Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Xu B. HPV related multiphenotypic sinonasal carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/HPVrelatedmultiphenotypiccarcinoma.html. Accessed April 3rd, 2025.
Definition / general
- Unique type of carcinoma characterized by its association with high risk human papillomavirus (HPV, in particular type 33), exclusive sinonasal location and mixed histologic phenotype (resembling both adenoid cystic carcinoma and squamous cell carcinoma)
Essential features
- Located exclusively within the sinonasal tract
- Positive for HPV, in particular type 33 and negative for MYB / MYBL1 / NFIB translocation
- Exhibits various histologic features, including areas that resemble adenoid cystic carcinoma, squamous cell carcinoma, carcinoma with basaloid appearance
Terminology
- HPV related sinonasal carcinoma with adenoid cystic carcinoma-like features
ICD coding
- Newly described in 2013 and does not have its own ICD code (Am J Surg Pathol 2013;37:185)
- Included in the current WHO classification as a provisional entity under sinonasal nonkeratinizing squamous cell carcinoma
- ICD-0: 8072/3 - squamous cell carcinoma, large cell, nonkeratinizing, NOS
Epidemiology
- Age of initial presentation: from 28 - 90 (mean age: 54)
- M:F = 1:1.6 (Am J Surg Pathol 2017;41:1690)
Sites
- Occurs exclusively in the sinonasal tract (Am J Surg Pathol 2017;41:1690)
- Approximately 57% affects nasal cavity, 10% paranasal sinus and the rest affects both sites
- Involvement of adjacent sites, e.g. lacrimal duct, cranial fossa and orbit, is rare but has been reported (Arch Pathol Lab Med 2019 Mar 6 [Epub ahead of print])
Etiology
- High risk HPV is detected in all reported cases (Am J Surg Pathol 2017;41:1690)
- HPV type 33 detected in 68% of cases; other uncommon HPV types are 35 (6% of cases), 56, 16, 52 and 26 (Head Neck Pathol 2018 Sep 26 [Epub ahead of print])
Clinical features
- Usually present with nonspecific symptoms, e.g. nasal congestion, discharge, nasal obstruction, epistaxis and pain
Radiology description
- Locally destructive mass involving nasal cavity or paranasal sinus (AJNR Am J Neuroradiol 2019;40:584)
Prognostic factors
- No known prognostic factor
- Overall appears to be more indolent than sinonasal squamous cell carcinoma
- Based on the reported cases
- Associated with high frequency (36%) of local recurrence, including late local recurrence decades after the initial surgery (J Pathol Transl Med 2019 Apr 25 [Epub ahead of print], Head Neck Pathol 2018;12:623)
