Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Sagan OA, Huber AR. Melanoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/anusmelanoma.html. Accessed January 17th, 2025.
Definition / general
- Rare primary malignant melanocytic neoplasm of the anal mucosa
Essential features
- Rare primary malignant melanocytic neoplasm of the anal mucosa, most common in White and female patients in the sixth decade of life
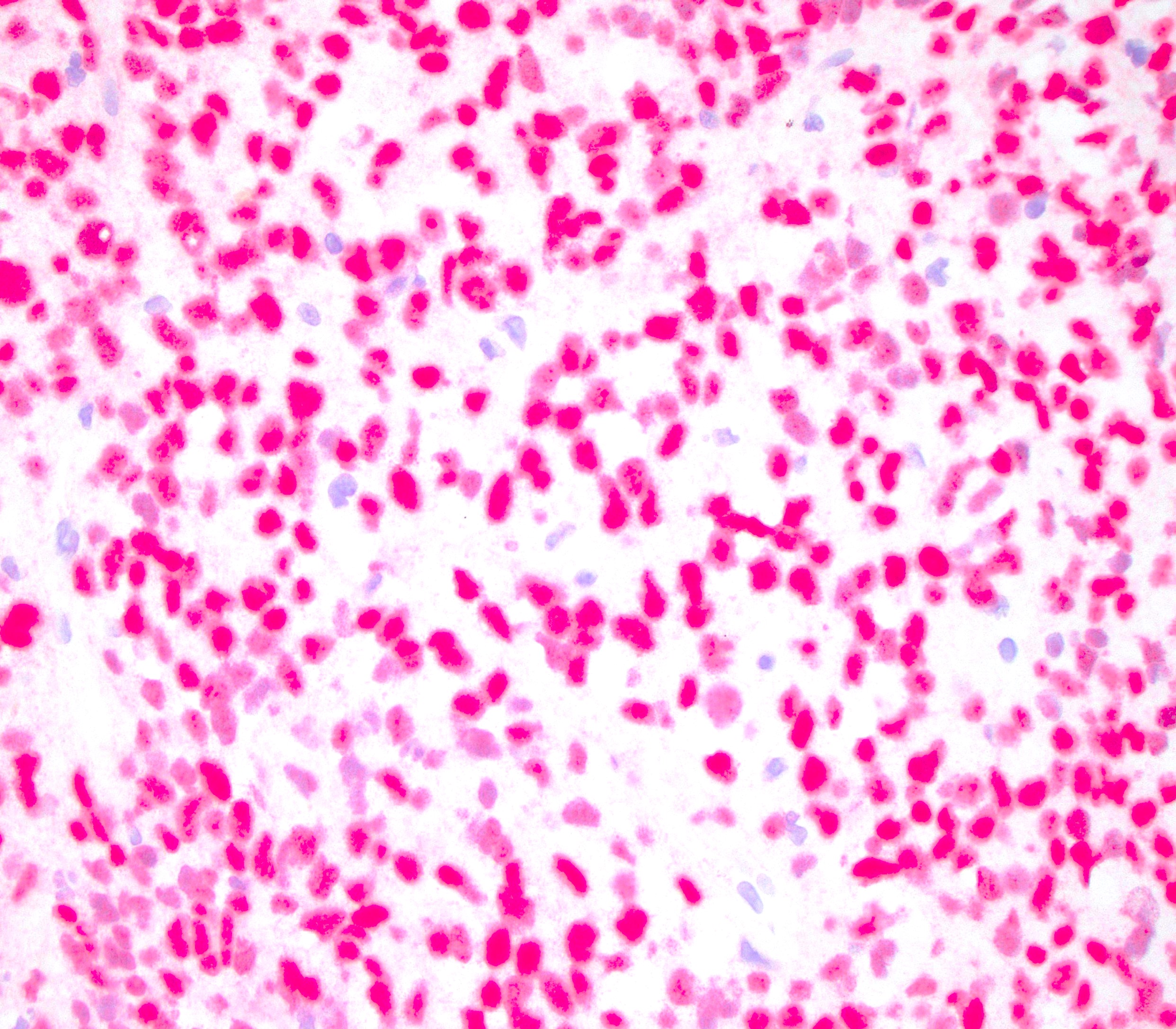
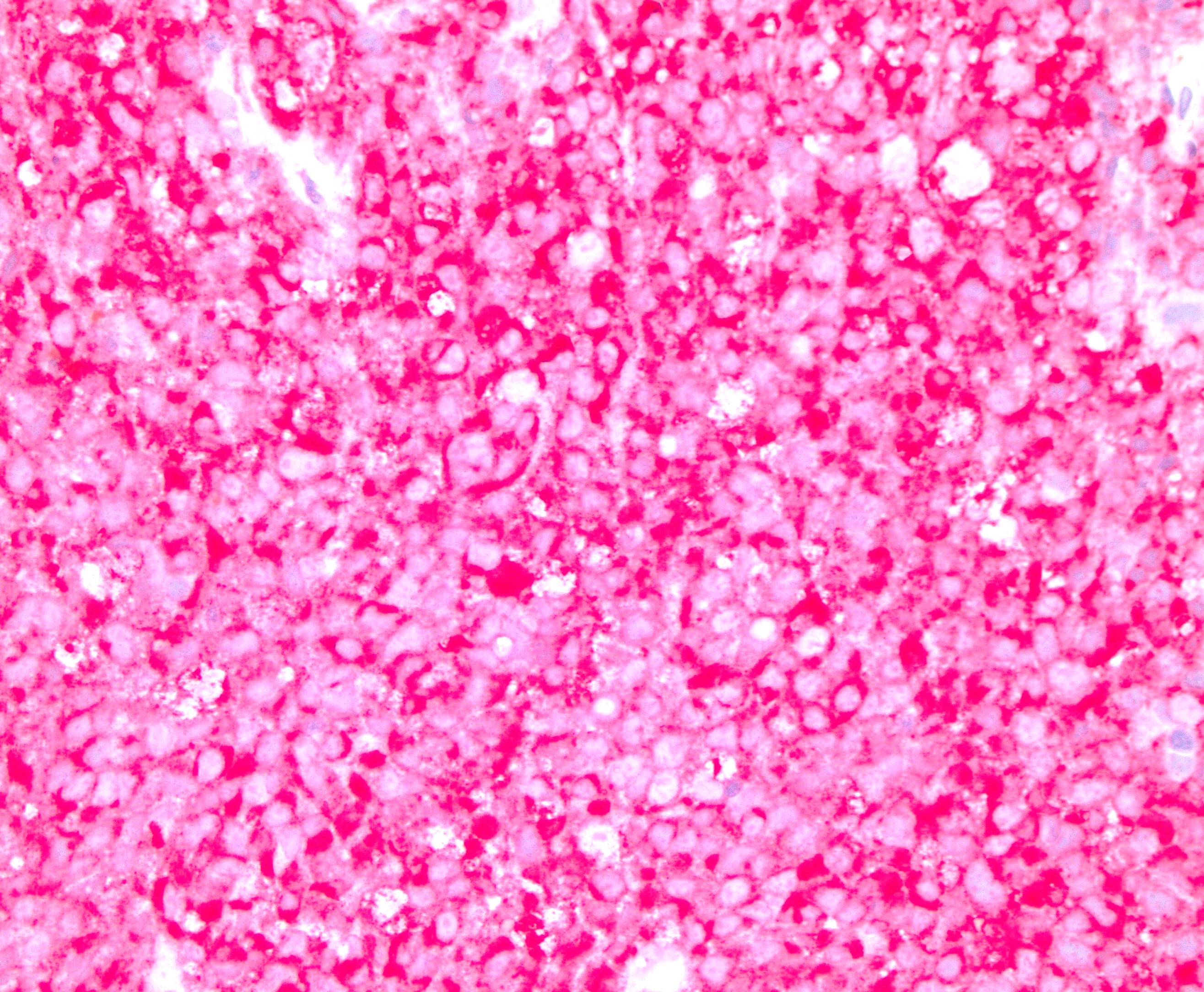
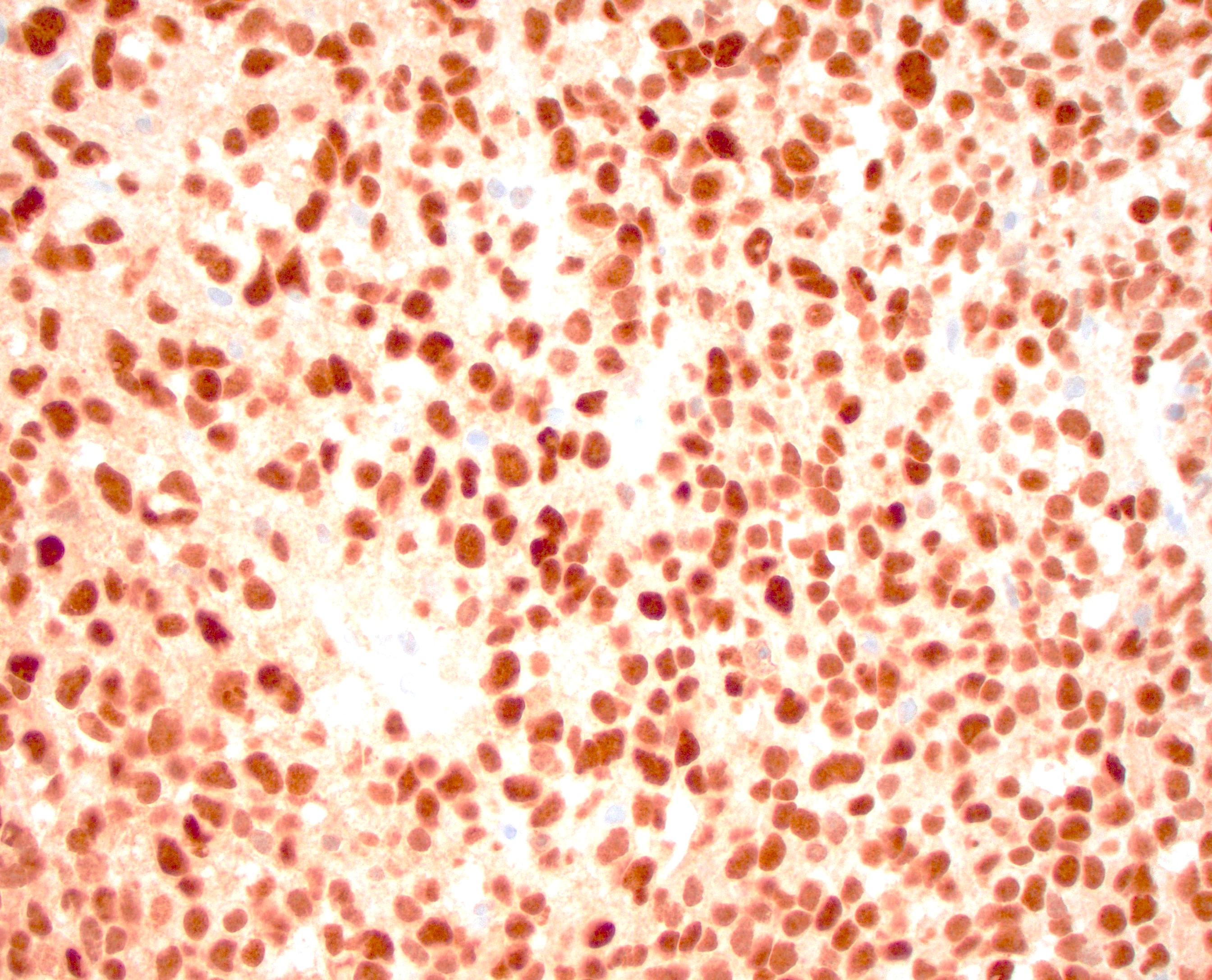
- Biopsy is necessary for diagnosis with positive melanocytic markers (SOX10, S100, HMB45, MelanA, etc.)
