Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Pathophysiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Gonzalez RS. Squamous cell carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/anusscc.html. Accessed April 1st, 2025.
Definition / general
- Primary squamous cell carcinoma of the anus
Essential features
- Most common carcinoma of the anal tract
- Increasing in incidence, although still relatively rare (incidence of < 1 per 100,000)
- Can arise either above or below the dentate line
Terminology
- WHO officially only recognizes squamous cell carcinoma
- Basaloid variant has also been termed cloacogenic or transitional
- Mucoepidermoid carcinoma may be used for tumors with prominent mucinous features, although the biology may be different (J Gastroenterol 2001;36:508)
ICD coding
- ICD-10: C44.520 - squamous cell carcinoma of anal skin
Epidemiology
- Tumors above dentate line: more common in women; usually diagnosed in sixth decade
- Tumors below dentate line: more common in men; usually diagnosed in third decade
Pathophysiology
- Tumors below the dentate line usually have an associated finding (condyloma, fistula, radiation, etc.)
- Can be caused by high risk HPV (Cancer Res 1999;59:753)
- EGFR overexpression is common (Mod Pathol 2006;19:942)
Clinical features
- Presenting symptoms include rectal bleeding, pain, mass
Diagnosis
- Tissue sampling
Radiology description
- MRI is the preferred imaging modality for staging purposes (Korean J Radiol 2017;18:946)
- On T2 weighted images: higher signal intensity than skeletal muscles but lower than ischioanal fat
- Markedly enhanced after injection of gadolinum contrast
Prognostic factors
- Prognosis depends on AJCC stage of tumor
- Distal tumors have a better prognosis (slower growth, earlier detection)
