Table of Contents
Definition / general | Essential features | ICD coding | Sites | Etiology | Clinical features | Diagnosis | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Gonzalez RS. Gangliocytic paraganglioma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/ampullaganglio.html. Accessed March 31st, 2025.
Definition / general
- Rare tumor of periampullary region and second part of duodenum
Essential features
- Duodenal neoplasm that rarely metastasizes
- Triphasic histology (epithelioid, spindle, ganglion type cells) and immunoprofile are characteristic and distinctive
ICD coding
- ICD-10: D13.2 - Benign neoplasm of duodenum
Sites
- Almost all arise in the duodenum or around ampulla of Vater
- May very rarely arise elsewhere (such as in the nasopharynx, Arch Pathol Lab Med 2001;125:1098)
Etiology
- May derive from endodermal neuroectodermal complexes in the embryonic ventral pancreas (Am J Surg Pathol 1985;9:31)
Clinical features
- 15 - 84 years (mean 52 years) (BMC Cancer 2011;11:187)
- M > F (1.5:1) (BMC Cancer 2011;11:187)
- Presents with GI bleeding or abdominal pain but may be incidental finding
- Usually benign and nonfunctional; very rarely produces hormones (J Gastrointest Oncol 2016;7:S107)
- Approximately 7% metastasize to lymph nodes (BMC Cancer 2011;11:187)
- Very rarely metastasizes widely and may cause patient death (World J Clin Cases 2017;5:222)
- May recur if incompletely excised
Diagnosis
- Tissue diagnosis required
Prognostic factors
- Almost always benign but distant metastases can rarely occur
Case reports
- 47 year old man with widely metastatic gangliocytic paraganglioma (World J Gastroenterol 2014;20:15454)
- 55 year old woman with gangliocytic paraganglioma of the thymus (J Pathol Transl Med 2016;50:165)
- 68 year old woman with gangliocytic paraganglioma metastatic to peripancreatic lymph node (Diagn Pathol 2017;12:57)
- 71 year old man with gangliocytic paraganglioma of the minor papilla (Intern Med 2017;56:1029)
- 73 year old woman with gangliocytic paraganglioma and concurrent ampullary adenocarcinoma (Intern Med 2018;57:2663)
Treatment
- Endoscopic resection (Gastroenterol Hepatol 2016;39:605)
Gross description
- Usually 1 - 3 cm, sessile or polypoid, no capsule
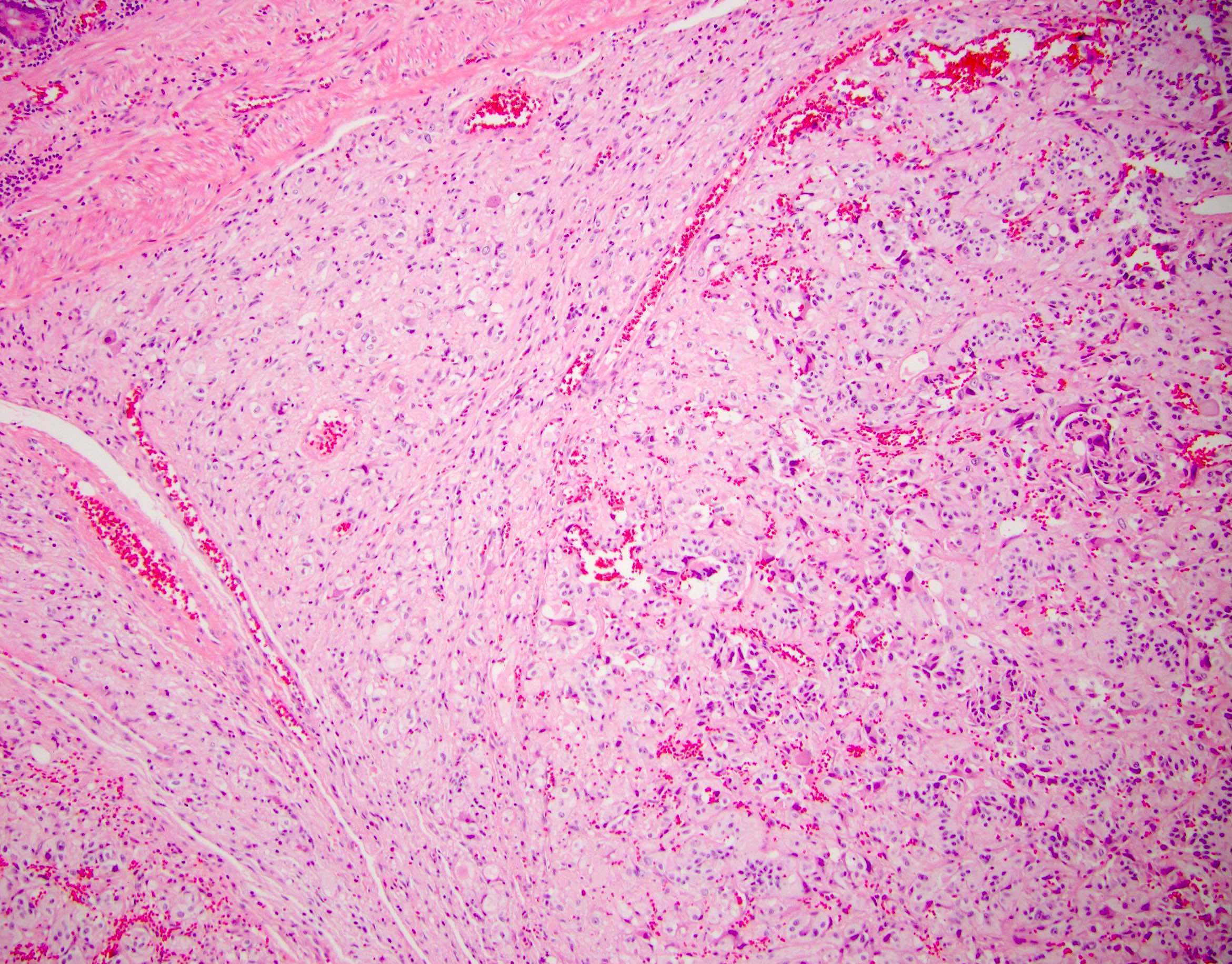
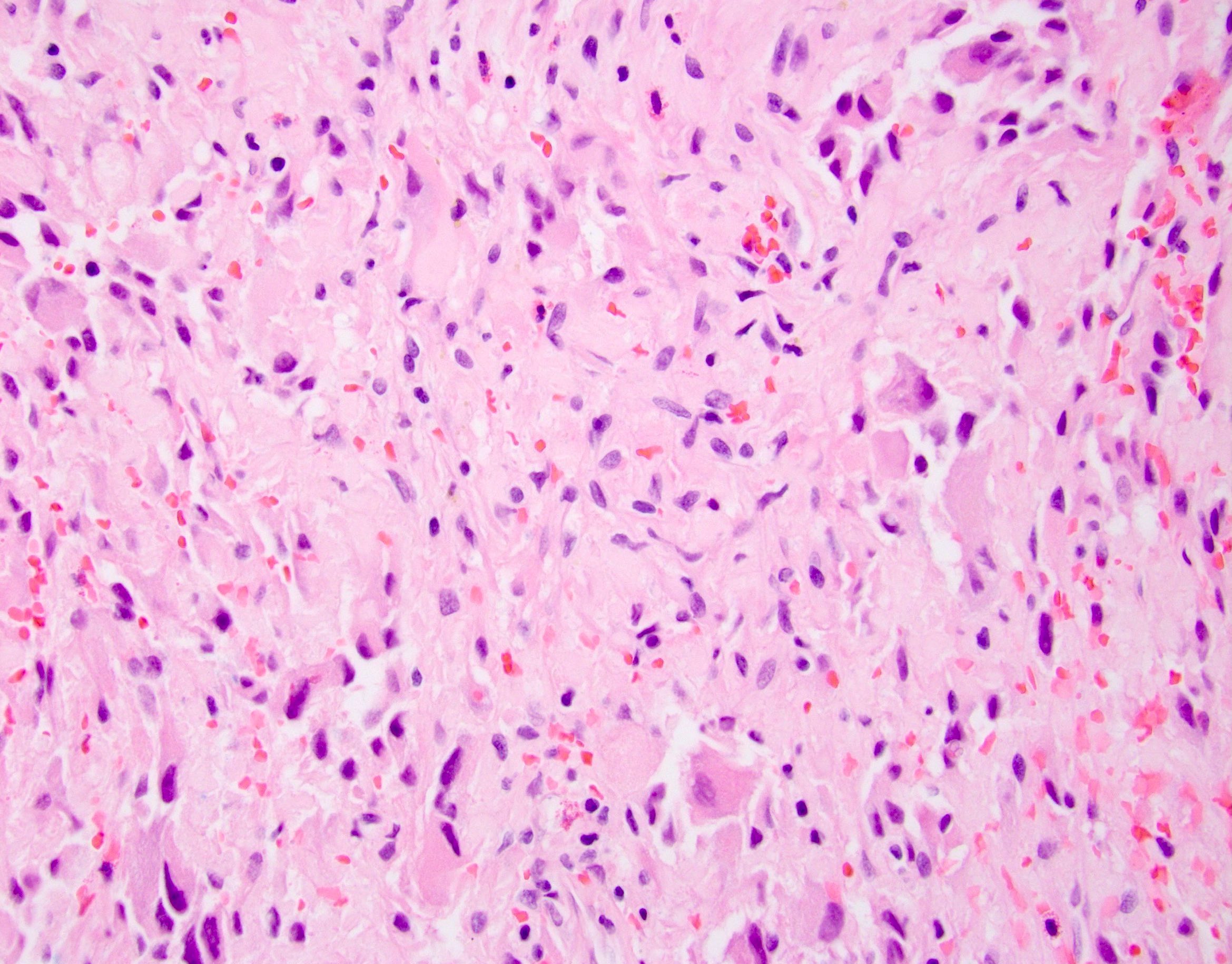
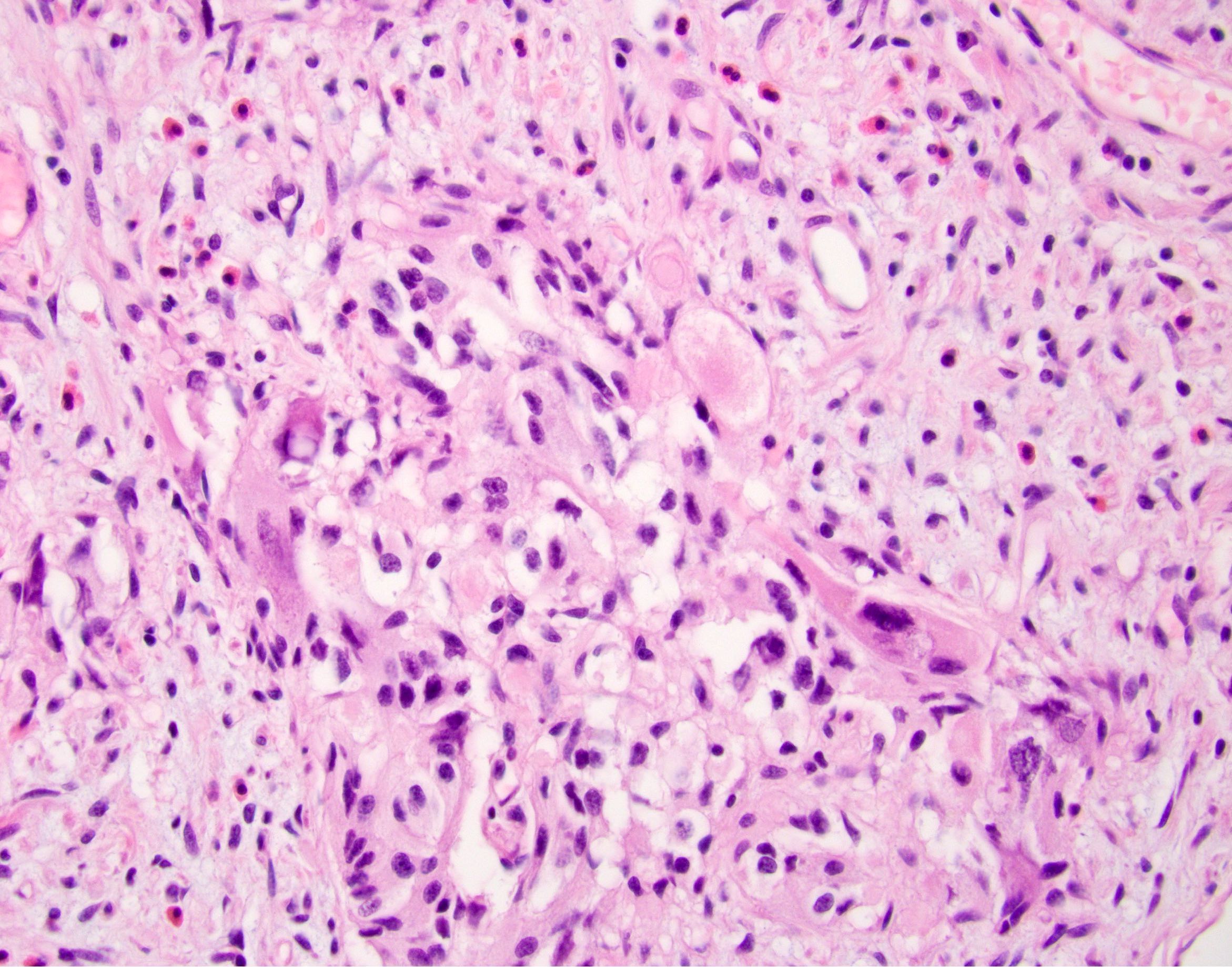
Microscopic (histologic) description
- Unencapsulated submucosal lesion
- Triphasic, with epithelioid, spindle cell (Schwann cell-like) and ganglion type cells of varying proportions