- Metastasis from another location must be ruled out before diagnosing primary anal melanoma
- There is currently no consensus on how to pathologically stage anal melanoma
- Patients have a poor prognosis due to advanced disease on presentation and aggressiveness of the tumor
Terminology
- Primary anal melanoma
- Anorectal melanoma
- Mucosal lentiginous melanoma
ICD coding
Epidemiology
- Comprises < 1% of all melanomas and colorectal cancers but is the most common site for primary gastrointestinal melanoma (Int J Cancer 2014;134:2961, Surg Oncol Clin N Am 2017;26:143, Surg Clin North Am 2020;100:629, Hum Pathol 2018;79:77)
- More common in White and female patients, with the average age of diagnosis of 60 years (Surg Oncol Clin N Am 2017;26:143, Surg Clin North Am 2020;100:629)
Sites
- Arises in the anus and can extend into the distal rectum (Clin Colon Rectal Surg 2006;19:78)
- Sometimes the primary site cannot be determined between the anus and the rectum (Surg Oncol Clin N Am 2017;26:143)
Pathophysiology
- See Etiology
Etiology
- Melanocytes are normally found at the anal transition zone and squamous zone (Clin Colon Rectal Surg 2011;24:171)
- Mucosal melanomas, including anal melanoma, are not associated with ultraviolet (UV) radiation exposure, unlike cutaneous melanomas (Nature 2017;545:175)
- Otherwise, the etiology of anal melanoma is not well established
Clinical features
- Symptoms are typically vague, including anorectal bleeding, pain, change in bowel habits and sometimes a mass, which can be confused with other conditions (e.g., hemorrhoids) and may lead to delayed diagnosis (Surg Clin North Am 2020;100:629)
- May be discovered as an incidental finding in a hemorrhoidectomy or anal polyp resection specimen (Surg Oncol Clin N Am 2017;26:143)