- Better prognosis with higher radiation dose and no / shorter treatment interruptions (Gastrointest Cancer Res 2008;2:10)
- Worse prognosis if older, male or with HIV (Dis Colon Rectum 2009;52:624, Dis Colon Rectum 2001;44:1496)
- HPV and p53 status can stratify prognosis (worst prognosis: HPV negative, p53 aberrant staining) (Mod Pathol 2021;34:1017)
Case reports
- 45 year old man with perianal mass (Int J Surg Case Rep 2021;81:105739)
- 62 year old woman with firm anal mass (Surg Case Rep 2022;8:119)
- 63 year old woman with brain metastases (J Neurooncol 2011;101:141)
Treatment
- Surgery with chemoradiation
Gross description
- Anal canal tumors are nodular, ulcerated, ≥ 3 - 4 cm
- Invade deeply into wall and spread proximally and distally into submucosa of the distal rectum and proximal anus
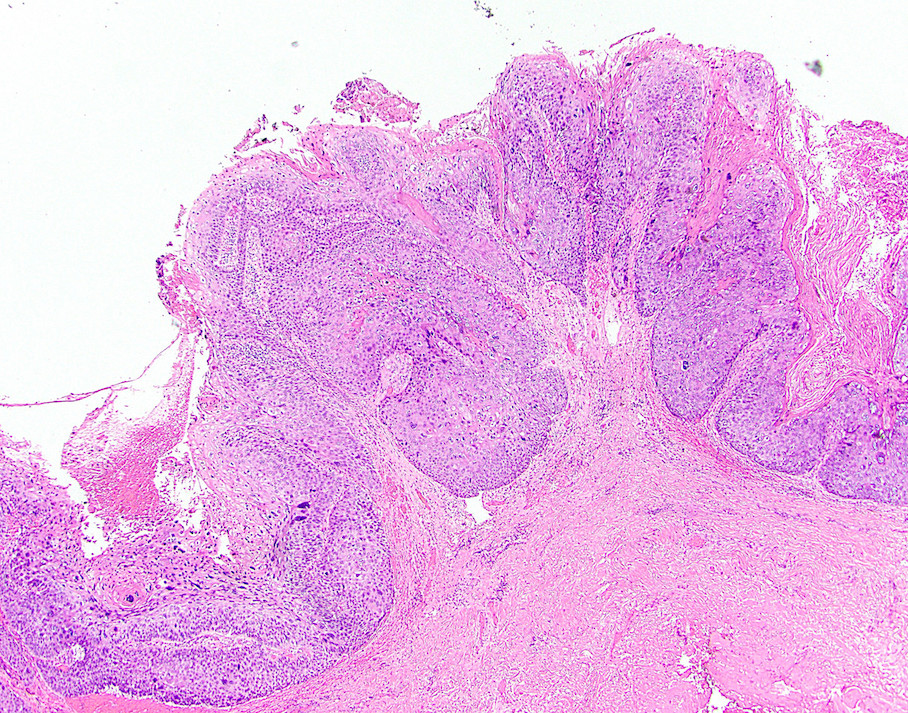
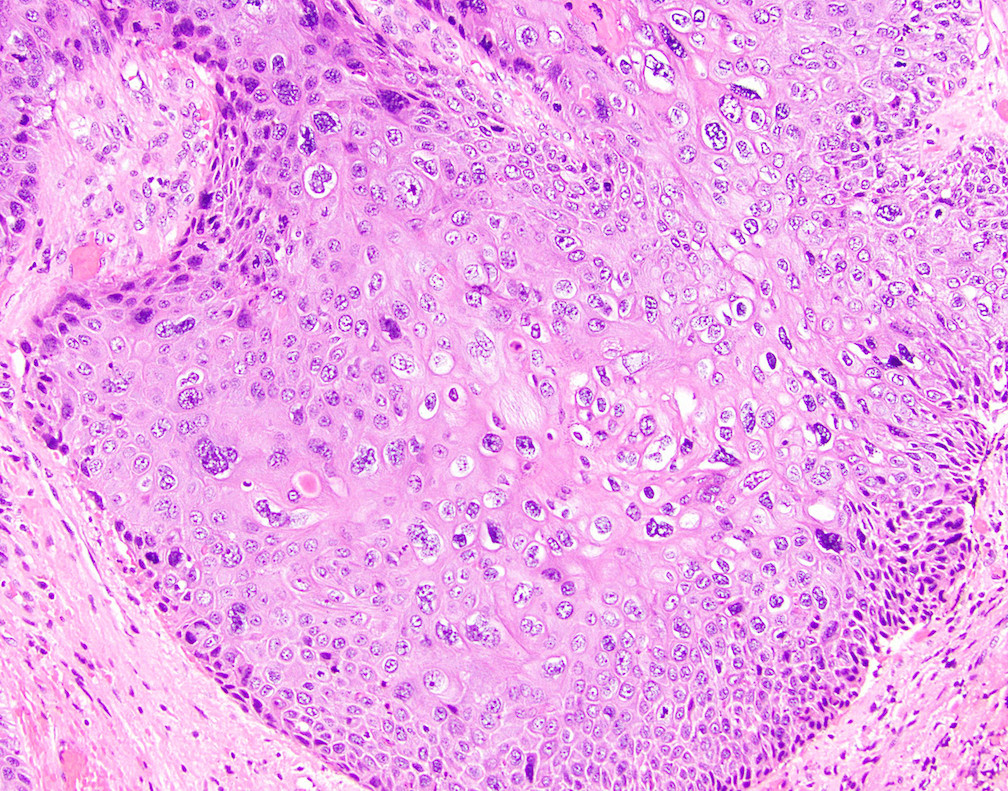
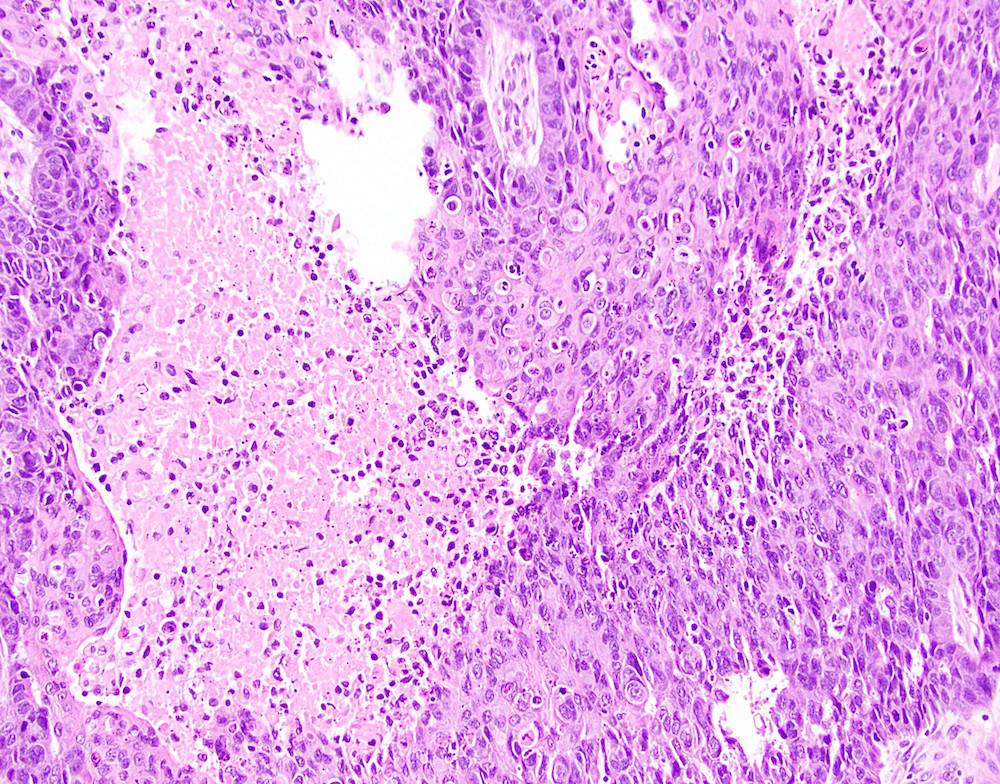
Microscopic (histologic) description
- Resembles squamous cell carcinoma as seen elsewhere in body
- Tumors often display multiple morphologic patterns, calling into question the utility of subdividing the entity
- May be keratinizing (usually below the dentate line) or nonkeratinizing (anywhere, although tumors above the dentate line are usually nonkeratinizing)
- Uncommon basaloid subtype shows plexiform pattern and palisading of small undifferentiated cells around the border, with central necrosis of tumor nodules (also mitotic figures, invasion, desmoplastic stroma) (Am J Surg Pathol 2016;40:354)
- May have massive eosinophilic infiltration, mucoepidermoid features (with mucinous microcysts) or poorly differentiated morphology
- Can show small cell anaplastic features (but without evidence of neuroendocrine differentiation)
- Often replaces crypts of adjacent rectal mucosa
- May show overlying / adjacent dysplastic changes (anal intraepithelial neoplasia)