- May therefore resemble well differentiated neuroendocrine tumor, paraganglioma or ganglioneuroma
- Variable stromal amyloid (Am J Surg Pathol 1977;1:207)
Microscopic (histologic) images
Cytology description
- All 3 cell types may be visible in aspirated material (Diagn Cytopathol 2013;41:650)
Positive stains
- Epithelioid cells: pancreatic polypeptide, progesterone receptor, somatostatin, synaptophysin, chromogranin, CD56 (BMC Cancer 2015;15:269)
- Ganglion cells: S100, pancreatic polypeptide, somatostatin, synaptophysin, chromogranin, CD56
- Spindle cells: S100, BCL2 (67%)
Negative stains
- Epithelioid cells: S100, p53 (BMC Cancer 2015;15:269)
- Ganglion cells: progesterone receptor, pancytokeratin, estrogen receptor, p53
- Spindle cells: pancreatic polypeptide, progesterone receptor, somatostatin, synaptophysin (25%), chromogranin, CD56, estrogen receptor, p53
Molecular / cytogenetics description
- May show HIF2A gain of function mutations (Endocr Relat Cancer 2016;23:L13)
Sample pathology report
- Ampulla, mass, resection:
- Gangliocytic paraganglioma (2.2 cm) (see comment)
- Margins of resection unremarkable.
- Comment: Immunohistochemical stains for S100 and synaptophysin highlight various components of this uncommon triphasic neoplasm, which is typically indolent but can rarely metastasize.
Differential diagnosis
- Ganglioneuroma:
- Rare in the ampulla / duodenum
- Difficult to distinguish if ganglion cells are predominant in gangliocytic paraganglioma
- Paraganglioma:
- Rare in the ampulla / duodenum
- S100+ sustentacular cells are arranged around nests of epithelioid cells, rather than forming regions of the tumor
- Well differentiated neuroendocrine tumor:
- Can be difficult, depending on sampling
- Progesterone receptor and pancreatic polypeptide staining may help (Arch Pathol Lab Med 2017;141:1309)
Board review style question #1
Which of the following cell types are seen in gangliocytic paraganglioma?
- Blister, ganglion and stem
- Epithelioid, ganglion and spindle
- Epithelioid, ganglion and sustentacular
- Epithelioid, stem and spindle
Board review style answer #1
Board review style question #2
Board review style answer #2
A. Similar tumors may rarely be seen outside the ampulla. The picture shows a gangliocytic paraganglioma, which usually occurs in the ampulla but can rarely arise in other gastrointestinal or extragastrointestinal sites.
Comment Here
Reference: Gangliocytic paraganglioma
Comment Here
Reference: Gangliocytic paraganglioma