- Patients often have delayed presentation or are misdiagnosed, which results in advanced disease, often with local lymph node metastasis (Surg Clin North Am 2020;100:629)
- Some association with human immunodeficiency virus (HIV) (Surg Oncol Clin N Am 2017;26:143)
Diagnosis
- Biopsy is necessary to confirm the diagnosis (Surg Clin North Am 2020;100:629)
- Colonoscopy is advisable to characterize the lesion and rule out the presence of a second malignancy of the colon (Dis Colon Rectum 2020;63:573)
- Additional imaging is needed for staging and to confirm location of primary disease or to rule out metastatic disease (Dis Colon Rectum 2020;63:573)
- Staged clinically
- Stage I - local disease only
- Stage II - local disease with regional lymph nodes
- Stage III - distant metastatic disease (Clin Colon Rectal Surg 2006;19:78)
- There is no current consensus on how to pathologically stage these lesions (Hum Pathol 2018;79:77)
Laboratory
- No specific findings for this entity
Radiology description
- MRI is preferred due to higher soft tissue resolution
- Melanin pigmented lesions typically demonstrate high signal intensity on T1 weighted imaging and mixed signal intensity on T2 weighted imaging
- It is common for amelanotic lesions to not display these characteristic findings on MRI
- Reference: BMJ Case Rep 2021;14:e247421
Radiology images
Prognostic factors
- 5 year survival is based on stage at diagnosis but is generally poor with 32% for local disease, 17% for regional spread and 0% for distant spread (Surg Clin North Am 2020;100:629)
- Gross and histologic features associated with poor prognosis include tumor size and thickness, regional lymph node involvement, perineural invasion and amelanotic subtype (Surg Clin North Am 2020;100:629, Surg Oncol Clin N Am 2017;26:143)
Case reports
- 63 year old woman with bleeding per rectum and painful defecation (Cureus 2021;13:e15474)
