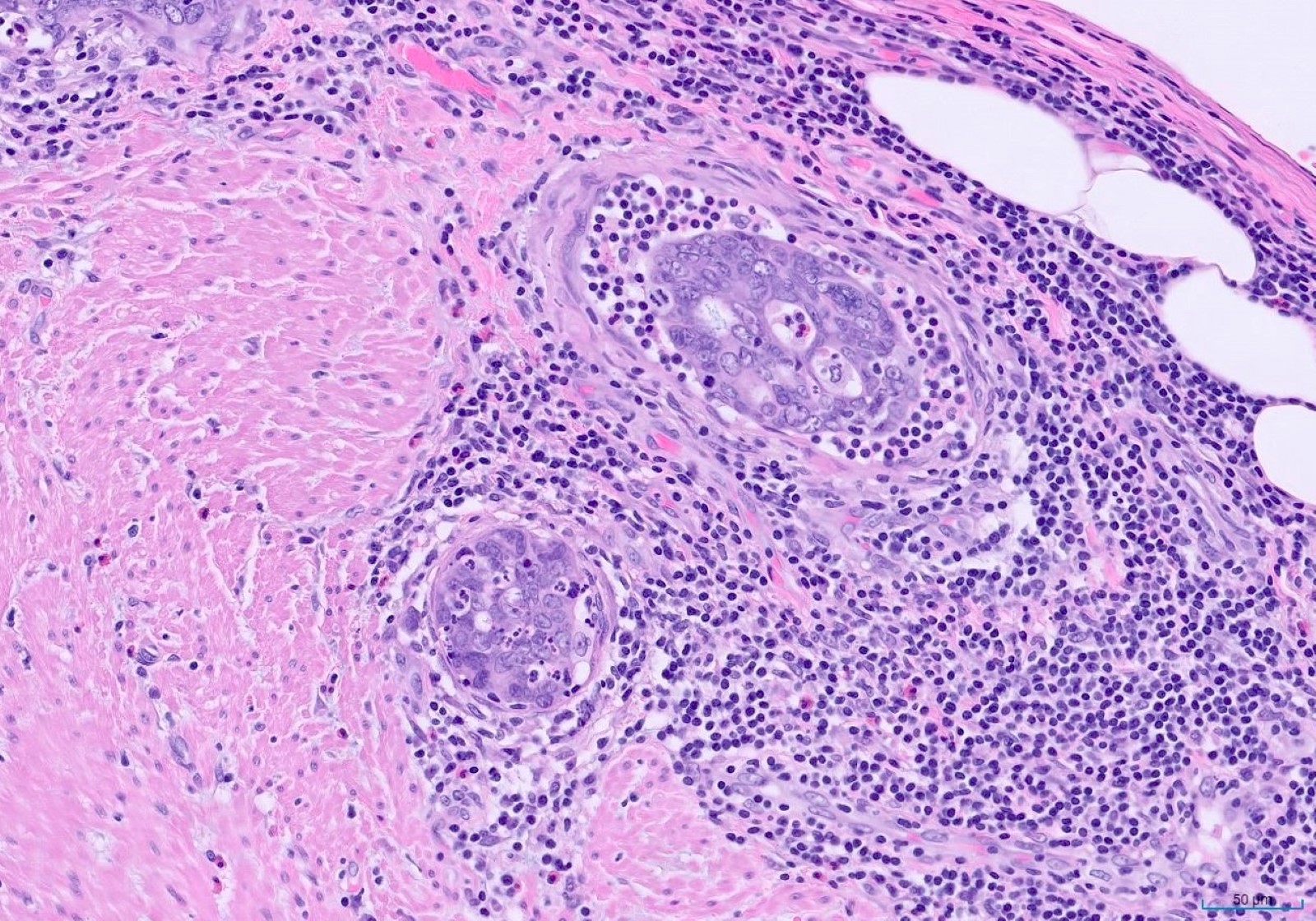
Microscopic (histologic) images
Negative stains
- CK7 variable, positive in 28 - 50% of cases (Crit Rev Clin Lab Sci 2021;58:369)
- PAX8, ER, CK14
Molecular / cytogenetics description
- Can harbor unique molecular profiling distinct from colorectal adenocarcinoma (Br J Cancer 2020;123:1262)
- KRAS, GNAS and TP53 frequently mutated (J Clin Oncol 2023;41:1553, Br J Cancer 2020;123:1262)
- Less frequent mutations: SMAD4, NRAS, ATM, SMAD2, TGFBR2, APC, RNF43, PIK3CA, SPX9, ARID1A, KMT2D; MYC amplification, CCND1 amplification (J Clin Oncol 2023;41:1553)
- Low prevalence of microsatellite instability (Br J Cancer 2020;123:1262)
Sample pathology report
- Appendix, appendectomy:
- Invasive, moderately to poorly differentiated adenocarcinoma of the proximal appendix, 1.0 cm in greatest dimension (see comment)
- Comment: The tumor arises in association with a tubular adenoma and invades transmurally to the visceral peritoneum (pT4a). Lymphovascular invasion is identified. Tumor deposits are identified (pN1c). There is no tumor or dysplasia present in the appendiceal resection margin. No lymph nodes are identified in the entirely submitted mesoappendiceal fibroadipose tissue.
- AJCC staging (8th edition): pT4a N1c Mx (stage group: IIIB)
Differential diagnosis
- Low grade or high grade appendiceal mucinous neoplasm:
- Low grade or high grade tumor showing pushing type invasion, with prominent fibrosis of the wall
- Goblet cell adenocarcinoma:
- Demonstrates a component of classical low grade goblet cell adenocarcinoma
- Cecal carcinoma extending into the base of appendix:
- Careful gross examination
- Microscopic examination of the precursor lesion may indicate the primary site of origin
Additional references
Board review style question #1
A 58 year old patient presents with acute right lower quadrant abdominal pain and is found to have an appendiceal mass during surgery. Histological examination of the resected specimen reveals a lesion as depicted in the images above. Which of the following is the correct diagnosis?
