Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Nguyen PN, Hassell LA. Buschke-Löwenstein tumor. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/anusbuschkelowenstein.html. Accessed April 2nd, 2025.
Definition / general
- Buschke-Löwenstein tumor (also known as giant condyloma acuminatum) was first described as a penile neoplasm by Buschke and Löwenstein in 1925
- Previously considered synonymous with verrucous carcinoma
- Recent studies and WHO 2019 have suggested that Buschke-Löwenstein tumors and verrucous carcinoma are 2 separate entities; while Buschke-Löwenstein tumors are associated with low risk HPV types (6,11), verrucous carcinomas usually have a non-HPV etiology (Mod Pathol 2012;25:1354, Histopathology 2017;70:938, WHO Classification of Tumours Editorial Board: Digestive System Tumours, 5th Edition, 2019)
Essential features
- Condylomatous squamous lesion without high grade dysplasia, with only low risk HPV types present, forming an exophytic mass, usually greater than 3 cm
Terminology
- Preferred term: Buschke-Löwenstein tumor (MeSH: Buschke-Lowenstein Tumor [Accessed 18 November 2020])
- Also called giant condyloma acuminatum, giant condyloma of Buschke and Löwenstein
ICD coding
- ICD-O: None
- ICD-11: 1A95.0 - Anal warts
Epidemiology
- Incidence rates: about 0.1% of the population; relatively few cases have been reported (GARD: Buschke-Lowenstein tumor [Accessed 18 November 2020])
- M > F (4.4:1)
- Risk factors:
- HPV 6, 11
- Immunodeficient state (HIV positive, immunosuppression)
- Anal receptive sex (homosexual men)
- Chronic irritation (perianal fistula, ulcerative colitis)
- Poor hygiene
- Cases in children raise the suspicion of sexual abuse, though this association is not well established (Am J Dis Child 1982;136:704, Arch Pediatr 2019;26:473)
Sites
- Anogenital region (involves both inside and outside of anal canal)
- Urinary bladder, genitalia, oropharynx
Pathophysiology
- Similar to the process in other skin and mucosal HPV induced tumors, viral DNA is incorporated into cellular DNA following exposure, redirecting cellular processes into dysregulated cellular proliferation (IARC Monogr Eval Carcinog Risks Hum 2007;90:1)
Etiology
- > 90% of cases associated with low risk HPV 6, 11
- A few cases reported with Netherton syndrome (Pediatr Dermatol 2017;34:e328, J Plast Reconstr Aesthet Surg 2011;64:1533)
Clinical features
- Presenting symptoms: perianal exophytic and cauliflower-like mass with or without abscess, fistula, pain, pruritus, bleeding and ulceration
- Slow growing, local extension
- Usually no perineural invasion or nodal metastasis at initial diagnosis
- Lymphadenopathy, if present, is usually caused by secondary infection (Clin Colon Rectal Surg 2019;32:386)
- Recurrence rate: from 23.7% up to 66% (Virchows Arch 2020;476:543, Dis Colon Rectum 1994;37:950)
- High risk HPV infection (16, 18) correlated with invasive Buschke-Löwenstein tumors (Virchows Arch 2020;476:543)