- 66 year old woman with anal bleeding, pain and tenesmus (World J Clin Cases 2021;9:11369)
- 81 year old woman with hematochezia and perianal pain (Am J Case Rep 2021;22:e933032)
- 84 year old woman with anal mass (Middle East J Dig Dis 2019;11:166)
- 85 year old woman with recurrent anal mass (BMC Surg 2020;20:68)
Treatment
- Managed with excision
- Adjuvant chemotherapy and radiation are recommended based on patient stage
- Reference: Surg Clin North Am 2020;100:629
Clinical images
Gross description
- Lesions can be varied in their presentation, including size, shape and color
- Usually present as large, expansive, nodular masses
- Majority of lesions are pigmented but can be nonpigmented
- Ulceration is common
- Reference: Surg Clin North Am 2020;100:629
Frozen section description
- Frozen section is not recommended
Microscopic (histologic) description
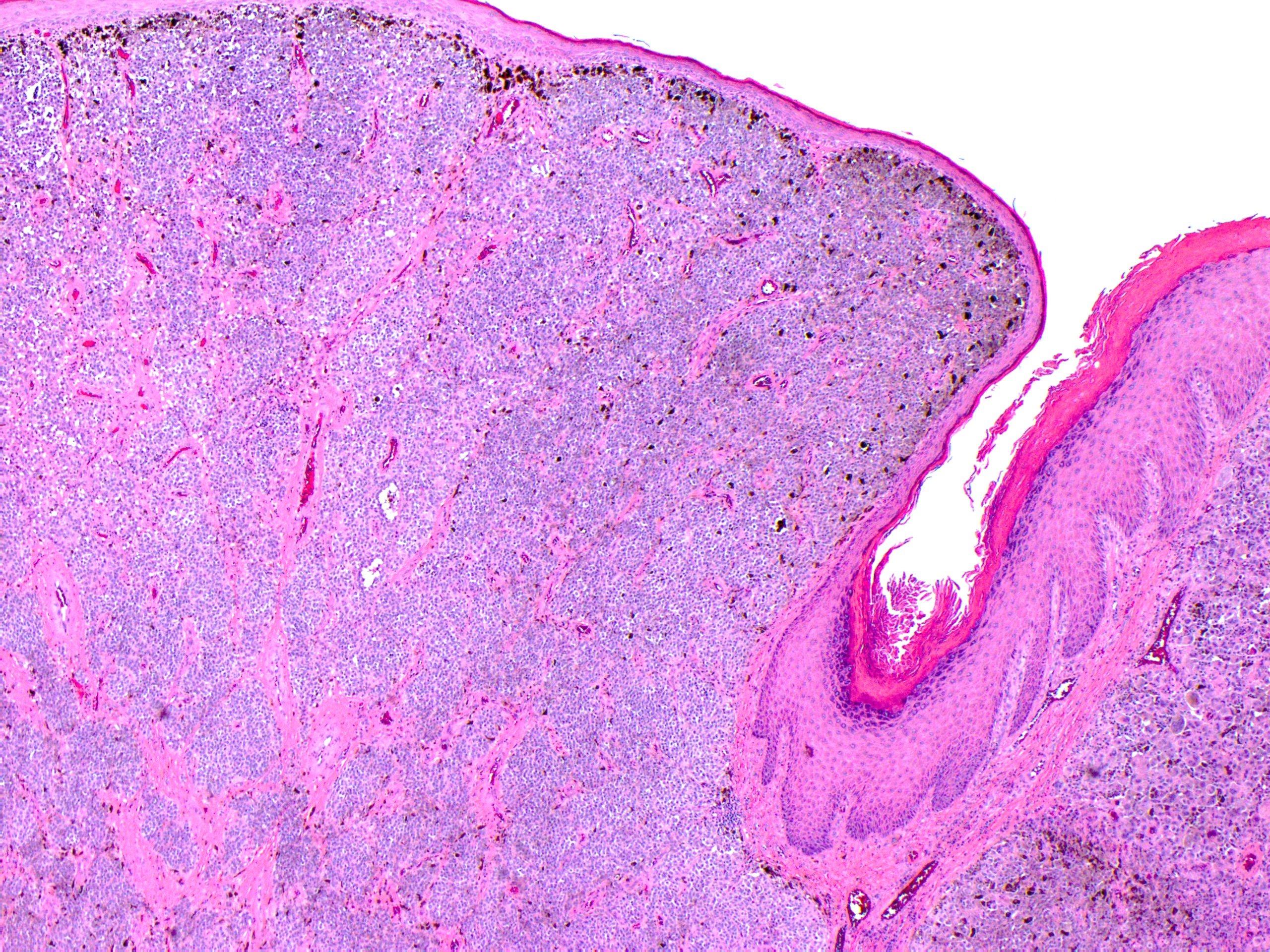
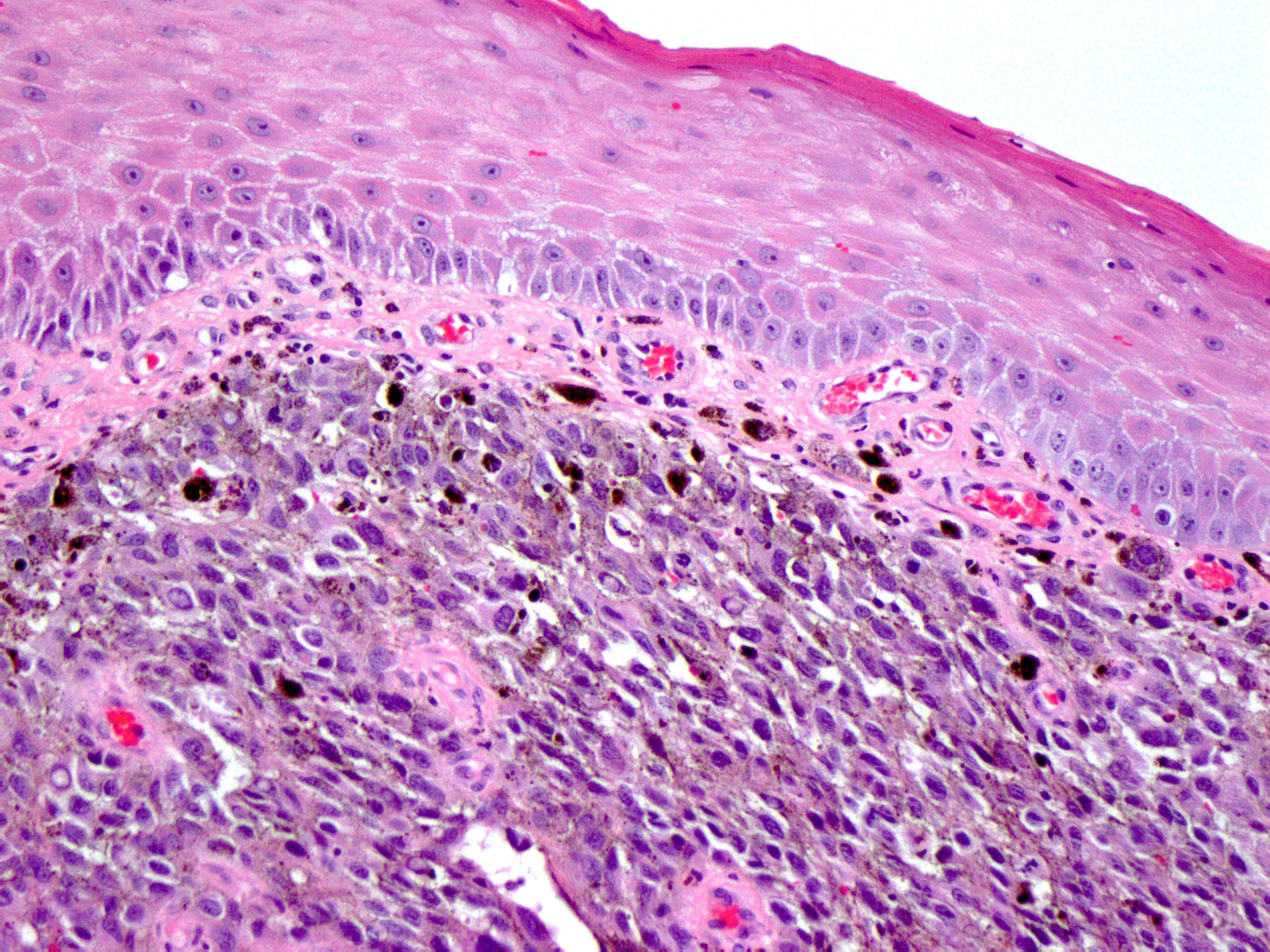
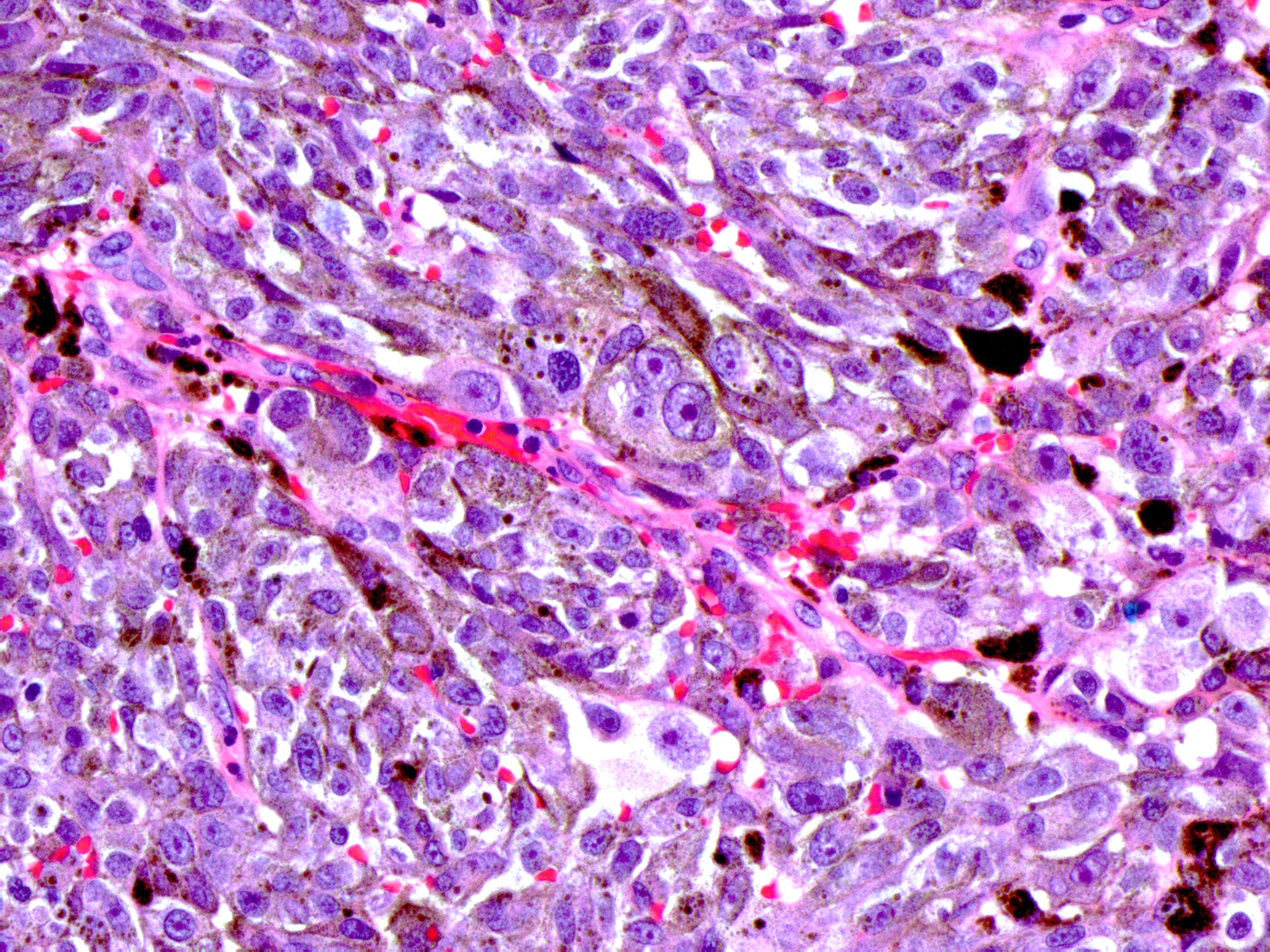
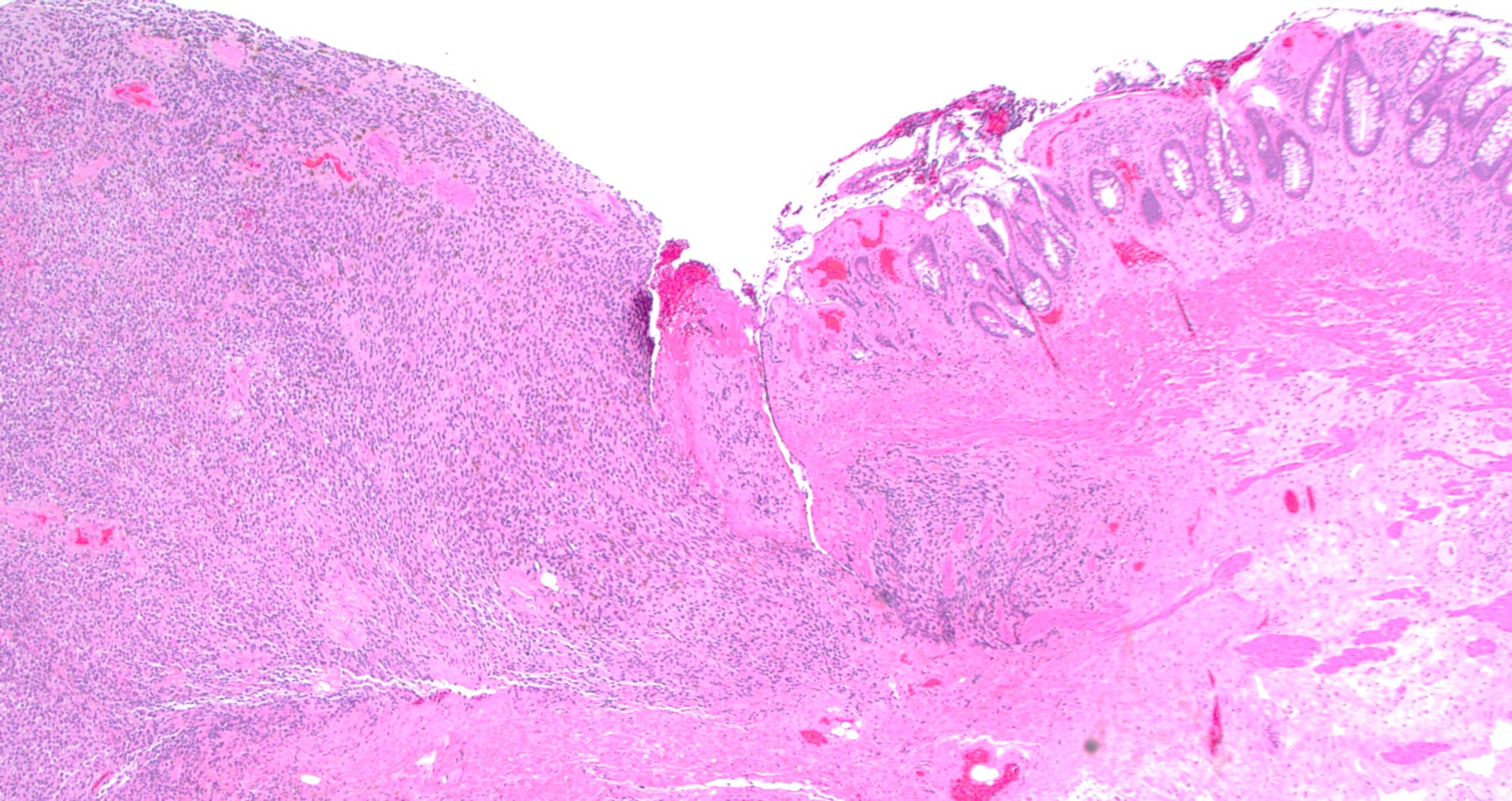
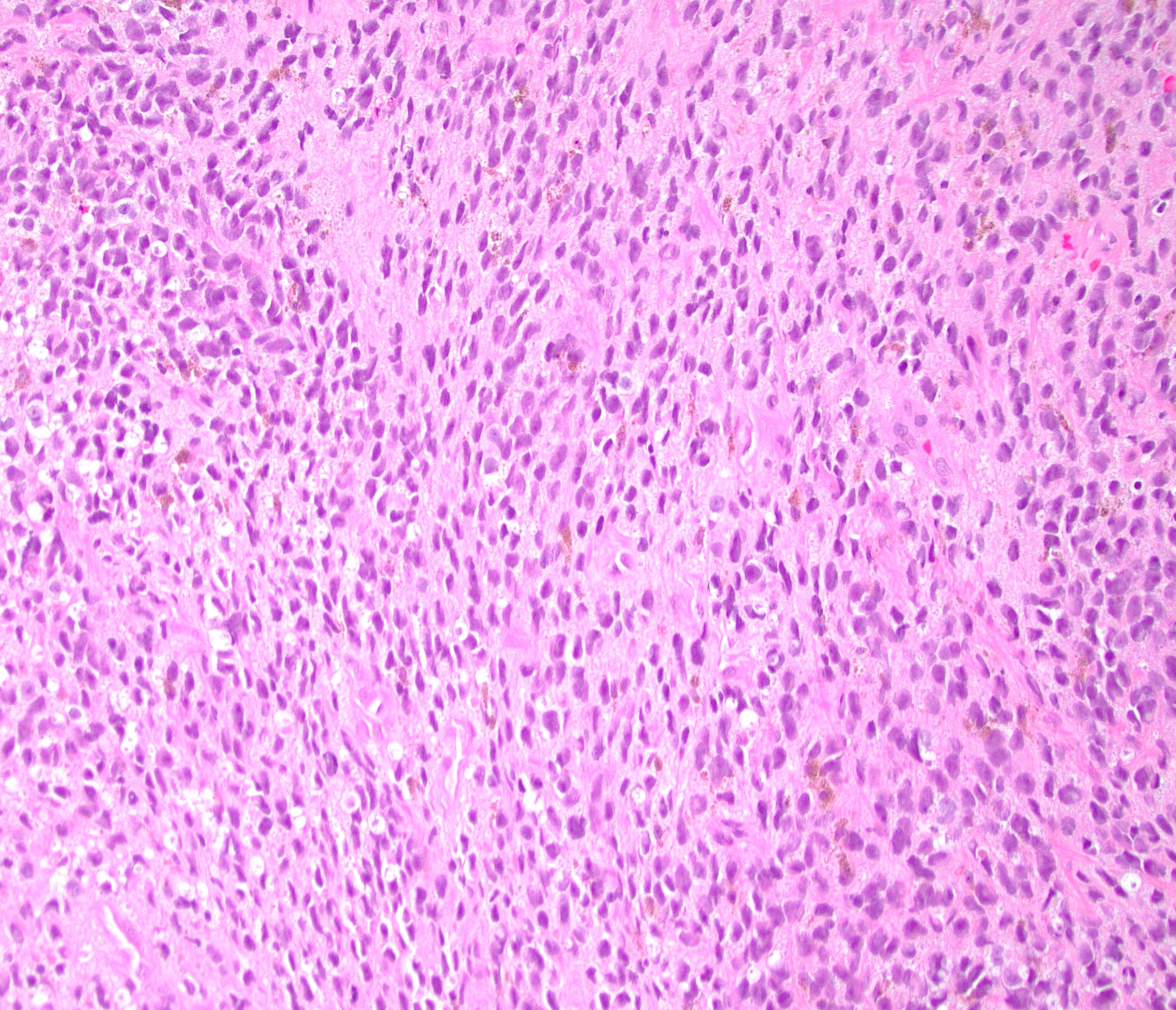
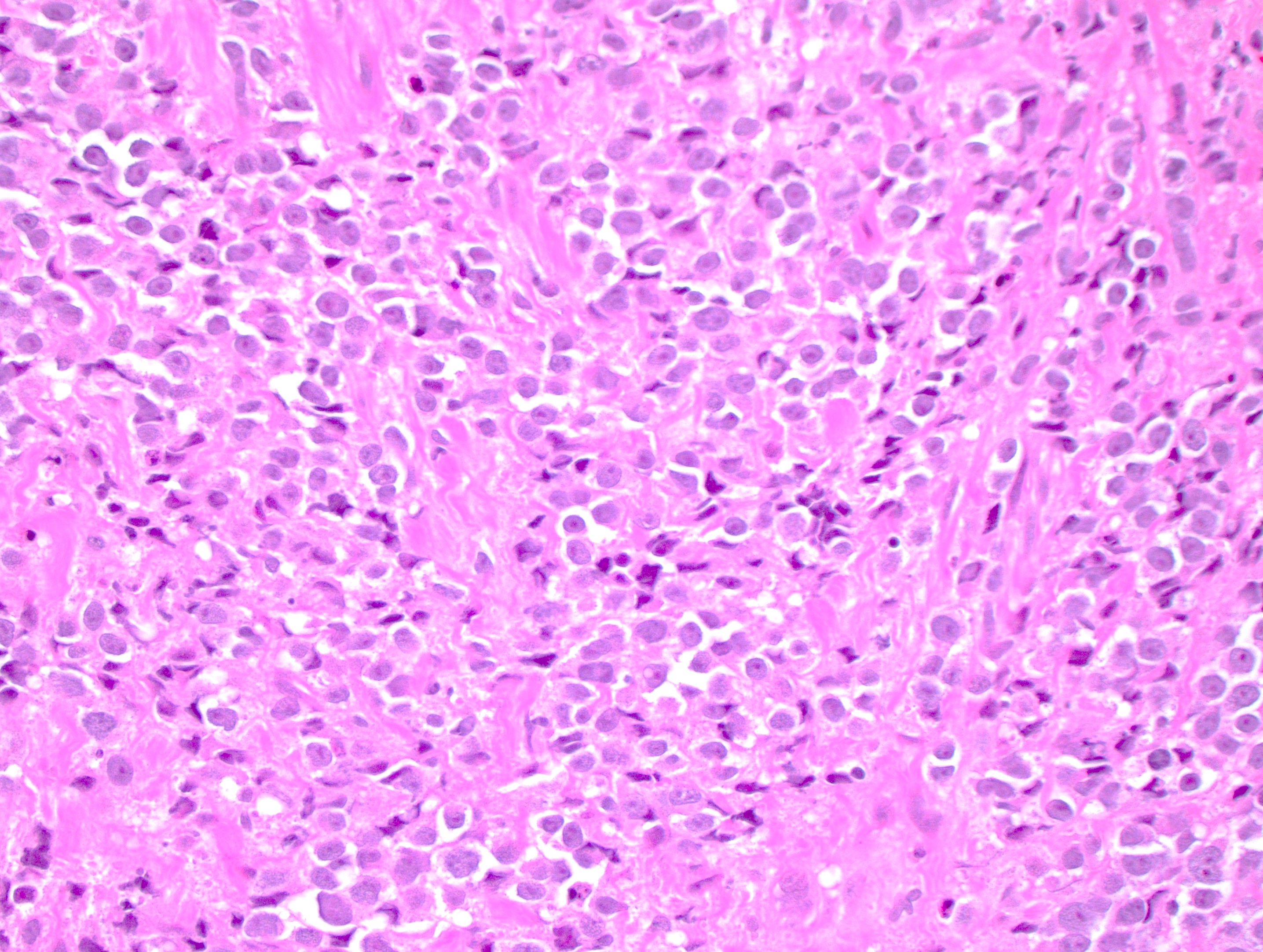
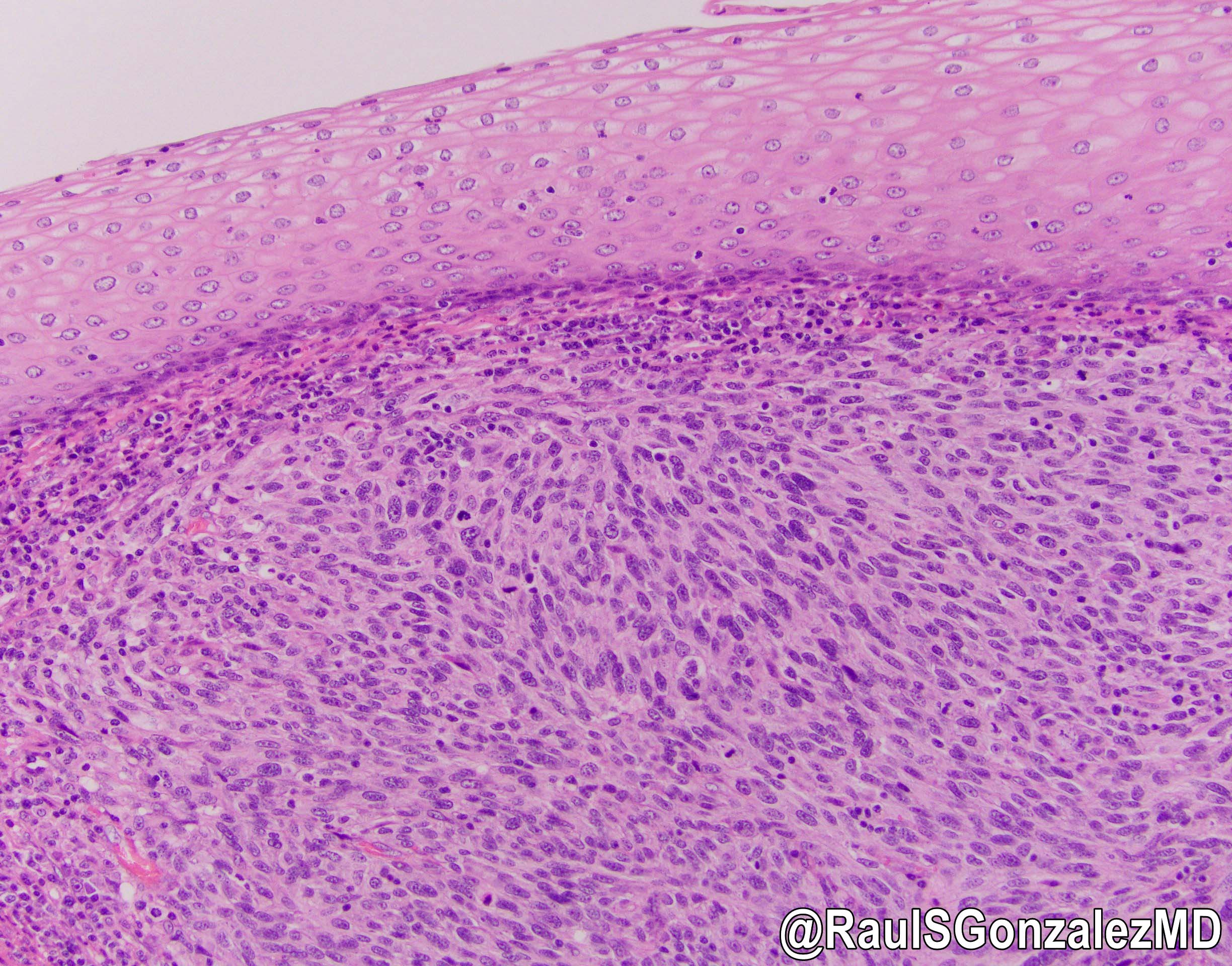
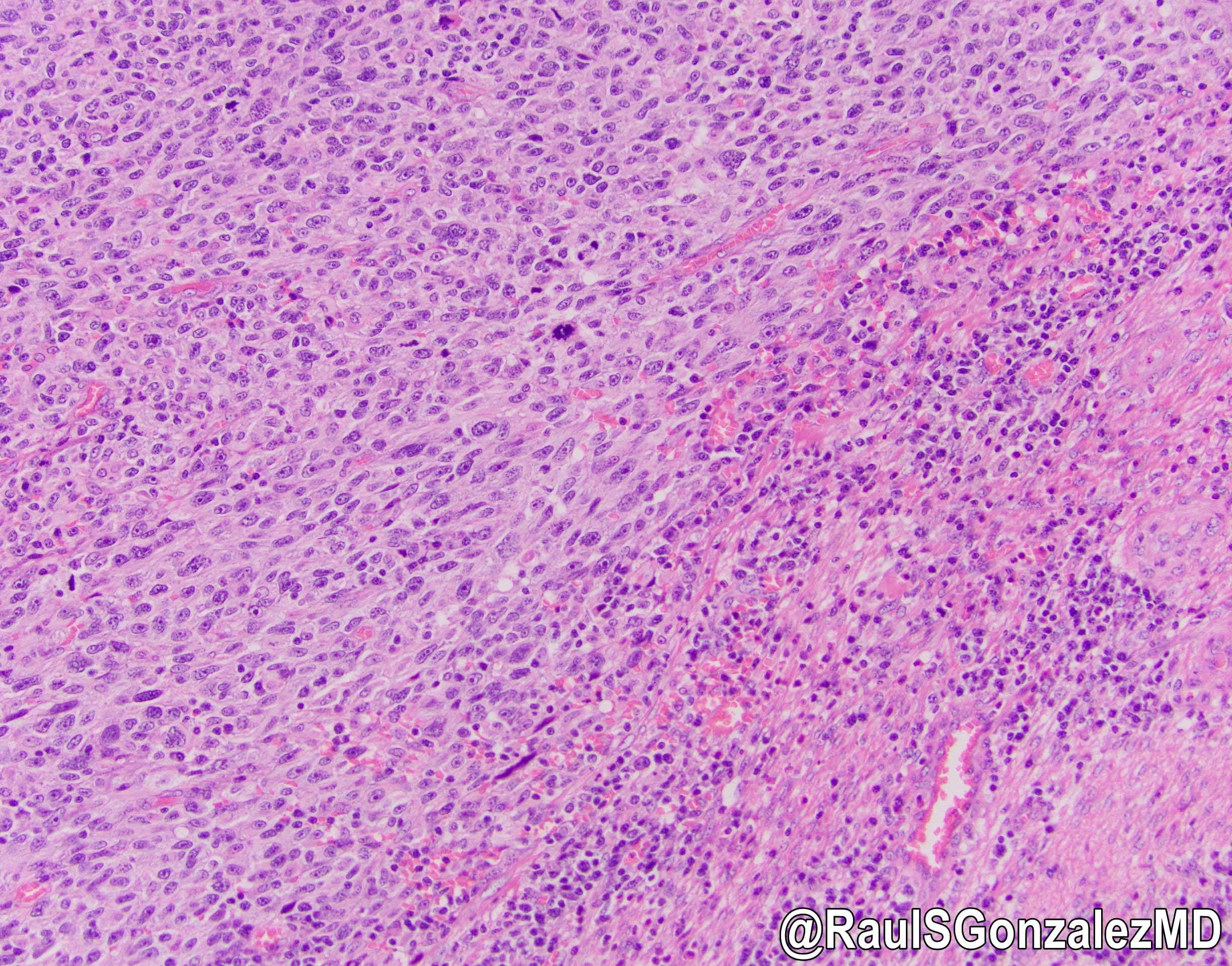
- Histomorphology can vary greatly but solid sheets of atypical epithelioid cells originating from the epithelium is the most common presentation; however, the cytomorphology may be composed of spindled, pleomorphic or small round blue cells while the architectural patterns may be nested, pseudopapillary or pseudoalveolar (Hum Pathol 2018;79:77)
- Pigmentation is variable and can be absent in up to 40% of cases, which is much more common than in cutaneous melanoma (< 5% amelanotic) (Hum Pathol 2018;79:77, Surg Oncol Clin N Am 2017;26:143)
- Ulceration can be present
