Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Sagan OA, Huber AR. Syphilis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/anussyphilis.html. Accessed March 30th, 2025.
Definition / general
- Sexually transmitted infection caused by Treponema pallidum, a gram negative spirochete
- Can affect multiple sites, including the anus, with multiple stages of disease and nonspecific presentations (the great imitator, which is believed to have been coined by Sir William Osler) (Can Med Assoc J 1976;114:503)
Essential features
- Syphilis infections are caused by T. pallidum and are generally regarded as sexually transmitted infections that disproportionally affect men who have sex with men and non-Hispanic persons
- Most cases demonstrate a dense plasma cell inflammatory infiltrate on histology
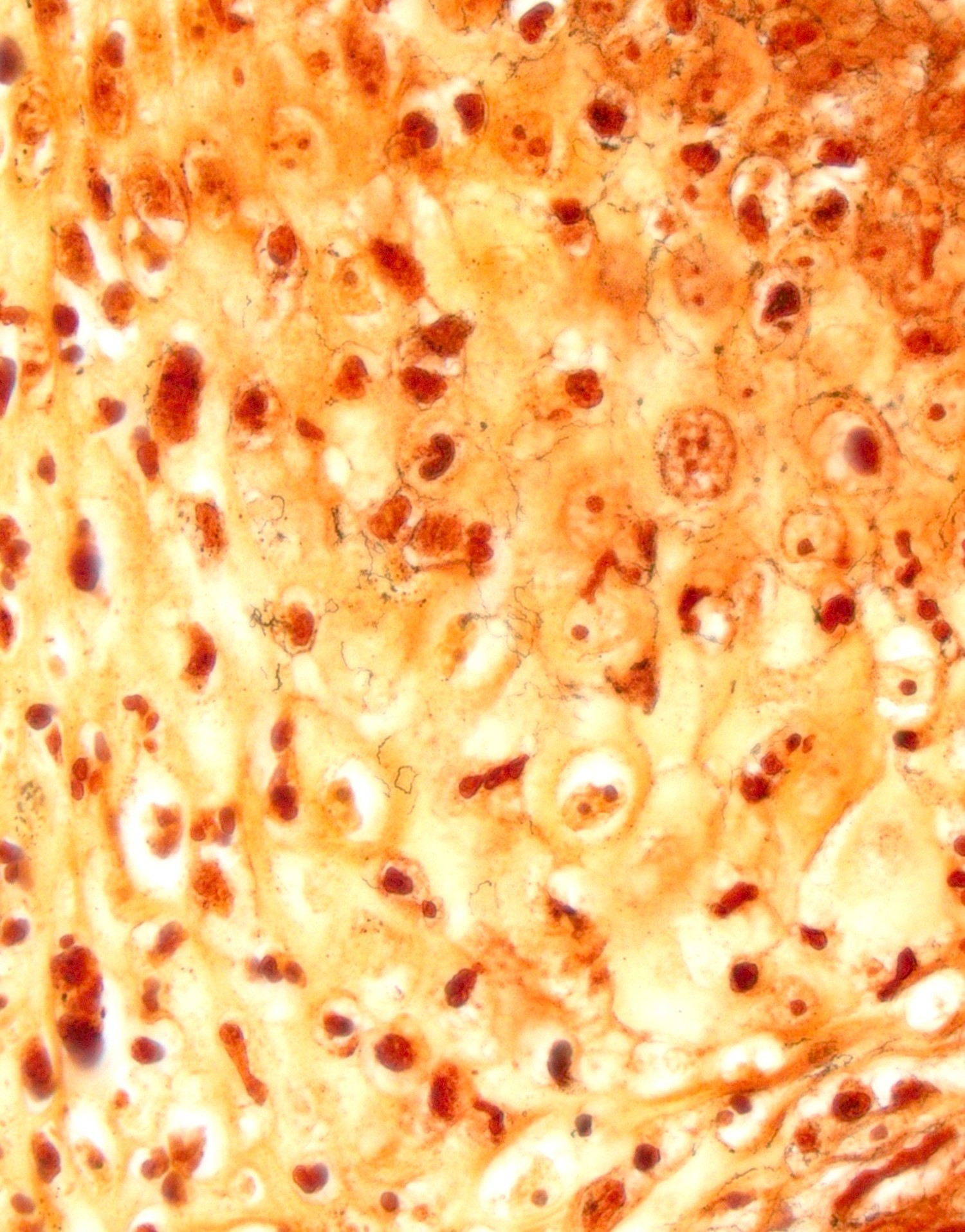
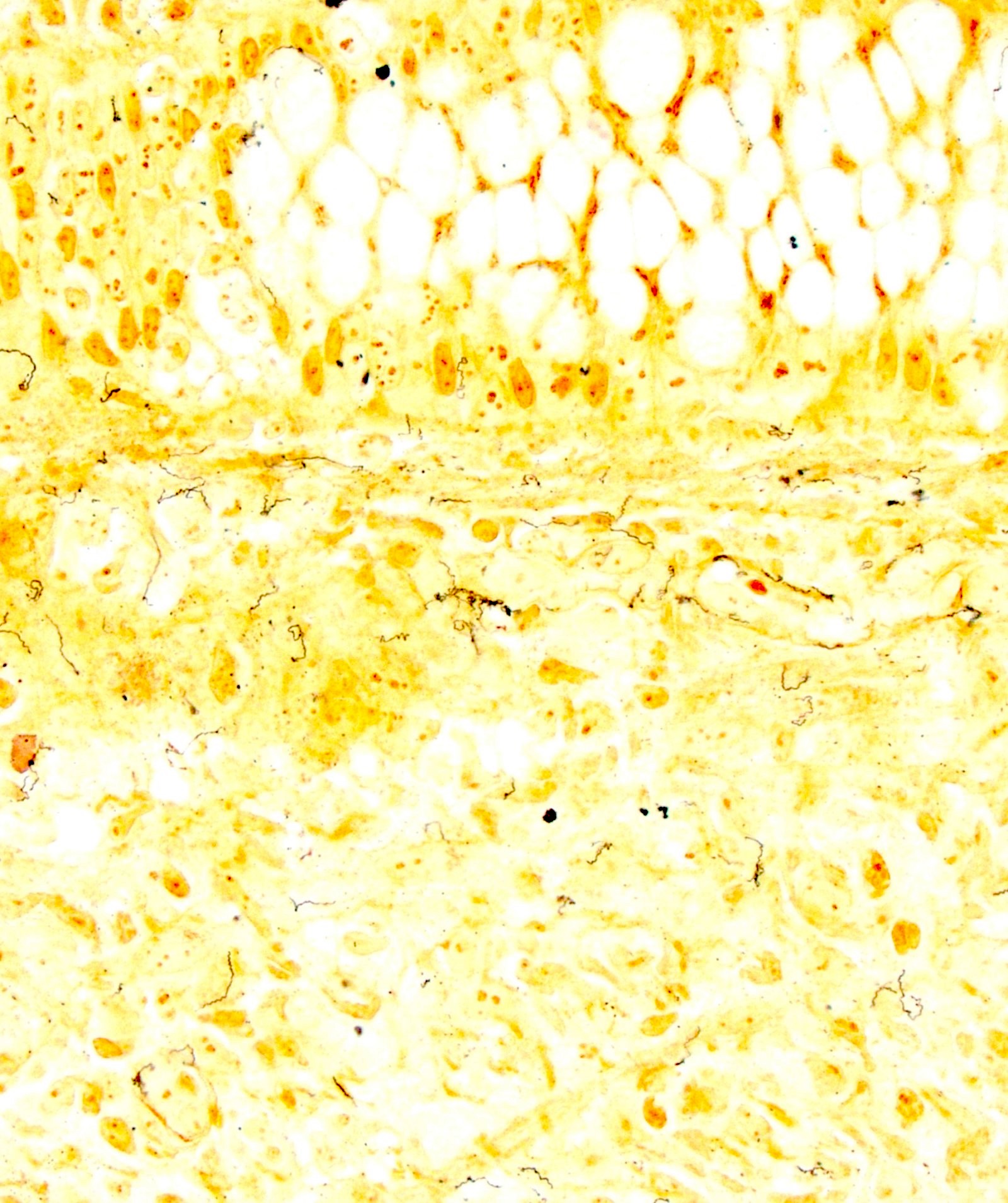
- T. pallidum IHC provides increased sensitivity and specificity over silver stains (Warthin-Starry or Steiner)
- Clinical and histopathologic features of all disease stages can be general and nonspecific, so appropriate clinical and pathologic work up should be done in all cases in which syphilis is suspected