- Squamous cell carcinoma transformation: 14 - 56%; more common in HIV positive patients (Virchows Arch 2020;476:543, Dis Colon Rectum 1994;37:950, AIDS Res Hum Retroviruses 2018;34:375)
Diagnosis
- Diagnosis is often based on clinical course, radiology and histopathology
Radiology description
- Preoperative CT / MRI is often required to evaluate local extension
Radiology images
Prognostic factors
- Overall mortality: 10.5 - 20% (Virchows Arch 2020;476:543, Dis Colon Rectum 1994;37:950)
- Prognosis related to:
- Size of tumor
- Local recurrence
- Squamous cell carcinoma transformation
- Immunosuppression and secondary infection (Case Rep Infect Dis 2018;2018:7267213)
Case reports
- 3 year old boy with HIV infection presenting with multiple warts in the anogenital region (Urol Case Rep 2016;7:14)
- 17 year old pregnant girl with giant masses that covered the perineal and perianal region (Dermatol Ther 2019;32:e12972)
- 21 year old woman with severe perineal pain, dysuria and burning micturition (JAAD Case Rep 2018;4:692)
- 31 year old man with anal discomfort due to a protruding mass (J Med Case Rep 2015;9:9)
- 61 year old man with HIV infection presenting with worsening pain and swelling in the anorectal area (Case Rep Infect Dis 2018;2018:7267213)
Treatment
- Preferred initial therapy: complete excision with wide margins
- Other treatment strategies: podofilox cream, topical 5-fluorouracil, regional radiation, CO2 laser or a combined chemoradiation regimen (J Obstet Gynaecol 2020;40:582)
Clinical images
Gross description
- Size: up to 13 cm (Histopathology 2017;70:938)
- Large, exophytic, cauliflower-like mass
- May show fistula, bleeding, ulceration, superficial infection
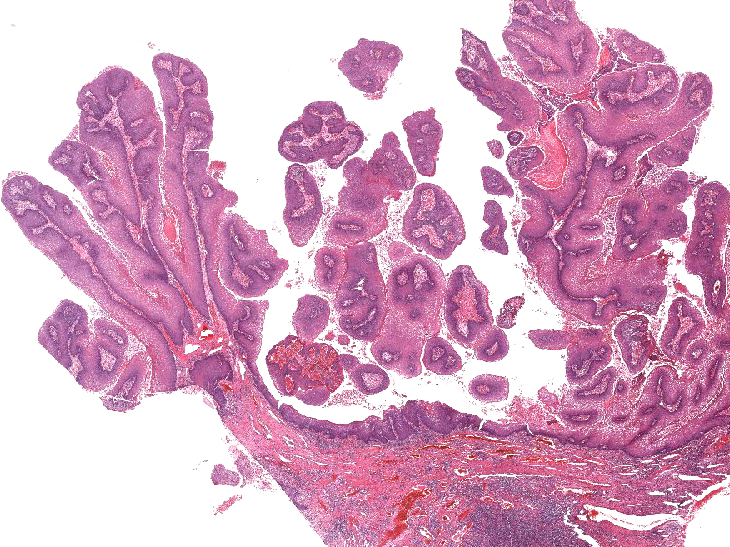
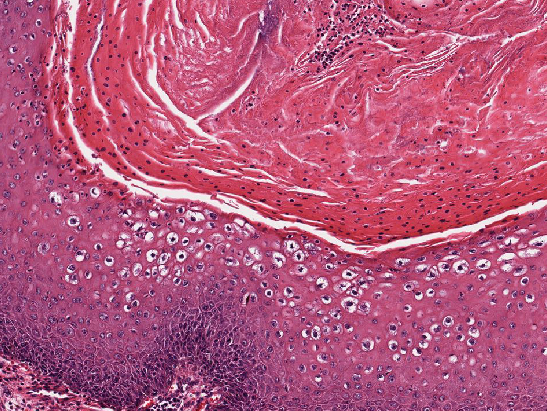
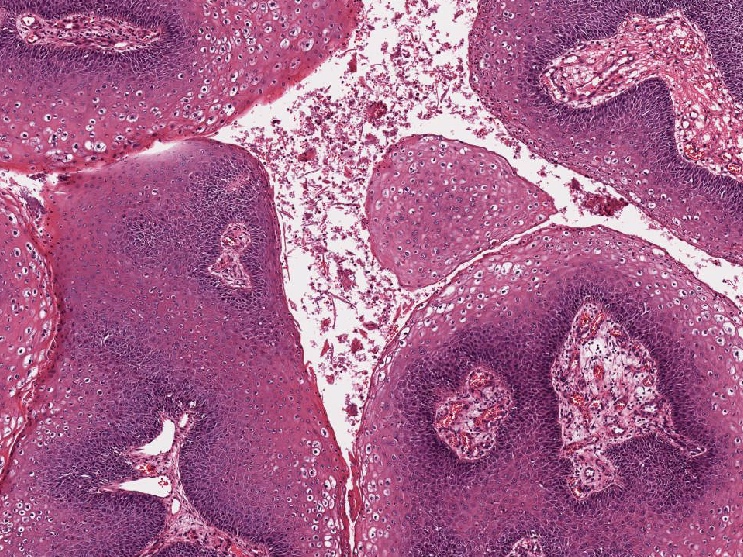
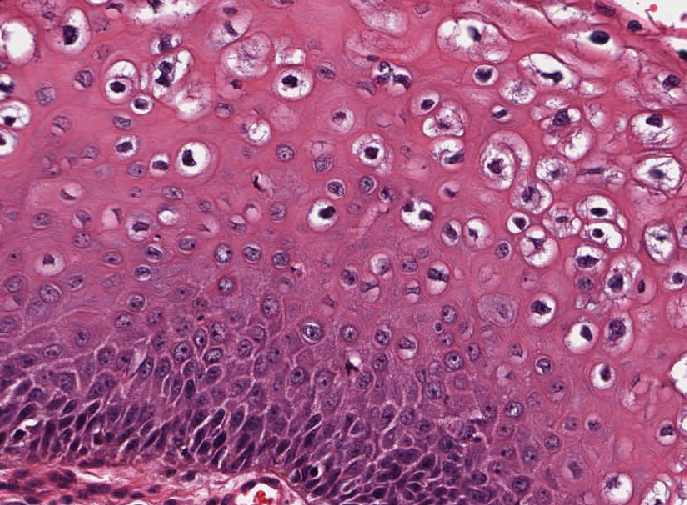
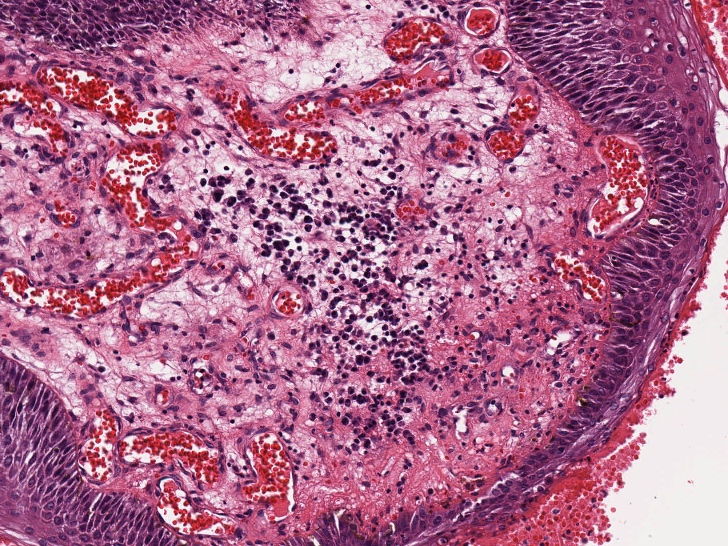
Microscopic (histologic) description
- Resembles condyloma acuminatum
- Diagnostic criteria
- Well formed papillae with a prominent central fibrovascular core
- Hyperkeratosis with parakeratosis and marked acanthosis
- Koilocytes on upper third of the squamous epithelium
- Chronic inflammatory infiltration
- Local extension and displacement of surrounding tissues but no evidence of dysplasia / invasion (WHO Classification of Tumours Editorial Board: Digestive System Tumours, 5th Edition, 2019)
- Low mitotic rate, usually confined to the basal layer with no abnormal mitoses (Histopathology 2017;70:938)
- About 30 - 35% may develop an invasive component; especially in high risk HPV positive cases (Virchows Arch 2020;476:543, Dis Colon Rectum 1989;32:481)
Microscopic (histologic) images
Positive stains
- Squamous markers (p40, p63), cytokeratins
- ISH for low risk HPV (6, 11) (Histopathology 2017;70:938, Virchows Arch 2020;476:543)
Negative stains
Videos
Giant condyloma
Sample pathology report
- Anal canal and perianal skin, complete excision:
- Buschke-Löwenstein tumor / giant condyloma acuminatum (see synoptic report)
| Tumor summary | Anus |