- Distant metastases are rare, occurring in 5% of patients 8 - 17 years after the initial resection
- No reported case with regional lymph node metastasis (Am J Surg Pathol 2017;41:1690)
Case reports
- 36 year old woman with nasal cavity mass that recurred 33 years after the initial resection (Head Neck Pathol 2018;12:623)
- 48 year old woman with epistasis and a nasal cavity mass (Head Neck Pathol 2018 Sep 26 [Epub ahead of print])
- 66 year old man with a polypoid lesion in the right nasal cavity (J Pathol Transl Med 2019 Apr 25 [Epub ahead of print])
Treatment
- Knowledge on the appropriate treatment for this rare tumor is limited; based on the reported cases (Am J Surg Pathol 2017;41:1690):
- Surgical resection with appropriate margin is the main treatment approach
- Approximately 40% of patients also receive adjuvant radiation therapy
- Given the reported negligible risk of regional lymph node metastasis and low risk of distant metastasis, routine regional lymph node dissection or chemotherapy may not be indicated
- Late local recurrence and distant metastasis may occur, therefore long term clinical follow up may be warranted
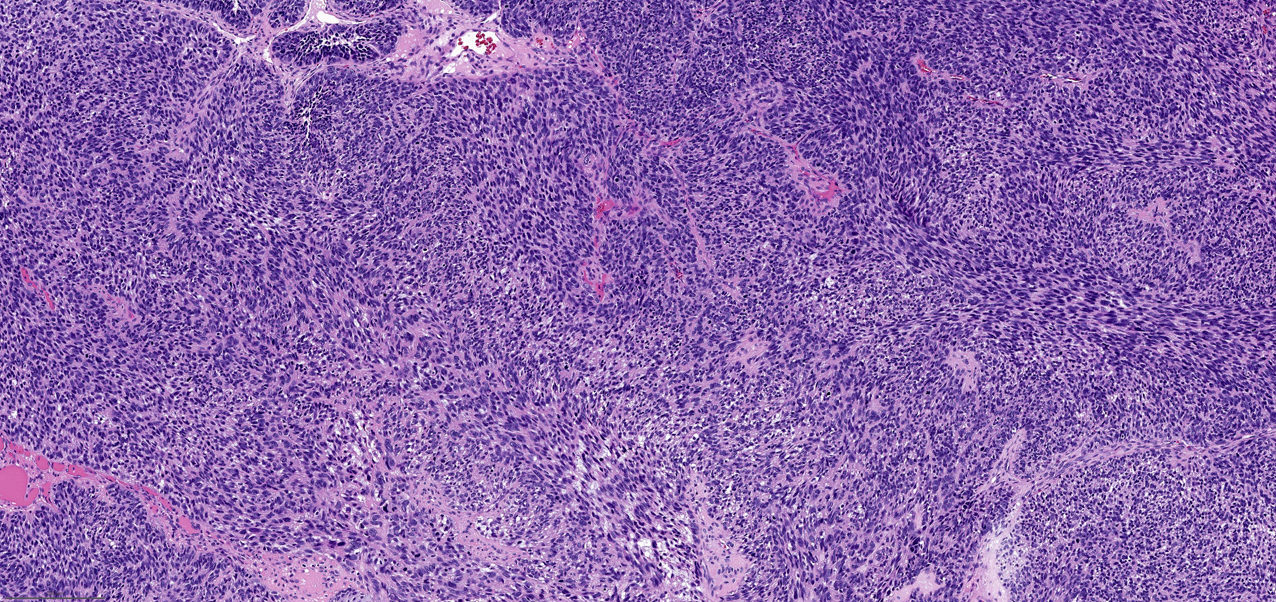
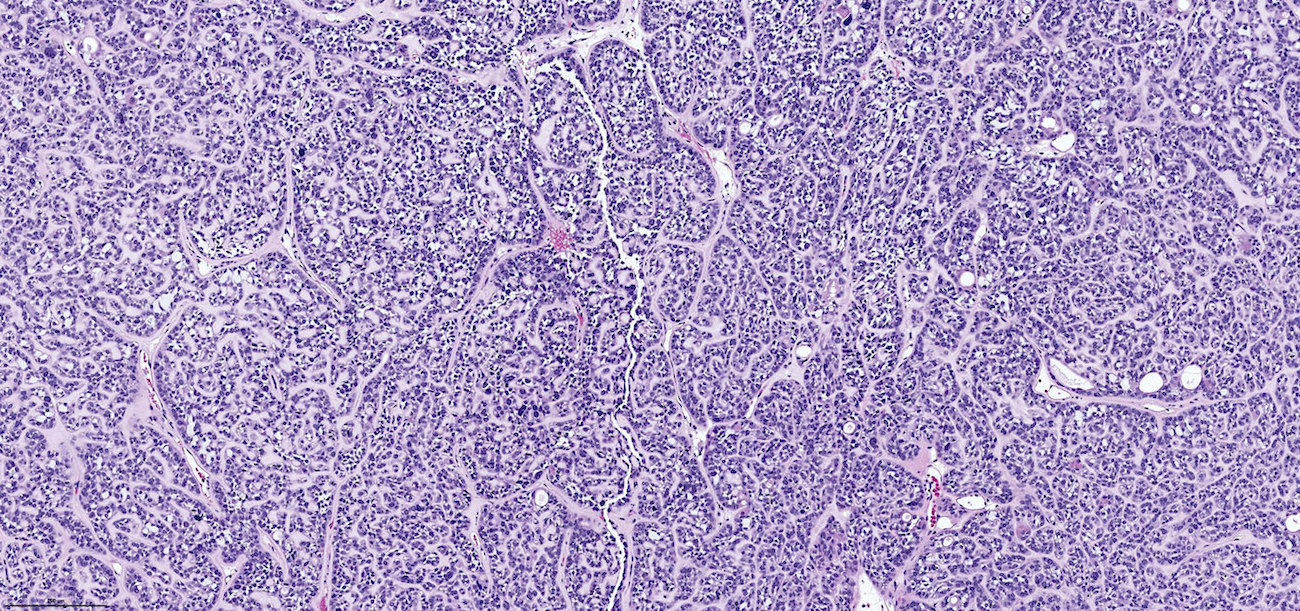
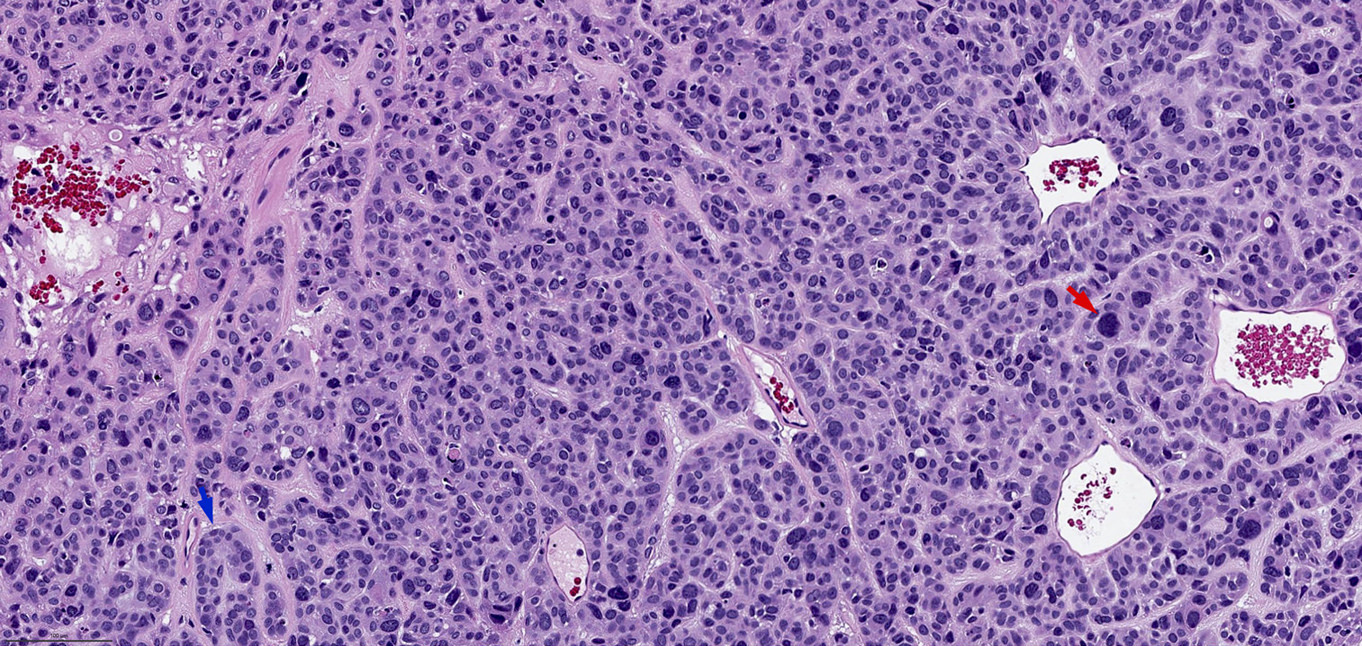
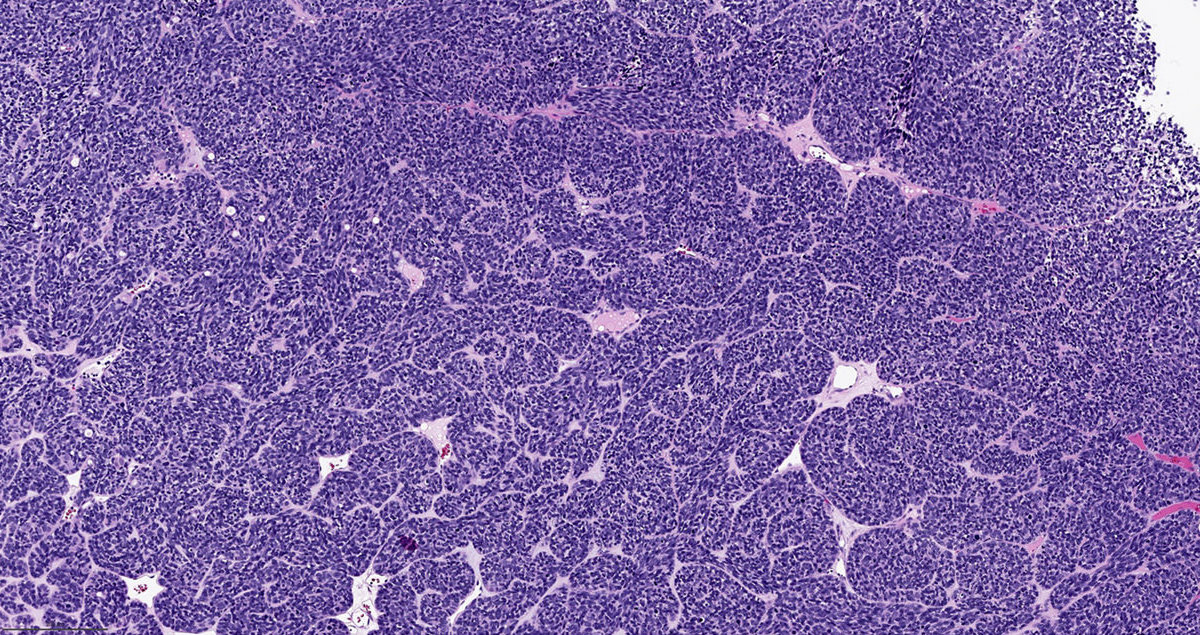
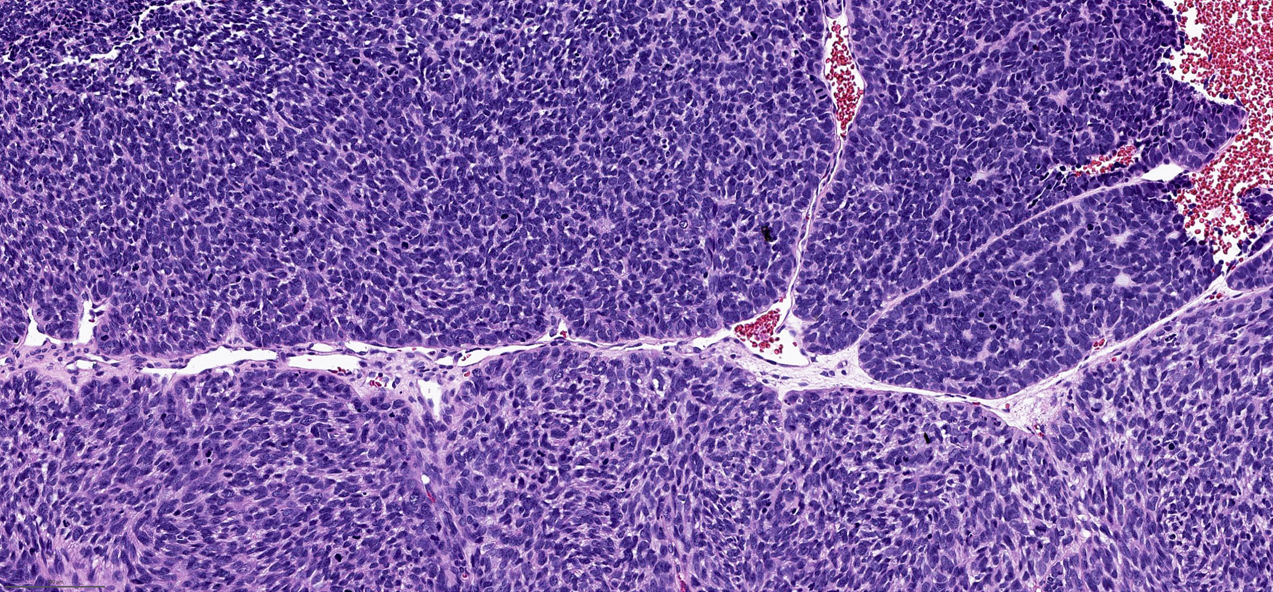
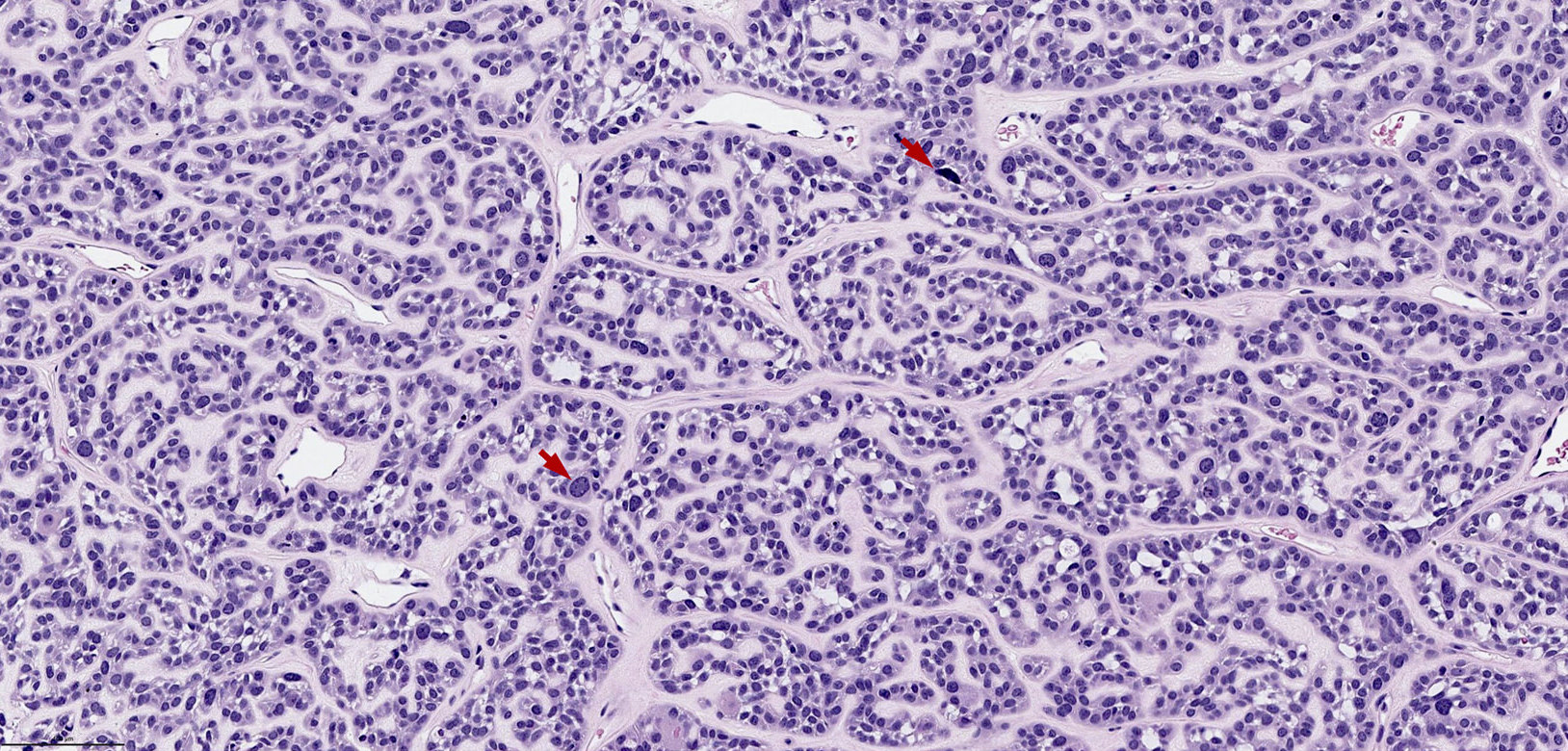
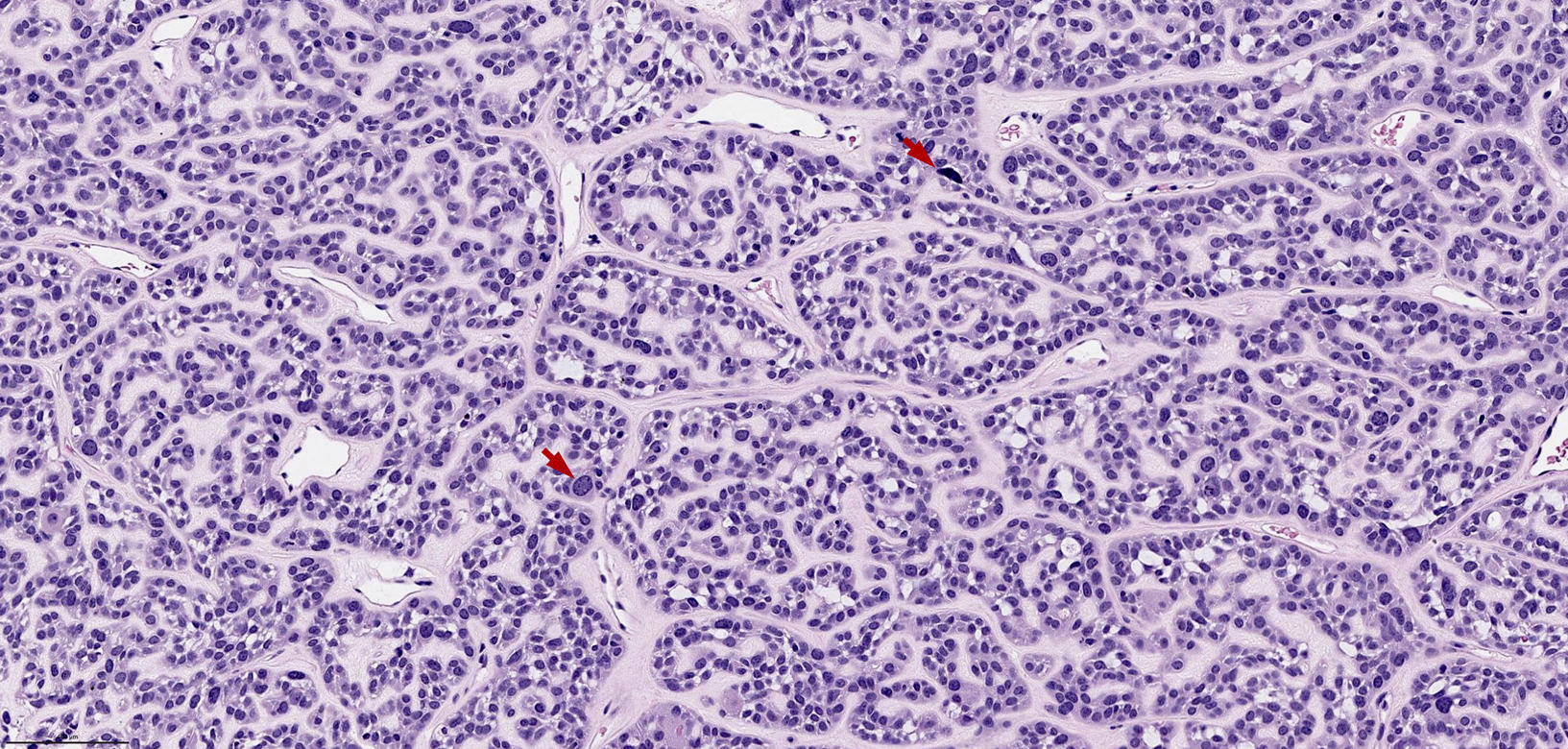
Microscopic (histologic) description
- Typical microscopic features include:
- Areas resemble adenoid cystic carcinoma of salivary gland origin, e.g. tubular, cribriform and solid architecture
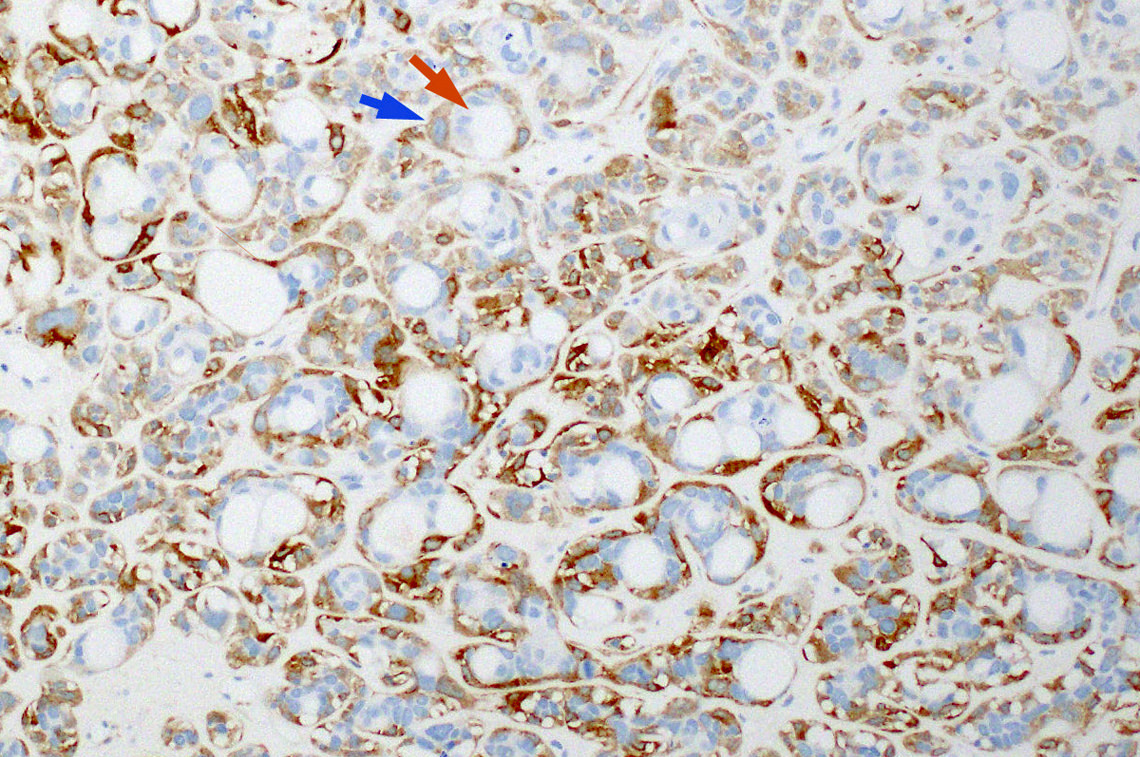
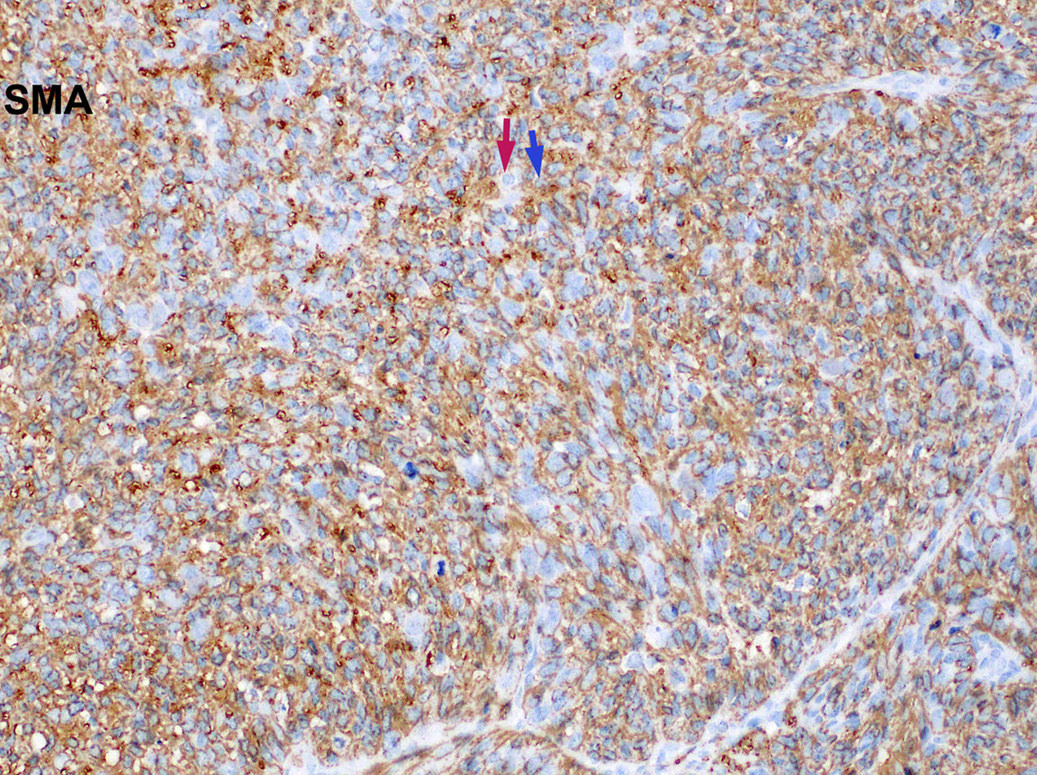
- Biphasic ductal and myoepithelial differentiation may be evident on H&E and on immunostain for myoepithelial markers (e.g. calponin, S100, SOX10 and smooth muscle actin)
- Areas showing definite squamous differentiation may be seen in the forms of true keratinization, keratin pearls and intracellular bridges
- Focally, the tumor may show basaloid features resembling cylindroma with peripheral palisading and high nuclear to cytoplasmic ratio, as well as tumor forming solid nests and lobules separated by hyalinized fibrous bands
- Surface involvement with marked nuclear pleomorphism may be seen in about 70% of cases
