Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Immunohistochemical subclassification | Flow cytometry description | Flow cytometry images | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Klairmont MM, Park CY. DLBCL, NOS. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomadiffuse.html. Accessed April 2nd, 2025.
Definition / general
- Large B cell lymphoma with a diffuse growth pattern which does not meet the criteria for other WHO defined large B cell lymphoma categories
Essential features
- Medium to large atypical lymphoid cells
- Nucleus ≥ size of histiocyte nucleus or 2 lymphocyte nuclei
- Does not meet criteria for other WHO defined large B cell lymphomas
- 2 main molecular subtypes: activated B cell (ABC) subtype and germinal center B cell (GCB) subtype
ICD coding
- ICD-O: 9680/3 - malignant lymphoma, large B cell, diffuse, NOS
Epidemiology
- Most common adult non-Hodgkin lymphoma (~30%) (Blood 2012;120:4795, Blood 2006;107:265)
- Median age = seventh decade but occurs across all ages
- Slight male predominance
Sites
- Lymph node
- 71% with ≥ 1 site of extranodal involvement (J Clin Oncol 1998;16:2780)
- 40% purely extranodal
- GI tract most common extranodal site (18%) but can present anywhere
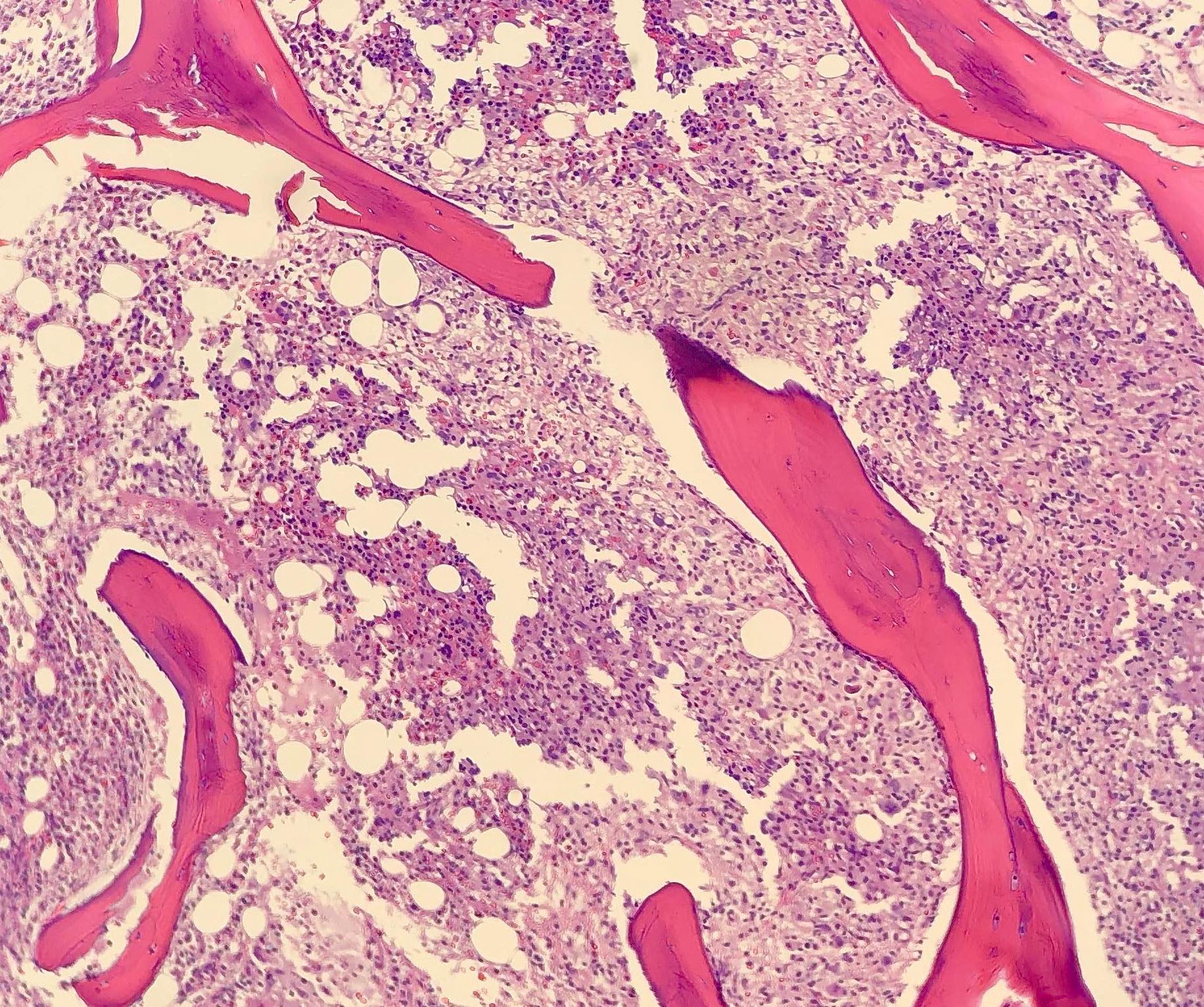
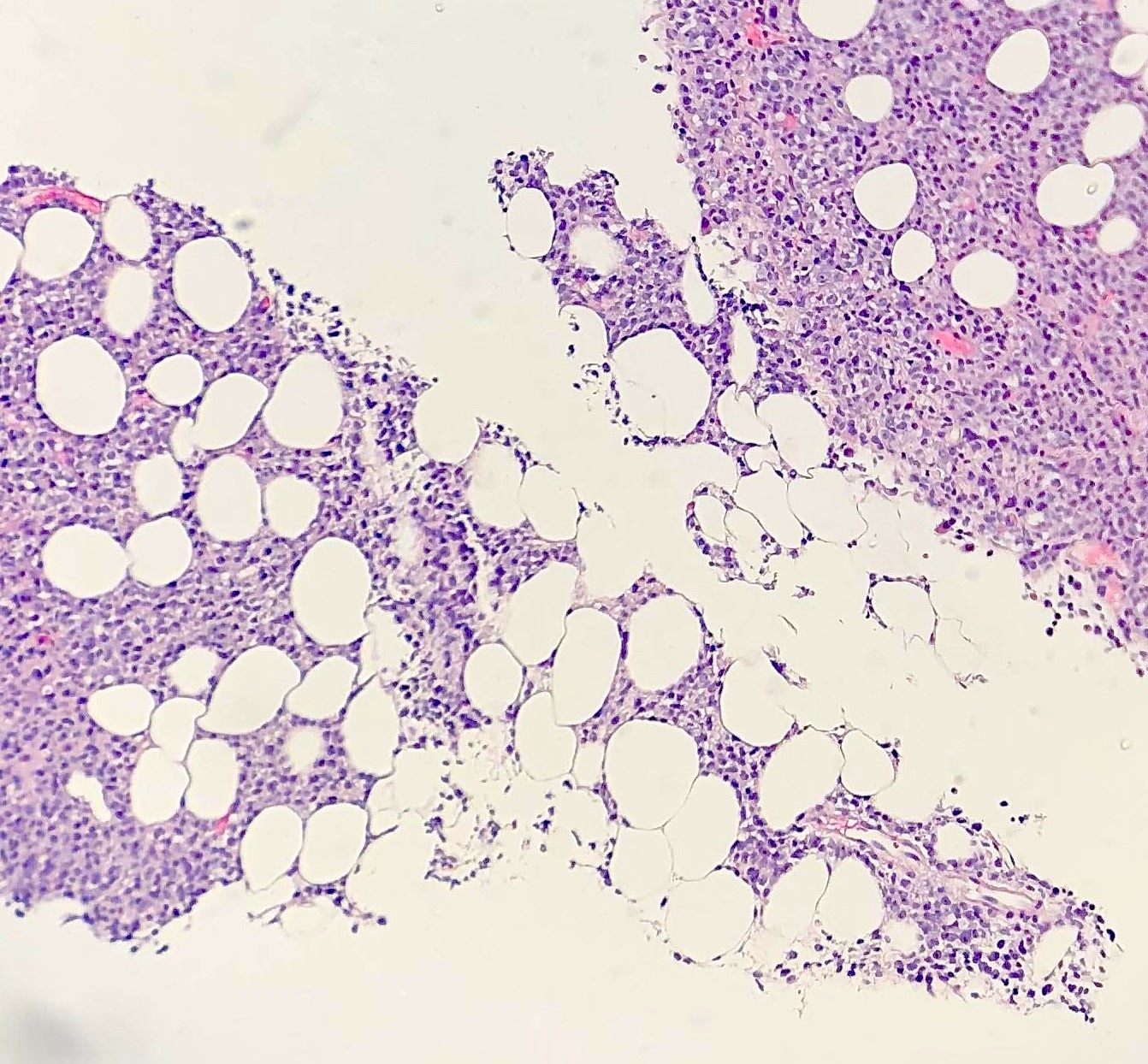