ICD coding
Epidemiology
- World Health Organization (WHO) estimated 7.1 million new adult cases of syphilis worldwide in 2020 with increasing incidence in the United States (WHO: Syphilis [Accessed 22 September 2023], CDC: Sexually Transmitted Disease Surveillance 2021 [Accessed 22 September 2023])
- Men who have sex with men and non-Hispanic persons are disproportionately affected (CDC: Sexually Transmitted Disease Surveillance 2021 [Accessed 22 September 2023])
- Dual diagnosis with HIV is common and syphilis increases the risk of acquiring HIV as well as other sexually transmitted infections
- Majority of cases are transmitted through vaginal, anogenital and orogenital contact with an infectious lesion during the primary or secondary stages of the disease
- Rarely can be transmitted through nonsexual contact including skin to skin and blood transfusion
- Congenital syphilis can be acquired, at any stage, via transplacental transmission or contact with an infectious lesion during birth (N Engl J Med 2020;382:845)
Sites
Pathophysiology
- Syphilis is primarily transmitted through contact with infectious lesions and disseminates through the blood stream and lymphatics within days, ultimately invading distant tissues (N Engl J Med 2020;382:845)
Etiology
- Sexually transmitted infection caused by Treponema pallidum, a gram negative spirochete
Clinical features
- Primary syphilis
- Single firm, round, painless sore called a chancre at the site of original infection
- Persists for 3 - 6 weeks before spontaneously resolving
- Secondary syphilis
- Maculopapular, nonpruritic rash, typically on the palms and soles
- Large white or gray raised lesions (condyloma lata), commonly on the perineum, which can ulcerate
- Fever, lymphadenopathy, patchy alopecia, weight loss, muscle aches and fatigue are also common
- Latent phase
- No clinical symptoms
- Can last for years
- Tertiary syphilis
- Can affect multiple organ systems, commonly causing destructive visceral, cardiovascular or neurological disorders as well as severe skin lesions (gummas)
- Can appear 10 - 30 years after initial infection
- Can be fatal
- References: CDC: Sexually Transmitted Diseases (STDs) - Syphilis - CDC Detailed Fact Sheet [Accessed 22 September 2023], WHO: Syphilis [Accessed 22 September 2023], Front Cell Infect Microbiol 2021;10:574806, N Engl J Med 2020;382:845