- At high power, typically shows randomly distributed tumor cells with marked nuclear pleomorphism and hyperchromasia
- Other rare features that may be seen
- Areas with pure sarcomatoid / spindle cell proliferation with or without dilated staghorn shaped vasculature
- Heterologous mesenchymal component e.g. chondroid or osseous differentiation
Microscopic (histologic) images
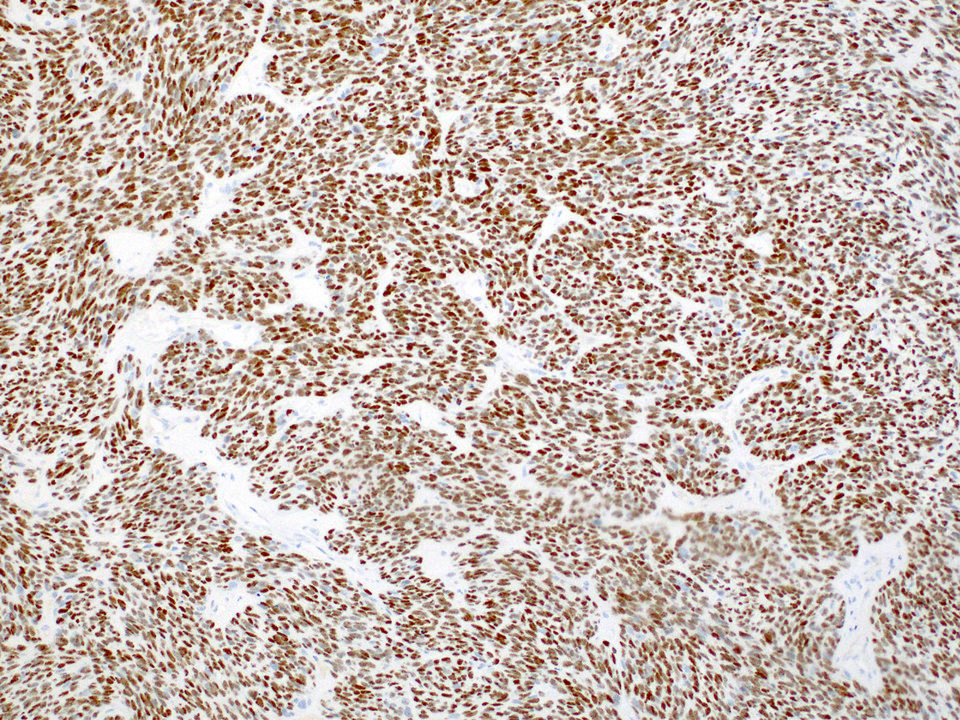
Positive stains
- p16 consistently shows diffuse and strong nuclear and cytoplasmic staining
- Myoepithelial differentiation by immunohistochemistry, i.e. it is typically positive for myoepithelial markers, e.g. calponin, S100 and smooth muscle actin
- Also shows squamous differentiation by immunohistochemistry, i.e. it is typically positive for p40, p63 and high molecular weight cytokeratin (e.g. CK5 / 6 and 34βE12)
- MYB immunohistochemistry can be positive (although negative for MYB fusion by FISH) (Head Neck Pathol 2019;13:220)
- INI1 (retained)
Negative stains
- Melanocytic markers, e.g. melanA and HMB45
- Neuroendocrine markers, e.g. synaptophysin, chromogranin and INSM1
Molecular / cytogenetics description
- All reported cases are positive for high risk HPV using various detection methods, e.g. DNA in situ hybridization (ISH), RNA ISH and PCR based essays