- High grade appendiceal mucinous neoplasm
- Low grade appendiceal mucinous neoplasm
- Mucinous appendiceal adenocarcinoma
- Signet ring cell adenocarcinoma
Board review style answer #1
C. Mucinous appendiceal adenocarcinoma. The tumor demonstrates infiltrative growth pattern with irregular glands and large mucin pools, adjacent to a low grade mucinous neoplasm. Answers A and B are incorrect because both low grade appendiceal mucinous neoplasm and high grade appendiceal mucinous neoplasm exhibit a pushing type of invasion, unlike the irregular infiltrative pattern seen here. Answer D is incorrect because signet ring cell adenocarcinoma should typically have a minimum of 50% of neoplastic cells displaying signet ring cell morphology.
Comment Here
Reference: Appendix - Adenocarcinoma
Comment Here
Reference: Appendix - Adenocarcinoma
Board review style question #2
You are reviewing a case of acute appendicitis and notice the findings in the images provided. Which of the following statements is true regarding this lesion?
- It is characterized by frequent microsatellite instability
- It is frequently positive for CK7 and negative for CK20
- It usually involves patients 30 - 50 years of age
- Signet ring cell type is associated with a worse prognosis
Board review style answer #2
D. Signet ring cell type is associated with a worse prognosis. The clinical and histological findings suggest appendiceal signet ring cell adenocarcinoma, which is associated with a worse prognosis compared to other types of appendiceal adenocarcinoma. Answer A is incorrect because appendiceal adenocarcinoma typically displays a low prevalence of microsatellite instability. Answer B is incorrect because appendiceal adenocarcinoma stains positive for CK20 but majority lacks CK7 expression. Answer C is incorrect because appendiceal adenocarcinomas usually occur in patients in their fifth to seventh decade of life.
Comment Here
Reference: Appendix - Adenocarcinoma
Comment Here
Reference: Appendix - Adenocarcinoma