- Bone marrow involvement in 16% (J Clin Oncol 1998;16:2780)
Etiology
- May arise de novo or by transformation from a low grade lymphoma
Clinical features
- Rapidly enlarging mass (≥ 5 cm in 76% of cases) (J Clin Oncol 1998;16:2780)
- B symptoms (33%) (J Clin Oncol 1998;16:2780)
- Some asymptomatic
- May represent transformation of existing low grade B cell lymphoma (e.g., follicular lymphoma, marginal zone lymphoma, chronic lymphocytic leukemia [CLL] / small lymphocytic lymphoma [SLL], nodular lymphocyte predominant Hodgkin lymphoma)
Diagnosis
- Morphologic evaluation, immunophenotyping, cytogenetics (FISH) and clinical history
Laboratory
- ↑ Lactate dehydrogenase (LDH) (53%) (J Clin Oncol 1998;16:2780)
Prognostic factors
- Unfavorable prognostic features:
- Clinical: ↑ age, ↑ LDH, Eastern Cooperative Oncology Group (ECOG) ≥ 2, Ann Arbor stage III / IV, extranodal disease, bulky disease (J Clin Oncol 2010;28:2373, Blood 2014;123:837)
- Cell of origin status (Blood 2004;103:275):
- Activated B cell subtype (~40%) and germinal center B cell subtype (~60%) associated with 5 year progression free survival rates of 40 - 50% versus 70 - 80%, respectively
- MYC translocation (Blood 2015;126:2466)
- Double expresser status: immunohistochemical coexpression of MYC (≥ 40% tumor cells) and BCL2 (≥ 50% tumor cells) in the absence of co-occurring MYC and BCL2 rearrangements