Diagnosis
- Diagnosis relies on history, physical examination and interpretation of laboratory tests (Front Cell Infect Microbiol 2021;10:574806)
- Definitive diagnosis methods for early stages of syphilis include (CDC: Sexually Transmitted Infections Treatment Guidelines, 2021 - Syphilis [Accessed 22 September 2023])
- Direct visualization of T. pallidum through darkfield microscopy
- Molecular tests detecting T. pallidum from lesion exudate or tissue, including PCR
- Darkfield microscopy is not a recommended technique for identification of T. pallidum in the gastrointestinal tract due to not being able to exclude commensal gut treponemes (Open Forum Infect Dis 2021;8:ofab157)
- Presumptive diagnosis of syphilis requires use of 2 laboratory serologic tests: both a nontreponemal test and treponemal test (CDC: Sexually Transmitted Infections Treatment Guidelines, 2021 - Syphilis [Accessed 22 September 2023])
Laboratory
- Nontreponemal tests include
- Venereal Disease Research Laboratory (VDRL)
- Rapid plasma reagin (RPR) test
- Generally used as screening tests
- Treponemal tests include
- T. pallidum passive particle agglutination (TPPA) assay
- Enzyme immunoassays (EIAs)
- Chemiluminescence immunoassays (CIAs) and immunoblots
- Rapid treponemal assays
- Treponemal antibodies appear earlier than nontreponemal antibodies and usually remain detectable for life, even after successful treatment
- Reference: CDC: Sexually Transmitted Infections Treatment Guidelines, 2021 - Syphilis [Accessed 22 September 2023]
Prognostic factors
- Favorable prognosis with early detection and appropriate treatment
- High risk sexual activity is the strongest risk factor for repeat infection (Open Forum Infect Dis 2020;7:ofaa019)
Case reports
- Man in his early 20s with perianal lesions (Aust Fam Physician 2016;45:209)
- 31, 44, 51 and 52 year old men with anal ulcers (Arch Pathol Lab Med 2015;139:1156)
- 35 year old woman with HIV and exophytic vulvar and perianal lesions (Gynecol Oncol Rep 2023;46:101158)
- 37 year old man with HIV and anal ulcer (Perm J 2018;22:17)
- 47 year old man with ulcerated mass at anorectal junction (BMJ Case Rep 2019;12:e226595)
Treatment
- Penicillin is the gold standard of treatment
- Type, dose and duration depends on disease stage