| Procedure | Complete excision |
| Tumor site | Perianal skin |
| Tumor size | 5 cm |
| Histologic type | Giant condyloma acuminatum |
| Margins | Free, 0.5 cm to radial |
| Extent | Anal canal, below the pectinate line |
| Tumor invasion | Not identified |
| Examined sections | 05 blocks |
| Lymph nodes, # sampled | 10 |
| Lymph nodes, # involved | 0 |
Ancillary study result
| Patchy, 5% of cells Restricted to parabasal layers |
Differential diagnosis
- Condyloma acuminatum:
- Histologically, Buschke-Löwenstein tumor resembles condyloma acuminatum
- Clinical findings help differentiate condyloma from Buschke-Löwenstein tumor (large size - usually > 3 cm, locally expansive and displacement of surrounding tissues)
- Verrucous carcinoma:
- No koilocytosis
- Invasion with pushing borders
- Negative for HPV
- Similar p16 staining pattern to Buschke-Löwenstein tumor (patchy / focal or negative) (Arch Pathol Lab Med 2019;143:821)
- Squamous cell carcinoma:
- Marked cytologic atypia with stromal invasion
- p16: diffusely positive
- Squamous papilloma of anus:
- Extremely rare (Endoscopy 2013;45:E42)
Board review style question #1
Which of the following features best distinguishes Buschke-Löwenstein tumor from verrucous squamous carcinoma?
- HPV ISH positivity
- p53 immunostatus
- Patient age less than 50 years
- Pushing invasion
- Size greater than 5 cm
Board review style answer #1
A. HPV ISH positivity. Buschke-Löwenstein tumor is an HPV related neoplasm whereas verrucous carcinoma is not, so HPV ISH staining (positive) would be expected with Buschke-Löwenstein tumor but not with verrucous carcinoma. Buschke-Löwenstein tumor is most often due to a low risk HPV type, such as HPV 6 or 11. Invasive or displacing type growth can be seen in either lesion.
Comment Here
Reference: Buschke-Löwenstein tumor
Comment Here
Reference: Buschke-Löwenstein tumor
Board review style question #2
Lymphadenopathy seen in conjunction with a bulky anovaginal tumor characterized by parakeratosis, superficial koilocytosis, HPV ISH positivity and minimal squamous atypia as seen in this image is most likely due to
- Associated lymphoma or other immune deficiency inducing state
- Fatty infiltration of the lymph nodes
- Metastasis from a well differentiated invasive component of the tumor
- Netherton syndrome
- Reactive lymphadenopathy related to tumor associated infection
Board review style answer #2
E. Reactive lymphadenopathy related to tumor associated infection. Buschke-Löwenstein tumor is frequently associated with fistulae and perirectal or peritumoral abscess formation, which can lead to regional lymphadenopathy. Metastasis is very uncommon. While immunocompromise may predispose to development of Buschke-Löwenstein tumor, the cause is infrequently due to a lymphoproliferative disorder that would enlarge the lymph nodes. Netherton syndrome is not primarily associated with adenopathy.
Comment Here
Reference: Buschke-Löwenstein tumor
Comment Here
Reference: Buschke-Löwenstein tumor