- Bone marrow involvement associated with increased risk of CNS relapse
Case reports
- 50 year old man with chest pain (Blood 2019;133:882)
- 61 year old man with B symptoms and leukocytosis (Blood 2017;130:2233)
- 61 year old woman with a lung nodule (Onco Targets Ther 2020;13:5837)
- 63 year old man with dysphagia (Case Rep Oncol 2019;12:39)
- 67 year old man with ptosis and blurry vision (Oncol Lett 2020;20:285)
Treatment
- R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine and prednisone); other rituximab based regimens
Frozen section description
- Large atypical lymphoid cells with a diffuse growth pattern consistent with a large cell lymphoma can be appreciated on frozen sections; however, ancillary immunophenotypic and cytogenetic studies are required to establish B cell lineage and further differentiate specific DLBCL subtypes
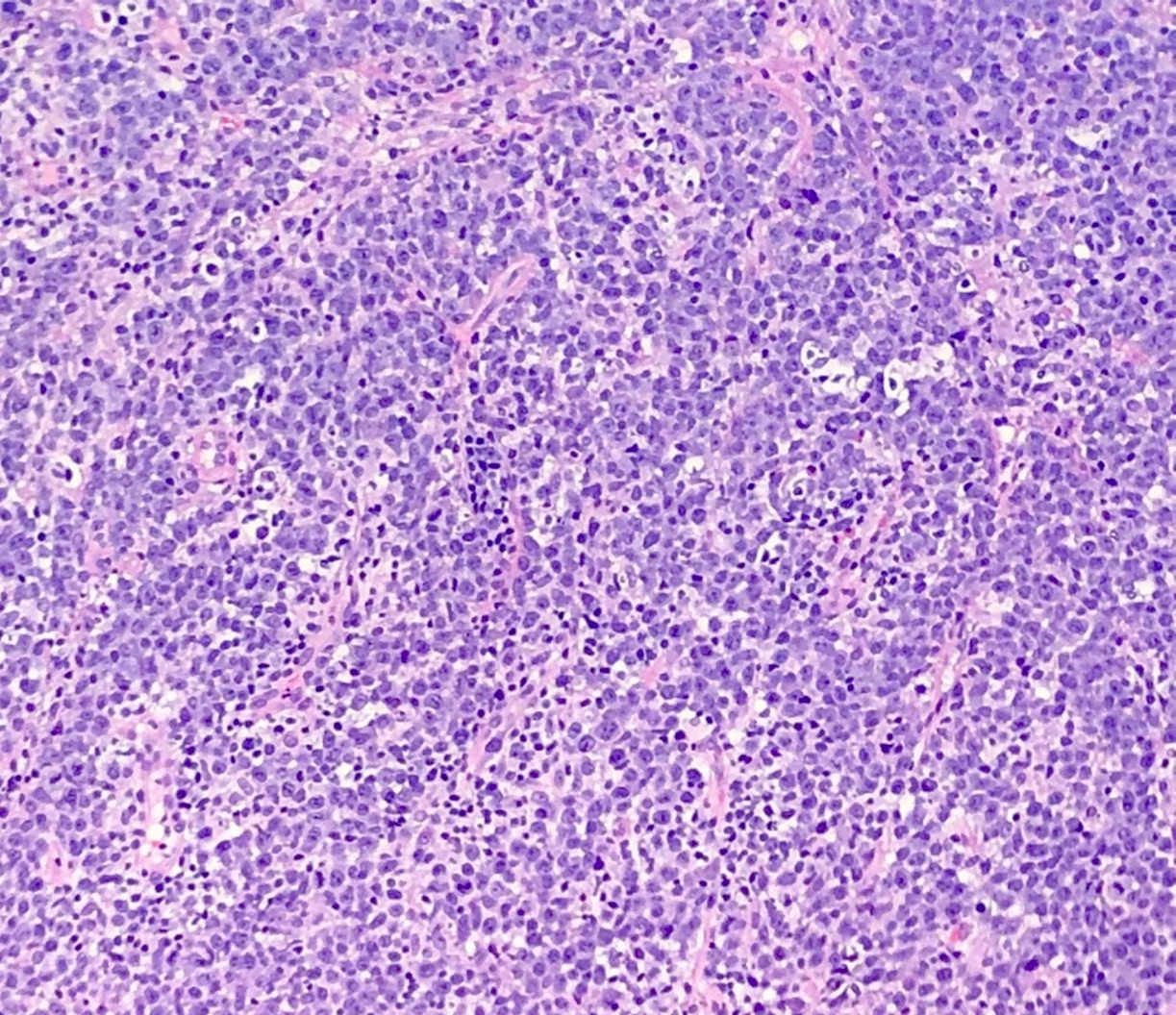
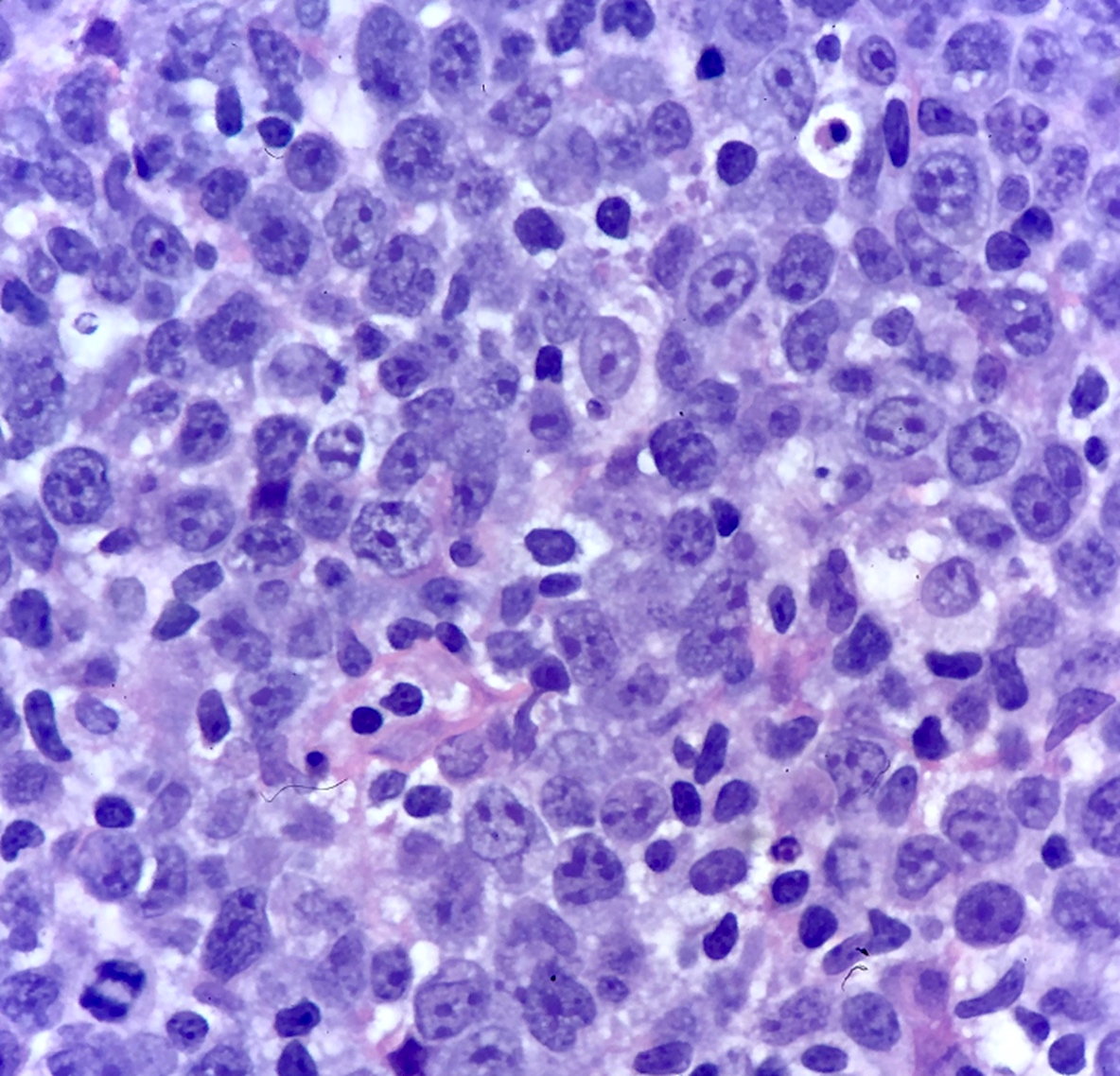
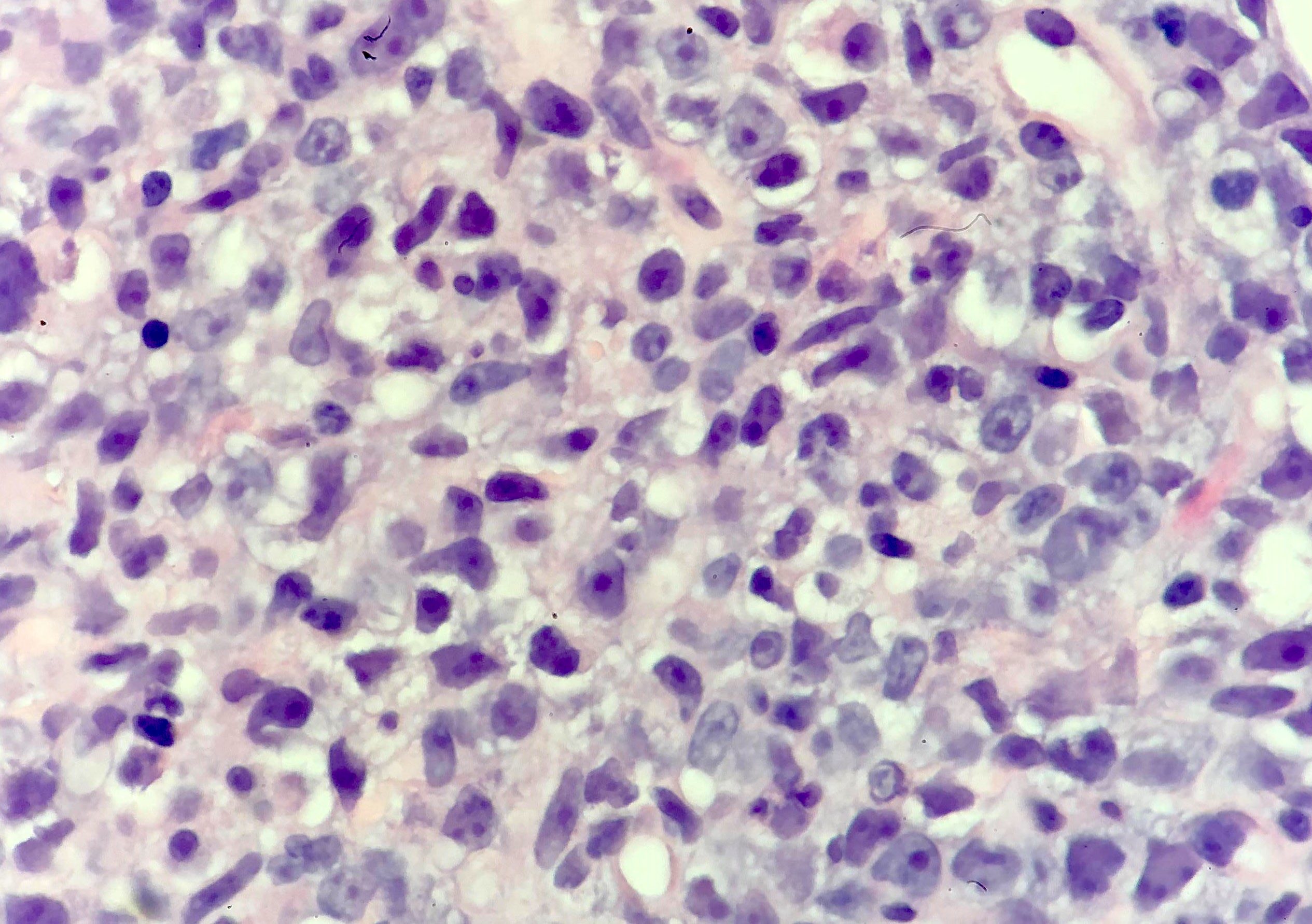
Microscopic (histologic) description
- Partial or complete effacement of normal tissue architecture by a diffuse infiltrate of large (or occasionally medium size) atypical B lymphoid cells with vesicular chromatin and prominent nucleoli