- Pregnant patients allergic to penicillin should be desensitized before receiving penicillin treatment
- Doxycycline, tetracycline and potentially ceftriaxone can be used in nonpregnant patients allergic to penicillin
- Condoms and other types of barrier protection can help prevent disease
- Reference: CDC: Sexually Transmitted Diseases (STDs) - Syphilis - CDC Detailed Fact Sheet [Accessed 22 September 2023]
Clinical images
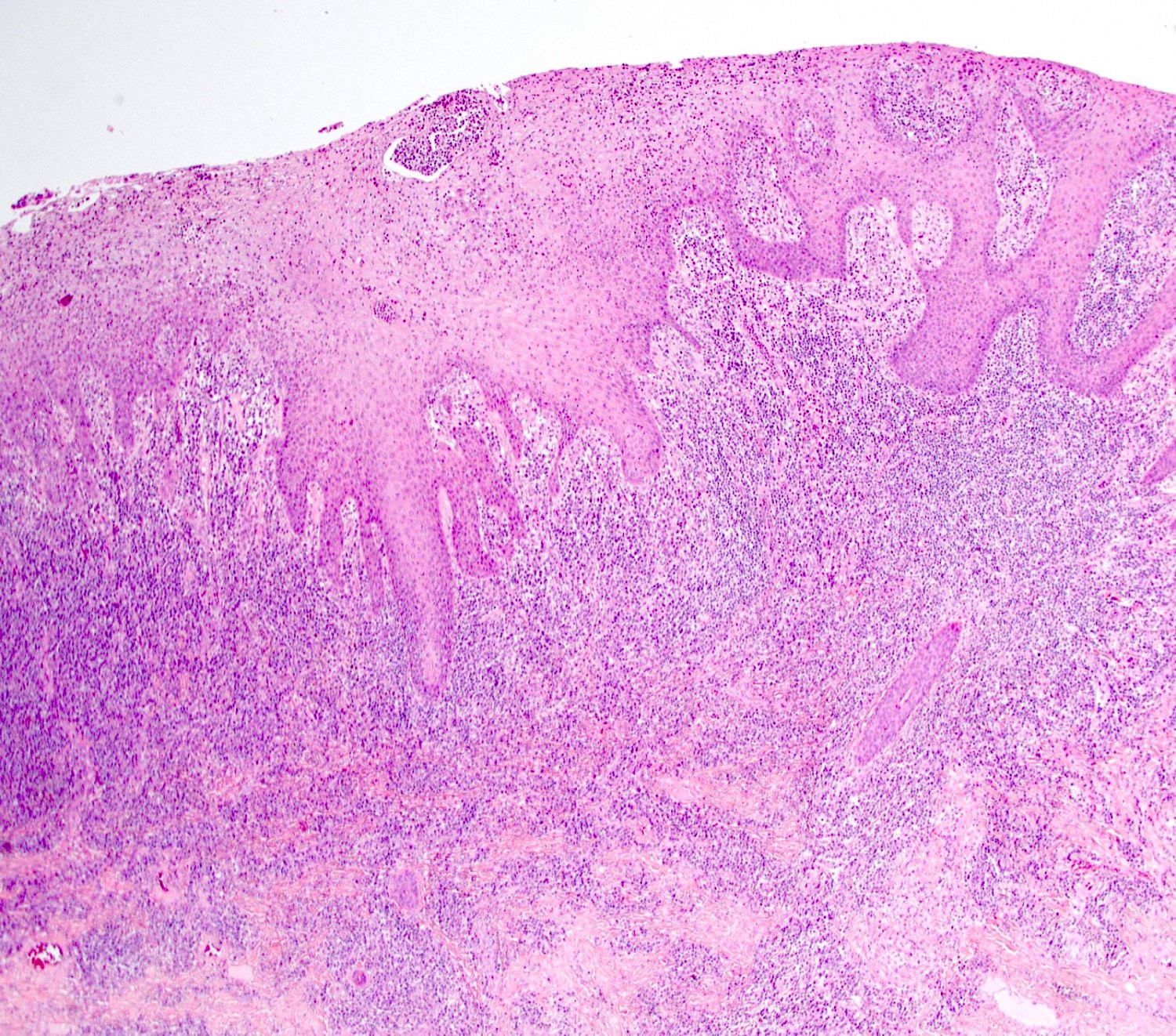
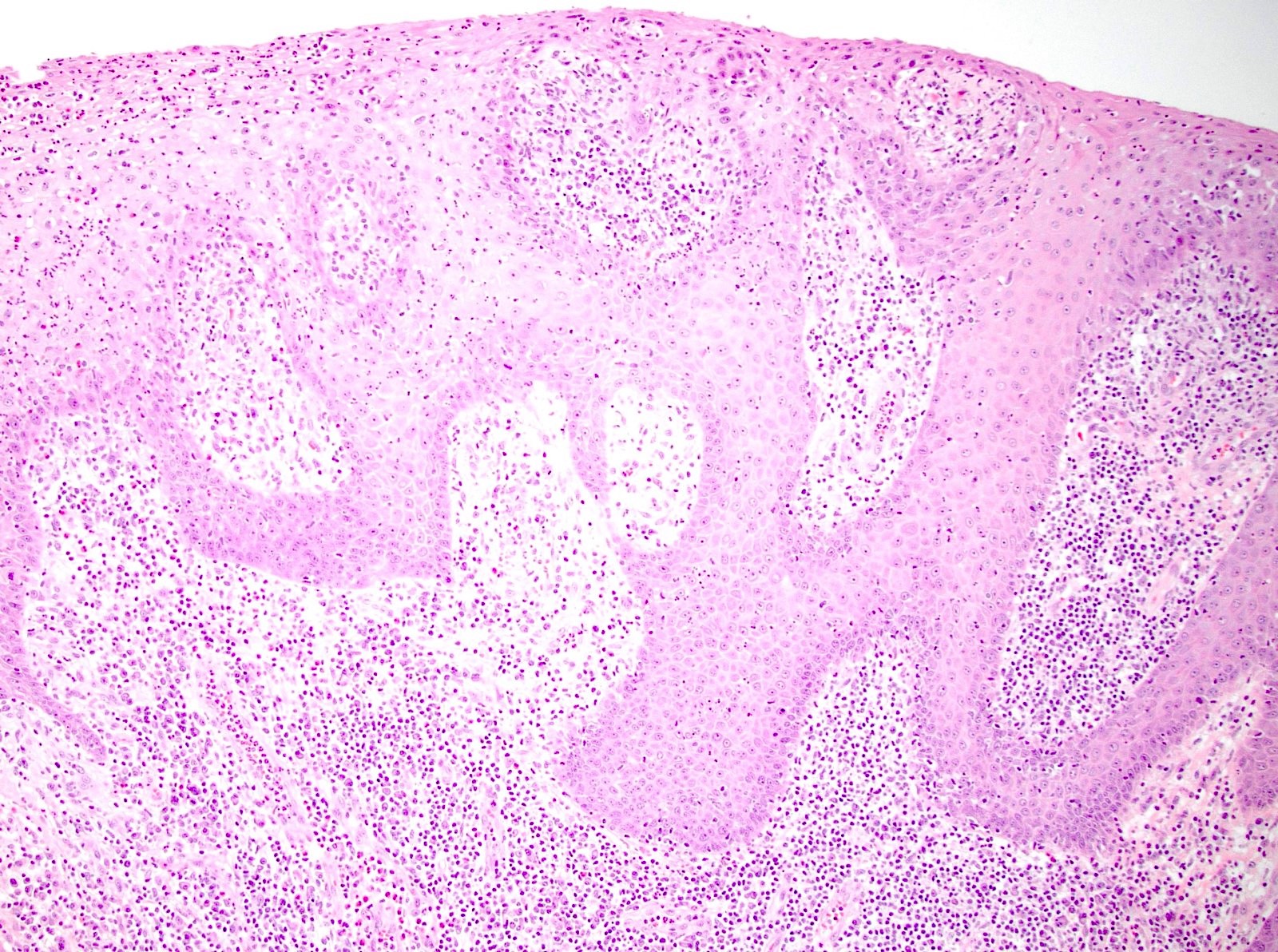
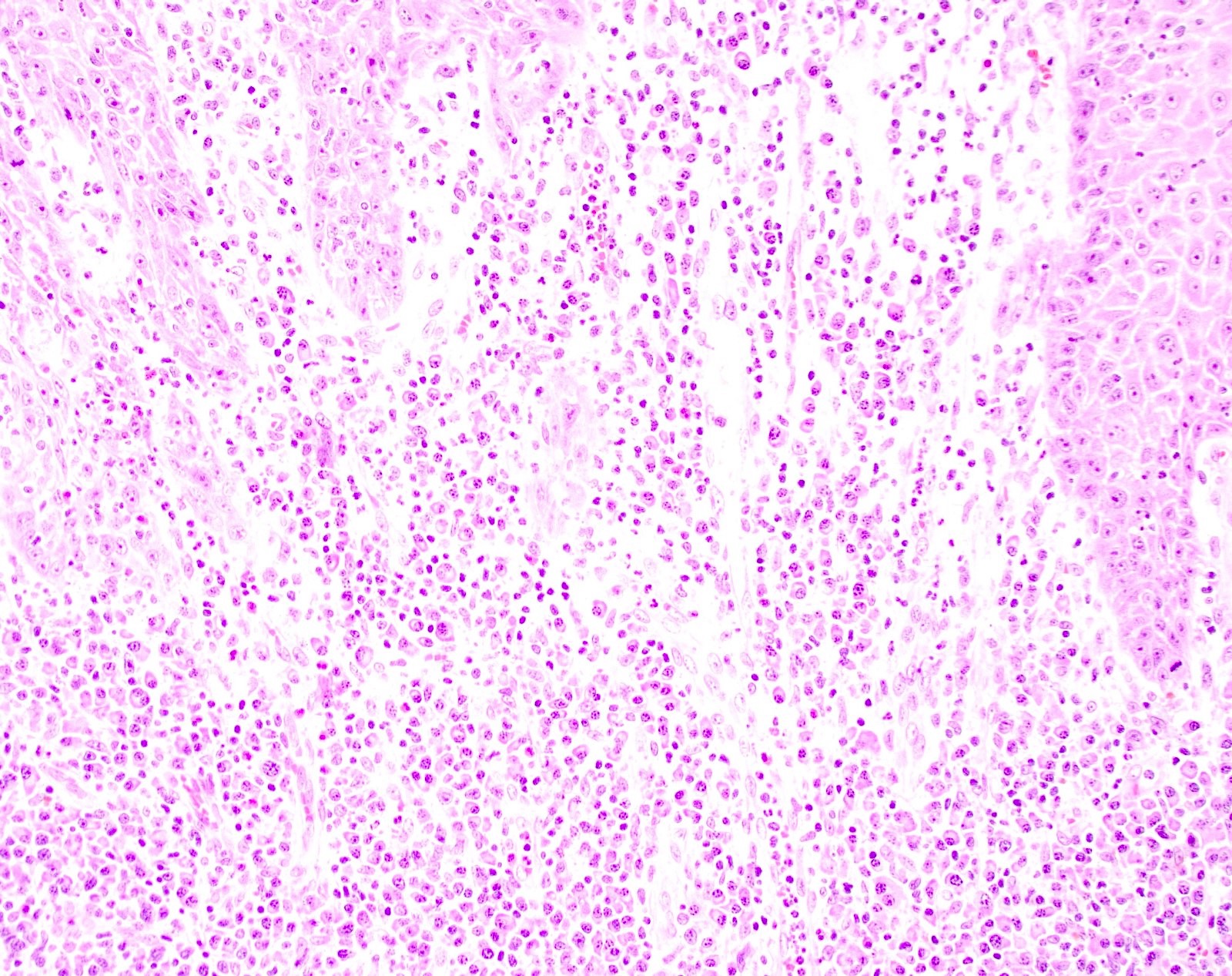
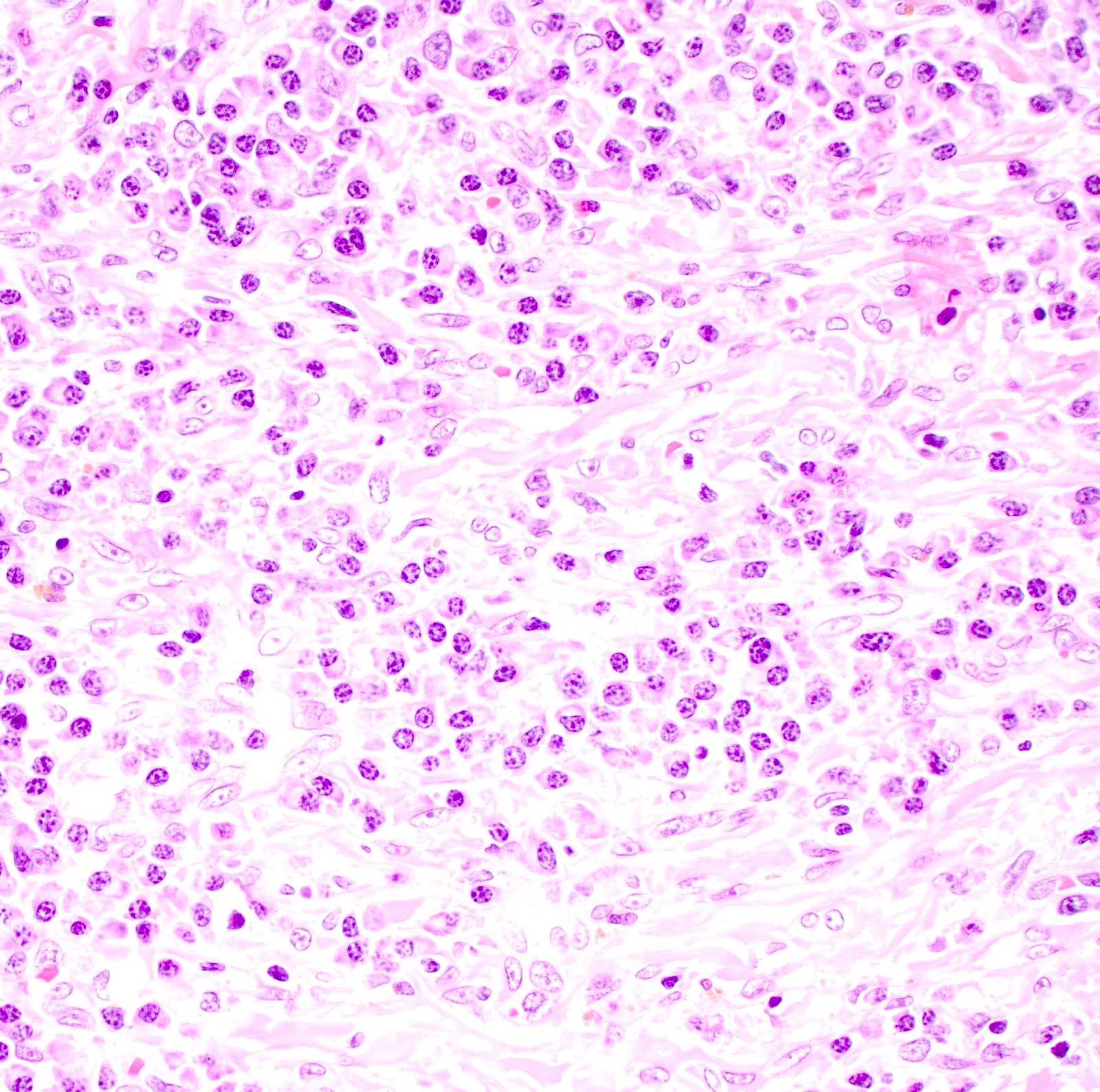
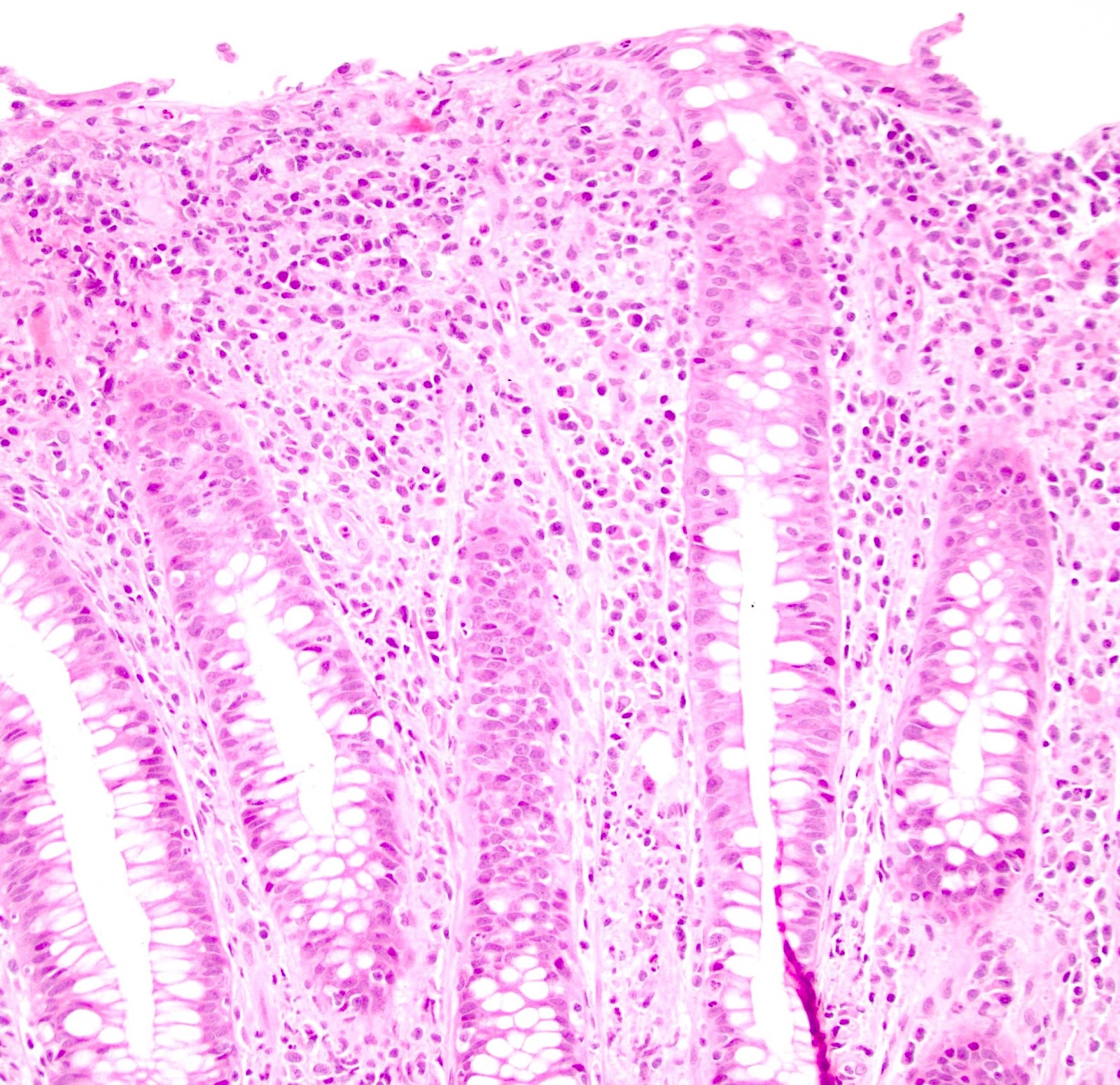
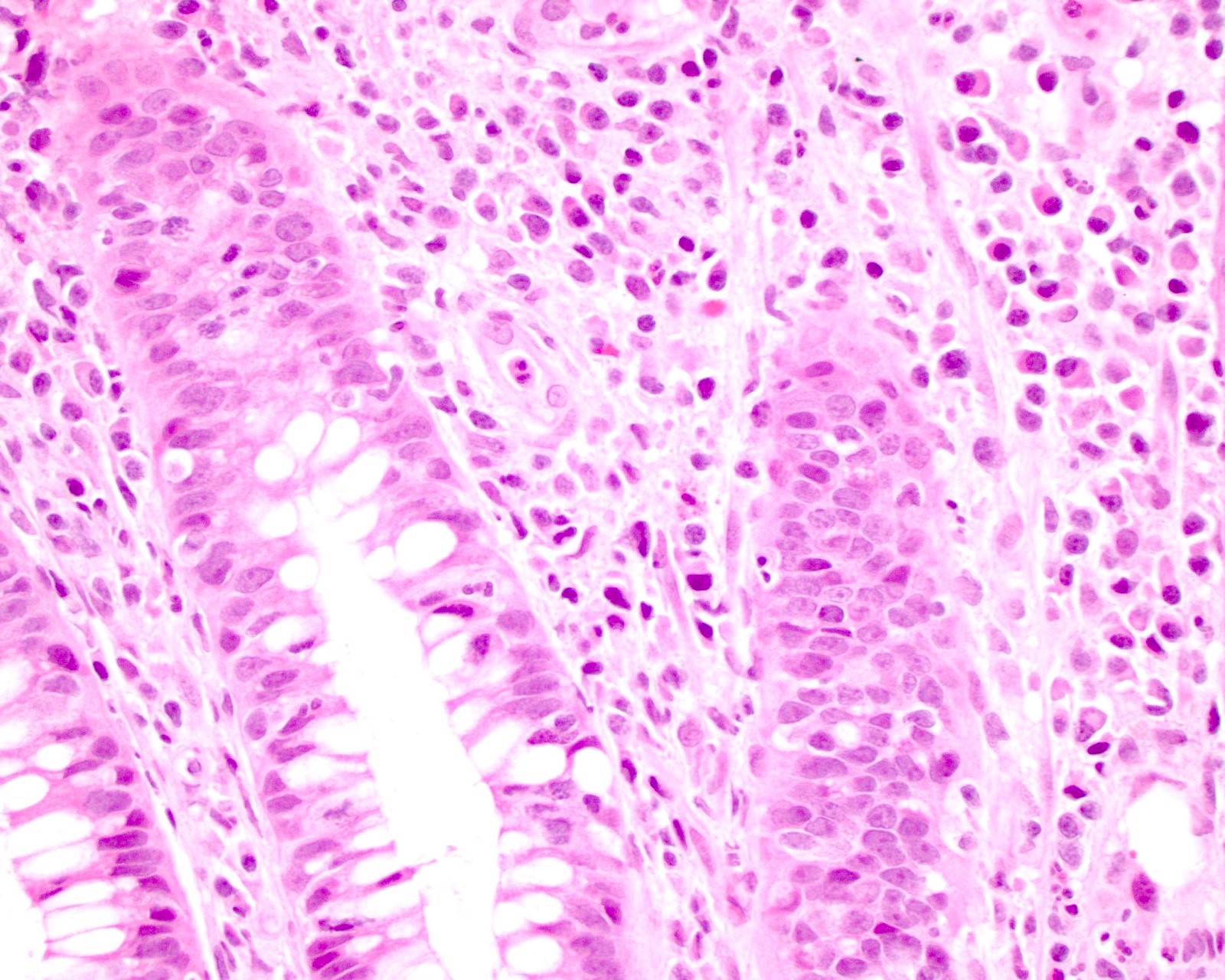
Microscopic (histologic) description
- Largely nonspecific on H&E sections
- While plasma cells can be present in all stages of the disease, plasma cells may be absent in some cases (Am J Surg Pathol 2018;42:472)
- Primary / chancre
- Ulcer with intense plasma cell infiltrate with scattered macrophages and lymphocytes
- Obliterative endarteritis with endothelial cell proliferation that progresses to intimal fibrosis
- Regional lymph nodes are enlarged due to nonspecific acute or chronic lymphadenitis, plasma cell rich infiltrates or granulomas