- Identification of a junctional component adjacent to the invasive tumor can support the diagnosis of primary anal melanoma (Surg Oncol Clin N Am 2017;26:143)
- Melanoma, including anorectal examples, may undergo dedifferentiation which is defined as a tumor that has lost evidence of melanocytic differentiation (morphologic and immunophenotypic) (Int J Surg Pathol 2019;27:923)
- These dedifferentiated examples may aberrantly express various nonmelanocytic markers
- Dedifferentiation is rare but is seen more commonly in metastases of cutaneous origin
Microscopic (histologic) images
Virtual slides
Cytology description
- FNA specimens are usually obtained from metastases
- Largely dispersed population of pleomorphic epithelioid cells or spindle cells
- Nuclear pleomorphism and prominent nucleoli
- Eccentric nuclei with pseudoinclusions can be seen
- Cytoplasmic melanin is seen as fine yellow-brown or blue granules, depending on the slide preparation
- May have cells with double image mirror nuclei (demons)
- References: Am J Clin Pathol 2007;127:385, Int J Clin Exp Pathol 2010;3:367, Cancer Cytopathol 2022;130:18
Positive stains
Negative stains
- Keratin, CD45, CDX2 and SATB2
- It is important to note that melanoma can aberrantly express many antigens and demonstrate divergent differentiation, which can be a potential diagnostic pitfall (Histopathology 2008;52:119, Int J Surg Pathol 2015;23:329)
Molecular / cytogenetics description
- Generally, mucosal melanomas are characterized by a relatively low mutational burden (Gastroenterology 2004;127:1815)
- C-KIT mutations can be seen more frequently in mucosal melanomas than in cutaneous melanoma (Clin Cancer Res 2017;23:6120)
- BRAF mutations can be present but not as commonly as in cutaneous melanoma (Gastroenterology 2004;127:1815)