- Large is defined as nucleus size ≥ histiocyte nucleus or > 2 lymphocyte nuclei
- Morphologic variants:
- Immunoblastic variant: single central nucleolus
- Centroblastic variant: 2 - 4 nucleoli
- Anaplastic variant: anaplastic nuclei, can mimic anaplastic large cell lymphoma or Reed-Sternberg cells
Microscopic (histologic) images
Cytology description
- Cytologic evaluation can identify large atypical lymphoid cells with vesicular chromatin and prominent nucleoli, consistent with a large cell lymphoma; however, classification as DLBCL, NOS requires immunophenotypic and cytogenetic studies
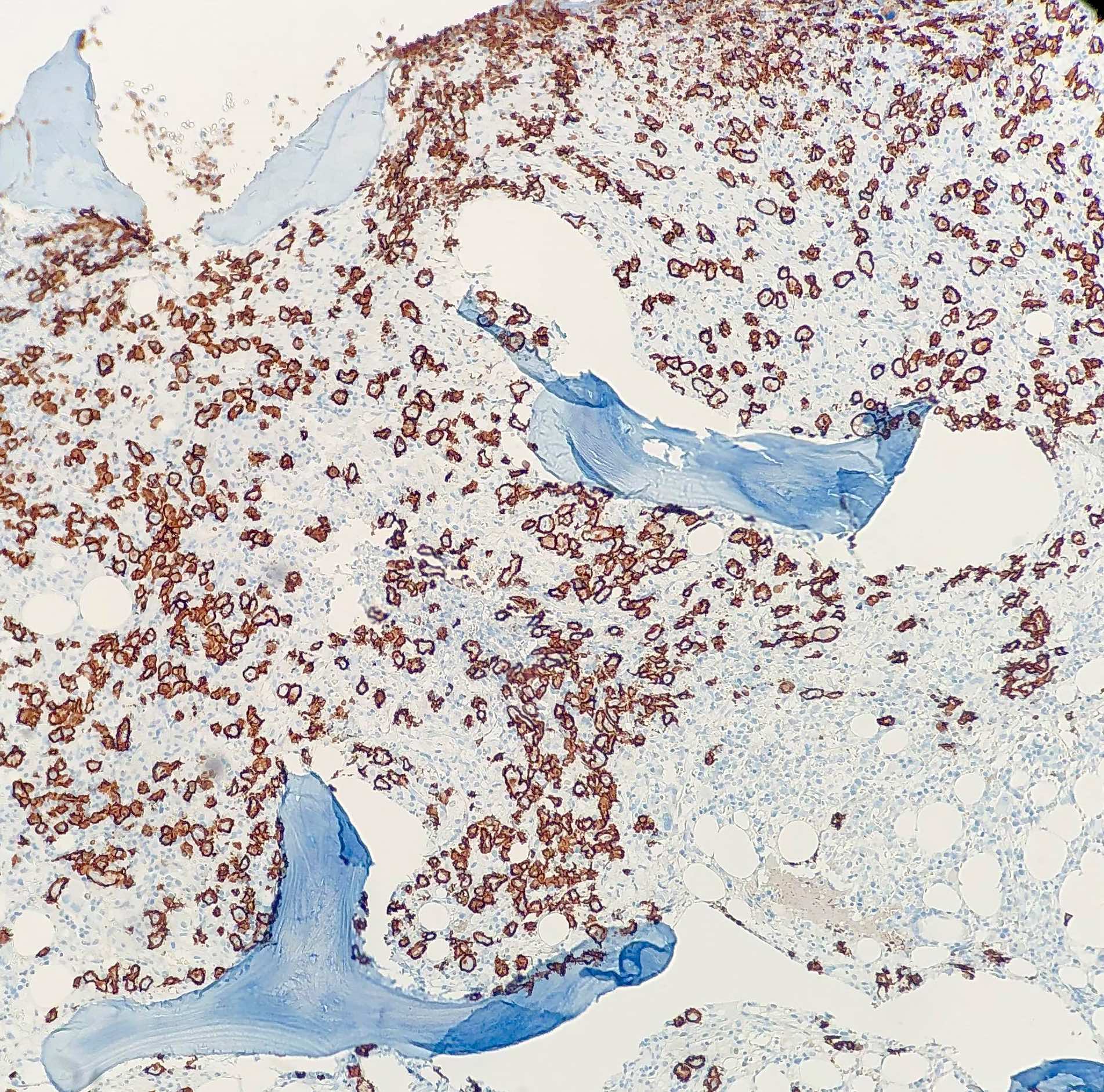
Positive stains
- B cell markers (CD20, PAX5, CD79a, CD19, CD22)
- Cell of origin subtyping: CD10 (30 - 50%), MUM1 (35 - 65%), BCL6 (60 - 90%)
- Evaluation of double expresser / possible double hit status: BCL2 (47 - 84%), MYC
- Ki67 (high)
- CD30 (14%), associated with anaplastic morphology (Blood 2013;121:2715)
- CD5 (12%) (Eur J Haematol 2017;98:415)
Negative stains
- CD3
- Cyclin D1 (98%); rare positive cases distinguished from mantle cell lymphoma by lack of t(11;14) and CD5 negativity (Cancer 2014;120:1818)
- TdT
- EBER ISH (DLBCL with > 80% EBER ISH positivity classified as EBV+ DLBCL, NOS)
- ALK (if positive, classified as ALK positive DLBCL) (J Clin Oncol 2009;27:4211)