- EBV ISH (EBER)
- Does not have any characteristic molecular or cytogenetic findings
- Consistently negative for fusions characteristics for adenoid cystic carcinoma, e.g. MYB, MYBL1 and NFIB (Am J Surg Pathol 2017;41:1690)
Sample pathology report
- Nasal cavity, left, resection:
- HPV related multiphenotypic sinonasal carcinoma (see comment)
- Comment: The tumor shows biphasic differentiation with ductal and myoepithelial cells arranged as tubular, cribriform and solid architecture. There are scattered tumor cells with marked nuclear pleomorphism. There is surface involvement. Immunohistochemistry studies show that the tumor is positive for S100, SMA, calponin and p16 (diffuse and strong nuclear and cytoplasmic). RNA in situ hybridization for high risk HPV is positive in this tumor. The overall histologic features and immunophenotype are consistent with the above diagnosis. In the current WHO classification (4th edition), HPV related multiphenotypic sinonasal carcinoma is considered as a provisional diagnosis in the category of sinonasal squamous cell carcinoma (Am J Surg Pathol 2017;41:1690).
Differential diagnosis
- Adenoid cystic carcinoma:
- No confirmed association with HPV infection (Am J Surg Pathol 2017;41:1422)
- 60 - 80% positive for MYB / MYBL1 / NFIB translocation
- Both HPV related multiphenotypic sinonasal carcinoma and adenoid cystic carcinoma can show
- Biphasic differentiation with ductal and myoepithelial elements
- Immunopositivity for myoepithelial markers (e.g. calponin, smooth muscle actin and S100)
- Tubular, cribriform and solid architecture
- Squamous differentiation (in adenoid cystic carcinoma with high grade transformation) (Am J Surg Pathol 2007;31:1683)
- Sinonasal squamous cell carcinoma:
- 15 - 30% can be positive for high risk HPV (Am J Surg Pathol 2013;37:185)
- Lacks biphasic or myoepithelial differentiation by histology and immunohistochemistry
- Both tumors can have squamous differentiation
- SMARCB1 deficient sinonasal carcinoma:
- Sinonasal undifferentiated carcinoma (SNUC):
- HPV negative
- Diagnosis of exclusion, i.e. the diagnosis can only be made when any specific diagnostic entity (e.g. HPV related multiphenotypic sinonasal carcinoma) has been excluded
Board review style question #1
A 45 year old man is present with a nasal cavity mass. A representative H&E of the mass is shown in the picture. Which of the following statements is true?
- Differential diagnoses include adenoid cystic carcinoma of salivary gland origin and HPV related multiphenotypic sinonasal carcinoma
- Tumor is consistently negative for myoepithelial markers, e.g. SMA, calponin and S100
- Tumor may be positive for EBV
- 80% are positive for EWSR1 fusion
Board review style answer #1
A. Differential diagnoses include adenoid cystic carcinoma of salivary gland origin and HPV related multiphenotypic sinonasal carcinoma
Comment here
Reference: HPV related multiphenotypic sinonasal carcinoma
Comment here
Reference: HPV related multiphenotypic sinonasal carcinoma
Board review style question #2
Which of the following statements is true for HPV related multiphenotypic sinonasal carcinoma?
- May contain areas resembling adenoid cystic carcinoma
- May show neuroendocrine differentiation
- Related with low risk HPV, e.g. type 6 and 11
- Typically negative for p40, p63 and high molecular weight cytokeratin
Board review style answer #2
A. May contain areas resembling adenoid cystic carcinoma
Comment here
Reference: HPV related multiphenotypic sinonasal carcinoma
Comment here
Reference: HPV related multiphenotypic sinonasal carcinoma
Back to top