- Secondary / condyloma lata
- Epithelial hyperplasia
- Plasma cell infiltrate with scattered macrophages and lymphocytes that can be less intense than primary syphilis
- Obliterative endarteritis with endothelial cell proliferation that progresses to intimal fibrosis
- Ulceration may be present
- Tertiary / gummas
- Centers of coagulative necrosis
- Edges of the lesion comprise of palisading macrophages and fibroblasts surrounded by a large amount of inflammatory cells that are mostly plasma cells
- T. pallidum is hard to visualize in these lesions, even with stains and IHC
- Reference: Int J Surg Case Rep 2015;17:69
Microscopic (histologic) images
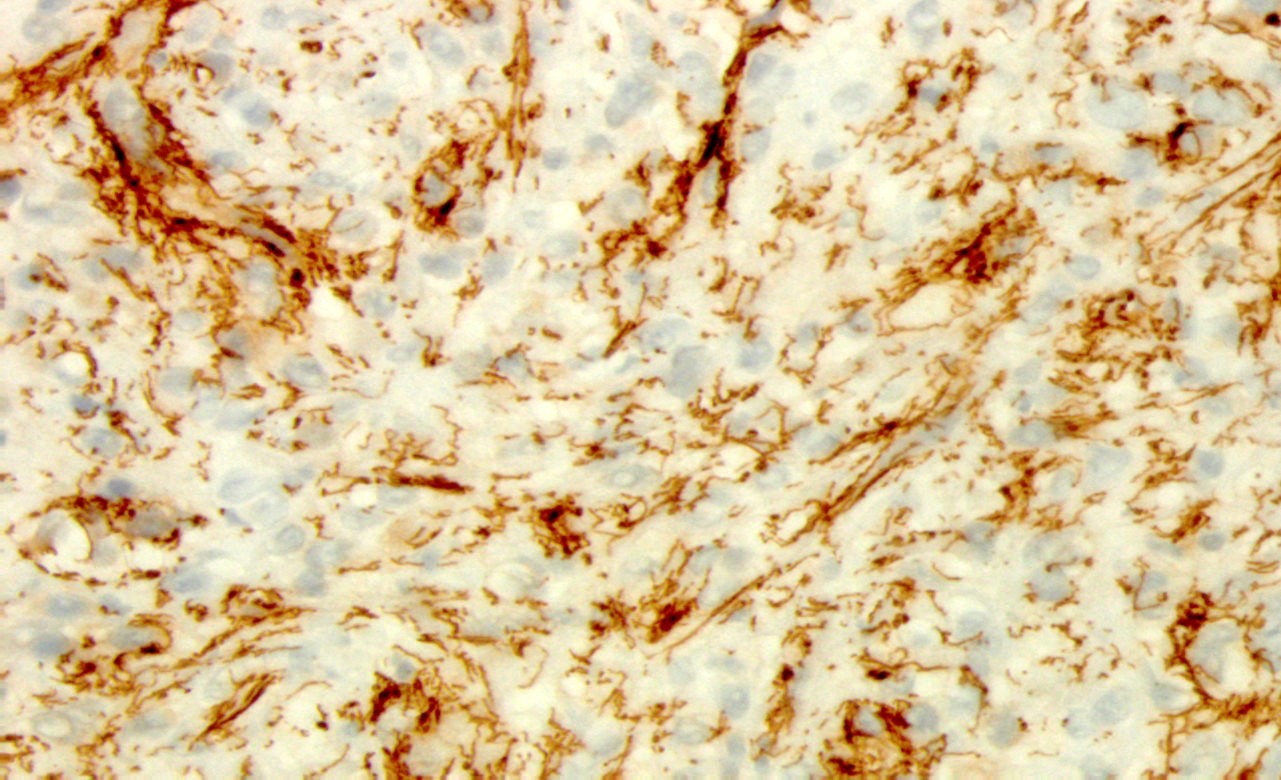
Positive stains
- Silver stains (Warthin-Starry or Steiner) were historically used
- T. pallidum IHC provides increased sensitivity and specificity (Front Cell Infect Microbiol 2021;10:574806)
Videos
Perianal condyloma lata
Syphilis stains and IHC
Sample pathology report
- Skin, perianal, biopsy:
- Spirochetes present on silver stain and T. pallidum immunostain, consistent with syphilis (see comment)
- Comment: Serologic and clinical correlation is recommended.