Immunohistochemical subclassification
- Cell of origin subtype prediction by IHC using the Hans algorithm (positivity defined as staining in ≥ 30% of cells) (Blood 2004;103:275):
- Germinal center B cell (GCB) subtype: CD10+ or CD10- / BCL6+ / MUM1-
- Non-GCB subtype (classifier that encompasses ABC subtype and unclassifiable cases by GEP): CD10- / BCL6- or CD10- / BCL6+ / MUM1+
- Double expresser status (30% of DLBCL, NOS):
- Positive staining for BCL2 (> 50% tumor cells) and MYC (> 40% tumor cells) in the absence of underlying chromosomal rearrangements (double expresser) is associated with increased risk of CNS relapse and inferior survival (J Clin Oncol 2017;35:2515)
- If MYC and BCL2 rearrangements confirmed by FISH, classified as high grade B cell lymphoma with MYC and BCL2 rearrangements (also known as double hit DLBCL)
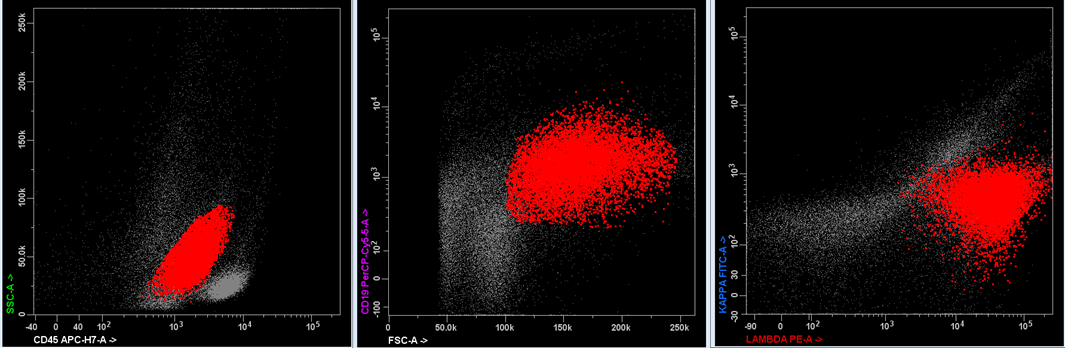
Flow cytometry description
- Flow cytometry shows a population of monoclonal B cells with high forward scatter (indicative of large size)
Molecular / cytogenetics description
- Gene expression profiling identifies activated B cell and germinal center B cell molecular subtypes of DLBCL, NOS
- Since gene expression profiling is not widely available in the clinical setting, immunohistochemical algorithms that approximate these molecular subtypes (i.e., Hans algorithm) are used as an alternative (see Immunohistochemical subclassification)