- Mutations of SF3B1 can also be seen (Clin Cancer Res 2017;23:6120)
Sample pathology report
- Anus, pigmented lesion, excision:
- Malignant melanoma (see comment)
- Margins are free of involvement
- Comment: Immunohistochemical staining was performed and the neoplastic cells showed positivity for SOX10 and PRAME, while they were negative for pancytokeratin. The immunophenotypic findings support the diagnosis of primary anal melanoma.
Differential diagnosis
- Secondary involvement by rectal adenocarcinoma:
- More common than anal adenocarcinoma
- Usually well or moderately differentiated gland forming carcinoma with marked desmoplasia
- CK20, CDX2 and SATB2 positive
- Anal adenocarcinoma:
- Squamous cell carcinoma:
- Most common carcinoma of the anal tract
- Resembles squamous cell carcinoma as seen elsewhere in body
- Positive for pankeratins and squamous markers (i.e., p40)
- Metastatic melanoma:
- History of melanoma or image findings consistent with a metastatic lesion
- Lack of intraepidermal component does not confirm metastasis
- Lymphoma:
- Atypical population of lymphocytes
- CD45 positive
- Neuroendocrine carcinoma:
- Small and large cell subtypes resemble morphology seen in other locations
- Solid nests of poorly differentiated cells
- Positive for keratin, p16, p63, HPV ISH and neuroendocrine markers (synaptophysin, chromogranin, INSM1)
- Usually high Ki67
- Hemorrhoids:
- Dilated thin walled vascular plexus within stroma
- Can display metaplastic changes in the surface epithelium
- Gastrointestinal stromal tumor (GIST):
- May be spindled or epithelioid but usually lacks the overt cytologic atypia seen in melanoma
- DOG1+
- Malignant peripheral nerve sheath tumor (MPNST):
Additional references
Board review style question #1
Board review style answer #1