Microscopic (histologic) images
Positive stains
Molecular / cytogenetics description
- May have mutations in PIK3CA, FBXW7, TP53, CDKN2A (Mod Pathol 2021;34:1017)
Sample pathology report
- Anus, mass, biopsy:
- Focal invasive squamous cell carcinoma, arising in a background of high grade squamous intraepithelial lesion (AIN 3)
- Anus, resection:
- Squamous cell carcinoma, moderately differentiated (see synoptic report)
Differential diagnosis
- Basal cell carcinoma:
- Fewer mitotic figures, smaller cells, retraction artifact
- Small cell carcinoma:
- Can resemble basaloid squamous cell carcinoma but expresses neuroendocrine markers
- Verrucous carcinoma:
- Grows in an exophytic, not infiltrative, pattern
Board review style question #1
Board review style answer #1
C. Patients with HIV have a worse prognosis. Poor prognostic factors in anal squamous cell carcinoma include older age, male sex and HIV positivity. Cases above the dentate line are more common in older women and cases below the dentate line are more common in younger men. Most cases are squamous cell carcinoma, NOS; basaloid examples are uncommon.
Comment Here
Reference: Squamous cell carcinoma
Comment Here
Reference: Squamous cell carcinoma
Board review style question #2
Which of the following etiologic subtypes of anal squamous cell carcinoma has the worst prognosis?
- HPV negative, p53 aberrant staining
- HPV negative, p53 wild type staining
- HPV positive, p53 aberrant staining
- HPV positive, p53 wild type staining
Board review style answer #2
A. HPV negative, p53 aberrant staining. Patients with this subtype have the worst prognosis. HPV positive cancers with p53 wild type staining confer the best prognosis and the other choices have an intermediate prognosis.
Comment Here
Reference: Squamous cell carcinoma
Comment Here
Reference: Squamous cell carcinoma