- FISH used to differentiate DLBCL, NOS from high grade B cell lymphoma with MYC and BCL2 and / or BCL6 rearrangements:
- BCL2 rearrangement (20 - 30%; < 5% activated B cell, 50% germinal center B cell)
- BCL6 rearrangement (30%; 30% activated B cell, 15% germinal center B cell)
- MYC rearrangement (8 - 14% for activated B cell and germinal center B cell; ~50% have co-occurring BCL2 or BCL6 rearrangement)
- PCR B cell gene rearrangement studies show clonal immunoglobulin gene rearrangement
- Mutational landscape very heterogeneous with recurrent alterations identified in over 150 genes
- Most frequently mutated genes include KMT2D (25%), MYD88 (17%), PIM1 (15%), CREBBP (12%), HIST1H1E (11%), BCL2 (10%), SPEN (10%), ARID1A (10%), TP53 (9%) (Cell 2017;171:481)
- Multiple integrative genomic classification models recently proposed but none currently incorporated into WHO classification guidelines (Cell 2017;171:481, N Engl J Med 2018;378:1396, Nat Med 2018;24:679, Blood 2020;135:1759)
- Common DLBCL genomic subtypes that have emerged from multiple independent studies include those characterized by:
- MYD88 L265P and CD79B mutations: mainly activated B cell subtype, 18q gain, genetically similar to primary extranodal lymphomas, poor survival
- BCL6 translocations and NOTCH2 mutations: mainly activated B cell subtype, constitutive B cell receptor signaling, genetically similar to marginal zone lymphoma, more favorable survival
- BCL2 translocations and mutations in EZH2 / other chromatin modifiers: mostly germinal center B cell subtype with genetic features similar to other B cell lymphomas of germinal center origin
- Common DLBCL genomic subtypes that have emerged from multiple independent studies include those characterized by:
Videos
Overview of histologic features
Sample pathology report
- Lymph node, left cervical, excisional biopsy:
- Diffuse large B cell lymphoma, NOS, GCB subtype (see comment)
- Comment: H&E sections show effacement of the normal nodal architecture by sheets of large atypical lymphoid cells with vesicular chromatin and prominent nucleoli. By immunohistochemistry, the tumor cells are positive for CD20, CD10 and BCL6, while negative for CD3, CD5, MUM1, BCL2, MYC and cyclin D1. EBER ISH is negative. The Ki67 proliferation index is 70%. Cytogenetic FISH studies are negative for rearrangements of BCL2, BCL6 and MYC. The morphologic, immunophenotypic and cytogenetic findings are diagnostic of diffuse large B cell lymphoma, NOS, GCB subtype (Hans algorithm).