Differential diagnosis
- Anal squamous cell carcinoma:
- Condyloma accuminata:
- Caused by HPV serotypes 6 and 11
- Hyperplastic papillary exophytic squamous epithelium
- Koilocytes in upper third of epithelium
- No plasmacytic inflammation
- p63 and low risk HPV ISH positive
- Negative T. pallidum testing
- Chancroid:
- Caused by Haemophilus ducreyi
- Painful genital ulcer associated with tender suppurative inguinal adenopathy
- Negative T. pallidum testing
- Granuloma inguinale:
- Caused by Klebsiella granulomatis
- Multiple ulcers
- Granulomatous inflammation
- Large vacuolated, foamy macrophages and histiocytes with multiple intracytoplasmic organisms (Donovan bodies)
- Negative T. pallidum testing
- Lymphogranuloma venereum:
- Caused by Chlamydia trachomatis
- Nonspecific features of ulceration and granulation tissue in dermis
- Suppurative inflammation of inguinal lymph nodes
- Negative T. pallidum testing
- Ulcerative colitis:
- Continuous pattern of ulceration progressing proximally from the rectum
- Cryptitis or crypt abscesses if active
- Crohn's disease:
- Transmural inflammation
- Cryptitis or crypt abscesses if active
- Nonnecrotizing granulomas
- Herpes simplex virus (HSV):
- Ulceration with multinucleated giant cells and nuclear inclusions
- Positive HSV DNA PCR
- Negative T. pallidum testing
- IgG4 related disease:
- Elevated total serum IgG or IgG4 levels
- Can have multiple masses in multiple different organs
- Negative T. pallidum testing
- Anal tuberculosis (TB):
- Very rare manifestation of TB
- Variety of morphologies with ulcerative being the most common (IDCases 2018;12:25)
- Chronic granulomatous inflammation
- AFB positive
- Negative T. pallidum testing
- Lymphoma:
- Atypical population of lymphocytes
- Syphilis lesions will show T cell predominate infiltrate with admixed polytypic B cells, typical of a reactive process (Am J Surg Pathol 2018;42:472)
Additional references
Board review style question #1
A 27 year old man presented with a diffuse maculopapular rash, including on his palms and soles and a 4 cm white-gray raised perianal lesion. A biopsy was done of the perianal lesions and the histology is depicted in the H&E image. Which further testing should be ordered on the biopsy to best help determine the diagnosis?
- AFB stain
- IgG4 IHC
- p63 IHC
- T. pallidum IHC
- Warthin-Starry silver stain
Board review style answer #1
D. T. pallidum IHC. The H&E image demonstrates epithelial hyperplasia with a dense subepithelial plasmacytic infiltrate indicative of condyloma lata. T. pallidum IHC is the most sensitive and specific method to highlight the spirochetes within the tissue.
Answer E is incorrect because while the Warthin-Starry silver stain may also be used to highlight T. pallidum, it is not as sensitive or specific as IHC for T. pallidum.
Answer A is incorrect because an AFB stain should be done when chronic granulomatous inflammation is seen to rule out anal tuberculosis.
Answer C is incorrect because p63 IHC is positive in condyloma accuminata, which will demonstrate koilocytes and should not have any plasmacytic inflammation.
Answer B is incorrect because IgG4 related disease presents with masses and does not present with a rash. The plasma cells in condyloma lata should also be negative for IgG4 IHC.
Comment Here
Reference: Anus & perianal area - Syphilis
Comment Here
Reference: Anus & perianal area - Syphilis
Board review style question #2
What histologic feature separates primary syphilis (chancre) from secondary syphilis (condyloma lata)?
- Coagulative necrosis
- Epithelial hyperplasia
- Granulomas
- Obliterative endarteritis
Board review style answer #2
B. Epithelial hyperplasia is seen with secondary syphilis lesions (condyloma lata) but not with primary syphilis lesions (chancre), in which ulceration is more common.
Answer C is incorrect because granulomas are not specific for any stage of syphilis nor specific for syphilis.
Answer A is incorrect because coagulative necrosis is seen in tertiary syphilis lesions (gummas) but not in chancres or condyloma lata.
Answer D is incorrect because obliterative endarteritis can be seen in both primary and secondary syphilis.
Comment Here
Reference: Anus & perianal area - Syphilis
Comment Here
Reference: Anus & perianal area - Syphilis