C. HMB45. The H&E image demonstrates anal melanoma. HMB45 is a melanocytic marker that would confirm the diagnosis of melanoma, along with the malignant features seen on H&E. Answer A is incorrect because CD45 is a lymphocytic marker. CD45 should be ordered to rule out lymphoma but a negative result would not confirm the diagnosis in this case. Answer D is incorrect because melanoma is typically pancytokeratin negative. This would be a good confirmatory stain but would not be diagnostic of melanoma by itself. Answer B is incorrect because CDX2 is a common marker for colonic adenocarcinomas. CDX2 should be used to rule out a primary rectal adenocarcinoma that involves the anus but will be negative for any anal malignancies, including melanoma.
Comment Here
Reference: Anal melanoma
Comment Here
Reference: Anal melanoma
Board review style question #2
Which of the following characteristics is similar for both cutaneous and anal melanoma?
- Pathologic staging
- Presentation
- Prognosis
- Staining / IHC
Board review style answer #2
D. Staining / IHC. Cutaneous and anal melanoma will stain with similar melanocytic markers (SOX10, S100, HMB45, MelanA, etc.). Answer C is incorrect because anal melanoma has a worse prognosis when compared to cutaneous melanoma, especially because patients with anal melanoma often have advanced disease on presentation due to the vague clinical symptoms and difficulty in diagnosis. Answer B is incorrect because anal melanoma typically presents with vague symptoms and not the typical ABCDE (asymmetry, border, color, diameter, evolving) criteria for cutaneous melanoma. Answer A is incorrect because anal melanoma does not have a standardized pathologic staging system. Anal melanomas can be staged similarly to cutaneous melanoma but this is not universal.
Comment Here
Reference: Anal melanoma
Comment Here
Reference: Anal melanoma