Differential diagnosis
- High grade B cell lymphoma with MYC and BCL2 and / or BCL6 rearrangements:
- Co-occurring rearrangements of MYC and BCL2 and / or BCL6
- Mantle cell lymphoma, pleomorphic and blastoid variants:
- Burkitt lymphoma:
- Morphology: medium sized tumor cells, nonoverlapping round nuclei with paracentric nucleoli, starry sky background
- IHC: Ki67 ~100%, CD10 / BCL6 / MYC positive, BCL2 negative or weak
- MYC translocation with simple karyotype (by contrast, MYC rearranged DLBCL associated with complex karyotype)
- Endemic subtype EBV+
- Follicular lymphoma, grade 3:
- EBV positive DLBCL, NOS:
- > 80% lymphoma cells EBER ISH positive
- EBV positive mucocutaneous ulcer:
- Primary mediastinal (thymic) large B cell lymphoma:
- T cell / histiocyte rich large B cell lymphoma:
- Large B cells scattered (do not form clusters or sheets as in DLBCL) and limited in number (less than roughly 10% of cellularity)
- Background small B cells minimal to absent
- Primary CNS lymphoma:
- Primary site: brain, spinal cord, leptomeninges or eye
- Intravascular large B cell lymphoma:
- Localized to lumina of vessels
- Primary cutaneous DLBCL, leg type:
- Primary cutaneous disease, typically involving leg
- Lymphomatoid granulomatosis:
- Angiocentric / angiodestructive growth pattern, EBV+, > 90% involve lungs
- DLBCL associated with chronic inflammation:
- Involves body cavities with longstanding chronic inflammation (e.g., pleural cavity with pyothorax)
- HHV8 positive DLBCL, NOS:
- HHV8+, plasmablastic morphology, IgM lambda, often associated with multicentric Castleman disease
- ALK positive large B cell lymphoma:
Additional references
Board review style question #1
A 60 year old man presents with an inguinal mass and recent onset of B symptoms. H&E sections of a core needle biopsy of the mass show sheets of large, pleomorphic lymphoid cells with vesicular chromatin and prominent nucleoli. By immunohistochemistry, the tumor cells are positive for CD20, CD5, CD10, BCL6 and MYC, while negative for CD3, MUM1, BCL2, SOX11 and cyclin D1. EBER ISH is negative. The Ki67 proliferation index is 90%. FISH studies are negative for rearrangements of BCL2, BCL6 and MYC. This lymphoma is best classified as
- Mantle cell lymphoma, pleomorphic subtype
- Burkitt lymphoma
- Diffuse large B cell lymphoma, NOS, with germinal center B cell phenotype
- Diffuse large B cell lymphoma, NOS, with nongerminal center B cell phenotype, with double expression of MYC and BCL6
- Diffuse large B cell lymphoma, NOS, with nongerminal center B cell phenotype
Board review style answer #1
C. Diffuse large B cell lymphoma, NOS, germinal center B cell subtype. Negative cyclin D1 and SOX11 IHC virtually rules out mantle cell lymphoma (answer A). Burkitt lymphoma is composed of intermediate size cells with round nuclei which lack significant pleomorphism and have a Ki67 proliferation index of approximately 100% (answer B). Coexpression of MYC and BCL2 (not BCL6) has been associated with inferior clinical outcomes and should be noted in the report (answer D). Co-occurring rearrangements of BCL6 and MYC would support the diagnosis of high grade B cell lymphoma with MYC and BCL2 and / or BCL6 rearrangements. The morphologic, immunophenotypic and cytogenetic findings are diagnostic of DLBCL, NOS, with a germinal center B cell phenotype (answer C). Per the Hans algorithm, CD10 positivity in DLBCL is predictive of a germinal center B cell subtype gene expression profile. Nongerminal center B cell phenotype: CD10- / BCL6- or CD10- / BCL6+ / MUM1+ (answer E).
Comment Here
Reference: DLBCL, NOS
Comment Here
Reference: DLBCL, NOS
Board review style question #2
A 65 year old woman presents with a rapidly enlarging neck mass. H&E sections of a core needle biopsy of the mass show sheets of large atypical lymphoid cells with vesicular chromatin and prominent nucleoli which by immunohistochemistry are positive for CD20. Which of the following immunohistochemical findings would support the diagnosis of diffuse large B cell lymphoma, NOS?
- Cyclin D1+
- ALK+
- TdT+
- CD21-
- BCL6-
Board review style answer #2
D. CD21-. CD21 marks follicular dendritic cell meshworks, the absence of which is a characteristic feature of DLBCL.
Positive cyclin D1 typically supports the diagnosis of mantle cell lymphoma (answer A).
ALK expression does not support the diagnosis of DLBCL, NOS (answer B). It is, however, a defining feature of the ALK+ large B cell lymphoma, which is also characteristically CD20 negative.
TdT is an immaturity marker characteristically expressed in acute lymphoblastic leukemia (answer C). Although high grade mature B cell lymphomas can on very rare occasion exhibit TdT expression, this finding does not support the diagnosis of DLBCL).
BCL6 is a germinal center marker used in the Hans algorithm to predict cell of origin status (answer E).
Comment Here
Reference: DLBCL, NOS
Comment Here
Reference: DLBCL, NOS